Preeclampsia medical management
Preeclampsia - Diagnosis and treatment
Diagnosis
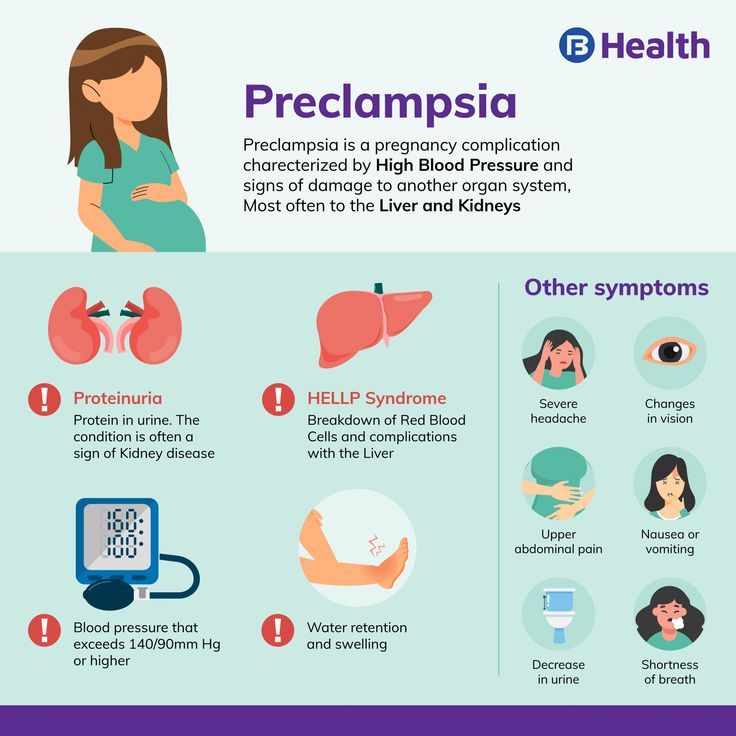
A diagnosis of preeclampsia happens if you have high blood pressure after 20 weeks of pregnancy and at least one of the following findings:
- Protein in your urine (proteinuria), indicating an impaired kidney
- Other signs of kidney problems
- A low blood platelet count
- Elevated liver enzymes showing an impaired liver
- Fluid in the lungs (pulmonary edema)
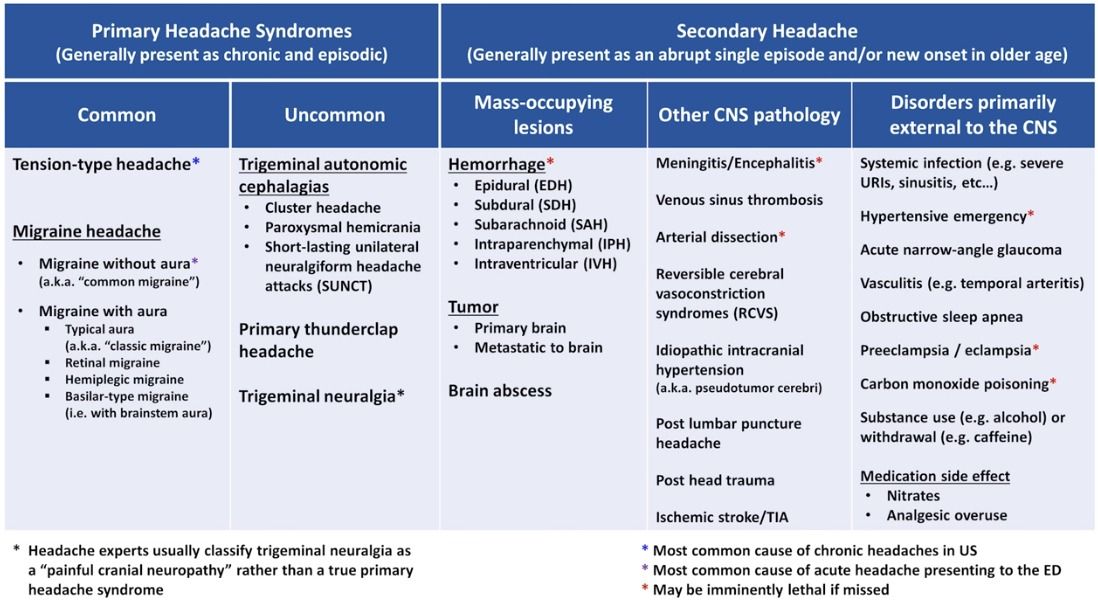
- New headaches that don't go away after taking pain medication
- New vision disturbances
High blood pressure
A blood pressure reading has two numbers. The first number is the systolic pressure, a measure of blood pressure when the heart is contracting. The second number is the diastolic pressure, a measure of blood pressure when the heart is relaxed.
In pregnancy, high blood pressure is diagnosed if the systolic pressure is 140 millimeters of mercury (mm Hg) or higher or if the diastolic pressure is 90 mm Hg or higher.
A number of factors can affect your blood pressure. If you have a high blood pressure reading during an appointment, your health care provider will likely take a second reading four hours later to confirm a diagnosis of high blood pressure.
Additional tests
If you have high blood pressure, your health care provider will order additional tests to check for other signs of preeclampsia:
- Blood tests. A blood sample analyzed in a lab can show how well the liver and kidneys are working. Blood tests can also measure the amount of blood platelets, the cells that help blood clot.
- Urine analysis. Your health care provider will ask you for a 24-hour urine sample or a single urine sample to determine how well the kidneys are working.
- Fetal ultrasound. Your primary care provider will likely recommend close monitoring of your baby's growth, typically through ultrasound. The images of your baby created during the ultrasound exam allow for estimates of the baby's weight and the amount of fluid in the uterus (amniotic fluid).
- Nonstress test or biophysical profile. A nonstress test is a simple procedure that checks how your baby's heart rate reacts when your baby moves. A biophysical profile uses an ultrasound to measure your baby's breathing, muscle tone, movement and the volume of amniotic fluid in your uterus.
More Information
- Nonstress test
Treatment
The primary treatment for preeclampsia is either to deliver the baby or manage the condition until the best time to deliver the baby. This decision with your health care provider will depend on the severity of preeclampsia, the gestational age of your baby, and the overall health of you and your baby.
If preeclampsia isn't severe, you may have frequent provider visits to monitor your blood pressure, any changes in signs or symptoms, and the health of your baby. You'll likely be asked to check your blood pressure daily at home.
Treatment of severe preeclampsia
Severe preeclampsia requires that you be in the hospital to monitor your blood pressure and possible complications.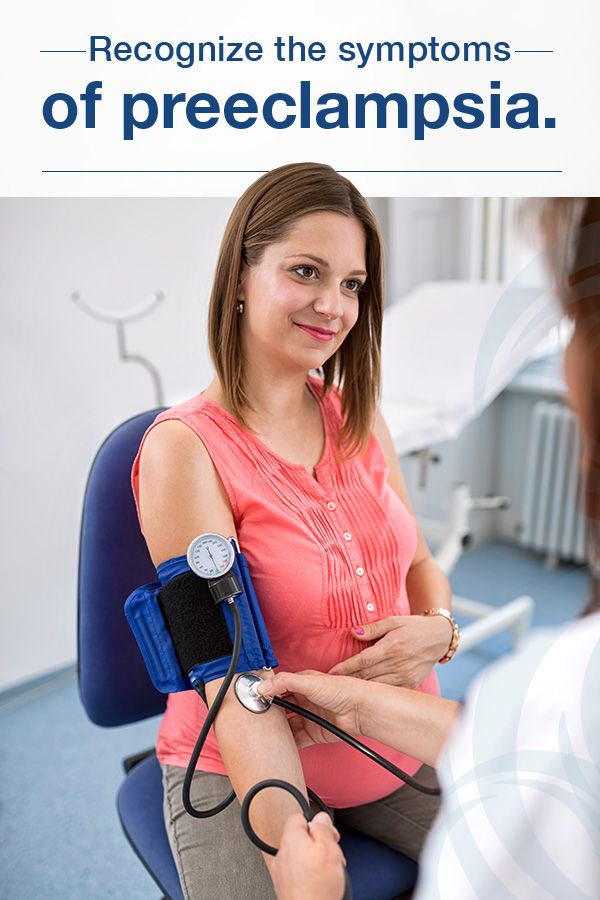 Your health care provider will frequently monitor the growth and well-being of your baby.
Your health care provider will frequently monitor the growth and well-being of your baby.
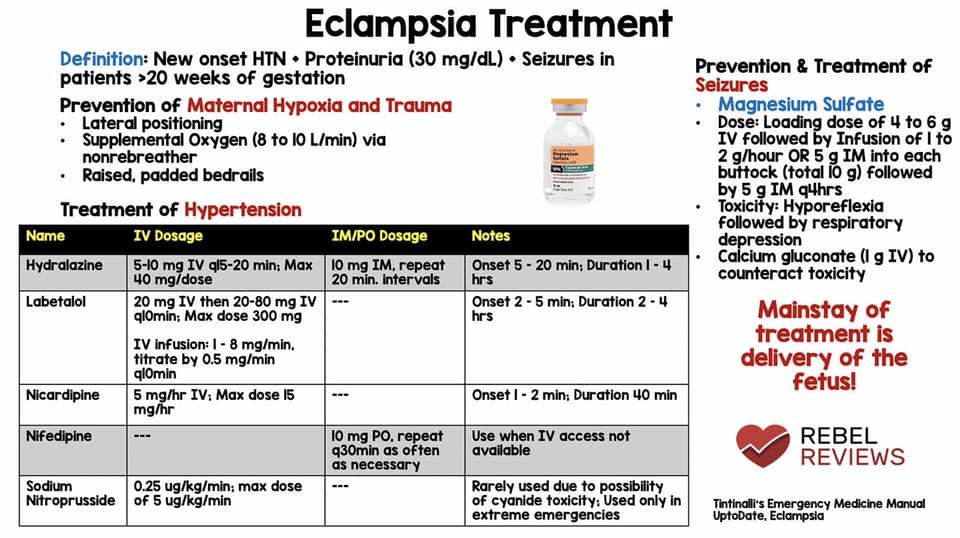
Medications to treat severe preeclampsia usually include:
- Antihypertensive drugs to lower blood pressure
- Anticonvulsant medication, such as magnesium sulfate, to prevent seizures
- Corticosteroids to promote development of your baby's lungs before delivery
Delivery
If you have preeclampsia that isn't severe, your health care provider may recommend preterm delivery after 37 weeks. If you have severe preeclampsia, your health care provider will likely recommend delivery before 37 weeks, depending on the severity of complications and the health and readiness of the baby.
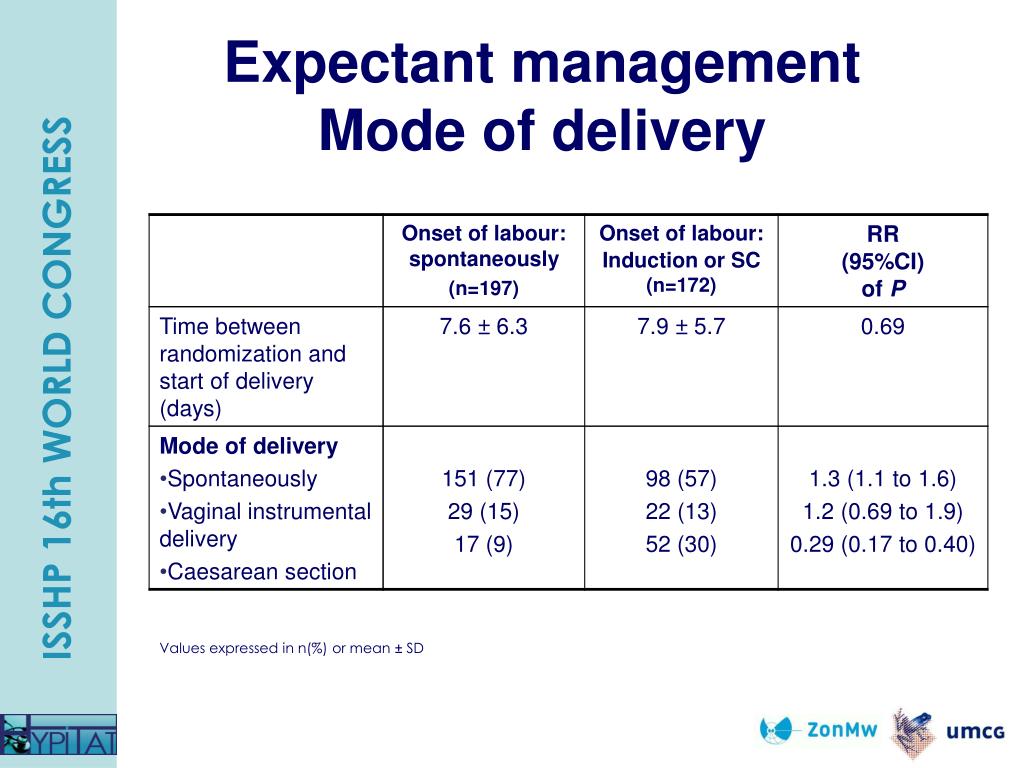
The method of delivery — vaginal or cesarean — depends on the severity of disease, gestational age of the baby and other considerations you would discuss with your health care provider.
After delivery
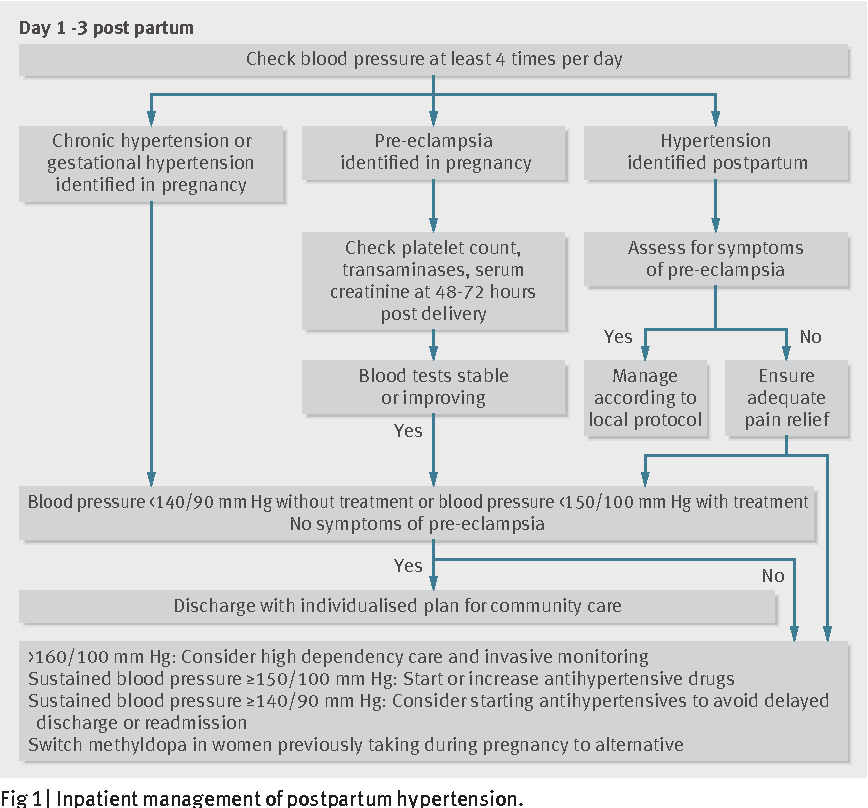
You need to be closely monitored for high blood pressure and other signs of preeclampsia after delivery. Before you go home, you'll be instructed when to seek medical care if you have signs of postpartum preeclampsia, such as severe headaches, vision changes, severe belly pain, nausea and vomiting.
Before you go home, you'll be instructed when to seek medical care if you have signs of postpartum preeclampsia, such as severe headaches, vision changes, severe belly pain, nausea and vomiting.
More Information
- C-section
- Labor induction
Request an appointment
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health. Click here for an email preview.
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices.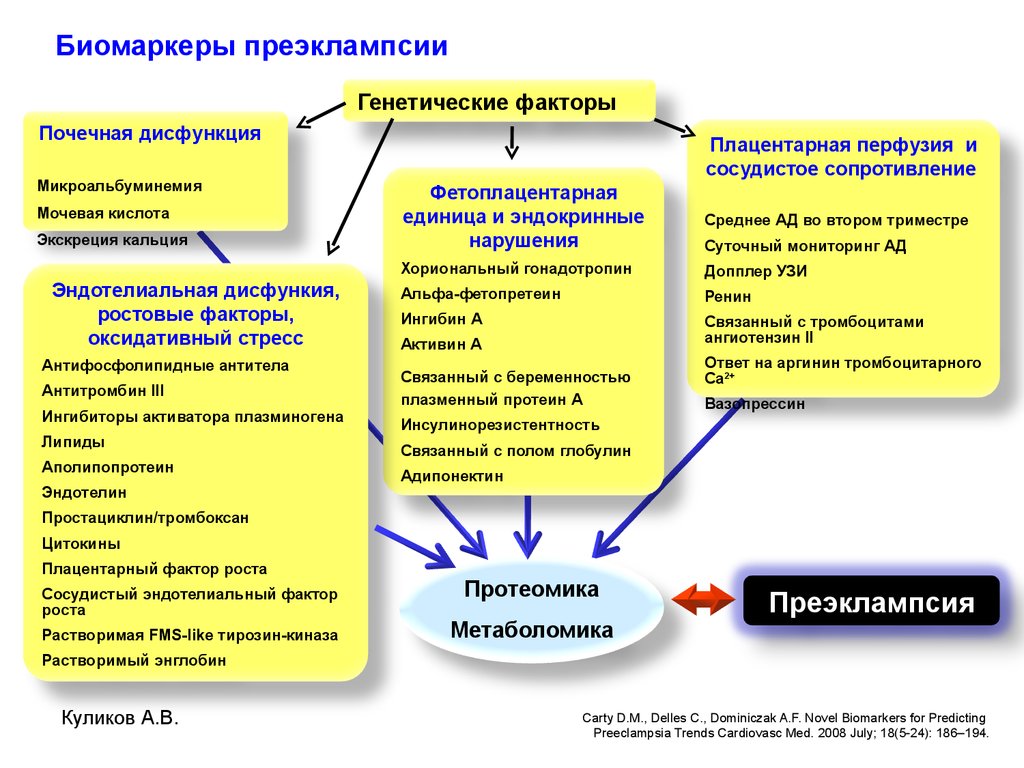 You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Coping and support
Discovering that you have a potentially serious pregnancy complication can be frightening.
If you're diagnosed with preeclampsia late in your pregnancy, you may be surprised to learn that immediate delivery may be recommended. If you're diagnosed earlier in your pregnancy, you may be concerned about monitoring signs and symptoms at home and keeping more frequent appointments with your primary care provider.
It may help to learn more about your condition. In addition to talking to your provider, do some research. Make sure you understand when to call your provider and how to monitor signs and symptoms.
Preparing for your appointment
Preeclampsia is often diagnosed during a regularly scheduled prenatal appointment. If your primary care provider recommends certain tests for a preeclampsia diagnosis, you may also be discussing some of the following questions:
- Did you have preeclampsia or other complications in a previous pregnancy?
- If you're having symptoms of preeclampsia, when did they begin?
- Has anything improved the symptoms or made them worse?
- Have you made any recent changes to your medications, vitamins or dietary supplements?
After a diagnosis of preeclampsia and at follow-up appointments, you might ask the following questions:
- How can I make sure I'm doing blood pressure readings correctly at home?
- How often should I check my blood pressure at home?
- What blood pressure reading should I consider high?
- When should I call the clinic?
- When should I get emergency care?
- How will we monitor my baby's health?
- When should I schedule my next appointment?
- How will we decide on the right time for delivery?
- What are the benefits and risks of delaying delivery?
- What care might my baby need after a preterm delivery?
By Mayo Clinic Staff
Related
Associated Procedures
News from Mayo Clinic
Products & Services
Diagnosis and Management of Preeclampsia
LANA K.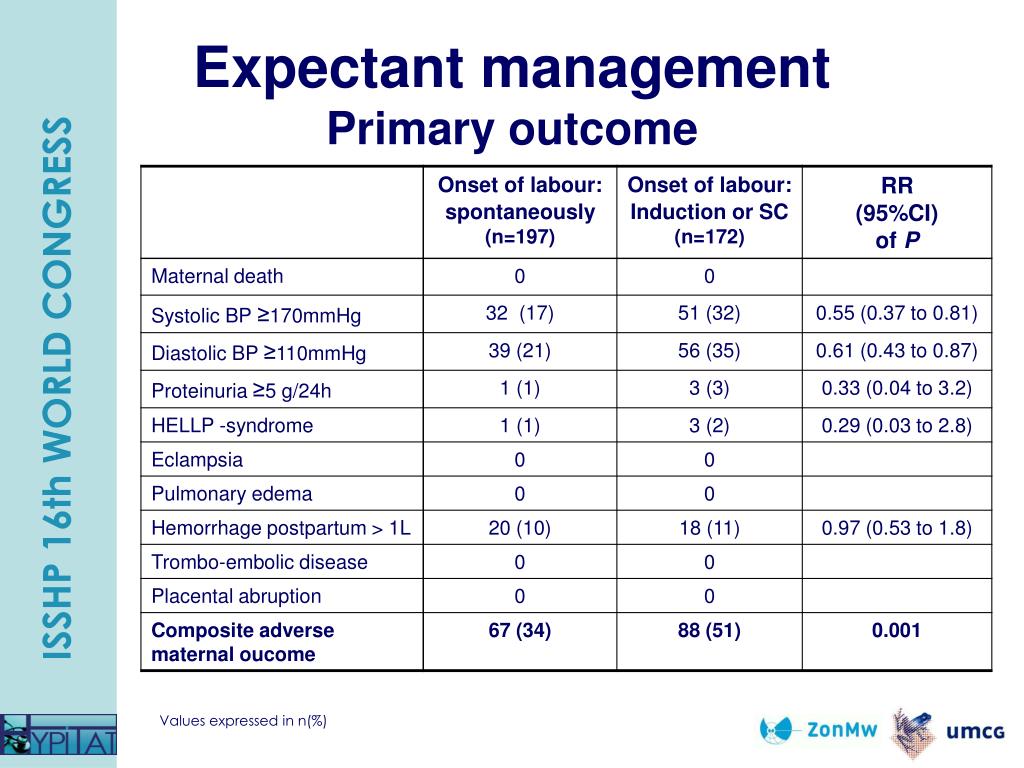 WAGNER, M.D.
WAGNER, M.D.
Am Fam Physician. 2004;70(12):2317-2324
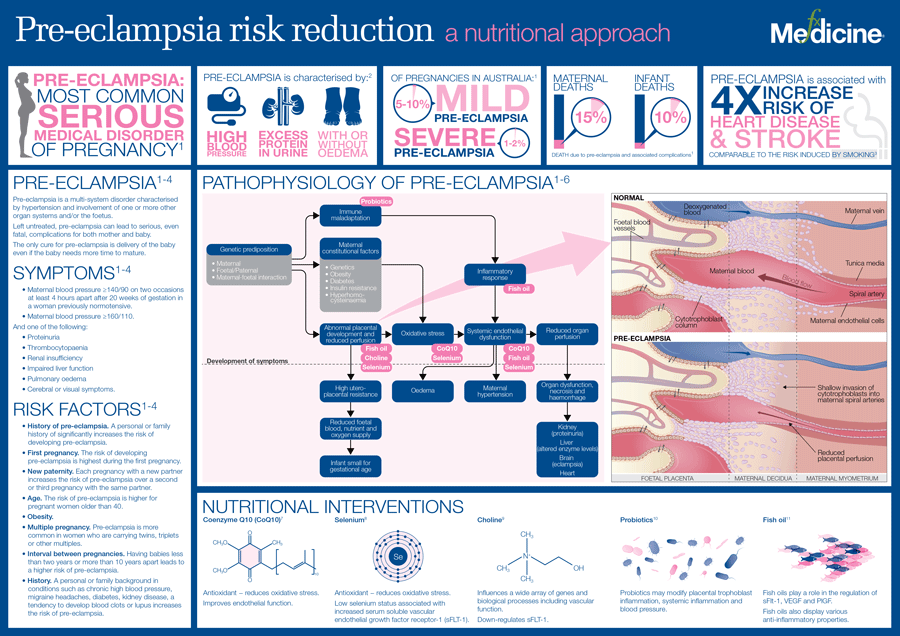
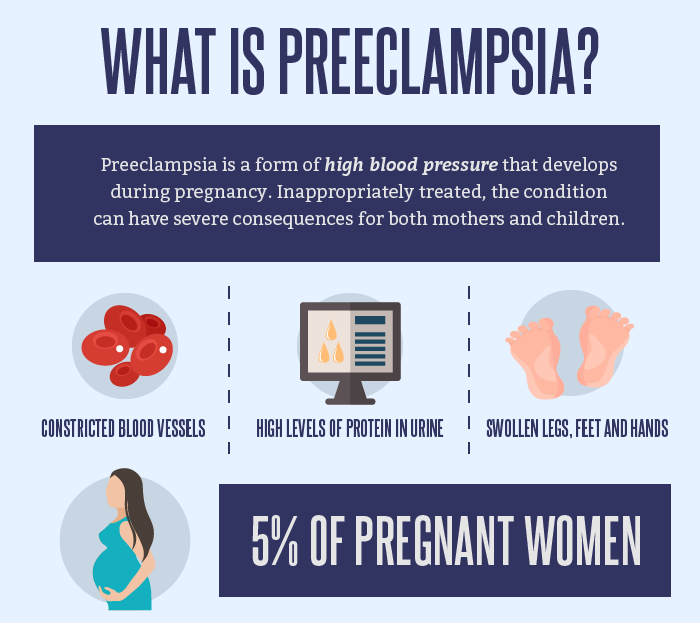
Preeclampsia is a pregnancy-specific multisystem disorder of unknown etiology. The disorder affects approximately 5 to 7 percent of pregnancies and is a significant cause of maternal and fetal morbidity and mortality. Preeclampsia is defined by the new onset of elevated blood pressure and proteinuria after 20 weeks of gestation. It is considered severe if blood pressure and proteinuria are increased substantially or symptoms of end-organ damage (including fetal growth restriction) occur. There is no single reliable, cost-effective screening test for preeclampsia, and there are no well-established measures for primary prevention. Management before the onset of labor includes close monitoring of maternal and fetal status. Management during delivery includes seizure prophylaxis with magnesium sulfate and, if necessary, medical management of hypertension. Delivery remains the ultimate treatment. Access to prenatal care, early detection of the disorder, careful monitoring, and appropriate management are crucial elements in the prevention of preeclampsia-related deaths.
Delivery remains the ultimate treatment. Access to prenatal care, early detection of the disorder, careful monitoring, and appropriate management are crucial elements in the prevention of preeclampsia-related deaths.
Preeclampsia is a pregnancy-specific, multisystem disorder that is characterized by the development of hypertension and proteinuria after 20 weeks of gestation. The disorder complicates approximately 5 to 7 percent of pregnancies,1 with an incidence of 23.6 cases per 1,000 deliveries in the United States.2
| Key clinical recommendation | Label | References |
|---|---|---|
| All pregnant women should be screened for preeclampsia at the first prenatal visit and periodically throughout the remainder of the pregnancy. | B | 25 |
Pregnant women with diastolic blood pressure of 105 to 110 mm Hg or higher should receive antihypertension medication. | C | 4,5 |
| Women at increased risk for preeclampsia who have low calcium intake should increase their calcium intake. | B | 27 |
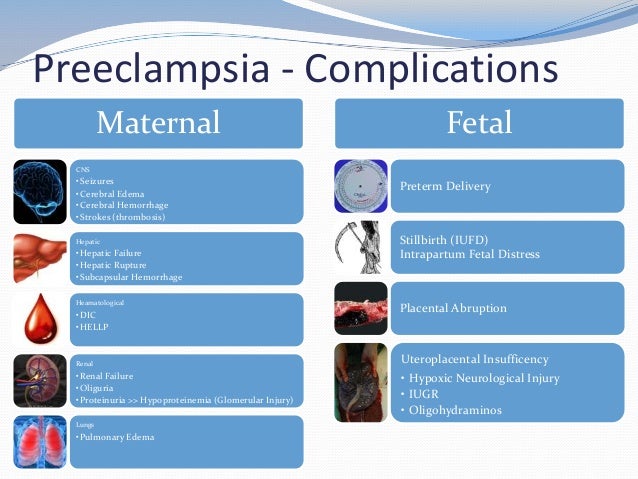
Complications of hypertension are the third leading cause of pregnancy-related deaths, superseded only by hemorrhage and associated with increased risks of placental abruption, acute renal failure, cerebrovascular and cardiovascular complications, disseminated intravascular coagulation, and maternal death.3 Consequently, early diagnosis of preeclampsia and close observation are imperative.
Diagnosis
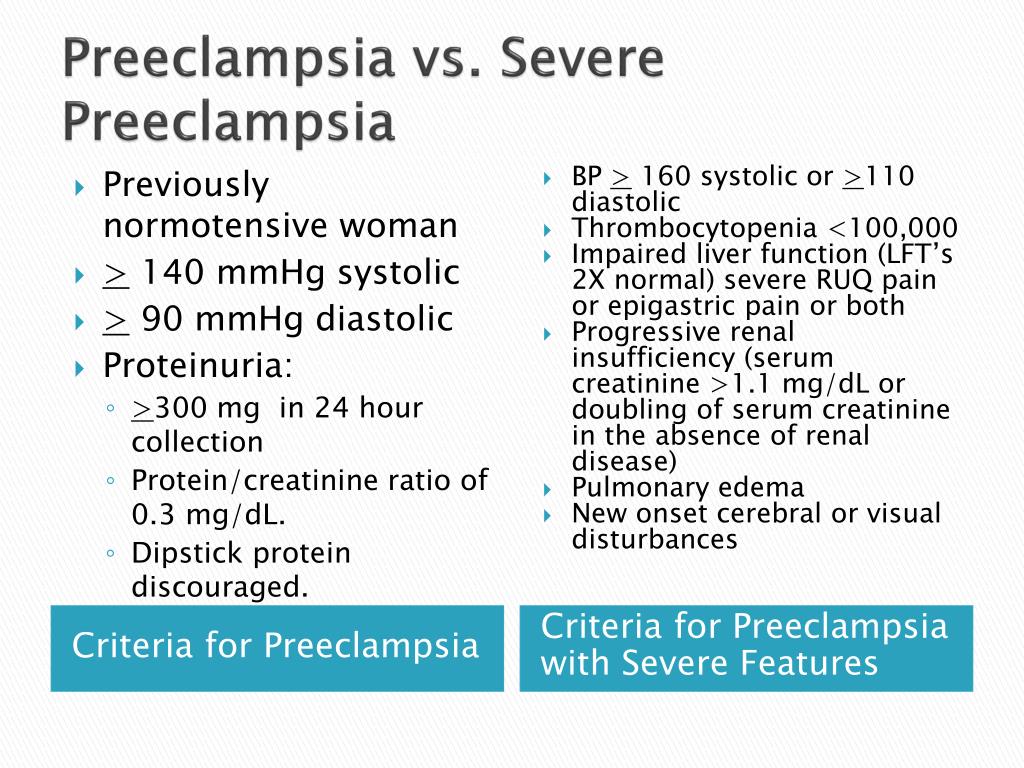
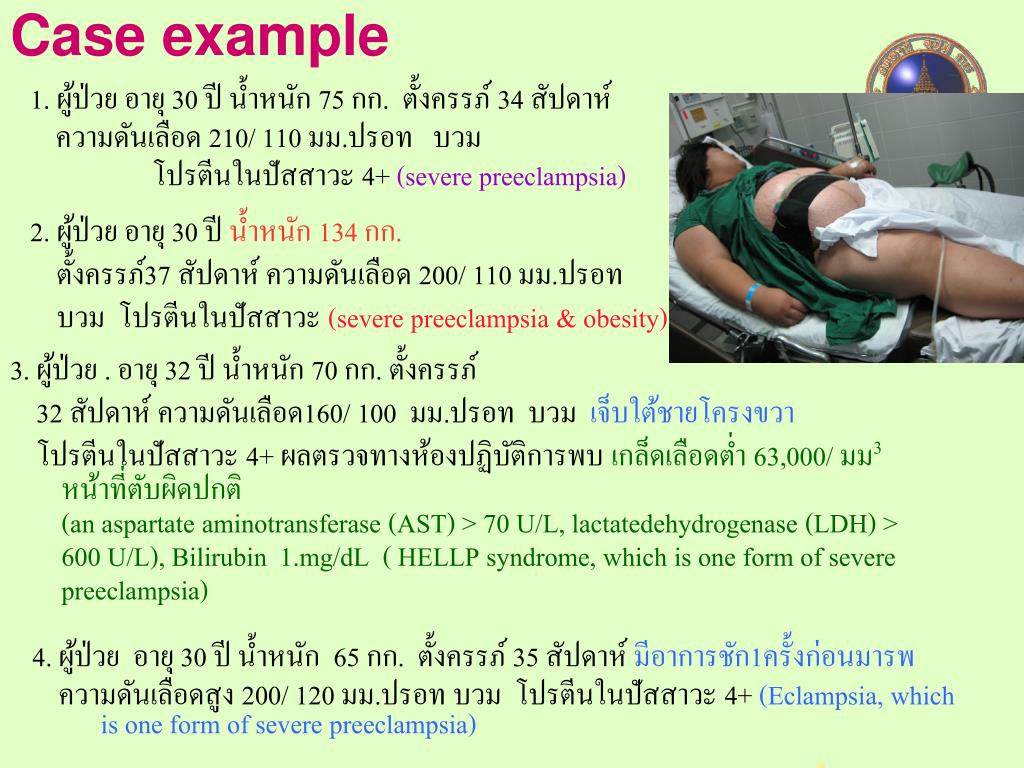
Diagnostic criteria for preeclampsia include new onset of elevated blood pressure and proteinuria after 20 weeks of gestation. Features such as edema and blood pressure elevation above the patient’s baseline no longer are diagnostic criteria.4,5 Severe preeclampsia is indicated by more substantial blood pressure elevations and a greater degree of proteinuria.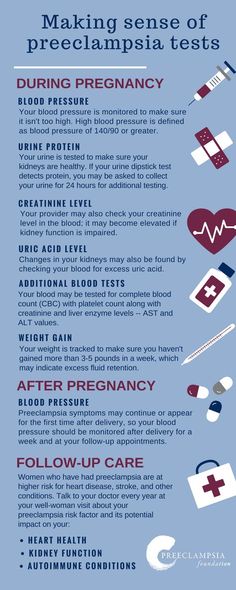 Other features of severe preeclampsia include oliguria, cerebral or visual disturbances, and pulmonary edema or cyanosis (Table 1).4,5
Other features of severe preeclampsia include oliguria, cerebral or visual disturbances, and pulmonary edema or cyanosis (Table 1).4,5
| Preeclampsia |
| Blood pressure: 140 mm Hg or higher systolic or 90 mm Hg or higher diastolic after 20 weeks of gestation in a woman with previously normal blood pressure |
| Proteinuria: 0.3 g or more of protein in a 24-hour urine collection (usually corresponds with 1+ or greater on a urine dipstick test) |
| Severe preeclampsia |
| Blood pressure: 160 mm Hg or higher systolic or 110 mm Hg or higher diastolic on two occasions at least six hours apart in a woman on bed rest |
| Proteinuria: 5 g or more of protein in a 24-hour urine collection or 3+ or greater on urine dipstick testing of two random urine samples collected at least four hours apart |
| Other features: oliguria (less than 500 mL of urine in 24 hours), cerebral or visual disturbances, pulmonary edema or cyanosis, epigastric or right upper quadrant pain, impaired liver function, thrombocytopenia, intrauterine growth restriction |
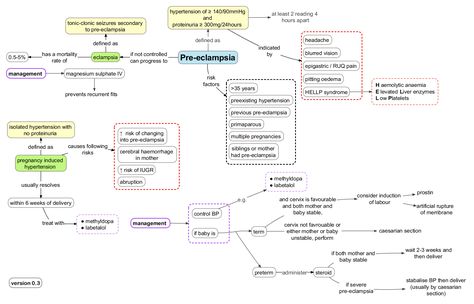
Diagnosis becomes less difficult if physicians understand where preeclampsia “fits” into the hypertensive disorders of pregnancy. These disorders include chronic hypertension, preeclampsia-eclampsia, preeclampsia superimposed on chronic hypertension, and gestational hypertension (Figure 1).5
These disorders include chronic hypertension, preeclampsia-eclampsia, preeclampsia superimposed on chronic hypertension, and gestational hypertension (Figure 1).5
Chronic hypertension is defined by elevated blood pressure that predates the pregnancy, is documented before 20 weeks of gestation, or is present 12 weeks after delivery.5 In contrast, preeclampsia-eclampsia is defined by elevated blood pressure and proteinuria that occur after 20 weeks of gestation. Eclampsia, a severe complication of preeclampsia, is the new onset of seizures in a woman with preeclampsia. Eclamptic seizures are relatively rare and occur in less than 1 percent of women with preeclampsia.1
Preeclampsia superimposed on chronic hypertension is characterized by new-onset proteinuria (or by a sudden increase in the protein level if proteinuria already is present), an acute increase in the level of hypertension (assuming proteinuria already exists), or development of the HELLP (hemolysis, elevated liver enzymes, low platelet count) syndrome.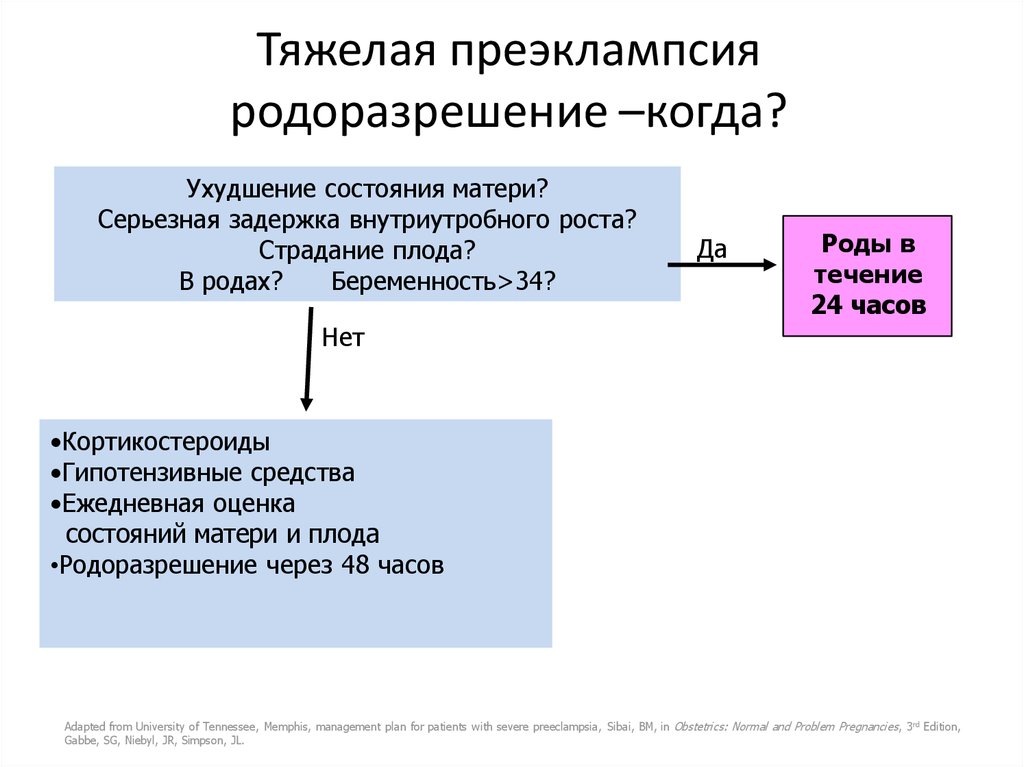 4
4
Gestational hypertension is diagnosed when elevated blood pressure without proteinuria develops after 20 weeks of gestation and blood pressure returns to normal within 12 weeks after delivery.4 One fourth of women with gestational hypertension develop proteinuria and thus progress to preeclampsia.6,7
Risk Factors
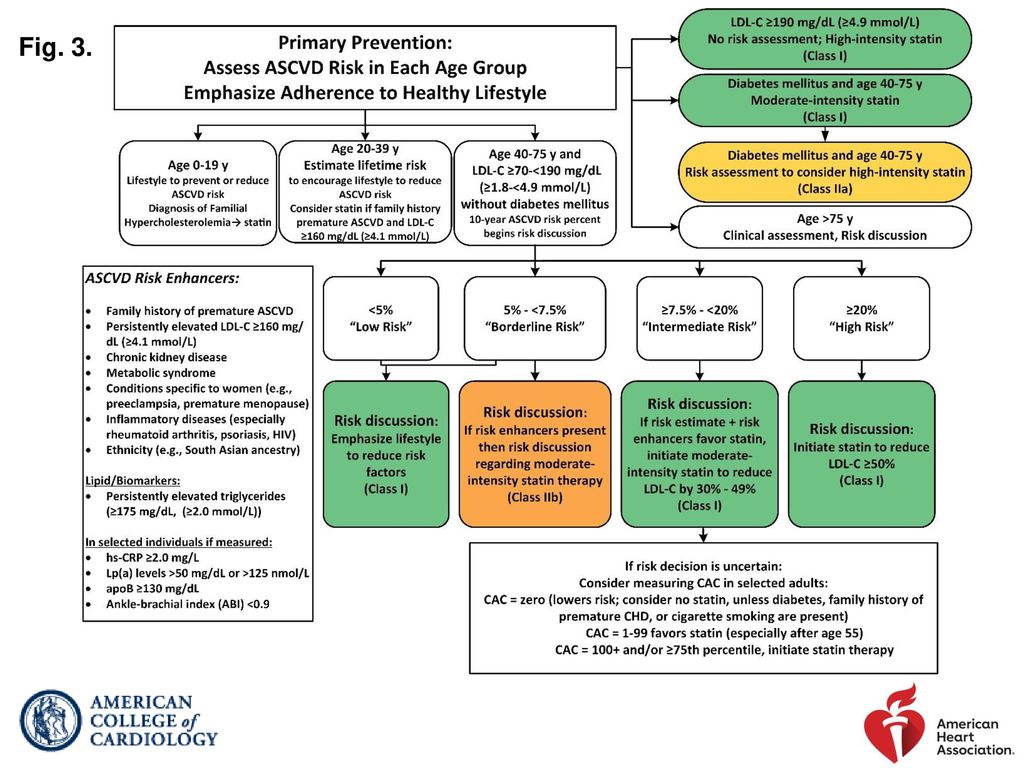
Risk factors for preeclampsia include medical conditions with the potential to cause microvascular disease (e.g., diabetes mellitus, chronic hypertension, vascular and connective tissue disorders), antiphospholipid antibody syndrome, and nephropathy.4,8 Other risk factors are associated with pregnancy itself or may be specific to the mother or father of the fetus (Table 2).4,8
| Pregnancy-associated factors |
| Chromosomal abnormalities |
| Hydatidiform mole |
| Hydrops fetalis |
| Multifetal pregnancy |
| Oocyte donation or donor insemination |
| Structural congenital anomalies |
| Urinary tract infection |
| Maternal-specific factors |
| Age greater than 35 years |
| Age less than 20 years |
| Black race |
| Family history of preeclampsia |
| Nulliparity |
| Preeclampsia in a previous pregnancy |
| Specific medical conditions: gestational diabetes, type I diabetes, obesity, chronic hypertension, renal disease, thrombophilias |
| Stress |
| Paternal-specific factors |
| First-time father |
| Previously fathered a preeclamptic pregnancy in another woman |
Pathophysiology
Although the exact cause of preeclampsia remains unclear,4,5 many theories center on problems of placental implantation and the level of trophoblastic invasion.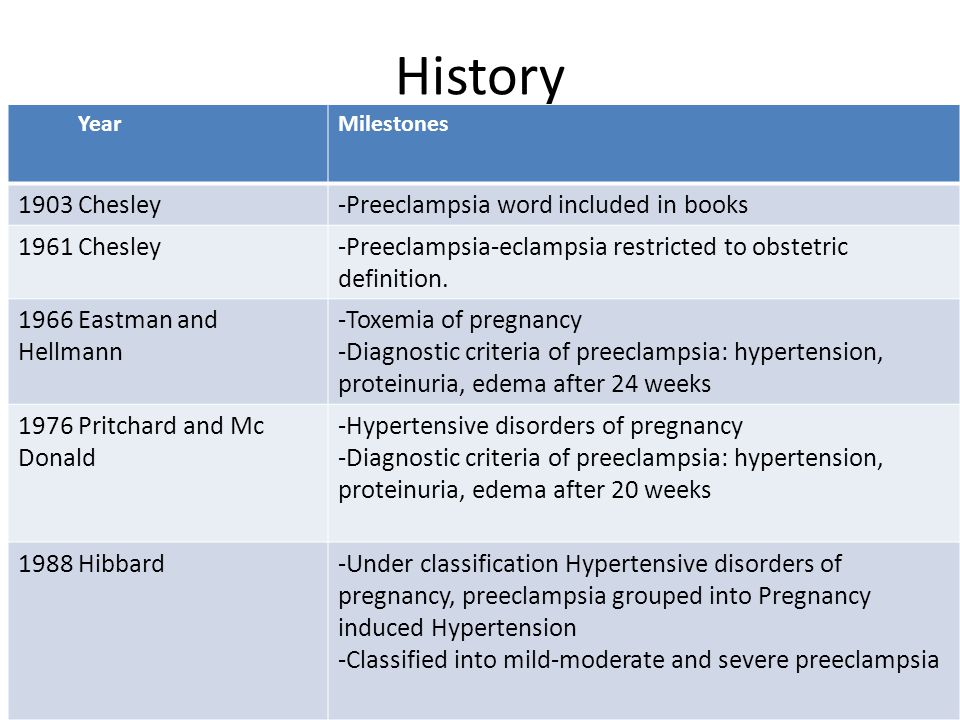 9,10 It is important to remember that although hypertension and proteinuria are the diagnostic criteria for preeclampsia, they are only symptoms of the pathophysiologic changes that occur in the disorder. One of the most striking physiologic changes is intense systemic vasospasm, which is responsible for decreased perfusion of virtually all organ systems.11Perfusion also is diminished because of vascular hemoconcentration and third spacing of intravascular fluids. In addition, preeclampsia is accompanied by an exaggerated inflammatory response and inappropriate endothelial activation.10Activation of the coagulation cascade and resultant microthrombi formation further compromise blood flow to organs.11
9,10 It is important to remember that although hypertension and proteinuria are the diagnostic criteria for preeclampsia, they are only symptoms of the pathophysiologic changes that occur in the disorder. One of the most striking physiologic changes is intense systemic vasospasm, which is responsible for decreased perfusion of virtually all organ systems.11Perfusion also is diminished because of vascular hemoconcentration and third spacing of intravascular fluids. In addition, preeclampsia is accompanied by an exaggerated inflammatory response and inappropriate endothelial activation.10Activation of the coagulation cascade and resultant microthrombi formation further compromise blood flow to organs.11
Clinical Presentation
The clinical presentation of preeclampsia may be insidious or fulminant. Some women may be asymptomatic at the time they are found to have hypertension and proteinuria; others may present with symptoms of severe preeclampsia, such as visual disturbances, severe headache, or upper abdominal pain.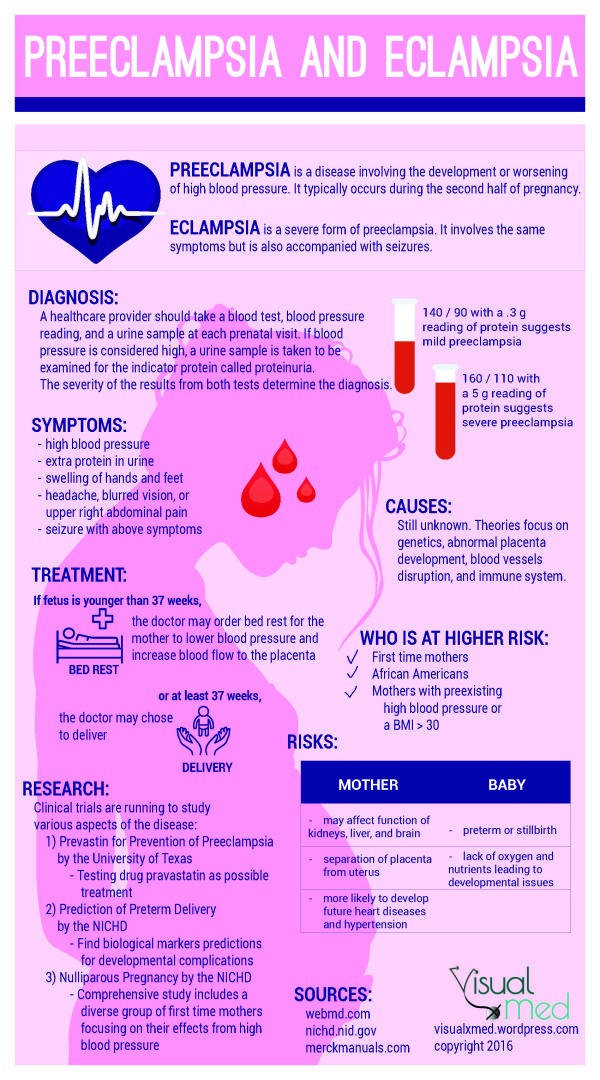 From 4 to 14 percent of women with preeclampsia present with superimposed HELLP syndrome.12 HELLP syndrome may be a variant of preeclampsia or a separate entity, but its development is ominous because mortality or serious morbidity occurs in 25 percent of affected women.13
From 4 to 14 percent of women with preeclampsia present with superimposed HELLP syndrome.12 HELLP syndrome may be a variant of preeclampsia or a separate entity, but its development is ominous because mortality or serious morbidity occurs in 25 percent of affected women.13
Preeclampsia-eclampsia may develop before, during, or after delivery. Up to 40 percent of eclamptic seizures occur before delivery; approximately 16 percent occur more than 48 hours after delivery.1 Death associated with preeclampsia-eclampsia may be due to cerebrovascular events, renal or hepatic failure, HELLP syndrome, or other complications of hypertension.3
Diagnostic Evaluation
HISTORY
As part of the initial prenatal assessment, pregnant women should be questioned about potential risk factors for preeclampsia. They should be asked about their obstetric history, specifically the occurrence of hypertension or preeclampsia during previous pregnancies.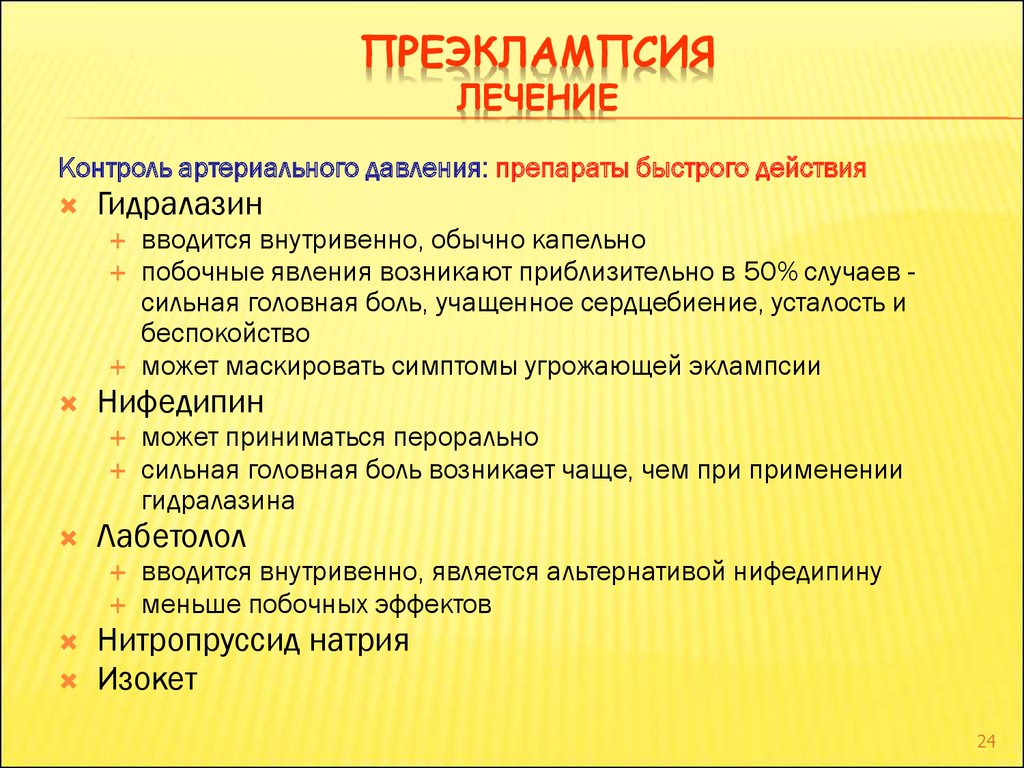 A thorough medical history should be obtained to identify medical conditions that increase the risk for preeclampsia, including diabetes mellitus, hypertension, vascular and connective tissue disease, nephropathy, and antiphospholipid antibody syndrome.
A thorough medical history should be obtained to identify medical conditions that increase the risk for preeclampsia, including diabetes mellitus, hypertension, vascular and connective tissue disease, nephropathy, and antiphospholipid antibody syndrome.
During prenatal visits after 20 weeks of gestation, pregnant women should be asked about specific symptoms, including visual disturbances, persistent headaches, epigastric or right upper quadrant pain, and increased edema. Questions about these symptoms are included in many standardized prenatal documentation forms.
PHYSICAL EXAMINATION
Blood pressure should be measured at each prenatal visit. As mentioned previously, increases above the patient’s baseline (greater than 30 mm Hg systolic or 15 mm Hg diastolic) are no longer considered to be criteria for the diagnosis of preeclampsia. However, such increases warrant close observation.5 To ensure accurate readings, an appropriate-size blood pressure cuff should be used, and blood pressure should be measured after a rest period of 10 minutes or more. During the blood pressure measurement, the patient should be in an upright or left lateral recumbent position with the arm at the level of the heart.4
During the blood pressure measurement, the patient should be in an upright or left lateral recumbent position with the arm at the level of the heart.4
Fundal height should be measured at each prenatal visit because size less than dates may indicate intrauterine growth retardation or oligohydramnios. These conditions may become apparent long before diagnostic criteria for preeclampsia are met. Increasing maternal facial edema and rapid weight gain also should be noted because fluid retention often is associated with preeclampsia. Although these symptoms (e.g., facial edema, rapid weight gain) are not unique to preeclampsia, it is wise to follow affected patients for hypertension and proteinuria.5 Edema involving the lower extremities frequently occurs during normal pregnancy and therefore is of less concern.
LABORATORY EVALUATION
There currently is no single reliable, cost-effective screening test for preeclampsia.4 The serum uric acid level once was used as an indicator of preeclampsia but has been found to lack sensitivity and specificity as a diagnostic tool.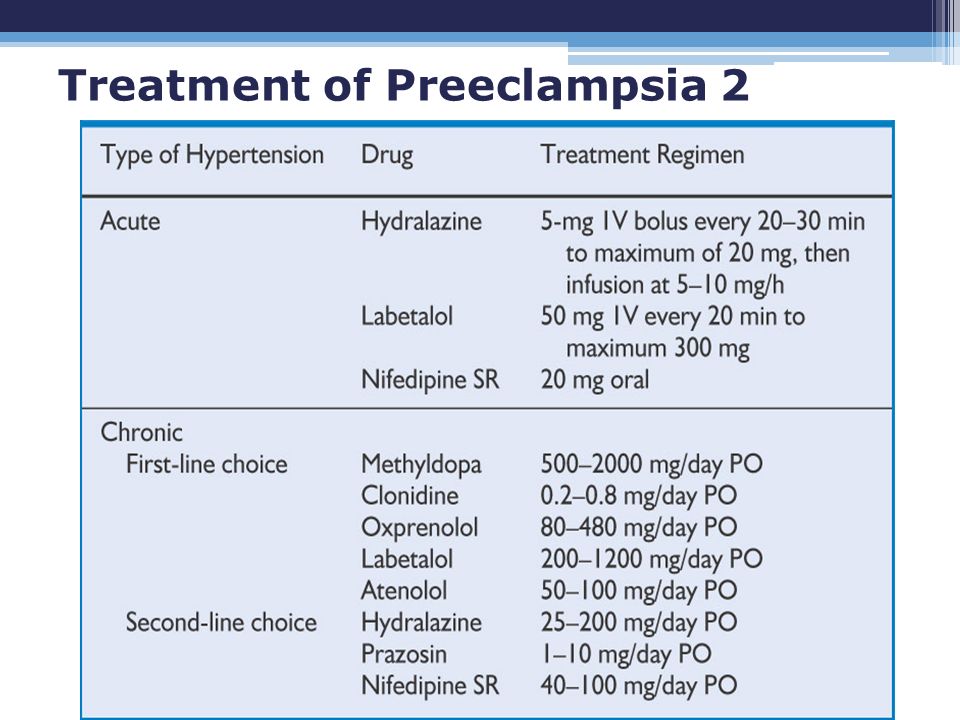 14 However, an elevated serum uric acid level may be of some use in identifying pregnant women with chronic hypertension who have an increased likelihood of having superimposed preeclampsia.14
14 However, an elevated serum uric acid level may be of some use in identifying pregnant women with chronic hypertension who have an increased likelihood of having superimposed preeclampsia.14
A baseline laboratory evaluation should be performed early in pregnancy in women who are at high risk for preeclampsia. Tests should include a hepatic enzyme level, a platelet count, a serum creatinine level, and a 12- to 24-hour urine collection for total protein measurement. Once the diagnosis of preeclampsia has been made, an expanded set of laboratory tests should be performed (Table 3).15 In women who have preeclampsia with no suspected progression, all laboratory tests should be conducted weekly.4,5 If progression of eclampsia is suspected, the tests should be repeated more frequently.
| Women at high risk for eclampsia |
| Hemoglobin level |
| Hematocrit |
| Platelet count |
| Urine protein collection (12 or 24 hour) |
| Serum creatinine level |
| Serum uric acid level |
| Women developing hypertension after 20 weeks of gestation |
| Same tests as in women at high risk |
| Serum transaminase levels |
| Serum albumin level |
| Lactic acid dehydrogenase level |
| Peripheral blood smear |
| Coagulation profile |
Small studies16–18 have shown that random There currently is no single reliable, cost-effective screening test for preeclampsia.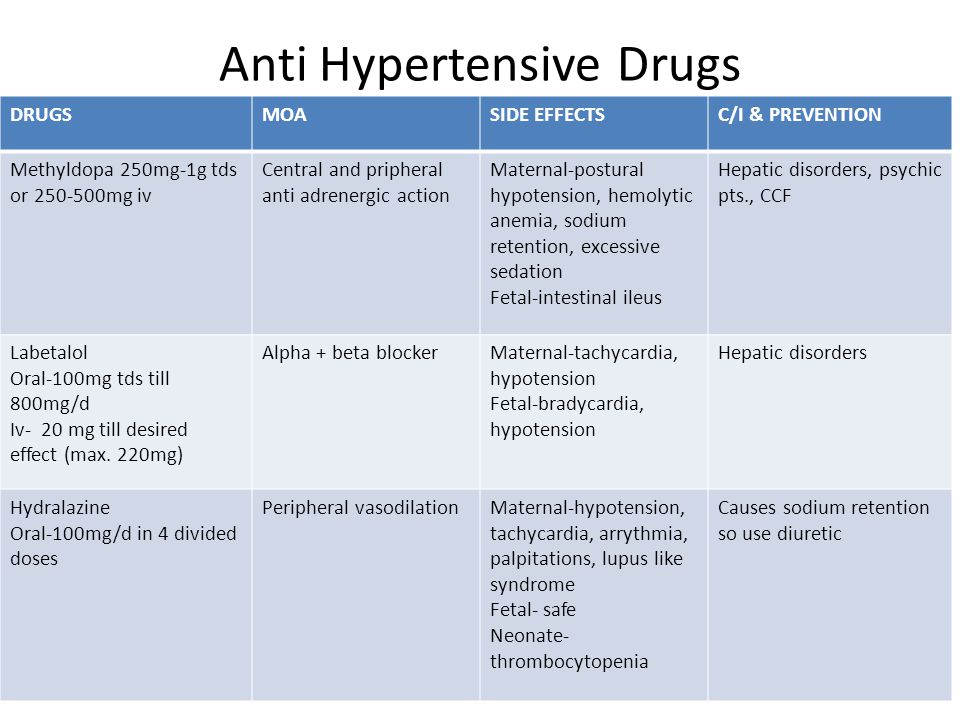 urinary protein-to-creatinine ratios predict the 24-hour urine total protein level and may provide a faster, simplified method of estimating proteinuria, providing that the protein values are less than 1 g in 24 hours.19 The urinary protein-to-creatinine ratio is not sensitive enough to differentiate mild and severe preeclampsia if significant proteinuria exists. However, a ratio of less than 0.2 effectively excludes the presence of significant proteinuria.20 A cutoff ratio of greater than 0.19 is a good predictor of significant proteinuria, with a sensitivity of 90 percent and a specificity of 70 percent. The negative predictive value of the urinary protein-to-creatinine ratio is 87 percent.17
urinary protein-to-creatinine ratios predict the 24-hour urine total protein level and may provide a faster, simplified method of estimating proteinuria, providing that the protein values are less than 1 g in 24 hours.19 The urinary protein-to-creatinine ratio is not sensitive enough to differentiate mild and severe preeclampsia if significant proteinuria exists. However, a ratio of less than 0.2 effectively excludes the presence of significant proteinuria.20 A cutoff ratio of greater than 0.19 is a good predictor of significant proteinuria, with a sensitivity of 90 percent and a specificity of 70 percent. The negative predictive value of the urinary protein-to-creatinine ratio is 87 percent.17
OTHER STUDIES
A baseline sonogram should be considered at 25 to 28 weeks of gestation to evaluate fetal growth in pregnant women at high risk for preeclampsia.5 In women who have already been diagnosed with preeclampsia, antepartum testing with a nonstress test, a biophysical profile, or both should be performed on a weekly basis starting at the time of diagnosis.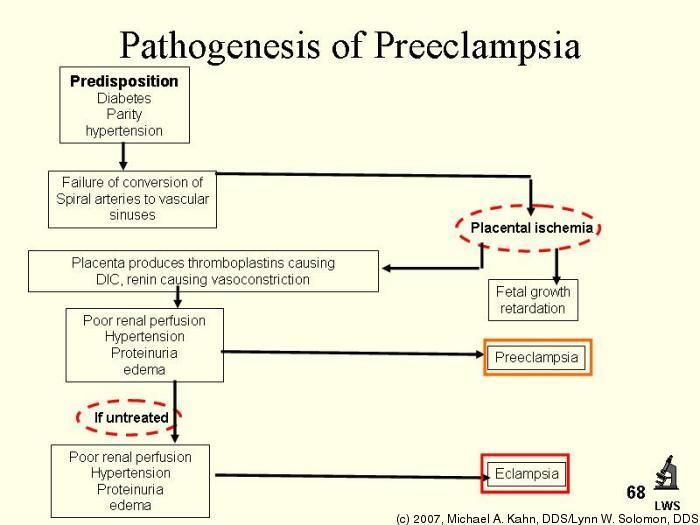 5 If intrauterine growth retardation or oligohydramnios is suspected, the tests should be performed at least twice weekly, and delivery should be contemplated if there are any signs of fetal compromise.4,5 Immediate antepartum testing or delivery is indicated for suspected placental abruption and nonreassuring fetal surveillance.5
5 If intrauterine growth retardation or oligohydramnios is suspected, the tests should be performed at least twice weekly, and delivery should be contemplated if there are any signs of fetal compromise.4,5 Immediate antepartum testing or delivery is indicated for suspected placental abruption and nonreassuring fetal surveillance.5
Treatment
Delivery remains the ultimate treatment for preeclampsia.4,5 Although maternal and fetal risks must be weighed in determining the timing of delivery, clear indications for delivery exist (Table 4).15 When possible, vaginal delivery is preferable to avoid the added physiologic stressors of cesarean delivery.5 If cesarean delivery must be used, regional anesthesia is preferred because it carries less maternal risk.5 In the presence of coagulopathy, use of regional anesthesia generally is contraindicated.5
| Fetal indications |
| Severe intrauterine growth restriction |
| Nonreassuring fetal surveillance |
| Oligohydramnios |
| Maternal indications |
| Gestational age of 38 weeks or greater* |
| Platelet count below 100 × 103 per mm3 (100 × 109 per L) |
| Progressive deterioration of hepatic function |
| Progressive deterioration of renal function |
| Suspected placental abruption |
| Persistent severe headache or visual changes |
| Persistent severe epigastric pain, nausea, or vomiting |
| Eclampsia |
Women with preeclampsia and preterm pregnancy can be observed on an outpatient basis, with frequent assessment of maternal and fetal well-being. Women who are noncompliant, who do not have ready access to medical care, or who have progressive or severe preeclampsia should be hospitalized. Women whose pregnancy is remote from term should be cared for in a tertiary care setting or in consultation with an obstetrician or family physician who is experienced in the management of high-risk pregnancies.4
Women who are noncompliant, who do not have ready access to medical care, or who have progressive or severe preeclampsia should be hospitalized. Women whose pregnancy is remote from term should be cared for in a tertiary care setting or in consultation with an obstetrician or family physician who is experienced in the management of high-risk pregnancies.4
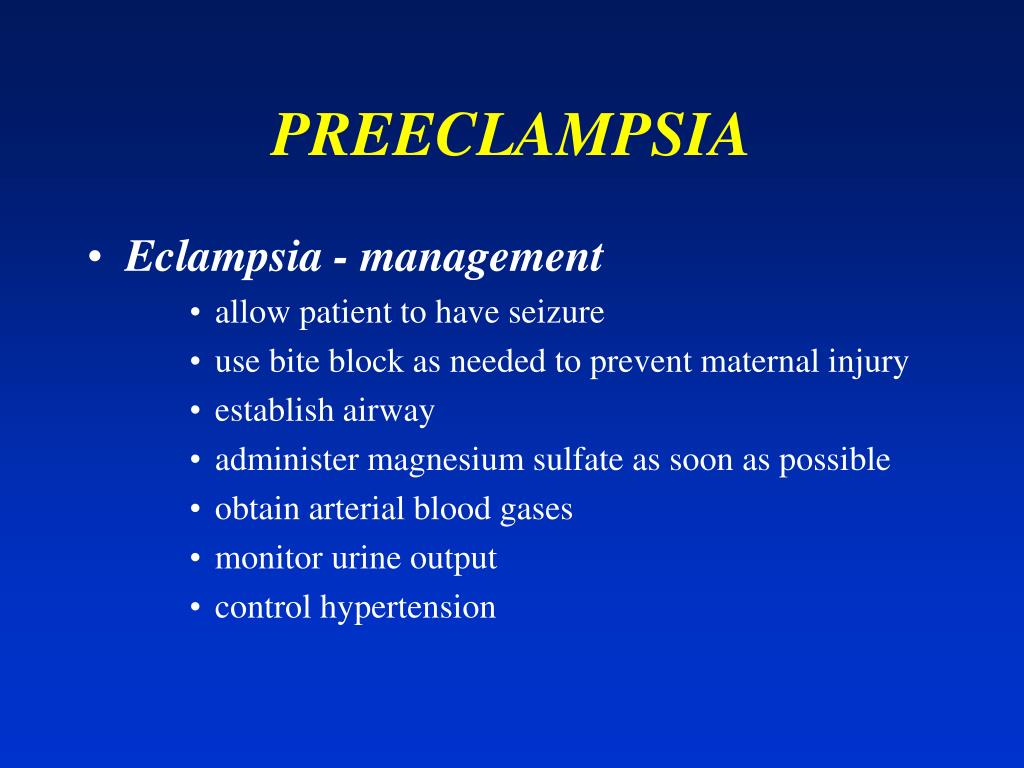
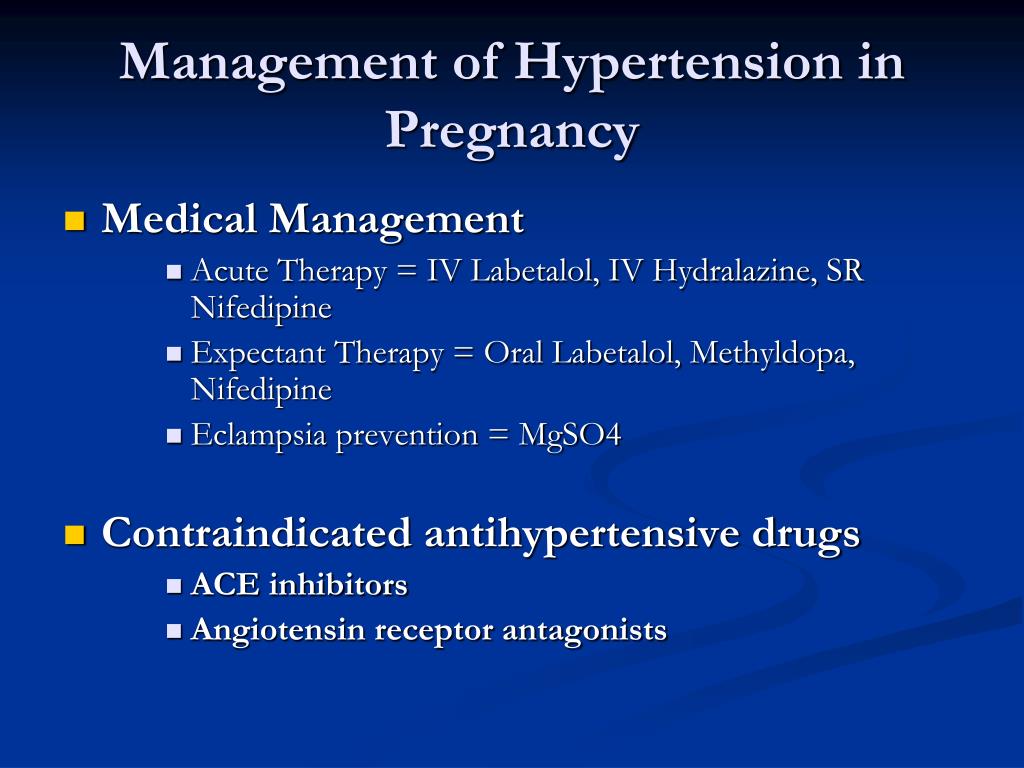
During labor, the management goals are to prevent seizures and control hypertension.4 Magnesium sulfate is the medication of choice for the prevention of eclamptic seizures in women with severe preeclampsia and for the treatment of women with eclamptic seizures.1,21 One commonly used regimen is a 6-g loading dose of magnesium sulfate followed by a continuous infusion at a rate of 2 g per hour.1 Magnesium sulfate has been shown to be superior to phenytoin (Dilantin) and diazepam (Valium) for the treatment of eclamptic seizures.1 Although magnesium sulfate commonly is used in women with preeclampsia, studies to date have been inadequate to show that it prevents progression of the disorder.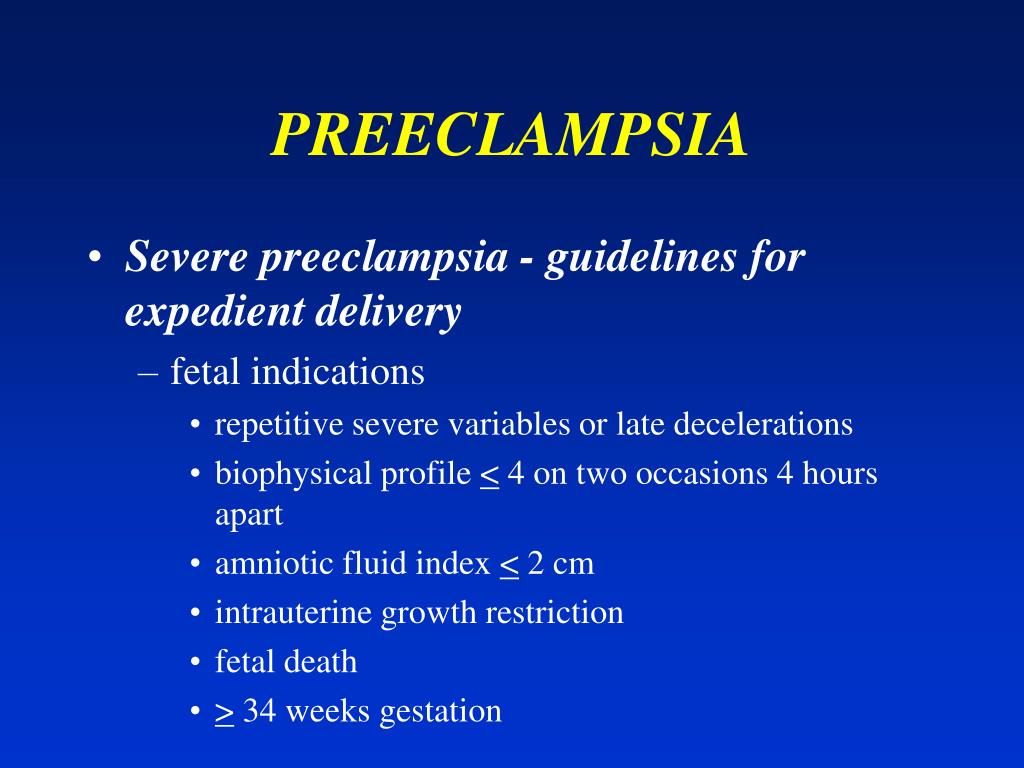 22,23
22,23
Antihypertensive drug therapy is recommended for pregnant women with systolic blood pressures of 160 to 180 mm Hg or higher24 and diastolic blood pressures of 105 to 110 mm Hg or higher4,5,25 The treatment goal is to lower systolic pressure to 140 to 155 mm Hg and diastolic pressure to 90 to 105 mm Hg. To avoid hypotension, blood pressure should be lowered gradually.5
Although evidence about the potential adverse effects of most antihypertensive drugs has been poorly quantified, use of many of these agents is contraindicated during pregnancy.7 Hydralazine (Apresoline) and labetalol (Normodyne, Trandate) are the antihypertensive drugs most commonly used in women with severe preeclampsia (Table 5).15 Nifedipine (Procardia) and sodium nitroprusside (Nitropress) are potential alternatives, but significant risks are associated with their use.5 Note that labetalol therapy should not be used in women with asthma or congestive heart failure.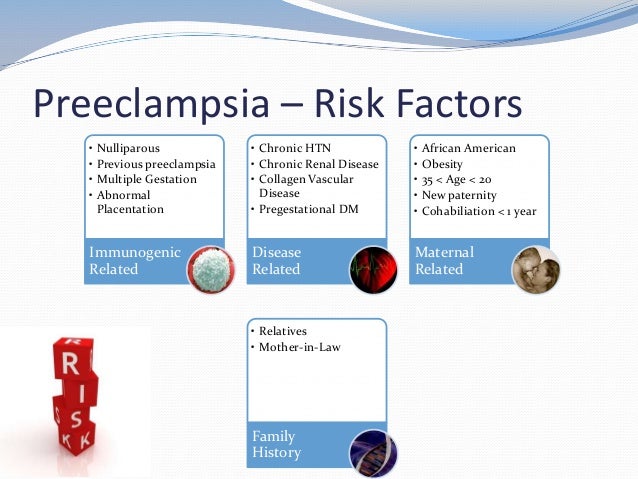 5 Use of angiotensin-converting enzyme inhibitors is contraindicated in pregnant women.
5 Use of angiotensin-converting enzyme inhibitors is contraindicated in pregnant women.
| Hydralazine (Apresoline)* |
| Initial dose: 5 mg IV or 10 mg IM |
| When blood pressure is controlled, repeat initial dose as needed (usually about every 3 hours; maximum, 400 mg per day). |
| If blood pressure is not controlled in 20 minutes, repeat initial dose every 20 minutes until maximum dosage is reached, or go immediately to next step. |
| If blood pressure is not controlled with a total of 20 mg IV or 30 mg IM, consider using a different antihypertensive drug (labetalol,† nifedipine [Procardia], sodium nitroprusside [Nitropress]). |
| Labetalol (Normodyne, Trandate)* |
| Initial dose: 20 mg in IV bolus |
If blood pressure is not controlled, give 40 mg 10 minutes after initial dose and then 80 mg every 10 minutes for two additional doses (maximum: 220 mg). |
| If blood pressure is not controlled, use a different antihypertensive drug (hydralazine, nifedipine, sodium nitroprusside). |
In women with preeclampsia, blood pressure usually normalizes within a few hours after delivery but may remain elevated for two to four weeks.26 As previously noted, a diagnosis of chronic hypertension is made if blood pressure remains elevated at 12 weeks postpartum.5
Women with preeclampsia should be counseled about future pregnancies. In nulliparous women with preeclampsia before 30 weeks of gestation, the recurrence rate for the disorder may be as high as 40 percent in future pregnancies.5 Multiparous women have even higher rates of recurrence.5
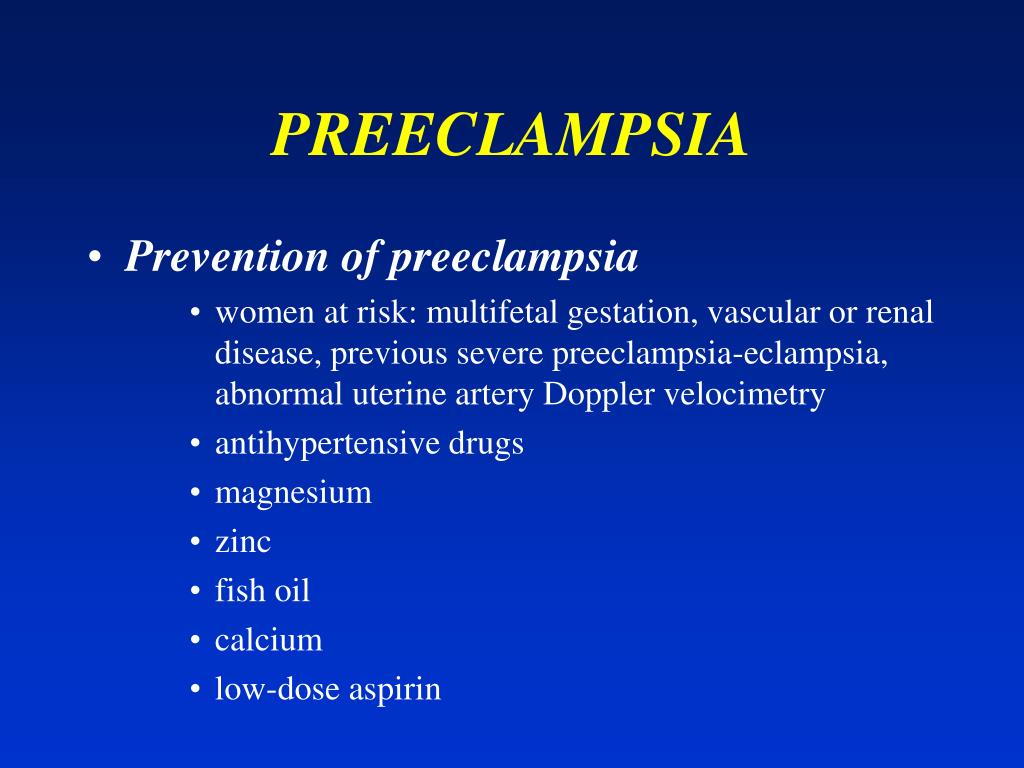
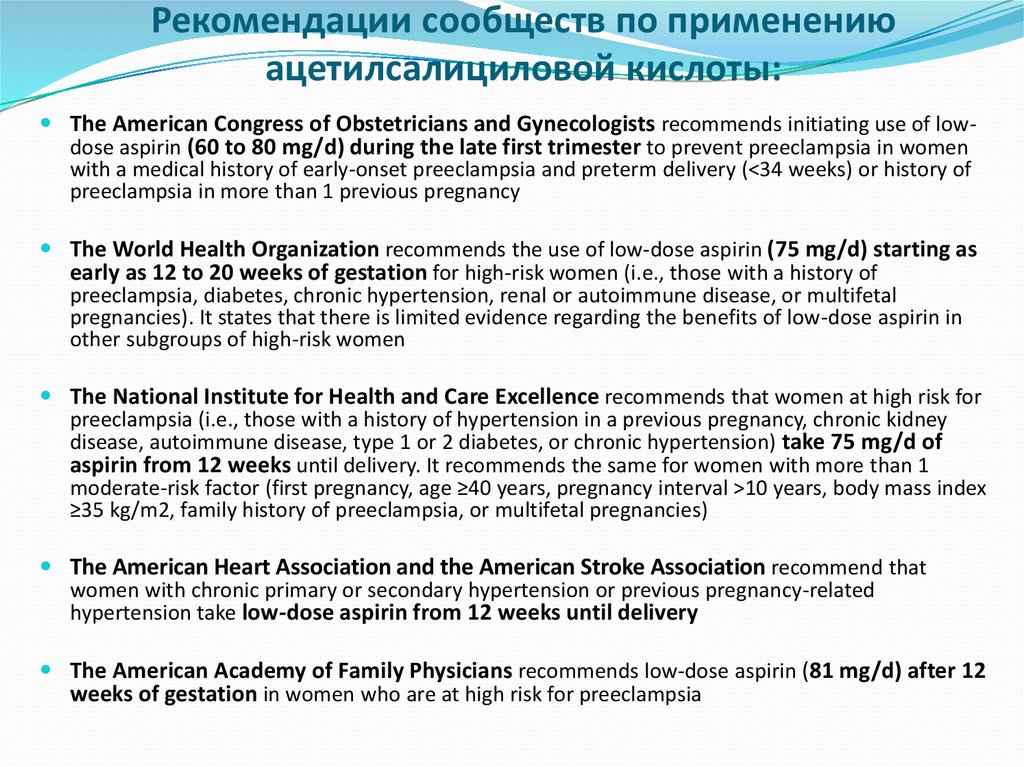
Prevention
There currently are no well-established measures for preventing preeclampsia.4,8 Both low-dose aspirin therapy and daily calcium supplementation have been studied as preventive measures but have not been shown to be beneficial in the general pregnant population and are not recommended for primary prevention of preeclampsia. 4,5 Some evidence does support the use of low-dose aspirin therapy and daily calcium supplementation in certain high-risk women. Calcium supplementation has been shown to produce modest blood pressure reductions in pregnant women who are at above-average risk for hypertensive disorders of pregnancy and in pregnant women with low dietary calcium intake.27 An optimum calcium dosage for these women has not been established.27 Low-dose aspirin therapy (100 mg per day or less) has been shown to reduce the incidence of preeclampsia in women who were found to have an abnormal uterine artery on Doppler ultrasound examination performed in the second trimester.28
4,5 Some evidence does support the use of low-dose aspirin therapy and daily calcium supplementation in certain high-risk women. Calcium supplementation has been shown to produce modest blood pressure reductions in pregnant women who are at above-average risk for hypertensive disorders of pregnancy and in pregnant women with low dietary calcium intake.27 An optimum calcium dosage for these women has not been established.27 Low-dose aspirin therapy (100 mg per day or less) has been shown to reduce the incidence of preeclampsia in women who were found to have an abnormal uterine artery on Doppler ultrasound examination performed in the second trimester.28
Research on the use of antioxidants in the prevention of preeclampsia is promising.29 However, further study is needed, and antioxidant therapy currently is not recommended.4,5,29
Although preeclampsia is not preventable, many deaths from the disorder can be prevented. Women who do not receive prenatal care are seven times more likely to die from complications related to preeclampsia-eclampsia than women who receive some level of prenatal care.3 Some studies indicate that preeclampsia-related fatalities occur three times more often in black women than in white women.3 Although the precise reasons for the racial differences remain elusive, the differences may be indicative of disparities in health status, as well as access to, and quality of, prenatal care.3 To decrease preeclampsia-related mortality, appropriate prenatal care must be available to all women. Early detection, careful monitoring, and treatment of preeclampsia are crucial in preventing mortality related to this disorder.3,8
Women who do not receive prenatal care are seven times more likely to die from complications related to preeclampsia-eclampsia than women who receive some level of prenatal care.3 Some studies indicate that preeclampsia-related fatalities occur three times more often in black women than in white women.3 Although the precise reasons for the racial differences remain elusive, the differences may be indicative of disparities in health status, as well as access to, and quality of, prenatal care.3 To decrease preeclampsia-related mortality, appropriate prenatal care must be available to all women. Early detection, careful monitoring, and treatment of preeclampsia are crucial in preventing mortality related to this disorder.3,8
Preeclampsia - treatment, symptoms, causes of the disease, first signs
Preeclampsia - treatment, symptoms, causes of the disease, first signsHome
Disease Guide
Preeclampsia
Description
- Description
- Symptoms
- Treatment
- Medications
-
Updated: December 24, 2020Time to read: 9 minutes women, developing in the second half of pregnancy (after 20 weeks) and characterized by arterial hypertension, an increase in the amount of protein in the urine, edema, multiple organ failure.

The global prevalence of preeclampsia is 0.9-3% on average. In Russia, this figure is higher and ranges from 12-17% of the total number of pregnancies.
The main factor determining the presence of the disease is the immunological conflict of the mother with the fetus and the fetal part of the placenta. In the first trimester of pregnancy, the trophoblast (the prototype of the placenta) does not fully grow into the uterine tissue. In the future, this entails underdevelopment of the placenta, as a result, the amount of uteroplacental blood flow decreases. As a result, by the 20th week of pregnancy, oxidative stress of the placenta is established. This condition is characterized by an increase in the amount of oxidants due to prolonged hypoxia (mainly oxygen superoxide) and a relative or absolute decrease in the amount of antioxidants.
The imbalance of oxidants and antioxidants is followed by the oxidation of proteins, lipids and the release of oxidation products into the mother's bloodstream.
 These products affect the function of the endothelium, which covers the vessels from the inside. As a result, platelets and leukocytes “stick” to the endothelium. This condition leads to dysfunction of the vessels, their narrowing, a decrease in circulating blood, an increased risk of developing disseminated intravascular coagulation syndrome.
These products affect the function of the endothelium, which covers the vessels from the inside. As a result, platelets and leukocytes “stick” to the endothelium. This condition leads to dysfunction of the vessels, their narrowing, a decrease in circulating blood, an increased risk of developing disseminated intravascular coagulation syndrome. Symptoms
Photo: rebenok.by
Classification of preeclampsia is determined by the severity of the disease. Distinguish between mild, severe preeclampsia and eclampsia:
- Mild preeclampsia includes:
- Arterial hypertension.
- Proteinuria.
- The diagnosis of "severe preeclampsia" is made by the presence of several criteria that complement the clinic for mild preeclampsia:
- High blood pressure (must be above 160/110 mmHg when measured on both arms).
- The content of proteins in the daily portion of urine is more than 5 grams.
- The amount of urine produced may be less than 400 ml.
- Accompanying neurological or visual disorders. These include impaired consciousness, blurred vision, severe headaches.
- Pulmonary edema. It develops due to an overload of the systemic circulation. This entails an increase in the load in the pulmonary circulation. This causes difficulty in breathing in patients with preeclampsia.
- Pain in the epigastric region in the right hypochondrium. This symptom may precede a dangerous complication: HELLP syndrome and liver rupture.
- Increased liver enzymes in the blood.
- Decreased platelet count in peripheral blood.
- Eclampsia. It is characterized by the addition of convulsive syndrome to preeclampsia.
There are atypical forms of preeclampsia. These include HELLP syndrome, acute fatty liver of pregnancy, cholestatic hepatosis of pregnant women.
HELLP-syndrome includes :
- H (hemolysis) - hemolysis, death and decay of red blood cells.
- EL (elevated liver enzymes) - an increase in the amount of liver enzymes in the blood.
- LP (low platelets) - low level of platelets in the blood.
The main life-threatening complications of HELLP syndrome are disseminated intravascular coagulation and liver rupture. When the liver capsule ruptures, profuse internal bleeding is formed, which is sometimes impossible to suspect because of its sudden onset and transience.
Acute fatty liver of pregnancy . It begins to appear with loss of appetite, accompanied by vomiting, pain in the epigastric region, anxiety, itching of the skin, weight loss. After about 14 days, jaundice develops (a consequence of severe hepatocellular insufficiency). The liver is reduced in size. Due to the low amount of albumin, edema of the extremities and ascites develop - a consequence of a decrease in liver function. DIC develops and the kidneys are affected.
Cholestatic hepatosis of pregnancy .
 Genetic factors play a major role in the development of this disease. Pregnancy acts only as a provoking factor. It develops in the third trimester of pregnancy. The disease is clinically identical to acute fatty hepatosis of pregnant women.
Genetic factors play a major role in the development of this disease. Pregnancy acts only as a provoking factor. It develops in the third trimester of pregnancy. The disease is clinically identical to acute fatty hepatosis of pregnant women. Diagnosis
Photo: vyborok.com
The main visible symptoms of preeclampsia (development of the disease after the 20th week of pregnancy, arterial hypertension, increased protein content in the urine, edema) are fundamental in the diagnosis. However, laboratory confirmation of the disease in question is needed:
- Complete blood count. During the development of preeclampsia in pregnant women, hemoglobin may be elevated (more than 110 g / l). In the leukocyte formula, an increase in the number of neutrophils is observed (neutrophilic leukocytosis, an increase in neutrophils - more than 68% of the total number of leukocytes). The number of platelets is usually below the norm, which is 100-450 * 10 9 / l.
- Hemostasis system is a complex of factors of blood coagulation and anticoagulation systems. If the balance of these systems is disturbed, the syndrome of disseminated intravascular coagulation (DIC) develops. Important indicators for assessing the state of the hemostasis system are: prothrombin index, APTT, INR. The decrease in these indicators relative to normal values is directly proportional to the severity of the pathology. An increase in hemostasis scores indicates chronic DIC:
- The prothrombin index is the ratio of the prothrombin time (PTT) of a control blood sample to the PTT of the test blood. In turn, PTT is the time of clot formation after the addition of thromboplastin to the test blood sample.
- APTT (activated partial thromboplastin time) - the time during which a blood clot is formed after the addition of a kaolin-kephalin mixture and calcium chloride to the blood plasma. This test shows the efficiency of the intrinsic pathway of blood clotting.
 With an increase in clotting time relative to the norm (more than 36.5 seconds), one can judge a decrease in blood clotting ability.
With an increase in clotting time relative to the norm (more than 36.5 seconds), one can judge a decrease in blood clotting ability. - INR (international normalized ratio) - this indicator is essentially a prothrombin index (PTI). But when using and calculating, ISI (International Sensitivity Index) is used. This index shows the activity of the clotting factor in the manufactured batch relative to the standard sample. The INR was introduced to standardize the results of the prothrombin index.
- Peripheral blood smear. In this study, particles of erythrocytes can be detected. This indicates the presence of hemolysis (breakdown of red blood cells).
- Liver tests include aspartic aminotransferase (AST), alanine aminotransferase (ALAT), lactate dehydrogenase (LDH) enzyme levels. Normal values for AsAT are 20-40 U/l, for ALT 12-32 U/l, for LDH 140-135 U/l. An increase in these enzymes in the blood indicates a severe course of preeclampsia and involvement in the pathological process of the liver.
- Indicators of a biochemical blood test will also indicate abnormal liver function. The production of blood proteins of albumin decreases (below 28 g/l). Elevated serum creatinine may indicate damage to liver cells (hepatocytes). Along with this, bilirubin in the peripheral blood will be increased, but this indicator may also indicate hemolysis of red blood cells.
Treatment
Photo: proaist.ru
The only way to get rid of life-threatening conditions in preeclampsia is delivery. By the 37th week of pregnancy, labor is artificially stimulated, because. further bearing of the fetus is impractical and life-threatening. Only patients with mild preeclampsia can be treated on an outpatient basis. In other cases, when signs of moderate, severe preeclampsia appear, hospitalization is necessary. Inpatient therapy will be broader than outpatient treatment. At home, only arterial hypertension with mild preeclampsia can be corrected.
Beta1-blockers, calcium channel blockers are prescribed on an outpatient basis to reduce pressure.
 Centrally acting antihypertensive drugs are used as "heavy artillery". If symptoms worsen against the background of ongoing therapy, it is necessary to consult a doctor and switch to inpatient treatment.
Centrally acting antihypertensive drugs are used as "heavy artillery". If symptoms worsen against the background of ongoing therapy, it is necessary to consult a doctor and switch to inpatient treatment. Prevention of preeclampsia in pregnant women at risk:
- Expansion of drinking regimen. To prevent preeclampsia, it is worth paying attention to the amount of fluid consumed. Low salt and water intake may contribute to a decrease in circulating blood volume (CBV). Low BCC causes a violation of the blood supply to the placenta, thereby stopping its development in the early stages.
- Replenishment of calcium deficiency during pregnancy. Calcium deficiency occurs when less than 600 mg of the mineral is consumed per day with food. To replenish it, you must additionally take calcium supplements. In this case, the amount of calcium consumed in the form of a drug should be at least 1 gram per day.
- Taking medicines that reduce blood viscosity. This item applies to women at risk of preeclampsia: family history, first pregnancy, pregnancy over age 40, type 1 obesity (body mass index greater than 35), multiple pregnancies, type 1 or type 2 diabetes, chronic hypertension.
Medicines
Photo: d-russia.ru
Calcium channel blockers (mainly mixed action). The drugs of this group inhibit the entry of calcium into cardiomyocytes (muscle cells of the heart) and into smooth muscle cells (SMC, muscles in the vessels). Because of this, the peripheral vessels dilate. This reduces blood pressure, total peripheral vascular resistance, and afterload on the heart. The coronary vessels (supplying blood to the heart) also dilate and bring more oxygen to the cardiomyocytes. The drugs slightly reduce the contractility of the heart, and at the same time, the need for oxygen and afterload decreases.
Contraindications: arterial hypotension, heart failure, collapse, cardiogenic shock, hypersensitivity to the drug (allergy).Beta1 blockers . The action of drugs in this group is to reduce the activity of the sympathetic nervous system and circulating catecholamines on the heart. Due to this, the heart rate decreases, due to a decrease in stroke volume and minute blood flow, blood pressure and total peripheral vascular resistance decrease.
Contraindications: atrioventricular block 2 and 3 degrees, sinoatrial blockade, arterial hypotension, bradycardia, chronic and acute heart failure, cardiogenic shock, hypersensitivity to the drug (allergy).Centrally acting antihypertensives . The effect is achieved by the action of drugs (or their metabolites) on the receptors of the vasomotor center in the medulla oblongata. As a result, sympathetic activity on the vessels decreases. Basically, the hypotensive effect is due to a decrease in the total peripheral vascular resistance. There is a slight decrease in heart rate and cardiac output.
Contraindications: acute and chronic liver disease, kidney disease, pheochromocytoma, depression, taking drugs that depress the activity of the central nervous system, parkinsonism, hypersensitivity to the drug (allergy).Folk remedies
At the first appearance of symptoms (swelling of the legs, increased blood pressure) closer to the 20th week of pregnancy, you should immediately contact a specialist.

For effective treatment and preservation of the fetus, the treatment prescribed by the doctor must be followed. Taking medicinal herbs and traditional medicine for mild preeclampsia is not prohibited, but this can only be done with the permission of the attending physician to correct the selected additional therapy.
Hawthorn fruits, cornflower flowers, motherwort infusion are used as means to normalize blood pressure. With the appearance of edema of the 1st degree (edema of the lower extremities), the use of diuretic herbal medicines is allowed: artichoke, birch leaves, corn stigmas, burdock. As an adjuvant therapy, sedatives are used (mint, valerian, motherwort, lemon balm, fireweed), as well as antigopixant herbs, fruits (dried apricot fruits, plums, birch leaves, lemon balm, linden).
The information is for reference only and is not a guide to action. Do not self-medicate. At the first symptoms of the disease, consult a doctor.
References
- Pristrom, AM Arterial hypertension in pregnancy: diagnosis, classification, clinical forms: textbook / AM Pristrom.
 - Minsk, 2011. - 103 p.
- Minsk, 2011. - 103 p. - Hypertensive disorders during pregnancy, childbirth and the puerperium. Preeclampsia. Eclampsia: federal clinical guidelines / G. T. Sukhikh [et al.]. - Moscow, 2013. - 85 p.
- Prystrom, A.M. Differentiated drug therapy for arterial hypertension in pregnant women / A.M. Pristrom, A.G. Mrochek // Modern aspects of prevention, diagnosis and treatment of arterial hypertension: materials of the IV Intern. scientific-practical. conf. - Vitebsk, 2007. - P. 115-119
- Hypertensive disorders during pregnancy, childbirth and the puerperium. Preeclampsia. Eclampsia: federal clinical guidelines / G. T. Sukhikh [et al.]. - Moscow, 2013. - 85 p.
- Antiperovich, T.G. Acute cerebrovascular pathology during pregnancy and after childbirth: a retrospective analysis of maternal deaths / T.G. Antiperovich, O.A. Peresada, A.V. Astapenko // Med. news. - 2005. - No. 1. - S. 88-91.
Your comments about symptoms and treatment
If you notice a mistake in the text, please highlight it and press Ctrl+Enter
Found error
pre-eclampsia
Every mother-to-be wants her pregnancy to be a time of joyful anticipation.
 But the fear of preeclampsia can darken the joy.
But the fear of preeclampsia can darken the joy. What is preeclampsia?
Pre-eclampsia is a potentially life-threatening disease that occurs during pregnancy and affects several organ systems and is characterized by high maternal blood pressure and protein in the urine, or in the absence of the latter, dysfunction of other organ systems. This can affect both you and your unborn child. If the risk of preeclampsia is known in advance, it can be prevented.
How common is preeclampsia?
Most women have a normal pregnancy. At the same time, pre-eclampsia is a relatively common disease during pregnancy, which occurs in two out of a hundred women in Estonia.
When does preeclampsia occur?
Preeclampsia occurs after the 20th week of pregnancy or up to six weeks after delivery. Most often, preeclampsia occurs between the 32nd and 36th weeks of pregnancy.
 The earlier in pregnancy the disease occurs, the more severe its course, and the more dangerous it is for the mother and child.
The earlier in pregnancy the disease occurs, the more severe its course, and the more dangerous it is for the mother and child. What causes preeclampsia?
The exact causes of preeclampsia are unknown, but it is believed that they lie in the violation of the attachment of the developing placenta to the uterus, as a result of which there is no reliable connection between the circulatory systems of the mother and child. At the same time, a rapidly developing fetus requires oxygen and nutrients from the mother's circulatory system for its growth. If oxygen deficiency occurs in the developing placenta, toxic substances are released into the mother's circulatory system, which damage the lining of the mother's blood vessels. This is how a systemic lesion of the internal organs of the mother is formed. In order to save the lives of mother and child, the child must be born. If this happens at a very early stage of pregnancy, the baby is not yet ready for extrauterine life.
How will this affect me?
Mostly mild form of the disease occurs at the end of pregnancy and the prognosis is good. But sometimes pre-eclampsia can get worse very quickly and begin to threaten the lives of the mother and child. Preeclampsia also has a long-term effect on a woman's health, as it doubles the incidence of cardiovascular disease in the future. Most women with preeclampsia are hospitalized, and often their children have to be born prematurely. If the health of the mother or child is at risk, labor is induced or a caesarean section is performed.
How will this affect my child?
Most children remain healthy even when their mothers have severe preeclampsia. But sometimes preeclampsia can threaten the life and health of both the fetus and the newborn. Maternal preeclampsia doubles the risk of a surviving child suffering from cerebral palsy, that is, brain damage that results in delayed physical and sometimes mental development.
 In addition, surviving children are more likely to develop cardiovascular disease, obesity and diabetes in the future. In preeclampsia, there is not enough oxygen and nutrients for the growth of the fetus, and intrauterine growth retardation occurs. Since the only treatment for preeclampsia is childbirth, sometimes the pregnancy has to be terminated. Until the 34th week of pregnancy, the lungs of the fetus have not yet fully developed, and steroid injections are given to the pregnant woman to stimulate them.
In addition, surviving children are more likely to develop cardiovascular disease, obesity and diabetes in the future. In preeclampsia, there is not enough oxygen and nutrients for the growth of the fetus, and intrauterine growth retardation occurs. Since the only treatment for preeclampsia is childbirth, sometimes the pregnancy has to be terminated. Until the 34th week of pregnancy, the lungs of the fetus have not yet fully developed, and steroid injections are given to the pregnant woman to stimulate them. How to recognize preeclampsia?
Unfortunately, in most women, the symptoms of the disease appear only at an advanced stage.
- Chronic headache not responding to painkillers
- Severe nausea and vomiting
- Visual disturbances, tinnitus
- Pain in the right hypochondrium
- Shortness of breath, shortness of breath
- Infrequent urge to urinate (less than 500 ml per day)
- Edema of hands, face and eyelids
- Rapid weight gain (more than 1 kg per week)
If you experience any of the above symptoms, contact your obstetrician, gynecologist or hospital doctor on call.
Am I at risk?
Although all pregnant women can develop preeclampsia, some women are more at risk than others.
You are at greater risk if
- this is your first pregnancy;
- you had preeclampsia during a previous pregnancy;
- your sister or mother had preeclampsia;
- Your body mass index is 35 kg/m 2 or more;
- You are at least 40 years old;
- the time between births was more than 10 years;
- You are expecting twins;
- You have become pregnant in vitro;
- you have any medical problem, such as hypertension, kidney problems, lupus, diabetes;
- You developed diabetes during this pregnancy.
At what stage of pregnancy is screening performed?
Pre-eclampsia screening can be performed in all three trimesters.
- First trimester, 11–13 weeks +6 (OSCAR test)
- Second trimester, 19-21 weeks +6 weeks (as part of fetal anatomy screening)
- Third trimester, 34-36 weeks (as part of a growth and fetal study)
A three-stage screening test for preeclampsia can prevent it from occurring or move it to a later stage of pregnancy.

How reliable is screening for preeclampsia?
In the first trimester, the OSCAR test can identify women at risk of developing early preeclampsia with 76% accuracy before the 37th week of pregnancy. Among pregnant twins, all women who can develop early preeclampsia can be identified before the 37th week of pregnancy.
In the second trimester, fetal anatomy screening can identify women at risk of developing early preeclampsia with an accuracy of 85% before the 37th week of pregnancy.
In the third trimester, growth and fetal ultrasound can detect with 85% accuracy women at risk for developing late preeclampsia after 37 weeks of pregnancy.
Why should I assess my risk for preeclampsia?
The best way to assess the risk of early preeclampsia is in the first trimester with the OSCAR test, when at-risk women will benefit from the preeclampsia-preventing effect of aspirin.
 Studies have shown that small doses of aspirin before the 16th week of pregnancy in 62% of cases reduce the risk of early preeclampsia, which may require delivery before the 37th week. Therefore, women with an increased risk of preeclampsia are advised to take 150 milligrams of aspirin once a day, in the evenings, until the 36th week of pregnancy. The goal of prophylactic treatment for women at high risk of preeclampsia is either to avoid the development of preeclampsia or to postpone its occurrence until later in pregnancy, when the child is ready for birth.
Studies have shown that small doses of aspirin before the 16th week of pregnancy in 62% of cases reduce the risk of early preeclampsia, which may require delivery before the 37th week. Therefore, women with an increased risk of preeclampsia are advised to take 150 milligrams of aspirin once a day, in the evenings, until the 36th week of pregnancy. The goal of prophylactic treatment for women at high risk of preeclampsia is either to avoid the development of preeclampsia or to postpone its occurrence until later in pregnancy, when the child is ready for birth. In the second trimester, fetal anatomy screening may reassess the risk of preeclampsia obtained from OSCAR or recommend screening for preeclampsia in women who were not assessed for risk by OSCAR.
In the third trimester, ultrasound examination of the growth and condition of the fetus can assess the risk of late preeclampsia. This is very important as 75% of preeclampsia cases develop after the 37th week of pregnancy.
 This makes it possible to more intensively examine women with an increased risk of preeclampsia and to detect the disease in a timely manner, as well as to prepare the baby's lungs for an early birth.
This makes it possible to more intensively examine women with an increased risk of preeclampsia and to detect the disease in a timely manner, as well as to prepare the baby's lungs for an early birth. How is preeclampsia screened?
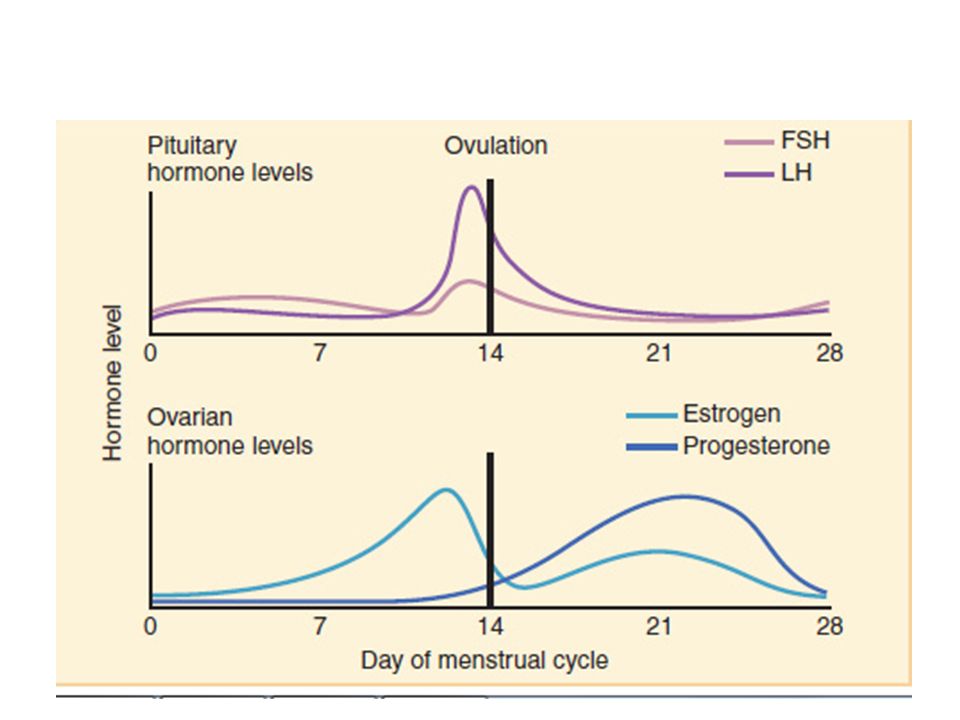
Screening for pre-eclampsia consists of an appointment with a nurse and an ultrasound examination by a gynecologist. The nurse interviews the pregnant woman, measuring her blood pressure, height and weight, and doing a blood test. The gynecologist performs an ultrasound examination and measures the blood flow indices of the uterine arteries feeding the placenta. Based on the blood test values of hormone levels and associated risk factors for preeclampsia, blood pressure parameters, body mass index and uterine arterial blood flow indices, the gynecologist uses a special computer program to assess the individual risk of early or late preeclampsia.
- The risk of preeclampsia can be assessed in one day.