Passing large clots during miscarriage
Miscarriage - Atlanta Gynecology and Obstetrics
Loss of pregnancy before 20 weeks is called a miscarriage. Spontaneous miscarriage is the most common complication of early pregnancy and the rate decreases as the pregnancy progresses.
Miscarriages occur in 8-20% of clinically-recognized pregnancies:
- 80% of these happen in the first 12 weeks of pregnancy
- The rate of loss for unrecognized or “chemical pregnancies” is 13-26%
- The overall risk of loss after 15 weeks is relatively low
Causes of miscarriage
Though it is difficult to identify what causes all miscarriages, most pregnancy losses are thought to be due to chromosomal defects.
- Chromosomal Abnormalities > 60%
- Maternal: Structural Abnormalities
- Uterine Fibroids, Septums, and Adhesions
- Trauma
- Acute Infections
- Blood Disorders (Thrombophilia)
- Unexplained
Loss of viability of the pregnancy usually occurs between 6-12 weeks. Recognition may not occur until weeks later. The course of treatment that you take will depend on your current condition, your desires, the size of your pregnancy, and your provider recommendations.
Factors associated with miscarriage
There can be many factors that affect the probability of having a miscarriage. In many cases, there is more than one factor that comes into play. If you know what these factors are, you can be more cautious.
- Age: Miscarriage risk increases with age. The risk can be as high as 40% at 40 years old and 80% after 45 years old
- Previous miscarriage: The rate of miscarriage increases with the number of previous miscarriages: 20% after one, 28% after two consecutive, and 43% after three or more consecutive losses
- Smoking: Increases the risk of loss
- Alcohol use: Studies have been inconsistent in proving that alcohol can cause an increased rate of pregnancy loss.
 One study indicated that there was an increase in miscarriages among women who drank more than 3 drinks a day
One study indicated that there was an increase in miscarriages among women who drank more than 3 drinks a day - Cocaine use
- Non-steroid anti-inflammatories (NSAIDs: Ibuprofen, Advil, Motrin): May be associated with an increased risk of miscarriage if used around the time of conception. The prostaglandin in NSAIDs may interfere with proper implantation
- Caffeine: The risks of miscarriage increase with high levels of consumption (>300mg /day)
Miscarriage at home
You may first note mild vaginal spotting and/or cramping. This bleeding and cramping will increase, at which point you may expel the tissue of the pregnancy. During the miscarriage, you may bleed heavily with large clots, soaking a pad every 10-20 minutes. The cramping may be significant. Tylenol and a heating pad are okay to use at this time. You should call the office or the on-call doctor if the heavy bleeding does not improve after two hours.
Once you have passed the pregnancy tissue, you will notice a decrease in bleeding and cramping. You may collect the passed tissue and store it in a clean and dry container and bring it to the office so that it may be sent out for pathological identification. You may call the office or the on-call doctor at any time for direction and advice.
Office Number: 404-299-9724 | After Hours Number: 404-487-2450
D&C at the hospital
A D&C is a surgical procedure performed under anesthesia to remove tissue from the uterus that has not started to or that has not entirely come out.
A D&C is an outpatient procedure that lasts for about 15-20 minutes. You usually go home about 1-2 hours after the procedure is completed. Most women return to light duties and activity the next day. Cramping and bleeding are common after a D&C. You may have bleeding for up to 2 weeks after your procedure.
Alternatively, we offer appropriate candidates a procedure called a Mechanical Vacuum Aspiration (MVA). This procedure is similar to the D&C, but it can be done in the office under local anesthesia. Recovery and warning signs are similar to those of the D&C procedure.
This procedure is similar to the D&C, but it can be done in the office under local anesthesia. Recovery and warning signs are similar to those of the D&C procedure.
With either of these procedures, we recommend that you do not put anything in the vagina (no tampons, douching, or intercourse) until you are seen again in the office.
Warning signs after a miscarriage or D&C
Call the office if you have:
- Temperature > 100.4
- Nausea and vomiting for > 12 hours
- Increasing pain or bleeding
- Foul-smelling vaginal discharge
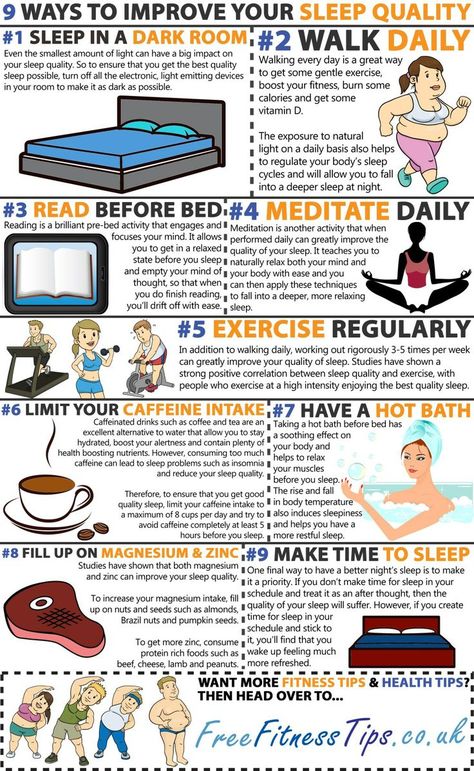
Coping with the loss of pregnancy
Emotional healing can take longer than physical healing. Grief after a pregnancy loss is a normal response. In the days and weeks after your pregnancy loss, you may experience a loss of appetite, emotional changes, irritability, sleep disturbances, and inability to focus on daily tasks. This is all normal and should resolve in a few weeks or months. If you find that these symptoms are severe or that you are unable to cope with these feelings, please call and make an appointment to talk to a provider in our practice. We will be able to help you and make any other referrals you may need.
If you find that these symptoms are severe or that you are unable to cope with these feelings, please call and make an appointment to talk to a provider in our practice. We will be able to help you and make any other referrals you may need.
The next pregnancy
Your next period should come within 4-6 weeks after your miscarriage. We recommend that you use contraception until after you have had a normal period. You may continue prenatal vitamins during and after this time. You may also discuss birth control at your post-miscarriage visit if you do not desire to become pregnant again.
What does a miscarriage look like? Symptoms and seeking help
Miscarriage, or pregnancy loss, can look and feel different for each person. Common symptoms include bleeding and cramping.
It is important to note that bleeding is common during pregnancy — especially in early pregnancy. It does not necessarily mean that anything is wrong.
The only way to accurately identify a pregnancy loss is to test pregnancy hormone levels and have an ultrasound of the uterus.
Read on to learn more about what pregnancy loss can look and feel like.
According to a 2016 study, not all pregnancy losses involve bleeding. Overall, they do not follow a single pattern. This is why it is crucial to seek medical care for bleeding and any unusual symptoms during pregnancy.
Pregnancy loss during the first trimester may involve:
- heavy bleeding
- bleeding that starts light and gets heavier
- passing blood clots or tissue
- cramping, which may come in waves
- a gush of fluid from the vagina
If a person takes a pregnancy test after experiencing a pregnancy loss during the first trimester, the result may be negative, or the test may have a positive line that gets fainter.
Experiencing pregnancy loss later in the first trimester and beyond will involve passing more tissue.
Second-trimester pregnancy loss can also cause intense cramping and sometimes even contractions.
In addition to bleeding and cramping, some people may notice larger blood clots.
According to a 2019 meta-analysis, one-quarter of pregnant women experience bleeding during the first trimester. Another study from 2016 puts that percentage higher, at closer to 20–40%.
A large-scale 2010 study found that about 12% of pregnant women experienced pregnancy loss, and about two-thirds of that group reported bleeding during their pregnancy.
Some differences between bleeding due to a pregnancy loss and other types of bleeding during pregnancy include:
- Amount of blood: Heavy bleeding is more likely to signal a pregnancy loss.
- Bleeding pattern: Bleeding that gets progressively heavier may indicate a pregnancy loss.
- Pain: Cramping, especially when it occurs in a clear pattern, is more likely to signal a pregnancy loss.
- Passing tissue: Some — not all — people who experience a pregnancy loss pass large blood clots or tissue.
For people who do experience bleeding during a pregnancy loss, the duration tends to depend on how far the pregnancy has progressed.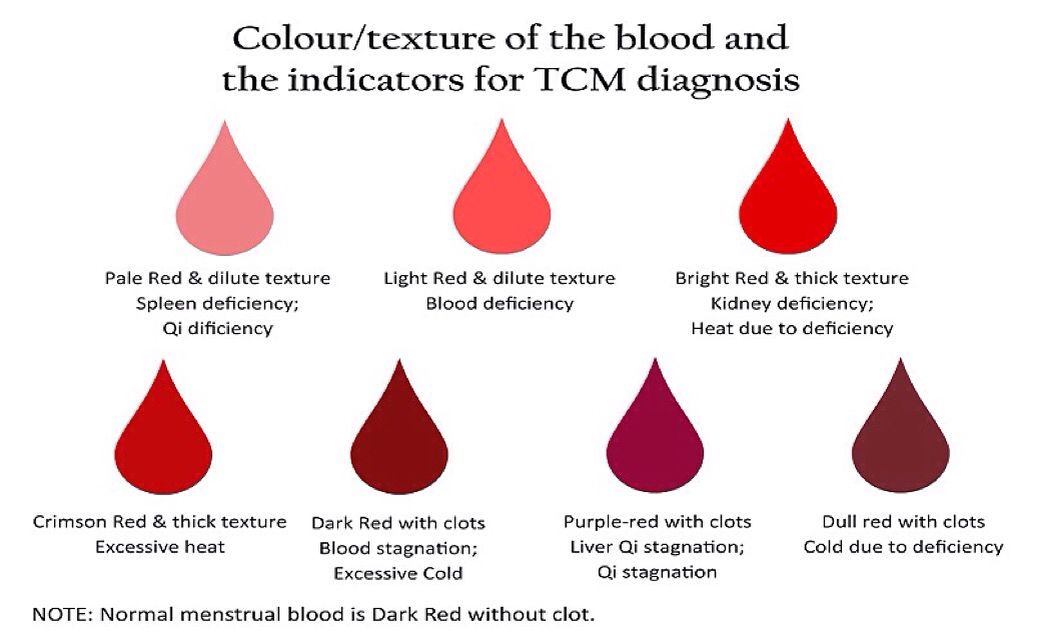
Pregnancy losses that occur in the first weeks of pregnancy tend to cause bleeding that lasts a few days. Those that occur later may cause bleeding that lasts for as long as 4 weeks.
Sometimes, the bleeding stops and starts again. Over time, it should get lighter.
A very early pregnancy loss is sometimes called a chemical pregnancy. These pregnancies are lost shortly after the embryo implants, usually within a few days or weeks.
A chemical pregnancy may be detectable by a pregnancy test, but it would likely not be seen on an ultrasound.
In many cases, early pregnancy losses can happen before a person knows they are pregnant.
In fact, around 80% of early pregnancy losses occur in the first trimester, or in weeks 0–13. The end of these early pregnancies may be mistaken for a period because the symptoms are similar.
For example, both a period and an early pregnancy loss can involve bleeding and cramping. Pregnancy tissue that passes out of the vagina may look like typical blood clots that occur during a period.
It is possible that a person will not realize they have missed a period. Instead, they may mistake the symptoms of a pregnancy loss for those of a menstrual period.
Pregnancy losses and periods can both cause:
- vaginal bleeding
- passing blood clots or tissue
- abdominal pain
However, a pregnancy loss will often cause additional symptoms that set it apart from a period, especially if the pregnancy loss occurs several weeks into the pregnancy. These symptoms include:
- larger clots or pregnancy loss tissue
- more clots than typical periods
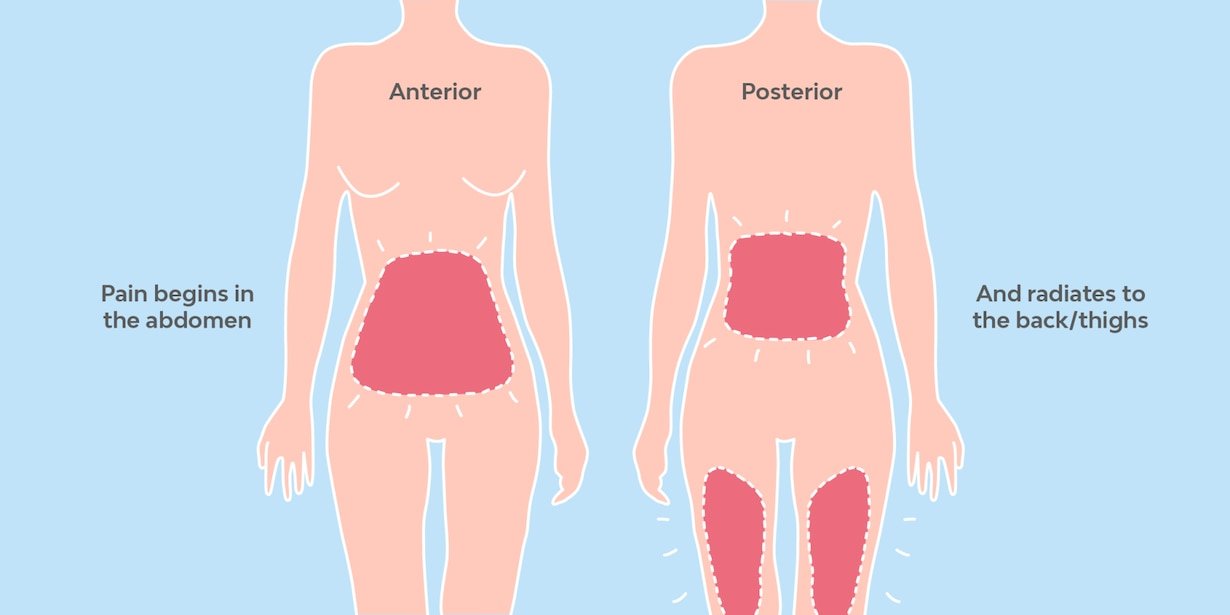
- lower abdominal cramping
- back pain
- passing a significant amount of clear or pinkish fluid
- sudden heavy bleeding, or heavier bleeding than a typical period
- longer bleeding
- sudden easing of some early pregnancy symptoms, such as nausea and breast tenderness
It is important to remember that bleeding during the first weeks of a pregnancy is not uncommon, and it is not always a sign of pregnancy loss or a problem with a pregnancy.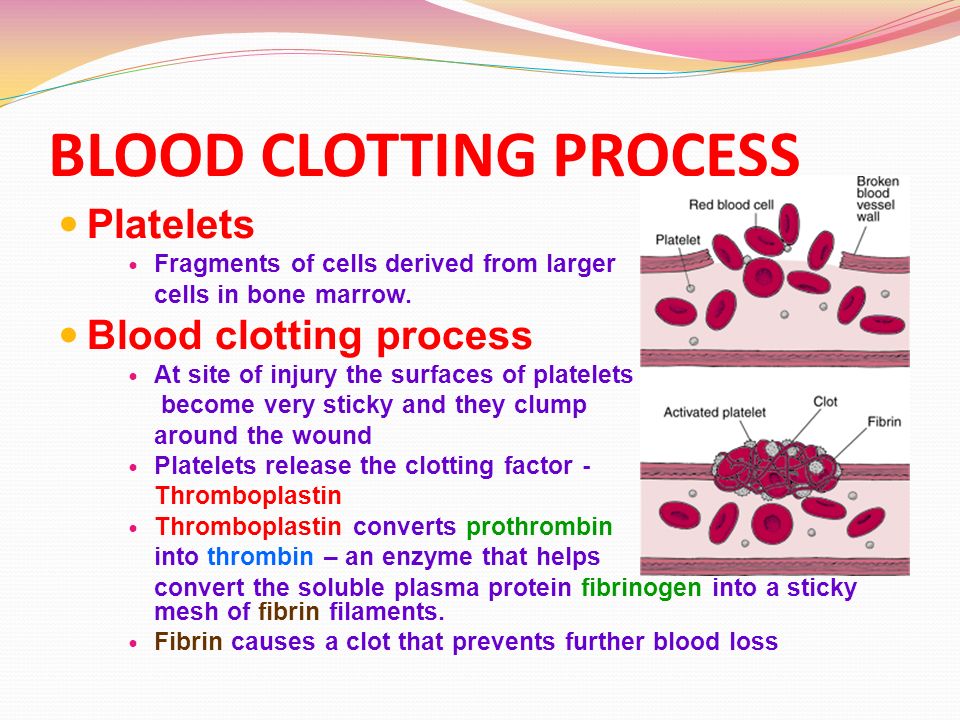
However, if a person experiences other symptoms of pregnancy loss, they should seek care from a doctor.
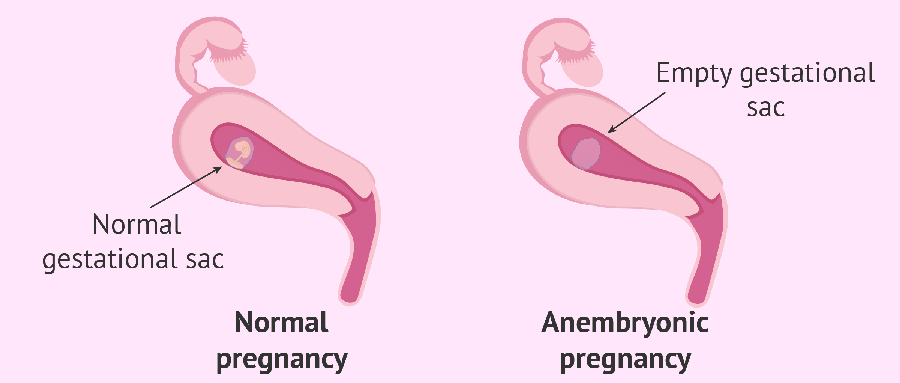
A “missed miscarriage” refers to a delay between the loss of the pregnancy and any bleeding or passing of tissue.
During a missed miscarriage, an embryo dies but does not leave the uterus for several weeks. In fact, a pregnant person may not realize the pregnancy has ended until an ultrasound finds no heartbeat.
When the embryo does leave the uterus, the blood, tissue, and clots may be dark brown. The tissue has had time to deteriorate, so bright red blood or heavy bleeding may not occur. The bleeding may last several days to several weeks.
A doctor may prescribe medication to help the person who has had the pregnancy loss bleed and pass the tissue. Surgery may also be necessary.
It is not possible for healthcare professionals to stop a pregnancy loss once it starts.
Call a doctor and schedule an appointment within 24 hours if any of the following occur:
- vaginal bleeding
- a fever
- intense pain or cramping
- bleeding that stops and starts again
- any other changes in the pattern of bleeding, even if a doctor has already addressed the cause
- bleeding that lasts for longer than 7 days, even if a doctor has already confirmed pregnancy loss
Pregnant people should receive emergency medical attention if they:
- experience heavy bleeding during the second trimester and cannot reach their doctor
- bleed heavily enough to soak through more than one pad per hour for more than 2 hours
- feel faint, lightheaded, or confused
- experience contractions, amniotic fluid leakage, the water breaking, or other signs of premature labor
Most pregnancy losses pass on their own.
In some cases, the fetus dies without causing any bleeding. When this happens, the person carrying the fetus may want to wait for the pregnancy to pass on its own or want it to be over as quickly as possible.
If a person wants to expedite a pregnancy loss, a doctor can supply medication that helps with passing the pregnancy at home. This approach is safest during early pregnancy.
A healthcare professional can also perform surgery to remove the remains of the embryo or fetus.
Sometimes a pregnancy loss is incomplete, leaving behind tissue that can lead to infection or other health problems. When this happens, a doctor may recommend medication or surgery.
Doctors used to advise couples to wait 1 month, or sometimes much longer, before trying to conceive again after a pregnancy loss.
However, research now shows that there is no medical justification for this recommendation. If a couple feels ready, it is safe to begin trying to conceive again right away.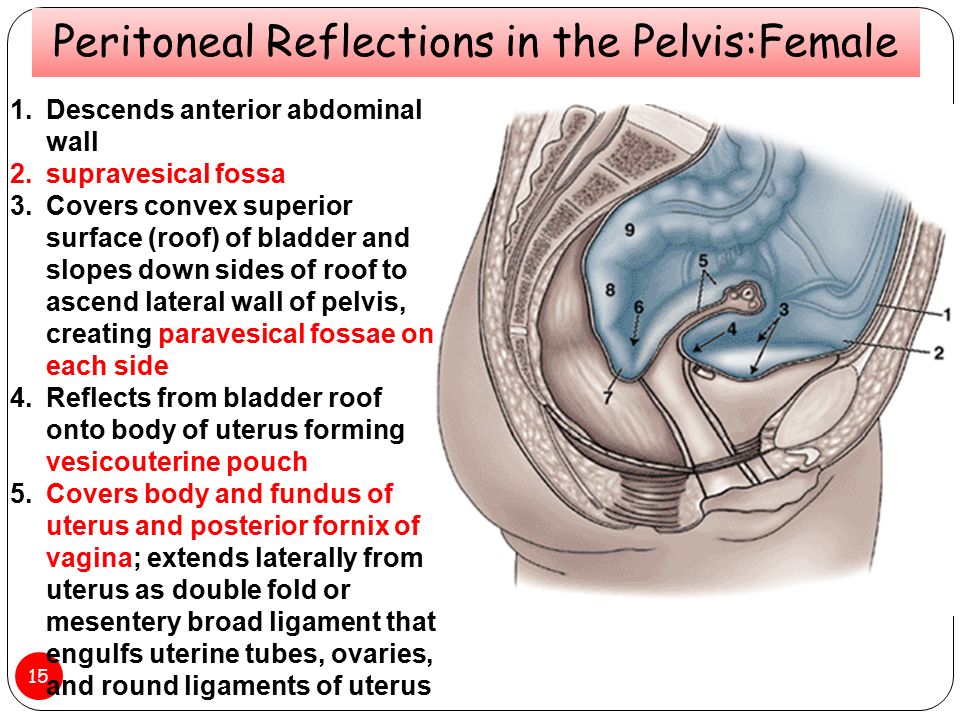
A 2017 study indicates that fertility may even be slightly higher immediately following a pregnancy loss.
Sometimes, however, it takes a while for a menstruating person’s cycle to resume following a pregnancy loss.
This can make it difficult to time sexual intercourse for conception and to accurately date a pregnancy — especially if a person becomes pregnant before the first menstrual period after a pregnancy loss.
To improve accuracy, it can be helpful to:
- monitor basal body temperature
- use ovulation tests
- try other ways to predict fertility
Early pregnancy losses can sometimes result from chromosomal irregularities. This means that the developing embryo or fetus has an irregular number of chromosomes.
These irregularities usually occur at random, meaning they are unlikely to reoccur. In other words, experiencing one pregnancy loss does not increase the likelihood of experiencing another.
A 2017 study finds that 15. 7% of women with a previous pregnancy loss had another during the 2-year study period.
7% of women with a previous pregnancy loss had another during the 2-year study period.
Meanwhile, a 2016 study finds that women were more likely to become pregnant in the 3 months following a pregnancy loss.
Many people become pregnant again shortly after a pregnancy loss, and a smaller number experience multiple losses in a row.
The risk of repeat pregnancy losses increases with age, according to a 2019 study. The risk is also higher among people with a history of:
- preterm labor
- gestational diabetes
- stillbirth
- cesarean delivery
A 2017 study found that 15.7% of participants whose most recent pregnancy ended in a pregnancy loss went on to have a second pregnancy loss.
A 2018 study focused on women who had three or more pregnancy losses. This study found that 64.5% of those women had a live birth within 5 years. Some of these participants may have received fertility treatments.
Pregnancy loss is one of the less common causes of bleeding during pregnancy, especially when the bleeding occurs early on.
But bleeding in early pregnancy is not always a sign of pregnancy loss.
Some other signs of pregnancy loss include cramping and passing blood clots or tissue.
Only a healthcare professional can accurately identify a pregnancy loss. For this reason, it is important to consult a doctor or nurse midwife about any bleeding during pregnancy.
What does an early miscarriage look like?
Bleeding is common in the early weeks of pregnancy. That is why bleeding alone should not be seen as an indication of an early pregnancy loss.
In addition to bleeding, an early pregnancy loss may cause a person to experience:
- a gush of clear or pale pink fluid from the vagina
- passing blood clots or tissue
- a sudden decrease in pregnancy symptoms (such as nausea and morning sickness)
- a negative result on a pregnancy test, or a positive sign that is very faint
How do I know if I’m miscarrying?
The signs and symptoms of a pregnancy loss will remain largely the same, no matter the week. But the further along a person is, the greater the amount of tissue loss during the miscarriage.
Symptoms of pregnancy loss include:
- sudden bleeding, sometimes heavy
- a gush of clear or pink fluid from the vagina
- mild to severe back pain and abdominal cramping
- contraction-like pain
What does miscarriage tissue look like?
The clots and tissue passed during a pregnancy loss may look like typical period clots, or they may be larger.
Pregnancy loss tissue includes:
- the fetus or embryo
- gestational sac
- placenta
When a pregnancy is more advanced (after 6 to 8 weeks), the gestational sac may be noticeable. Before that, it may be too small to see.
The tissue passed during a pregnancy loss may be:
- brown
- black
- dark red
- bright red or pink
- white or gray, in some cases
If the pregnancy began to deteriorate before the start of bleeding, the clots may be smaller and darker. This is common with a missed miscarriage.
What does miscarriage tissue vs. a blood clot look like?
It is not always easy to tell the difference between pregnancy loss tissue and a blood clot. Both may look like typical period clots, though it is not uncommon for them to be larger than normal.
Actual pregnancy tissue may not be discernible until after the eighth week. Then, the tissue may look like pink, white, or gray tissue. A person may also be able to see a fluid-filled sac in the passed tissue.
Blood clots during menstruation, why large blood clots can come out during menstruation, what to do
Contents
- Physiological causes
- Predisposing factors
- When do blood clots during menstruation indicate gynecological pathology?
Normal menstruation is the basis of a woman's reproductive health. The concept of the norm includes regular (every 21–35 days) painless menstruation, during which 40–150 ml of blood is released within 3–7 days. Menstrual flow has a dark red or brownish (at the end of the cycle) color and a uniform consistency. 1
Any deviation from the specified parameters should alert the woman. One of the most common concerns is blood clots during menstruation
PHYSIOLOGICAL CAUSES
Menstruation occurs after an egg produced by the female body has not been fertilized. The inner layer of the uterus (endometrium), where the embryo was supposed to be fixed, is rejected. Menstrual flow is thicker than normal blood, precisely due to the content of endometrial tissue in it. Why can blood clots form during menstruation in absolutely healthy women? The fact is that when walking and other active movements, menstruation comes out gradually and freely. However, after a night's sleep or sitting for a long time, a woman may notice the release of one or more jelly-like clots. This happens because the blood lingers in the uterus and has time to clot. Also, the appearance of thickening contributes to a large amount of secretions. The alternation of heavy and scanty menstruation is characteristic of periods of hormonal changes (puberty, premenopause).
PREDISPOSING FACTORS
In order to understand why menstruation comes with blood clots, we list the possible causes of this process:
Hormone therapy, taking oral contraceptives. The appearance of such a side effect of drugs as increased menstrual bleeding is often observed with the independent use of drugs without consulting a gynecologist.
Hormone therapy, oral contraceptives. The appearance of such a side effect of drugs as increased menstrual bleeding is often observed with the independent use of drugs without consulting a gynecologist.
First menstruation after abortion or gynecological surgery.
Heavy periods may be the only symptom of early miscarriage. Elements of the fetal egg, which look like a small clot, can be detected by a woman, but more often go unnoticed.
WHEN DO THE BLOOD CLOTTS DURING THE MENTOR SAY ABOUT GYNECOLOGICAL PATHOLOGY?
The main pathological causes of this process are:
- Endometriosis is the growth of endometrial-like tissue outside the uterus.
A variation of this disease is adenomyosis, in which the inner lining of the uterus grows into its muscle tissue. Both of these pathologies are accompanied by pain in the lower abdomen and heavy prolonged menstruation. If during menstruation a large blood clot came out, resembling a liver in appearance, then there is reason to suspect that the patient has one of these diseases.
- Uterine polyps - focal hyperplasia of the endometrium in the form of single or multiple formations on a wide base or on a stalk. One of the manifestations of the disease is an increase in the amount of menstrual flow. The appearance of large clots is especially often caused by a polyp, which is located on the cervix, as it prevents the timely release of secretions.
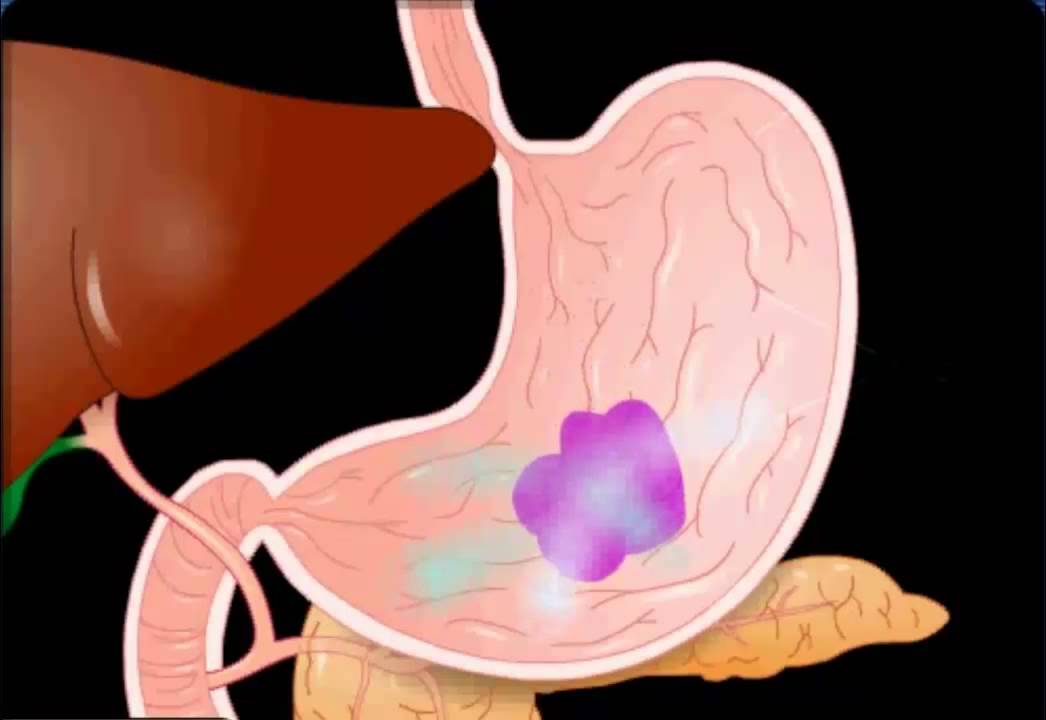
- Uterine fibroids. The growth of this benign tumor-like formation leads to the appearance of pain, as well as lengthening and intensification of menstrual bleeding.
In addition, blood during menstruation may be released more slowly and thicken in some congenital pathologies. These include such anomalies in the structure of the female genital organs, such as a saddle, bicornuate or septate uterus.
WHAT TO DO IF THERE IS BLOOD CLOTS?
In case of any changes in the nature of menstruation (their frequency, duration, consistency, etc.), a woman should visit a gynecologist. In the event that large blood clots come out during menstruation, this must be done as quickly as possible. The doctor will interview the patient in detail, conduct a gynecological examination and prescribe the necessary laboratory and instrumental studies to the patient. After identifying the exact cause of the phenomenon, treatment of the underlying disease is prescribed, which led to the appearance of thickening of menstrual blood. It is impossible to figure out on your own why blood clots appear during menstruation. At the same time, a specialist can easily determine the cause of this symptom and effectively eliminate it. Self-medication for various menstrual irregularities can be very dangerous due to the development of serious complications and even infertility.
References:
- Smetnik V.P. All about menstruation.
Pieces of meat during menstruation is an egg or a miscarriage?
#1
#2
#3
#4
#5
You can't see an egg with the naked eye, no matter how hard you try.
#6
Guest
This is a piece of endometrium
Your "Yaza Yaza" is simply the most large coast endometrium. The egg itself is transparent and negligible for you to notice.
#9
#10
#13
Japanese samurai
Stay away, nifiga! it's the author's liver falling out.
ahhahaaa)))))))))))))
#14
#15
#16
#18
#20
#21
#22 900
GOST
GOSTIC blood clots look like pieces of meat. well, sho for youth went a
#24
Guest
The endometrium does not come out in pieces, donate blood for coagulation for hemostasis and d_dimers, most likely you have a tendency to form blood clots. Not a good sign, fraught with endometriosis. October 24, 2010 23:55
#26
Guest
why doesn't it come out in pieces? Well, not in pieces of course, but in formations up to 2cm. Is it a lot?
#27
Audrey
Guest
Why doesn't it come out in pieces? Well, not in pieces of course, but formations up to 2cm. Is it a lot?
It always happens to me, even before pregnancy I asked the gynecologist when I wanted to get pregnant, then my period came with a delay, I thought it was a miscarriage, so she told me everything in detail! so it's ok! I have 1-2 pieces. such, it happens that they are very tiny or not
Woman.ru experts
-
Vladimir Weiss
Neopsychologist
102 answers
-
Vladimir Titarenko
Fitness nutritionist
218 answers
-
Maria Burlakova
Psychologist
350 answers
-
Sadovnikov Ernest
Psychologist....
100 answers
-
Ivanova Svetlana
Coach
91 answers
-
Yuri Anatolyevich Ionov
Psychologist, Supervisor,.
..
13 answers
-
Anna Antonchik
Female psychologist
231 answers
-
Nikita Nosov
Practicing psychologist
43 answers
-
International Institute
Psychology, psychotherapy,...
26 answers
-
Maxim Sorokin
Practicing psychologist
1 055
#28
Marquise
This is the endometrium, which grows by the beginning of menstruation and is rejected every month under the influence of hormones. The endometrium is rejected in the form of clots, the vessels at the site of its separation are exposed and bleed - this is the so-called. "period".
You can't see an egg with the naked eye, no matter how hard you try.
#29
Anna
This is the endometrium. Nutrient "soil" for a fertilized egg, which covers the inner surface of the uterus during ovulation. If the egg is not fertilized, then this "soil" is rejected by the uterus and comes out in the form of bleeding. In the next cycle, the process is repeated. Your "piece of meat" is simply the largest endometrial clot. The egg itself is transparent and negligible for you to notice.
#30
Audrey
KitKat
Endometrium is....What kind of people are gone...they don't know shit about their body. ..
Go to the gynecologist, let him give you a lecture!
#31
Invented stories
-
I am infuriated with my children and grandchildren ...
1 509 answers
9000 9000 9000 9000man Immediately warned. that all property is registered on children
1 149 answers
-
This salary - I don't want to work
759 answers
-
A 22 year long lie. How to destroy?
1016 answers
-
Husband left, 2 months of depression... How will you cope if you are left all alone?
207 answers
So an ultrasound or hcg will give you a concrete answer.
Not very competently, but she told me as best she could.
#33
Guest
The author, I had a delay, went for an ultrasound, they said I was pregnant, the period was 2 weeks. And suddenly menstruation begins with huge clots. I arrive at the hospital, the doctor says she is no longer pregnant, everything came out in these clots. And she also told me that I was so meticulous, I went for an ultrasound ahead of time, and found out that I was pregnant, and if I hadn’t gone, I wouldn’t have paid attention to these clots. He says that many women do not even know that during menstruation they have a spontaneous miscarriage for a short time. So an ultrasound or hCG will give you a specific answer. Not very well, but as she could tell.
#34
#35
#36
#36 #36
#36 #36 #36 #36 #36 #36 #36 #36 #36 #36 #36 #36 #36 #36 #36 #36 #36 #36
Has anyone experienced this?
So far, there is no way to go to the doctor. I am in another city ..
#38
#39
#40
#41
Natalie
Girls, tell me, please, I'm 3 weeks pregnant, but my period started with big clots she said that most likely a miscarriage and an ultrasound should be done and advised to do a test. The test is positive, but she hasn’t done an ultrasound yet. What could it be?
#42
New Topics
-
Why do overweight girls not want to lose weight?
10 answers
-
Miscarriage and vacuum aspiration: how it happened Before going to bed I measure the pressure
8 answers
-
How to treat a herniated disc?
8 answers
-
Suggest a strong sedative
9 answers
#43
#44
I also have
#45
#46
#47
#48
Nu here and think what it was.