Turning a breech baby naturally
What Can I Do if My Baby is Breech?
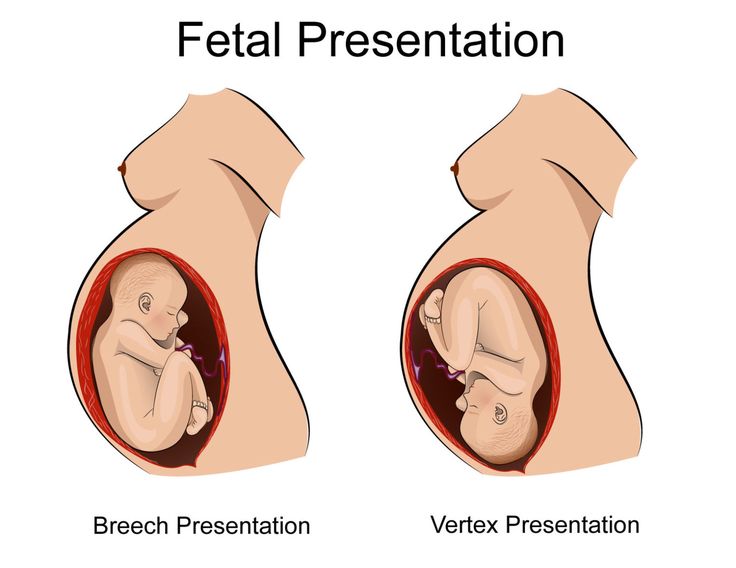
Right before birth, most babies are in a headfirst position in the mother’s uterus. Sometimes, the baby is in a bottom-first (or feet-first) position. This is called a breech birth or breech baby. Babies can be breech early in pregnancy. Most of them turn on their own to be headfirst by the time of delivery. As you get closer to your due date, your doctor will be able to tell if your baby is breech. They can check by a physical exam, ultrasound, or both.
Breech babies are more likely in these cases:
- Early, or premature births
- Multiple births (two or more babies)
- An abnormal level of amniotic fluid
- An abnormal shaped uterus
It’s important to see your doctor regularly throughout your pregnancy. Your doctor can tell if your baby is breech and help plan what to do. There are several ways to try and turn your baby. Your doctor may suggest methods to help turn the baby naturally. These could be the first attempt if it is still early and there are no health problems or concerns. Another option is to do a procedure called external cephalic version (ECV). Or your doctor may want to schedule a cesarean delivery (C-section).
ECV is one way to turn a baby from breech position to head down position while it’s still in the uterus. The doctor will apply pressure to your stomach to turn the baby from the outside. Sometimes, they use ultrasound as well.
Many women who have normal pregnancies can have ECV. You should not have ECV if you have:
- Vaginal bleeding
- A placenta that is near or covering the opening of the uterus
- A low level of fluid in the sac that surrounds and protects the baby
- An abnormal fetal heart
- Premature rupture of the membranes
- Twins or other multiples pregnancy
ECV usually is done in a hospital toward the end of pregnancy, around 37 weeks. Before the procedure, the doctor will do an ultrasound to confirm that your baby is breech. They also will monitor your baby’s heart rate to make sure it is normal. The doctor may give you medicine to relax the muscles in your uterus. This can help decrease discomfort and increase the success of turning your baby. The medicine may be given as a shot or through a vein (IV). It is very safe, with no risk to your baby.
Before the procedure, the doctor will do an ultrasound to confirm that your baby is breech. They also will monitor your baby’s heart rate to make sure it is normal. The doctor may give you medicine to relax the muscles in your uterus. This can help decrease discomfort and increase the success of turning your baby. The medicine may be given as a shot or through a vein (IV). It is very safe, with no risk to your baby.
During the ECV, you will lie down and the doctor will place their hands on your stomach. After locating the baby’s head, the doctor will gently try to turn the baby to the headfirst position.
After the procedure, your doctor will monitor your baby’s heart rate again. If the procedure is successful, you shouldn’t have to stay in the hospital. Your chance of having a normal vaginal delivery is high. However, there is a chance that the baby can turn back around to the breech position. The success rate of ECV depends on several factors:
- How close you are to your due date
- The amount of fluid around your baby
- How many pregnancies you have had
- The weight of your baby
- How the placenta is positioned
- The position of your baby
If the procedure is not successful, your doctor will talk to you about delivery. They will discuss the pros and cons of having a vaginal delivery or a C- section. The doctor may suggest repeating the ECV.
They will discuss the pros and cons of having a vaginal delivery or a C- section. The doctor may suggest repeating the ECV.
The risks of ECV are small, but include:
- Early onset labor
- Premature rupture of the membranes
- Minor blood loss for either the baby or the mother
- Fetal distress leading to an emergency C-section
Some people look to natural ways to try and turn their baby. These methods include exercise positions, certain stimulants, and alternative medicine. They may help but there is no scientific evidence that they work.
- Breech tilt, or pelvic tilt: Lie on the floor with your legs bent and your feet flat on the ground. Raise your hips and pelvis into a bridge position. Stay in the tilt for about 10 to 20 minutes. You can do this exercise three times a day. It may help to do it at a time when your baby is actively moving in your uterus.
- Inversion: There are a few moves you can do that use gravity to try and turn the baby.
 They help relax your pelvic muscles and uterus. One option is to rest in the child’s pose for 10 to 15 minutes. A second option is to gently rock back and forth on your hands and knees. You also can make circles with your pelvis to promote activity.
They help relax your pelvic muscles and uterus. One option is to rest in the child’s pose for 10 to 15 minutes. A second option is to gently rock back and forth on your hands and knees. You also can make circles with your pelvis to promote activity. - Music: Certain sounds may appeal to your baby. Place headphones or a speaker at the bottom of your uterus to encourage them to turn.
- Temperature: Like music, your baby may respond to temperature. Try placing something cold at the top of your stomach where your baby’s head is. Then, place something warm (not hot) at the bottom of your stomach.
- Webster technique: This is a chiropractic approach. It is meant to align your pelvis and hips and relax your uterus. The goal is to encourage your baby to turn.
- Acupuncture: This is a form of Chinese medicine. It involves placing needles at pressure points to balance your body’s energy. It may help relax your uterus and stimulate your baby’s movement.

It is not always possible to turn your baby from being breech. Some breech babies can be safely delivered through the vagina, but usually doctors deliver them by C-section. Risks involved with a C-section include bleeding and infection. There also can be a longer hospital stay for both the mother and her baby.
Other risks can occur for breech babies who are born vaginally. These include:
- Injuries during or after delivery
- Separation of the baby’s hip socket and thigh bone
- Problems with the umbilical cord. For example, the umbilical cord can be flattened during delivery. This can cause nerve and brain damage due to a lack of oxygen.
- How can I tell if my baby is breech?
- If my baby is breech, does it mean there is something wrong with them?
- What are the benefits and risks of ECV?
- What are my options for delivery if my baby remains in the breech position?
- What are the health risks to my baby and me if they are born breech?
Copyright © American Academy of Family Physicians
This information provides a general overview and may not apply to everyone. Talk to your family doctor to find out if this information applies to you and to get more information on this subject.
Talk to your family doctor to find out if this information applies to you and to get more information on this subject.
Techniques for Turning a Breech Baby Naturally
Flipping a breech baby is your best chance for a natural birth. Here’s are 8 proven techniques for turning a breech baby naturally and safely.
Is your baby breech? (If you’re not sure, check out this post!) While many women dread learning this, know that you have options when it comes to turning a breech baby. First off, delivering a breech baby is not impossible. For centuries, women had no other choice and doctors were trained to deliver breech babies. You can read more about the risks and options with a breech baby delivery here.
However, with the invention of modern medicine, U.S. hospitals choose to err on the side of caution by, in most instances, mandating breech babies be delivered via cesarean. The trend in the U.S., as well as other countries like Ireland, shows that 9 out of 10 breech babies are delivered via cesarean. This means approximately 140,000 [U.S.] babies each year face being delivered via C-section simply because they present as breech at the onset of labor.
This means approximately 140,000 [U.S.] babies each year face being delivered via C-section simply because they present as breech at the onset of labor.
If you desire to experience natural childbirth, it is imperative to have baby in the head-down position, and if necessary, finding safe methods of turning a breech baby.
Before We Start: A Special Gift for You
I cover a ton of material in this post. Want a really simple one-pager?
Download my cheat sheet on How to Turn a Breech Baby.
Techniques for Turning a Breech Baby
Okay so you’ve been doing the daily optimal baby positioning exercises. You’re past 30 weeks… and baby is still breech! Now what? Here is a list of self-care and professional techniques that can help flip your baby:
Hypnobabies
Hypnobabies is an MP3 series that offers various types of proven medical hypnosis techniques to create peaceful, relaxing, and more comfortable pregnancy and birth. Some call it “hypno-birthing.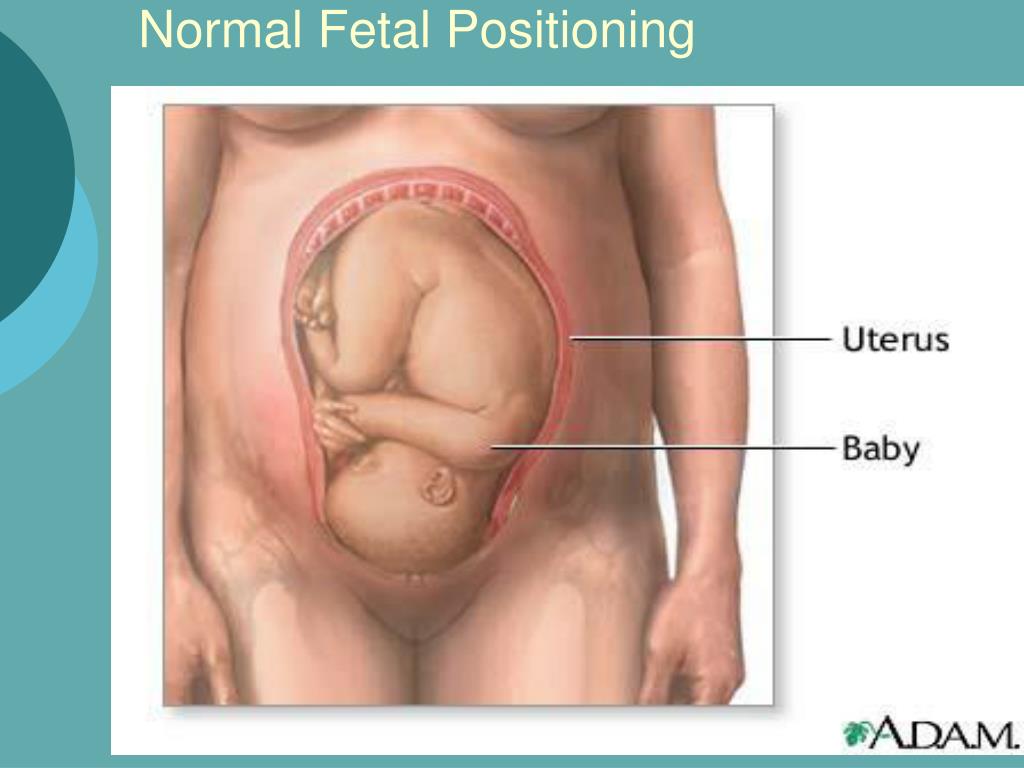 ” They have one specifically for turning a breech baby entitled, “Turn Baby Turn.” It’s a mere $15-$20, and money well spent. I LOVED this technique! It was my favorite hands-down. It was so healing. It bonded me with my baby exponentially. I can’t say enough about this technique. It created a profound and peaceful connection between me and Griffin, ensuring an optimal and loving unison throughout the flipping process. It’s a great technique to create calm and reduce anxiety, for both.
” They have one specifically for turning a breech baby entitled, “Turn Baby Turn.” It’s a mere $15-$20, and money well spent. I LOVED this technique! It was my favorite hands-down. It was so healing. It bonded me with my baby exponentially. I can’t say enough about this technique. It created a profound and peaceful connection between me and Griffin, ensuring an optimal and loving unison throughout the flipping process. It’s a great technique to create calm and reduce anxiety, for both.
Breech tilt
This technique is like the Bridge Pose in Yoga. If you are not sure the position of your baby, DO NOT do this technique. Just as it can aid in turning a breech baby head down, it could also inadvertently turn a head-down baby to a breech baby.
Inversion
This technique is like a Yoga downward facing dog with extra support. You’ll need a chair or couch to kneel on. Make sure the first couple times you try this you have someone nearby supporting you, as it is an awkward position. I did this technique a couple of times when trying techniques for turning a breech baby.
I did this technique a couple of times when trying techniques for turning a breech baby.
With a trained doula or midwife, you can take your chest-to-floor inversion up a notch with a rebozo wrap. A rebozo is a Mexican shawl that is often used for babywearing that can also be used to help turn a breech baby by supporting the hips. Watch Mexican midwife Naoli Vinaver demonstrate how here:
As demonstrated above, Naoli Vinaver is knowledgable in many techniques for flipping a baby. As the founder of Luz de Luna Home Birth Services, Vinaver is no stranger to helping mamas achieve natural, empowered births. In addition to the rebozo inversion, Vinaver also advocates for other positions including breech tilt and wide crawling, as seen in the image below. You can also learn more about Naoli’s teachings here.
You can also learn more about Naoli’s teachings here.
Water handstand
Some folks recommend you go to a nearby pool because water increases amniotic fluid. More room, more movement. Do a handstand in the water. I didn’t do this technique for turning a breech baby, but many say it works well.
Light and temperature
Baby responds to dark/light and hot/cold. Start by having Dad place a flashlight at the base of your pelvis and sing, talk, and coax the baby downward. Many say this works, as baby instinctively moves towards the light and soothing sound. It certainly gives new meaning to “follow the light.”
Baby also responds to temperatures. Many women place ice packs in the rib area and/or heating pads at the base of the pelvis to entice baby away from the cold and/or towards the warmth.
Webster technique
This technique is done by a professional chiropractor. The Webster technique is a specific adjustment that reduces the effects of SI joint dysfunction. Often, pregnant mothers with breech babies get this adjustment that frequently facilitates optimal fetus positioning. It’s not going to turn a breech baby right then and there, but it does create the right alignment for baby to naturally move into a head-down position.
Often, pregnant mothers with breech babies get this adjustment that frequently facilitates optimal fetus positioning. It’s not going to turn a breech baby right then and there, but it does create the right alignment for baby to naturally move into a head-down position.
Miles Circuit
The inversion with rebozo wrap pops up again in the Miles Circuit. Your doula or midwife may suggest the Miles Circuit, if your labor has stalled or if your baby is not in the ideal position. The circuit consists of three moves (read more in this post on inducing labor naturally) that help encourage your baby into the proper position for birth, but be sure to only do these moves with your midwife’s permission.
Tip: It’s really important to dedicate your time for these moves; it can take time to flip a baby. You may need to stay in these positions for 30 minutes at a time.
External Cephalic Version (Version or ECV)
This technique is a medical procedure used for physically turning a breech baby. When it was determined Griffin was breech, my midwife performed ECV and flipped him in a snap! She manipulated his head and butt from my outer belly and basically moved him with her hands. When he was sort of sideways, he instantly flipped into a head down position himself. She said it was easy, because of the good quantity of amniotic fluid in the sac. It was shocking how easy and simple it was. It freaked me out really. Mostly, because I wasn’t prepared for the information that he was breech, but then to have him flipped in the same 5 minutes was a lot to take in.
When it was determined Griffin was breech, my midwife performed ECV and flipped him in a snap! She manipulated his head and butt from my outer belly and basically moved him with her hands. When he was sort of sideways, he instantly flipped into a head down position himself. She said it was easy, because of the good quantity of amniotic fluid in the sac. It was shocking how easy and simple it was. It freaked me out really. Mostly, because I wasn’t prepared for the information that he was breech, but then to have him flipped in the same 5 minutes was a lot to take in.
Since then, I’ve found out that ECV is common, typically around 37 weeks. Sometimes it is used during labor, before the amniotic sac has ruptured. Because mine was done so early (34 weeks), Griffin didn’t stay head down, which is not unusual and is one of the reasons ECV is often performed closer to labor.
ECV’s have a success rate of about 60% so it’s definitely worth a try if all else fails. Do know there are some risks so be sure to discuss with your midwife or doctor to see what is best for your situation.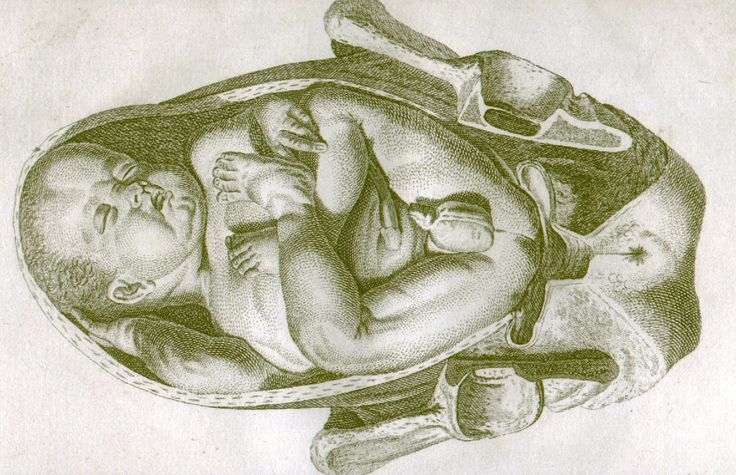
Moxibustion acupuncture
This was the weirdest thing I did while trying techniques for turning a breech baby, but people swear by it. The technique has been around for over 3500 years!
Between weeks 30-34 gestation with a breech baby, an acupuncturist will stick the needles (very thin and narrow) in your pinky toes, both sides. Then, moxibustion incense, comprised of an herb called mugwort, is burned and the smoke is swirled close around the needles. The hot cherry of the incense is also put close (but not on) the needles. The combination of smoke, heat, and acupressure points stimulate the uterus to get baby to turn head down. It doesn’t hurt. It’s strange. But my acupuncturist claims that only two of the women she has ever treated for breech babies didn’t work. Later, she found out that one baby had the cord wrapped around its neck, so instinctively the baby knew not to turn. And the other baby was a wild baby in utero all the way up into labor.
Learn to have an amazing birth – Birth Course Promo [In-article]
(without leaving your couch)
See How
What If You’re Having Trouble Turning a Breech Baby?
Here’s a whole post on your options for delivery when you techniques for turning a breech baby don’t work.
How Other Natural Mamas Turned Breech Babies
I asked the moms on my Facebook page if they were successful in turning a breech baby. Here are some of their responses.
- Chiropractic! I had a 9lb 4oz baby with a head measuring 4 weeks “too big.” She was breech at 37 weeks. I called my chiro ASAP, and she did an adjustment using the Webster technique, plus acupuncture on my pinky toes. My melon-headed baby was back down where she belonged within 24 hours! — Betsy S.
- I tried a lot of time inverted. Ice/hot (warm) packs and music played below the belt to draw him near. I did so much research on spinning babies and also watched you, Mama Natural, on turning Griff before his birth. My son decided the day of his scheduled c-section to turn. Literally right before they began to wheel me away. They luckily sent me home to allow me to give birth naturally. — Jennifer D.
- Prenatal massage at 38 weeks 5 days. My body relaxed enough for baby to flip.
 It was wild watching the sheet going crazy from the movement! — Lauren H.
It was wild watching the sheet going crazy from the movement! — Lauren H. - Table pose in prenatal yoga turned both of mine. — Caitlin R.
- Chiro and handstands in a pool! — Catherine F.
- Talking to my baby. I pressed hard on the top of my belly and said “Your feet and bum go here.” Rubbed my belly clockwise. Then pressed down low on my belly and said “Your head goes here.” Repeated several times a day for about two weeks. This worked more than once—the latest one was 35 weeks. — Kadie J.
- A friend of mine told me a old wives tale that if you scrub your kitchen floor clean on your hands and knees the baby will flip. Sure enough at 37 weeks while scrubbing the floor she flipped! — India R.
Get a Printable Cheat Sheet on Turning a Breech Baby.
Don’t forget to download my exclusive cheat sheet on turning a breech baby!
Breech Baby How to Turn Yours Naturally Cheat Sheet
References
- https://www.
 acog.org/patient-resources/faqs/pregnancy/if-your-baby-is-breech
acog.org/patient-resources/faqs/pregnancy/if-your-baby-is-breech - http://thefarmmidwives.org/faq/
- https://sciencebasedmedicine.org/is-breech-vaginal-delivery-safe/
- https://www.reuters.com/article/us-breech-births/most-breech-births-are-now-by-c-section-study-idUSBRE83G15Z20120417
- https://www.wsj.com/articles/breech-delivery-process-is-reconsidered-1402354629
The problem of breech presentation of the fetus. External obstetric rotation of the fetus on the head.
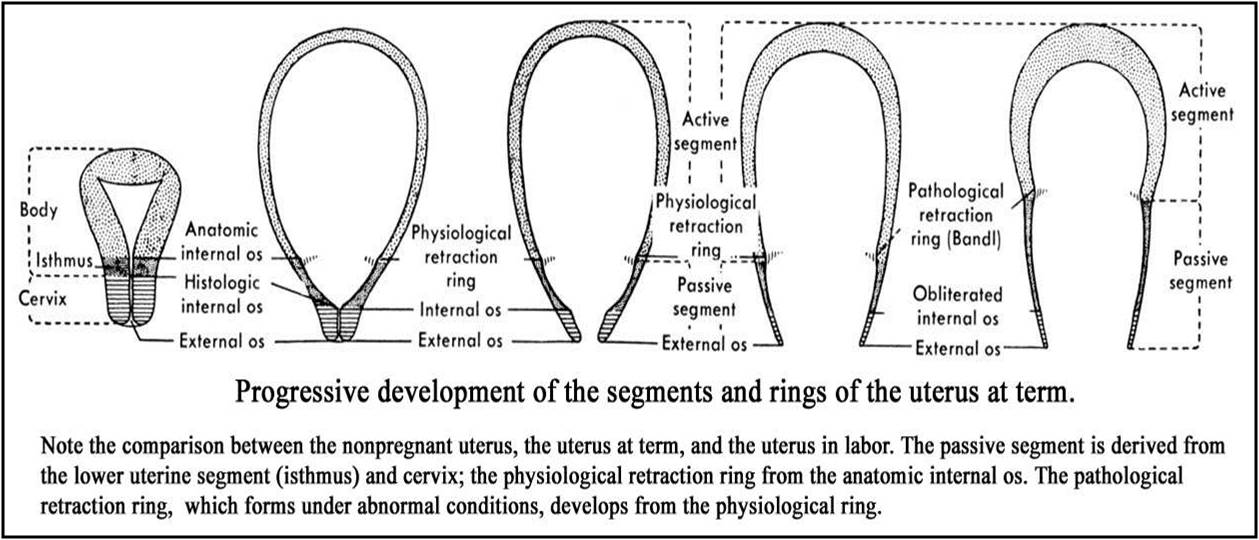
Breech presentation of the fetus occurs in 3% -5% of cases at full-term pregnancy. Vaginal delivery with breech presentation is associated with high risks both on the mother's side and on the fetus's side. Thus, breech presentation is currently considered pathological, even if the conditions necessary for childbirth through the birth canal are ideally met, and the fetus is relatively small relative to the size of the mother's pelvis. During vaginal delivery, the arms and head of the fetus may tilt back, which can lead to injury.
Currently the most common method of delivery in breech presentation is a caesarean section (90%). Among the indications for the use of caesarean section, breech presentation ranks third among others in the world. However, this the operation does not make it possible to completely eliminate the risk of trauma to the fetus, since when it is removed, it is also possible to tilt the arms and head of the fetus, and their release requires the use of complex manipulations.
To correct breech presentation today, the world is using EXTERNAL OBTETAL TURNING OF THE FETUS ON THE HEAD proposed at the end the century before last by the Russian obstetrician Arkhangelsky B.A.
External obstetric cephalic rotation (EFRT) is a procedure during which the doctor turns the fetus from the outside through the wall of the uterus breech presentation in the head. A successful attempt at NAPP allows women to give birth on their own, avoiding a caesarean section.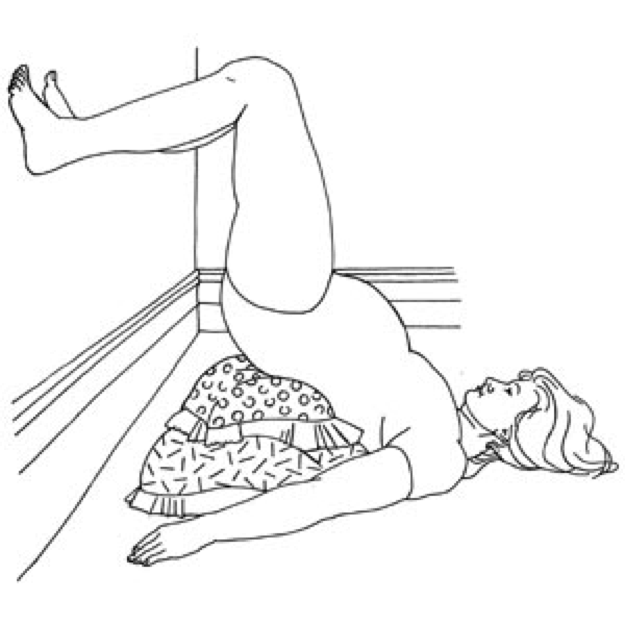
What is required for external cephalic fetal rotation?
External obstetric rotation of the fetus on the head is performed before the onset of labor, usually starting from 36 weeks of pregnancy.
It is necessary to consult a doctor and conduct an ultrasound examination to confirm the fact breech presentation of the fetus and determine the conditions for NAPP, starting from 34-35 weeks of pregnancy.
| The operation of external rotation of the fetus on the head in breech presentation |
When NAPP is possible:
- From 36 to 37 weeks, since with earlier use, it is likely that it will return to the breech presentation.
- In the presence of a singleton pregnancy.
- Subject to the mobility of the buttocks of the fetus (if they are tightly pressed against the entrance to the mother's pelvis, it will be extremely difficult to change the position of the fetus).
- Sufficient amount of amniotic fluid. With oligohydramnios, this manipulation can be traumatic for the fetus, while with polyhydramnios there is a high probability of a reverse rotation of the fetus in a breech presentation.
- Sufficient amount of amniotic fluid. With oligohydramnios, this manipulation can be traumatic for the fetus, while with polyhydramnios there is a high probability of a reverse rotation of the fetus in a breech presentation.
- Fetal head flexed
When NAPP is not possible:
- With the outflow of amniotic fluid.
- If the patient has contraindications to the use of drugs used to relax the uterus (tocolysis).
- In the presence of obstetric indications or indications from the health of the mother for delivery by caesarean section.
- With the extensor position of the fetal head.
- If the fetus has congenital developmental features.
- With multiple pregnancy.

- In the presence of structural features of the uterus in a pregnant woman
However, in addition to this, there are a number of factors that may favor or, on the contrary, serve as a contraindication to external obstetric turning the fetus on the head, and which can only be determined by a doctor during a direct examination of a pregnant woman.
How NAPP is conducted
For manipulation, hospitalization in the maternity hospital is necessary. Preliminarily, an additional examination of the pregnant woman is carried out in the required volume, including ultrasound.
During the NAPP:
Immediately before the start of the manipulation, a CTG is recorded to assess the condition of the fetus.
Drugs are administered to prevent uterine contractions (tocolytics).
Further, under constant ultrasound and KGT control, as well as the continued administration of drugs that relax the uterus, the doctor performs a turn.
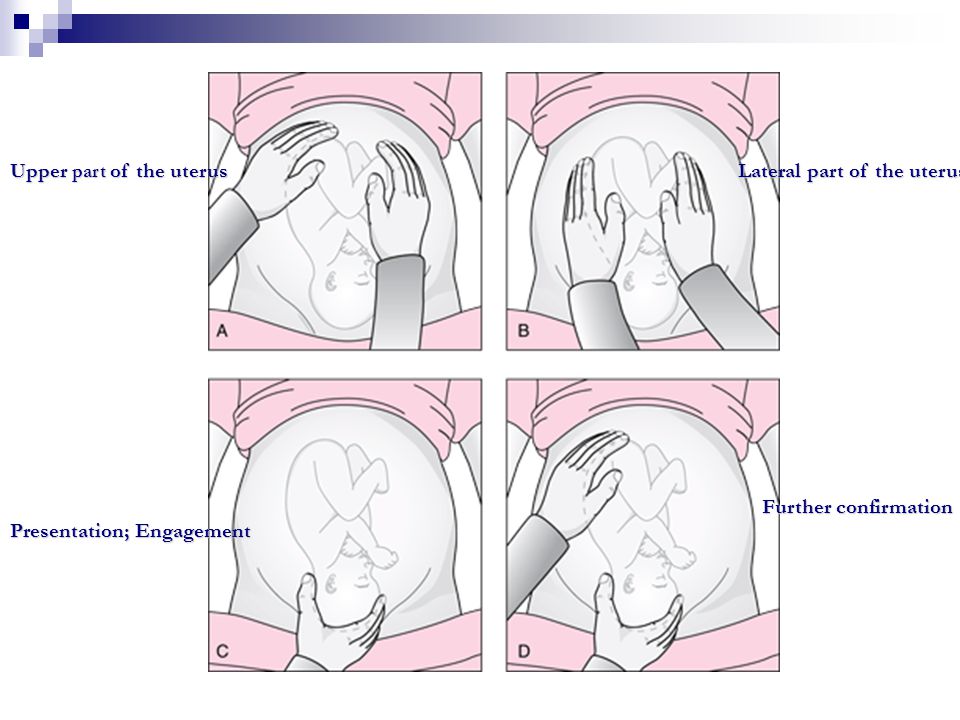
Holding both hands on the surface of the pregnant woman's abdomen, one on the head of the fetus, and the other on the buttocks of the fetus, the doctor pushes and rotates the fetus to the upside down position. A pregnant woman may feel some discomfort during the procedure. The degree of discomfort depends on the individual sensitivity of each patient.
After the procedure is successfully completed, the CTG is recorded again, to make sure that the fetus feels well and has successfully undergone the procedure. Usually during the day, the condition of the mother and fetus is monitored, after which the patient is discharged and continues the pregnancy until spontaneous delivery occurs.
If the doctor notices a deterioration in the condition of the fetus according to the monitoring data, then the procedure is immediately stopped.
If the first attempt was not successful, your doctor may suggest another attempt if the fetus is in good health.
APP is performed ONLY in a maternity ward where there is an opportunity for an emergency delivery, if necessary.
Risks associated with NAPP
Subject to constant monitoring of the condition of the fetus, constant tocolysis (administration of drugs that relax the uterus) The risks associated with this procedure are minimal. Complications from its use occur in less than 1-2% of cases.
Complications of NAPP include:
- compression or "twisting" of the umbilical cord. In this case, constant monitoring of the condition of the fetus allows you to immediately fix its deterioration and stop the procedure.
- discharge of amniotic fluid or the development of labor. This complication can be considered relative, since the rotation in most cases is carried out at full-term pregnancy.
Any deviation from the normal course of the procedure serves as a reason to stop the manipulation and decide on the choice of further management tactics.
Carrying out NAPP with Rh-negative mother's blood.
The presence of Rh isoimmunization (that is, the presence of anti-Rh antibodies in the mother's blood) is a contraindication to this procedure, as it increases the risk of anemia in the fetus.
In the absence of isoimmunization (absence of anti-Rhesus antibodies) it is possible to carry out NAPP with prophylaxis by introducing anti-Rhesus immunoglobulin.
If you have a breech presentation of the fetus and you want to know about further options for pregnancy management, delivery, external obstetric rotation of the fetus on the head, the presence of indications and contraindications for its implementation, please consult our specialists.
Breech presentation
Elina Kukharskaya
experienced breech presentation
Author profile
Breech presentation of the fetus in term pregnancy occurs in 3-5% of cases. It is possible to give birth to a child without surgery, but it didn’t work out for me.
It is possible to give birth to a child without surgery, but it didn’t work out for me.
At 30 weeks pregnant, I had a screening ultrasound. The doctor told me that the child is in breech presentation, that is, it lies not with its head down, but with its buttocks, and, most likely, will not roll over.
I started looking for information about what awaits me and whether I can contribute to the rotation of the fetus: I consulted with my gynecologist at the antenatal clinic, an obstetrician at the maternity hospital, signed up for an external obstetric rotation - a procedure by which they try to rotate the baby. Then she came again for consultations, did a second ultrasound, read the protocols for managing pregnancy and childbirth in breech presentation, as well as foreign websites and articles.
As a result, it turned out that my child was entwined with the umbilical cord - this is a contraindication for external obstetric rotation. As early as the 40th week, the fetus weighed 3600 grams according to ultrasound - this is too much weight for natural childbirth in breech presentation. I had a caesarean section, and an absolutely healthy baby was born.
I will tell you what I learned about the breech presentation of the fetus during pregnancy and whether there are chances in this case to give birth to a child without a cesarean.
Go see a doctor
Our articles are written with love for evidence-based medicine. We refer to authoritative sources and go to doctors with a good reputation for comments. But remember: the responsibility for your health lies with you and your doctor. We don't write prescriptions, we make recommendations. Relying on our point of view or not is up to you.
What is breech presentation
Almost all babies change their position in the uterus several times as they grow. However, by the end of the gestation period, most take a head-down position: this is how they pass through the birth canal. First the head is born, and then everything else.
9 vaccinations that can be given during pregnancy
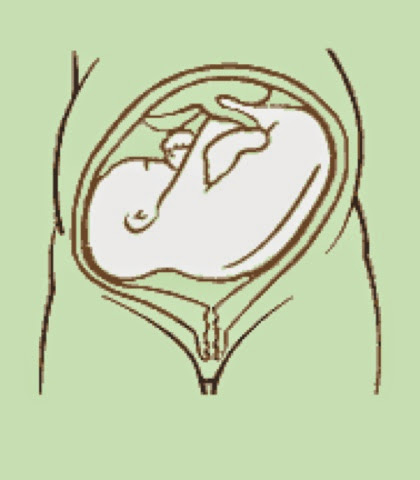
In breech presentation, the fetus remains in the buttocks down position. In this case, the management of pregnancy and the method of resolving childbirth depend on many factors: the weight and position of the child, the condition of the mother, and others.
Breech presentation frequency - Medscape
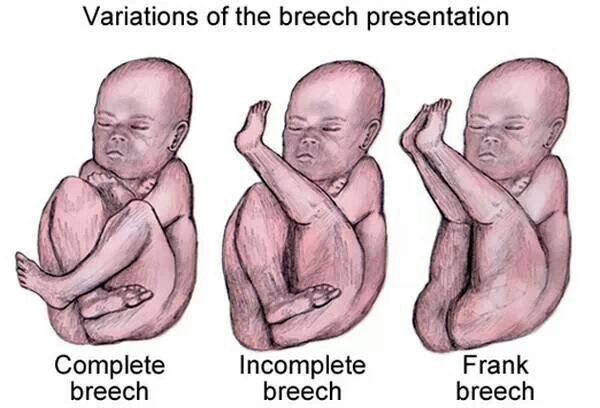
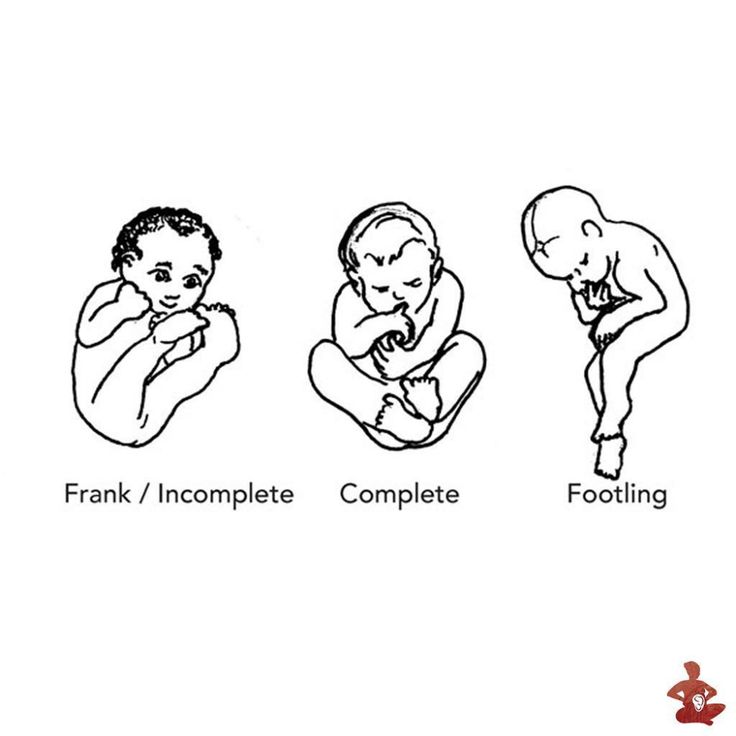
The baby in the womb chooses one of several types of breech presentation:
- Buttock - when the baby lies on the buttocks towards the birth canal, and the legs are extended up along the body.
- Mixed - the child has bent his knees and sits with his buttocks down.
- Foot - both legs or one of them pointing down.
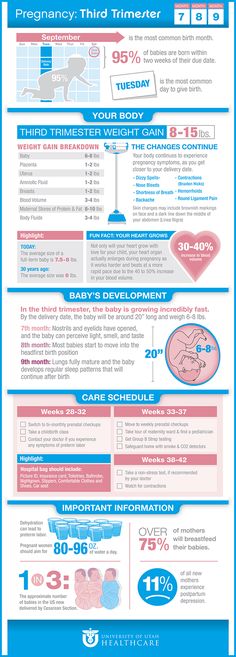
With increasing gestational age, most of the children assume a normal position
| Pregnancy age | Breech presentation |
|---|---|
| 21-24 weeks | 33% |
| 25-28 weeks | 28% |
| 29-32 weeks | 14% |
| 33-36 weeks | 9% |
| 37-40 weeks | 3-4% |
The term of pregnancy
Pitement
21-24 weeks
33%
25-28 weeks
28%
29–32 weeks
14%
9000 33-36 weeks of week9%
37-40 weeks
3-4%
Why the baby is in a breech presentation
There can be several reasons why the baby may be in the wrong position. In most cases - up to 75% - it is not clear why this happens. It's probably just a coincidence.
Overview of breech presentation - Uptodate
Some known causes of breech presentation are: uterine fibroids, placenta previa, pelvic bone injury, abnormal development of the uterus in a woman.
There is also a Finnish study that shows that one of the risk factors is the woman's age. If she is older than 35 years, this increases the likelihood of breech presentation.
Moreover, even if a woman has any of the above, it is not at all necessary that the child will take the wrong position. And vice versa: even if there are no predisposing factors, the child may not turn his head down. So it was with me - none of the doctors could find the cause.
/list/pregnancy-myths/
“You can’t keep cats and dye your hair”: 9 myths about pregnancy money for treatment - in your mail twice a month on Thursdays. Free
How to rotate the fetus to the normal position before delivery: external obstetric rotation
In the breech presentation pregnancy and birth protocol, the ob/gyn should discuss external obstetric rotation with the woman at 36-37 weeks.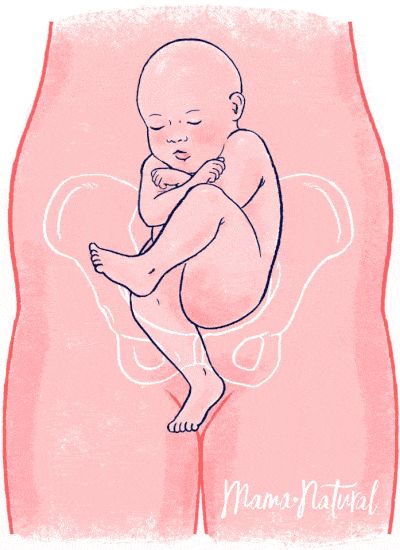 This procedure is included in the OMS.
This procedure is included in the OMS.
Breech presentation of the fetus - clinical recommendations of the Ministry of Health
External obstetric rotation is a rotation on the head, which is done with almost any incorrect position of the fetus in the uterus. The turning procedure itself is painless, but it can cause discomfort.
External OB Rotation - Cleveland Clinic Blog Article
My OB/GYN didn't even mention the OB rotation. She immediately said that I would have a caesarean section. When I tried to find out more about the procedure, the doctor replied that this is not practiced in our hospital and maternity hospital. At the same time, she added that if I decide on the procedure, then after that they will leave me in the hospital and I will need to lie motionless so that the child does not roll over on the buttocks again.
I was determined to have a natural birth without surgery, so I tried to find out more information on my own.
I found out that in Moscow, indeed, not all maternity hospitals practice external obstetric rotation.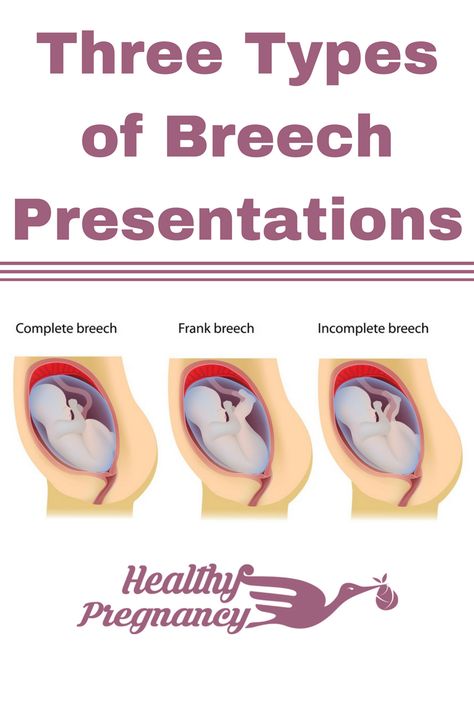 I clarified this issue in maternity hospitals No. 17 and 20 - they were the most suitable for me territorially, but both refused me this. Through my friends, I found out that external obstetric rotation can be done in maternity hospital No. 24.
I clarified this issue in maternity hospitals No. 17 and 20 - they were the most suitable for me territorially, but both refused me this. Through my friends, I found out that external obstetric rotation can be done in maternity hospital No. 24.
I went to a free consultation with a doctor, and she told me about all the risks associated with obstetric rotation:
- Before the procedure, I must be examined by a doctor, and I must also undergo a control CTG and ultrasound. At any time before the start of the procedure, I have the right to refuse it.
- There are risks. They are less than 1% that something will go wrong and I will have an emergency c-section. Therefore, the procedure itself takes place in the operating room.
- On average, only about 70% of external obstetric turns are successful and the baby turns upside down.
- There is a possibility that even if the child turns over as a result of manipulation, then he may again be in breech presentation.

As a result of the consultation, I decided to do an external obstetric turn and signed up for the procedure. It was far to go to the hospital, so the day before the appointed date, I decided to do another ultrasound near my house in a paid clinic. According to the results, it turned out that the child also has an umbilical cord entwined around the neck - this is a contraindication to external obstetric rotation. I canceled the appointment.
/list/childbirth/
“Giving birth is about the same as treating teeth”: questions to obstetrician-gynecologist Ivan Lugovsky
In addition to external obstetric rotation, some doctors recommend special gymnastics, yoga, osteopathy to change the position of the fetus. But these funds have no evidence of effectiveness.
The conclusion of the ultrasound, after which I abandoned the idea of doing an external obstetric rotationIs it worth doing an external obstetric rotation and when this procedure is contraindicated
Anastasia Degteva
obstetrician-gynecologist of the Fomin Clinic network
Pre-pregnancy harms the mother or baby, but childbirth with him is associated with a high risk of injury to the fetus and woman. It would seem that you can choose a caesarean section, but even in this case, there is a high probability that additional benefits will have to be applied.
It would seem that you can choose a caesarean section, but even in this case, there is a high probability that additional benefits will have to be applied.
External obstetric rotation can only be performed in the maternity hospital so that the woman can be helped if something goes wrong. The procedure is done starting from the 36-37th week of pregnancy. Previously, it makes no sense due to the high risk of reverse rotation of the fetus into breech presentation.
When you can do an external obstetric turn. The procedure is done if the pregnancy is singleton, the buttocks of the fetus are mobile, and the head is in a flexed position.
There should also be enough amniotic fluid. With oligohydramnios, manipulation can be traumatic for the fetus, and with polyhydramnios, it is highly likely to turn back to its previous position.
When external obstetric rotation is not possible. The procedure is not performed if the woman has a multiple pregnancy, there are structural features of the uterus, contraindications for vaginal delivery, she should not be given tocolytics - drugs that prevent uterine contractions.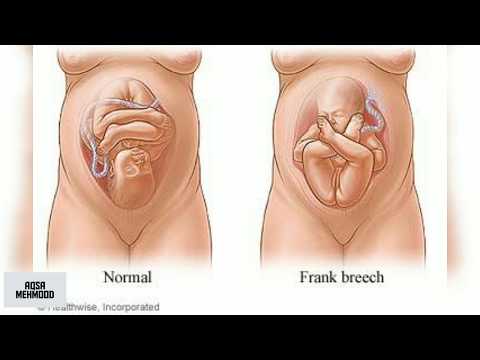
Also, manipulation is contraindicated in case of fetal malformations, after the outflow of amniotic fluid and in some other cases.
How to perform an external obstetric rotation. First, a woman is examined to clarify the absence of contraindications, in particular, an ultrasound is performed. Cardiotocography is also recorded to assess the condition of the baby. Next, drugs are injected that relax the uterus, then the doctor performs a turn under the control of ultrasound and CTG.
If the turn is successful, the woman is again recorded with CTG, recommended to use a prenatal bandage and sent home. There is a myth that bed rest is necessary after the procedure, but this is not true.
What are the possible complications of the procedure. With external obstetric rotation, complications occur rarely, in 1-2% of cases, these can be:
- Compression or "twisting" of the umbilical cord. In this case, constant monitoring of the fetal condition allows you to immediately fix its deterioration and stop the procedure.
- Descent of amniotic fluid or development of labor activity. This complication can be considered relative, since the rotation in most cases is carried out at full-term pregnancy.
Any deviation from the normal course of the procedure is a reason to stop it and decide on the choice of further management tactics.
How to give birth if the baby is in a breech presentation: caesarean or vaginal delivery
A caesarean section is a surgical procedure used to deliver a baby. During it, an incision is made in the lower abdomen, then the baby and the placenta are taken out of the uterus.
Clinical guidelines for caesarean section in Russia
Sometimes, when the baby is in a breech presentation, doctors unequivocally refer the woman for a caesarean section. But in other cases, with breech presentation, you can try the natural method of delivery.
Several conditions must match for this to happen. Here are the main ones:
- Pure breech presentation, not mixed or foot presentation.
- No tilting of the handles, the head is pressed against the chest, and not thrown back.
- The weight of the child is not less than 2500 and not more than 3600 grams.
- At least 36 weeks of gestation.
- The width of the woman's pelvis corresponds to the anatomical norms.
In case of any abnormalities in the development of the fetus or complications of pregnancy, doctors will insist on an operation.
However, even if the necessary conditions are met, a woman has the right to refuse natural childbirth and prefer a caesarean section. In Russia, it is usually impossible to perform a caesarean section at the request of the mother, but with a breech presentation, women have a choice.
/cesarean-section/
What is a caesarean section
When choosing, all the pros and cons should be weighed:
- 5 cases per 1000 births.
- Vaginal delivery in breech presentation increases the risk of a low Apgar score, but there is no data on the rate of complications for the child in the long term.
- Approximately 40% of women with breech presentation require an emergency caesarean section for planned vaginal delivery.
- Elective caesarean section is accompanied by a slight increase in the rate of complications for the mother, and also increases the risk of complications in future pregnancies. With a successfully completed vaginal delivery, complications for the mother are the least.
For example, in the United States, a caesarean section is increasingly being chosen for breech presentation. The authors of one of the studies involving more than 2,000 patients came to the conclusion that when the child is in the wrong position, a planned caesarean section is better than a vaginal birth.
What are the chances of giving birth spontaneously in breech presentation and is it worth trying
Anastasia Degteva
obstetrician-gynecologist of the Fomina Clinic network
If external obstetric rotation fails, women with low risks of complications can try vaginal delivery.
This is possible if there are no contraindications to vaginal delivery, there were no caesarean sections in the past, the pregnancy is full-term, labor begins spontaneously at term.
At the same time, the maternity hospital must have qualified personnel who can deliver in a breech presentation. Resources and equipment for a safe emergency caesarean section should also be available: anesthesiologists, surgeons, a prepared operating room, and so on.
If something goes wrong during childbirth - the condition of the fetus is disturbed, weakness of labor activity and other complications occur - the patient is given a caesarean section.
How is vaginal delivery with breech presentation of the fetus
For vaginal delivery, you need to choose a maternity hospital in advance. When you choose, check with the medical staff or administration what level of readiness it belongs to. There are three of them, depending on whether obstetricians and anesthesiologists are on duty around the clock, whether there is all the necessary equipment for resuscitation care for mothers and babies, whether high-tech operations are performed there.
The maternity hospital for natural birth in breech presentation should be at least the second group with readiness for an emergency caesarean section if something goes wrong in childbirth. Ordinary maternity hospitals of the first group, where women with full-term pregnancies and without complications are delivered, are not suitable.
Anesthesiologist and neonatologist must be present during the birth process. The birth process itself will be slightly different from the birth process when the baby is in the head presentation.
Many of my friends who gave birth vaginally said that they lived through the process of contractions on a fitball or in an upright position, someone could even take a bath or shower, someone could walk around the ward. But during childbirth in breech presentation, women continuously undergo cardiotocography - this is necessary in case the child's condition worsens, this moment cannot be missed.
/preparation-for-childbirth/
How I prepared for childbirth and spent about 30,000 R on it
With the CTG machine, you won’t be able to move freely during labor, but you can take a comfortable position for childbirth, even giving birth vertically if so it will be convenient for doctors.
To help the child be born, special obstetric aids are used during childbirth, for example, the Tsovyanov aid technique. At the same time, the obstetrician takes the child's buttocks with his hands, and puts his thumbs on the hips.
Further, as the fetus is born, the doctor holds the child's legs so that they are pressed against the body and at the same time press the arms crossed on the chest.
How I gave birth to a baby in a breech presentation without a caesarean section
Tatyana Rumyantseva
obstetrician-gynecologist, mother of two children
My second birth was in a breech presentation. I really wanted to give birth naturally without a cesarean, especially since the first birth went well.
I found out that the baby was in breech presentation in the third trimester. Then there was still time for him to roll over, but this did not happen. I didn’t know the baby’s gender until his birth: it wasn’t visible on the ultrasound for a long time, I decided that I probably didn’t need this information. There is a myth that boys cannot be born in breech presentation without surgery, but girls can, but this is not true.
There is a myth that boys cannot be born in breech presentation without surgery, but girls can, but this is not true.
Before giving birth, I tried external obstetric rotation - few people in Russia know how to do it, but there are still such doctors. The effectiveness of the technique is far from 100%, in my situation it did not work.
I was looking for a maternity hospital with a large flow of patients, where they can deliver in breech presentation. Where I gave birth to my first child, they honestly told me that they don’t take such things: the flow of women is small, there is no experience.
There is a restriction on the weight of the fetus for natural birth with breech presentation according to Russian orders - it should not exceed 3600 grams. My child's weight was around this limit - 3610 grams. There were many skeptics, but I enlisted the support of doctors and decided to try to give birth myself. There was an important agreement with the doctors: in case of any doubts, I immediately go to the operating room without any objections.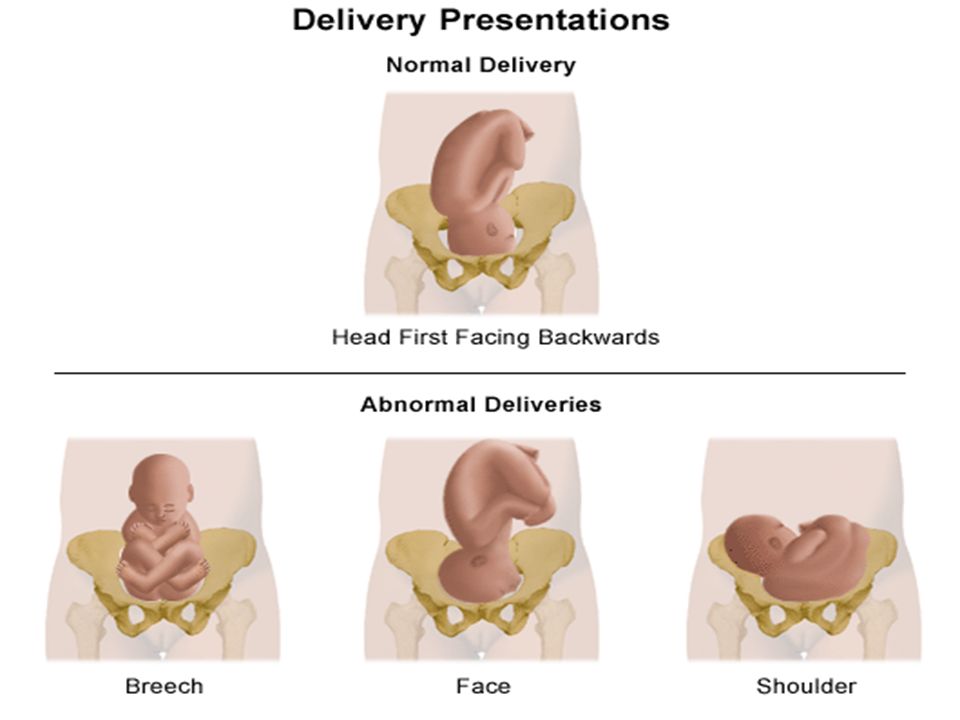
The delivery was easy, under epidural anesthesia. At some point, I asked her to put it in, although the process was already close to completion and the doctors dissuaded me.
It was easier to give birth than the first time in cephalic presentation. But, firstly, the birth was the second, I already went through it, and secondly, with breech presentation, the softest part of the child appears first, and only then the head. The birth of a head is the most risky moment, cooperation with doctors is needed.
In my situation, everything went smoothly and calmly, a healthy boy was born. However, each case must be considered separately: the condition of the mother with the baby, the skills of doctors, and the wishes of the woman should be taken into account.
How I gave birth to a breech baby by caesarean section
I was determined to give birth on my own. Moreover, my husband and I planned a partner birth - he prepared all the certificates for this, I really wanted him to be present at the birth of my son. The maternity hospital was on compulsory health insurance, did not conclude a paid contract.
The maternity hospital was on compulsory health insurance, did not conclude a paid contract.
At the antenatal clinic, they gave me a referral to a maternity hospital, where such childbirth was carried out. I arrived there in advance for a consultation.
There I was told that if the birth process does not start earlier, then I need to come for planned hospitalization between 39th and 40th weeks. We were waiting for this moment, at 40 weeks and 2 days I arrived at the maternity hospital.
/rody-v-mashine/
How I paid 113,500 R for childbirth, but gave birth myself in the car
The baby's weight according to ultrasound was 3600 grams. This was an indication for a caesarean section, and I was hospitalized in the prenatal ward. I was a little upset, but I still understood that the health of the child is more important than my plans, and if the risks are higher than acceptable, it is better to have an operation.
I spent a day in the prenatal ward, during this time I was examined. I also met with the doctor who operated on me the next day and the anesthetist.
I also met with the doctor who operated on me the next day and the anesthetist.
The operation was scheduled for seven in the morning. I put on my compression stockings, they gave me an enema, although there are studies that this procedure does not have any significance, CTG, then they sent me to the operating room.
I had a spinal anesthetic that kept me awake. When they got the child, they showed it to me, after which they performed the necessary manipulations. Since I was very worried about the baby, my first question was: “How many Apgar scores?” The rating turned out to be 8/9 points - good.
How to quickly assess the condition of the baby on the Apgar scale
After the baby was attached to the chest, I was sewn up and sent to the recovery room. In it, the child was brought to me twice more for feeding, and then we were transferred to the postpartum department.
Prenatal ward I am having a CTG before surgeryPeculiarities of children who were in breech presentation
There is no evidence that healthy children who were in breech presentation differ in any way from children who were positioned head down.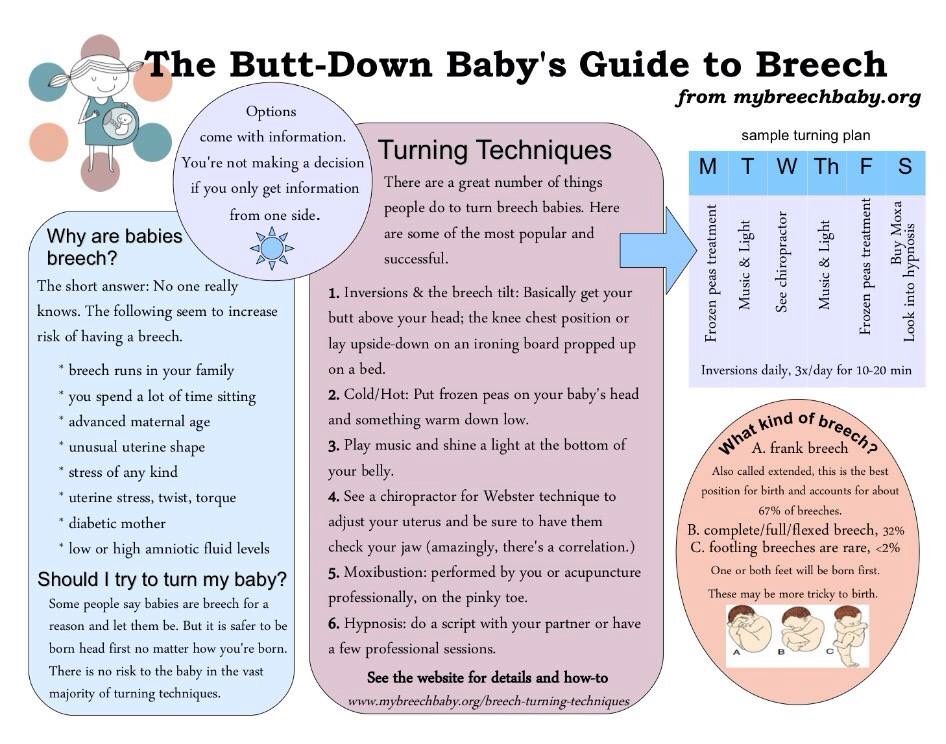
In the maternity hospital, the nurse told me this: “Your baby’s legs are somehow strange, I could hardly swaddle him.” A little later, the doctor on the round said that everything would be back to normal soon, the main thing is not to swaddle the child tightly - this advice applies to all children.
/swaddling-babies/
Is swaddling really good for babies?
Remember
- Breech presentation of the fetus during full-term pregnancy occurs in 3-5% of cases. Most often, the child rolls over into a normal position.
- Incorrect position of the fetus in most cases is not dangerous for mother and baby, but can be a problem in childbirth.
- External obstetric rotation can be tried to turn the baby before delivery, but this procedure is not 100% effective.
- With a breech presentation, a caesarean section is more often suggested, but in some cases, if the baby lies safely and the woman has no contraindications, vaginal delivery is possible.