Tetanus shot how often child
Tetanus (for Parents) - Nemours KidsHealth
What Is Tetanus?
Tetanus, also known as lockjaw, is a serious but preventable disease that affects the body's muscles and nerves.
Starting at 2 months of age, all babies in the United States are vaccinated against tetanus. The disease is much more common in developing countries than it is in the United States.
What Causes Tetanus?
Tetanus is caused by a type of
bacteriacalled Clostridium tetani that usually live in soil. The bacteria make a toxin (a chemical or poison that harms the body). This toxin attaches to nerves around a wound area and travels inside the nerves to the brain or spinal cord. There it interferes with the normal activity of nerves, especially the motor nerves that send direct messages to muscles.
In the United States, most cases of tetanus follow a contaminated cut or deep puncture injury, such as a wound caused by stepping on a nail. Sometimes the injury is so small the person never even sees a doctor.
Tetanus is most common in:
- injuries that involve dead skin, such as burns, frostbite, gangrene, or crush injuries
- wounds contaminated with soil, saliva (spit), or feces, especially if not cleaned well
- skin punctures from nonsterile needles, such as with drug use or self-performed tattooing or body piercing
What Is Neonatal Tetanus?
Another form of tetanus, neonatal tetanus, happens in newborns born in unsanitary conditions, especially if the umbilical cord stump becomes contaminated. Routine immunizations and sanitary cord care have made newborn tetanus very rare in developed countries.
Page 1
What Are the Signs & Symptoms of Tetanus?
Tetanus often begins with muscle spasms in the jaw (called trismus). Someone also can have trouble swallowing and stiffness or pain in the muscles of the neck, shoulders, or back.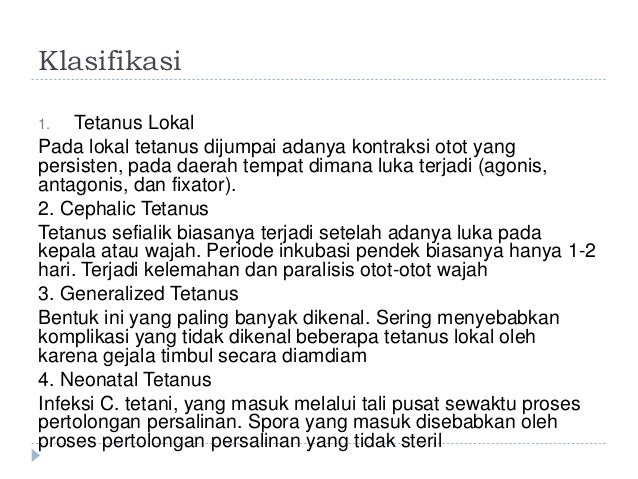 The spasms can spread to the muscles of the belly, upper arms, and thighs. The symptoms can happen days to months after exposure to the bacteria.
The spasms can spread to the muscles of the belly, upper arms, and thighs. The symptoms can happen days to months after exposure to the bacteria.
How Is Tetanus Treated?
Someone who has tetanus will be treated in a hospital, usually in the intensive care unit (ICU). There, they usually get antibiotics to kill bacteria and tetanus immune globulin (TIG) to neutralize the toxin already released. They'll also get medicines to control muscle spasms and may need treatment to support vital body functions.
Can Tetanus Be Prevented?
Yes. The two most important ways to prevent tetanus are:
- getting vaccinated against tetanus
- getting a shot (post-exposure tetanus prophylaxis) after an injury that could cause tetanus
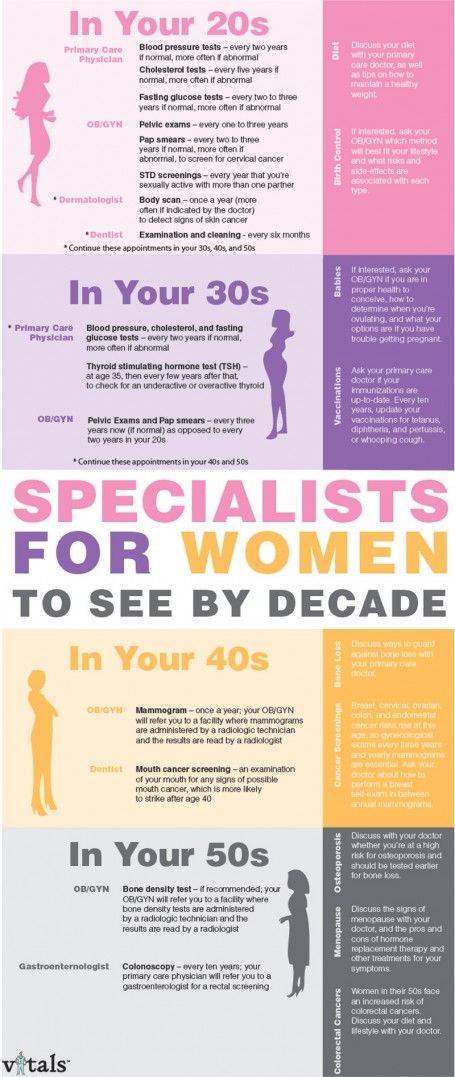
Tetanus immunization is part of the DTaP (diphtheria, tetanus, and acellular pertussis) vaccinations. Kids usually get:
- a series of four doses of DTaP vaccine before 2 years of age
- another dose at 4–6 years of age
- a booster (Tdap) at 11–12 years of age, or later if it was missed
Then, they should get a Tdap or a tetanus and diphtheria (Td) booster every 10 years through adulthood.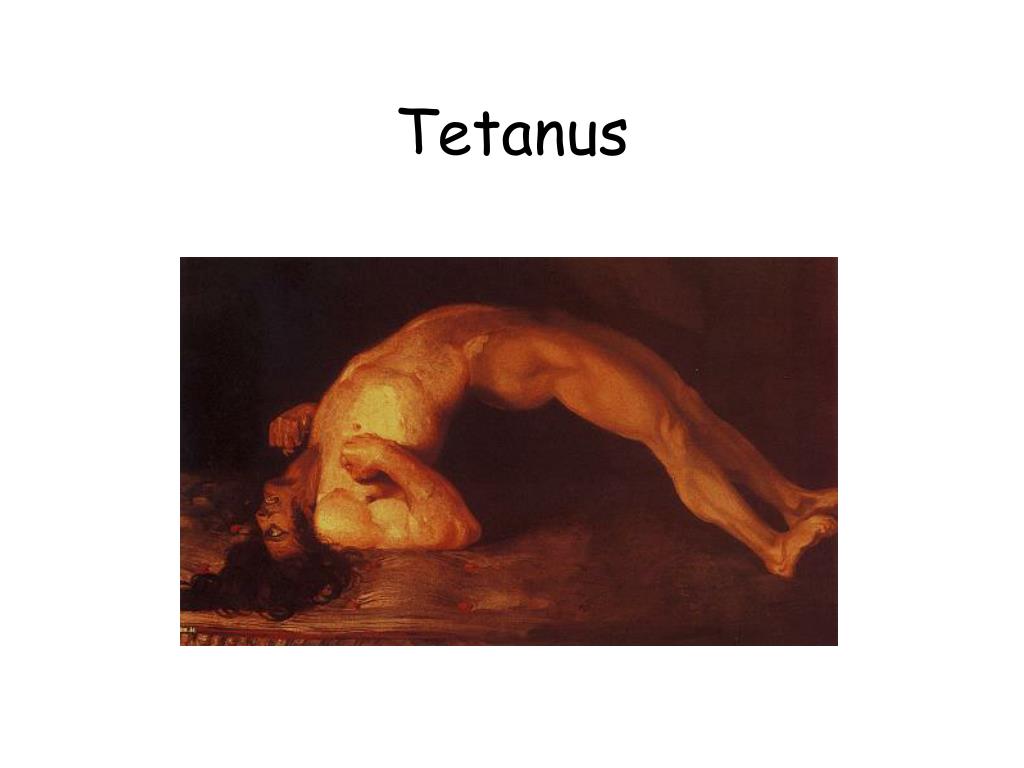
The Tdap vaccine is also recommended for all pregnant women during the second half of each pregnancy, regardless of whether they had the vaccine before, or when it was last given.
Neonatal tetanus can be prevented by making sure that all pregnant women have had their tetanus immunizations, by delivering babies in sanitary conditions, and by proper umbilical cord care.
Post-exposure tetanus prophylaxis involves getting tetanus shots after an injury. Shots given will depend on:
- when the patient last had a booster
- the total number of tetanus vaccinations the patient has had
- the nature of the wound
Any skin wound — especially a deep puncture or a wound that may be contaminated with feces, soil, or saliva — should be cleaned and dressed right away.
When Should I Call the Doctor?
If you're not sure whether your kids have gotten their tetanus vaccinations, or if you know they're not fully immunized, call your doctor. If it's been more than 10 years since someone in your family got a tetanus booster, see your doctor to bring immunizations up to date.
If it's been more than 10 years since someone in your family got a tetanus booster, see your doctor to bring immunizations up to date.
If a puncture or other deep wound happens, clean the wound and call the doctor to ask about post-exposure tetanus prophylaxis. If your child develops lockjaw or muscle spasms — particularly after a wound — get medical care right away.
Reviewed by: Ryan J. Brogan, DO
Date reviewed: April 2022
How Long Does a Tetanus Shot Last? Vaccine Schedule and Purpose
What’s the recommended tetanus vaccination schedule?
When it comes to the tetanus vaccination, it’s not one and done.
You receive the vaccine in a series. It’s sometimes combined with vaccines that protect against other diseases, such as diphtheria. A booster shot is recommended every 10 years.
In children
The DTaP vaccine is one immunization that protects against three diseases: diphtheria, tetanus, and pertussis (whooping cough).
The American Academy of Pediatrics (AAP) recommends children receive the DTaP vaccine at the following intervals:
- 2 months
- 4 months
- 6 months
- 15-18 months
- 4-6 years
The DTaP vaccine isn’t given to children older than age 7.
Children should receive the Tdap booster shot at about age 11 or 12. Tdap is similar to DTaP since it protects against the same three diseases.
Ten years after receiving the Tdap, your child will be an adult and should receive the Td shot. The Td shot provides protection against tetanus and diphtheria.
In adults
Adults who were never vaccinated or who didn’t follow the complete set of vaccinations as a child should receive a Tdap shot followed by the Td booster dose 10 years later, according to the Centers for Disease Control and Prevention (CDC).
The Immunization Action Coalition has different recommendations for those who were never vaccinated. Check with your doctor to see which catch-up schedule is right for you.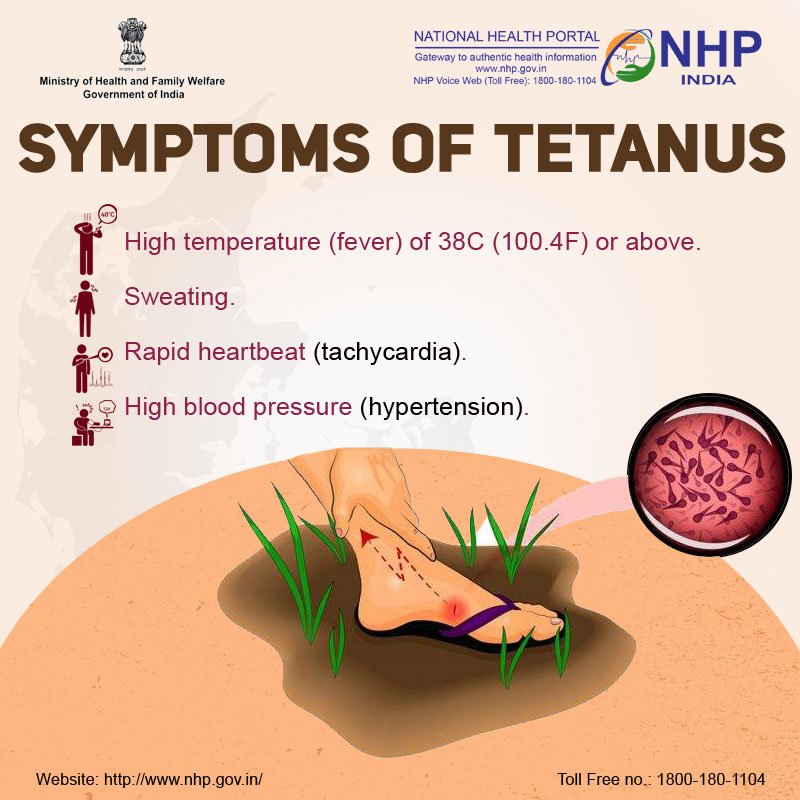
In people who are pregnant
The Tdap vaccination is recommended for anyone who is pregnant. This shot gives your unborn baby a head start on protection against pertussis (whooping cough).
If you didn’t get the Td or Tdap shot in the last 10 years, the shot may provide your unborn baby with protection from tetanus. It also reduces your risk of diphtheria. These conditions can be deadly to newborns.
The Tdap vaccine is safe during pregnancy.
For optimal immunity, the CDC generally recommends receiving the shot between 27 and 36 weeks, but it’s safe to receive at any point in your pregnancy.
If you don’t know if you’ve been vaccinated, you may need a series of shots.
The tetanus vaccine doesn’t provide lifelong immunity. Protection begins to decrease after about 10 years, which is why doctors advise booster shots every decade.
A doctor may recommend children and adults get a booster shot earlier if there’s a suspicion they may have been exposed to tetanus-causing spores.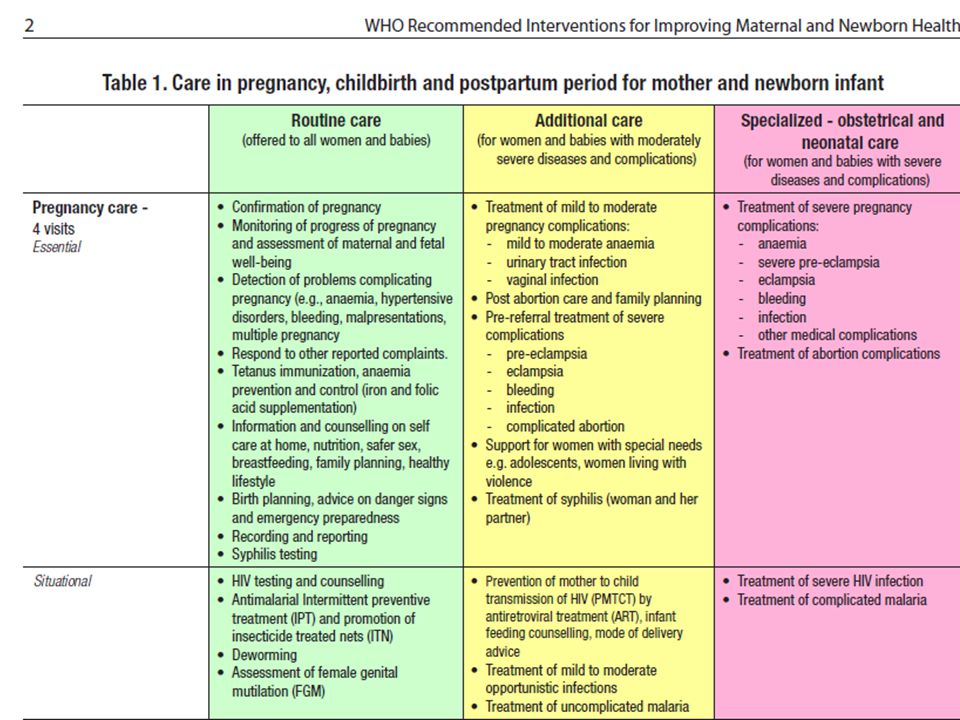
For example, if you step on a rusty nail or have a deep cut that’s been exposed to infected soil, your doctor may recommend a booster.
Tetanus is rare in the United States. An average of only 30 cases are reported each year.
Nearly all cases involve people who have never received a tetanus shot or who don’t stay current with their boosters. Vaccination is essential to prevent tetanus.
Complications from tetanus vaccinations are extremely rare, and the disease itself poses far more risks than the vaccine.
When side effects do occur, they’re generally mild and may include:
- fever
- fussiness in babies
- swelling, pain, and redness at the injection site
- nausea or stomach pain
- tiredness
- headache
- body aches
Serious problems are extremely rare, but can include:
- an allergic reaction
- seizures
If you think you or your child may be having an allergic reaction to the vaccine, seek immediate medical help. Signs of an allergic reaction may include:
Signs of an allergic reaction may include:
- hives
- difficulty breathing
- a fast heartbeat
Some people shouldn’t be vaccinated, including people who:
- had severe reactions to previous doses of the vaccine
- have Guillain-Barré syndrome, a neurological immune disorder
Tetanus is a serious disease caused by bacteria called Clostridium tetani.
The spores of the bacteria live in soil, dust, saliva, and manure. If an open cut or wound is exposed to the spores, they can enter your body.
Once inside the body, the spores produce toxic bacteria that affects muscles and nerves. Tetanus is sometimes called lockjaw because of the stiffness it can cause in the neck and jaw.
The most common scenario for catching tetanus is stepping on a dirty nail or sharp shard of glass or wood that pierces through the skin.
Puncture wounds are most prone to tetanus because they’re narrow and deep. Oxygen can help kill the spores of the bacteria, but unlike gaping cuts, puncture wounds don’t allow oxygen much access.
Other ways you may develop tetanus:
- contaminated needles
- wounds with dead tissue, such as burns or frostbite
- a wound that’s not cleaned thoroughly
You can’t catch tetanus from someone who has it. It’s not spread from person to person.
The time between exposure to tetanus and the appearance of symptoms ranges between a few days to a few months.
Most people with tetanus will experience symptoms within 14 days of exposure.
Symptoms you may experience include:
- headache
- stiffness in your jaw, neck, and shoulders, which can gradually extend to other parts of the body, causing muscle spasms
- trouble swallowing and breathing, which can lead to pneumonia and aspiration
- seizures
Tetanus can be fatal. The Immunization Action Coalition states that about 10 percent of reported cases have led to death.
There’s no cure for tetanus. You can manage symptoms by using sedatives to control muscle spasms.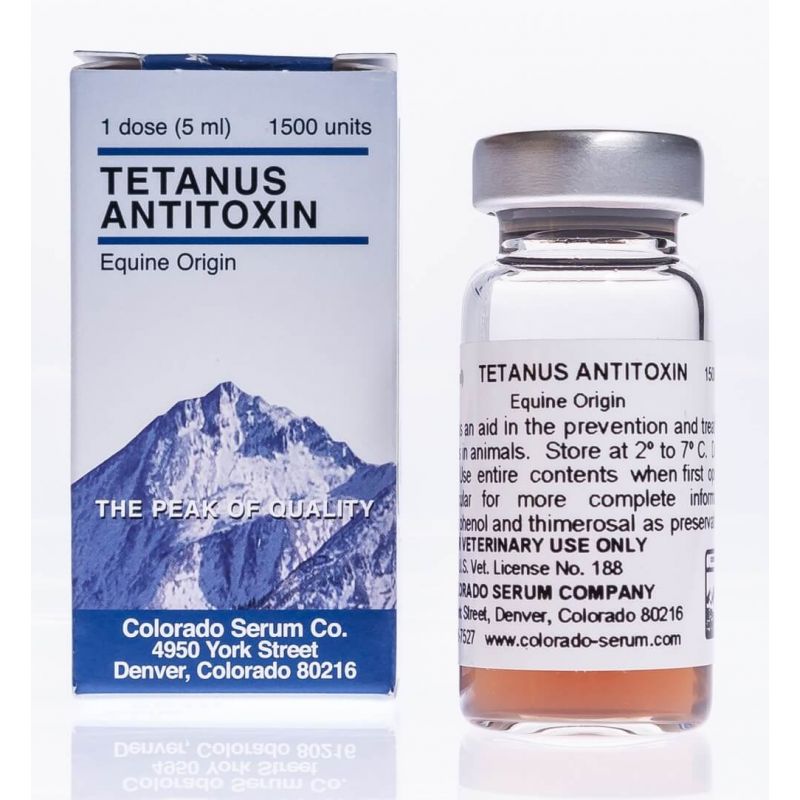
Most treatment consists of trying to reduce exposure to the toxins produced by the bacteria. To do that, your doctor may advise:
- thorough wound cleaning
- a shot of tetanus immune globulin as an antitoxin, although this will only affect toxins that aren’t yet bound to nerve cells
- antibiotics
- the tetanus vaccine
Tetanus is a potentially deadly disease, but it can be prevented by staying up-to-date on your vaccine schedule and getting boosters every 10 years.
If you suspect you may have been exposed to tetanus, see your doctor. In some cases, they may recommend a booster following the injury.
Tetanus: why take risks when you can protect yourself?
October 6, 2016
Tetanus is an acute infectious disease with symptoms of toxicosis and tonic-clonic convulsions resulting from damage to the CNS motor cells by toxin.
Pathogen bacterium Clostridium tetani , rod-shaped, forms a strong exotoxin that acts on the nervous system.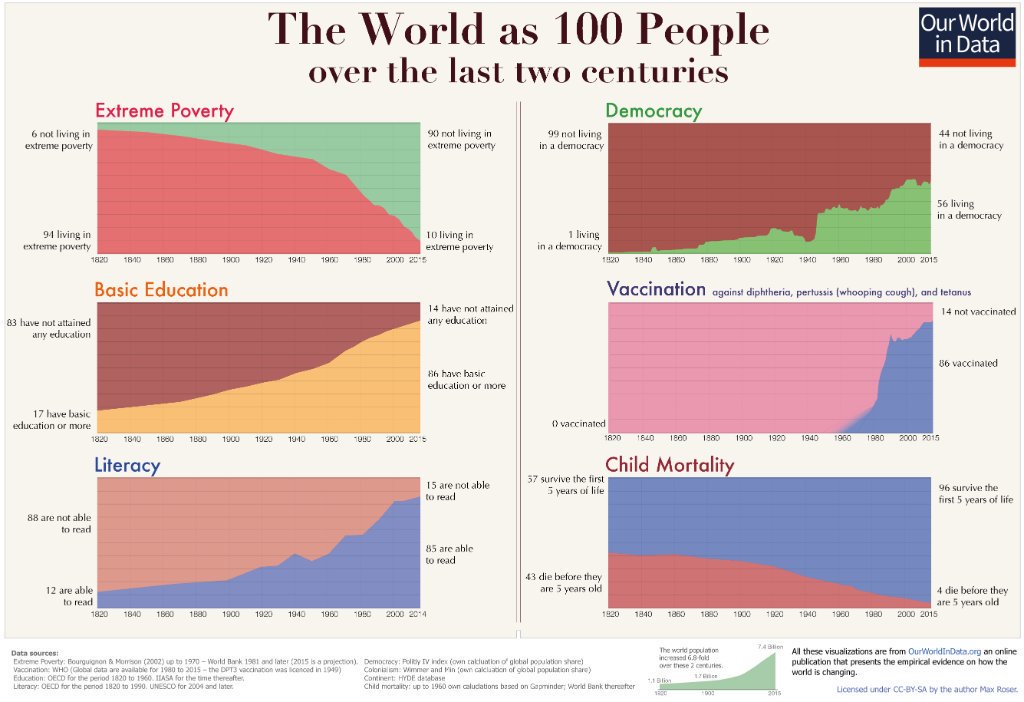
Prevalence . The tetanus bacillus is widely distributed in nature. It is usually found in the soil around settlements, where it enters with the feces of herbivores. It can be found in the intestines of healthy people without causing disease in them.
Infection occurs when the pathogen enters through broken skin or mucous membranes. Contamination of lacerations and stab wounds is especially dangerous, although infection is also possible when microtraumas that have gone unnoticed are infected.
In children, the most common cause of infection is leg injuries - wounds of the feet when walking barefoot, pricks with sharp objects, thorns, etc. In newborns, the umbilical cord residue infected in violation of the rules of asepsis and antisepsis can serve as an entrance gate. Tetanus is more common in children aged 3 to 7 years. At this age, they are especially mobile and more likely to receive various injuries.
There is no natural immunity. Immunity after the disease is short-lived. Susceptibility is very high in people of all age groups.
Susceptibility is very high in people of all age groups.
Clinic . The disease usually begins acutely. There are unpleasant sensations in the wound in the form of burning, tingling, pain with irradiation along the nerve trunks. With an acute onset, trismus (cramps) of the masticatory muscles becomes the first symptom. During trismus, the patient cannot open his mouth, eating is difficult, and speech is impossible. In severe cases, the teeth are compressed, it is not possible to open the mouth even with a spatula. Immediately after trismus, spasms of facial muscles appear. The patient's face takes on a peculiar expression: a smile is combined with crying ("sardonic smile"). The forehead is going into wrinkles, the mouth is stretched in width, its corners are lowered. After a while, a general convulsive syndrome occurs. Opisthotonus occurs - the patient arches on the bed in the form of an arch, leaning only on the heels and the back of the head. With the further development of the disease, convulsions arise from the slightest stimuli and continue almost continuously.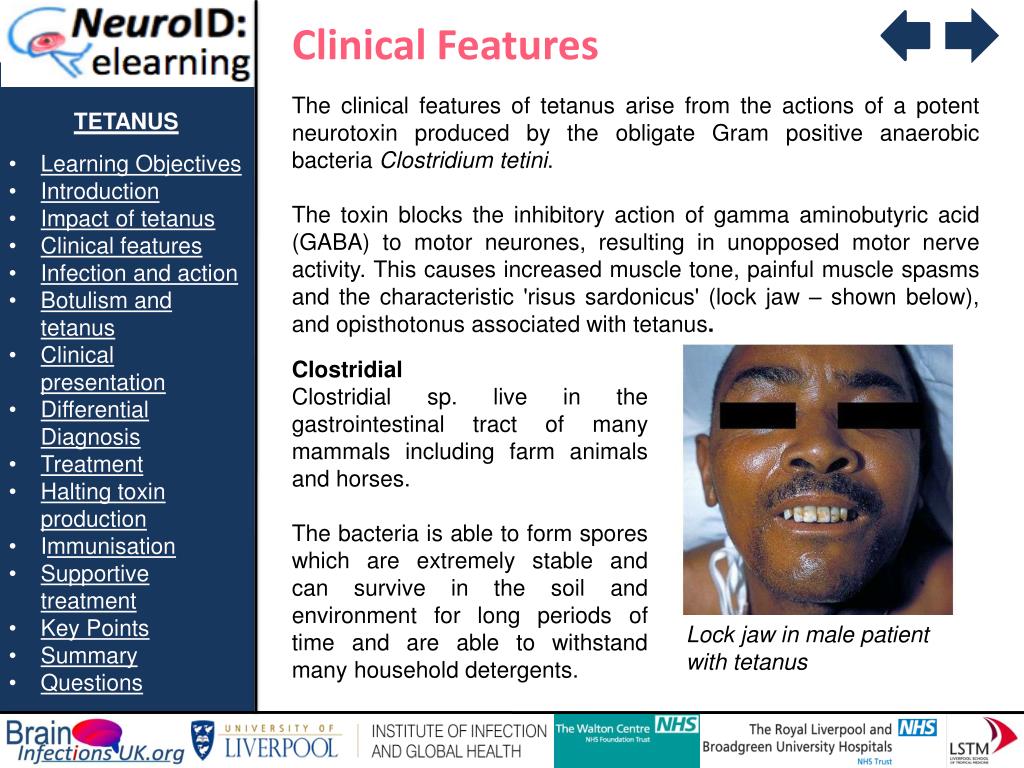 With increasing phenomena of asphyxia and circulatory disorders, a fatal outcome can occur.
With increasing phenomena of asphyxia and circulatory disorders, a fatal outcome can occur.
Vaccination course and routine vaccinations.
Tetanus shot for children . To create immunity against tetanus, all children from the age of 3 months are injected with tetanus toxoid, which is part of the domestic DTP vaccine (ADS) and its foreign analogues (Pentaxim, Infanrix, Infanrix Hexa). Vaccination is carried out three times with an interval of 45 days and a single revaccination 12 months after the 3rd vaccination, i.e. at 18 months of age. Further, according to the vaccination schedule, revaccination is carried out with ADS-anatoxin at 7 and 14 years and then every 10 years.
Adult tetanus shot . In Russia, adults are vaccinated against tetanus once with a combined ADS-M vaccine every 10 years, starting from the last vaccination at the age of 14-16 years (hereinafter at 24-26 years old, 34-36 years old, etc.). If an adult does not remember when he was last vaccinated against tetanus, he should receive a vaccination with Td-M twice at an interval of 45 days and with a single booster 6-9 months after the 2nd dose.
If an adult does not remember when he was last vaccinated against tetanus, he should receive a vaccination with Td-M twice at an interval of 45 days and with a single booster 6-9 months after the 2nd dose.
Tetanus vaccination is available at all polyclinics in the community free of charge as part of the compulsory health insurance program.
Tetanus emergency prophylaxis.
Emergency prophylaxis of tetanus is carried out in case of:
- injuries with violation of the integrity of the skin and mucous membranes;
- frostbite and burns (thermal, chemical, radiation) of the second, third and fourth degree;
- penetrating lesions of the gastrointestinal tract;
- community-acquired abortions; 90,051 deliveries outside health facilities;
- gangrene or tissue necrosis of any type, long-term abscesses, carbuncles;
- animal bites.
Emergency prophylaxis of tetanus consists of primary debridement and simultaneous administration of a vaccine (DT or ADT-M). Emergency tetanus immunoprophylaxis should be carried out as early as possible and up to 20 days after injury, given the length of the incubation period for tetanus disease.
Emergency tetanus immunoprophylaxis should be carried out as early as possible and up to 20 days after injury, given the length of the incubation period for tetanus disease.
For the purpose of emergency prevention of tetanus, it is necessary to contact the district trauma centers (round the clock):
- Center for Traumatology and Rehabilitation, St. Petersburg City Clinic No. Generala Khruleva, house 7a;
- Traumatology department of the polyclinic department No. 121, St. Petersburg State Budgetary Institution of Health "City Polyclinic No. 114" for adults, st. Kamyshovaya, d.50, building 1,
or to the emergency room of St. Petersburg GBUZ "Clinical Infectious Diseases Hospital named after S.P. Botkin" at the address: st. Mirgorodskaya, 3 (round the clock).
Tetanus shot for children - vaccination schedule and side effects of vaccines
Tetanus is a serious illness caused by a bacterial toxin that attacks the nervous system and causes painful muscle contractions, especially in the muscles of the jaw and neck.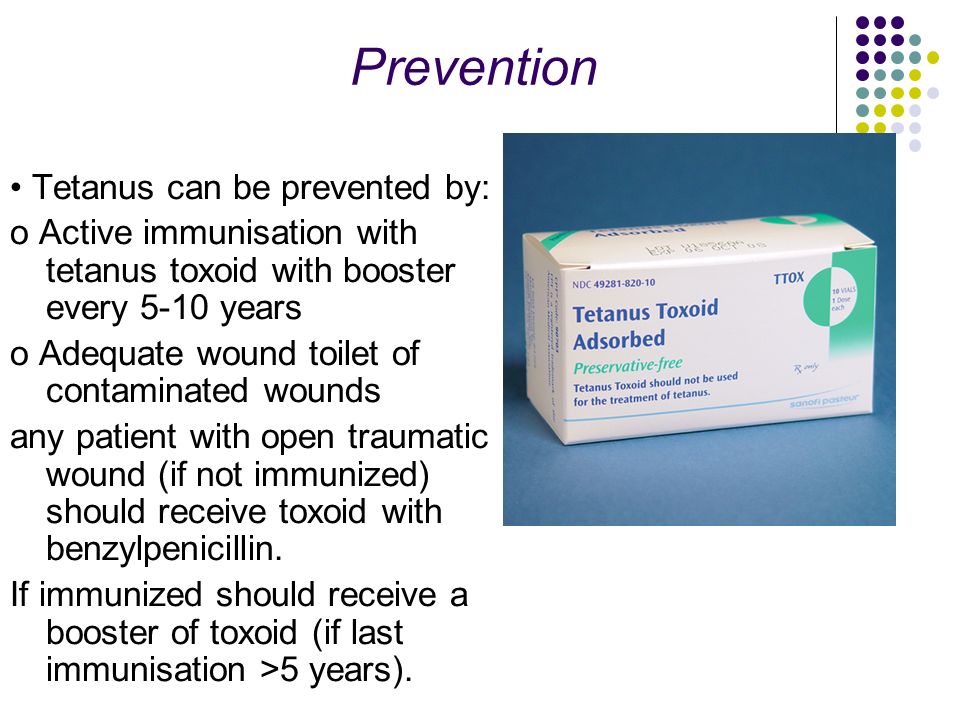 Tetanus can interfere with the ability to breathe and can be life-threatening. The main habitat for dangerous bacteria is soil, saliva and animal feces.
Tetanus can interfere with the ability to breathe and can be life-threatening. The main habitat for dangerous bacteria is soil, saliva and animal feces.
The daily life of children and adults is impossible without injuries that affect the integrity of the skin and mucous membranes. And if the wound is contaminated with soil elements in the absence of immunity to tetanus, this can cause infection. Tetanus vaccination is the only protection against this disease. In order for the human body to develop immunity to the disease, it is necessary to administer special vaccines containing neurotoxin and tetanus toxoid. When children are vaccinated against tetanus, these substances are released into the bloodstream, activating the immune system and producing protective antibodies.
Where can I get a tetanus shot? The RebenOK clinic in Moscow vaccinates the population in accordance with established standards and deadlines. You must first make an appointment with a pediatrician to exclude possible contraindications.
Once tetanus toxin binds to nerve endings, it cannot be removed. Full recovery from a tetanus infection requires the development of new nerve endings, which can take several months.
Consequences of a tetanus infection:
· Fractures. Rigidity of muscle spasms can lead to fractures of the spine and other bones.
Development of pulmonary embolism. The displaced clot may block the main artery of the lung or some of its branches.
· Death. Severe muscle spasms caused by tetanus can cause respiratory arrest, which is the most common cause of death.
To prevent a sad outcome, it is recommended that the child be vaccinated against tetanus at the scheduled time.
The tetanus shot is an inactivated vaccine (not live) and contains a toxin produced by the bacterium but completely devoid of toxicity (toxoid). Once injected, it cannot cause disease, but retains its ability to stimulate antibody production.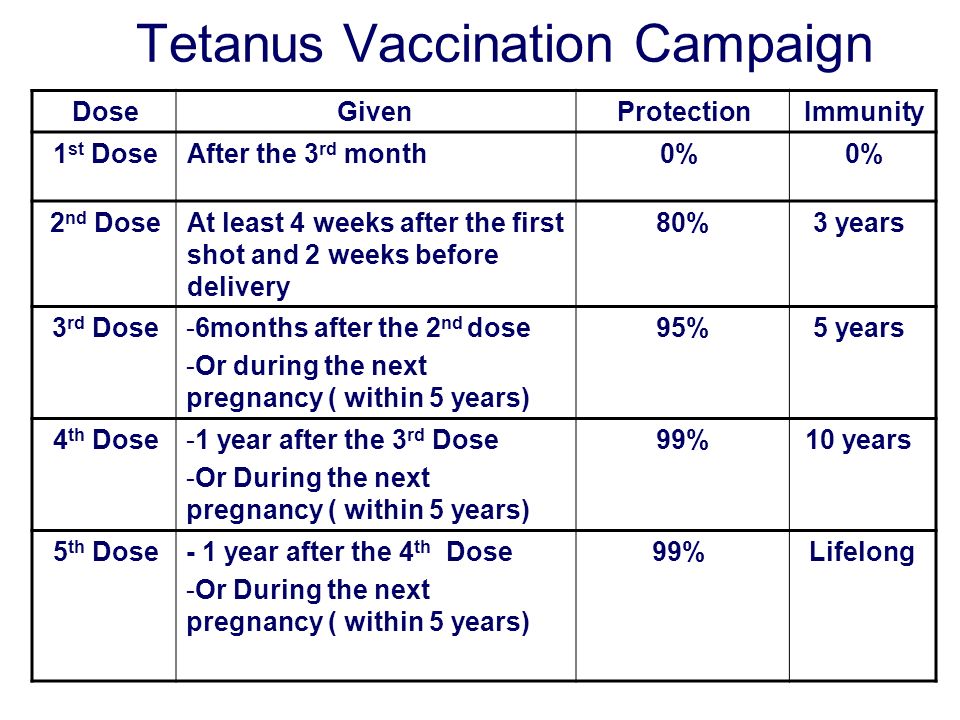 The tetanus vaccine is always included in combination vaccines that include other components.
The tetanus vaccine is always included in combination vaccines that include other components.
Where is the tetanus shot given? It all depends on the drug. The vaccine is administered intramuscularly in the subscapular region, in the thigh or shoulder.
Types of tetanus vaccines at the RebenOK clinic:
· "Adasel". The vaccine is intended for patients aged 4-64 years. Efficacy and safety confirmed. Revaccination is carried out once at a dose of 0.5 ml. The vaccine is injected into the deltoid muscle of the shoulder intramuscularly.
· "ADS-M". Used for children aged 6 years and for adults. Introduced every 10 years. It is prescribed mainly if other drugs need to be replaced due to complications. Forms strong immunity. Requires revaccination every 10 years. Inoculation is introduced under the shoulder blade or in the anterior outer part of the thigh.
· "AKDS". Adsorbed drug for tetanus, diphtheria and whooping cough. Suitable for children from 3 months of age to 4 years of age. Vaccination consists of three injections 45 days apart, followed by a booster one year after the third vaccination. Good protection is guaranteed if revaccination recommendations are followed.
Vaccination consists of three injections 45 days apart, followed by a booster one year after the third vaccination. Good protection is guaranteed if revaccination recommendations are followed.
· "Pentax". Vaccination against tetanus, diphtheria, whooping cough, polio and Haemophilus influenzae infection. Forms strong immunity throughout life. The vaccine is given to children from 3 months of age.
· "Infanrix Hexa" (Belgium). Combined drug for tetanus, hepatitis B, diphtheria, Haemophilus influenzae, whooping cough and polio.
The choice of drug is up to the doctor. The pediatrician must first study the child's medical history and select the most appropriate vaccine, taking into account individual characteristics.
Tetanus vaccination for children has a low reactogenicity, so there are practically no restrictions on the composition. The main contraindication is the occurrence of allergic reactions or neurological damage after a previous injection.
Temporary contraindications for tetanus vaccination:
Influenza and acute respiratory infections;
diathesis, eczema and other skin manifestations;
Allergic reactions and immunodeficiency;
· An increase in body temperature.
Vaccination in these cases is carried out after full recovery. A preliminary consultation with a pediatrician is a prerequisite.
The clinical efficacy of tetanus toxoid is estimated at 100%. After the primary vaccination series, all vaccinated have antibody titers above the level of protection. How long does the tetanus vaccine last? Protective antibodies in properly vaccinated people persist for more than 20 years.
The decrease in the incidence of tetanus since the introduction of systematic vaccination confirms the effectiveness in preventing this disease. Tetanus toxoid is considered a safe drug.
All vaccines should be treated like a medicine, so they may have side effects. In the case of the tetanus vaccine, adverse reactions are moderate.
In the case of the tetanus vaccine, adverse reactions are moderate.
The most commonly reported symptoms are:
Pain, redness and inflammation at the injection site;
Headache and slight fatigue;
· Nausea and vomiting (especially in adolescents).
Currently, there are fewer contraindications, as purified antigens are used. If adverse reactions occur, you should consult a doctor for the appointment of symptomatic therapy.
The tetanus shot rarely causes complications. But you should be prepared for the occurrence of the following disorders:
· anaphylactic shock;
urticaria;
angioedema;
convulsions;
dermatitis.
But such complications are very rare.
A slight increase in temperature after vaccination should not cause alarm. So the child's body can react to the injected substance. There is a process of processing vaccination antigens and the formation of immunity to the disease. There is a release of components that cause an increase in temperature.
There is a release of components that cause an increase in temperature.
It should be remembered that any manifestations are individual in nature. Adults and children may react differently.
If the temperature does not rise above 37.5 degrees and lasts no more than 3 days, there is no need to consult a doctor. This is considered a normal reaction of the body. An elevated temperature, as a reaction to a vaccination, usually manifests itself after 5-7 hours, in some babies the next day. If the temperature lasts longer and its increase is noted, it is necessary to seek help, as there may be other causes of this symptom.
In a children's clinic, during preventive examinations, parents are informed when they are vaccinated against tetanus. Full vaccination of children includes the administration of a total of 6 doses of the drug in accordance with the recommendations of the vaccination schedule for children:
· 3 doses during the first year of life 45 days apart, starting at 3 months of age (3, 4, 5 and 6 months), administered in a combined pentavalent or hexavalent vaccine;
A year later, a booster (additional) dose is administered - in the form of a pentavalent combined vaccine;
6-7 years Another dose using a low antigen load vaccine in combination with diphtheria toxoid and a low antigen load (dpaT) component of pertussis can also be used with the standard combination (DPaT).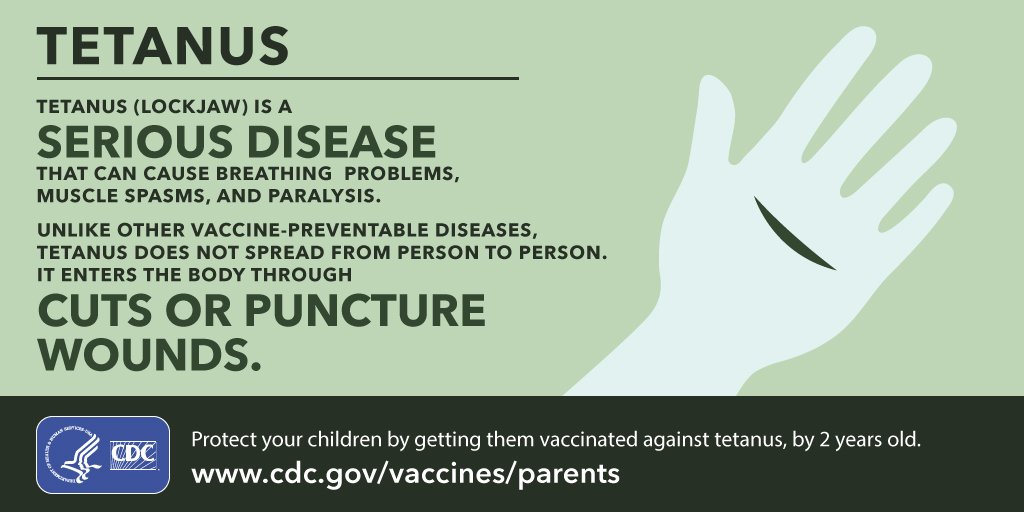
At age 14, another dose is given that uses a low-load vaccine (antigenic diphtheria toxoid plus tetanus toxoid and pertussis (dpaT)).
How often is the tetanus shot given? Revaccination is offered every 10 years to the entire population.
The causative agent of tetanus, clostridium (tetanus bacillus), is widely distributed throughout the world and is resistant to environmental influences. When it enters the body of a child, the stick releases an exotoxin, which has a high damaging ability. The course of the disease is fulminant and very rapid. The increase in symptoms occurs instantly, mortality rates are very high.
Treatment of tetanus is carried out in stationary conditions in intensive care units. Muscle relaxants are prescribed to relieve seizures. Quite often, patients are transferred to artificial ventilation of the lungs. The pH level of the blood is corrected with medication, and support for the work of the cardiovascular, excretory and respiratory systems is also required.