Can mastitis affect baby
Mastitis | Breastfeeding Challenges | Start for Life
There may be times when breastfeeding is challenging. Never ignore any issues you may have – talk to your health visitor, midwife, GP or breastfeeding specialist as soon as possible, they will be able to help you sort it out quickly.
Here are some common breastfeeding issues, and tips on what to do.
- Colic
- Constipation
- Mastitis
- Milk supply
- Reflux
- Sore nipples
- Thrush
- Tongue-tie
Mastitis
Mastitis makes your breast tissue inflamed and painful. You might notice a lump around the sore area, sometimes the inflammation turns into an infection. Mastitis can make you feel achy and run down, with flu-like symptoms or a fever.
Symptoms
Usually, mastitis affects one of your breasts, but can sometimes affect both. Signs and symptoms of mastitis often develop quickly and can include:
- sore breasts that feel swollen, hot, painful to touch.
You may also have red patches, but redness can be harder to see on brown and black skin
- a lump or hard area on your breast
- feeling tired, run down and feverish – you may have flu-like symptoms
What causes mastitis?
If you're breastfeeding, mastitis is usually caused when the milk in your breast builds up faster than it's being removed. This creates a blockage in your milk ducts (known as 'milk stasis') and can be brought on by:
- your baby not latching on properly
- missing feeds, or not feeding often enough
- feeding from one breast more often than the other
- an injury that damages a milk duct or gland
If you aren't breastfeeding, mastitis can be caused by infection. The infection could happen if your nipples are sore or cracked, or through a nipple piercing.
How long does mastitis last?
If you catch the early signs of mastitis, it's quick and easy to treat. If the pain continues for more than a few days, it may be a sign that you've got an infection, and it's time to make a GP appointment.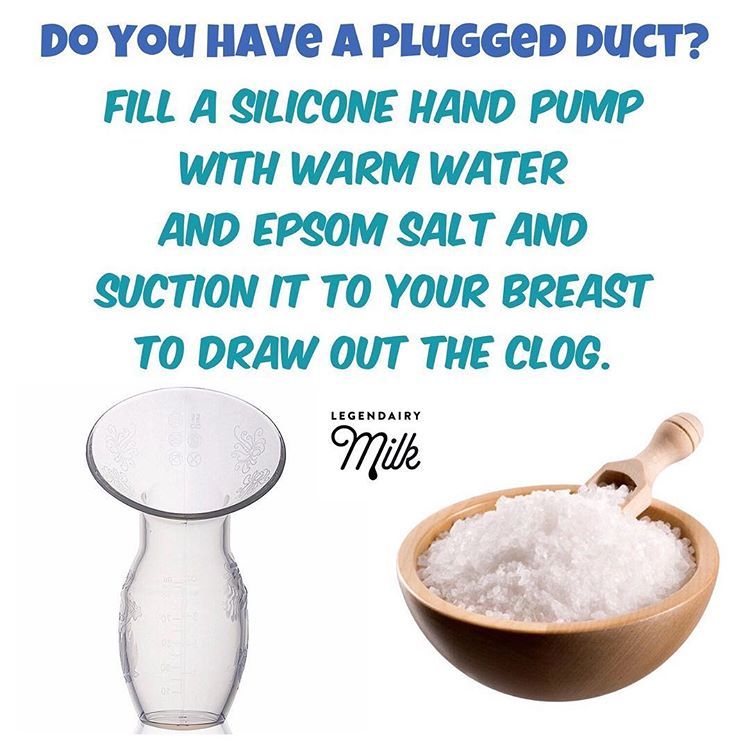 Your GP may prescribe a course of antibiotics, which should clear up the infection in a few days.
Your GP may prescribe a course of antibiotics, which should clear up the infection in a few days.
Treating mastitis
The main thing to do is carry on breastfeeding (even though it may be extremely painful). By stopping breastfeeding, the blockage will only get worse. Even if you have an infection, breastfeeding won't harm your baby (although your milk may taste a little salty).
Make sure your baby is latched on properly and aim to feed 8 to 12 times a day (including at night). Try putting a warm flannel over your breast before feeding, this will help ease the pain and encourage the let-down reflex.
After feeds, make sure any leftover breast milk is drained by expressing by hand or with a pump.
Don't leave it too long. If you feel that you're not improving and continuing to feed regularly isn't making a difference, see your doctor. They'll be able to assess whether your mastitis is caused by an infection. If it is, you may need antibiotics. It would also help to see a breastfeeding specialist who would be able to check your baby's attachment and positioning.
Self-help methods
- Remember to drink fluids when you are thirsty.
- Get plenty of rest – take your baby to bed and feed frequently (8 to 12 times every day, including night time).
- Express your milk in between and after feeds to make sure all your breast milk is removed.
- Medication such as paracetamol and ibuprofen can reduce pain. Although some paracetamol can enter your breast milk, it's not enough to harm your baby.
- Avoid wearing tight, restrictive clothes and bras which can restrict milk flow.
- Ease the pain by putting a warm flannel over your breast – warm showers and baths may help.
- Massage the affected area if it's not too painful, gently massage on and around the affected area.
Breastfeeding Friend from Start for Life
The Breastfeeding Friend, a digital tool from Start for Life, has lots of useful information and expert advice to share with you – and because it's a digital tool, you can access it 24 / 7.
Preventing mastitis
Luckily, once it's diagnosed, mastitis is easy and quick to treat. But remember, prevention is better than cure.
Reducing the risk of mastitis
- If possible, breastfeed exclusively (avoid using first infant formula to top up, or a dummy).
- Feed frequently and responsively – long gaps in between feeds can create a build-up of breastmilk.
- Encourage your baby to feed if you feel your breasts are getting full.
- Make sure your baby latches on properly – try different breastfeeding positions to work out which is most comfortable.
- Wait for your baby to finish feeding – usually, they'll release when they're finished.
- When you want to stop breastfeeding, try cutting down your feeds gradually (don't suddenly go longer between feeds).
- Avoid wearing a bra or clothing that is too tight and puts pressure on your breasts.
What is Mastitis and What Can You Do About it?
Mastitis is inflammation of the breast that may be accompanied by infection.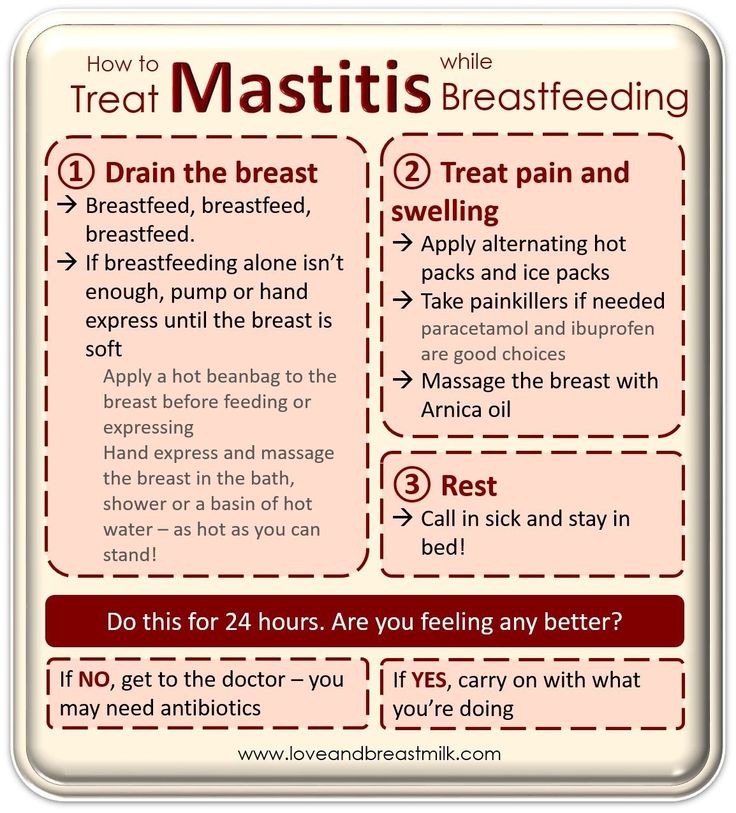 Mastitis affects about 20% of Australian women. Mastitis mostly occurs during the first six weeks postpartum, however, it can also occur at any other point during your breastfeeding journey...
Mastitis affects about 20% of Australian women. Mastitis mostly occurs during the first six weeks postpartum, however, it can also occur at any other point during your breastfeeding journey...
Share this content
To help you understand this condition, we have prepared a list of its potential causes. Then, more importantly, we have offered a few suggestions for how to deal with mastitis.
Mastitis Can Be Caused By the Following
Here are a few of the many factors that can influence the development of mastitis.
- An untreated blocked duct
- Having cracks or damage on your nipples, which may allow bacteria to enter your breast
- A baby’s poor attachment to the breast
- Having long periods of time between feeds
- Having breasts that are too full
- Wearing a bra or clothing which is too tight and “cutting in” to your skin
- Weaning from breastfeeding quickly
- Breastfeeding attachment difficulties; i.
 e. a baby with a tongue-tie
e. a baby with a tongue-tie - In some cases, women with over-supply may experience mastitis
Signs and Symptoms Which You May Experience
Here are a few things that you may notice if you think that you are developing mastitis.
- A red area on the breast
- Soreness or tenderness in the breast
- A warm or hot area on the breast
- You may feel like you have the flu – feeling hot and cold with aching joints
- You may have a temperature (over 38.5 C)
It is also important to consider the following when you think that you may be suffering from mastitis.
- Mastitis may affect one or both breasts
- It can get worse within just a few hours. So, it’s important to be alert and to start treatment as soon as possible
How to Manage Mastitis
In addition to considering the recommendations below, it is important to seek help from a lactation consultant, maternal child health nurse or GP.
- Start treatment at the first signs of mastitis
- Rest as much as you can – Get help from family, friends, and neighbours to help you over the next few days. Rest is important… but, we know how difficult for it can be to find for new mums. This is the time when you call out for help from those around you.
- Aim to breastfeed or express as frequently as you can (8-12 times in 24 hours). Try and keep the affected breast as drained as possible.
- Your breast milk is safe for your baby even if you have mastitis
- Drink plenty of water or fluids and eat nutritious food
- Apply a warm heat pack or face washer to the affected breast before feeding or expressing.
- Breastfeed or express from the affected breast first at each feed. If this is too painful, breastfeed off of the non-affected side for a short while first. This will help the affected breast’s milk to start flowing. Then put your baby back on the affected breast once more. As the milk has already been stimulated to flow it should make the breastfeeding on this side feel easier.
- If you are finding that it is hard to get the milk flowing, try hand expressing before feeds.
- Get help to ensure you are positioning and attaching your baby to the breast correctly.
- Try different breastfeeding positions, as this may help to clear the blockage
- Gently but firmly massage the affected area towards the nipple during the feed
- If, after a breastfeed, you still feel full, express until the breast feels well drained
- Using a cold pack (a packet of frozen peas wrapped in a cloth) after a breastfeed or expression may be soothing and reduce some inflammation
- An anti-inflammatory, such as ibuprofen is safe to use for pain relief. If you are unable to take this type of medication take paracetamol as directed on the box.
It is Important to See a Doctor When Any of the Following Occur
While it never hurts to give your doctor a call with any concerns, it is especially important that you reach out for professional help if any of the following happen.
- Symptoms have not improved within 12 hours of management (as above). Antibiotics are usually recommended by your GP at this stage.
- Mastitis has been cleared up and then reoccurs some days or weeks later
- There is presence of pus or blood in your breastmilk
- The mastitis is hospital-acquired (you developed mastitis during an inpatient stay in the hospital)
- The mastitis is severe or unusual – if you have any concerns or are not sure it is highly advised you are reviewed by a doctor.
In these cases (above), laboratory investigations or other diagnostic procedures will be recommended by your doctor.
Will My Milk Supply Be Affected by Mastitis?
Some mums do notice a temporary drop in their milk supply following a bout of mastitis.
Sometimes a baby may be fussier on the affected breast during mastitis. This is because the milk can become salty in taste, or, if your supply has dropped and is no longer flowing as quickly as baby is used to, it can cause them to be fussier during feeds.
Even if the milk supply drops in the affected breast, the other side will increase in milk to keep your baby well fed.
Once you are well again, try to feed your baby more frequently or add in an extra expression after feeds on the previously affected breast. This will send signals to your breasts to increase the milk supply again. And, of course, if you are concerned about your milk supply please seek extra help from a lactation consultant.
For community support, please check out the following resources:
Australian Breastfeeding Association – ABA helpline
1800 686 2 686 (1800 mum 2 mum)
https://www.breastfeeding.asn.au/services/index
https://www.breastfeeding.asn.au/bfinfo/index.html
The Maternal & Child Health Line
Available 24 hours a day, 7 days a week - 13 22 29
Maternal and Child Health Nurse local centers
Contact your local council
Lactation consultants at local hospital
Some hospitals have their own breastfeeding clinics. Phone your local hospital for an appointment
Phone your local hospital for an appointment
Private Lactation consultants
LCANZ
Health Direct
https://www.healthdirect.gov.au/breastfeeding-problems
For more information head over to our Medela Australia Facebook page.
What questions do you have about breastfeeding? How would you describe your breastfeeding experience so far? Let’s have a chat here or on our Medela Australia Facebook page.
Mastitis: symptoms and treatment | Philips Avent
search support iconSearch Keywords
Home ›› Breastfeeding mastitis symptoms and treatment
Home ›› Breastfeeding mastitis symptoms and treatment
↑ top
breastfeeding - one of the most natural processes for a woman, but it is not always easy. Along with the individual aspects of breastfeeding, there are some general problems that new breastfeeding mothers may face.
One of them is mastitis, an inflammatory disease that causes tenderness and tenderness in the breast tissue.
The frequency of lactational mastitis among women in different countries ranges from 2% to 33% and averages about 10%*.
Mastitis in breastfeeding women is caused by a bacterial infection of the milk ducts that enters through cracks, irritation of the nipple, or a nipple piercing.
Lactational mastitis is dangerous because it can cause pain while breastfeeding, interfere with the bonding process between mother and baby, or even interfere with milk production.
To protect the health and comfort of mother and baby, and the mother's milk supply, this problem must be addressed urgently.
So, here are the answers to the most frequently asked questions about mastitis and the fight against it: “How does mastitis occur?”, “What are the symptoms of mastitis?” and "Is it possible to breastfeed with mastitis?".
Ask your doctor for more information.
Signs of mastitis
What does mastitis feel like? In addition to pain and discomfort, symptoms of mastitis can also include fatigue and a feeling of exhaustion.
How mastitis manifests:
- fever (>38.5°C) and/or flu-like symptoms;
- nausea;
- vomiting;
- yellowish discharge from the nipple;
- chest warm or hot to the touch;
- pink or red breasts.
These symptoms of mastitis are similar to the symptoms of breast engorgement, but there is a fundamental difference between these conditions. Mastitis differs from engorgement in that it usually only affects one breast, not both.
Causes of mastitis
Mastitis can develop in a new mother at any time, but it usually occurs within the first two to three weeks after childbirth. A common cause of this disease is long breaks between feedings - for example, when the baby begins to sleep through the night.
Other possible causes of mastitis are:
- improper breastfeeding;
- incomplete outflow of milk from the mammary glands, for example, due to blockage of the milk duct;
- unattended breast engorgement;
- regular pressure on some part of the breast, wearing tight clothing;
- chest injury caused by injury or impact.
In short: mastitis usually develops as a result of too much milk in the breast, known as milk stasis. Stagnation of milk provokes the growth of bacteria, which causes mastitis and symptoms of pain and fever. Therefore, to prevent mastitis and stagnation of milk, it is important to make sure that it is removed from the breast properly.
Blockage of the milk ducts can also be the cause. Mastitis is indeed caused by milk stagnation or too long milk in the breast, but this condition and the subsequent symptoms of mastitis - fever and pain - are precisely due to the rapid multiplication of bacteria due to milk stagnation.
Prevention of mastitis while breastfeeding
The good news is that there are many ways to prevent mastitis. Below you will find some tips on how to avoid mastitis.
1. Care for your breasts to prevent nipple irritation. Proper breast care can help prevent mastitis by gently massaging and keeping your nipples dry with soft bra pads.
Find out more about breast care in our article here.
2. Feed your baby often. For complete emptying of the breast, it is important to feed regularly and on time. Even if the baby is sleeping, it should be woken up when it's time for feeding. If the mother cannot be with the baby during feeding, she should express milk from the breast using a breast pump.
Choose an easy-to-use breastpump, such as a single electric breastpump. It allows you to express gently and naturally thanks to the special Natural Motion technology. Many of the complications of breastfeeding can be avoided if the baby latch on properly.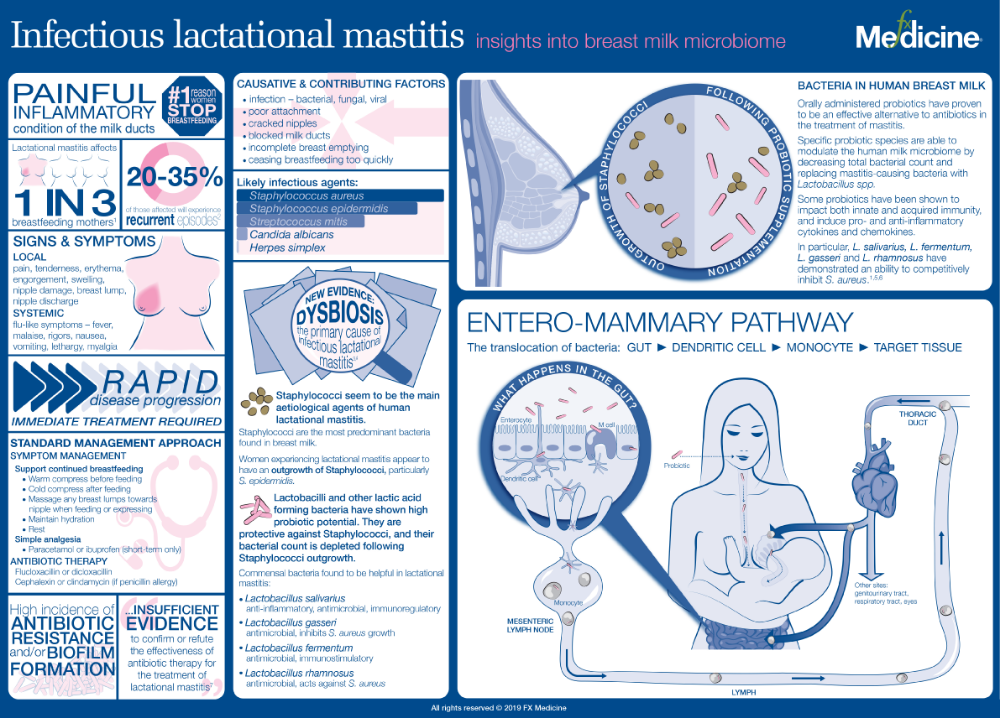 Try different breastfeeding positions to find one in which the baby will properly latch onto the breast. This will help prevent mastitis and other problems. We talk more about breastfeeding positions in the article at the link.
Try different breastfeeding positions to find one in which the baby will properly latch onto the breast. This will help prevent mastitis and other problems. We talk more about breastfeeding positions in the article at the link.
4. Wean your baby gradually. To minimize the chance of complications, it is necessary to reduce milk production by gradually reducing the number of breastfeeds.
If you're interested in stopping breastfeeding, check out our tips for weaning your baby in the article here.
Treatment of mastitis in women
One of the most common questions that breastfeeding mothers face with mastitis is: “Can I continue to breastfeed?” Answer: yes. What's more, breastfeeding for mastitis can help clear the infection without causing harm or side effects.
An important point: if you have symptoms of mastitis, contact your doctor immediately. Doctors usually prescribe antibiotics (such as acetaminophen or ibuprofen) to relieve symptoms of mastitis after making sure that the prescribed drug is safe for breastfeeding.
Mastitis can be uncomfortable, but there is no reason to panic or despair. This is a common problem that many new mothers experience when breastfeeding for the first time. By following the advice in this article, you can reduce the likelihood of developing mastitis, but if something bothers you, you should seek the help of a specialist.
Articles and tips from Philips Avent
*Lactational mastitis and lactostasis: tactical contraversion. O.A. Void. Peoples' Friendship University of Russia, Moscow, 2013
Baby+ app
Download the app and track your child's development and growth with trackers, and save these special moments forever.
Download App:
App Pregnancy+
Download one of the world's best pregnancy tracking apps for weekly helpful information, articles and tips about pregnancy and baby development.
Download app:
You are leaving the Philips Healthcare (“Philips”) official website. Any links to third party websites that may be included on this site are provided solely as a convenience to you. Philips makes no warranties regarding any third party websites or the information they contain.
Any links to third party websites that may be included on this site are provided solely as a convenience to you. Philips makes no warranties regarding any third party websites or the information they contain.
I understand
You are about to visit a Philips global content page
Continue
You are about to visit the Philips USA website.
I understand
Mastitis
➢ Incomplete recovery from primary mastitis may predispose to recurrence. If you have been prescribed antibiotics, it is important to take the entire course. If a previously prescribed antibiotic was ineffective, a milk culture and a swab from the child's throat will help determine the appropriate medicine.
➢ Fatigue and stress from everyday problems, or from some extraordinary events, for example, from travel, holidays, parties, moving, can lead to breast disease
➢ Anemia can also be one of the factors. A hematologist will examine you and determine if you need to take vitamins or iron supplements.
A hematologist will examine you and determine if you need to take vitamins or iron supplements.
➢ Smoking reduces resistance to infections. In addition, smoking inhibits hot flashes (milk ejection reflex). This can lead to recurring breast infections as the milk "stagnates" in the breast.
➢ Excess milk can prevent the baby from completely emptying the breast. Let your baby finish sucking on the first breast before offering the second. If your breasts are very engorged, you can express some milk to ease the discomfort.
➢ An inflamed, cracked or bleeding nipple is a possible gateway for infection. If the problem with the nipples persists, you need to carefully monitor the correct application. Consult a mammologist to find out what can cause cracked nipples.
➢ If you notice a dried discharge covering one of the pores on the nipple, apply a warm, damp compress and then express some milk until the hole is clear. Some mothers have noticed a thick yellowish plug coming out when pumping. (It won't harm your baby if he sucks it on his own while feeding)
(It won't harm your baby if he sucks it on his own while feeding)
➢ Nipple shields can slow down the flow of milk and promote infection. The use of pacifiers and nipples can affect the baby's suckling technique and contribute to nipple problems and lactose intolerance.
➢ Some babies are reluctant to breastfeed or refuse to breastfeed intermittently, possibly due to sensitivity or other problems. Irregular feedings can contribute to recurring breast infections. A mammologist can help you find the cause of your baby's refusal to breastfeed.
➢ Make sure your clothes are not too tight. Pay special attention to the bra. Some bras and swimwear, especially those with underwire, can squeeze your breasts too much. Even a heavy shoulder bag or frequent use of a sling or kangaroo can cause breast problems. In this case, a frequent change of the shoulder on which you carry the bag or kangaroo will help.
➢ The seat belt in the car can also cause recurring mastitis. Too tight belt can put pressure on the chest. Another reason is that the belt cuts into the chest during heavy braking. Other injuries leading to lactostasis may be pushing or hitting an older child who has raged. The resulting stagnation of milk is treated with rest, warmth and frequent feedings.
Too tight belt can put pressure on the chest. Another reason is that the belt cuts into the chest during heavy braking. Other injuries leading to lactostasis may be pushing or hitting an older child who has raged. The resulting stagnation of milk is treated with rest, warmth and frequent feedings.
➢ The risk of infection is increased if the mother has ever had surgery or breast trauma or lumps in it.
➢ One researcher suggested that cutting out saturated fat from the diet and taking one tablespoon of lecithin a day could help moms who have had lactose and/or mastitis.
➢ Excessive salt intake can lead to fluid retention in tissues, which reduces resistance to infections. On the other hand, lack of salt can also be the cause of recurring mastitis.
➢ Food allergies and exposure to other allergens are also a possible factor in the development of recurrent mastitis.
➢ An excessive amount of repetitive shoulder movements is also considered a factor predisposing to recurrence of mastitis.