Difference between uti and pregnancy
UTI During Pregnancy: Is It Dangerous?
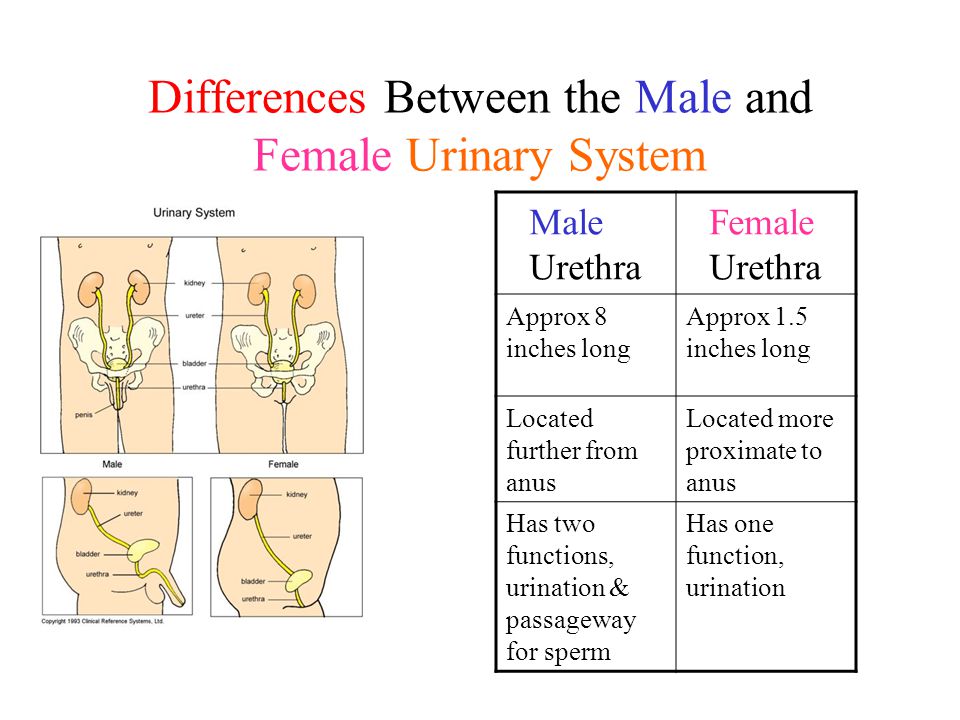
A urinary tract infection happens when bacteria colonize the areas through which urine exits the body. During pregnancy, the chance of getting these infections increases due to changes in the urinary tract and immune system.
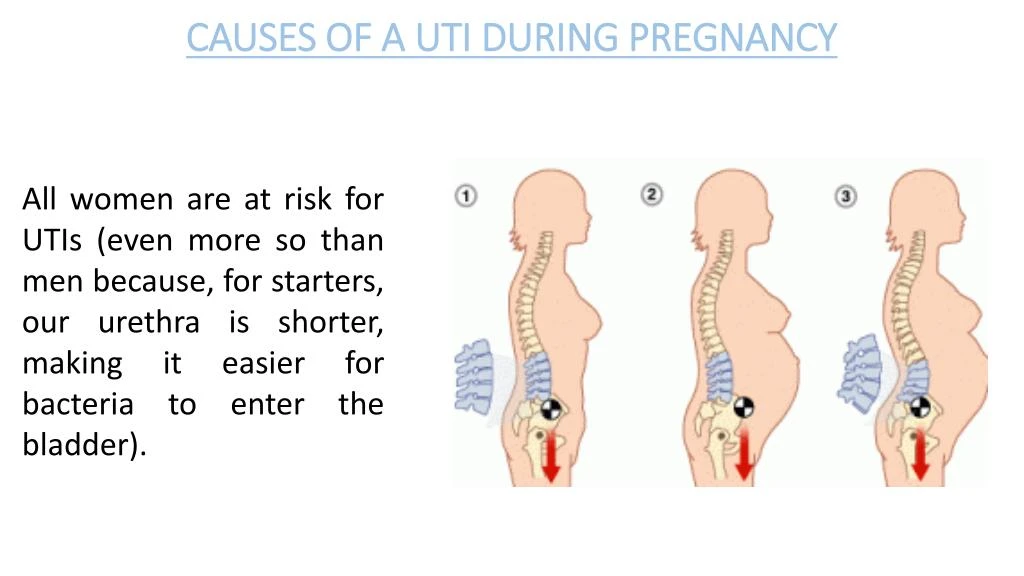
As your fetus grows, your uterus expands. This puts pressure on your bladder and ureters (the tubes that connect the kidneys to the bladder). Under pressure, the urinary tract may become blocked and unable to drain urine properly. Pregnancy hormones may also cause the relaxation of smooth muscles, which can result in urine retention.
In this situation, bacteria can readily grow and thrive throughout the urinary tract, causing an infection.
Some people who get a UTI in pregnancy may not experience any overt symptoms. For others, UTI symptoms can appear quickly.
Here are some of the most common UTI symptoms during pregnancy to look for:
- A burning feeling when you’re urinating
- Cloudy urine
- Urinating more frequently
- Strong urge to urinate
- Unusual urine odor
- Pain in the lower abdomen and lower back
- Fever and chills
- Nausea
- Painful sex
These symptoms often indicate a UTI. If you experience any of them, talk to your health care provider to ensure that your pregnancy is managed safely.
If you suspect a urinary tract infection, visit a health care provider as soon as possible. At the medical facility, the health care provider will request a urine sample for testing.
First, your provider will observe the appearance and smell of your sample. A normal urine sample should be clear and slightly yellow. If you have an infection, your urine will most likely have an odor and appear cloudy.
To pinpoint the kind of bacteria responsible for the infection, the provider will use medical technology to examine your urine and a blood sample.
After a health care provider determines the cause of your symptoms, they can propose the appropriate treatment for UTI in pregnancy.
Most patients receive antibiotics during pregnancy for UTI. These antibiotics are mainly antimicrobials from two specific groups — penicillins and macrolides. These include amoxicillin, azithromycin, and erythromycin.
Other drugs (fluoroquinolones and sulfonamides, trimethoprim-sulfamethoxazole, nitrofurantoin, and cephalosporins) can pose health risks to a baby. It’s important to steer clear of them. Your health care provider will prescribe one of the safe drugs depending on the kind of infection and any allergies you may have.
You’ll need to take the antibiotics for three to seven days, depending on the prescription. Most symptoms will disappear in one to two days, but your health care provider will still instruct you to take the drugs until the prescription is gone to ensure the bacteria don’t become resistant to treatment.
My husband & I are trying to get pregnant so I downloaded this app to predict my periods/ovulation. It’s been nothing short of perfect! It’s predicted my period accurately to the day, so I’m happy to know without a doubt if I’ve missed a period. You can log pretty much anything you’d ever want to, from your moods, symptoms, intercourse, and of course period info. You can also log pregnancy test results, ovulation test results, and it also tracks your movement/steps throughout the day and gives you tips to getting pregnant. They also have a “pregnancy mode” which I’m excited to (hopefully) check out soon! Highly recommend this app.
You can also log pregnancy test results, ovulation test results, and it also tracks your movement/steps throughout the day and gives you tips to getting pregnant. They also have a “pregnancy mode” which I’m excited to (hopefully) check out soon! Highly recommend this app.
Other than anemia, urinary tract infections are the most common condition experienced during pregnancy.
Thankfully, with prompt treatment, the infection can be stopped. Some people develop asymptomatic infections that can spread within the body without any unusual sensations.
These asymptomatic UTIs can negatively affect the health of the fetus. Scientists have conducted studies that show these kinds of UTIs lead to pyelonephritis — an infection of the kidneys.
This condition affects your health and the health of your baby. Bacteria can release substances called endotoxins, which can lead to anemia, prompt uterine contractions, and potentially prevent labor.
Pyelonephritis can cause low birth weight. Sometimes, babies whose mothers had advanced, untreated UTIs experienced delays in mental development.
Sometimes, babies whose mothers had advanced, untreated UTIs experienced delays in mental development.
In rare cases, a UTI and pregnancy can influence the risk of miscarriage and even infant mortality.
So, can a UTI affect pregnancy? Simply put, yes.
Love Flo, tried a few and this is definitely my favorite. Love the pregnancy mode as well. My favorite is the articles and the personal “messages” u can have during different times of your cycle. So useful and full of information. Makes you feel like you are definitely not alone during anything weird you’re experiencing. Thank you Flo!
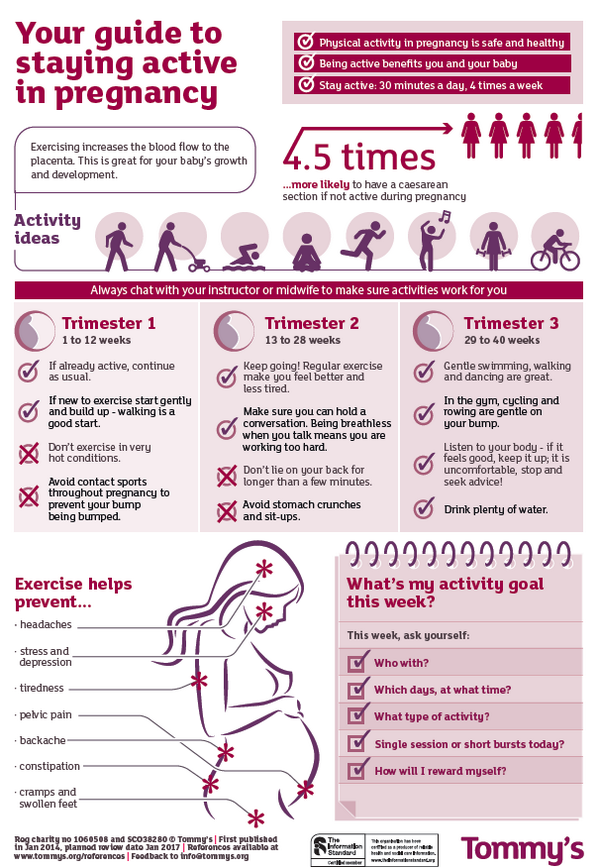
To encourage the best experience for you and your baby during pregnancy, it’s important to prevent bacteria from causing an infection in your urinary tract.
Nobody can completely rule out the chance of getting an infection, but you can do a few simple things to shift the odds in your favor.
You can prevent UTIs by:
- Keeping properly hydrated, drinking at least eight glasses of water a day
- Urinate at least once every two to three hours to empty your bladder
- Wiping from front to back whenever you go to the bathroom
- Urinating before and after sexual intercourse
- Avoiding douching
- Taking showers instead of baths
- Wearing loose-fitting pants
- Wearing cotton underwear
For the many people who experience UTIs in pregnancy, plenty of questions may arise.
Here are some of the most common ones, with answers that provide some insight into the relationship between these infections and pregnancy.
Can a UTI affect a pregnancy test?
A pregnancy test is designed to detect the hormone human chorionic gonadotropin (hCG). This hormone is produced by the placenta when a fertilized egg implants into the uterine wall.
Infections and their byproducts, however, cannot cause the body to produce this hormone. If you have a UTI and become pregnant, talk to your health care provider for guidance.
Can a UTI be a sign of pregnancy?
A urinary tract infection isn’t a sign of pregnancy. However, engaging in unprotected intercourse can cause some infections that might coincide with pregnancy.
Can a UTI be mistaken for a pregnancy?
Early in your pregnancy — especially in the first trimester — you may notice some signs that could point to a UTI. These include fatigue, frequent urination, back pain, and nausea.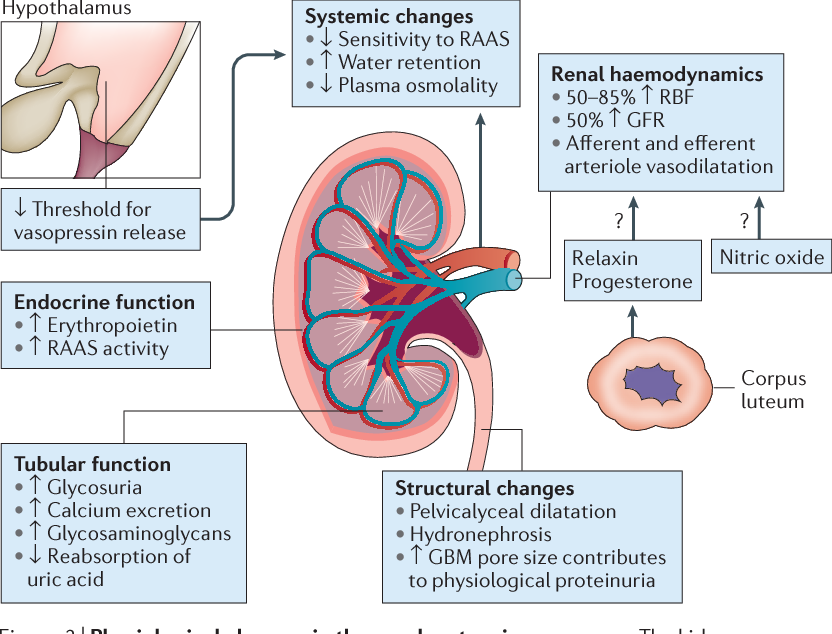 Bad cramps during early pregnancy can also feel similar to the cramps you’d have with an infection.
Bad cramps during early pregnancy can also feel similar to the cramps you’d have with an infection.
A health care provider can help rule out an infection or pregnancy since there are shared signs.
Can a urinary tract infection prevent pregnancy?
If an infection goes untreated, it can affect your kidneys. Your kidneys remove waste from the body, and they can’t do their job properly if they are infected. This can disrupt other body functions, including ovulation.
As a result, some people with untreated UTIs may not conceive.
Key Takeaways
Developing a UTI during pregnancy is common because of the numerous changes happening in your body.
These changes can allow bacteria to thrive in your urinary tract. These bacteria can proliferate quickly, spreading the infection.
If the infection reaches the kidneys, it can cause inflammation or pulmonary complications. If you suspect you may have a UTI, contact your health care provider for testing and treatment.
UTIs During Pregnancy: Symptoms, Treatment, Common Questions
Urinary tract infections (UTIs), also known as bladder infections, are the most common type of bacterial infection diagnosed today, according to research published in the American Journal of Medicine. Roughly 31 percent of pregnant women will have either a symptomatic or an asymptomatic (without symptoms) UTI during pregnancy, research suggests. UTIs occur when bacteria enters into the usually sterile urinary tract and multiplies, causing painful urination and other symptoms. Certain factors during pregnancy make this occurrence more likely to happen. Here’s what you need to know to keep you and your baby healthy.
RELATED: 8 Home Remedies for Urinary Tract Infection (UTI) Symptoms
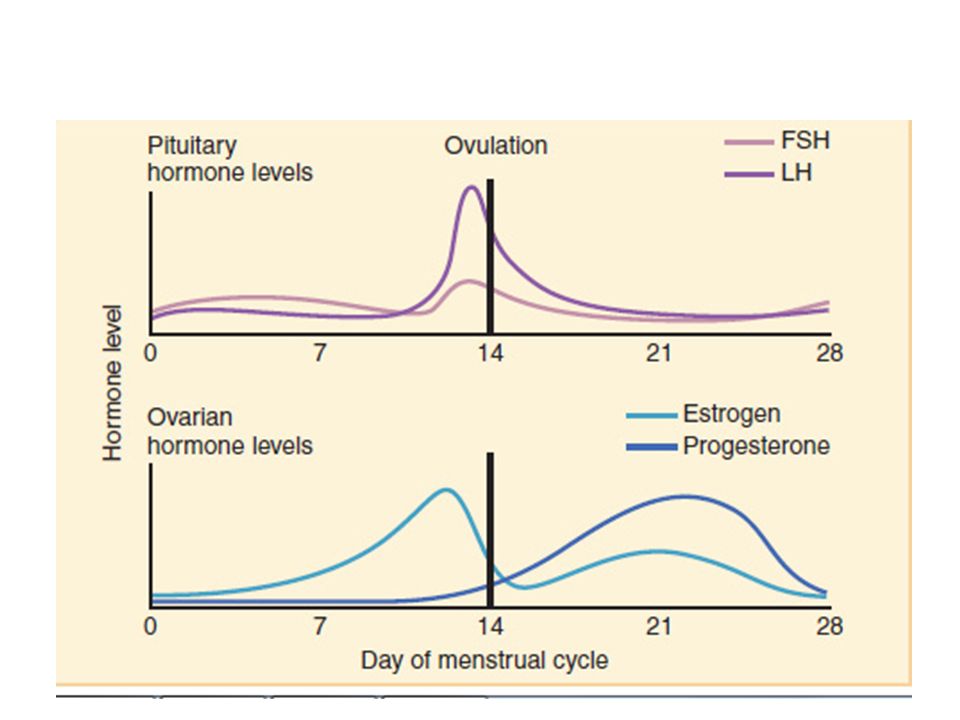
Why Are UTIs Common in Pregnant Women?When you’re pregnant, the anatomy of your urinary tract actually changes. For instance, your kidneys become larger and your growing uterus can compress your ureters and bladder. Because of this compression, fully emptying your bladder during pregnancy becomes more difficult. In addition, your progesterone and estrogen levels increase during pregnancy, which can weaken your bladder and ureters. Pregnancy also alters the makeup of your urine, reducing the acidity and increasing the amount of protein, hormones, and sugar in your urine. That excess sugar, for one, can encourage bacterial growth. All of the above contribute to a heightened chance of developing a UTI in pregnancy. And that is why it’s recommended that all pregnant women receive a urinalysis and urine culture at 12 to 16 weeks or during the first prenatal visit.
Because of this compression, fully emptying your bladder during pregnancy becomes more difficult. In addition, your progesterone and estrogen levels increase during pregnancy, which can weaken your bladder and ureters. Pregnancy also alters the makeup of your urine, reducing the acidity and increasing the amount of protein, hormones, and sugar in your urine. That excess sugar, for one, can encourage bacterial growth. All of the above contribute to a heightened chance of developing a UTI in pregnancy. And that is why it’s recommended that all pregnant women receive a urinalysis and urine culture at 12 to 16 weeks or during the first prenatal visit.
RELATED: 7 Things an Anesthesiologist Wants You to Know About Pain
UTIs by Pregnancy TrimesterYour risk of UTI goes up beginning at week 6 of your pregnancy; the chances you’ll have a UTI vary by trimester.
First TrimesterAbout 41 percent of UTIs are diagnosed during the first trimester.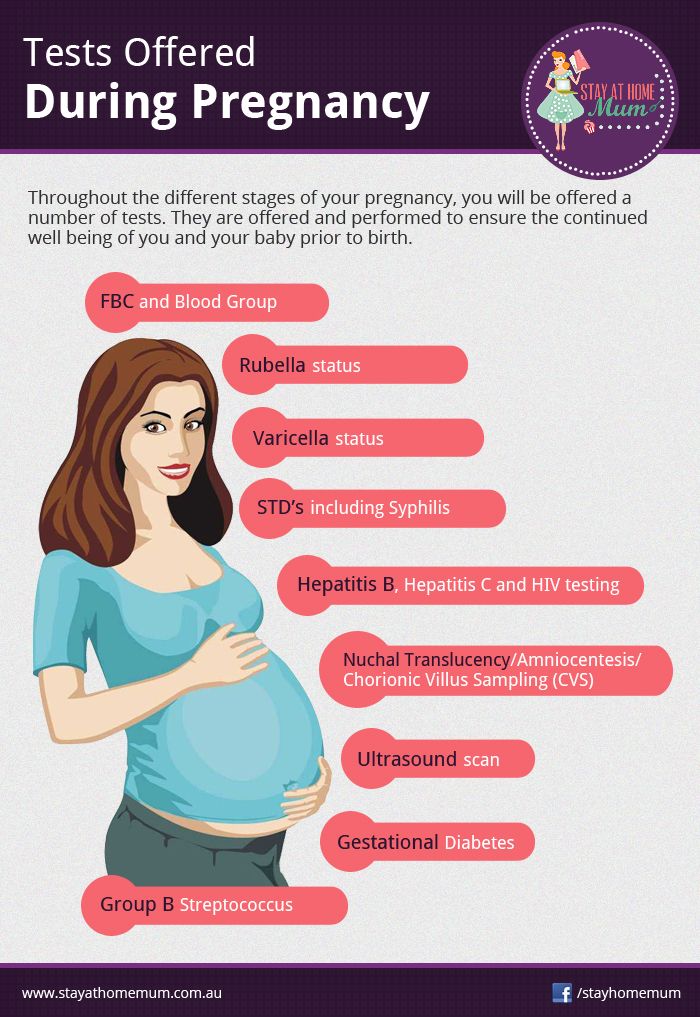 Because getting a UTI during the first trimester is so common, the U.S. Preventive Services Task Force recommends that your healthcare provider obtain a urinalysis and urine culture at your first prenatal visit. That recommendation holds whether you present with UTI symptoms or not.
Because getting a UTI during the first trimester is so common, the U.S. Preventive Services Task Force recommends that your healthcare provider obtain a urinalysis and urine culture at your first prenatal visit. That recommendation holds whether you present with UTI symptoms or not.
According to the Centers for Disease Control and Prevention, about half as many pregnant women are diagnosed with a UTI during their second trimester compared with the first trimester.
Third TrimesterCompared with the second trimester, the number of women who experience a UTI during the third trimester is almost halved. However, 80 to 90 percent of acute kidney infections in pregnancy (many caused by the progression of an untreated UTI) occur in the second and third trimesters, according to research published in the Archives of Medical Science. Thus, it’s recommended to do a repeat urine culture during the third trimester, too.
“While mildly painful urination during pregnancy can often mean a yeast infection, not a UTI, it’s always best to see your healthcare provider if you experience any symptoms,” says Heather Bartos, MD, an ob-gyn in Cross Roads, Texas. After all, research suggests that about 18 percent of UTIs that occur during pregnancy are symptomatic UTIs, meaning the telltale UTI signs and symptoms are present:
- Strong and frequent urge to use the bathroom
- Burning while urinating
- Regularly passing only small amounts of urine
- Cloudy, red, pink or cola-colored urine
- Foul-smelling urine
- Pelvic pain, usually in the center of the pelvis
In pregnancy, women are also more susceptible to asymptomatic UTIs, meaning you have significant bacteria in your urine but your urinary tract is free of signs and symptoms. Experiencing no symptoms, however, does not mean that asymptomatic UTIs are benign. “An asymptomatic UTI can lead to a symptomatic UTI or even a kidney infection,” says Dr. Bartos. In fact, research shows that if asymptomatic UTIs are left untreated, 30 percent of pregnant women will go on to develop a symptomatic UTI, and half of those women will eventually be diagnosed with acute pyelonephritis (a kidney infection). Up to 23 percent will have a kidney infection recurrence during the same pregnancy. It’s important to note that classic UTI signs, like frequent and painful urination, may or may not occur with a kidney infection. Here, some signs to look out for:
“An asymptomatic UTI can lead to a symptomatic UTI or even a kidney infection,” says Dr. Bartos. In fact, research shows that if asymptomatic UTIs are left untreated, 30 percent of pregnant women will go on to develop a symptomatic UTI, and half of those women will eventually be diagnosed with acute pyelonephritis (a kidney infection). Up to 23 percent will have a kidney infection recurrence during the same pregnancy. It’s important to note that classic UTI signs, like frequent and painful urination, may or may not occur with a kidney infection. Here, some signs to look out for:
- High-grade fever
- Chills and rigors (sudden feeling of cold with shivering)
- Headache
- Nausea or vomiting
- Lower back pain
- Flank pain (often right side)
- Possible reduced urine output
“UTIs can rapidly progress to a kidney infection in pregnancy, which can be much more dangerous than a kidney infection in nonpregnant women,” says Bartos. “Severe infections can lead to respiratory problems and sepsis, which can then lead to preterm labor or even the need to urgently deliver the baby.” Beyond a kidney infection, simply having a UTI during pregnancy appears to possibly be a contributing factor to low birth weight. Women who have a UTI in pregnancy also have a 1.31-fold higher risk of developing preeclampsia, a pregnancy complication characterized by high blood pressure, according to a meta-analysis published in September 2018 in the journal Medicine. It’s thought that a UTI may alter a pregnant woman’s inflammatory response, which can spur preeclampsia.
“Severe infections can lead to respiratory problems and sepsis, which can then lead to preterm labor or even the need to urgently deliver the baby.” Beyond a kidney infection, simply having a UTI during pregnancy appears to possibly be a contributing factor to low birth weight. Women who have a UTI in pregnancy also have a 1.31-fold higher risk of developing preeclampsia, a pregnancy complication characterized by high blood pressure, according to a meta-analysis published in September 2018 in the journal Medicine. It’s thought that a UTI may alter a pregnant woman’s inflammatory response, which can spur preeclampsia.
RELATED: National Period Day Is October 19
Can Having a UTI While Pregnant Hurt the Baby?Possibly. “A UTI itself doesn’t hurt the baby directly,” says Bartos. “It’s the failure to treat a UTI that can cause things like preterm birth or, rarely, infection of the amniotic sac.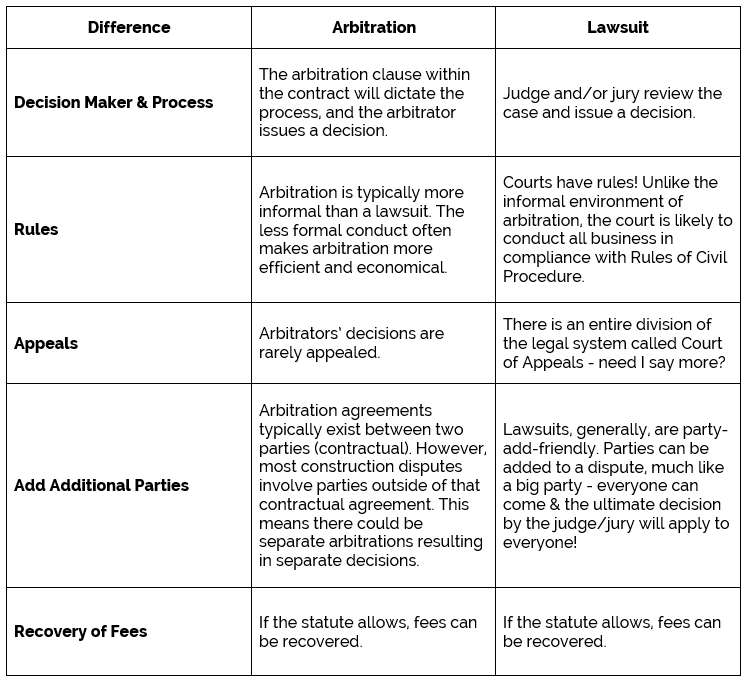 ” For example, research published in American Family Physician shows that treating pregnant women who have asymptomatic UTIs decreases the incidence of preterm birth and low-birth-weight infants. That’s why screening and prompt treatment are important.
” For example, research published in American Family Physician shows that treating pregnant women who have asymptomatic UTIs decreases the incidence of preterm birth and low-birth-weight infants. That’s why screening and prompt treatment are important.
Urinary tract infections are not associated with preterm labor, according to research published in the Journal of the Chinese Medical Association. However, if a urinary tract infection is left untreated, it can progress to a kidney infection. And a kidney infection (pyelonephritis) during pregnancy can modestly increase your chances of early contractions and delivery. Research published in the American Journal of Obstetrics & Gynecology notes that women diagnosed with acute pyelonephritis in pregnancy have a 10.3 percent chance of preterm delivery compared with the 7.9 percent chance among women without a kidney infection during pregnancy.
RELATED: Common Types of Vaginal Infections
Do UTIs Differ by Trimester?At week 6, UTI risk starts to go up, with two-fifths of UTIs occurring during the first trimester. Because of the likelihood of getting a UTI during the first trimester, the U.S. Preventive Services Task Force recommends that pregnant women have a urinalysis and urine culture at their first prenatal visit — whether they have UTI symptoms or not. In the second trimester, about half as many pregnant women are diagnosed with a UTI as in the first trimester, according to the Centers for Disease Control and Prevention, and that number is almost halved again for the third trimester. However, 80 to 90 percent of acute kidney infections in pregnancy (many caused by the progression of an untreated UTI) occur in the second and third trimesters, according to data published in the Archives of Medical Science, so pregnant women should have a repeat urine culture during the third trimester.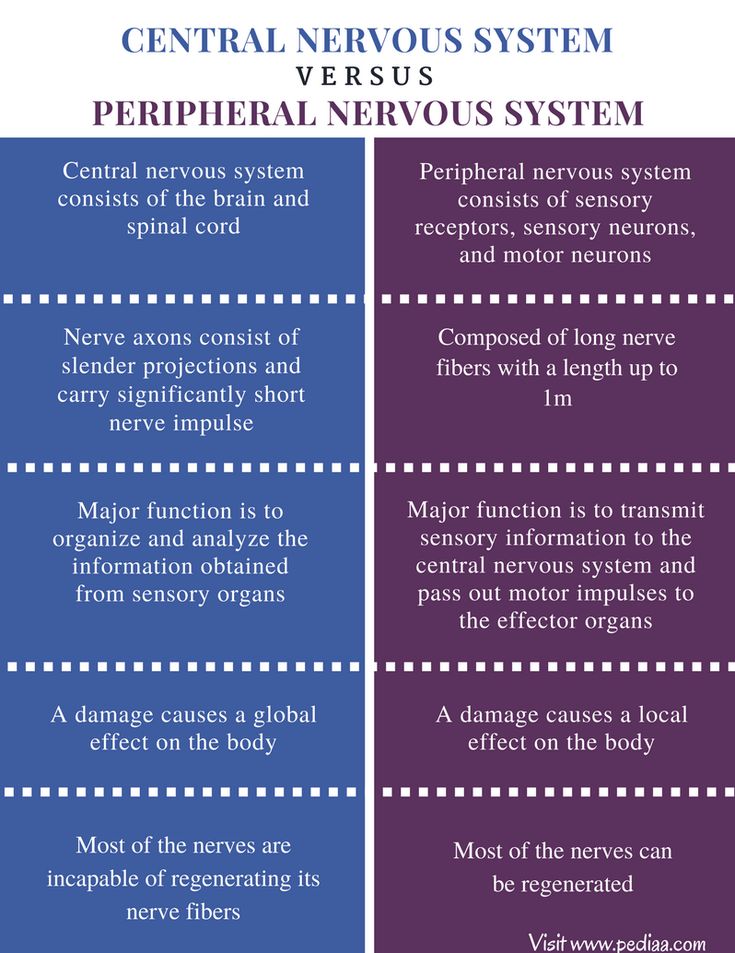
RELATED: March Is Endometriosis Awareness Month
What Are Pregnancy-Safe UTI Treatment Options?How do you treat a UTI when pregnant? It’s similar to how you treat a UTI when not pregnant — with a few key differences. A short-course of antibiotics is the standard treatment for asymptomatic and symptomatic urinary tract infections that occur during pregnancy. There are, however, two important contrasts in treating UTIs in pregnant women versus nonpregnant women. First, asymptomatic UTIs diagnosed during the first trimester are treated with antibiotics, whereas nonpregnant women’s infections are often not treated in this manner. (Outside of pregnancy, asymptomatic bacteriuria is usually not treated with antibiotics.) Also, the preferred antibiotic drugs used to treat UTI in pregnancy often differ than what would be used while not pregnant. For instance, the following antibiotics have not been associated with any birth defects, thus are likely safe to use at any point during pregnancy:
- Penicillins Amoxicillin, ampicillin, and augmentin are in this group.
- Erythromycin Some of the brand names include Ery-Tab, Akne-Mycin, E.E.S. Eryc, and Pediamycin.
- Cephalosporins Keflex (cephalexin) is a cephalosporin.
UTI history and resistance patterns must be considered before prescribing any of these drugs.
Because certain antibiotics pose a potential risk for birth defects (anencephaly, heart defects, and cleft palate) when taken during the first trimester, they are only considered a first-line treatment for UTIs occurring during the second and third trimesters, according to the American College of Obstetricians and Gynecologists. Prescribing the antibiotics listed below during the first trimester is considered appropriate only when no other suitable alternative treatments are available:
- Nitrofurantoin Macrobid, Furadantin, and Macrodantin are in this category.
- Sulfonamides Bactrim (trimethoprim-sulfamethoxazole) is part of this class.
Be sure to double-check what your healthcare provider is prescribing, since despite the warnings, nitrofurantoin remains the most frequently prescribed antibiotic during the first trimester.
Urinary Tract Infections Linked to Bacteria in Meat
E. coli is the leading cause of UTI infections, but a new study reveals that over half a millions cases each year could come from E. coli originating ...
By Lisa Rapaport
What Is a Urinary Tract Infection (UTI)? Symptoms, Causes, Diagnosis, Treatment, and Prevention
A UTI is a common condition that occurs when bacteria migrates into the urinary tract and multiplies. Symptoms include a frequent urge to urinate, even...
By Holly Pevzner
Diagnosing UTI: Tests and Screenings, Early Diagnosis, and Your Doctors
Urinary tract infections (UTIs) can be diagnosed several different ways. Learn about OTC tests, signs of the infection, doctor tests, diagnosis, and recurrent...
By Holly Pevzner
Signs and Symptoms of Urinary Tract Infections
Symptoms of a UTI include pain or burning when urinating, needing to urinate urgently or frequently, and pelvic pain. Learn about early signs, diagnostic...
By Holly Pevzner
How to Prevent Urinary Tract Infections, or UTIs
Help prevent urinary tract infections, or UTIs, with expert tips. Habits such as urinating frequently, as well as after having sex, drinking lots of water...
By Holly Pevzner
Hormone Therapy May Prevent UTIs in Post-Menopausal Women
Age-related estrogen level decreases cause increased risk of urinary tract infections (UTIs).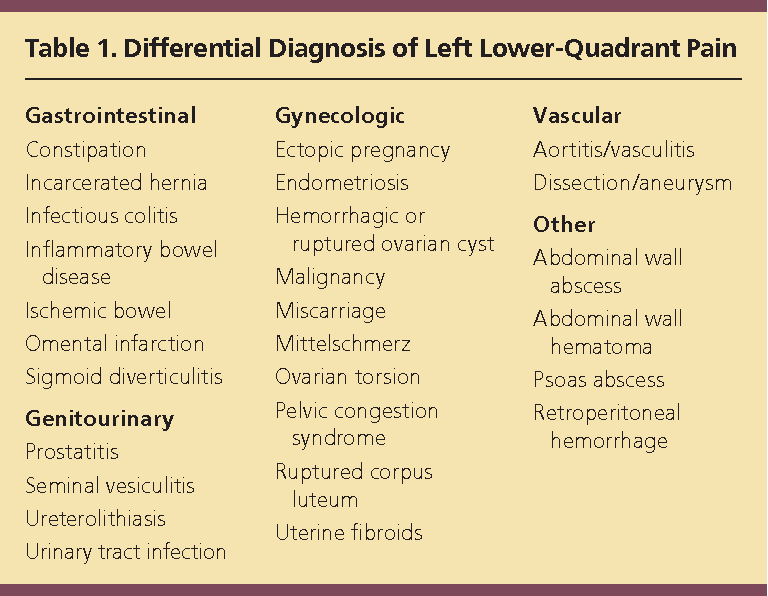 New research hints that when post-menopausal women are treated...
New research hints that when post-menopausal women are treated...
By Meryl Davids Landau
Causes and Risk Factors of UTIs
Urinary tract infection (UTI) risk factors include a history of diabetes, UTIs, or kidney stones; problems in men may relate to prostrate problems while...
By Lindsey Konkel
False pregnancy in women | Symptoms, causes and how to track false sensations of pregnancy
Varvara
Mytishchi
A false pregnancy is a condition that is characterized by signs of pregnancy in its actual absence. This disorder is the result of self-hypnosis in women who passionately dream of a child, or, on the contrary, are afraid of pregnancy and childbirth. As a rule, a false pregnancy develops against the background of hormonal disorders and nervous diseases: neurosis, depression. One of the most striking examples of the development of an imaginary pregnancy is the wife of Nicholas II, Empress Alexandra Feodorovna. After giving birth to four daughters who were not eligible for the throne, she was obsessed with the birth of an heir. For many months, the queen was sure that she was expecting a child, but this was not true.
False pregnancy in women: symptoms
A false pregnancy is accompanied by signs characteristic of a normal pregnancy:
- a woman stops menstruating;
- mood swings are observed;
- mammary glands increase in volume and become painful;
- classic symptoms of toxicosis occur: food preferences change, nausea and vomiting appear;
- growing belly;
- woman feels fetal movements;
- colostrum is secreted from the breast.
These symptoms cannot be called far-fetched. A woman really feels the signs of pregnancy, and they arise due to changes developing in the body.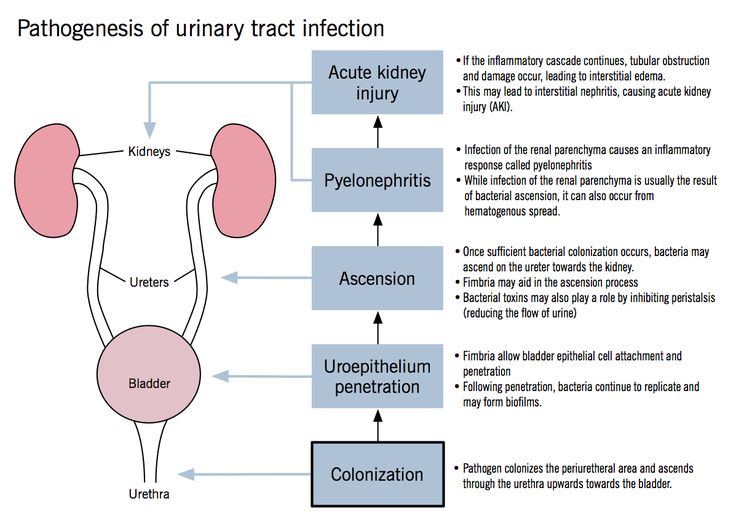 So, for example, the stomach increases due to the growth of subcutaneous tissue, and "baby movements" appear due to constipation and gases.
So, for example, the stomach increases due to the growth of subcutaneous tissue, and "baby movements" appear due to constipation and gases.
False pregnancy in women: causes
The psychological state of a woman plays a large role in the appearance of false symptoms of pregnancy. There are various reasons that stimulate their development:
- the girl is sexually active and burdened by guilt;
- a woman has been unsuccessfully struggling with infertility for many years;
- a woman wants to have a baby to save her marriage;
- a widowed woman;
- a couple is experiencing the death of a child;
- a close friend or relative is pregnant;
- a woman is terrified of childbirth.
In some cases, the psychological factor turns out to be secondary. Physiological causes are leading.
- Hormonal failure. Violations in the endocrine system can lead to amenorrhea - the disappearance of menstruation for six or more months.
 Against the background of this symptom, a woman can convince herself of the onset of pregnancy.
Against the background of this symptom, a woman can convince herself of the onset of pregnancy. - Tumors in the pelvic organs. They can also cause menstruation to stop and obsessive thoughts about the upcoming birth of a child.
In both cases, specialists observe disturbances in the functioning of the central nervous system and hormonal imbalance. In a false pregnancy in women, the level of follicle-stimulating hormone and prolactin increases, and the levels of luteinizing hormone decrease.
How long does a false pregnancy last?
An imaginary pregnancy can last 3-4 months. In exceptional cases, it is delayed up to 7 months, but on condition that the woman refuses to diagnose her condition.
Modern methods for determining pregnancy allow you to confirm or refute a woman's suspicions in a matter of minutes. Pregnancy tests are very popular. They are sensitive to human chorionic gonadotropin (hCG), a hormone that begins to be actively produced from day 2 after implantation of a fertilized egg.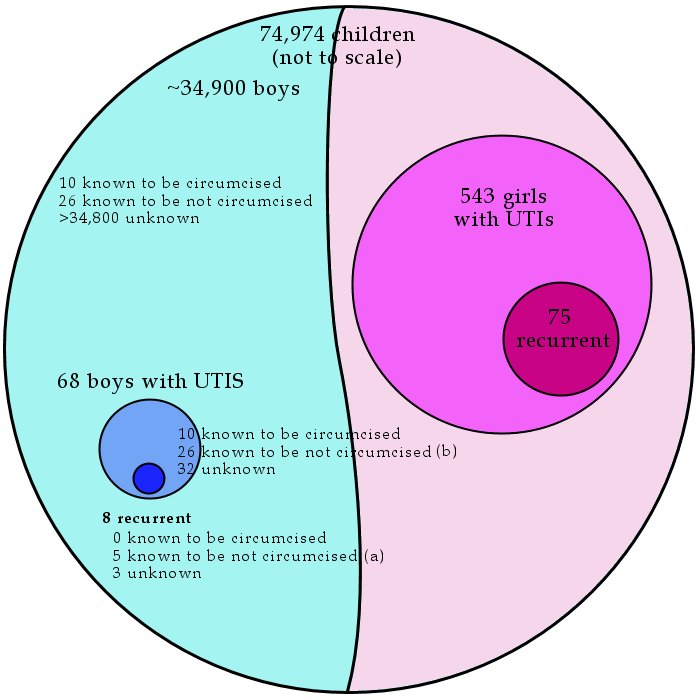 However, in some cases, pregnancy tests are false positive. Errors happen:
However, in some cases, pregnancy tests are false positive. Errors happen:
- if the test is defective;
- if, after a recent termination of pregnancy, embryonic tissue remains in the uterus;
- if the woman is taking fertility drugs containing hCG;
- if the woman has tumors (hydatidiform mole or uterine chorionepithelioma).
For a more accurate diagnosis, it is advisable to contact a gynecologist. The standard list of studies includes:
- Gynecological examination. Objective signs of pregnancy are already visible at 5-6 weeks. The uterus increases in size, and its body softens. The hue of the mucosa also changes - it becomes cyanotic (cyanotic).
- Blood test for hCG. Laboratory research eliminates the error. With the help of the analysis, you can find out the concentration of hCG and the exact gestational age.
- Ultrasound diagnostics. Allows you to detect pregnancy, starting from 3-4 weeks.
If the cause of a false pregnancy is a psychological disorder, the absence of pregnancy may come as a shock to the woman.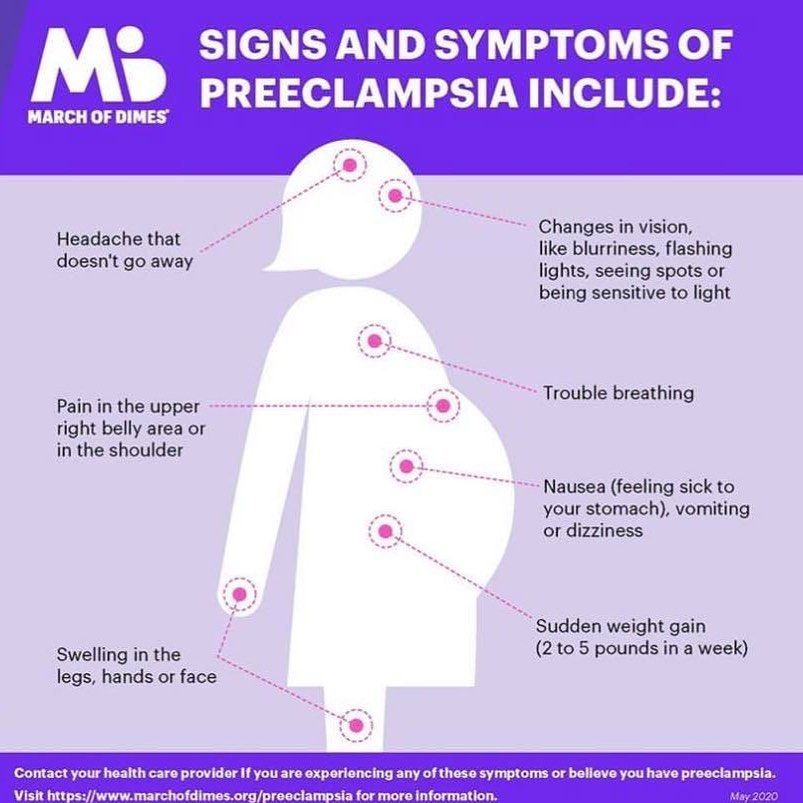 Therefore, during the consultation based on the results of the examination, the doctor should show maximum tact. The imaginary pregnant woman must understand and accept the fact that she is mistaken. After that, the false sensations of pregnancy should disappear. If this does not happen, the help of a psychologist or psychiatrist may be required.
Therefore, during the consultation based on the results of the examination, the doctor should show maximum tact. The imaginary pregnant woman must understand and accept the fact that she is mistaken. After that, the false sensations of pregnancy should disappear. If this does not happen, the help of a psychologist or psychiatrist may be required.
If the symptoms of a false pregnancy are provoked by physiology, a woman needs to undergo an additional examination and find out the exact cause of her condition. In case of hormonal imbalance, experts recommend a course of treatment with combined oral contraceptives (COCs). They normalize the level of hormones in the blood and the menstrual cycle.
Can a false pregnancy be repeated? In the vast majority of cases, this condition does not relapse. A pregnancy that occurs after a false pregnancy, as a rule, turns out to be real.
Topics:
health pregnancy false pregnancy combined oral contraceptives (COCs)
How to distinguish PMS from pregnancy, signs and symptoms of both PMS and pregnancy
Contents
- Symptoms of PMS and early pregnancy
- Diagnosis
- Doctors' advice
Every woman who plans to conceive wants to know how to distinguish PMS from pregnancy. Unfortunately, there are no clear specific signs for these two conditions. An unequivocal answer can only be obtained when conducting specific tests (for example, determining the level of hCG in the body).
Unfortunately, there are no clear specific signs for these two conditions. An unequivocal answer can only be obtained when conducting specific tests (for example, determining the level of hCG in the body).
SYMPTOMS OF PMS AND EARLY PREGNANCY
Signs of PMS and early pregnancy are practically the same. In both states, a woman may be disturbed by typical manifestations. If she previously had no problems before and during menstruation, then any "new symptom" can be regarded by her as a desired conception. However, we should not forget that PMS can also manifest itself in this way. Many patients who experience physical and emotional discomfort during and before menstruation for several years know "their" symptoms very well. Therefore, when such manifestations change, a woman immediately begins to think that "something is wrong." However, one cannot completely rely on "one's own instinct" in this situation.
It should be understood that the body of each woman is individual and the onset of pregnancy may differ from typical standards. Sometimes the absence of "habitual" signs of PMS will indicate an imminent delay. 2.3
DIAGNOSIS
Accurately answer the question: “PMS or pregnancy?” - can test. You can determine the level of hCG (human chorionic gonadotropin) in the urine yourself. There are very sensitive tests that allow three days before the expected menstruation (subject to a stable cycle) to detect the fact of a successful conception.
Also, a woman can go to a gynecologist and donate blood for hCG. An examination by a doctor will help not only to establish pregnancy, but also to identify diseases of the reproductive system, if any. 4
DOCTOR'S ADVICE
Early detection of pregnancy can be difficult if a woman does not keep a menstrual calendar. Therefore, gynecologists advise every month to mark the beginning of "critical days". Since the symptoms of PMS and early pregnancy are very similar, doctors recommend that all patients who suffer from cyclic illness undergo full treatment at the stage of preconception preparation. If, during therapy, undesirable signs cease to occur, it will be easier for a woman to recognize the first manifestations of life emerging in the body. Moreover, the treatment of premenstrual syndrome will prepare the female body for bearing the fetus. After all, it includes a healthy lifestyle, proper nutrition, an adequate daily routine, the intake of herbal remedies with a high content of vitamins, macro- and microelements. One such drug is Time Factor®. It is a non-hormonal complex of vitamins, minerals and plant extracts and can be used for PMS and various disorders of the monthly cycle. 1
References:
- Esina E.V., Svidinskaya E.A. Possibilities of using the vitamin-mineral complex Time-Factor® for the correction of menstrual disorders and the reduction of manifestations of premenstrual syndrome // BC. 2005. No 14, pp. 825–829.
- Yakovleva E.B., Babenko O.M., Pilipenko O.N. Premenstrual syndrome // Emergency Medicine. 2014. No 3 (58). pp.