Cervical cancer during pregnancy
Pregnancy | Cervical cancer | Cancer Research UK
If you're diagnosed with cervical cancer when you are pregnant, what will happen depends on:
- the type of cervical cancer you have
- how big the tumour is and whether it has spread (its stage)
- how many weeks pregnant you are
- what your wishes are
Multi disciplinary team
Your doctor is part of a multi disciplinary team who will discuss your situation, and decide together what the best treatment options are in your case. This team includes a:
- doctor specialising in cancer drug treatment such as chemotherapy (medical oncologist)
- doctor specialising in radiotherapy and cancer drug treatment (clinical oncologist)
- surgeon specialising in cancer of the female reproductive system (gynaecological oncologist)
- doctor specialising in the care of women during pregnancy (obstetrician)
- doctor specialising in the care of newborn babies (neonatal doctor)
- expert in examining and identifying cells (pathologist)
- nurse specialist
To make a decision, you will need full information from your medical and nursing team about your options. They can tell you about the benefits and possible risks of each option.
Treatment
Most women diagnosed with cervical cancer during pregnancy have early stage disease. Research so far suggests that cervical cancers diagnosed during pregnancy grow no more quickly and are no more likely to spread than cervical cancers in women who are not pregnant.
In the second or third trimester
If you are more than 3 months pregnant, your obstetrician will probably say that you can continue the pregnancy but you may have the baby early by caesarean section. You might have your womb removed at the same time. You may then need further treatment with chemotherapy and radiotherapy (chemoradiotherapy).
Less than 3 months pregnant
If you are less than 3 months pregnant, your doctor may want to treat you straight away. Your doctor may feel more than 6 months is too long to leave a cervical cancer without treatment.
If you decide to have treatment then you may need to end the pregnancy.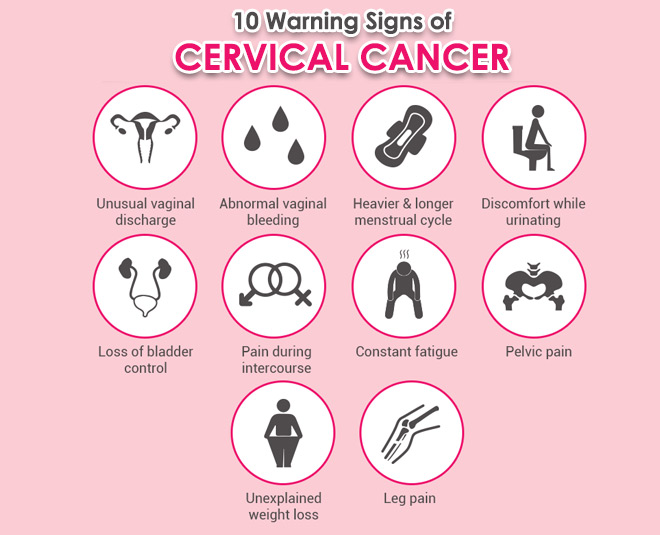 This can be very distressing but remember that you will have support from your nurses and doctors.
This can be very distressing but remember that you will have support from your nurses and doctors.
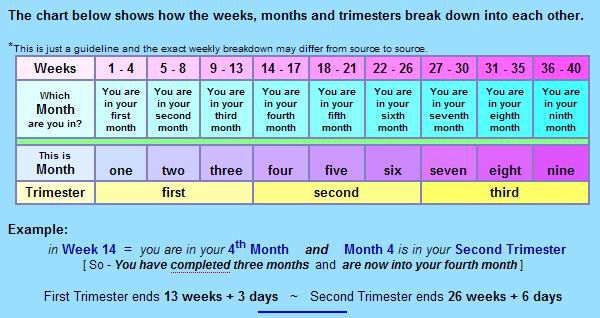
If you want to continue with your pregnancy, your doctor will delay treatment until you are more than 3 months pregnant, during the second trimester. You can't have chemotherapy during the first trimester as it can damage the baby or cause a miscarriage.
Cancer treatment during pregnancy is experimental as there are few cases and no large trials. Also there is little information on the long term outlook of women treated during pregnancy.
For small tumours
For some small tumours it may be possible to have treatment with cone biopsy or trachelectomy. Trachelectomy means removing most of the cervix and the upper part of the vagina.
There are very few women who have had a trachelectomy during pregnancy. There is a risk of bleeding and of losing the baby shortly after the operation. Your doctor will talk this through with you before the operation.
For larger tumours
For larger tumours, your doctor may suggest having chemotherapy to shrink or control the cancer until the baby is born. You can't have chemotherapy during the first trimester as it can damage the baby or cause a miscarriage.
You can't have chemotherapy during the first trimester as it can damage the baby or cause a miscarriage.
Research looking at chemotherapy given after the first trimester of pregnancy has so far not shown an increased risk of birth defects compared to the general population. But researchers need to collect more information over a longer time so we can understand more about the long term outlook for children.
Making decisions about treatment
Deciding on treatment when you are pregnant can be very difficult. You will need some time to think and to find out what all your options are. Make sure you have had the opportunity to ask all the questions you need to ask. You can also ask if there is anyone else you (and your partner) can talk to such as a specialist nurse or counsellor.
Last reviewed:
08 Apr 2020
Next review due:
08 Apr 2023
Print page
-
Gynecologic cancers in pregnancy: guidelines of a second international consensus meeting
F Amant and others
International Journal of Gynecological Cancer, 2014. Volume 24, Issue 3
Volume 24, Issue 3 -
Cancer, pregnancy and fertility: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up
F Peccatori and others
Annals of oncology, 2013. Volume 24, Supplement 6 -
Cervical cancer in pregnant women: treat, wait or interrupt? Assessment of current clinical guidelines, innovations and controversies
S Han and others
Therapeutic advances in medical oncology, 2013. Volume 5, Issue 4
Diagnosis and treatment of cervical cancer in pregnant women
1. Nguyen C, Montz FJ, Bristow RE. Management of stage I cervical cancer in pregnancy. Obstet Gynecol Surv. 2000;55:633. [PubMed] [Google Scholar]
2. Creasman WT. Cancer and pregnancy. Ann N Y Acad Sci. 2001;943:281. [PubMed] [Google Scholar]
3. Smith LH, Dalrymple JL, Leiserowitz GS, Danielsen B, Gilbert WM. Obstetrical deliveries associated with maternal malignancy in California, 1992 through 1997. Am J Obstet Gynecol. 2001;184:1504. [PubMed] [Google Scholar]
Am J Obstet Gynecol. 2001;184:1504. [PubMed] [Google Scholar]
4. Smith LH, Danielsen B, Allen ME, Cress R. Cancer associated with obstetric delivery: results of linkage with the California cancer registry. Am J Obstet Gynecol. 2003;189:1128. [PubMed] [Google Scholar]
5. Demeter A, Sziller I, Csapó Z, et al. Outcome of pregnancies after cold‐knife conization of the uterine cervix during pregnancy. Eur J Gynaecol Oncol. 2002;23:207. [PubMed] [Google Scholar]
6. Duggan B, Muderspach LI, Roman LD, et al. Cervical cancer in pregnancy: reporting on planned delay in therapy. Obstet Gynecol. 1993;82:598. [PubMed] [Google Scholar]
7. Shiping Z, Lushan ZQ, et al. Progress in diagnosis and treatment of pregnancy complicated with cervical cancer. J Pract Med. 2018;25(4):400‐402. [Google Scholar]
8. Meihao OG. The effect of pregnancy with cervical cancer on mother and child and the principle of diagnosis and treatment. Adv Modern Obstetr Gynecol. 2008;17(1):64‐66. [Google Scholar]
[Google Scholar]
9. Morice P, Uzan C, Gouy S, Verschraegen C, Haie‐Meder C. Gynaecological cancers in pregnancy. Lancet. 2012;379(9815):558‐569. [PubMed] [Google Scholar]
10. Morimura Y, Fujimori K, Soeda S, et al. Cervical cytology during pregnancy: comparison with non‐pregnant women and management of pregnant women with abnormal cytology. Fukushima J Med Sci. 2002;48(1):27‐37. [PubMed] [Google Scholar]
11. Li T, Wang J, Song F. Progress in the diagnosis and treatment of gynecological malignant tumors during pregnancy. Cancer Progression. 2018;16(13):1589‐1592, 1615. [Google Scholar]
12. Jain AG, Higgins RV, Boyle MJ. Management of low‐grade squamous intraepithelial lesions during pregnancy. Am J Obstet Gynecol. 1997;177(2):298‐302. [PubMed] [Google Scholar]
13. Schaefer K, Peters D, Aulmann S, Sohn C, Eichbaum M. Value and feasibility of LLETZ procedures for pregnant women with suspected high‐grade squamous intraepithelial lesions and microinvasive cervical cancer.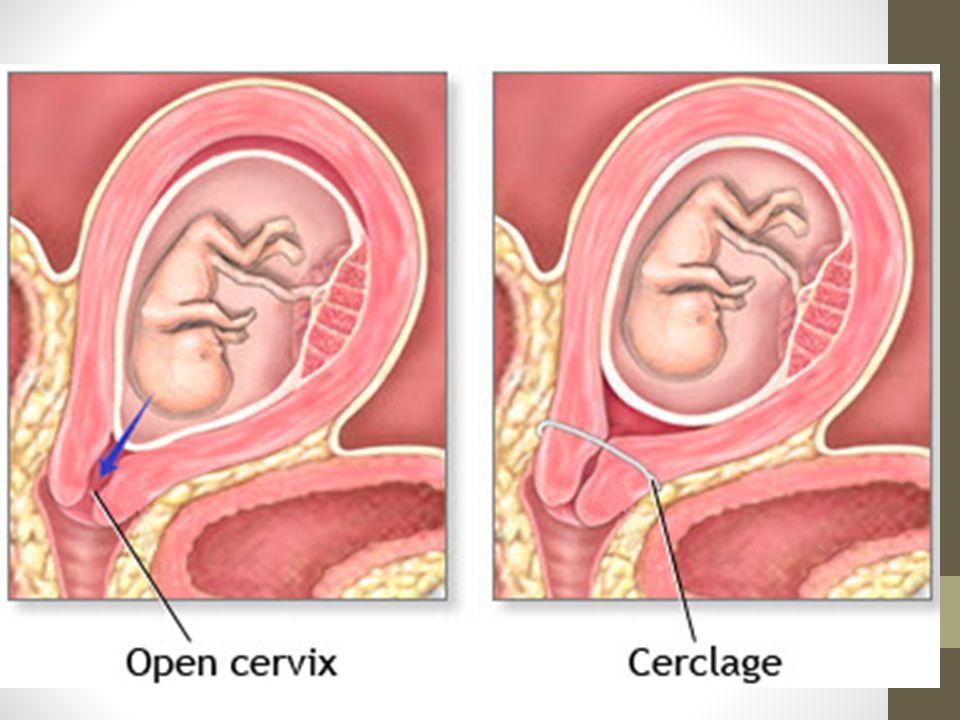 Int J Gynaecol Obstet. 2012;118(2):141‐144. [PubMed] [Google Scholar]
Int J Gynaecol Obstet. 2012;118(2):141‐144. [PubMed] [Google Scholar]
14. Lihui W, Yun Z, Xing X, et al. Expert consensus on the management of cervical cancer in pregnancy. Chinese J Obstetr Gynecol. 2018;19(2):190‐192. [Google Scholar]
15. Siegler E, Lavie O, Amit A, Vaknin Z, Auslander R, Blumenfeld Z. Should the risk of invasive cancer in pregnancy and the safety of loop electrosurgical excision procedure during the first 15 weeks change our practice?. J Low Genit Tract Dis. 2017;21(4):299‐303. [PubMed] [Google Scholar]
16. Robova H, Rob L, Pluta M, et al. Squamous intraepithelial lesion‐microinvasive carcinoma of the cervix during pregnancy. Eur J Gynaecol Oncol. 2005;26(6):611‐614. [PubMed] [Google Scholar]
17. Amant F, Halaska MJ, Fumagalli M, et al. Gynecologic cancers in pregnancy: guidelines of a second international consensus meeting. Int J Gynecol Cancer. 2014;24(3):394‐403. [PubMed] [Google Scholar]
18. Weinmann S, Naleway A, Swamy G, et al.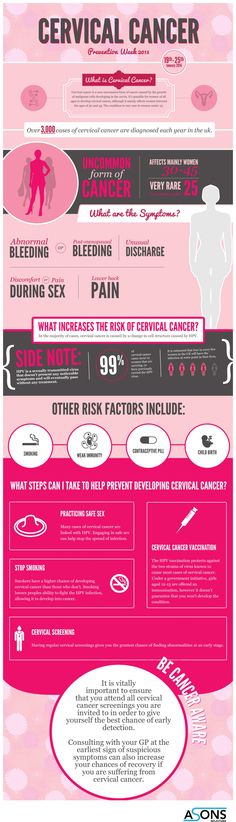 Pregnancy outcomes after treatment for cervical cancer precursor lesions: an observational study. PLoS ONE. 2017;12(1):e0165276. [PMC free article] [PubMed] [Google Scholar]
Pregnancy outcomes after treatment for cervical cancer precursor lesions: an observational study. PLoS ONE. 2017;12(1):e0165276. [PMC free article] [PubMed] [Google Scholar]
19. Botha MH, Rajaram S, Karunaratne K. Cancer in pregnancy. Int J Gynecol Obstet. 2018;143:137‐142. [Google Scholar]
20. Rob L, Skapa P, Robova H. Fertility‐sparing surgery in patients with cervical cancer. Lancet Oncol. 2011;12(2):192‐200. [PubMed] [Google Scholar]
21. Căpîlna ME, Szabo B, Becsi J, Ioanid N, Moldovan B. Radical trachelectomy performed during pregnancy: a review of the literature. Int J Gynecol Cancer. 2016;26(4):758‐762. [PubMed] [Google Scholar]
22. Peccatori FA, Azim HA, Orecchia R, et al. pregnancy and fertility: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow‐up. Ann Oncol. 2013;24(suppl 6):vi160‐vi170. [PubMed] [Google Scholar]
23. Silva LB, Silva‐Filho AL, Traiman P, et al. Sentinel node mapping in a pregnant woman with cervical cancer: a case report. Int J Gynecol Cancer. 2006;16(3):1454‐1457. [PubMed] [Google Scholar]
Int J Gynecol Cancer. 2006;16(3):1454‐1457. [PubMed] [Google Scholar]
24. Jianhuan Z. Progress in the diagnosis and treatment of cervical cancer with pregnancy. China Pract Med. 2010;5(6):245‐246. [Google Scholar]
25. Yukun L, Yinglin L, Shuning Z, et al. Clinical analysis of malignant tumors in pregnancy. Chinese J Clin Med Women Children. 2013;9(1):9‐14. [Google Scholar]
26. Song YZ, Liu Y, Lin M, et al. Efficacy of neoadjuvant platinum‐based chemotherapy during the second and third trimester of pregnancy in women with cervical cancer: an updated systematic review and meta‐analysis. Drug Des DevelTher. 2019;13:79‐102. [PMC free article] [PubMed] [Google Scholar]
27. Calsteren KV, Verbesselt R, Devlieger R, et al. Transplacental transfer of paclitaxel, docetaxel, carboplatin, and trastuzumab in a baboon model. Int J Gynecol Cancer. 2010;20(9):1456‐1464. [PubMed] [Google Scholar]
28. Köhler C, Oppelt P, Favero G, et al. How much platinum passes the placental barrier? analysis of platinum applications in 21 patients with cervical cancer during pregnancy. Am J ObstetGynecol. 2015;213(2):206.e1‐206.e5. [PubMed] [Google Scholar]
Am J ObstetGynecol. 2015;213(2):206.e1‐206.e5. [PubMed] [Google Scholar]
29. Cardonick E, Iacobucci A. Use of chemotherapy during human pregnancy. Lancet Oncol. 2004;5(5):283‐291. [PubMed] [Google Scholar]
30. Furukawa S, Hayashi S, Usuda K, Abe M, Hagio S, Ogawa I. Effect of cisplatin on rat placenta development. ExpToxicolPathol. 2013;65(1/2):211‐217. [PubMed] [Google Scholar]
31. Kozuki N, Lee AC, Katz J, et al. Moderate to severe, but not mild, maternal anemia is associated with increased risk of small‐for‐gestational‐age outcomes. J Nutr. 2012;142(2):358‐362. [PubMed] [Google Scholar]
32. Zagouri F, Sergentanis TN, Chrysikos D, Bartsch R. Platinum derivatives during pregnancy in cervical cancer: a systematic review and meta‐analysis. ObstetGynecol. 2013;121(2 Pt 1):337‐343. [PubMed] [Google Scholar]
33. da Fonseca AJ, Dalla‐Benetta AC, Ferreira LP, et al. Neoadjuvant chemotherapy followed by radical surgery in pregnant patient with invasive cervical cancer: case report and literature review. Rev Bras GinecolObstet. 2011;33(1):43‐48. [PubMed] [Google Scholar]
Rev Bras GinecolObstet. 2011;33(1):43‐48. [PubMed] [Google Scholar]
Management of pregnant women with invasive cervical cancer | Payanidi Yu.G., Borovkova E.I., Dobrokhotova Yu.E., Arutyunyan A.M.
Introduction
Cervical cancer (CC) is one of the most common malignancies in pregnant women, with an incidence of 0.8 to 1.5 cases per 10,000 births. During pregnancy and during the first year after childbirth, up to 3% of cases of the disease are verified [1, 2].
There have been no large randomized trials on which recommendations for the management of pregnant women with cervical cancer can be based. And in the treatment of this category of patients, recommendations based on materials from studies involving non-pregnant patients are applied. At the same time, the tactics of managing pregnant women with cervical cancer is additionally determined by the gestational age, the stage of the tumor process, and the patient's desire to maintain the pregnancy.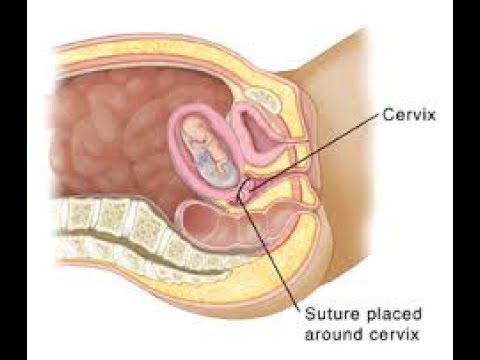 Treatment should be individual, timely, with minimal risk to the woman and fetus [2].
Treatment should be individual, timely, with minimal risk to the woman and fetus [2].
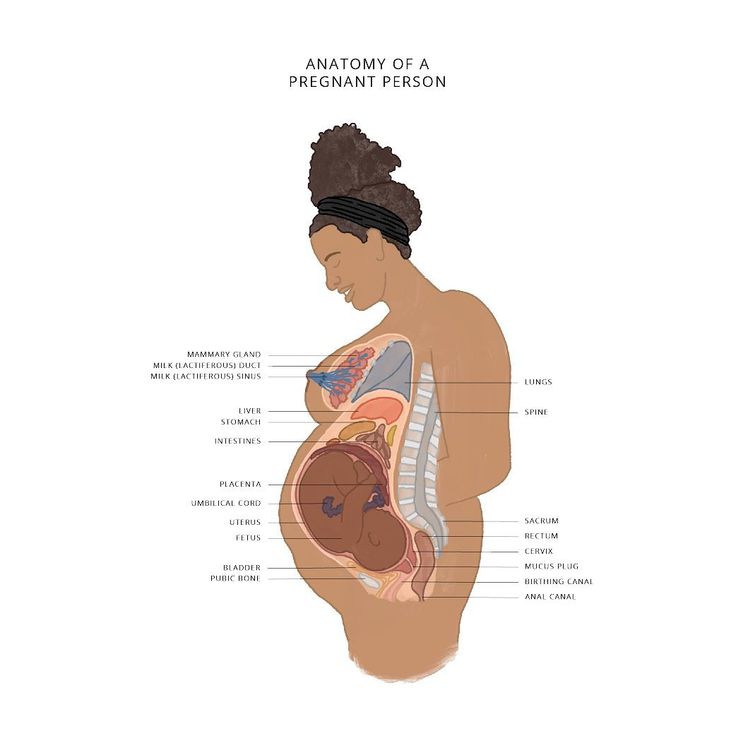
During pregnancy, cervical cancer in most cases is diagnosed in the early stages, and the average gestational age is 19.5 weeks. [3, 4]. Clinical manifestations of cervical cancer during pregnancy are often absent or may be mistaken for obstetric complications (vaginal bleeding, pelvic pain, pain along the sciatic nerve, anemia).
Treatment tactics for patients with cervical cancer
The tactics of treating patients with cervical cancer is determined by the stage of the disease, gestational age, as well as the involvement of regional lymph nodes in the process. The main methods of treatment are surgical and medical (chemotherapy) [5–7] (Table 1).
According to the order of the Ministry of Health of Russia No. 572n dated November 1, 2012, all pregnant women are subject to mandatory cytological screening, which allows for a timely diagnosis.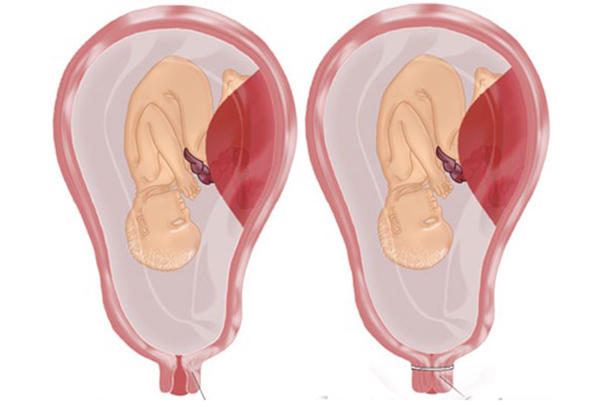 If signs suspicious of a microinvasive process are identified, an atypical conization of the cervix is performed with a cone height of not more than 1.5 cm. During pregnancy, curettage of the cervical canal is not performed due to the high risk of abortion after this manipulation. Cervical conization can be performed at any gestational age, but not less than 4 weeks before. before the expected birth. In stage IA1 (invasion up to 3 mm and horizontal extension up to 7 mm without vascular invasion), conization is the optimal and safe method of treatment. The risk of metastasis is 0.8% for squamous cell carcinoma and 1.5% for adenocarcinoma. If pelvic lymph node involvement is suspected, pelvic lymphadenectomy (PLAE) or sentinel lymph node biopsy is indicated [8].
If signs suspicious of a microinvasive process are identified, an atypical conization of the cervix is performed with a cone height of not more than 1.5 cm. During pregnancy, curettage of the cervical canal is not performed due to the high risk of abortion after this manipulation. Cervical conization can be performed at any gestational age, but not less than 4 weeks before. before the expected birth. In stage IA1 (invasion up to 3 mm and horizontal extension up to 7 mm without vascular invasion), conization is the optimal and safe method of treatment. The risk of metastasis is 0.8% for squamous cell carcinoma and 1.5% for adenocarcinoma. If pelvic lymph node involvement is suspected, pelvic lymphadenectomy (PLAE) or sentinel lymph node biopsy is indicated [8].
Case management up to 22 weeks . gestation with IA2 and IB1 stage and tumor up to 2 cm.
At the first stage, an atypical conization of the cervix with lymphadenectomy is performed.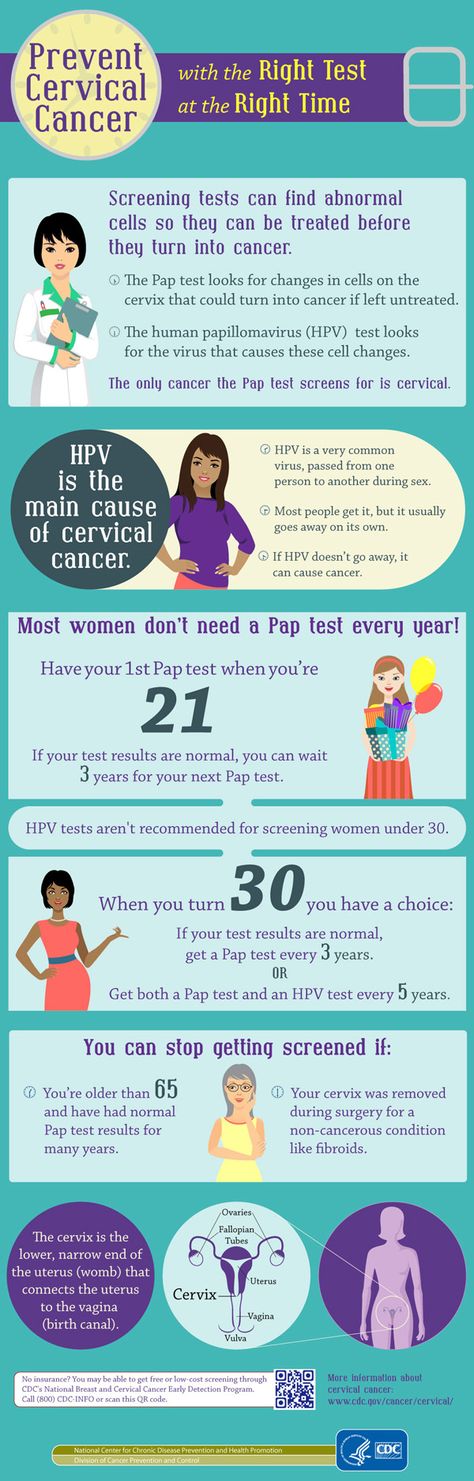 If lymph node metastasis is confirmed, termination of the pregnancy should be considered. In the absence of lymph node involvement, it is possible to prolong pregnancy with standard therapy after delivery (in stage IA2) or neoadjuvant chemotherapy (NAHT) (in stage IB1) with delayed standard treatment after delivery [9] (Fig. 1).
If lymph node metastasis is confirmed, termination of the pregnancy should be considered. In the absence of lymph node involvement, it is possible to prolong pregnancy with standard therapy after delivery (in stage IA2) or neoadjuvant chemotherapy (NAHT) (in stage IB1) with delayed standard treatment after delivery [9] (Fig. 1).
Management of patients over 22 weeks. with IA2 and IB1 stage with a tumor up to 2 cm. At this gestational age, atypical cervical conization is performed to stage the process. Pelvic lymphadenectomy is not performed due to technical limitations related to the size of the uterus. When stage IA2 is confirmed, standard treatment is carried out after delivery; at stage IB1, neoadjuvant polychemotherapy is started [9].
Management of pregnant women up to 22 weeks. with IB1 stage and tumor up to 2–4 cm. TLAE is carried out to clarify the prevalence of the process. If lymph node involvement is confirmed, termination of pregnancy is recommended followed by standard treatment. In case of intact lymph nodes after 12 weeks. start NAC [9].
In case of intact lymph nodes after 12 weeks. start NAC [9].
Pregnant women up to 22 weeks' gestation. with confirmed cervical cancer IB2 and stage IIA , termination of pregnancy is recommended regardless of the involvement of the lymph nodes [9]. After 22 weeks conduct several NACT courses. The last course must be completed no later than 3 weeks. before childbirth [9].
Surgical treatment
Diagnosis of cervical cancer is based on histological examination, but the prognosis of the disease is determined by the size of the tumor and the involvement of the lymph nodes in the pathological process. In the first half of pregnancy (up to 22 weeks), laparoscopic PLAE is a safe and highly informative operation [10]. When metastases are detected, termination of pregnancy and chemoradiotherapy are indicated [11]. Prolongation of pregnancy is acceptable with intact lymph nodes and the onset of NAC [11]. Trachelectomy during pregnancy is not recommended due to low efficiency and high risk of miscarriage (up to 34%) [12].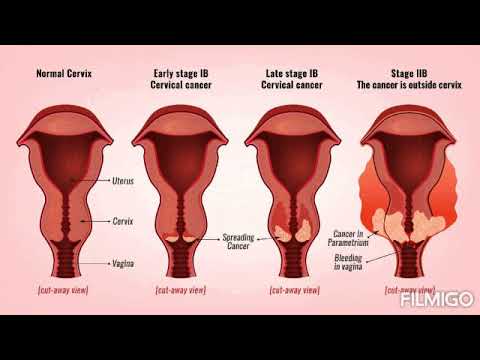
Neoadjuvant chemotherapy
In the case of prolongation of pregnancy in patients with locally advanced cervical cancer, NAC allows to stabilize the tumor process [6]. The calculation of the therapeutic dose and the choice of the drug is identical to those outside of pregnancy. However, it must be taken into account that the physiological changes associated with pregnancy (hemodilution, hypoproteinemia, acceleration of the glomerular filtration rate, the appearance of a third space - the amniotic cavity) affect the pharmacokinetic properties of chemotherapy drugs.
According to international protocols, chemotherapy is not performed in the first trimester of pregnancy due to the high risk of embryotoxic and teratogenic effects. During pregnancy in patients with cervical cancer, chemotherapy can be performed starting from the second trimester: with stage IB1, no metastases in the lymph nodes and tumor size <2 cm; at stage IB1 and tumor size of 2–4 cm, in the absence of metastases to the lymph nodes or when lymphadenectomy is impossible, as well as at stages IB2–IIB - until the period of fetal maturity [4, 12].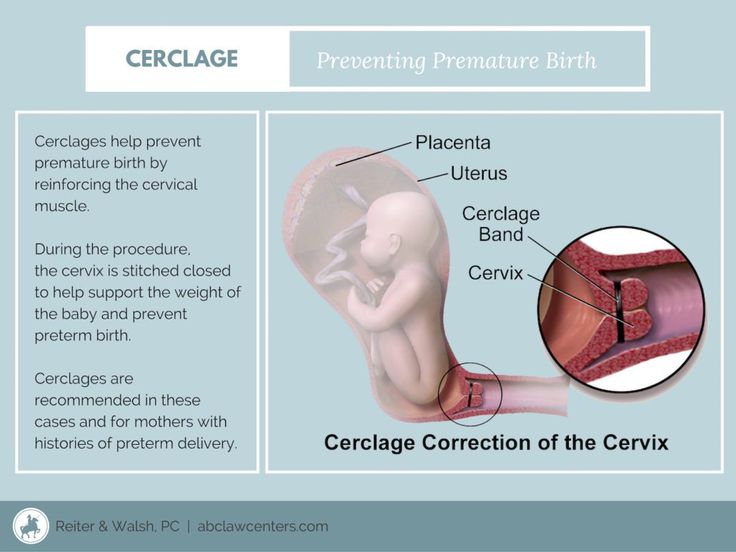
In the vast majority of cases, NAC allows to stabilize the tumor process and prolong pregnancy until the fetus reaches viability and maturity. The most common regimen includes cisplatin (50–100 mg/m 2 ) alone or in combination with paclitaxel (175 mg/m 2 ). Courses are held at intervals of every 3 weeks. [13]. Less common is the combination of cisplatin (75 mg/m 2 ) with ifosfamide 2 g/m 2 cycles every 2 weeks. [12, 14].
Tactics of delivery of pregnant women with cervical cancer
The last course of polychemotherapy should be completed within 3 weeks. before the expected date of birth. This is associated with the risk of giving birth to a child with suppressed bone marrow and a high probability of developing infectious complications in him [14, 15]. Currently, it is recommended to prolong pregnancy at least until full term (37 weeks), in the absence of such an opportunity, at least up to 34 weeks.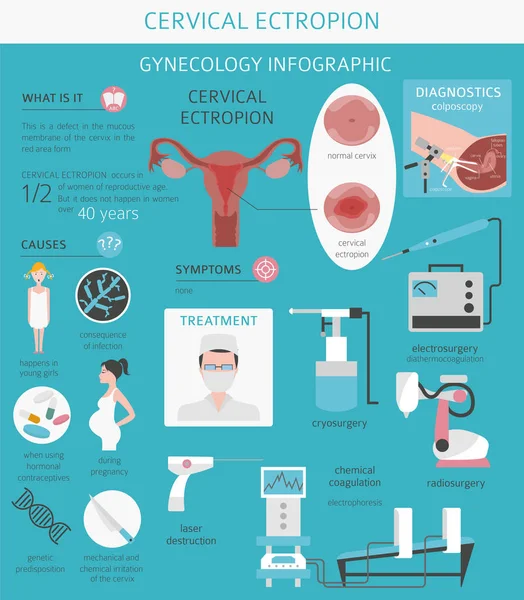 [14–17].
[14–17].
After conization of the cervix, performed at stages IA1–IA2, vaginal delivery is theoretically possible [9]. In the case of advanced cervical cancer, the method of delivery is a corporal caesarean section followed by a Wertheim operation. The choice of delivery method depends on the stage of the disease, taking into account the desire of the patient to maintain fertility [1, 2, 12, 18–20].
Conclusion
The "gold standard" for the treatment of cervical cancer in pregnant women has not yet been developed. It should be recognized that the above ESGO clinical guidelines, unfortunately, cannot answer all questions. For example, from our point of view, an important prognostic factor is the biological characteristics of the neoplasm, which are not taken into account in the recommendations. It is also not clear what the tactics of treatment are at the advanced stages of the process and whether the recommended vaginal delivery is not risky at the IA2 stage of the disease, etc. based on world experience. It is necessary to emphasize the special role of a multidisciplinary approach with the participation of an oncogynecologist, an obstetrician-gynecologist, a neonatologist, chemo- and radiation therapists, a psychologist, and a lawyer in solving a number of important issues.
based on world experience. It is necessary to emphasize the special role of a multidisciplinary approach with the participation of an oncogynecologist, an obstetrician-gynecologist, a neonatologist, chemo- and radiation therapists, a psychologist, and a lawyer in solving a number of important issues.
Information about the authors:
1 Payanidi Yuliya Gennadievna — Doctor of Medical Sciences, Senior Researcher of the Gynecological Department, ORCID iD 0000-0001-5950-4543;
2Borovkova Ekaterina Igorevna – Doctor of Medical Sciences, Professor of the Department of Obstetrics and Gynecology, Faculty of Medicine, ORCID iD 0000-0001-7140-262Х;
2 Dobrokhotova Yuliya Eduardovna — Doctor of Medical Sciences, Professor, Head of the Department of Obstetrics and Gynecology, Faculty of Medicine, ORCID iD 0000-0001-6571-3448;
2 Harutyunyan Anna Meruzhanovna — postgraduate student of the Department of Obstetrics and Gynecology, Faculty of Medicine, ORCID iD 0000-0002-6392-5444.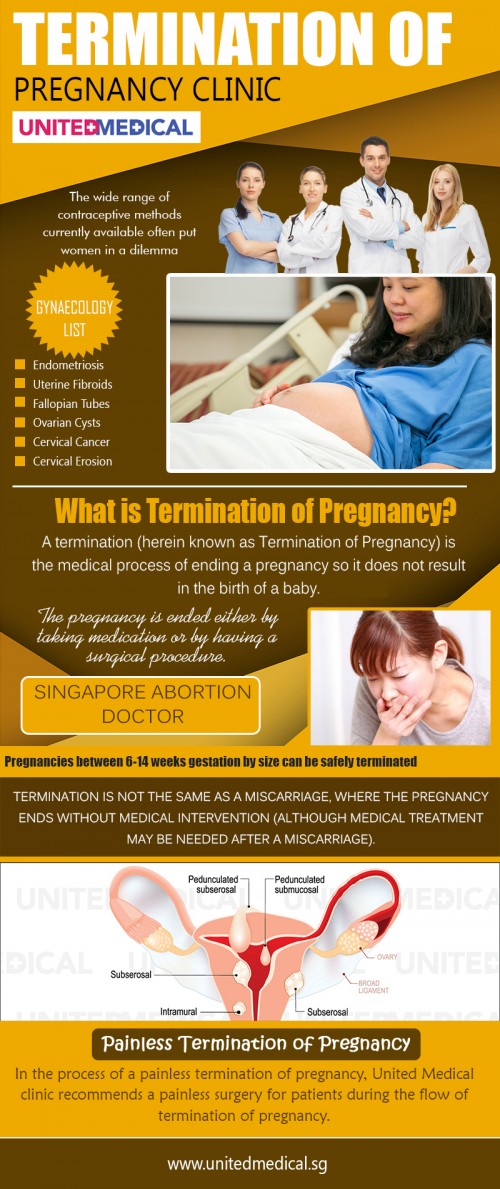
1 N.N. N.N. Blokhin" of the Ministry of Health of Russia. 115478, Russia, Moscow, Kashirskoye shosse, 24.
2 N.I. Pirogov of the Ministry of Health of Russia. 117997, Russia, Moscow, st. Ostrovityanova, 1.
Contact information: Borovkova Ekaterina Igorevna, e-mail: [email protected]. Financial transparency: none of the authors has a financial interest in the presented materials or methods. No conflict of interest . Article received 12/13/2018.
About the authors:
1 Yulia G. Payanidi - MD, PhD, Senior Researcher of the Department of Gynecology, ORCID iD 0000-0001-5950-4543;
2 Ekaterina I. Borovkova — MD, PhD, Professor of the Department of Obstetrics and Gynecology, Medical Faculty, ORCID iD 0000-0001-7140-262Х;
2 Yulia E. Dobrokhotova – MD, PhD, Professor, Head of the Department of Obstetrics and Gynecology, Medical Faculty, ORCID iD 0000-0001-6571-3448;
2 Anna M. Arutunyan — post-graduate student of the Department of Obstetrics and Gynecology, Medical Faculty, ORCID iD 0000-0002-6392-5444.
Arutunyan — post-graduate student of the Department of Obstetrics and Gynecology, Medical Faculty, ORCID iD 0000-0002-6392-5444.
1 Blokhin Cancer Research Center. 24, Kashirskoye shosse, Moscow, 115478, Russian Federation.
2 Pirogov Russian National Research Medical University,
1 Ostrovityanova str., Moscow, 117997, Russian Federation.
Contact information: Ekaterina I. Borovkova, e-mail: [email protected]. Financial Disclosure: no authors have a financial or property interest in any material or method mentioned. There is no conflict of interests. Received 12/13/2018.
National Medical Research Center of Oncology. N.N. Blokhin
“They drove me from everywhere - we don’t treat such people. Everything was twisted at my temple - are you crazy? They came home, knocked on the door with their fists - for an abortion!
Evening. The corridors of the polyclinic of the Cancer Center were empty. In one of the offices on the 3rd floor, two people were bending over the phone - Dr. Korolenkova and Muscovite Natalya Antoshchenko. - This is Sasha skiing in the forest, here he is with his dad, frying kebabs in the country, Sasha helps, and this is in the bath, we love the bath with the whole family, - Natalya flips through the photo with her 5-year-old son. And this scene, rather, resembles a family one, as if mother and grandmother are looking at the pictures - there is so much warmth and lively interest in the eyes of Professor Korolenkova.
In one of the offices on the 3rd floor, two people were bending over the phone - Dr. Korolenkova and Muscovite Natalya Antoshchenko. - This is Sasha skiing in the forest, here he is with his dad, frying kebabs in the country, Sasha helps, and this is in the bath, we love the bath with the whole family, - Natalya flips through the photo with her 5-year-old son. And this scene, rather, resembles a family one, as if mother and grandmother are looking at the pictures - there is so much warmth and lively interest in the eyes of Professor Korolenkova.
This story begins in January 2016. 34-year-old Natalya Antoshchenko, a design engineer by profession, alarmed by the broken cycle, turned to a gynecologist. There I heard the news that she was pregnant. Or rather, two news - on the cervix, according to the doctor, "some spots with a modified structure." She and her husband Arthur already raised an 8-year-old daughter, they did not plan a second child, but they were very happy with the news. Just what are the stains? What Natalya heard in one of the federal oncology centers, where smears were taken for analysis, sounded like a thunderclap - this is the initial stage of cervical cancer and she urgently needs an abortion: “We don’t treat cancer with pregnancy.”
Just what are the stains? What Natalya heard in one of the federal oncology centers, where smears were taken for analysis, sounded like a thunderclap - this is the initial stage of cervical cancer and she urgently needs an abortion: “We don’t treat cancer with pregnancy.”
“I’m back to the antenatal clinic,” says Natalya, “they look at me with wild, round eyes: “Urgently for an abortion, don’t even think about it!”. And I'm already 14 weeks old, the baby will soon move. I sobbed so much that I couldn’t think of anything else, how is it an abortion? Kill the living, little being inside of me? His heart is beating! The husband was also very worried: “If doctors say to have an abortion, then have an abortion, you will die now!” In the antenatal clinic, they were very afraid that the disease would progress and they would have to answer. They didn’t leave me alone, they came home, I didn’t want to open them, they knocked on the door with their fists - for an abortion! You know, it was like being in a horror movie.
“What happiness it was to hear at the Kulakov obstetrics center that the pregnancy can be saved,” continues Natalya Antoshchenko, “I was sent to the Blokhin Cancer Center: “We are ready to observe your pregnancy only if Professor Korolenkova takes you.” I sob again - what if he doesn’t take it? On the first day, I sat under her office from 9 am until the evening and did not get in, so many people came to her. The next day I got it, she examined me: “I can’t give guarantees and forecasts, there is a chance.” There is!
“Desired pregnancy, in cytological smears there are repeatedly severe lesions corresponding to cancer insitu, these are precancerous lesions, stage zero,” comments Professor Lyubov Korolenkova, senior researcher at the Oncocenter’s scientific advisory department, MD. - The situation is not completely clear, because. without conization ( removal of a cone-shaped area of cervical tissue ) we cannot exclude invasion - a real tumor process that has contact with blood and lymph.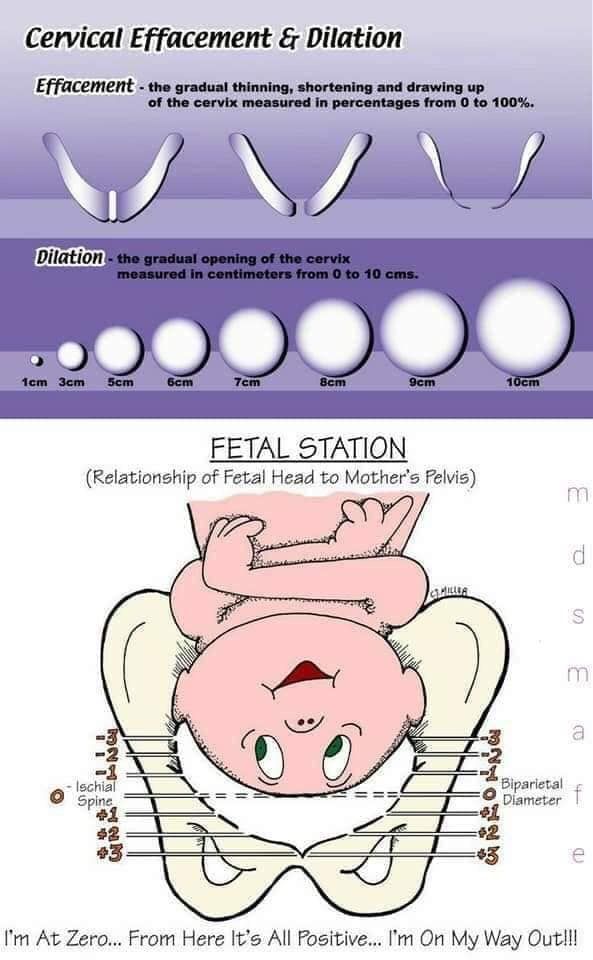
Cutting off a layer of tissue along the entire cone of the cervix in order to understand the extent of the cancerous lesion, with a high degree of probability, can provoke a miscarriage in a pregnant woman. But a multifocal biopsy, which is taken from several areas of the cervix, still needed to be done. - Lyubov Ivanovna asks me: “Do you agree to a biopsy? 50% that there may be a miscarriage, ”says Natalia. - And my first child was premature, I gave birth to a daughter at 6.5 months. I was very worried, I wanted to convey. We pulled with this for two weeks, and then only then she “pinched off” me. Eye-diamond, the most pathological piece "bit off" and passed for analysis. It worked out, Lyubov Ivanovna did it very carefully and unexpectedly, I did not have time to get scared. And then the results of the biopsy came - I have cervical cancer with 3 mm germination. I don't know how I survived it. Every two weeks, neither alive nor dead, she came to see Korolenkova, afraid of bad news. There was an agreement - if she doesn’t like something, then we immediately induce childbirth. And at the same time I went to the Kulakov center - to measure the length of the cervix, whether there is a possibility of contraction, i.e. miscarriage.
There was an agreement - if she doesn’t like something, then we immediately induce childbirth. And at the same time I went to the Kulakov center - to measure the length of the cervix, whether there is a possibility of contraction, i.e. miscarriage.
– Despite the presence of invasion, i.e. germination in the tissue, ultrasound data did not show such a volume of the tumor that would be accessible to ultrasound for visualization, says Dr. Korolenkova. – The patient was observed with a slight negative dynamics due to the growth of the tumor epithelium against the background of the action of pregnancy hormones, which stimulate cell reproduction. Those. they provide not only the growth of the fetus, but the growth of the existing tumor. Fortunately, the invasive component of the tumor that went into the extended biopsy did not have time to reproduce itself. There was no negative dynamics in this part of the cervix. Such a favorable scenario is not for everyone.
“My first ultrasound during pregnancy was an ultrasound here in Blokhin,” Natalya recalls. - So from the oncologist at 16 weeks I learned that I had a boy. And at 36 weeks, the water broke at home, on August 2, 2016, in the center of Kulakov, I was “caesarean”. The child was born perfectly healthy, with a weight of 3400. I was afraid that he would not sleep, because the whole pregnancy shook in lines under the doors of hospital rooms and sobbed. But he was the perfect baby - he ate and slept. My husband, however, barely survived during my pregnancy. He went with me everywhere, holding my hand. First, I lost weight on nervous grounds, then, on the contrary, I ate because I was nervous and recovered greatly.
- So from the oncologist at 16 weeks I learned that I had a boy. And at 36 weeks, the water broke at home, on August 2, 2016, in the center of Kulakov, I was “caesarean”. The child was born perfectly healthy, with a weight of 3400. I was afraid that he would not sleep, because the whole pregnancy shook in lines under the doors of hospital rooms and sobbed. But he was the perfect baby - he ate and slept. My husband, however, barely survived during my pregnancy. He went with me everywhere, holding my hand. First, I lost weight on nervous grounds, then, on the contrary, I ate because I was nervous and recovered greatly.
- Sasha is growing up very independent - he knows how to occupy himself, he plays himself, he looks at pictures in books, - his mother rejoices. - Reads at the age of 5 already as a schoolboy. This child saved my life. I would not have known that I had cancer for a very long time. Nothing bothered me, the cycle was like clockwork and nothing hurt. And here's what, Lyubov Ivanovna told me - women who got scared and had an abortion have a 50% higher risk of relapse, after 2-3 years the disease returns!
“After childbirth, the patient had residual lesions of the cervix,” summarizes Professor Korolenkova, “because the effect of proteomes was removed ( specific proteins in a pregnant woman) and the hormonal effect of pregnancy on the tumor epithelium, it was already deprived of its proliferative activity, which was fed by pregnancy hormones ( proliferative activity, this is an indicator for determining the phenotype of a neoplasm, which determines the rate of tumor growth, the risk of metastasis and the response to therapy). After HPV conization ( human papillomavirus causing cervical cancer ) became negative, according to cytology, the resection margins were "clean" and the patient has been observed without progression for more than five years.
After HPV conization ( human papillomavirus causing cervical cancer ) became negative, according to cytology, the resection margins were "clean" and the patient has been observed without progression for more than five years.
By the way, according to Lyubov Korolenkova, in 93% of patients with insitu and microinvasive cancer, if, according to the results of a histological examination of the removed material, there are no cancer cells at the edges of the resection, after conization, the HPV test becomes negative and this is an indicator of the radicalness of the performed excision, i.e. excision. Chemotherapy treatment is not required. According to international recommendations, if an invasion, i.e. the germination does not exceed 3 mm and the resection margins are "clean" after conization, we can talk about the patient's cure. Natalia Antoshchenko has an excellent prognosis. For five years, she had twice a year an MRI with contrast, a comprehensive ultrasound examination, a colposcopy, an HPV test, and it remains negative. Now, after a 5-year period, it is enough to conduct control studies once a year.
Now, after a 5-year period, it is enough to conduct control studies once a year.
- Everything is over, I'm healthy, - Natalya Antoshchenko smiles. - Three years ago, I suddenly became interested in sports shooting with my husband. The whole family travels a lot around the country, we often go to the Volga, to Astrakhan. We have our own boat. We ride it along the Oka, the cottage is there, in the Tula region. We take it with us on trips, it is like a trolley - we attached it to the car and drove off. Lyubov Ivanovna says - if you want to give birth, give birth. The arches of the cervix remained, if it is necessary to endure the pregnancy, the stitches are applied and there are no big problems. Well, frankly, as long as there are no such plans, the four of us are fine.
Professor Korolenkova began her great research work in 2008. “I studied the natural course of cervical carcinogenesis,” she says, “and it was clear that insitu cancer exists before the appearance of significant invasion – 8, 10 or more years. And the period of pregnancy against the background of the tumor process of the initial stage is not life-threatening. You can report pregnancy and during this time there is no rapid progression, and with insitu cancer, the transition to invasion also happens quite rarely. If it happens, then microinvasive cancer is treated well, including conization, if up to 3 mm of invasion without histologists detecting tumor cells in the vessels.
And the period of pregnancy against the background of the tumor process of the initial stage is not life-threatening. You can report pregnancy and during this time there is no rapid progression, and with insitu cancer, the transition to invasion also happens quite rarely. If it happens, then microinvasive cancer is treated well, including conization, if up to 3 mm of invasion without histologists detecting tumor cells in the vessels.
“I have given birth to 388 children from patients with pre-invasive and micro-invasive cancer,” Professor Korolenkova declares not without pride, showing the babies in her office in the photo. – Every 4th patient has microinvasive cervical cancer. There was also the experience of managing more than 31 patients with invasive cancer in combination with pregnancy, this happens much less often. Because against the background of a significant amount of the tumor process and the greater prevalence of the process, fertility is extremely reduced due to ovulation disorders. This was our first experience in the whole country, we performed neoadjuvant (preoperative) chemotherapy in the context of prolongation of pregnancy and then women gave birth by caesarean section. If a woman was operable, our specialists performed a simultaneous operation on her, when, after a caesarean section, the uterus is removed along with the cervix and regional lymph nodes. Three patients later switched to radiation therapy, and out of these 31 patients, three women with a widespread process died. The rest, despite the fact that 4 of them were with stage III disease, still live without progression.
This was our first experience in the whole country, we performed neoadjuvant (preoperative) chemotherapy in the context of prolongation of pregnancy and then women gave birth by caesarean section. If a woman was operable, our specialists performed a simultaneous operation on her, when, after a caesarean section, the uterus is removed along with the cervix and regional lymph nodes. Three patients later switched to radiation therapy, and out of these 31 patients, three women with a widespread process died. The rest, despite the fact that 4 of them were with stage III disease, still live without progression.
What needs to be done so that women with cervical cancer can endure desired pregnancies and give birth to babies? According to Professor Korolenkova, it is necessary to have domestic Russian clinical guidelines that will allow doctors to offer such patients pregnancy. Now Lyubov Ivanovna, on the basis of her huge database of registered cases of cervical cancer in pregnant women, is preparing an atlas for the education of doctors for publication. You need to create a learning module.
You need to create a learning module.
“A doctor must observe a woman with cervical cancer with mandatory video recording,” insists Dr. Koroenkova. “But so far, it’s nowhere to be found. Colposcopically they do not monitor patients, this is an absolute violation of existing norms and rules. Each patient visit must be video recorded. There should be a colposcopic picture of the patient, cytological control and ultrasound control, which will show that there is no hidden tumor. This monitoring needs to be streamlined with the help of clinical guidelines, relevant atlases and training of local doctors. If the atlas is issued centrally, then it will be possible to train a certain number of colposcopists. Abroad, such patients are observed, their pregnancy is not interrupted, women bear healthy children without risk to their health. But they should be observed by a specialist who has experience with such patients during pregnancy. We have a long way to go, - Lyubov Korolenkova is sure.