Cow milk intolerance in babies
What should I do if I think my baby is allergic or intolerant to cows' milk?
If you think your baby is having a reaction to cows' milk, see your GP or health visitor to discuss your concerns.
They will be able to assess if your baby's symptoms may be caused by a cows' milk allergy or something else. Make sure you get medical advice before taking cows' milk out of your child's diet as it contains important nutrients.
Cows' milk allergy in babies
Cows' milk allergy (CMA), also called cows' milk protein allergy, is one of the most common childhood food allergies. It is estimated to affect around 7% of babies under 1, though most children grow out of it.
CMA typically develops when cows' milk is first introduced into your baby's diet either in formula or when your baby starts eating solids.
More rarely, it can affect babies who are exclusively breastfed because of cows' milk from the mother's diet passing to the baby through breast milk.
There are 2 main types of CMA:
- immediate CMA – where symptoms typically begin within minutes of having cows' milk
- delayed CMA – where symptoms typically begin several hours, or even days, after having cows' milk
Symptoms of cows' milk allergy
Cows' milk allergy can cause a wide range of symptoms, including:
- skin reactions – such as an itchy rash or swelling of the lips, face and around the eyes
- digestive problems – such as stomach ache, vomiting, colic, diarrhoea or constipation
- hay fever-like symptoms – such as a runny or blocked nose
- eczema that does not improve with treatment
Occasionally CMA can cause severe allergic symptoms that come on suddenly, such as swelling in the mouth or throat, wheezing, cough, shortness of breath, and difficult, noisy breathing.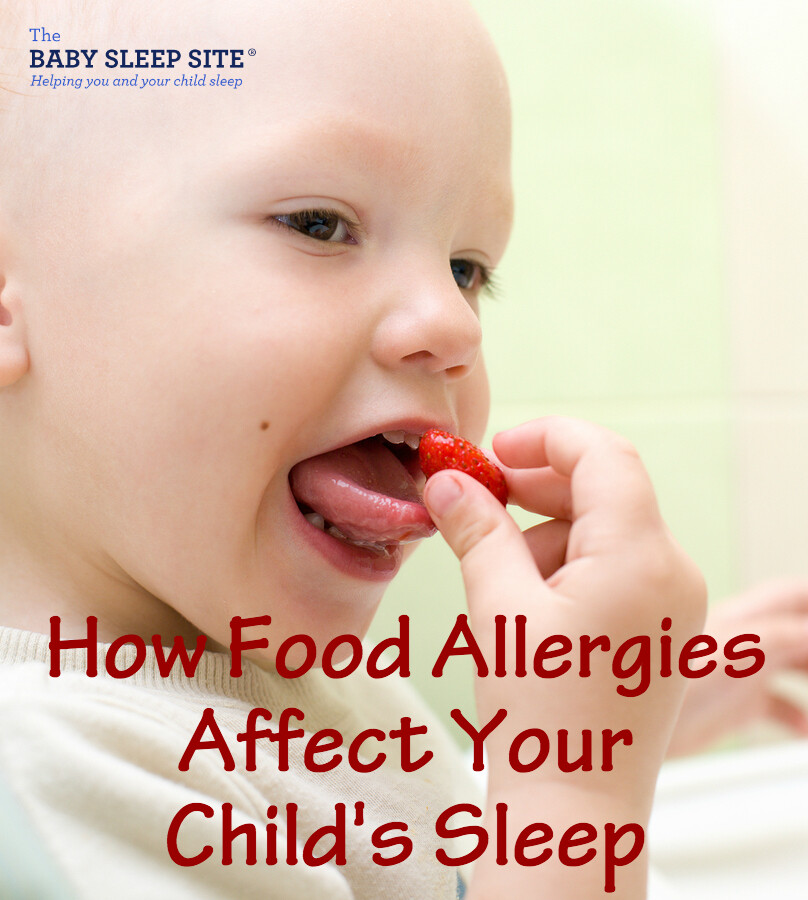
A severe allergic reaction (anaphylaxis) is a medical emergency. Call 999 for an ambulance immediately if you think your child has anaphylaxis (even if they start to feel better).
Treatment for CMA
If your baby is diagnosed with CMA, you'll be offered advice by your GP or an allergy specialist on how to manage their allergy. You may also be referred to a dietitian.
Treatment involves removing all cows' milk from your child's diet for a period of time.
If your baby is formula-fed, your GP can prescribe special infant formula.
Do not give your child any other type of milk without first getting medical advice.
If your baby is exclusively breastfed, the mother will be advised to avoid all cows' milk products.
Your child should be assessed around every 6 to 18 months to see if they have grown out of their allergy.
Read more about cows' milk allergy in children on National Institute for Health and Care Excellence (NICE).
Could it be lactose intolerance?
Lactose intolerance is another type of reaction to milk, when the body cannot digest lactose, a natural sugar found in milk. However, this is not an allergy.
Lactose intolerance can be temporary – for example, it can come on for a few days or weeks after a tummy bug.
Symptoms of lactose intolerance include:
- diarrhoea
- vomiting
- stomach rumbling and pains
- wind
Treatment for lactose intolerance
Treatment depends on the extent of your child's intolerance. Some children with lactose intolerance may be able to have small amounts of dairy products without having symptoms.
Your child may be referred to a dietitian for specialist advice.
Read more about treatment for lactose intolerance.
Further information:
- Colic
- Food allergies in babies and children
- Reflux in babies
- How can I tell if my baby is seriously ill?
- Your baby's first solid foods
- National Institute for Health and Care Excellence (NICE): food allergy in children
Page last reviewed: 28 November 2022
Next review due: 28 November 2025
Milk intolerance in babies and children
Milk intolerance in babies and children | Pregnancy Birth and Baby beginning of content6-minute read
Listen
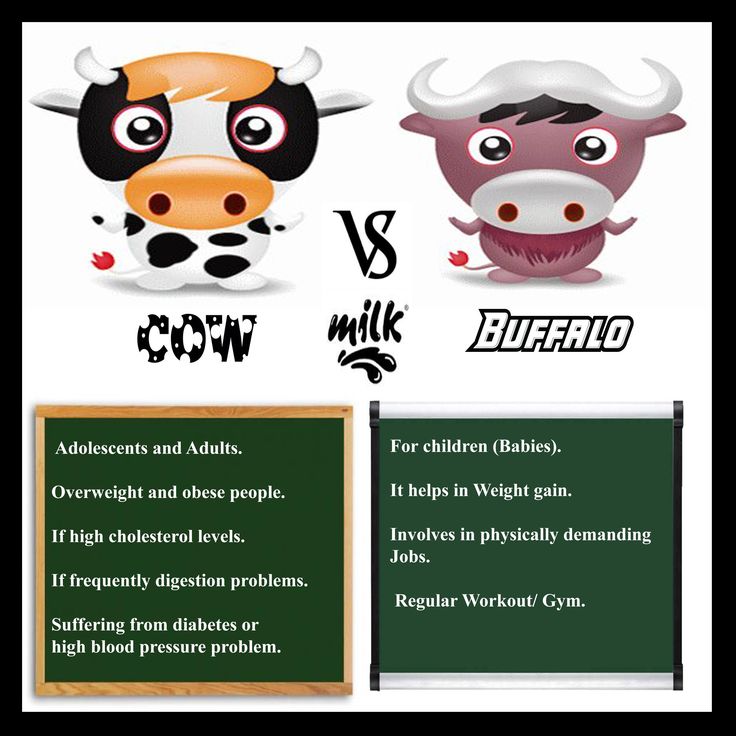
Some babies and children have a reaction when they drink cow's milk or formula made from cow's milk. This could be due to 2 things: a lactose intolerance or an allergy to milk. If your child has one of these conditions, you will have to alter their diet to cut down on milk or avoid it altogether.
This could be due to 2 things: a lactose intolerance or an allergy to milk. If your child has one of these conditions, you will have to alter their diet to cut down on milk or avoid it altogether.
Call triple zero (000) for an ambulance if your child has the following symptoms. They could be having a severe allergic reaction and will need urgent medical attention.
- wheezing or difficulty breathing
- a swollen tongue
- vomiting
- they are pale and floppy or unconscious
What is milk intolerance and milk allergy?
Around 1 in 10 young children has a reaction when they drink cow's milk. This could be because they have a lactose intolerance or a milk allergy. Milk allergy is much more common than lactose intolerance in children under 5.
Lactose intolerance is a problem with the digestive system – it means your child doesn't have the enzyme needed to digest lactose, which is the sugar in milk.
Milk allergy, however, is a problem with the immune system — the body reacts to the protein in milk. An allergy usually involves other parts of the body as well as the stomach, and may cause symptoms such as a skin rash or swelling of the face.
An allergy usually involves other parts of the body as well as the stomach, and may cause symptoms such as a skin rash or swelling of the face.
Your doctor can confirm whether your child is lactose-intolerant or has a milk allergy by doing some medical tests. Don't use unproven tests such as Vega, kinesiology, Alcat or allergy elimination tests for children. A milk intolerance is very unlikely to be the cause of mucus or coughing.
Many young children grow out of their intolerance or allergy. But don't start giving them cow's milk until your doctor tells you it's safe to do so.
Lactose intolerance
Causes
Lactose is the sugar found in the milk produced by all mammals, including humans. Sometimes people don't produce enough of the enzyme lactase in their gut to break down the lactose.
Very few babies have true lactose intolerance, a rare genetic condition where they're born without any lactase enzymes at all. (This is called primary lactose intolerance).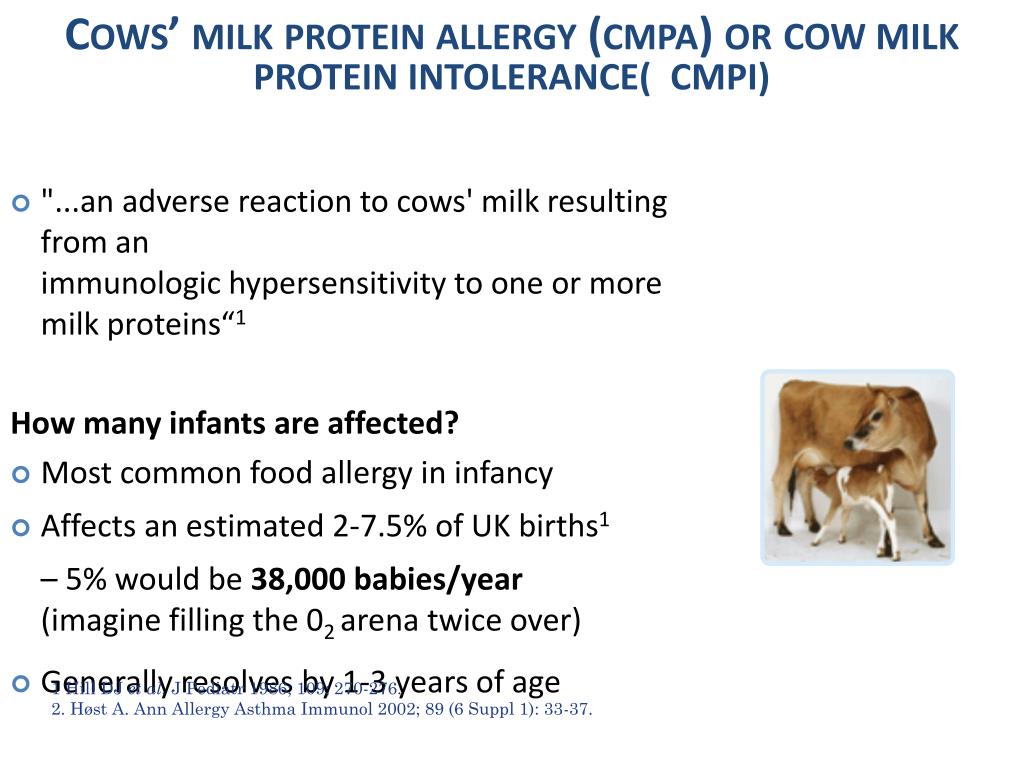 However, many people develop lactose intolerance later in life, after the age of 5. It is more common in Aboriginal Australians and people from Asia, Africa, the Middle East and some Mediterranean countries.
However, many people develop lactose intolerance later in life, after the age of 5. It is more common in Aboriginal Australians and people from Asia, Africa, the Middle East and some Mediterranean countries.
Babies and young children can become intolerant to milk if the lining of their gut is damaged by an illness such as gastroenteritis, or an allergy or intolerance to another food. This is called secondary lactose intolerance and will go away once the gut heals, usually over a few months.
Symptoms and diagnosis
The symptoms of lactose intolerance in babies and children are:
- liquid, sometimes green, frothy stools
- being irritable
- stomach aches
- bloating
- passing a lot of gas
- not putting on weight
- nappy rash
All of these symptoms are common in babies and don't necessarily mean they have lactose intolerance. But if your child has diarrhoea and isn't putting on weight, see your doctor. Don't stop breastfeeding unless your doctor tells you to.
Tests include a breath test to measure the hydrogen in your child's breath, or cutting out dairy to see if their symptoms improve. This is known as an elimination diet.
Treatment
If the lactose intolerance is caused by a tummy upset, keep on breastfeeding. If your baby is formula fed, talk to your doctor or child and family health nurse before switching to low-lactose or lactose-free formula.
Older children will need to cut down on, but not eliminate, dairy foods from their diet. They can still have some cheeses, yogurt, calcium-fortified soy products, lactose-free milk, butter and cream. Your doctor or a dietitian will advise you on the best diet for your child.
Cow's milk allergy
Cow's milk allergy is one of the most common food allergies in young children. It usually disappears by the time they reach school age. It occurs when your child's immune system reacts to the protein in milk.
Symptoms and diagnosis
Reactions to milk can occur within minutes or not for several days.
Rapid reactions include:
- hives (urticaria)
- swelling of the lips, face or eyes
- stomach pain
- vomiting
- diarrhoea
- noisy breathing or wheezing
- a swollen tongue
- a swollen or tight throat
- a hoarse voice
- change in consciousness or floppiness in babies or young children
Delayed reactions include:
- an increase in eczema
- blood or mucus in stools
- vomiting and/or diarrhoea 2-24 hours after having milk
It is very important to see a doctor if your child has the symptoms of milk allergy. The condition is diagnosed using the history of symptoms or can sometimes be confirmed with an allergy test.
Treatment
If your child is allergic to milk, you need to completely remove dairy products from their diet. Follow your doctor's or allergy specialist's advice and read food labels carefully. You may also need to avoid milk from other animals, such as goats, as well as coconut milk products. Watch out for other words used to describe milk on food labels, such as butter, buttermilk, cream, curd, ghee, milk, cheese, dairy, milk solids, whey, yoghurt, casein and caseinates.
Watch out for other words used to describe milk on food labels, such as butter, buttermilk, cream, curd, ghee, milk, cheese, dairy, milk solids, whey, yoghurt, casein and caseinates.
If your baby is formula-fed, you can use soy protein formula (unless they are also allergic to soy), extensively hydrolysed formula (EHF) or amino acid-based formula (AAF). Do not use formula made from cow's milk, goat's milk, sheep milk, HA, A2 milk or lactose-free.
If your child is over the age of one, they can be given soy milk, calcium-enriched rice, and oat or nut milks. It is important to make sure they are getting enough calcium.
You may be advised to carry an Epipen adrenaline autoinjector if your child is allergic to milk. Severe allergic reactions can sometimes lead to anaphylaxis, which is serious and can even be fatal. An adrenaline autoinjector can be used to give first aid in the event of anaphylaxis.
Breastfeeding a baby who can't tolerate milk
If your baby is lactose-intolerant, you don't need to change your diet. It doesn't matter how much dairy you consume, the amount of lactose in your milk will be the same.
It doesn't matter how much dairy you consume, the amount of lactose in your milk will be the same.
However, if your baby is diagnosed with milk allergy, you will need to remove all dairy from your own diet too. You will need calcium and vitamin D supplements every day. Your doctor or allergy specialist will advise you.
Where to seek more help
Don't try to deal with milk intolerance yourself. You can get help from:
- your doctor
- Pregnancy, Birth and Baby on 1800 882 436
- Australasian Society of Clinical Immunology and Allergy
- Australian Breastfeeding Association on 1800 686 268
Sources:
Australasian Society of Clinical Immunology and Allergy (Cow's milk (dairy) allergy), Australasian Society of Clinical Immunology and Allergy (Infant Feeding and Allergy Prevention Clinical Update), Australian Breastfeeding Association (Lactose intolerance and the breastfed baby), Raising Children Network Australia (Lactose intolerance: babies, children and teenagers), Royal Children’s Hospital (Allergy and Immunology), Sydney Children’s Hospitals Network (Allergy - Milk allergy and milk-free diet)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: July 2020
Back To Top
Related pages
- Reactions to food
- How to introduce allergy foods
- Airborne allergies
Need more information?
Lactose intolerance - MyDr.com.au
Lactase deficient people do not have enough lactase, the enzyme that helps break down lactose and they suffer from lactose intolerance. The main symptoms of lactose intolerance are bloating and wind.
Read more on myDr website
Lactose intolerance - Better Health Channel
Symptoms of lactose intolerance include bloating, gas, abdominal pain and diarrhoea.
Read more on Better Health Channel website
ASCIA Guide for Milk Substitutes in Cow’s Milk Allergy - Australasian Society of Clinical Immunology and Allergy (ASCIA)
Guide for Milk Substitutes in Cow’s Milk Allergy
Read more on ASCIA – Australasian Society of Clinical Immunology and Allergy website
Allergy - Cow's milk allergy and milk free diet | Sydney Children's Hospitals Network
How common is cow’s milk allergy? Cow’s milk allergy is one of the most common food allergies in childhood affecting about 1-2% of preschool children
Read more on Sydney Children's Hospitals Network website
Cow's milk (dairy) allergy | Dietitians Australia
Cow's milk allergy is common in babies and children, and symptoms can range from mild to severe.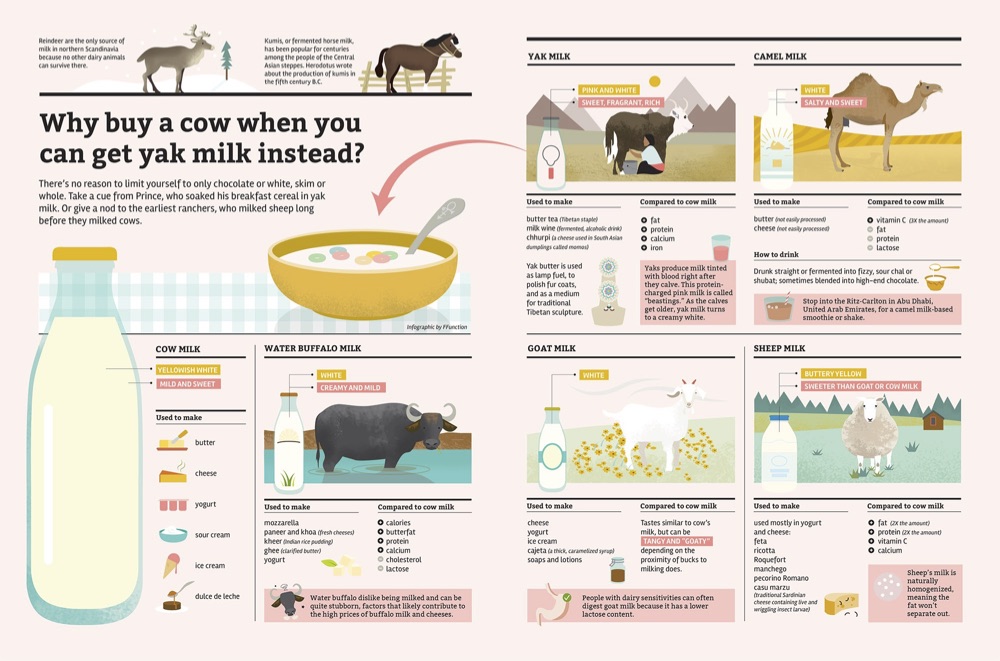 Avoiding cow's milk and other dairy-containing foods is the only effective way to manage a cow's milk allergy, but it's important to seek specialist advice.
Avoiding cow's milk and other dairy-containing foods is the only effective way to manage a cow's milk allergy, but it's important to seek specialist advice.
Read more on Dietitians Australia website
Cow’s milk allergy - Better Health Channel
Milk allergy symptoms range from mild to a life-threatening severe allergic reaction. Avoid food containing milk only under strict medical supervision
Read more on Better Health Channel website
Food allergy versus food intolerance - MyDr.com.au
A food allergy is an immune response triggered by eating specific foods that cause certain well known symptoms to develop.
Read more on myDr website
Cow`s milk (dairy) allergy - Australasian Society of Clinical Immunology and Allergy (ASCIA)
Cow's milk is a common cause of food allergy in infants. In Australia and New Zealand around 2 per cent (1 in 50) infants are allergic to cow's milk and other dairy products. Although most children outgrow cow's milk allergy by the age of 3-5 years, in some people cow's milk allergy may not resolve.
In Australia and New Zealand around 2 per cent (1 in 50) infants are allergic to cow's milk and other dairy products. Although most children outgrow cow's milk allergy by the age of 3-5 years, in some people cow's milk allergy may not resolve.
Read more on ASCIA – Australasian Society of Clinical Immunology and Allergy website
Food intolerances: children & teenagers | Raising Children Network
Food intolerance symptoms in children and teens include bloating, diarrhoea and stomach pain. If you think your child has food intolerance, talk to your GP.
Read more on raisingchildren.net.au website
Food intolerance - Australasian Society of Clinical Immunology and Allergy (ASCIA)
Around 1 in 20 infants and 1 in 100 adults are allergic to food. Severe reactions result in difficulty breathing, severe rashes, swelling of the face or throat, dizziness, stomach upset or a drop in blood pressure (shock) and loss of consciousness.
Severe reactions result in difficulty breathing, severe rashes, swelling of the face or throat, dizziness, stomach upset or a drop in blood pressure (shock) and loss of consciousness.
Read more on ASCIA – Australasian Society of Clinical Immunology and Allergy website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.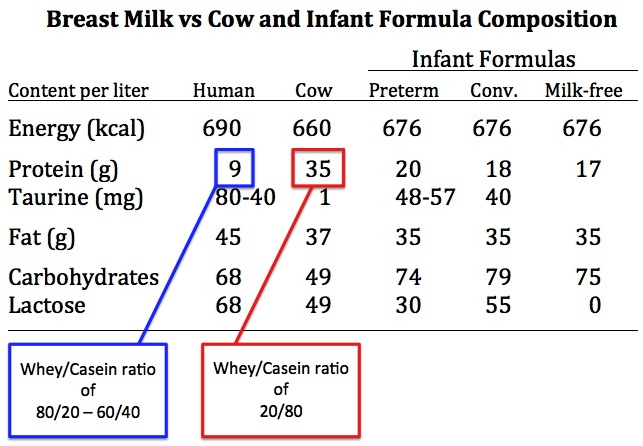
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Allergy to cow's milk proteins (CMP)
- Nestlé Health Science
- health care
- The concept of "Allergy to cow's milk proteins (CMP)"
The concept of "Allergy to cow's milk proteins (CMP)"
What is food allergy?
Food allergies occur when the body's immune system (the body's own defense mechanism) reacts incorrectly to certain foods. Normally, the immune system helps the body fight harmful things, such as infectious agents. In a food allergy, the immune system misrecognizes certain food components as harmful, leading to unpleasant and sometimes life-threatening allergy-related signs and symptoms.
Normally, the immune system helps the body fight harmful things, such as infectious agents. In a food allergy, the immune system misrecognizes certain food components as harmful, leading to unpleasant and sometimes life-threatening allergy-related signs and symptoms.
More than 120 foods are known to cause food allergies. Cow's milk protein allergy (CMP) is the most common type of food allergy in infants under one year of age.
Do not confuse CMPA with lactose intolerance
Sometimes CMPA is confused with lactose intolerance. Both diseases have some common signs and symptoms, but different causes and treatments.
CMPA usually develops at an early age, while lactose intolerance is extremely rare before the age of 5 years.
What is ABKM?
CMA is a type of food allergy in which the child's immune system reacts to proteins found in cow's milk. As a result, the child develops allergy symptoms: skin problems (rash, hives, dry, flaky or itchy skin), digestive system disorders (diarrhea, vomiting, constipation and reflux) and respiratory problems (noisy breathing, cough, runny nose). CMPA usually occurs before a child's first birthday.
CMPA usually occurs before a child's first birthday.
What is lactose intolerance?
Unlike CMPA, lactose intolerance does not depend on the immune system. This is actually lactase deficiency, the inability to digest the lactose sugar found in cow's milk, and is very rare in children under 5 years of age. Lactose is one of the most important carbohydrates (sugars) in breast milk and is very beneficial for babies. Lactose promotes healthy intestinal flora and calcium absorption.
Cow's milk protein allergy and lactose intolerance are different diseases
learn more about cow's milk protein allergy
All about CMPA
How common is CMPA?
Is CMPA hereditary?
Why does my child have CMPA?
Can CMPA be cured?
What is the difference between the AAA line and hypoallergenic formulas?
Your steps towards the diagnosis of CMPA
Allergy symptoms can be frightening, but CMPA can be easily managed with the right diet, so it's important to get the right diagnosis from your doctor and get treatment on time. If you notice any symptoms in your child that could be associated with CMPA, first of all, don't worry. Discuss the problems with the doctor, the doctor will take the necessary actions to make a final diagnosis. Follow the links below for information and guidance regarding the diagnosis of CMPA and the common signs and symptoms of CMPA.
If you notice any symptoms in your child that could be associated with CMPA, first of all, don't worry. Discuss the problems with the doctor, the doctor will take the necessary actions to make a final diagnosis. Follow the links below for information and guidance regarding the diagnosis of CMPA and the common signs and symptoms of CMPA.
SIGNS AND SYMPTOMS OF CMPA
CMPA is a food allergy, but symptoms can affect more than just the digestive system, they can also affect the respiratory system and skin.
Learn more about the signs and symptoms of CMPA
Symptom Analysis
Diagnosis
To make a diagnosis, the doctor will examine the child and ask about any symptoms you may notice. If an allergy to cow's milk proteins is suspected, a doctor may do certain tests. Once diagnosed, the symptoms of CMPA can be easily managed under the experienced guidance of a physician.
Find out more about the diagnosis of CMDD
Get ready for your doctor's visit
Would you like some help preparing for your doctor's visit? By printing and completing My Child's Symptom Diary, you can be sure that your doctor will have all the information you need to make an accurate diagnosis.
Symptom diary
IMPORTANT NOTE: Breastfeeding may continue if the infant is allergic to cow's milk protein. To do this, the mother needs a special diet with the exclusion of all sources of cow's milk protein. Only if these measures do not bring the desired effect, the doctor recommends the use of a special therapeutic mixture intended for children from 0 to 1 year old. It is important to follow the correct methods of preparing the mixture: using boiled water, sterilized bottles and following the rules for diluting the mixture. Medicinal mixtures intended for diet therapy of CMPA should be used under the supervision of a physician.
Allergy to cow's milk protein in children
Food allergy is a food-induced adverse (pathological) reaction based on immune mechanisms. In children under one year of age, the most common cause of food allergy is cow's milk protein (CMP).
A distinction is made between cow's milk protein allergy and cow's milk protein intolerance. In the first case immune mechanisms are involved, in the second case — the baby simply does not have enough enzymes to digest cow's milk protein (for example, lactase deficiency).
There are only 36 cow's milk protein allergens, but 4 of them most often cause food allergies.
Casein is 80% BCM, it is thermostable (does not break down when boiled) and is not a species-specific protein. This means that if you are allergic to it, you may be allergic to the milk of other animal species.
This means that if you are allergic to it, you may be allergic to the milk of other animal species.
β - lactoglobulin has the highest allergenic activity, species-specific, not destroyed by boiling. This protein is not found in human milk.
α - lactalbumin is destroyed by boiling, species-specific.
Bovine serum albumin is not destroyed by boiling, if an allergy to this cow's milk protein is detected, the child may also react to beef and veal meat.
It should be noted that mainly children who are bottle-fed with mixtures based on cow's milk protein suffer from an allergy to cow's milk protein.
This type of allergy can also develop in children who are breastfed - if the diet of a nursing mother contains products containing cow's milk protein (milk, cheese, cottage cheese, sour cream, butter, fermented milk products), especially in large quantities.
What symptoms suggest that the baby may be allergic to CMP:
- Skin manifestations (dry skin, dry nummular rashes, skin itching).
- Gastrointestinal manifestations (bloating, regurgitation, vomiting, loose stools, possibly mucus and blood-streaked stools).
- Respiratory manifestations (itchy eyes, cough, nasal congestion and even urticaria and Quincke's edema). These symptoms are rare in toddlers, but still possible.
Diagnosis
I must say that if the first manifestations of food allergy in a baby appeared after switching to artificial feeding with a "regular" adapted formula based on cow's milk, then this is a reason to suspect cow's milk proteins as an allergen.
Further correct history taking : the doctor will definitely find out if anyone in your family suffers from allergic diseases (bronchial asthma, allergic rhinitis, atopic dermatitis, hay fever). If the family has these diseases, the risk of developing allergies in the baby increases.
At the doctor's discretion, it is possible to take blood from a child for the presence of immunoglobulin E (IgE) antibodies to cow's milk proteins, which were mentioned above.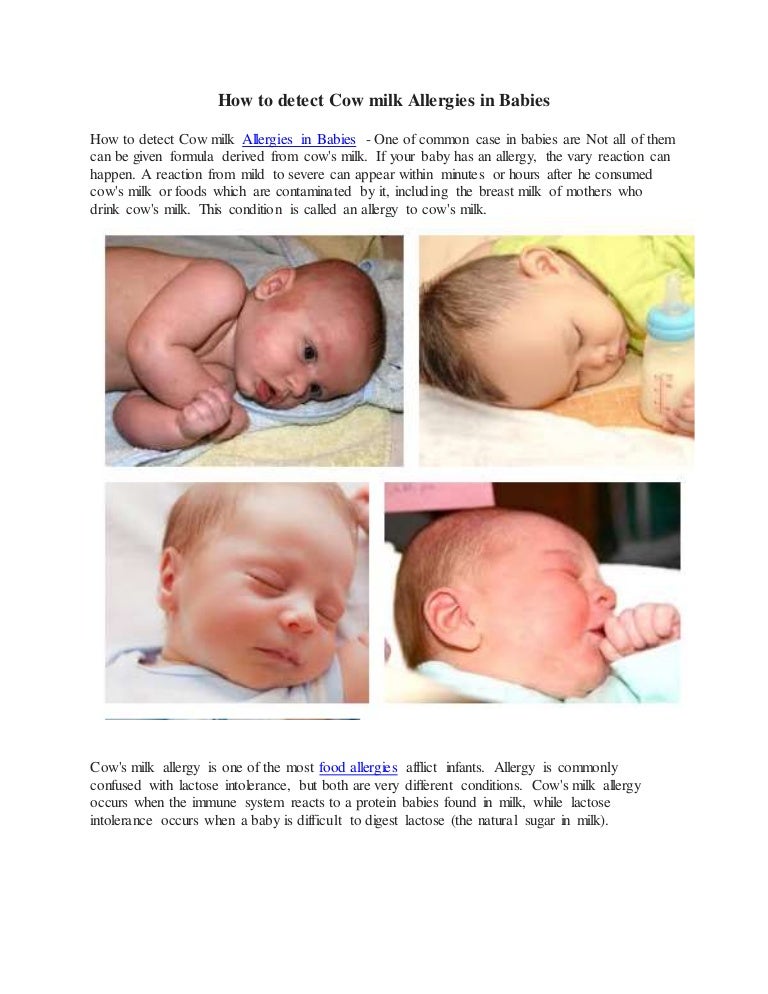 In the presence of IgE antibodies to CMP in the baby's blood, almost 100% confirms that he has an allergy. Paradoxically, the absence of these antibodies does not rule out an allergy to cow's milk proteins, but only indicates that the allergy proceeds through a different type of allergic reaction.
In the presence of IgE antibodies to CMP in the baby's blood, almost 100% confirms that he has an allergy. Paradoxically, the absence of these antibodies does not rule out an allergy to cow's milk proteins, but only indicates that the allergy proceeds through a different type of allergic reaction.
And the simplest, most important and accessible method is the diagnostic diet with the exclusion of products from the child's diet (or from the mother's diet during breastfeeding) containing CMP. The duration of this diet is from 1-2 to 4 weeks. If during these periods there is no improvement in the condition of the baby, then an allergy to CMP is unlikely.
If the child's condition improves, you may need challenge test . This means the introduction of dairy products into the child's diet again. And if the manifestations of allergies return, this will prove an allergy to BCM. This test is carried out under strict medical supervision.
In children who are fed exclusively with breast milk, it is necessary to exclude from the diet of mothers products containing CMP.
There are 3 types of mixtures:
- based on the hydrolysis of whey proteins;
- based on the hydrolysis of the casein fraction;
- based on amino acids.
Allergy is possible to the first two options, the reaction is very unlikely to the third option.
If the baby is bottle-fed, then it must be transferred to amino acid blend or highly hydrolyzed blend. Most infant formulas are made with whole proteins and are therefore not suitable for babies allergic to CMP. They also do not recommend hypoallergenic mixtures, since the protein in them is not sufficiently split and mixtures in goat's milk (cross-reactions).
Usually, allergists first transfer children to mixtures based on complete hydrolysis of BCM or casein, if there is no proper effect within 2-3 weeks, it is recommended to transfer the baby to an amino acid mixture.
Perhaps, if the child has pronounced manifestations of food allergies, the doctor will advise you to immediately transfer the baby to an amino acid mixture. By agreement with the doctor, it is possible to transfer the child to a mixture based on soy protein isolate (from 6 months).
Amino acid mixtures are more easily tolerated by children with various forms of food allergies, as they do not have the bitter taste characteristic of mixtures with a high degree of protein hydrolysis.
Amino acid mixtures can be used both for the short term diagnosis of CMP allergy and as a dietary base for long term use in children with food allergies.
Diet duration — at least 6 months . Then the issue of transferring the baby to a hypoallergenic mixture is decided. In case of recurrence of symptoms, the introduction of dairy products is postponed for another 6 months.
The prognosis for CMP allergy in infants and young children with the correct management of patients is favorable.