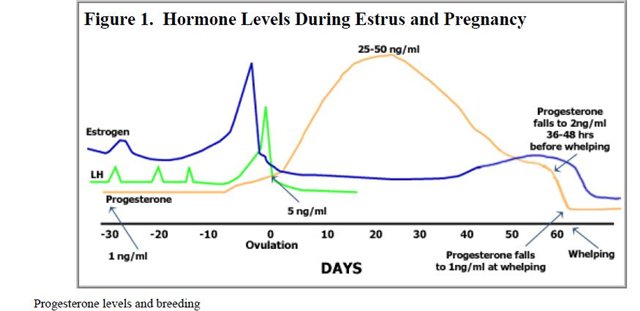
Low hormone levels during pregnancy
Low hCG Levels: Causes, Treatments, and Symptoms
Low hCG Levels: Causes, Treatments, and SymptomsMedically reviewed by Karen Gill, M.D. — By Becky Young on November 3, 2017
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission. Here’s our process.
What is an hCG test?
Human chorionic gonadotropin (hCG) is a hormone produced by your placenta once an embryo implants in the uterus.
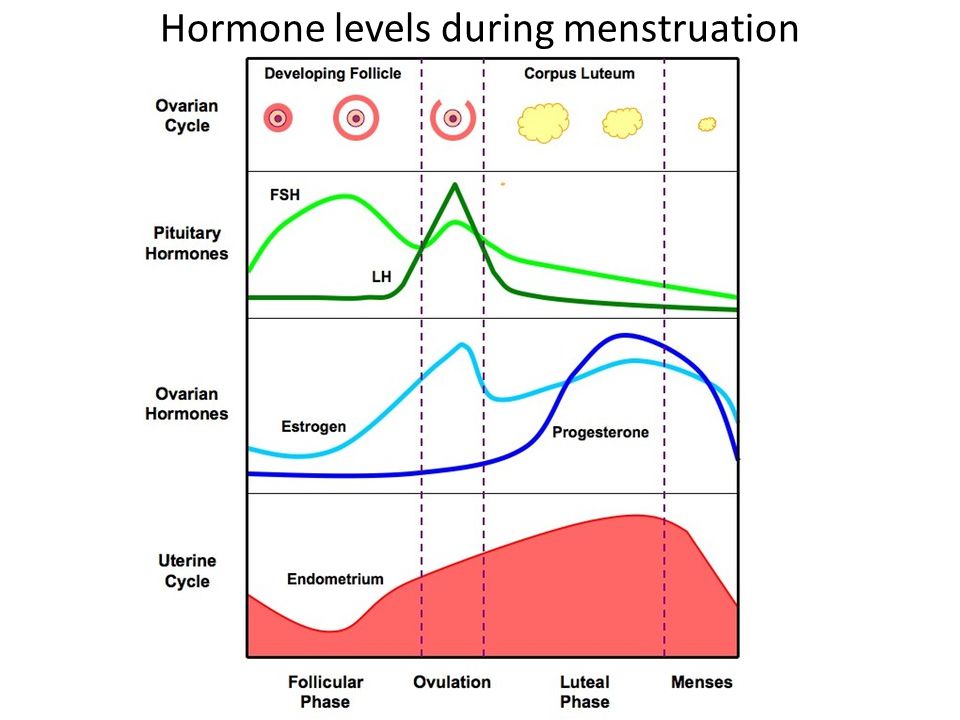
The purpose of the hormone is to tell your body to continue to produce progesterone, which prevents menstruation from occurring. This protects the endometrial uterine lining and your pregnancy.
A pregnancy test can detect hCG in your urine if your levels are high enough. This is how the test identifies that you are pregnant. But only a blood test can give you a precise numerical hCG reading.
Purchase pregnancy tests here.
Standard hCG levels
Standard hCG levels vary quite massively from woman to woman. This is because hCG levels really depend on what is normal for you, how your body responds to pregnancy, as well as how many embryos you are carrying. The way a woman’s body reacts to pregnancy is entirely unique.
The table below gives you a guideline as to the normal wide range of hCG levels in each week of pregnancy. hCG levels are measured in milli-international units of hCG hormone per milliliter of blood (mIU/mL).
hCG levels usually consistently rise until around week 10–12 of your pregnancy, when the levels plateau or even decrease. This is the reason why pregnancy symptoms can be greater in the first trimester and ease off after this time for many women.
In early pregnancy, hCG levels usually double every two to three days. Interestingly, when the measurements start off high they don’t expand at the same rate. If they start off more slowly, the increase ends up happening much quicker.
If your hCG levels fall below the normal range, your doctor may want you to have a blood test every two to three days to ensure the levels are increasing.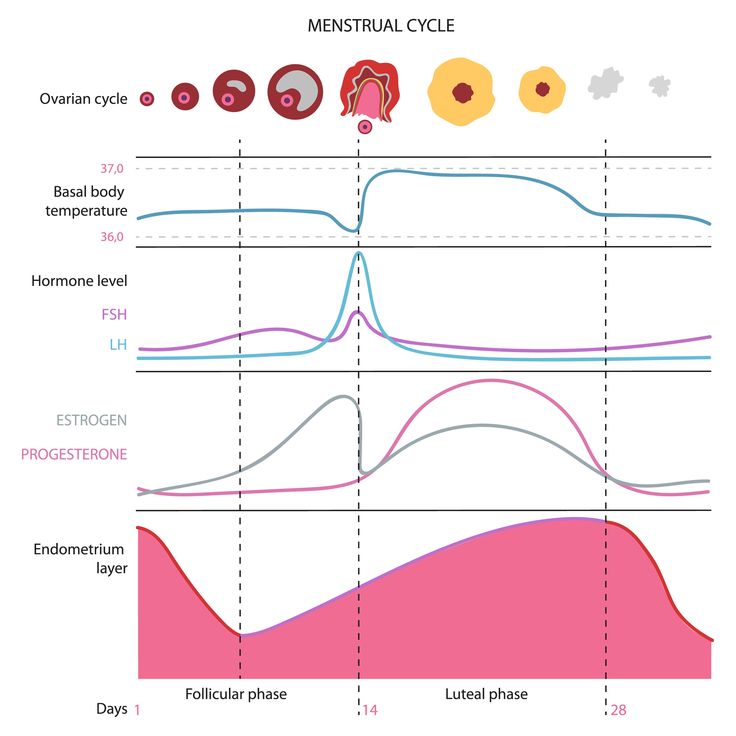 A single measurement of your hCG level is not useful. To give an accurate indication, a series of hCG blood tests needs to be taken a couple of days apart and the readings compared. There is often variation with a rapid increase in numbers, especially in the first few weeks of pregnancy.
A single measurement of your hCG level is not useful. To give an accurate indication, a series of hCG blood tests needs to be taken a couple of days apart and the readings compared. There is often variation with a rapid increase in numbers, especially in the first few weeks of pregnancy.
Causes of low hCG levels
If your hCG levels fall below the normal range, it’s not necessarily a cause for concern. Many women have gone on to have healthy pregnancies and babies with low hCG levels. Most women don’t ever have cause to find out what their hCG levels are specifically.
However, sometimes low hCG levels can be caused by an underlying problem.
Gestational age miscalculated
Typically, the gestational age of your baby is calculated by the date of your last menstruation. This can be easily miscalculated, particularly if you have a history of irregular periods or are unsure of your dates.
When low hCG levels are detected, it’s often because a pregnancy that was thought to be between 6 and 12 weeks is actually not that far along. An ultrasound and further hCG tests can be used to calculate the gestational age correctly. This is usually the first step when low hCG levels are detected.
An ultrasound and further hCG tests can be used to calculate the gestational age correctly. This is usually the first step when low hCG levels are detected.
Miscarriage
A miscarriage is a pregnancy loss that occurs before 20 weeks of gestation. Sometimes low hCG levels can indicate that you have had or will have a miscarriage. If the pregnancy fails to develop a placenta, then the levels may be normal initially but fail to rise. Common signs that you are experiencing a miscarriage are:
- vaginal bleeding
- abdominal cramps
- passing tissue or clots
- cessation of pregnancy symptoms
- discharge of white/pink mucus
Blighted ovum
This is when an egg is fertilized and attaches to the wall of your womb, but does not continue to develop. When the gestational sac develops, hCG hormone can be released, but the level does not rise since the egg doesn’t develop.
This occurs very early in pregnancy. Most women won’t even know that it’s taken place.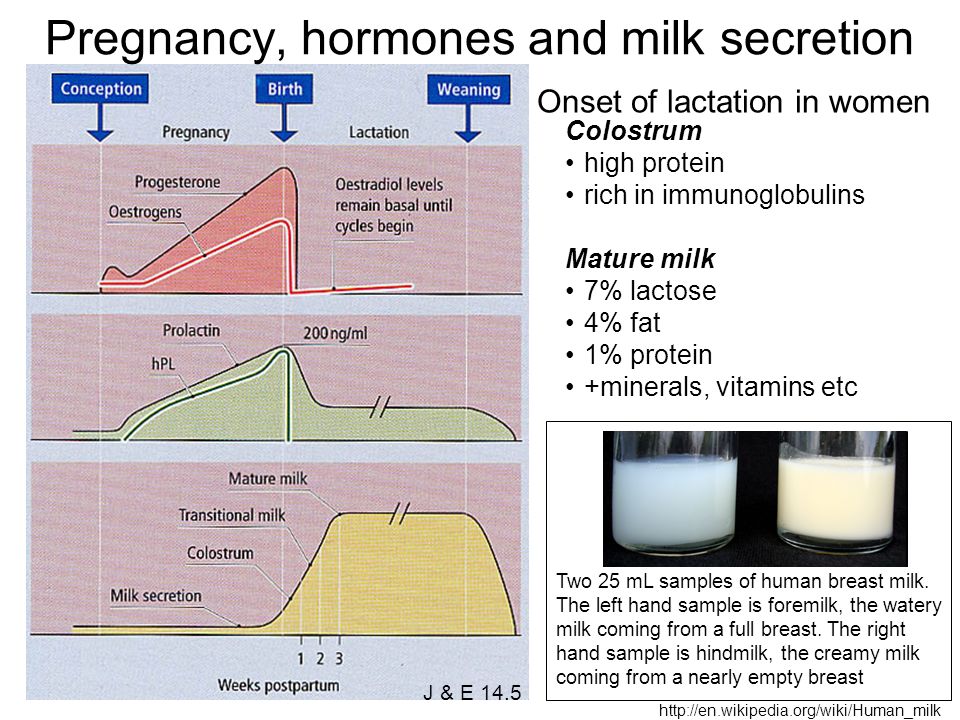 Usually you’ll experience your normal menstruation symptoms and assume it’s your usual period. However, if you’re trying to conceive, you may do an early pregnancy test that could pick up the presence of hCG.
Usually you’ll experience your normal menstruation symptoms and assume it’s your usual period. However, if you’re trying to conceive, you may do an early pregnancy test that could pick up the presence of hCG.
Ectopic pregnancy
An ectopic pregnancy is when the fertilized egg remains in the fallopian tube and continues to develop. It’s a dangerous and life-threatening condition, as it may cause the fallopian tube to rupture and bleed excessively. Low hCG levels can help to indicate an ectopic pregnancy. At first the symptoms of an ectopic pregnancy can be similar to those of a normal pregnancy, but as it progresses you can experience the following:
- abdominal or pelvic pain that worsens with straining or movement (this can happen strongly on one side initially and then spread)
- heavy vaginal bleeding
- shoulder pain caused by internal bleeding (the bleeding aggravates the diaphragm and presents as pain at the tip of the shoulder)
- pain during intercourse
- pain during a pelvic examination
- dizziness or fainting due to internal bleeding
- symptoms of shock
How is it treated?
Unfortunately, there is nothing that can be done to treat low hCG levels, though low levels alone are not always a cause for concern.
If your low hCG levels have been caused by a miscarriage, it’s possible that you may need treatment if any pregnancy tissue is left inside your womb. If there’s no tissue retained, then you won’t require any treatment at all. If there is, then there are three treatment options available:
- You can wait for the tissue to pass naturally.
- You can take medication to help you to pass the tissue.
- You can have it surgically removed.
Your doctor will discuss with you what the best course of action is.
The treatments for an ectopic pregnancy are similar. Medications are given to prevent the pregnancy from continuing to grow. If surgery is required, it’s standard for the doctors to remove the affected fallopian tube as well as the pregnancy.
What’s the outlook?
Low hCG levels alone are not necessarily a reason to be worried. There are many factors that affect the levels, and the normal range varies hugely between individual women. Your doctor will be able to monitor your hCG levels for you if you have concerns. Even if they remain low, there is nothing that you can do. It’s also important to remember that low hCG isn’t caused by anything you’ve done.
Your doctor will be able to monitor your hCG levels for you if you have concerns. Even if they remain low, there is nothing that you can do. It’s also important to remember that low hCG isn’t caused by anything you’ve done.
If your low hCG levels are due to a pregnancy loss, this doesn’t necessarily mean that you won’t be able to get pregnant and carry to term in the future. If you lose a fallopian tube due to an ectopic pregnancy, your fertility shouldn’t change significantly as long as your other tube is functioning. Even if it isn’t, reproductive technologies like in vitro fertilization can help lead to successful pregnancy.
Last medically reviewed on November 3, 2017
- Parenthood
- Pregnancy
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.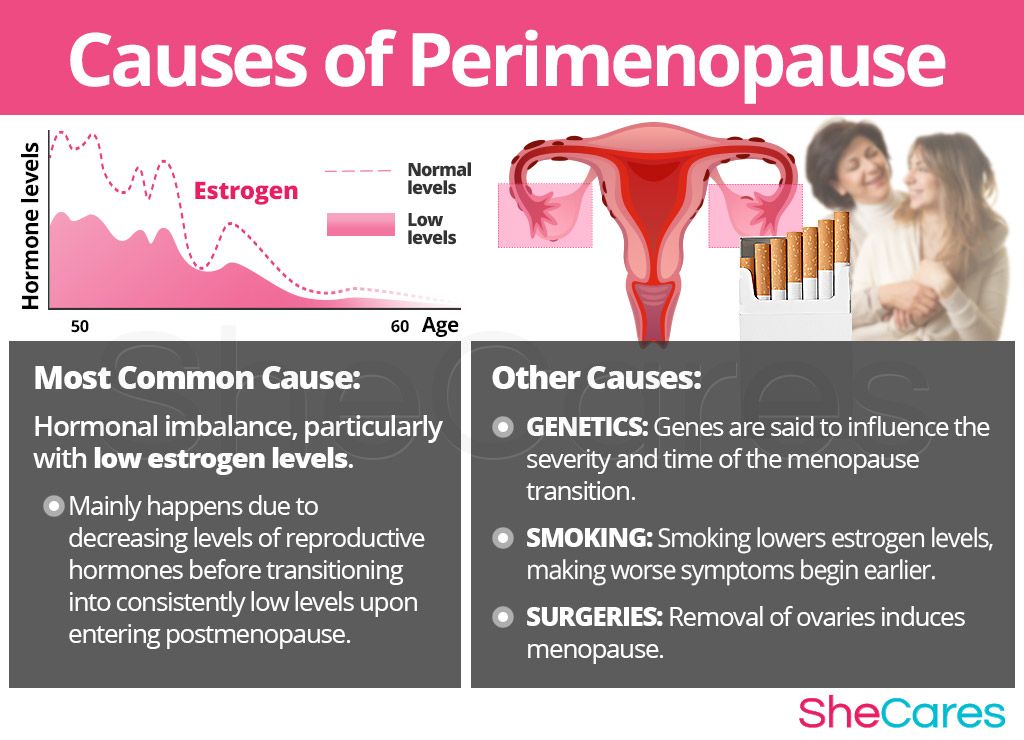
- Fan J, et al. (2017). Advances in human chorionic gonadotropin detection technologies: A review.
ncbi.nlm.nih.gov/pubmed/29056064 - Human chorionic gonadotropin (HCG): The pregnancy hormone. (2017).
americanpregnancy.org/while-pregnant/hcg-levels/ - Lawrenz B, et al. (2017). Luteal phase serum progesterone levels after GnRH-agonist trigger – how low is still high enough for an ongoing pregnancy?
ncbi.nlm.nih.gov/pubmed/29037085 - Matson PL, et al. (1990). Measurement of human chorionic gonadotropin during early pregnancy: A comparison of two immunoradiometric assays.
link.springer.com/article/10.1007/BF01135683 - Schumacher A. (2017). Human chorionic gonadotropin as a pivotal endocrine immune regulator initiating and preserving fetal tolerance.
ncbi.nlm.nih.gov/pubmed/29039764
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.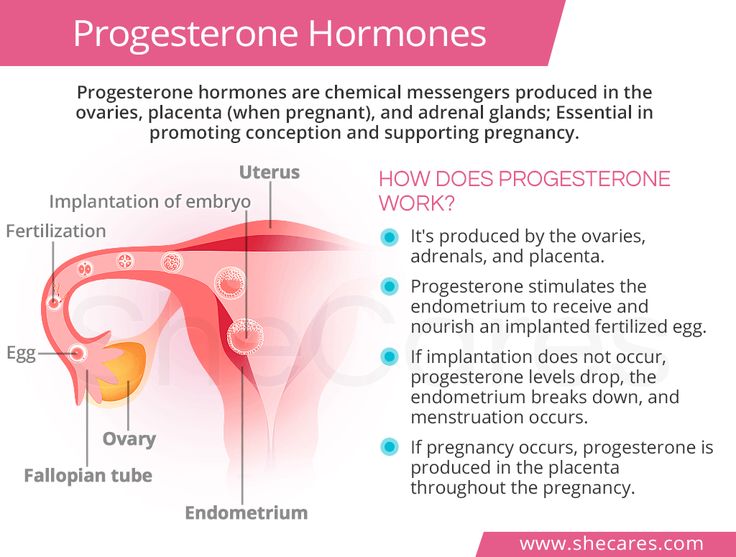
Current Version
Nov 3, 2017
By
Becky Young
Edited By
Phil Riches
Medically Reviewed By
Karen Richardson Gill, MD
Share this article
Medically reviewed by Karen Gill, M.D. — By Becky Young on November 3, 2017
Read this next
Human Chorionic Gonadotropin (hCG) Blood Test
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT
Get the facts on the human chorionic gonadotropin (hCG) blood test. Although it's often used to detect pregnancy, it has other uses such as detecting…
READ MORE
Can Taking Prometrium Vaginally Prevent Miscarriage?
Medically reviewed by Debra Sullivan, Ph.D., MSN, R.N., CNE, COI
Progesterone is known as the “pregnancy hormone.” Without enough progesterone, a woman’s body can’t continue to grow a fertilized egg. If you’ve…
READ MORE
How Does Clomid Work for Fertility?
Medically reviewed by Amanda Kallen, MD
Clomid is also known as clomiphene citrate.
 It’s an oral medication that is often used to treat certain types of female infertility.
It’s an oral medication that is often used to treat certain types of female infertility. READ MORE
How Many Eggs Are Women Born With? And Other Questions About Egg Supply
If you're looking to get pregnant, you may wonder how many eggs you have at various points in life. The short answer: It goes from millions to none.
READ MORE
Your Guide to the Egg Donation Process
Medically reviewed by Fernando Mariz, MD
There are many reasons you might consider donating your eggs. Learn more about the egg donation process, including possible risks, legal…
READ MORE
What’s the Connection Between Your Biological Clock and Fertility?
Medically reviewed by Amanda Kallen, MD
The biological clock describes the pressure people may feel to get pregnant while at the peak of their reproductive years, before fertility declines.
READ MORE
How Polycystic Ovary Syndrome (PCOS) Affects Fertility and What to Do
Medically reviewed by Amanda Kallen, MD
Polycystic ovary syndrome is a common cause of infertility. We'll discuss why and what you can do.
READ MORE
Low hCG levels in pregnancy: What does it mean?
Human chorionic gonadotropin (hCG) is a hormone that is produced by cells in the placenta during pregnancy. Its job is to nurture and feed the embryo that is attached to the wall of the uterus.
Lower than normal levels of hCG may indicate a problem with the pregnancy including:
- miscarriage
- ectopic pregnancy
- fetal death
Levels of hCG can vary significantly between individuals and from one pregnancy to the next in the same person. But, typically, hCG levels follow a typical range throughout a healthy, uncomplicated pregnancy.
Levels of hCG typically increase in the first trimester of a healthy pregnancy.
Levels of hCG usually increase during the first trimester, peak by weeks 8 to 11, and then decline to a steady level in the later stages of the pregnancy.
This means that as the pregnancy develops, hCG becomes less useful as a way to monitor it. When hCG levels do not increase or decrease as they should, it may be a sign of a problem with the pregnancy.
Increasing levels of hCG usually mean that a pregnancy is healthy. However, low hCG levels are not always a sign that something is wrong.
Possible causes of low hCG levels are:
Blighted ovum
A blighted ovum occurs when a fertilized egg attaches to the wall of the uterus, but the embryo fails to develop.
This can happen during early pregnancy, sometimes before a person even knows they are pregnant.
Miscarriage
Miscarriage is also known as spontaneous abortion and happens when the embryo dies naturally before 20 weeks of gestation.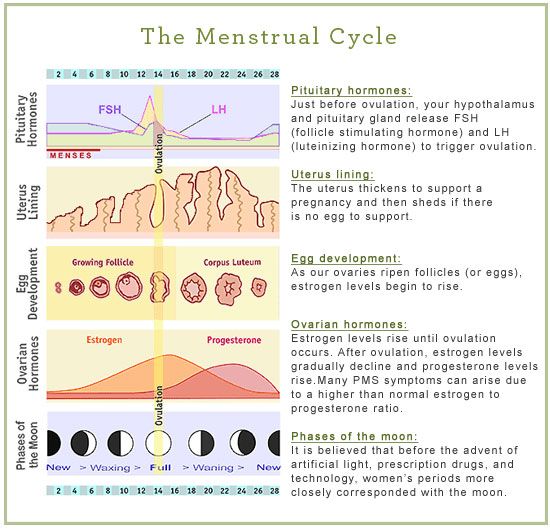
Levels of hCG may rise initially in these situations but fail to increase or decrease as they should afterward.
Miscalculated gestational age
Share on PinterestLevels of hCG may appear low if a doctor has miscalculated the baby’s due date.
This happens when the stage of pregnancy and the estimated date of birth are wrong.
Calculating these events is based on the dates of a woman’s last menstrual period, so miscalculations can occur if someone experiences irregular periods or is not sure when they had their last period.
Low levels of hCG can indicate whether a pregnancy is in a stage where low hCG levels are normal, such as in very early pregnancy, or in a pregnancy that is post-11 weeks.
Sometimes, in cases of miscalculated gestational age, the level of hCG may be lower than expected but not abnormal for the pregnancy.
Ectopic pregnancy
This is an abnormal pregnancy where the embryo attaches outside of the uterus, usually inside the fallopian tube, the tube that carries the egg from the ovary to the uterus.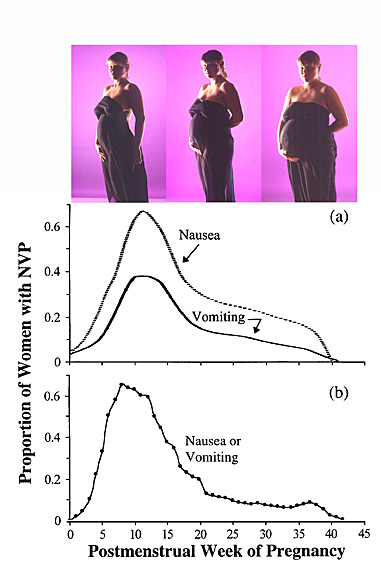
Symptoms can include abdominal pain and vaginal bleeding. An ectopic pregnancy can be a very serious, and even life-threatening, condition. Levels of hCG remain low during an ectopic pregnancy.
Low levels of hCG are not always a sign of a problem.
Unfortunately, there is no cure for situations where low hCG levels are a cause for concern.
However, treatment is available for the underlying conditions that cause low hCG levels, such as a miscarriage or an ectopic pregnancy.
In case of a miscarriage
Treatment may involve removing any pregnancy tissue that has been left inside the uterus and might include medication or a surgical procedure.
In case of an ectopic pregnancy, the doctor may also prescribe medications or surgery to remove the affected fallopian tube and the pregnancy itself.
Low hCG levels that result from a miscarriage or an ectopic pregnancy are usually accompanied by abdominal pain, with or without vaginal bleeding.
There is currently no way to prevent low hCG levels or its associated complications, such as a blighted ovum, a miscarriage, or an ectopic pregnancy.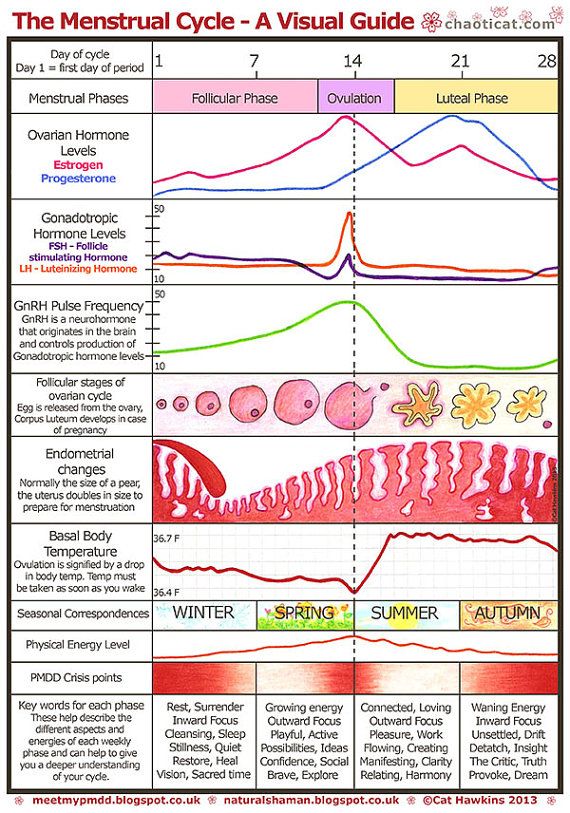
Low levels of hCG are not always a cause for concern. Levels of hCG can differ between individuals and between different pregnancies in the same person. Some people may naturally have lower levels of hCG than others.
Taking measurements of levels throughout the pregnancy can indicate if the pregnancy is developing as expected.
Even if a complication associated with low hCG levels occurs, such as a miscarriage or an ectopic pregnancy, this does not mean that someone will be unable to get pregnant again or that their fertility is compromised. A successful pregnancy is still possible with low hCG levels.
Hormonal studies during pregnancy / Nyanya.ru
02/27/2012
Nona Hovsepyan, Consultant Physician, Independent Laboratory INVITRO
Why is it necessary to control the level of hormones?
Hormones are amazing biologically active substances that affect not only the state of health, but also the inner world of a person. Nature provides that in the female body immediately after conception, special pregnancy hormones are activated, which not only help the baby to fully develop, but also set up the expectant mother for the desired motherhood, teach them to love the baby growing inside and get used to taking care of him.
Nature provides that in the female body immediately after conception, special pregnancy hormones are activated, which not only help the baby to fully develop, but also set up the expectant mother for the desired motherhood, teach them to love the baby growing inside and get used to taking care of him.
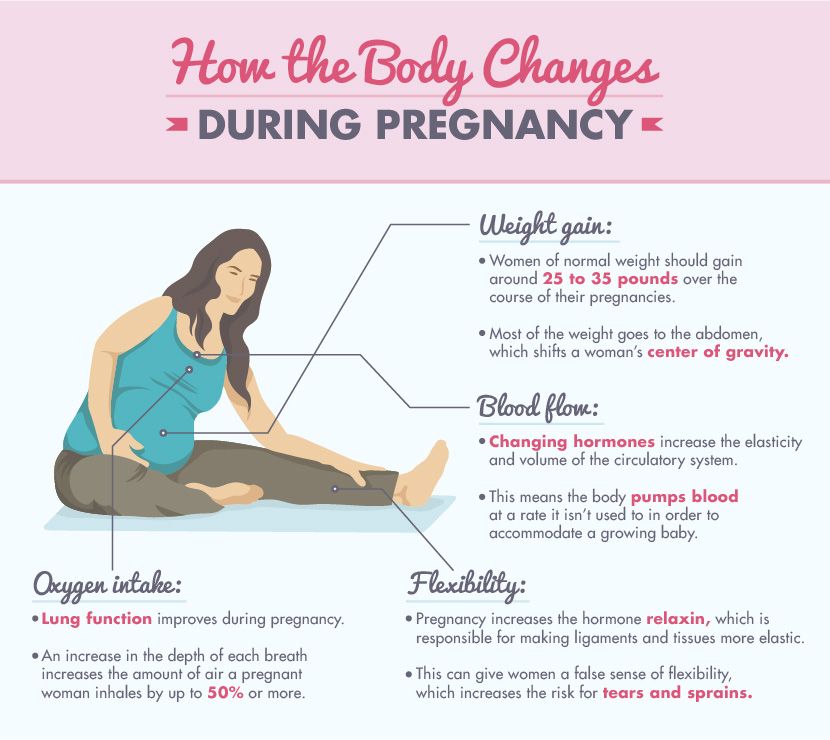
During the period of expectation of a baby, serious changes occur in the whole body of a woman, especially her hormonal levels. Changes occur throughout the endocrine system. The body of the future mother, completely rebuilding, creates the conditions for the bearing and normal development of the baby, and from the first days of pregnancy begins to prepare for childbirth.
All hormonal indicators of the future mother's body play a huge role - namely, they are the most important indicators of fetal development. Therefore, the level of hormones is necessarily monitored by the attending physician with the help of special examinations - prenatal screenings, which a woman needs to undergo at least 2 times: in the first trimester (11-12 weeks) and in the second trimester (16-19weeks). Let's figure out what indicators are included in this mandatory examination, what the increase or decrease in the level of a particular hormone indicates, and what their role is.
Hormones that the body of the unborn baby "produces"
HCG. This is human chorionic gonadotropin, a hormone that is actively produced by the cells of the chorion (fetal membrane) immediately after it attaches to the wall of the uterus. The "production" of this hormone is vital for the preservation and maintenance of pregnancy! It is hCG that controls the production of the main pregnancy hormones - estrogen and progesterone. With a serious lack of hCG, the fertilized egg is detached from the uterus, and menstruation occurs again - in other words, a spontaneous miscarriage occurs. Normally, the concentration of hCG in the blood of the expectant mother is constantly growing, reaching a maximum by the 10-11th week of pregnancy, then the concentration of hCG gradually decreases to remain unchanged until the very birth.
Testing for hCG during pregnancy plays a huge role.
Firstly, an analysis of the level of hCG in the blood can confirm that you will become a mother already 5-6 days after conception. This is much earlier and, most importantly, much more reliable than using conventional rapid tests.
Secondly, the test is needed to determine the exact gestational age. Very often, the expectant mother cannot give the exact date of conception, or she calls it, but incorrectly. At the same time, certain indicators of growth and development correspond to each period, deviations from the norm may indicate the occurrence of complications.
Thirdly, the level of hCG in the blood can quite accurately “tell” whether your baby is developing correctly.
An unplanned increase in the level of hCG usually occurs with multiple pregnancy, preeclampsia, taking synthetic gestagens, diabetes in the expectant mother, and may also indicate some hereditary diseases in the baby (for example, Down's syndrome) and multiple malformations. An abnormally low level of hCG can be a sign of an ectopic and non-developing pregnancy, fetal growth retardation, the threat of spontaneous abortion, and chronic placental insufficiency.
However, do not rush to sound the alarm: increased or decreased values may also indicate that the gestational age was initially set incorrectly. Your doctor will help you interpret the test results correctly.
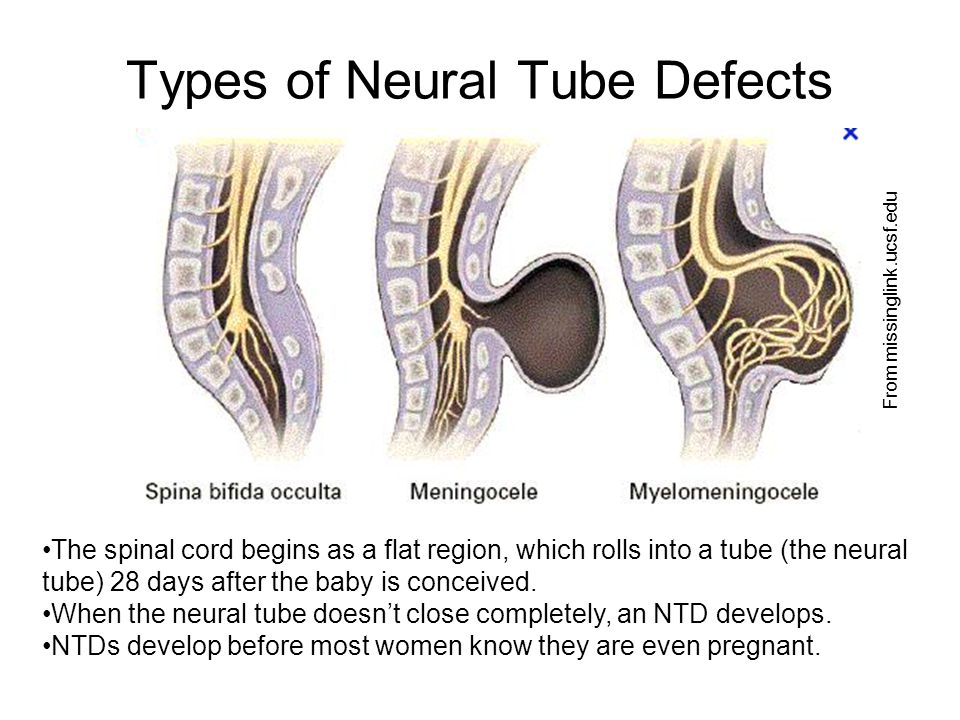
Placental lactogen and free estriol. Controlling the level of these hormones is extremely important for assessing the risk of developing hereditary chromosomal abnormalities in an unborn baby (these are Down, Edwards, Turner, Patau syndromes, neural tube defects, etc.)
Free estriol is "produced" by the placenta. This hormone improves blood flow through the vessels of the uterus, and also contributes to the development of the ducts of the mammary glands, preparing the body of the expectant mother to feed the baby. The level of free estriol changes in any pathological conditions:
- with fetoplacental insufficiency, when the normal blood flow and nutrition in the placenta changes;
- for fetal growth retardation;
- for suspected post-term pregnancy.
Placental lactogen (PL) is also “produced” by the placenta and can be detected in the blood of the expectant mother as early as 5-6 weeks of pregnancy. It reaches its maximum value by 37-38 weeks, then the hormone level gradually decreases. However, the level of PL must be monitored throughout the entire period of pregnancy - first of all, this is necessary to assess the condition of the placenta and timely diagnosis of placental insufficiency. A sharp decrease in the level of PL by more than 2 times (compared to the average level in accordance with the gestational age) may indicate a delay in fetal development. In this case, it is necessary to take emergency measures to prevent a decrease in the level of PL by 80 percent or more - this can lead to the death of the baby.
Pregnancy hormones
Estradiol and progesterone. Hormonal studies necessarily include tests for the level of progesterone and estradiol.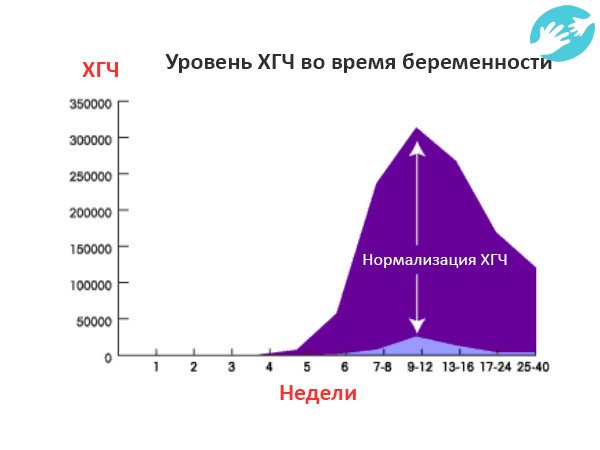 It is they who take care of your unborn baby, maintaining the normal course of pregnancy, which is why they are called the main hormones of gestation (pregnancy).
It is they who take care of your unborn baby, maintaining the normal course of pregnancy, which is why they are called the main hormones of gestation (pregnancy).
Estradiol is produced by the ovaries and during pregnancy also by the placenta. During pregnancy, the level of the hormone rises sharply, and it is not surprising - estradiol is "responsible" for the normal course of pregnancy. In the early stages, the concentration of this hormone evaluates the functioning of the placenta. A decrease in the level of estradiol indicates a serious threat of abortion.
By the way, it is under the influence of this hormone that a woman feels a natural desire to “build a nest”, arrange everything and prepare for the birth of a baby. Before childbirth, the concentration of the hormone in the body of the expectant mother reaches its “peak”, which is also due to natural causes - estradiol, acting as the strongest natural pain reliever, helps to make the process of giving birth to a baby less painful.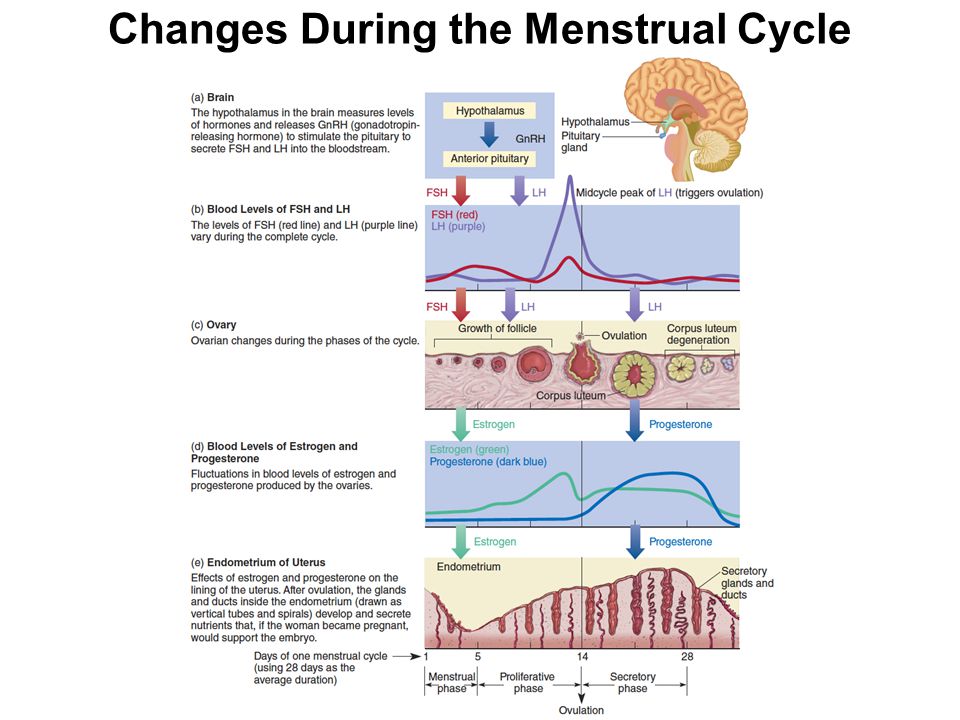
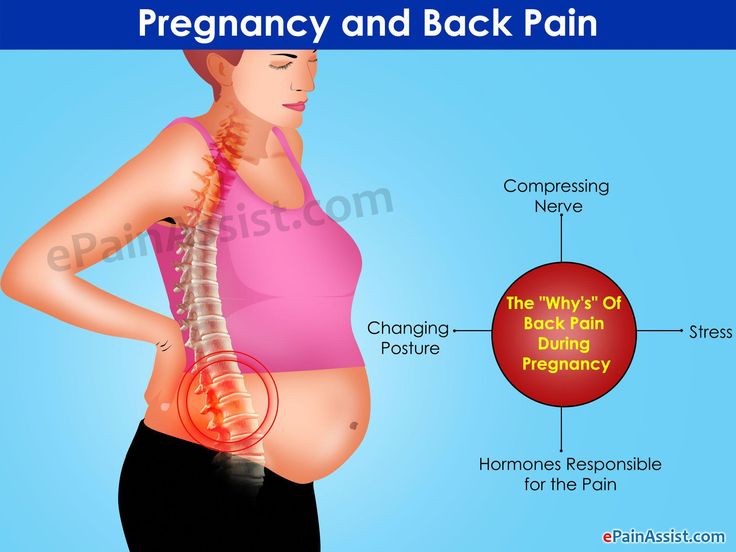
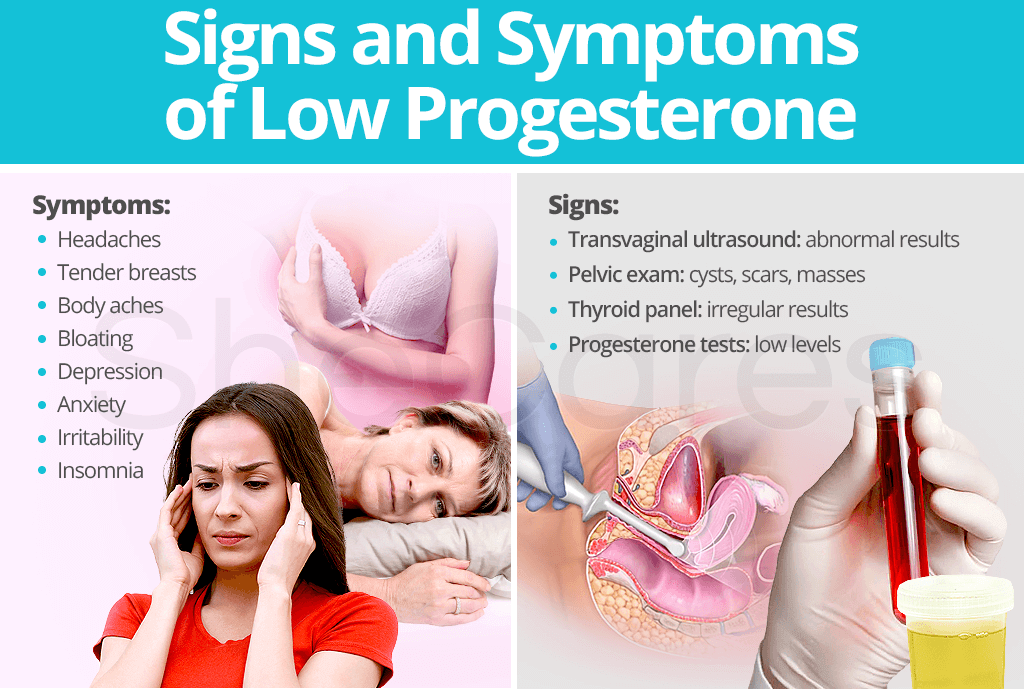
Progesterone is also the main “pregnancy hormone”, the main task of which is to maintain pregnancy and create the necessary conditions for the development of the fetus. A normal level of progesterone is necessary for conception to occur. Together with estrogens, the hormone promotes the attachment of a fertilized egg to the endometrium and carefully reduces the increased tone of the uterus, preventing miscarriage. During the bearing of the baby, progesterone stimulates the growth and maturation of the mammary glands, “preparing” the body of the expectant mother for breastfeeding, and psychologically, it calms her down and morally supports her. Unfortunately, this hormone also has "side" effects that are familiar to every pregnant woman - this is increased drowsiness, nausea, frequent urination, soreness and swelling of the breast.
With a lack of progesterone, pregnancy can occur with serious complications. Hormone deficiency must be urgently replenished, otherwise the risk of non-developing pregnancy and miscarriage increases.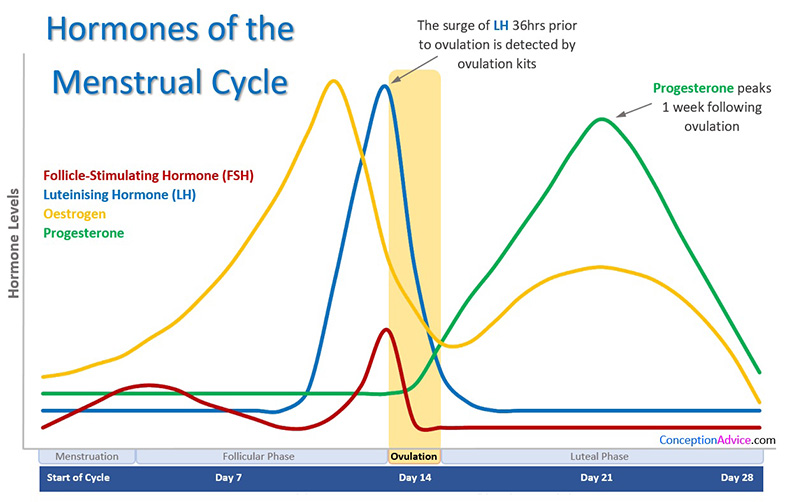
Important! Testing for estradiol and progesterone levels is carried out both during pregnancy and in preparation for the birth of a child, this is especially necessary in cases where a woman has already had a miscarriage.
Thyroid hormones
The normal functioning of the thyroid gland of the expectant mother plays an important role in the development of the baby. The corresponding hormones (TSH, T3 and T4) can also “tell” about the presence of hypo- or hyperfunction of the gland.
Maternity hormones
Pituitary hormones (an endocrine gland located in the hypothalamic part of the brain) also play an indispensable role while waiting for a baby. During childbirth, the pituitary gland releases the hormone oxytacin into the blood, which stimulates uterine contractions. And after childbirth, an active synthesis of the hormone prolactin begins, which is “responsible” for lactation. With a lack of prolactin, a woman simply would not be able to fully feed her baby with breast milk.
In addition, prolactin and oxytacin are also called "maternity hormones", because thanks to them, the mother's heart is filled with tenderness, she feels the pleasure of feeding and communicating with the child, which binds her to the baby even more. These hormones, in fact, provide a magical “transformation” of a woman into a mother - under their influence, priorities change dramatically, study, work, career and personal success fade into the background, and the main place in a woman’s heart is occupied by a small native creature. It is believed that the more a woman has these same "maternity hormones", the stronger her desire to constantly be with the baby, feel his warmth, take care of him. However, one should not expect that this “transformation” will happen as if by magic: normally, the level of hormones in a woman’s body changes gradually, so that her psyche has time to prepare for the changes without stress. The main thing during pregnancy is to make every effort to endure a strong and healthy baby.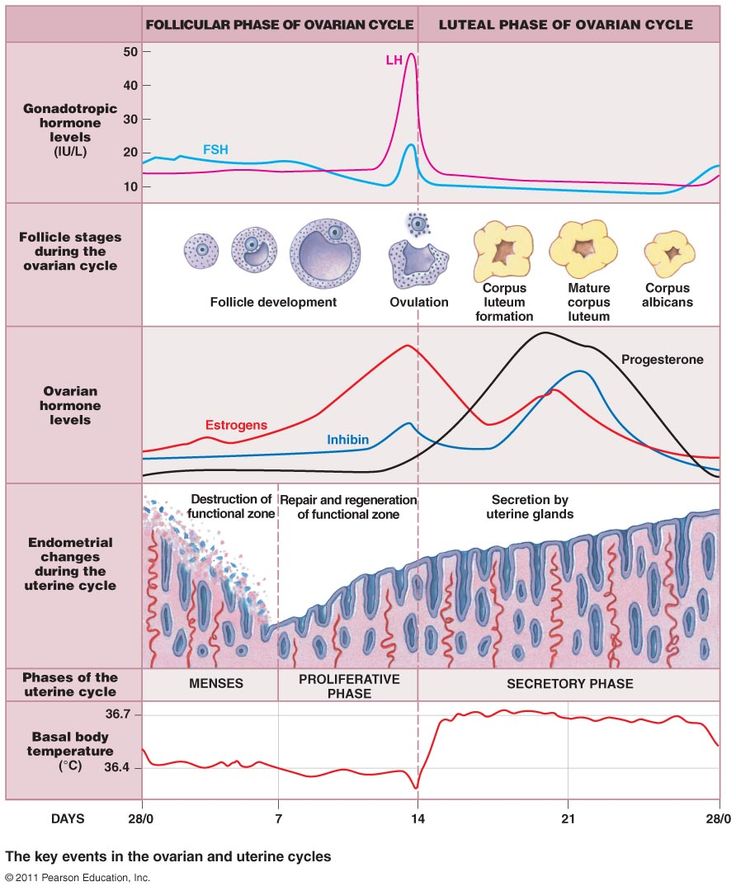
Changes in thyroid function during pregnancy
O.V. Ushakova, D.V. Pozdnyakova, A.M.
Municipal Budgetary Institution of Health Care "Clinical Diagnostic Center" of the Health Department of the Administration of Khabarovsk
Abstract: The aim of the study is to assess the prevalence of changes in thyroid function in pregnant women.
The study showed that in the first trimester only 45.6% of cases during pregnancy have a normal functioning of the thyroid gland.
In 39.6% of cases, there was an increase in thyroid function. The average TSH level in women in the second group was 0.08±0.01 μIU/ml, free T4 - 29.2±0.8 pmol/l. Taking into account the absence of a thyrotoxicosis clinic, this condition was regarded as transient gestational thyrotoxicosis due to the production of chorionic gonadotropin by the placenta, therefore, thyrostatics were not treated. In the second trimester, the levels of thyroid hormones in women of this group were restored to normal values.
Subclinical hypothyroidism occurs in 12% of women.
Key words: pregnancy, gestational thyrotoxicosis, subclinical hypothyroidism.
Summary: A research objective – to estimate the prevalence of changes of function of a thyroid gland at pregnant women.
Research showed that in the first trimester only at 45.6% of cases during pregnancy function is noted normal functioning of a thyroid gland.
In 39.6% of cases increase of function of a thyroid gland was noted. The average value of the level of TTG at women in the second group made 0.08±0.01 mkME/ml, free T4 – 29.2±0.8 pmol/l the accounting of absence of clinic thyrotoxicosis, this condition was regarded as passing gestational thyrotoxicosis, caused by production of a horionichesky gonadotrophin by a placenta therefore treatment by the tireostatiky wasn't carried out. In the second trimester indicators of levels of hormones of a thyroid gland at women of this group were restored to normal values.
In 12% of cases at women the subclinical hypothyroidism meets.
Keywords: pregnancy, gestational hyperthyroidism, subclinical hypothyroidism.
Introduction:
In the context of deteriorating somatic and reproductive health of women, the most promising issues are early diagnosis, prevention and correction of conditions leading to the development of a threat of miscarriage, the birth of a healthy child. The course of pregnancy, the physical development of the child, and his intellectual potential depend on how effectively the thyroid gland produces thyroid hormones during pregnancy. During pregnancy, the level of thyroid hormones should increase by 30-50%. At this time, a temporary endocrine organ is formed in women - the placenta, which secretes chorionic gonadotropin, placental lactogen, estriol, estradiol, progesterone into the woman's body. Produced in the first trimester of pregnancy, human chorionic gonadotropin has a structural similarity with thyroid-stimulating hormone (TSH), which allows stimulating thyroid function.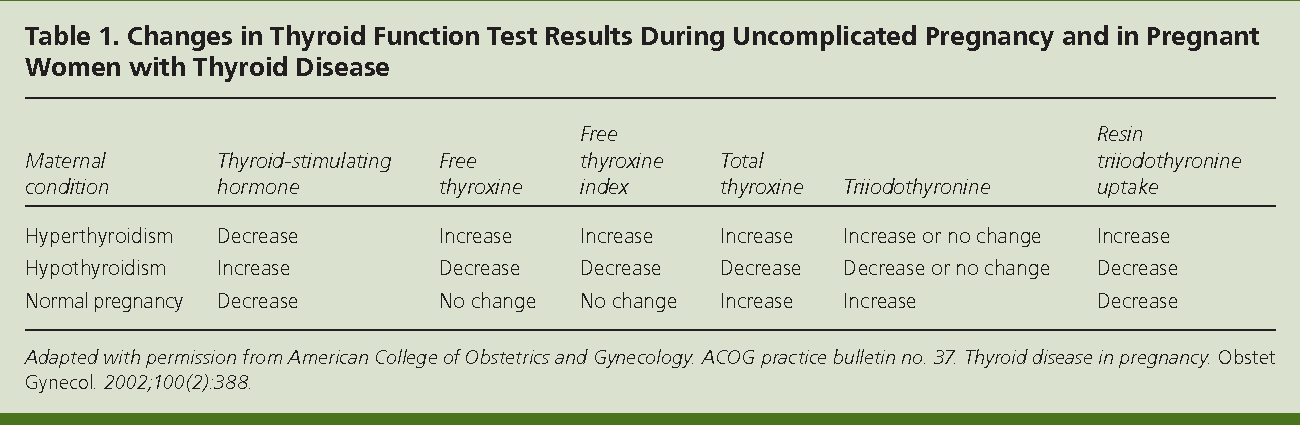 From its influence, the level of the hormone T4f increases. and the level of TSH decreases, up to the development of gestational thyrotoxicosis with clinical manifestations. The next mechanism for stimulating thyroid function is an increase in the formation of thyroxin-binding globulin (TSG) under the influence of placental estrogens, which leads to an increase in blood levels of T3 and total T4, resulting in the level of T4f. decreases, stimulating the production of TSH levels and further stimulation of the thyroid gland.
From its influence, the level of the hormone T4f increases. and the level of TSH decreases, up to the development of gestational thyrotoxicosis with clinical manifestations. The next mechanism for stimulating thyroid function is an increase in the formation of thyroxin-binding globulin (TSG) under the influence of placental estrogens, which leads to an increase in blood levels of T3 and total T4, resulting in the level of T4f. decreases, stimulating the production of TSH levels and further stimulation of the thyroid gland.
In addition, during pregnancy, as a result of increased glomerular filtration and renal clearance of iodine, the transplacental transfer of iodine to the fetus, a relative iodine deficiency develops in the woman's body, which also helps to stimulate the function of the thyroid gland.
It is known that in the first trimester the thyroid gland of the fetus is just being formed, and its development will be carried out exclusively under the influence of the mother's thyroid hormones.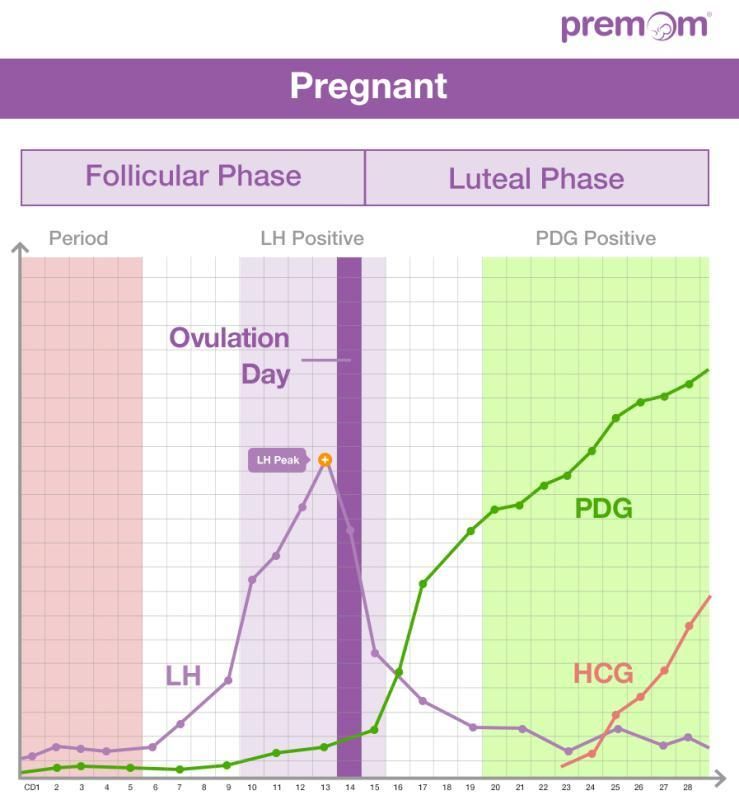 The presence of both overt and subclinical hypothyroidism in the mother can have irreversible consequences for the development of the fetus and its brain functions.
The presence of both overt and subclinical hypothyroidism in the mother can have irreversible consequences for the development of the fetus and its brain functions.
Study aims to evaluate the prevalence of changes in thyroid function in pregnant women.
Materials and methods: study of the level of thyroid hormones TSH and T4f. was conducted in 414 pregnant women aged 18 to 38 years who were registered in the first trimester, and in 98 pregnant women who were registered in the second trimester. The examination was carried out in the clinical diagnostic laboratory of the municipal budgetary healthcare institution "Clinical Diagnostic Center" of the Health Department of the Administration of Khabarovsk.
Statistical analysis was carried out using a package of standard statistical programs: Office 2000 and Statistica 6.0 for Windows.
Results and discussion
The functional activity of the thyroid gland according to the literature is determined by the level of TSH: euthyroid - TSH 0.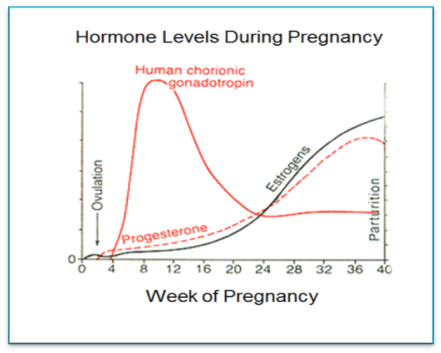 4–4.0 µIU/ml; hyperthyroid - TSH less than 0.4 μIU / ml; hypothyroid - TSH more than 4.0 μIU / ml. For the correct interpretation of laboratory parameters reflecting the activity of the thyroid gland, the combined determination of the level of TSH and free T4 is important. The determination of total T4 and T3 is not informative, since during pregnancy their levels are always increased by 1.5 times
4–4.0 µIU/ml; hyperthyroid - TSH less than 0.4 μIU / ml; hypothyroid - TSH more than 4.0 μIU / ml. For the correct interpretation of laboratory parameters reflecting the activity of the thyroid gland, the combined determination of the level of TSH and free T4 is important. The determination of total T4 and T3 is not informative, since during pregnancy their levels are always increased by 1.5 times
The study showed (table 1) that in 45.6% of the total number of pregnant women examined in the first trimester, the level of TSH and free T4 remained within the normal range. In other cases, there was a deviation in the level of TSH and T4sv. both in combination and for each type of hormones from established norms (Table 2). So the level of TSH in the first trimester of pregnancy was reduced in combination with an increased level of free T4 in 39.6% of the total number of women examined. In 12% of pregnant women out of the total number of those examined, an increase in the level of TSH was noted above the norm without a change in the level of free T4, in 2.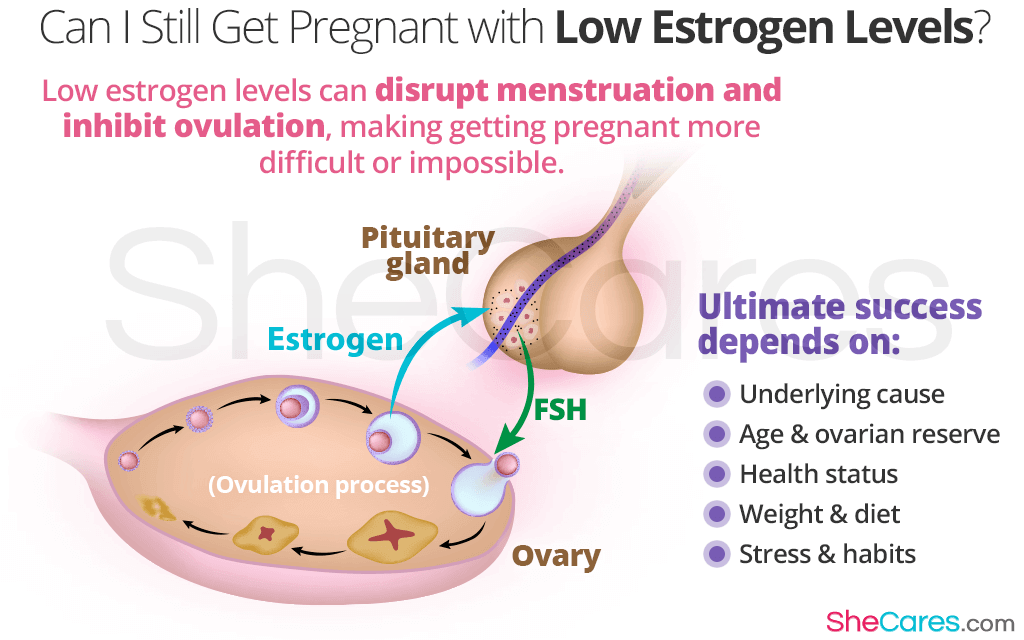 8% of cases there was an isolated decrease in the level of free T4.
8% of cases there was an isolated decrease in the level of free T4.
Thus, depending on the state of thyroid function, three groups of women were identified: the first group of women in a euthyroid state, the second group - a group of women with increased thyroid function, the third group of women with reduced thyroid function.
The average TSH level in women in the second group was 0.08±0.01 μIU/ml, free T4 - 29.2±0.8 pmol/l. This condition was regarded as transient gestational thyrotoxicosis due to the production of chorionic gonadotropin by the placenta. When examining women, dynamic monitoring of them, it was noted that the change in thyroid function was not manifested by clinical signs of thyrotoxicosis, was not accompanied by vomiting, the level of free T4 on average exceeded the normal value by 1.2 times, therefore, treatment with thyreostatics was not prescribed.
During the re-examination in the second trimester, there was a normalization of indicators characterizing the function of the thyroid gland.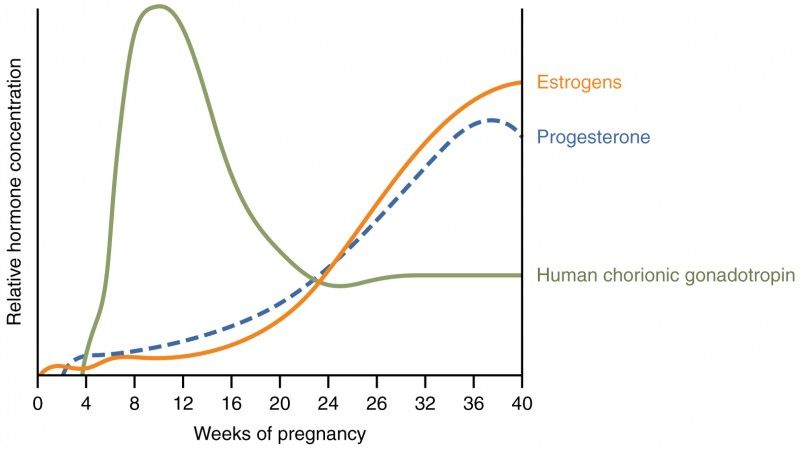 The average TSH level in women of this group was 0.4±0.08 μIU/ml, free T4 - 21±0.7 pmol/l.
The average TSH level in women of this group was 0.4±0.08 μIU/ml, free T4 - 21±0.7 pmol/l.
The average TSH level in women in the third group was 5.1±0.09 μIU/ml, free T4 level was 18±0.04 pmol/l. This condition was regarded as subclinical hypothyroidism, in connection with which the women were prescribed levothyroxine replacement therapy with maintenance of TSH levels in the first trimester up to 2.5 µIU/ml, in the second trimester up to 3 µIU/ml.
Among women registered for pregnancy in the second trimester (Table 3), in 93.9% of the total number of studies, the level of TSH and free T4 was within normal limits. The average level of TSH was 1.2±0.04 µIU/ml, free T4 was 19.2±0.4 pmol/l.
In 6.1% of cases, an elevated TSH level was noted with free T4 levels within the normal range. The average TSH level in women of this group was 4.9±0.08 µIU/ml, free T4 level was 16.7±0.07 pmol/l. This group of women was prescribed l-thyroxine at a dose that allows maintaining the recommended TSH level within 3 µIU/ml.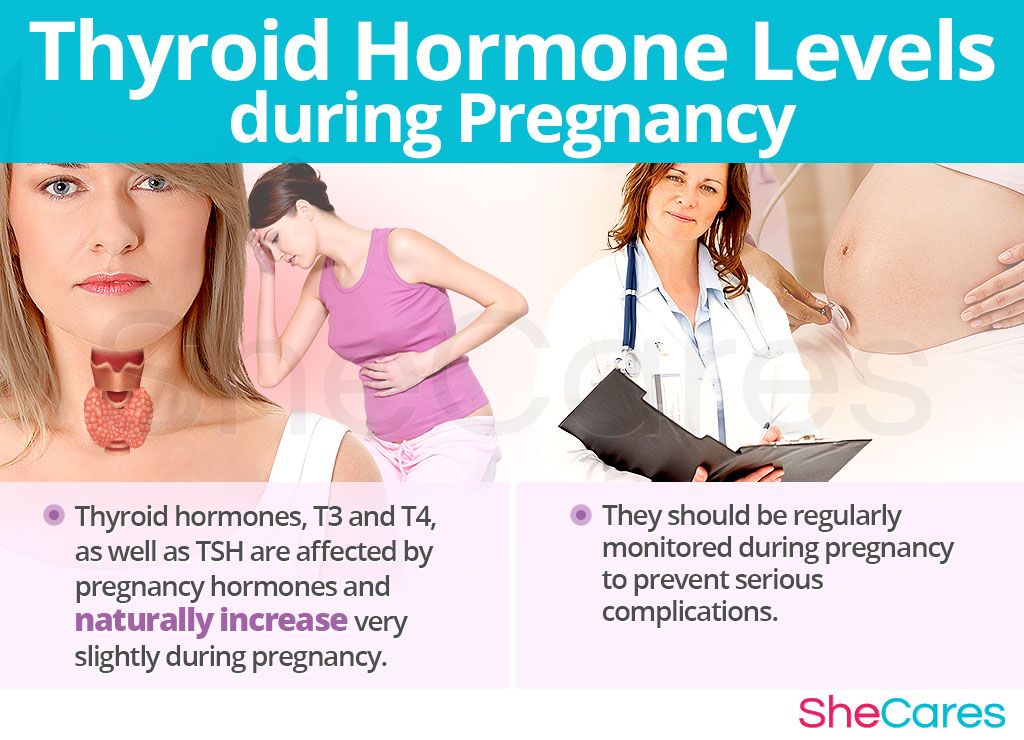
Subsequently, in women receiving replacement therapy with l-thyroxine, a deviation during pregnancy, childbirth was not observed.
For a full-fledged physiological adaptation of the thyroid gland during pregnancy, due to the developing iodine deficiency state, all women were prescribed potassium iodide at a dose of mcg per day for preventive purposes.
Conclusions:
- Pregnancy is a provoking factor in the development of changes in thyroid function. At 396% of cases in the first trimester develop transient gestational thyrotoxicosis.
- In the second trimester of pregnancy in women with transient gestational thyrotoxicosis in the first trimester, thyroid function returns to normal.
- The combination of hypothyroidism and pregnancy is relatively rare. When examining pregnant women according to the MBUZ CDC, hypothyroidism was detected in 12% of cases among pregnant women.
References:
1. Dedov I.I. Melnichenko G.A., Pronin V.S. and others. Clinic and diagnosis of endocrine disorders: Educational and methodological guide. - M., 2005.
Dedov I.I. Melnichenko G.A., Pronin V.S. and others. Clinic and diagnosis of endocrine disorders: Educational and methodological guide. - M., 2005.
2. Dedov I.I., Melnichenko G.A., Andreeva V.N. Rational pharmacotherapy of diseases of the endocrine system and metabolic disorders: A guide for practitioners / Ed. ed. I.I. Dedova, G.A. Melnichenko. - M.: Litera, 2006.
3. Sviridov N.Yu. Questions of therapy of hypothyroidism // Russian Medical Journal - 2012 - No. 13 - p. 633 – 637.
4. Helen E. Turner, John A.H. Wass. Oxford Handbook of Endocrinology and Diabetes. second edition. Oxford, University Press - 2009- P.1-83.
5. Nohr S.B., Laurberg P. Opposite variations in maternal and neonatal thyroid function induced by iodine supplementation during pregnancy // J. Clin. Endocrinol. Metab. - 2000 - Vol. 85-P. .
Table 1
Values of thyroid hormone levels in pregnant women in the first trimester (n=414)
| TSH ˂ 0. | TSH 04-4 µIU/ml | TSH ˃ 4 µIU/ml | T4 St. 10-23.2 pmol/l | T4sv. ˃23.2 pmol/l | T4 St. ˂ 10 pmol/l | ||||||
| Abs. | % | Abs. | % | Abs. | % | Abs. | % | Abs. | % | Abs. | % |
| 164 | 39.6 | 189 | 45.6 | 49 | 12 | 189 | 45.6 | 164 | 39.6 | 12 | 2.8 |
Table 2
Structure of changes in thyroid hormone levels in pregnant women registered in the first trimester (n=414)
 2 µIU/mL
2 µIU/mL