Do babies with spina bifida kick in the womb
New fetal surgery for spina bifida may be safer for baby and mom
Exclusive
By Usha Lee McFarling May 28, 2019
Reprints
Gilda and Arnuf Giron with their newborn daughter, Abigail. Kendrick Brinson for STATLOS ANGELES — Gilda Giron was 13 weeks pregnant and barely showing when she started to worry. Something wasn’t right with her ultrasound image. At 16 weeks, Gilda and her husband, Arnuf, received the devastating news: Their baby had myelomeningocele, the most severe form of spina bifida. Her tiny spinal cord was open, exposed and leaking fluid. The birth defect meant she had nerve damage that could cause paralysis and an inability to control her bladder or bowels. She faced spending life with a shunt implanted in her brain.
Many parents who receive a diagnosis of spina bifida early in pregnancy choose to terminate. But Arnuf and Gilda, who works with disabled people, were determined to keep their baby. They turned to the next option: surgery in the womb to repair the defect.
The fetal surgery for spina bifida is complex. Because it requires cutting through the mother’s abdomen and uterus, like a C-section, it involves a long recovery, something that would have been difficult for Gilda, who has two other young children. The “open surgery” carries some risk of premature birth and complications during birth. It also means having a cesarean, for this and any future births because of the risk of uterine rupture.
advertisement
In their extensive research, the couple found a few hospitals — Texas Children’s and Johns Hopkins among them — offered a new, less-invasive surgery that opened the mother’s abdomen but required only tiny incisions to the uterus; the delicate surgery on the fetus was done with specialized instruments placed through the holes. But the Girons’ insurance would only pay for the conventional procedure, which involved traveling to San Francisco from their home in the Los Angeles suburb of Whittier.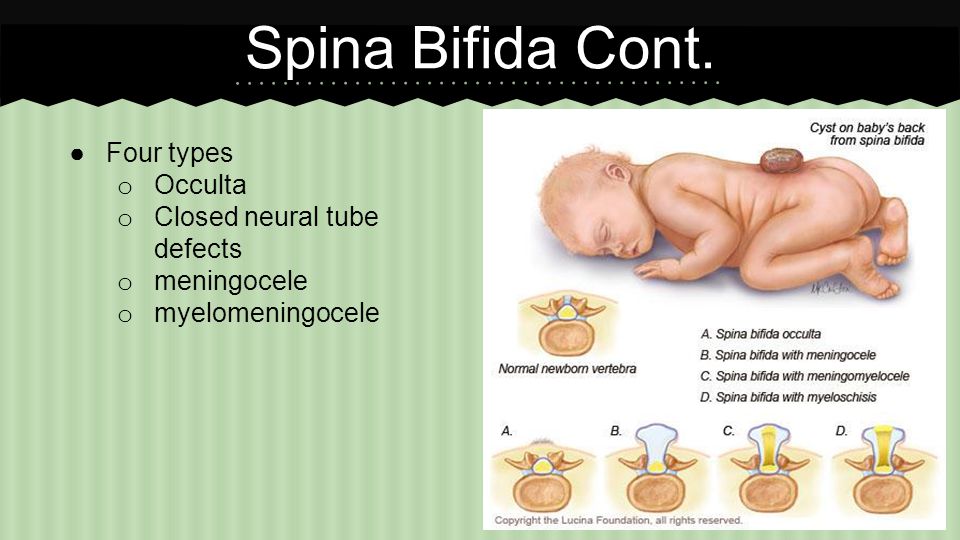
Gilda, 35, was frantic. Because the operation is ideally done about 25 weeks into pregnancy, the Girons had just a few weeks to decide what to do and figure out if they’d need to move their family out of state and burn through their savings to pay for the newer surgery. Then one day, out of the blue, their obstetrician offered an alternative. A pilot study for a new kind of fetal surgery for spina bifida — one that would be much easier on Gilda — had just been launched, and the procedure would be covered by their insurance. Better still, the study was occurring right in town, at the University of Southern California and Children’s Hospital Los Angeles.
advertisement
Gilda and Arnuf, 34, immediately went to meet the lead surgeon, Dr. Ramen Chmait, a veteran fetal surgeon who directs the Los Angeles Fetal Surgery program.
“I went into the meeting saying, ‘I want to do this, I just don’t want to be the first one,’” Gilda said. “He said, ‘Well, you are the first one. ’”
’”
Gilda underwent the experimental operation this past February, and she and the surgeons talked about it for the first time last week with STAT — a week after their baby, Abigail, was born.
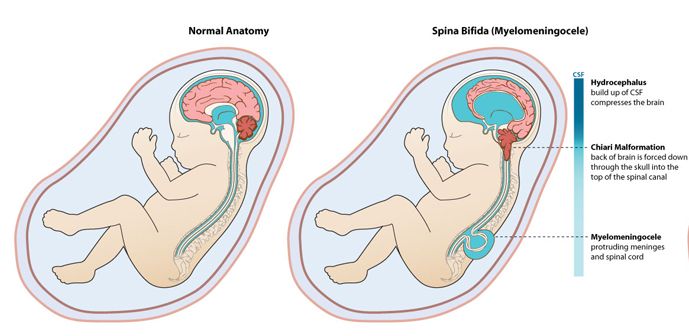
From left, neurosurgeon Dr. Jason Chu, fetal surgeon Dr. Ramen Chmait, and USC Keck OB-GYN Dr. Andrew Chon perform the fetal surgery at Huntington Hospital on Feb. 19. Courtesy Ramen ChmaitFor decades, the standard treatment for babies with spina bifida was to operate on them after birth to patch the opening of their spinal cords. But a lot of damage can occur in the womb: There can be too much or too little cerebrospinal fluid around the brain, the brain can move out of place, and exposed nerves can get damaged. Most babies with spina bifida who are operated on after birth require lifelong shunts to control brain swelling and have problems walking and controlling their bladder and bowels. This wasn’t what Gilda and Arnuf wanted for their baby girl.
Doctors had long thought they could do better.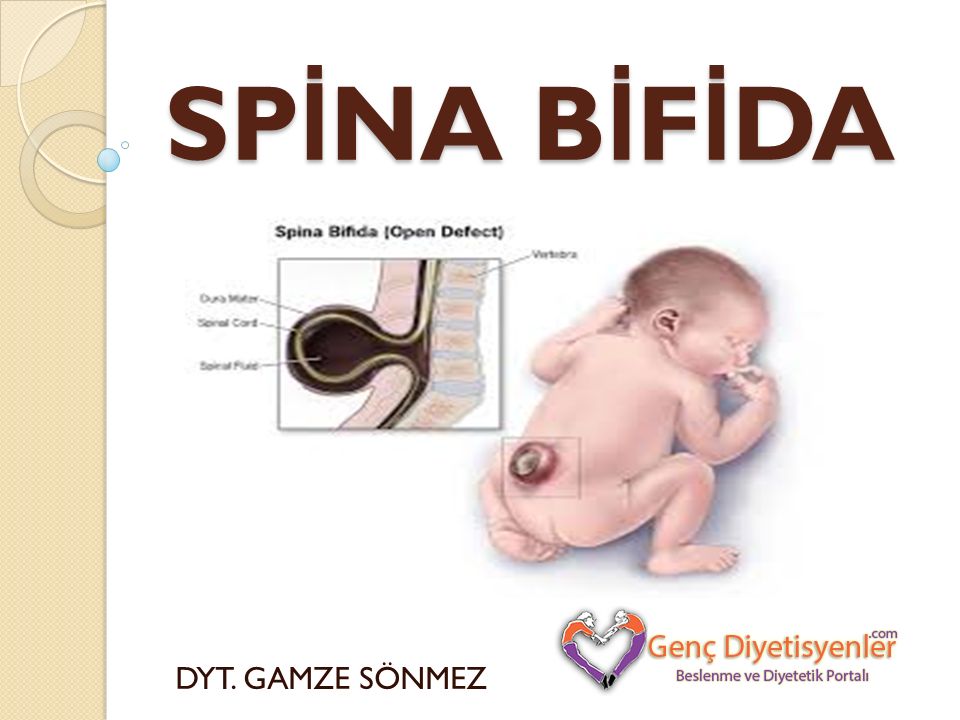 In 2002, a trio of U.S. hospitals started a randomized clinical trial, known as the MOMS trial, to see if babies with spina bifida fared better if they were operated on in the womb. They set out to treat 200 fetuses but stopped the trial early because the results were so conclusive that fetal surgery was better: Babies operated on in utero were less likely to require shunts and more likely to be able to walk without crutches or braces.
In 2002, a trio of U.S. hospitals started a randomized clinical trial, known as the MOMS trial, to see if babies with spina bifida fared better if they were operated on in the womb. They set out to treat 200 fetuses but stopped the trial early because the results were so conclusive that fetal surgery was better: Babies operated on in utero were less likely to require shunts and more likely to be able to walk without crutches or braces.
After the landmark results were published in 2011, fetal surgery for spina bifida became the standard of care. It’s a procedure now offered at about a dozen medical centers around the U.S, but it increases both maternal risk and the risk of premature birth. As a result, some parents still choose to wait until after birth to operate.
In 2014, surgeons at Texas Children’s Hospital started performing a spina bifida repair surgery in which the mother’s abdomen is opened, but the uterus remains intact. The uterus is pulled out of the abdomen and puffed full of carbon dioxide. Endoscopic surgical tools called trocars and a tiny camera are then inserted into the uterus through small holes.
Endoscopic surgical tools called trocars and a tiny camera are then inserted into the uterus through small holes.
After doing some 50 of these “fetoscopic” procedures, Dr. Michael Belfort, the surgeon who pioneered this approach, said he believes it is equivalent to the open surgery in terms of helping the fetus, although more long-term data are needed, and said the obstetric benefits are “immense.” But it still means the mother must withstand a major surgical incision to her abdomen. Chmait wanted to go one step further. He didn’t want to slice open the abdomen at all.
Chmait is the director of the Los Angeles Fetal Surgery program at Children’s Hospital Los Angeles and an associate professor at Keck Medicine of USC. University of Southern CaliforniaChmait has done thousands of fetal surgeries. He’s treated fetuses with broken heart valves, lung tumors, blocked bladders, and teratomas growing on their tailbones. He’s used lasers to carefully tease out the abnormal blood vessels that sprout when identical twins share a placenta. Even the most delicate of these procedures require only minimally invasive, endoscopic surgery. It’s long bothered him that a spina bifida repair is the only fetal surgery that still required opening the abdomen. “We always thought this should be next in line,” he said.
Even the most delicate of these procedures require only minimally invasive, endoscopic surgery. It’s long bothered him that a spina bifida repair is the only fetal surgery that still required opening the abdomen. “We always thought this should be next in line,” he said.
About a decade ago, Chmait heard about a pioneering Brazilian scientist and surgeon, Dr. Denise Lapa, who had spent years developing a way to repair spina bifida in the womb without making large incisions in the uterus or the abdomen. (Brazil, where abortion is illegal and malnutrition is more common, has a high rate of spina bifida.) Lapa has done nearly 100 of the surgeries and, according to Chmait, helped with the first one performed in the United States, at New York-Presbyterian Hospital last year; it was not publicized.
For years, Chmait has traveled to Brazil to observe and learn the technique, in which the uterus and fetus remain inside the body during the procedure. He practiced on a setup invented at Texas Children’s: a baby doll covered in chicken skin and inserted into a rubber ball. After spending years getting approval from the Food and Drug Administration as well as the four institutions involved in the study — Children’s Hospital LA, Keck Medicine of USC, Huntington Hospital in Pasadena, and Wellington Regional Medical Center in Florida — Chmait was ready to proceed.
After spending years getting approval from the Food and Drug Administration as well as the four institutions involved in the study — Children’s Hospital LA, Keck Medicine of USC, Huntington Hospital in Pasadena, and Wellington Regional Medical Center in Florida — Chmait was ready to proceed.
There were still uncertainties. The baby’s spinal cord lesion had to be imaged to make sure she qualified for surgery. Ultrasounds showed she didn’t have enough fluid to cushion her brain. “Those five weeks felt like a long time,” Gilda said.
On Feb. 19, the surgery was done at Huntington Hospital. Lapa flew in to observe, support, and cheerlead, an addition to the operating room that thrilled the nervous mother.
It’s a long surgery — it takes a full hour just to insert the trocars, remove amniotic fluid, and inflate the uterus, Chmait said. The procedure went smoothly. Assisted by pediatric neurosurgeon Dr. Jason Chu from Children’s Hospital LA, Chmait dissected out the spinal cord and nerves that were exposed. As he operated, he could see the cerebrospinal fluid leaking out in large drops. Chmait and Chu gently placed the spinal cord back in position and covered the opening in the baby’s back with a collagen patch. Chmait then sewed the baby’s skin over the patch and replaced the amniotic fluid that had been withdrawn.
As he operated, he could see the cerebrospinal fluid leaking out in large drops. Chmait and Chu gently placed the spinal cord back in position and covered the opening in the baby’s back with a collagen patch. Chmait then sewed the baby’s skin over the patch and replaced the amniotic fluid that had been withdrawn.
Throughout the six-hour procedure, Arnuf waited anxiously outside. As soon as the operating team came out, he knew it had gone well. “It was like an ’80s flick where the basketball team wins the championship,” he said. “There were high-fives all around. They didn’t even have to say a word.”
While the surgery was successful, the Girons remained nervous, because premature delivery was still a risk. They celebrated every week that passed. While they were hoping for a vaginal birth, Gilda was scheduled for a cesarean at 39 weeks. As the due date approached, the baby was both breech and facing the wrong direction, meaning Gilda would require not only a C-section, but the more onerous vertical cesarean.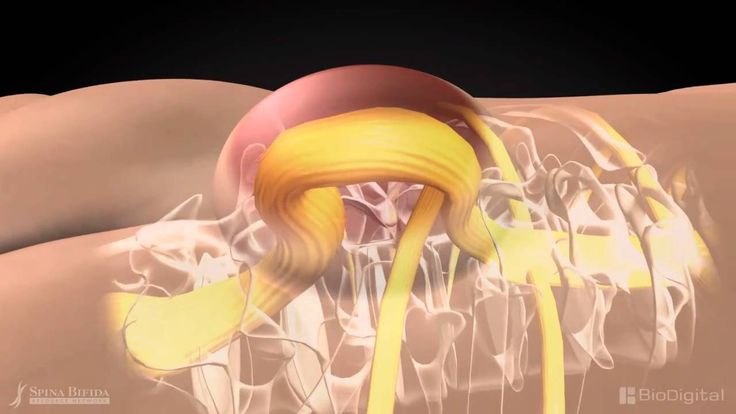
At her 37-week check up, though, the baby had moved into a more ideal position. The physicians decided there was no reason to wait. They induced labor.
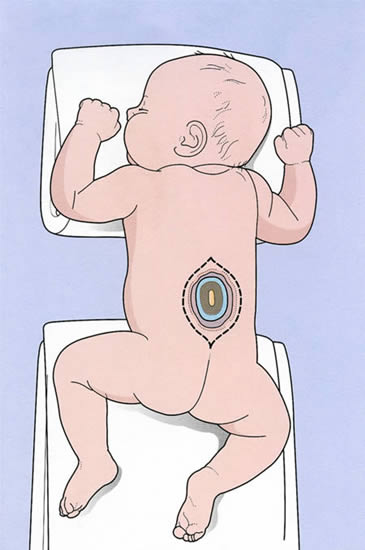
Gilda Giron feeds Abigail at Children’s Hospital Los Angeles. Kendrick Brinson for STATAbigail Coraline Giron was born at 9:22 a.m. on May 16 without the need for a C-section. She weighed 5.5 pounds, with a head covered with silky dark brown hair. The patch over her spinal cord was intact. No cerebrospinal fluid was leaking out. Her hips were in the correct position. But she had a frighteningly large wound on her back, and it wasn’t yet clear whether her brain was swelling. “We were a crazy mix of happiness and fear,” said Gilda.
“Every birth is a great experience,” she added. “But this was really, really emotional.”
Just a few hours after birth, Abigail was taken by ambulance across the street to the newborn and infant critical care unit at Children’s Hospital LA while Gilda waited an agonizing day to be discharged to join her.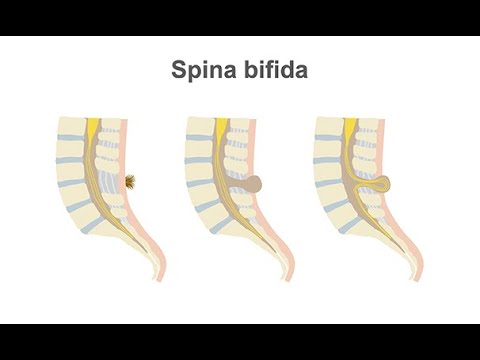
When he first saw Abigail, Dr. Philippe Friedlich, director of the hospital’s fetal and neonatal institute, could barely believe his eyes. In 24 years at the hospital, Friedlich has cared for many babies with spina bifida who have corrective surgery after birth. “Most of the babies stay with us for a while. They have surgery, anesthesia, get catheters. They’re intubated and extubated and in and out of intensive care,” he said. “We didn’t have to do any of that with Abigail. This is life-changing for me.”
Will this new surgery soon become the standard treatment for spina bifida? Chmait feels certain it will. The team is planning the third surgery Tuesday and plans to do a total of 10 in the pilot study and then hopefully expand into a larger clinical trial. They will gather preliminary results on both mothers and babies over the next two years. Chu, the pediatric neurosurgeon, trained at Texas Children’s where he observed their procedure and has also done postnatal spina bifida repairs.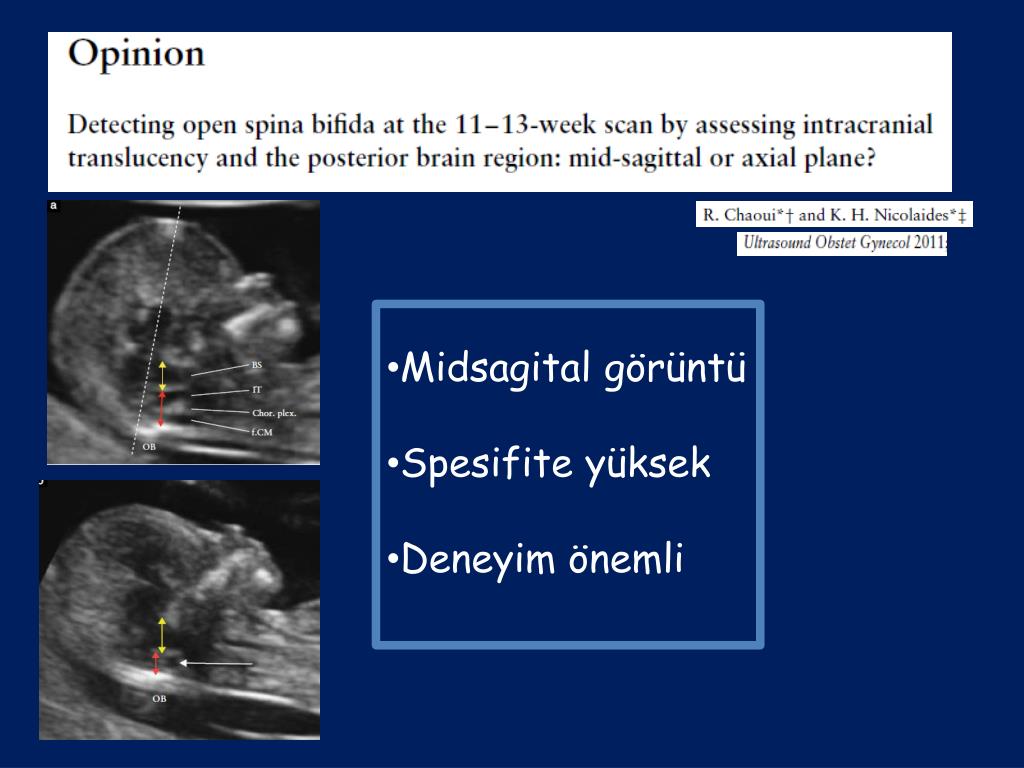 While this approach is still new, he’s optimistic based on what he’s seen.
While this approach is still new, he’s optimistic based on what he’s seen.
Dr. Nalin Gupta was the surgical lead for the MOMS study at UCSF Benioff Children’s Hospital, which pioneered fetal surgery and where the open procedure is still used. He’s encouraged to hear about the work in Los Angeles because it could limit risk to both mother and fetus. “Any procedure where maternal risk is lower is definitely valuable,” he said. But Gupta isn’t planning on changing his procedure until he sees more data on whether the babies fare as well after the minimally invasive surgery. He’s not yet convinced that endoscopic surgery allows for as much intricate anatomical work on the spinal cord and nerves as open surgery.
As she grows, Abigail will help provide those answers. As part of the study, her health and development will be followed closely for five years. Early indications look very good. There turned out to be no brain swelling at birth that required placement of a shunt.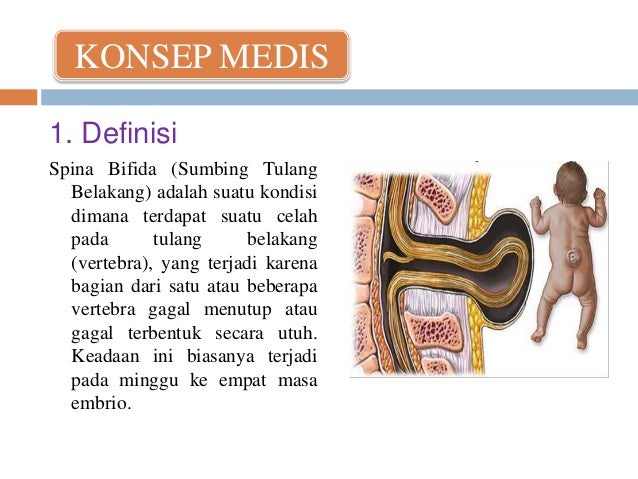 So far, she does not require a catheter to urinate.
So far, she does not require a catheter to urinate.
When Dr. Alex Van Speybroeck, who directs the spina bifida program at Children’s Hospital LA, checked on Abigail a week after she was born, he pulled away her blanket and went directly for the area he was most concerned about — her feet. He was excited to see her moving them back and forth, like she was pushing a little gas pedal. “She’s wiggling her toes so much and she’s ticklish,” he said as he examined Abigail. “That’s great.”
Van Spaybroek will be monitoring the wound on her back, which is still healing, and the baby’s bladder function. The surgical repair of spina bifida can limit further harm caused by the defect but is not a cure for all damage that may have occurred early in fetal development. While it’s possible Abigail may need a brace, Van Spaybroek is optimistic she will be able to walk on her own.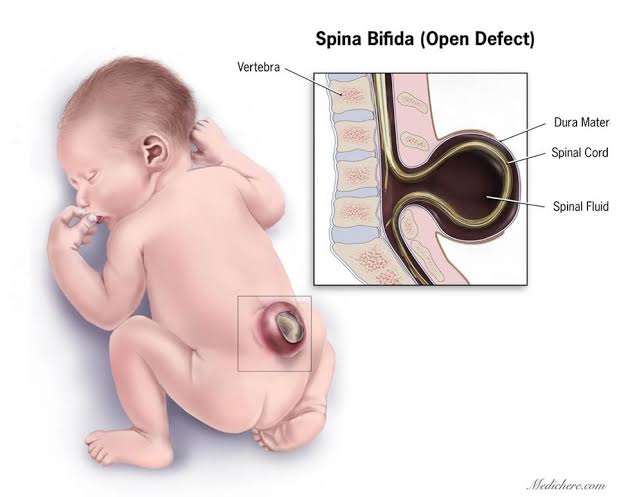
“Abby is going to go home with no operative intervention at all, and is going home in about a week,” he said. “I have never seen that in my career.”
Abigail is expected to go home Tuesday or Wednesday. She was so healthy that she probably could have left the hospital in a few days, but she has stayed nearly two weeks so doctors could run tests needed for the study. After all, she is the first.
About the Author Reprints
Spina Bifida (for Parents) - Nemours KidsHealth
What Is Spina Bifida?
Spina bifida (SPY-nuh BIF-ih-duh) is when a baby's backbone (spine) does not form normally before birth.
The condition can be mild or severe. Treatments can help babies born with spina bifida.
What Are the Types of Spina Bifida?
All types of spina bifida cause an opening in the spine's bones:
- Spina bifida occulta: This is a gap in the bones in the spine but the spinal cord and meninges do not push through it.
 They are in their normal place inside the spinal canal, and there's no opening on the baby's back.
They are in their normal place inside the spinal canal, and there's no opening on the baby's back. - Meningocele: This is when a sac that contains spinal fluid pushes through the gap in the spine. The spinal cord is in its normal place in the spinal canal. The skin over the meningocele often is open.
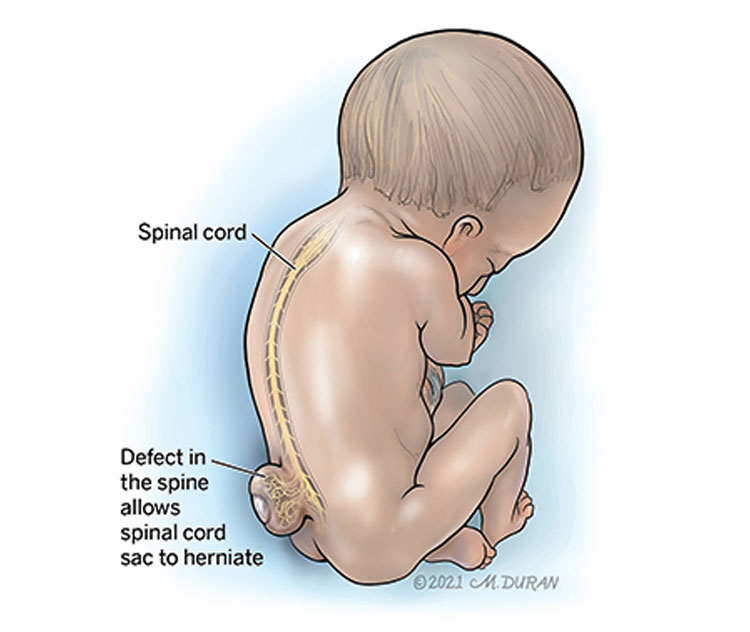
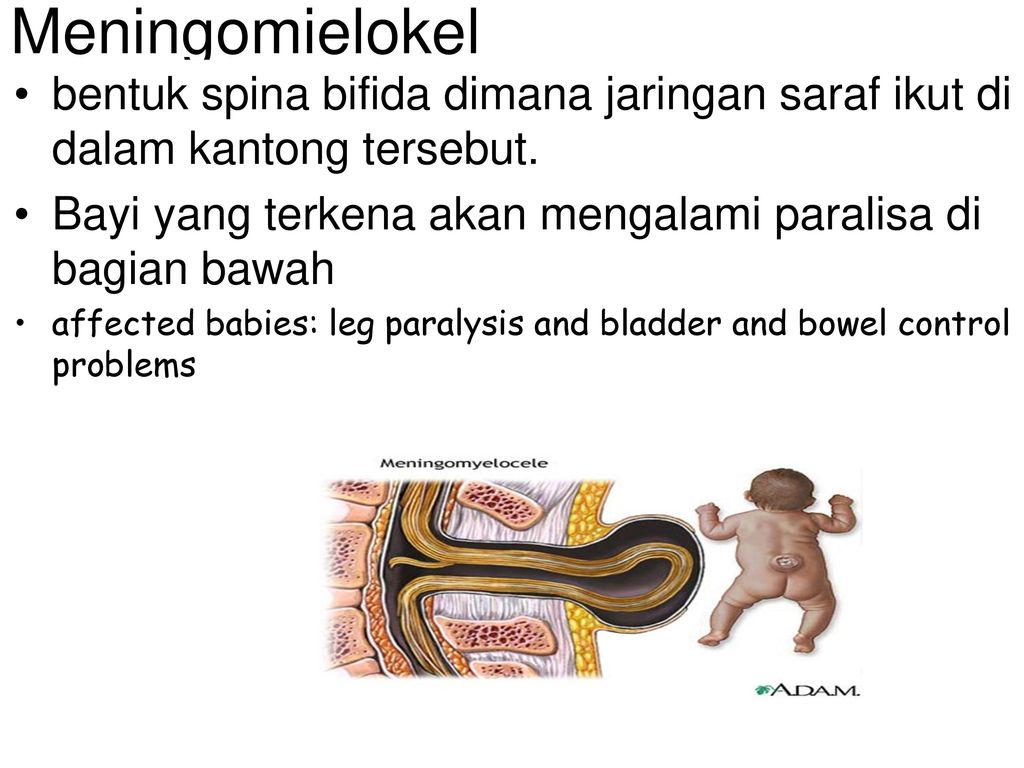
- Myelomeningocele: This is when a sac that contains the meninges, spinal fluid, and part of the spinal cord pushes through the gap in the spine and the skin. You can see it on the baby's back.
What Are the Signs & Symptoms of Spina Bifida?
Symptoms depend on what kind of spina bifida a baby has and where it is on the spine. Some babies with spina bifida have few or no problems. But sometimes the condition can cause serious problems, including weakness, loss of bladder control, or paralysis.
What Causes Spina Bifida?
All types of spina bifida happen in the first month of pregnancy. At first, a fetus' spinal cord is flat. It then closes into a tube called a neural tube. If this tube does not fully close, the baby is born with spina bifida.
If this tube does not fully close, the baby is born with spina bifida.
It’s not clear why some babies get spina bifida. The condition can happen if the mother doesn’t get enough of the vitamin folic acid early in their pregnancy, or:
- took some types of seizure medicines during pregnancy
- already has had a baby with spina bifida
- has diabetes
How Is Spina Bifida Diagnosed?
During pregnancy, a blood test called alpha-fetoprotein (AFP) can tell if a woman has a higher risk of having a baby with spina bifida. A prenatal ultrasound or fetal MRI can show whether a baby has it.
If it's not diagnosed during pregnancy, sometimes the condition is seen right away when the baby is born.
Spina bifida occulta, though, usually doesn't cause symptoms. Often, it's found when doctors do an X-ray or other imaging study of the spine for another reason. Sometimes doctors find spina bifida by doing an ultrasound after they notice a dimple, patch of hair, or red patch at the base of a baby's spine.
How Is Spina Bifida Treated?
Treatment for spina bifida depends on how severe it is. Many babies with spina bifida occulta do not need any treatment.
Babies with meningocele or myelomeningocele will need care from a team that can include a neurosurgeon, urologist, orthopedic surgeon, physical therapist, occupational therapist, and social worker.
Sometimes, doctors can treat spina bifida with surgery while the baby is still in the womb.
How Can Parents Help?
A child whose spina bifida is severe may need medical care for life. This can feel overwhelming for any family. But you're not alone, and many resources are available to help you and your family. Talk to anyone on the care team about ways to find support. You also can find more information online at:
- Spina Bifida Association
- Spina Bifida Resource Network
Reviewed by: Amy W. Anzilotti, MD
Date reviewed: January 2022
Operate before birth - Such cases
- Medical assistance
- Context
- Reporting
- 24.
 08.2016
08.2016
Many pregnant women do not know why the doctor prescribes folic acid to all of them. A defect in the formation of the neural tube of the fetus, spina bifida, myelomeningocele, herniated spinal cord - every year in Russia, one and a half to two thousand children are born with this disease. Everyone has problems with the bladder, one in two cannot feel their legs, one in five is paralyzed and has a huge head. Very often, children with spina bifida are abandoned by their parents. And yes, spina bifida can be successfully treated.
children with Chiari syndrome experience constant headache, the skull bursts from the inside, the head becomes so huge that there is no strength to tear it off the pillow. The three largest clinics - the Philadelphia Children's Hospital, Vanderbilt University and the University of California at San Francisco - divided patients with a diagnosis of "fetal neural tube defect" into two groups of 100 people. The first group underwent intrauterine operations, the second group - postnatal (that is, after birth). It turned out that if a child with spina bifida is operated postnatally, then in 9In 8% of cases, the child dies or needs a shunt to the head. In the case of a fetal (that is, intrauterine) operation, mortality or the need for a shunt to the head is reduced to 68%. In other words, if a child with spina bifida and Chiari syndrome is operated postnatally, then the child will almost certainly be severely disabled. And if you operate in utero, there is a 32% chance to save your head and avoid paralysis.
The first group underwent intrauterine operations, the second group - postnatal (that is, after birth). It turned out that if a child with spina bifida is operated postnatally, then in 9In 8% of cases, the child dies or needs a shunt to the head. In the case of a fetal (that is, intrauterine) operation, mortality or the need for a shunt to the head is reduced to 68%. In other words, if a child with spina bifida and Chiari syndrome is operated postnatally, then the child will almost certainly be severely disabled. And if you operate in utero, there is a 32% chance to save your head and avoid paralysis.
Spina bifida Illustration: Centers for Disease Control and Prevention; Aksana Zinchenko
In addition, the development of motor functions in infants undergoing intrauterine surgery is assessed significantly higher on the Bailey scale than in infants operated after birth.
On December 7, 2010, the independent committee that oversaw MOMS recommended that the study be stopped because intrauterine surgery appears to be more effective than postnatal surgery. By the time MOMS was stopped, 158 of the 200 patients who were supposed to be included in the study had been operated on.
By the time MOMS was stopped, 158 of the 200 patients who were supposed to be included in the study had been operated on.
This is not a panacea, not a miracle cure. Intrauterine operations are not shown to everyone. There are contraindications. There are additional risks of uterine rupture or placental abruption for a woman. But intrauterine surgery is a thirty percent chance for an unborn child to avoid disability, and for those who cannot avoid disability, this is a chance to reduce the degree of pathological changes.
The most blood-supplying organ
To perform an intrauterine operation, two anesthesias are used at once - general and epidural. Under general anesthesia, in fact, they operate. Epidural anesthesia will be switched on when the operation is completed, so that the uterus of the awakened patient does not contract too much from postoperative pain, and the fetus does not die from pain.
This is a very delicate operation. At the 24th week of pregnancy, the fetus is the size of a newborn kitten, and the hernia on its back is no larger than a pea.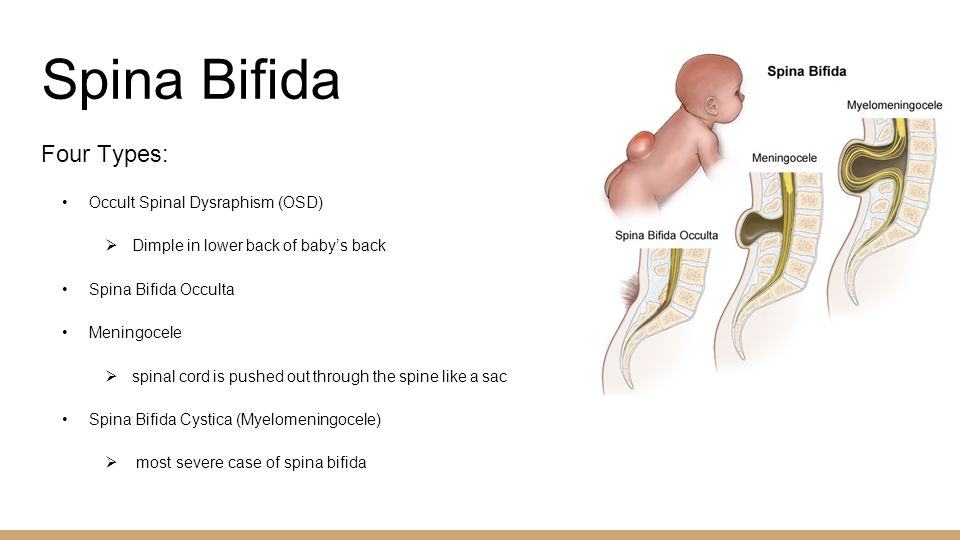 The skin is cut, the cerebrospinal fluid flows out of it, and at this moment, with the naked eye, you can see how the spinal cord is drawn into the spine. And the ultrasound shows how the occipital regions of the brain are released and returned to their place inside the skull. Professor Moily still tried to show me how the roots of the spinal cord are laid out in places, but it seems that a person without special education is not able to see this.
The skin is cut, the cerebrospinal fluid flows out of it, and at this moment, with the naked eye, you can see how the spinal cord is drawn into the spine. And the ultrasound shows how the occipital regions of the brain are released and returned to their place inside the skull. Professor Moily still tried to show me how the roots of the spinal cord are laid out in places, but it seems that a person without special education is not able to see this.
AT THE 24TH WEEKS OF PREGNANCY THE FETUS IS THE SIZE OF A NEWBORN KITTEN, AND THE HERNIA ON ITS BACK IS NO MORE THAN A PEA
The first person who, after a caesarean section, brings a baby to his mother is a rehabilitation specialist, a physical therapist. His task is to explain to the mother how to pick up a child folded in half, how to put a child who has an unprotected spinal cord right under the skin, how to feed a child who cannot be held under her back.
A newborn baby with spina bifida, even if the operation is successful, is different from a healthy baby.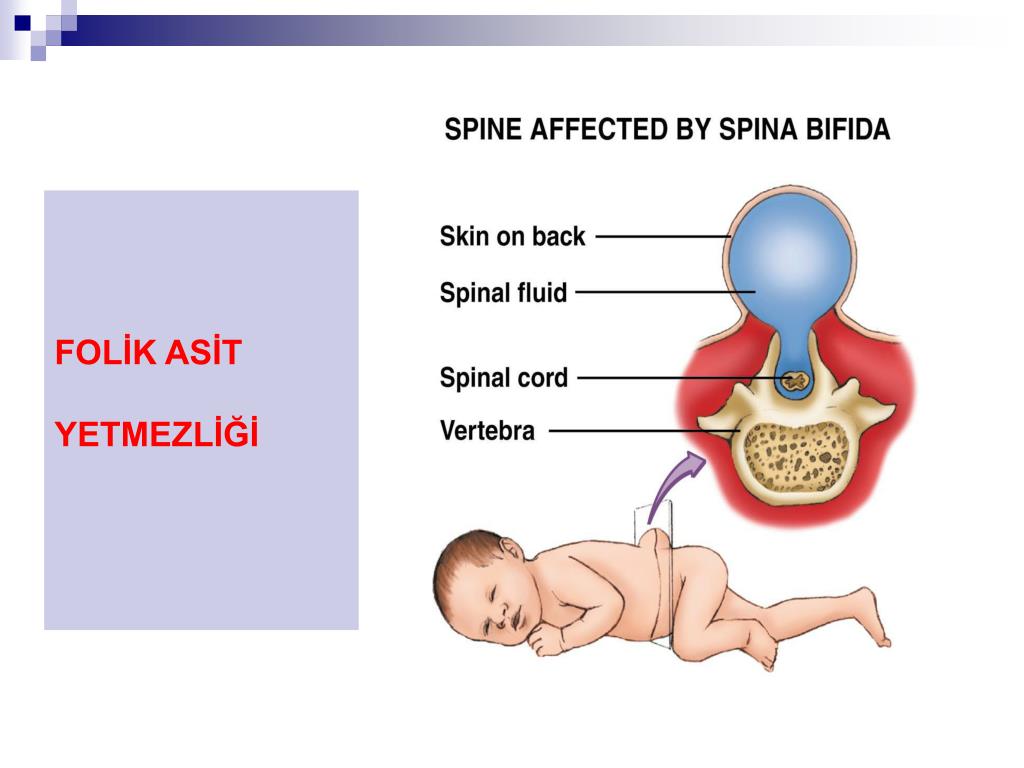 It is as if folded in half - legs to the head
It is as if folded in half - legs to the head
The baby and mother spend the first week of life in the intensive care unit, that is, in intensive care. Here, for children with spina bifida, there are also special rules: for example, they cannot take a blood test, like healthy children, from the heel, or from the head. Because about children with a herniated spinal cord, it is not known how sensitive the legs of a newborn are, and whether an injection in the heel, which does not feel anything, will lead to serious hemorrhagic disorders.
Spina bifida (spina bifida) - treatment, symptoms, causes, diagnosis
Spina bifida (spina bifida) is a complex congenital defect in the development of the spinal cord and spine. This is a type of open neural tube defect in which there is an abnormal development of the back of the spine, the spinal cord, the surrounding nerves, and/or the fluid-filled sac that surrounds the spinal cord.
Spina bifida (back bifida) is an incurable, life-long condition that affects the neuromuscular and musculoskeletal systems.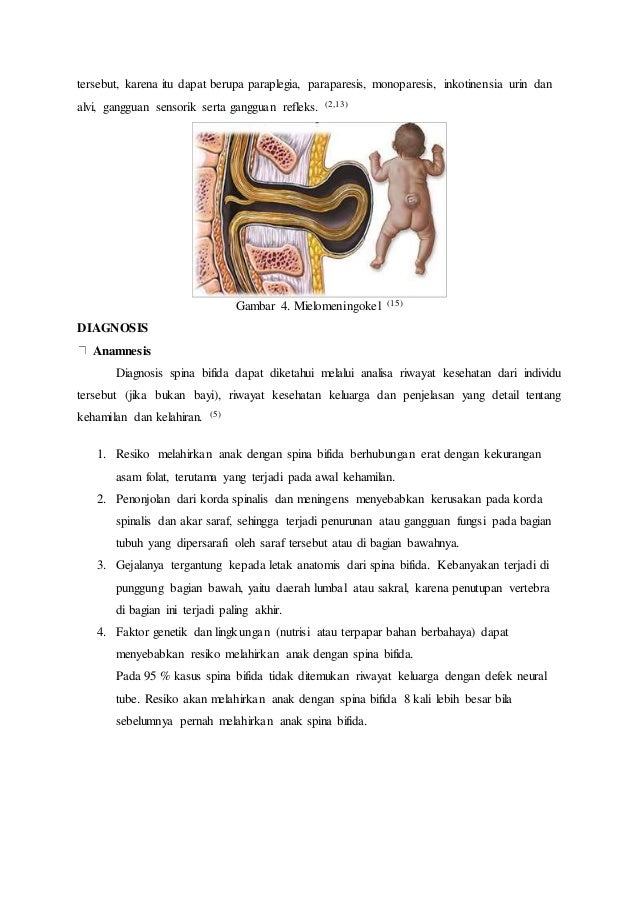
This defect varies by type and ranges from moderate to severe.
Children with such a defect may need corsets as they grow, and in severe cases, a wheelchair.
Treatment is mainly aimed at slowing down the deformity and maintaining motor activity.
The defect may occur along the entire length of the spine and may present as part of the spinal cord and surrounding tissues protruding outward rather than inward. Approximately 85 percent of defects occur in the lower back and 15 percent in the neck and thoracic region. Surgically, it is possible to restore the integrity of the spinal column, but nerve damage cannot be restored, and if they are pronounced, then patients have various degrees of paresis of the lower extremities. The higher the defect on the spinal column, the more severe the nerve damage and movement disorders (paresis and paralysis).
According to studies, this developmental anomaly occurs in 7 cases per 10,000 newborns. There are several types of spina bifida that have varying degrees of severity.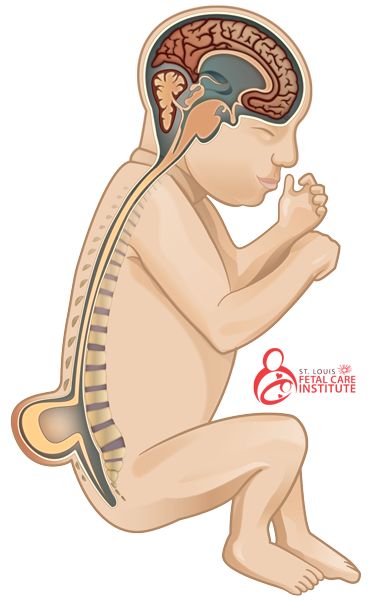
- Latent spina bifida (spina bifida occulta) - the most moderate form, in which there are no obvious signs of malformation and changes in the skin. In this form, at least one vertebra changes, but the nerves and spinal cord do not bulge. A child at birth may have a spot or depression in the area of the anomaly. And usually, the baby will not have symptoms. With this form of anomaly (as well as with others), there may be an anomaly in the development of the spinal cord, characterized by attachment of the spinal cord to the spine to the end of the lumbar region, when normally the spinal cord ends at the level of the first lumbar vertebrae and sags freely without attachment to the spine.
- Meningocele is a moderate (and the most common) anomaly in which the spinal canal is not properly closed and the meninges (membranes that cover the spinal cord) bulge outside the bony structures of the spinal canal, but the spinal cord itself remains intact. The cystic mass is covered with skin.
 Most children with meningocele have normal limb function, but may have partial paresis or abnormalities of the bladder or bowel. With this anomaly, there is often underdevelopment of the spinal cord. Almost all patients with this anomaly require surgery to close the defect and free the spinal cord.
Most children with meningocele have normal limb function, but may have partial paresis or abnormalities of the bladder or bowel. With this anomaly, there is often underdevelopment of the spinal cord. Almost all patients with this anomaly require surgery to close the defect and free the spinal cord. - Lipomeningocele is an anomaly in which fatty tissue is attached to the spinal cord and puts pressure on it. Children with this form of anomaly may not have severe nerve damage, but bladder and bowel function may be impaired. In these cases, surgical treatment is also often used.
- Myelomeningocele: the most severe common form and associated with spina bifida. The spinal canal is not closed, and the bulging mass consists of the meninges, pathologically altered spinal cord, and nerves. In addition, in this area the skin is also underdeveloped. In children with this form of spinal cord splitting, paresis below the defect and dysfunction of the pelvic organs are observed in whole or in part.
 In addition, nerve damage and other pathologies are observed.
In addition, nerve damage and other pathologies are observed.
Symptoms
The symptoms of spina bifida vary greatly, depending on the form and severity of the individual child. For example, at birth:
- With occult cleavage (spina bifida occulta), there may be no obvious signs or symptoms—only a small spot, depression, or birthmark.
- With a meningocele, there will be a sac-like protrusion that will be located on the back in the spinal region.
- With myelomeningocele, there will also be a protrusion, but with altered skin, there will be a release of nerves and spinal cord.
In severe spina bifida with localization in the lumbar spine, the following symptoms may occur: paralysis of the lower extremities, dysfunction of the bladder, intestines. In addition, these patients usually have other developmental anomalies:
- Hydrocephalus occurs in 75 percent of myelomeningocele cases and this condition requires operative endoscopic treatment in order to restore normal CSF flow or a shunt to drain excess fluid from the brain.

- Chiari anomaly (displacement of the brain into the upper cervical vertebrae) can cause pressure on the brainstem, which can manifest as impaired speech, swallowing, and motor disorders in the limbs.
- Spinal Cord Underdevelopment Orthopedic problems including scoliosis, kyphosis, hip dysplasia (congenital dislocation), combined deformities, clubfoot, etc.
- Precocious puberty (especially in girls with spina bifida and hydrocephalus).
- depression and other neurotic conditions
- obesity
- dermatological problems
- anomalies in the development of the urinary tract.
- heart diseases
- vision problems
Diagnosis
Diagnosis may be performed during pregnancy to evaluate the fetus for spina bifida. These include:
- Amniocentesis: A procedure in which a long, thin needle is inserted through the mother's abdomen into the amniotic sac to remove a small amount of amniotic fluid for examination.
 The fluid is analyzed to determine the presence or absence of an open neural tube defect. Although the analysis is very reliable, it does not allow diagnosing small or closed defects.
The fluid is analyzed to determine the presence or absence of an open neural tube defect. Although the analysis is very reliable, it does not allow diagnosing small or closed defects. - Prenatal ultrasound: this technique, being absolutely harmless, allows non-invasive assessment of the condition and visualization of the internal organs, vessels, tissues of the fetus. Sometimes it is possible to diagnose not only spina bifida, but also other anomalies.
- Blood tests: It is recommended that blood tests be performed between 15 and 20 weeks of gestation for all women who have not previously had a child with an open neural tube defect and who have no family history of the condition. A blood test for alpha-fetoprotein and other biochemical parameters can determine how high the risk of developing spinal anomalies is.
- At birth, severe cases of spina bifida are evident by the presence of a fluid-filled sac bulging on the back of the newborn. Visual indicators of mild forms (spina occulta) may be a hairy patch on the skin or a depression along the spine.
 Unusual weakness or lack of coordination in the lower extremities also suggests spina bifida. In children and adults, this anomaly is often diagnosed during routine studies or, if necessary, to differentiate neurological symptoms using instrumental research methods (MRI, CT, radiography).
Unusual weakness or lack of coordination in the lower extremities also suggests spina bifida. In children and adults, this anomaly is often diagnosed during routine studies or, if necessary, to differentiate neurological symptoms using instrumental research methods (MRI, CT, radiography).
Causes
During pregnancy, the human brain and spinal column begin to form as a flat sheet of cells that folds into a tube called the neural tube. If all or part of the neural tube fails to close, then the open area is called an open neural tube defect. An open neural tube is open in 80 percent of cases, and is covered by bone or skin in 20 percent of cases. The cause of spina bifida (spina bifida and other defects) remains unknown, but is most likely the result of a combination of genetic, nutritional, and environmental factors, such as:
- deficiency of folic acid (vitamin B) in the mother's diet during pregnancy (sufficient folic acid intake during pregnancy may reduce the risk of this anomaly).
- maternal uncontrolled diabetes
- Certain medicines (antibiotics, anticonvulsants).
- The genetic factor, as a rule, matters only in 10 percent of cases.
- Mother's age
- Which births are on the bill (firstborns are more at risk).
- Socioeconomic status (children born in lower socioeconomic families are at higher risk).
- ethnicity
- obesity or excessive consumption of alcohol by a pregnant woman
- When a pregnant woman is exposed to hyperthermia in the early stages (sauna, jacuzzi).
Treatment
Spina bifida can be treated immediately after birth. If this defect is diagnosed prenatally, then a caesarean section is recommended in order to reduce possible damage to the spinal cord during the passage of the birth canal. Newborns with meningocele or myelomeningocele are recommended to have surgery within 24 hours of birth. With such an operation, the bone defect is closed and it is possible to preserve the function of the intact part of the spinal cord.