Swollen ankle rash
Swollen Legs and Ankles with Red Blotches - Blog
In This Article:
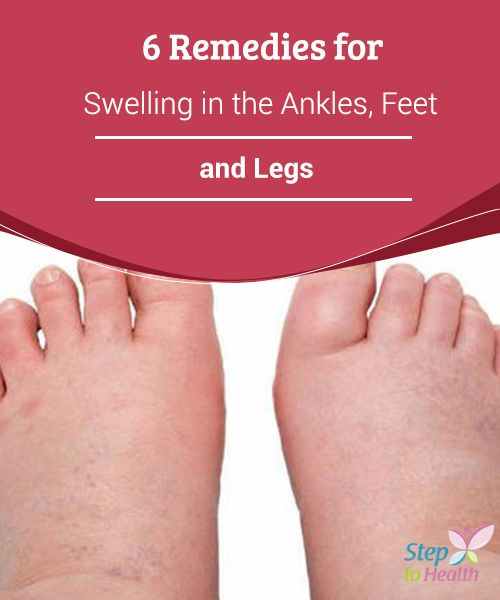
- If you have swollen legs and ankles, especially if you work on your feet, it could be a sign of edema. Edema is a condition in which fluid builds up in certain tissues of the body, namely in the arms and legs.
- Edema can be caused by temporary water retention issues, vein blockage, valve problems, muscle pump failure, adverse effects of a medication or an allergic reaction. It can also appear as a symptom of a more serious disease.
- To prevent leg and ankle swelling, wear loose-fitting clothing and shoes, get enough exercise, limit your salt intake and wear support stockings.
Swollen Legs and Ankles: When to Visit the Doctor
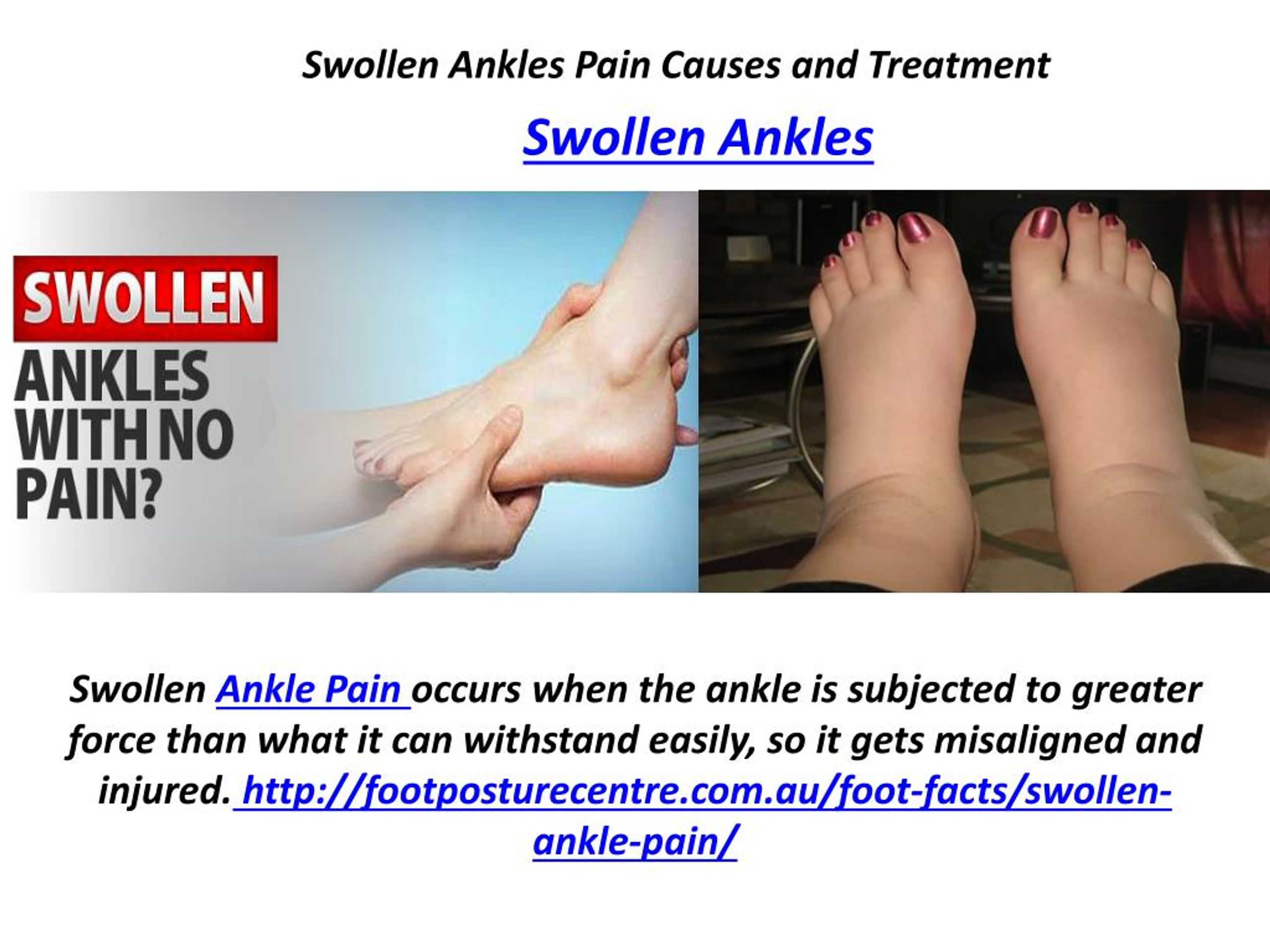
If you’ve begun to notice an abnormal amount of swelling in your legs and ankles, you may want to schedule an appointment with your primary care physician. Swollen legs and ankles along with red blotchy skin can occur for a variety of reasons, but several may require examination and treatment.
If you have swollen legs and ankles, especially if you frequently work on your feet all day, it could be a sign of what’s called edema. Edema is a condition in which fluid builds up in certain tissues of the body, most commonly in the hands, arms, ankles, legs and feet in what’s known as peripheral edema. According to the National Institute of Health, signs of edema include:
- Swelling in your lower extremities, feet, ankles, and legs
- Swelling in your upper extremities, hands and arms
- Swelling in your face or abdomen
- Skin that is puffy, shiny, or looks slightly dented after being pressed
- Shortness of breath, a cough, or irregular heartbeat
- Clothing and jewelry feels tightened
Edema itself can be attributable to a variety of causes. Some more serious than others. It’s important to see a doctor and check what is causing it to make sure it gets treated correctly.
Edema can be caused by:
- Temporary water retention issues that should take care of itself
- A symptom of a more serious disease that requires treatment
- An obstruction or blockage in the veins, such as from a tumor or deep vein thrombosis.

- A problem with the valves in the veins.
- A muscle pump failure due to inactivity, neuromuscular disease, aging, arthritis, or sedentary lifestyle, such as being on your feet for long periods of time.
- Adverse effects of medication or an allergic reaction
Make an appointment with your healthcare provider right away if you begin to notice swelling stretched or shiny red skin and pain. Helping your doctor answer questions about your medical and life history can help them make an accurate diagnosis.
Factors that can play a role in affecting your circulation can include diabetes, liver or kidney disease, high blood pressure, obesity, multiple pregnancies, heart disease and more. Even work/living conditions can play a role, whether it be standing or sitting all day. Call 911 immediately if you experience
- Shortness of breath
- Difficulty breathing
- Chest pain
Steps to Prevent Swollen Legs and Ankles
If you do experience symptoms of edema, make an appointment with your primary care physician before attempting any treatment. Your doctor may make the following recommendations:
Your doctor may make the following recommendations:
Get more comfortable
Wearing more loose-fitting clothing and shoes can help ease swelling. Additionally, try to avoid being in the same position all day, in other words, don’t be on your feet all day and don’t sit all day. When laying down, elevate your feet with a pillow.
Light exercise
Your doctor may also recommend light exercise to help improve your leg circulation. This can include walking, stretching or bicycling. However, you may not be advised to walk or stand too much.
Limit salt
Avoiding salty and high-fat foods such as bacon, chips or french fries can help lower your risk of high blood pressure.
Support stockings
Support stockings help to support your veins and muscles in the lower legs, thus assisting with your lower leg circulation. You should put the stockings on first thing in the morning before your legs start to swell.
For more information about swollen legs and ankle treatment, make an appointment with your primary care physician. Call 1 (833) VLLYWSE to make an appointment today.
Call 1 (833) VLLYWSE to make an appointment today.
Sources:
1. https://www.ncbi.nlm.nih.gov/books/NBK279409/
Quick Tip
NowDo you suffer from one or more of the edema symptoms listed above? Don’t wait to seek help — the sooner you get treatment the better. Schedule a virtual or in-person appointment today!
Book an Appointment
Find a Location
About the Author
This website uses cookies to improve your experience. We’ll assume you’re ok with this but you can opt-out. Accept Reject Learn More
Stasis Dermatitis and Ulcers: Causes, Symptoms, and Prevention
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission. Here’s our process.
Healthline only shows you brands and products that we stand behind.
Our team thoroughly researches and evaluates the recommendations we make on our site. To establish that the product manufacturers addressed safety and efficacy standards, we:
To establish that the product manufacturers addressed safety and efficacy standards, we:
- Evaluate ingredients and composition: Do they have the potential to cause harm?
- Fact-check all health claims: Do they align with the current body of scientific evidence?
- Assess the brand: Does it operate with integrity and adhere to industry best practices?
We do the research so you can find trusted products for your health and wellness.
Read more about our vetting process.What is stasis dermatitis?
Stasis dermatitis is skin inflammation that develops in people with poor circulation. It most often occurs in the lower legs because that’s where blood typically collects.
When blood collects or pools in the veins of your lower legs, the pressure on the veins increases. The increased pressure damages your capillaries, which are very small blood vessels. This allows proteins to leak into your tissues.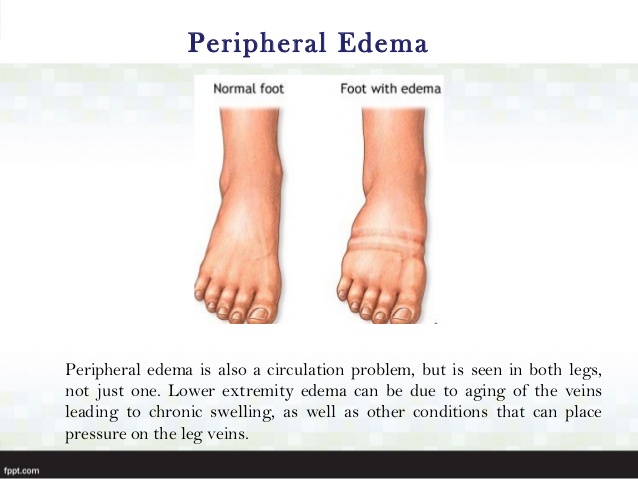 This leakage leads to a buildup of blood cells, fluid, and proteins, and that buildup causes your legs to swell. This swelling is called peripheral edema.
This leakage leads to a buildup of blood cells, fluid, and proteins, and that buildup causes your legs to swell. This swelling is called peripheral edema.
People with stasis dermatitis usually experience swollen legs and feet, open sores, or itchy and reddish skin.
One theory is that a protein called fibrinogen may be responsible for the changes you see in your skin. When fibrinogen leaks into your tissues, your body converts it to the active form of the protein, which is called fibrin. As it leaks out, the fibrin surrounds your capillaries, forming what are known as fibrin cuffs. These fibrin cuffs may prevent oxygen from entering your tissues. And when your cells don’t receive enough oxygen, they can become damaged and die.
The symptoms of stasis dermatitis include:
- skin discoloration
- itching
- scaling
- ulcers
You may also experience symptoms of venous insufficiency, including:
- leg swelling
- calf pain
- calf tenderness
- a dull ache or heaviness in your legs that gets worse when you stand
In the early stages of stasis dermatitis, the skin on your legs may look thin. Your skin may also itch, but try not to scratch it. Scratching can cause the skin to crack and fluid to seep out.
Your skin may also itch, but try not to scratch it. Scratching can cause the skin to crack and fluid to seep out.
Over time, these changes can become permanent. Your skin may eventually thicken, harden, or turn dark brown. This is called lipodermatosclerosis. It may also look lumpy.
In the final stages of stasis dermatitis, your skin breaks down and an ulcer, or sore, forms. Ulcers from stasis dermatitis usually form on the inside of your ankle.
Poor circulation causes stasis dermatitis. Typically, poor circulation is the result of a chronic (long-term) condition called venous insufficiency. Venous insufficiency occurs when your veins have trouble sending blood to your heart.
There are one-way valves inside your leg veins that keep your blood flowing in the right direction, which is toward your heart. In people with venous insufficiency, these valves become weak. This allows blood to flow back toward the feet and pool in your legs instead of continuing to flow toward your heart.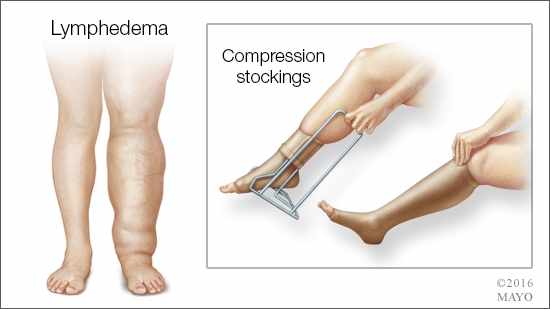 This pooling of blood is what causes stasis dermatitis.
This pooling of blood is what causes stasis dermatitis.
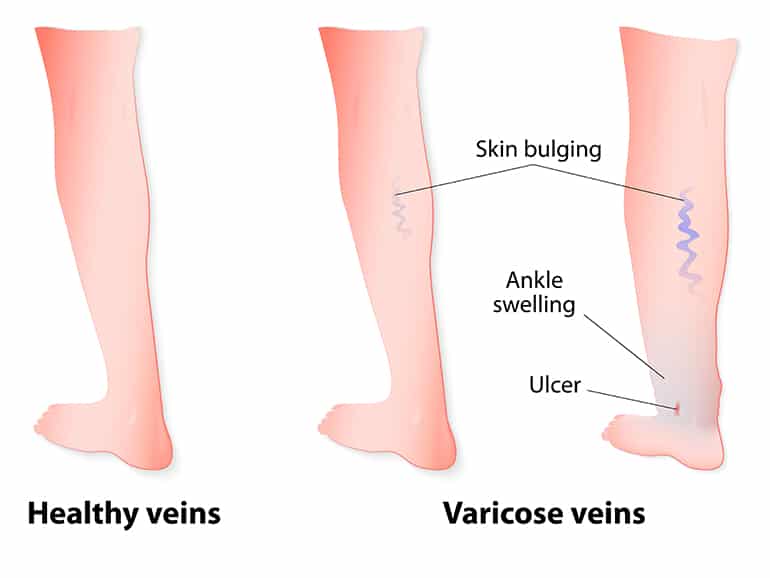
Varicose veins and congestive heart failure are also known causes of leg swelling and stasis dermatitis.
Most of the conditions that cause stasis dermatitis usually develop in people as they get older. However, there are also several causes that are unrelated to age, including:
- surgery, such as using a leg vein for bypass surgery
- deep vein thrombosis in your leg
- traumatic injury to your lower legs
Stasis dermatitis affects people with poor circulation. It’s common among adults over the age of 50. Women are more likely to get it than men.
A number of diseases and conditions can increase your risk for developing stasis dermatitis, including:
- high blood pressure
- venous insufficiency (occurs when your veins have difficulty sending blood from your legs to your heart)
- varicose veins (swollen and enlarged veins that are visible under your skin)
- congestive heart failure (occurs when your heart doesn’t pump blood efficiently)
- kidney failure (occurs when your kidneys can’t remove toxins from your blood)
- obesity
- injury to your lower legs
- numerous pregnancies
- deep vein thrombosis in your leg (a blood clot in your leg vein)
Your lifestyle can also affect your risk. You may be at a higher risk of getting stasis dermatitis if you:
You may be at a higher risk of getting stasis dermatitis if you:
- are very overweight
- don’t get enough exercise
- sit or stand without moving for long periods of time
See your doctor if you notice leg swelling or any symptoms of stasis dermatitis, especially if the symptoms include:
- pain
- redness
- open wounds or ulcers
- pus-like drainage
You can connect to a primary care doctor in your area using the Healthline FindCare tool.
To diagnose stasis dermatitis, your doctor will closely examine the skin on your legs. Your doctor may also order a venous Doppler ultrasound. This is a noninvasive test that uses sound waves to check the blood flow in your legs.
There are several things you can do at home to help treat stasis dermatitis:
- Avoid standing and sitting for long periods of time.
- Prop up your feet when sitting.
- Wear compression stockings.
- Wear loose-fitting clothing to avoid irritating your skin.

Shop online for compression stockings.
Ask your doctor about the types of skin creams and ointments you can use. Avoid using the following products:
- lanolin
- calamine and other lotions that dry your skin
- topical antibiotic ointments such a neomycin, due to possible allergic reactions
- benzocaine and other numbing medications
Your doctor might tell you to put wet bandages on your skin and might prescribe topical steroid creams and ointments. Your doctor may also prescribe antibiotics if your skin becomes infected. Surgery may be recommended to correct varicose veins if they become painful.
Treating conditions that cause venous insufficiency (such as high blood pressure and congestive heart failure) can also help control your stasis dermatitis.
If it’s left untreated, stasis dermatitis can result in:
- chronic leg ulcers
- osteomyelitis, which is a bone infection
- a bacterial skin infection, such as abscesses or cellulitis
- permanent scarring
Stasis dermatitis is usually the result of a chronic illness, such as congestive heart failure, so it’s difficult to prevent if you’re already ill.
However, you can reduce your risk by preventing the swelling in your legs (the peripheral edema) that causes it.
You can also lower your risk by exercising. Exercise is a great way to improve your circulation and reduce your body fat. Limiting the amount of sodium you consume can also help.
Rash in a child on the body, legs, back
We treat children according to the principles of evidence-based medicine: we choose only those diagnostic and treatment methods that have proven their effectiveness. We will never prescribe unnecessary examinations and medicines!
Make an appointment via WhatsApp
Prices Doctors
The first children's clinic of evidence-based medicine in Moscow
No unnecessary examinations and medicines! We will prescribe only what has proven effective and will help your child.
Treatment according to world standards
We treat children with the same quality as in the best medical centers in the world.
The best team of doctors in Fantasy!
Pediatricians and subspecialists Fantasy - highly experienced doctors, members of professional societies. Doctors constantly improve their qualifications, undergo internships abroad.
Ultimate treatment safety
We made pediatric medicine safe! All our staff work according to the strictest international standards JCI
We have fun, like visiting best friends
Game room, cheerful animator, gifts after the reception. We try to make friends with the child and do everything to make the little patient feel comfortable with us.
You can make an appointment by calling or by filling out the form on the website
Other Pediatric services
- Pediatrician's consultation
- Child Health Management Program
Frequent calls
- Acute bronchiolitis in children: diagnosis and treatment
- SARS
- Angina streptococcal tonsillitis
- Frequently ill child
- Intestinal infections
- Pneumonia (pneumonia) in children
- Colic
- Feeding problems
- Prolonged cough in a child: diagnosis and treatment
- Acute bronchitis in children: diagnosis and treatment
- Pneumonia (pneumonia) in children: diagnosis and treatment
- False croup in a child
- Coxsackie virus in a child
- The child was bitten by a tick! What to do?
Online payment
Documents online
Online services
How to reduce the risk of developing lymphedema in the legs
This information tells you how to reduce the risk of developing lymphedema in the legs.
About Lymphedema
Lymphedema is a condition of swelling that can develop in the legs after a lymph node has been removed or injured. Lymph nodes are small, bean-shaped structures found throughout the body. They drain fluid from different parts of your body. The impossibility of outflow of fluid leads to tissue edema.
Your pelvic lymph nodes were removed during surgery to get rid of any remaining cancer cells. This increases the risk of developing lymphedema in the legs. The risk is higher if you have had radiation therapy or had lymph nodes removed in your groin. If you only have lymph nodes removed in your pelvis, you are less likely to develop lymphedema in your legs.
Lymphedema may develop immediately after surgery or years later.
back to top of pageRisk factors for leg lymphedema
Risk factors for developing lymphedema in the legs include:
- weight gain or overweight;
- infection of the affected leg;
- pelvic radiotherapy;
- recurrence of cancer.

There are other factors that seem to increase this risk. These include:
- Sedentary lifestyle.
- Flying in an airplane.
- Compression of the leg. It occurs when there is a tight pressure ring in one area of the leg and is often caused by wearing certain clothing.
- Exposure to extreme temperatures.
How to reduce the risk of developing lymphedema
It is impossible to predict which patient will develop lymphedema, but there are preventive measures that reduce the risk of developing it.
Protect the skin
One of the steps to reduce the risk of developing lymphedema is to protect the skin as much as possible from injury or infection. This is due to the fact that cells begin to enter the affected area that fight infection, which, in turn, causes swelling. The legs may simply not be able to handle this extra fluid.
Treat cuts and scrapes
- Wash area with soap and water.
- Apply first aid ointment.
- Place a clean, dry gauze or bandage over the top (Band-Aid ® ).
Treat burns
- Wrap an ice pack in a towel and apply to the burn for 15 minutes. You can also rinse the burn with cold water.
- Wash area with soap and water.
- Apply first aid ointment.
- Place a clean, dry gauze pad or bandage over the top.
Watch for signs of infection, which include:
- redness;
- edema;
- heating surrounding tissues;
- sensitivity.
Call your doctor or nurse if you have these symptoms.
Do not wear tight clothing
Do not wear tight clothing that leaves deep marks on your legs, such as socks or sweatpants with elastic cuffs. Wear loose-fitting clothing that won't leave marks on your feet.
Compression garments that prevent severe swelling work differently. It provides uniform pressure on the leg and the correct flow of fluid through it. You can learn more about compression stockings in the Compression Stockings section of this resource.
You can learn more about compression stockings in the Compression Stockings section of this resource.
Avoid exposure to extreme temperatures
Extreme heat and cold can cause fluid to accumulate in the leg and cause swelling. Avoid or reduce your time in hot tubs or saunas.
Be careful when flying
If you are at risk of developing lymphedema, air travel is associated with certain negative factors, including:
- Cabin pressure. Aircraft cabin pressure is usually slightly less than ground pressure. Because of this, the skin is stretched and fluid can accumulate in the legs.
- Sitting still for long periods of time. If you don't move for a long period of time, fluid can build up in your legs.
- Lifting and carrying luggage can cause muscle strain.
- Dehydration (when your body doesn't get the amount of water it needs).
Here are a few tips to help reduce your risk of developing lymphedema:
- Buy a seat with adequate legroom, such as a front seat.
- Ask for help carrying, lifting or removing luggage that is too heavy for you.
- Get up and walk up and down the aisle of the aircraft if possible.
- While sitting, do simple exercises with your feet and ankles. Exercise throughout the flight will help restore circulation and movement of the lymphatic fluid. You can try the following exercises:
- Point your toes towards the ceiling and then lower towards the floor.
- Circle your feet in one direction and then in the other.
- Wear loose-fitting clothing.
- Drink plenty of fluids to avoid dehydration.
- Do not eat salty foods.
- Ask your doctor if you need to take a prescription for antibiotics with you when you travel.
Other ways to reduce risk
- Do not give injections (shots) or acupuncture in the affected leg(s).
- Do not use sharp pedicure tools. Use a cuticle remover and file your nails instead of trimming them.

- Moisturize frequently to avoid flaking and cracking.
- Keep the area between your toes clean and dry to prevent infections.
- Don't go barefoot.
- Make sure your shoes fit your foot to avoid blisters.
- Keep your toe rings or ankle bracelets loose.
- Try to sit cross-legged as little as possible.
- Choose a sunscreen with an SPF of at least 30 to protect your skin from sunburn.
- Try not to gain weight, as being overweight is one of the risk factors for developing lymphedema. If you are overweight, try to lose weight.
- Limit your salt intake. Its use can lead to edema, which will lead to an excessive load on the lymphatic system.
How to recognize the first signs of lymphedema
After surgery, all patients develop swelling at the site of the incision (surgical suture). This is normal and goes away a few weeks after surgery.
Swelling due to lymphedema usually occurs in the lower leg(s).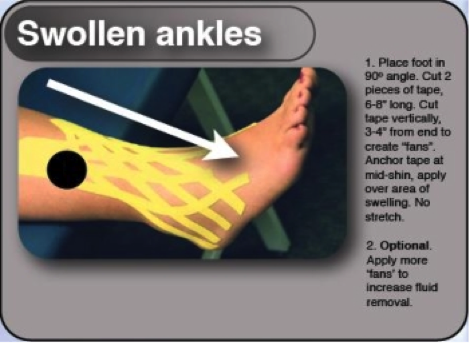 If left untreated, it can spread throughout the leg all the way to the torso. At first, such edema may appear and disappear. It may decrease when you raise your leg above your chest.
If left untreated, it can spread throughout the leg all the way to the torso. At first, such edema may appear and disappear. It may decrease when you raise your leg above your chest.
Other early symptoms may include a feeling of heaviness in the leg(s) or a feeling that clothes, socks or shoes are crushing you.
back to top of pageLymphedema Treatment
As the lymphedema progresses, the swelling will stay longer or not go away at all. Raising your legs up may help in the beginning, but this method will eventually stop working. At this stage, you will need the help of a lymphedema therapist. This therapy is called complex anti-edematous therapy.
It includes:
- wearing a brace;
- manual lymphatic drainage;
- compression stockings;
- skin care;
- physical activity.
wearing a brace;
A bandage is a special tight bandage for your legs. Wearing a bandage is not for everyone. If you need to put on a bandage, this can be done in various ways. You will discuss them with your therapist and choose the best one for you.
You will discuss them with your therapist and choose the best one for you.
manual lymphatic drainage;
Manual lymphatic drainage (MLD) is a gentle massage. It removes fluid from your feet to where it can be more easily processed by your body. MLD is performed in a certain sequence, depending on which lymph nodes are removed. Your therapist will tell you which manual lymphatic drainage sequence is right for you.
compression stockings;
Compression stockings help the lymphatic system function more efficiently. Some people choose to wear them to reduce their risk of developing lymphedema. It is important to choose the right stockings. Incorrectly selected stockings can cause the development of lymphedema.
- Make sure that the stockings do not irritate or leave marks on the skin. It's best to have a lymphedema therapist fit your stockings. This way you can be sure that they are right for you.
- We recommend wearing light compression stockings.
 Light compression stockings will be marked with a pressure of 15 to 20 mmHg. If swelling increases, you may need higher compression stockings.
Light compression stockings will be marked with a pressure of 15 to 20 mmHg. If swelling increases, you may need higher compression stockings. - Compression stockings come in different heights, they can reach the knee, thigh or be in the form of pantyhose.
skin care;
Keep your skin clean and moisturized. This is important to reduce the risk of infection. The risk of developing lymphedema is lower if you don't have leg infections.
Exercise
Light exercise such as walking is a great way to get fluids moving more efficiently through your body. Try to walk every day if possible.
We list some exercises that will help you maintain flexibility and strength. Before you start exercising, check with your doctor.
If your doctor approves, do the exercises once a day. Stop doing them if you feel pain, discomfort, weakness (unusually very tired or weak), or if you notice swelling.
The video below will help you learn how to do these exercises and stretches.
Deep breathing
To stimulate fluid movement, start with deep breathing. Take no more than 3 deep breaths at a time to avoid dizziness.
Walking in place
- Sit in a chair with your feet flat on the floor.
- Slowly raise 1 knee without tilting or leaning back (see Figure 1).
- Lower your leg and place your foot back on the floor.
- Repeat 10-15 times.
- Do this exercise for the other leg.
Figure 1. Walking in place
Sitting leg swing
- Sit on a chair. Place your feet on the floor.
- Swing 1 foot forward from the floor so that it is extended in front of you (see picture 2).
- Stay in this position while counting out loud to 5.
- Lower your foot to the floor.
- Repeat 10-15 times.
- Do this exercise for the other leg.
Fig. 2 Leg swings in sitting position
Ankle Alphabet
Move your feet as if you were writing the letters of the alphabet (see figure 3). Write letters with each foot at least 2 times.
Write letters with each foot at least 2 times.
Figure 3. Ankle alphabet
Stretching
As you recover, you will be able to do stretching exercises. They will help relax the muscles of the legs and hips. The time you can do these exercises will depend on the type of surgery you had. Do these stretching exercises only when your doctor confirms that it is safe to do so.
Calf Stretch
- Sit with your legs straight.
- Place a towel around the ball of your foot (see Figure 4).
- Gently pull the towel without bending your knee.
- Hold this position for 30 seconds.
- Repeat 5 times. Then do the exercise for the other leg.
Figure 4 Calf Stretch
Hamstring Stretch
- Sit with your legs straight.
- Reach to touch your toes, keeping your knees and back straight (see Figure 5).
- Hold this position for 30 seconds.
- Repeat 5 times.
Figure 5 Hamstring Stretch
Hip Stretch
- Lie on your back with your knees bent.
- Cross your legs and pull on the leg closest to your chest (see figure 6).
- Hold this position for 30 seconds.
- Repeat 5 times. Then do a stretch for the other leg.
Figure 6 Hip Stretch
Other treatments for lymphedema
There are other treatments for lymphedema. Discuss with your doctor or lymphedema therapist which ones are right for you.
Other treatments for lymphedema include:
- Scar treatment. Scars left after surgery can make it harder for your body to get rid of fluid. Scar treatment helps to soften the area around the scar and make it less tight. It will help drain fluid from your feet.
- Posture improvement.
- Use of kinesiology tape for athletes.
Call your doctor or nurse if you have:
- a temperature of 100.4°F (38°C) or higher;
- chills;
- a new or incomprehensible type of pain or tenderness in the legs or feet;
- increased feeling of warmth in the legs around the affected skin;
- redness of the leg(s) or foot that does not go away;
- more severe swelling of the legs(s) or feet;
- feeling of heaviness in the legs, which does not stop within 1 week.
Appointment
To make an appointment with a lymphedema therapist, contact your PCP. Together they will decide which lymphedema therapy is right for you. After your doctor gives you a referral, you will be contacted to make an appointment. If you have any questions, call the Rehabilitation Service at 212-639-7833.
Lymphedema therapy is available at several Memorial Sloan Kettering centers. See www.mskcc.org/cancer-care/diagnosis-treatment/symptom-management/rehabilitation/medicine-therapy for more information.
To find a lymphedema therapist in your area, you can go to the following websites:
Klose Training
www.klosetraining.com
Norton School of Lymphatic Therapy therapy)
www.nortonschool.com
Academy of Lymphatic Studies
www.acols.com
Lymphatic Association of North America (9004 052) 9004 902 .