Spotting while pregnant third trimester
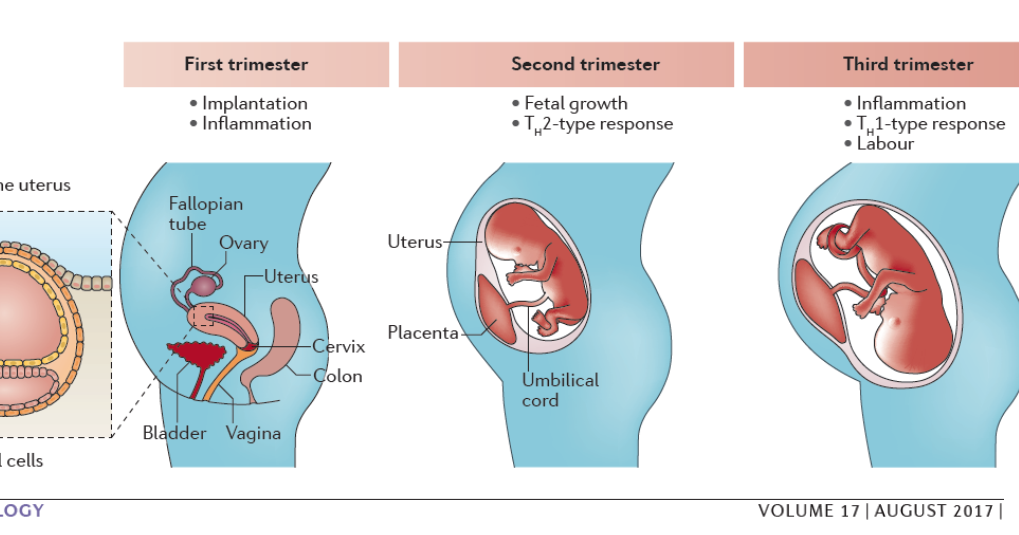
What to Expect, Fetal Development
Written by Stephanie Watson
In this Article
- What Is the Third Trimester?
- New Fetal Development
- Third Trimester Changes in Your Body
- Red Flag Symptoms
- Third Trimester Tips for Twins
What Is the Third Trimester?
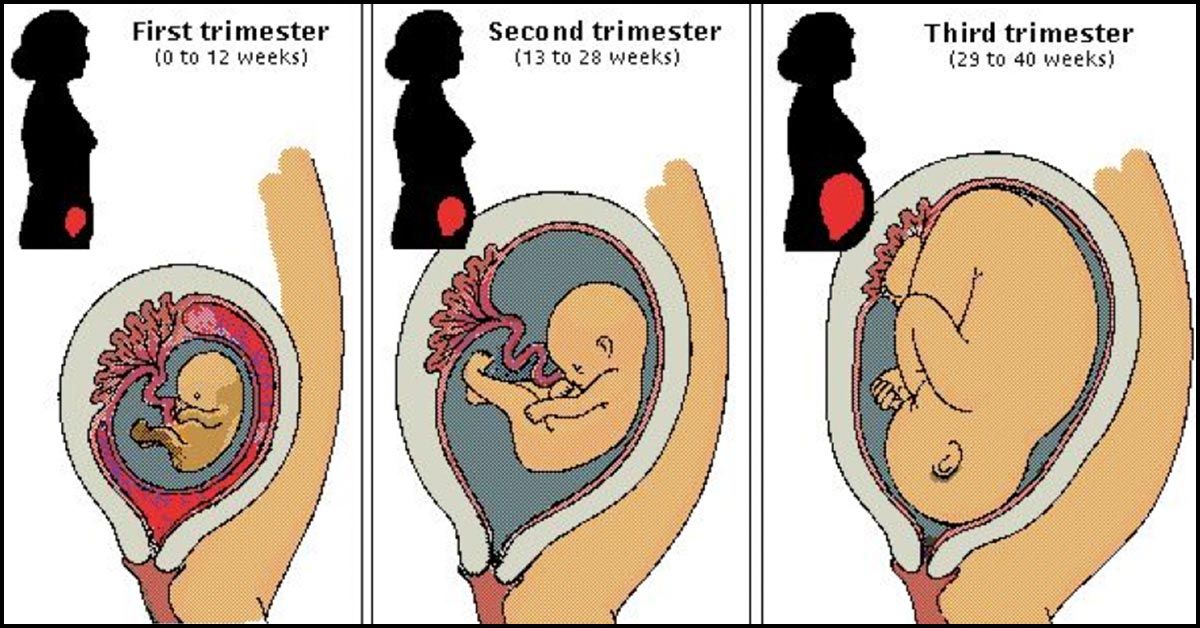
The third trimester is the last phase of your pregnancy. It lasts from weeks 29 to 40, or months 7, 8, and 9. During this trimester, your baby grows, develops, and starts to change position to get ready for birth.
Now that you've reached the third trimester, you're in the home stretch of your pregnancy. You've only got a few more weeks to go, but this part of your pregnancy can be the most challenging.
New Fetal Development
In the third trimester, your baby keeps growing. By the end, a full-term baby usually is between 19 and 21 inches long and between 6 and 9 pounds.
Your baby begins to turn itself head-down to get ready for delivery. At week 36, the baby’s head should begin to move into your pelvic area, also called lightening. It will stay in this down-facing position for the last 2 weeks of your pregnancy.
Your baby develops in other important ways in the third trimester. During this phase, it’s able to:
- Open its eyes and see
- Hear
- Suck on its thumb
- Cry
- Smile
Your baby’s brain continues to develop. Its lungs and kidneys mature. It gains muscle tone and about 16% body fat. The bones at the top of its skull are soft to ease delivery. Most babies have blue eyes at this stage, and they’ll stay that color until a few days or weeks after they’re born. It also has nails on its toes and reaching to the ends of its fingers. If it’s a boy, the testes have descended into the scrotum.
During the third trimester, the vernix caseosa, a protective coating, covers your fetus’ skin. Soft body hair called the lanugo falls out and is almost gone by the end of week 40.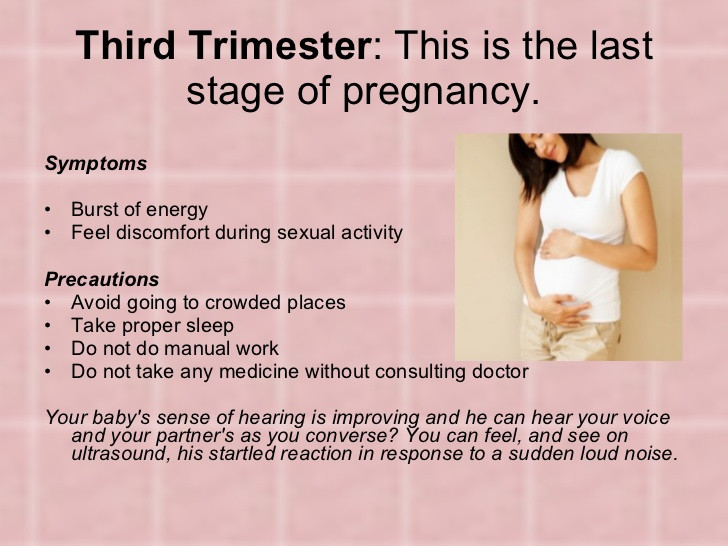
Third Trimester Changes in Your Body
- Abdominal achiness. As your baby grows, it takes up more room in your abdomen. This can cause you to have some aches and discomfort. You may find it hard to get comfortable when you’re in bed at night trying to go to sleep. You may even feel like it’s harder to take deep breaths.
- Backache. The extra weight you've gained puts added pressure on your back, making it feel achy and sore. You might also feel discomfort in your pelvis and hips as your ligaments loosen to prepare for labor. To ease the pressure on your back, try to practice good posture. Sit up straight and use a chair that provides good back support. At night, sleep on your side with a pillow tucked between your legs. Wear low-heeled, comfortable shoes with good arch support. To ease back pain, use a heating pad. Ask your doctor whether it's OK for you to take acetaminophen.
- Bleeding. Some light bleeding toward the end of your pregnancy might be a sign that labor is starting.
 But spotting may sometimes be a sign of a serious problem, including placenta previa (the placenta grows low and covers the cervix), placental abruption (separation of the placenta from the uterine wall), or preterm labor. Call your doctor as soon as you notice any bleeding.
But spotting may sometimes be a sign of a serious problem, including placenta previa (the placenta grows low and covers the cervix), placental abruption (separation of the placenta from the uterine wall), or preterm labor. Call your doctor as soon as you notice any bleeding. - Braxton-Hicks contractions. You might start to feel mild contractions, which are warm-ups to prepare your uterus for the real labor to come. Braxton-Hicks contractions often aren't as intense as real labor contractions, but they may feel a lot like labor and can eventually progress to it. One main difference is that real contractions gradually get closer and closer together -- and more intense. If you're red in the face and out of breath after your contractions, or they're coming regularly, call your doctor.
- Breast enlargement and leaking. By the end of your pregnancy, your breasts will have grown by as much as 2 pounds. Make sure you're wearing a supportive bra so your back doesn't suffer.
 Close to your due date, you may start to see a yellowish fluid leaking from your nipples. This substance, called colostrum, will nourish your baby in the first few days after birth.
Close to your due date, you may start to see a yellowish fluid leaking from your nipples. This substance, called colostrum, will nourish your baby in the first few days after birth. - Vivid dreams. It’s common to have more vivid dreams or nightmares in your third trimester. This can disrupt your sleep. Your wild dreams are likely caused by changes in hormone levels from pregnancy.
- Clumsiness. You may feel clumsy or out of balance during the third trimester. You may drop things. Part of the reason is that you’ve gained weight in your belly area. That makes it harder to balance your body.
- Discharge. You might see more vaginal discharge during the third trimester. If the flow is heavy enough to soak through your panty liners, call your doctor. Close to your delivery date, you might see a thick, clear, or slightly blood-tinged discharge. This is your mucus plug, and it's a sign that your cervix has begun dilating in preparation for labor.
 If you experience a sudden rush of fluid, it may mean that your water has broken (although only about 8% of pregnant women have their water break before contractions begin). Call your doctor as soon as possible after your water breaks.
If you experience a sudden rush of fluid, it may mean that your water has broken (although only about 8% of pregnant women have their water break before contractions begin). Call your doctor as soon as possible after your water breaks. - Fatigue. You might have been feeling energetic in your second trimester, but are weary now. Carrying extra weight, waking up several times during the night to go to the bathroom, and dealing with the anxiety of preparing for a baby can all take a toll on your energy level. Eat healthy food and get regular exercise to give yourself a boost. When you feel tired, try to take a nap, or at least sit down and relax for a few minutes. You need to reserve all your strength now for when your baby arrives and you're really not getting any sleep.
- Frequent urination. Now that your baby is bigger, its head may be pressing down on your bladder. That extra pressure means you'll have to go to the bathroom more frequently -- including several times each night.
 You might also find that you're leaking urine when you cough, sneeze, laugh, or exercise. To relieve the pressure and prevent leakage, go to the bathroom whenever you feel the urge and urinate completely each time. Avoid drinking fluids right before bedtime to cut down on unwanted late-night bathroom visits. Wear a panty liner to absorb any leakage. Let your doctor know if you have any pain or burning with urination. These can be signs of a urinary tract infection.
You might also find that you're leaking urine when you cough, sneeze, laugh, or exercise. To relieve the pressure and prevent leakage, go to the bathroom whenever you feel the urge and urinate completely each time. Avoid drinking fluids right before bedtime to cut down on unwanted late-night bathroom visits. Wear a panty liner to absorb any leakage. Let your doctor know if you have any pain or burning with urination. These can be signs of a urinary tract infection. - Heartburn and constipation. They're caused by extra production of the hormone progesterone, which relaxes certain muscles -- including the muscles in your esophagus that normally keep food and acids down in your stomach, and the ones that move digested food through your intestines. To relieve heartburn, try eating more frequent, smaller meals throughout the day and avoid greasy, spicy, and acidic foods (like citrus fruits). For constipation, increase your fiber intake and drink extra fluids to keep things moving more smoothly.
 If your heartburn or constipation is really bothering you, talk to your doctor about what medications may be safe for you to take for symptom relief.
If your heartburn or constipation is really bothering you, talk to your doctor about what medications may be safe for you to take for symptom relief. - Hemorrhoids. Hemorrhoids are actually varicose veins -- swollen veins that form around the anus. These veins enlarge during pregnancy because extra blood is flowing through them and the weight of pregnancy increases the amount of pressure to the area. To relieve the itch and discomfort, try sitting in a warm tub or sitz bath. Ask your doctor whether you can also try an over-the-counter hemorrhoid ointment or stool softener.
- Sciatica. Nerve pain that shoots from your lower back to your buttocks and down your leg is more likely in the third trimester. Sciatica may be caused by hormone changes during pregnancy, or because your baby’s growing body presses against the sciatic nerve. Sciatica pain may come and go or be constant. Yoga, massage, or physical therapy are ways to relieve the pain, but it usually goes away after your baby is born.

- Shortness of breath. As your uterus expands, it rises up until it sits just under your rib cage, leaving less room for your lungs to expand. That added pressure on your lungs can make it more difficult to breathe. Exercising can help with shortness of breath. You can also try propping up your head and shoulders with pillows while you sleep.
- Spider and varicose veins. Your circulation has increased to send extra blood to your growing baby. That excess blood flow can cause tiny red veins, known as spider veins, to appear on your skin. Spider veins may get worse in your third trimester, but they should fade once your baby is born. Pressure on your legs from your growing baby may also cause some surface veins in your legs to become swollen and blue or purple. These are called varicose veins. They should improve within a few months after you deliver. Although there's no way to avoid varicose veins, you can prevent them from getting worse by:
- Getting up and moving throughout the day
- Wearing support hose
- Propping up your legs whenever you have to sit for long periods.

- Stretch marks. You may develop stretch marks on your breasts, butt, tummy, or thighs. Stretch marks are a type of scar that happens when your skin stretches during pregnancy. Not everyone gets them. If you do, they may be red, purple, pink, or brown in color.
- Swelling. Your rings might be feeling tighter these days, and you may also notice that your ankles and face are looking bloated. Mild swelling is the result of excess fluid retention (edema). To reduce swelling, put your feet up on a stool or box whenever you sit for any length of time, and elevate your feet while you sleep. If you have sudden onset of swelling though, seek medical attention immediately as it may be a sign of preeclampsia, a dangerous pregnancy complication.
- Weight gain. Aim for a weight gain of 1/2 pound to 1 pound a week during your third trimester. By the end of your pregnancy, you should have put on a total of about 25 to 35 pounds (your doctor may have recommended that you gain more or less weight if you started out your pregnancy underweight or overweight).
 The extra pounds you've put on are made up of the baby's weight, plus the placenta, amniotic fluid, increased blood and fluid volume, and added breast tissue. If your baby seems to be too small or too big based on the size of your belly, your doctor will do an ultrasound to check the baby’s growth.
The extra pounds you've put on are made up of the baby's weight, plus the placenta, amniotic fluid, increased blood and fluid volume, and added breast tissue. If your baby seems to be too small or too big based on the size of your belly, your doctor will do an ultrasound to check the baby’s growth.
Red Flag Symptoms
Any of these symptoms could be a sign that something is wrong with your pregnancy. Don't wait for your regular prenatal visit to talk about it. Call your doctor right away if you experience:
- Severe abdominal pain or cramps
- Severe nausea or vomiting
- Bleeding
- Severe dizziness
- Pain or burning during urination
- Rapid weight gain (more than 6.5 pounds per month) or too little weight gain
Third Trimester Tips for Twins
Expecting twins? You might want to add these things to your third trimester to-do list:
- Go stroller shopping. Side-by-side or tandem? Take a few double strollers for a test drive to see which type feels best to you.
 Look for one that's easy to open and maneuver.
Look for one that's easy to open and maneuver. - Get breastfeeding tips. Breastfeeding two babies is more of a challenge than one, but you can definitely do it. Ask your doctor ahead of time for tips.
- Check your iron. Ask your doctor if you need to take iron supplements. As a mom-to-be of twins, you're four times more likely to have iron-deficiency anemia.
- Know the signs of preeclampsia. Carrying twins doubles your risk of this serious condition. Tell your doctor right away if you have a headache, trouble seeing, or sudden weight gain.
- Find a support group. Start looking for groups of moms of multiples in your area. You may appreciate exchanging tips and getting support from other moms in the same boat.
- Create a schedule. Read up on how to get your twins on the same sleeping and eating schedule.
 Learning some tips now may save your sanity when you have two newborns.
Learning some tips now may save your sanity when you have two newborns.
Health & Pregnancy Guide
- Getting Pregnant
- First Trimester
- Second Trimester
- Third Trimester
- Labor and Delivery
- Pregnancy Complications
- All Guide Topics
Vaginal bleeding in late pregnancy: MedlinePlus Medical Encyclopedia
One out of 10 women will have vaginal bleeding during their 3rd trimester. At times, it may be a sign of a more serious problem. In the last few months of pregnancy, you should always report bleeding to your health care provider right away.
You should understand the difference between spotting and bleeding:
- Spotting is when you notice a few drops of blood every now and then on your underwear. It is not enough to cover a panty liner.
- Bleeding is a heavier flow of blood. With bleeding, you will need a liner or pad to keep the blood from soaking your clothes.

When labor begins, the cervix starts to open up more, or dilate. You may notice a small amount of blood mixed in with normal vaginal discharge, or mucus.
Mid- or late-term bleeding may also be caused by:
- Having sex (most often just spotting)
- An internal exam by your provider (most often just spotting)
- Diseases or infections of the vagina or cervix
- Uterine fibroids or cervical growths or polyps
More serious causes of late-term bleeding may include:
- Placenta previa is a problem of pregnancy in which the placenta grows in the lowest part of the womb (uterus) and covers all or part of the opening to the cervix.
- Placenta abruptio (abruption) occurs when the placenta separates from the inner wall of the uterus before the baby is born.
To find the cause of your vaginal bleeding, your provider may need to know:
- If you have cramping, pain, or contractions
- If you have had any other bleeding during this pregnancy
- When the bleeding began and whether it comes and goes or is constant
- How much bleeding is present, and whether it is spotting or a heavier flow
- The color of the blood (dark or bright red)
- If there is an odor to the blood
- If you have fainted, felt dizzy or nauseated, vomited, or had diarrhea or a fever
- If you have had recent injuries or falls
- When you last had sex and if you bled afterward
A small amount of spotting without any other symptoms that occurs after having sex or an exam by your provider can be watched at home.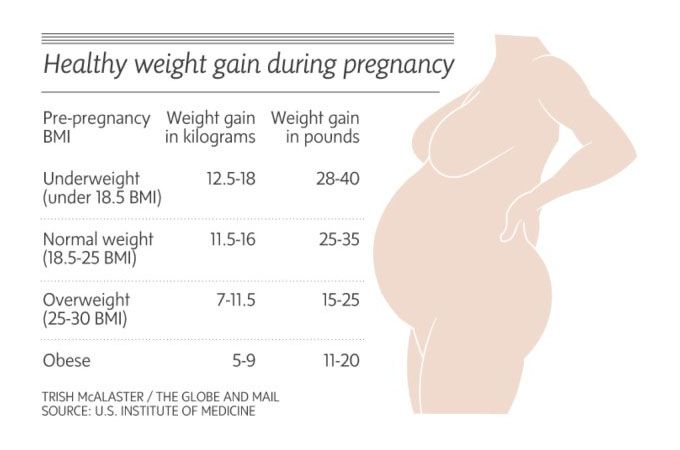 To do this:
To do this:
- Put on a clean pad and recheck it every 30 to 60 minutes for a few hours.
- If spotting or bleeding continues, call your provider.
- If the bleeding is heavy, your belly feels stiff and painful, or you are having strong and frequent contractions, you may need to call 911 or your local emergency number.
For any other bleeding, call your provider right away.
- You will be told whether to go to the emergency room or to the labor and delivery area in your hospital.
- Your provider will also tell you whether you can drive yourself or you should call an ambulance.
Baeseman ZJ. Vaginal bleeding in pregnancy. In: Kellerman RD, Rakel DP, eds. Conn's Current Therapy 2021. Philadelphia, PA: Elsevier 2021:1227-1229.
Francois KE, Foley MR. Antepartum and postpartum hemorrhage. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Philadelphia, PA: Elsevier; 2021:chap 18.
Hull AD, Resnik R, Silver RM. Placenta previa and accreta, vasa previa, subchorionic hemorrhage, and abruptio placentae. In: Resnik R, Lockwood CJ, Moore TR, Greene MF, Copel JA, Silver RM, eds. Creasy and Resnik's Maternal-Fetal Medicine: Principles and Practice. 8th ed. Philadelphia, PA: Elsevier; 2019:chap 46.
Salhi BA, Nagrani S. Acute complications of pregnancy. In: Walls RM, Hockberger RS, Gausche-Hill M, eds. Rosen's Emergency Medicine: Concepts and Clinical Practice. 9th ed. Philadelphia, PA: Elsevier; 2018:chap 178.
Updated by: John D. Jacobson, MD, Professor of Obstetrics and Gynecology, Loma Linda University School of Medicine, Loma Linda Center for Fertility, Loma Linda, CA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Browse the Encyclopedia
|
1 week 2nd week 3rd week 4 week 5 week 6 week 7 week 8 week 9 week 10 week 11 week 12 week | 3 weeks pregnant
As a child grows:
HCG is an early pregnancy test. At weeks 1-2, it reaches values of 25 - 300 mU / ml, and at 3-4 weeks 1500 - 5000 mU / ml (in non-pregnant women, hCG < 5 mU / ml).
Meanwhile, amniotic fluid begins to collect around the accumulation of blastocytes, forming the amniotic sac.
Inside the womb - implantation
Note: The development of each child in the womb may be slightly different. Our information gives you an overview of your baby's development.
How your life is changing:
Surprising facts: Early symptoms of pregnancy.
Some women feel pregnant even before the test is positive. Earliest signs include:
As tempting as it may be, don't rush to use a home pregnancy test. The vast majority of them do not work correctly on these terms. Things to do this week of pregnancy:
1. Buy a pregnancy test in case you don't have your period next week.
|
What is it? Normal and abnormal discharge during pregnancy
Today we will talk with Elena Yurievna Romanova, an obstetrician-gynecologist at the Expert Center for Pregnancy Management at the Mother and Child Clinic, about what discharges during pregnancy should be feared and what discharges from the genital tract are regarded as normal.
Increased vaginal discharge during pregnancy is natural
Normal pregnancy discharge is milky white or clear mucus without a strong odor (although the smell may change from before pregnancy), this discharge does not irritate the skin and does not cause discomfort to the pregnant woman. The discharge can have a different color - from completely colorless (most often) to whitish and yellowish. The consistency of discharge at the beginning of pregnancy resembles raw chicken yolk - they are thick, jelly-like, often released in the form of clots. nine0005
With normal discharge, it is enough to use panty liners or change underwear twice a day.
Due to the activity of progesterone in the first 12 weeks of pregnancy, the discharge will be scarce and viscous.
Due to the increase in estrogen activity from 13 weeks, the discharge becomes less viscous and more abundant.
By the end of the pregnancy, vaginal discharge becomes more and more abundant. Each time you need to evaluate the nature of the discharge, change the gasket. If the fluid continues to ooze, this may mean leakage of amniotic fluid and the need to contact an obstetrician-gynecologist in the emergency department of a hospital with a maternity ward. There are auxiliary tests, thanks to which, as well as obstetric ultrasound, leakage of water can be excluded. nine0005
Not all discharge in pregnant women is the norm.
For example, a white, thick, crumbly, odorless discharge that itchs and burns the skin and causes discomfort during intercourse is likely a sign of a yeast infection (candidiasis).
White or grayish discharge, the smell of which after sex begins to resemble the smell of fish, is the main symptom of bacterial vaginosis, vaginal dysbacteriosis.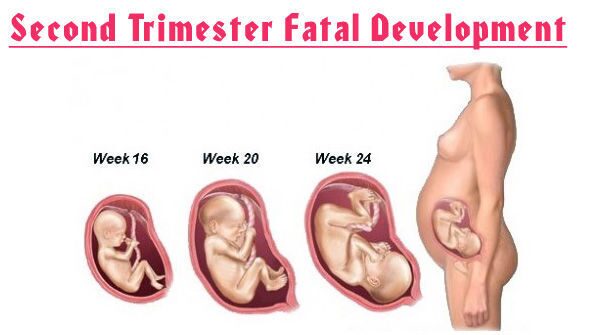
A yellowish or greenish discharge that has a strong unpleasant odor usually occurs with nonspecific vaginitis, and a foamy discharge is a sign of trichomoniasis, a sexually transmitted disease. nine0005
In all these cases, contact your doctor immediately. It should not be treated with over-the-counter drugs and folk remedies. According to some external signs, a diagnosis cannot even be made by a doctor, in addition, infections in pregnant women should be treated especially carefully and only by a professional. After proper treatment, the discharge returns to normal. There is no need to get rid of the usual discharge for pregnant women. After childbirth, they will stop naturally, and before that they are a sign of the normal course of pregnancy. nine0005
Allocations can change their nature and amount under the influence of irritants or intolerance to a particular substance, for example, when using panty liners. Such secretions are transparent and abundant, they stop when the irritant is removed.
"Thrush" is a disease caused by fungi of the genus Candida, present in small quantities in all women. During pregnancy, immunity decreases and fungi begin to actively multiply, causing inflammation, abundant white flocculent discharge with a sour smell, burning and itching in the vulva. The disease can manifest itself throughout pregnancy. nine0005
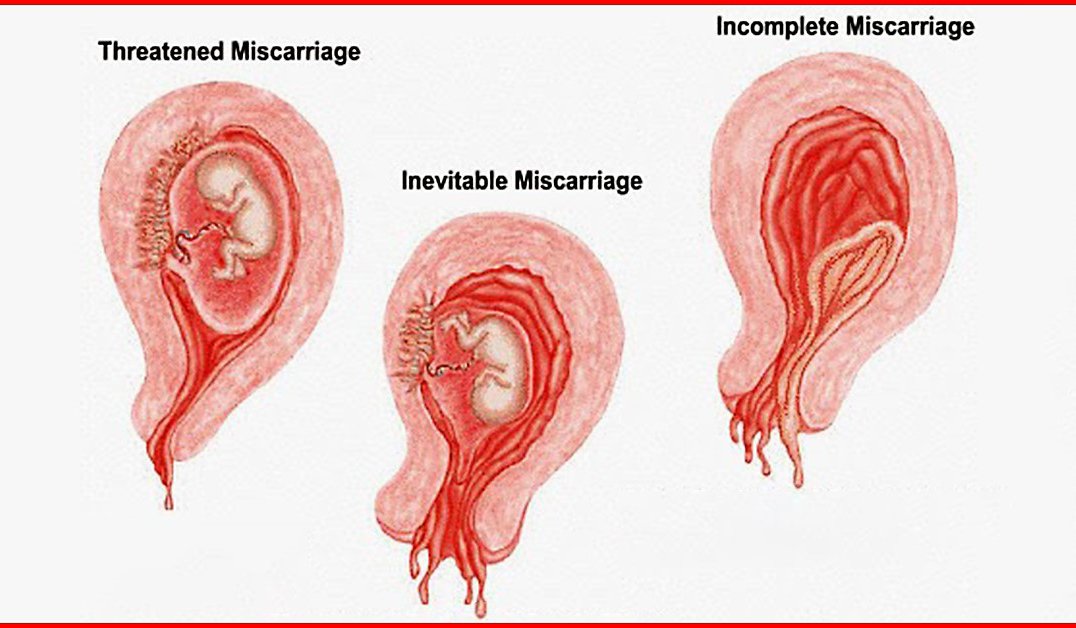
Bloody discharge in the first half of pregnancy usually indicates a lack of the hormone progesterone, which can lead to spontaneous miscarriage. Discharge may be accompanied by pain in the lower abdomen and lower back. In the treatment of the threat of abortion, the appointment of progesterone drugs, such phenomena disappear.
If bleeding from the vagina appeared during pregnancy during the second or third trimester, then this is a sign of a formidable complication, namely, placenta previa or its premature detachment. With improper attachment of the placenta in the uterine cavity and overlapping of the placental tissue with the area of the internal pharynx, they speak of placenta previa.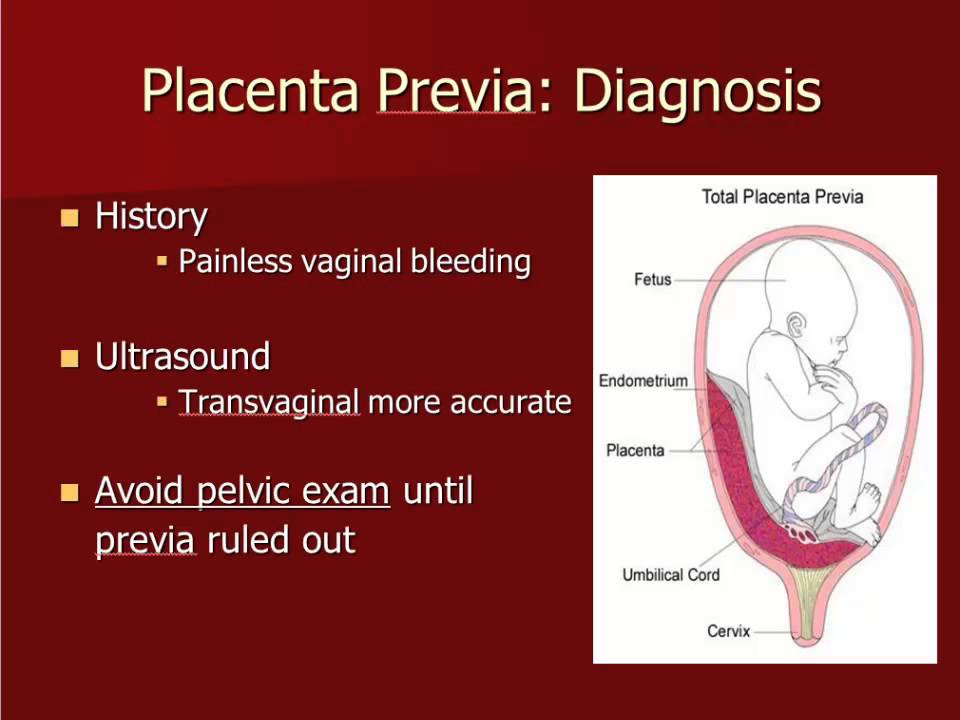 In this case, spotting occurs in a third of pregnant women. This most often occurs between 28 and 30 weeks, when the lower segment of the uterus is most prone to stretching and thinning. The discharge is repeated, the woman does not experience any pain, so it may be too late to see a doctor for an examination. This threatens the child with a lack of nutrients and oxygen, because it is through the placenta that the fetus is nourished. For a pregnant woman, this is fraught with acute placental abruption and severe bleeding, which is always problematic to stop, especially at home. nine0005
In this case, spotting occurs in a third of pregnant women. This most often occurs between 28 and 30 weeks, when the lower segment of the uterus is most prone to stretching and thinning. The discharge is repeated, the woman does not experience any pain, so it may be too late to see a doctor for an examination. This threatens the child with a lack of nutrients and oxygen, because it is through the placenta that the fetus is nourished. For a pregnant woman, this is fraught with acute placental abruption and severe bleeding, which is always problematic to stop, especially at home. nine0005
Bloody discharge during pregnancy should force a woman to immediately contact her obstetrician-gynecologist.
Brown discharge during pregnancy also indicates the threat of termination of pregnancy, or bleeding "erosion" (decidual polyp) of the cervix. Therefore, you should not understand these issues on your own; when brown discharge appears, it is better to consult your doctor.
Brown discharge during a delay in menstruation as a sign of an ectopic pregnancy is very dangerous. This condition requires immediate surgical care, as the growing embryo can rupture the wall of the fallopian tube at any time and cause internal bleeding. Therefore, with pain in the lower abdomen, which is accompanied by brown discharge from the genital tract and delayed menstruation, you should immediately call an ambulance. nine0005
This condition requires immediate surgical care, as the growing embryo can rupture the wall of the fallopian tube at any time and cause internal bleeding. Therefore, with pain in the lower abdomen, which is accompanied by brown discharge from the genital tract and delayed menstruation, you should immediately call an ambulance. nine0005
When the vagina becomes inflamed, the mucous discharge acquires a mucopurulent character, a greenish-yellow color, an unpleasant odor, burning and itching appear in the genital area. This is how chlamydia, mycoplasmosis, ureaplasmosis, trichomoniasis manifest themselves. Is it necessary to treat the infection during pregnancy, or is it better to do it after childbirth?
All sexually transmitted infections in pregnant women require treatment, as they can pass to the fetus and cause intrauterine infection (IUI). IUI is very dangerous for a child - it leads to his death or serious illness. Infection of a child during childbirth can lead to such serious complications as pneumonia, severe damage to the brain, kidneys, liver, and blood poisoning (sepsis). nine0005
nine0005
Today, obstetricians and gynecologists have learned to treat any infection in pregnant women in accordance with special guidelines for the timing of pregnancy, so that it is effective and safe for mother and fetus. It is not the treatment that should be feared, but the infection itself and its consequences.
Medicines that are used to treat pregnant women have passed the necessary clinical trials, during which it was proved that they do not have a negative effect on the pregnant woman and the fetus, including that they do not have a teratogenic effect (do not cause deformities in the fetus). nine0005
Sometimes the discharge is mucous in nature, occurs upon contact with an irritant or allergen. It can be synthetic tight underwear, allergies to fabrics, toiletries, personal care products. If irritation and allergens are not eliminated in time, then an infection that lives on the mucous membranes of the genital organs will definitely join.
Hygiene measures are mandatory for pregnant women.
 Your baby is still just a tiny "ball", consisting of several hundred cells, the number of which is multiplying at an insane pace. As soon as the “ball” of cells (these cells are called blastocysts) is located in the uterus, the part of it, from which the placenta will develop later, begins to produce the pregnancy hormone hCG (human chorionic gonadotropin). HCG "instructs" the ovaries to stop producing eggs, and also provides the synthesis of progesterone and estrogens necessary to maintain pregnancy. HCG stimulates the growth of the placenta, supports the existence of the corpus luteum until the "fetus-placenta" complex acquires the ability to independently form the necessary hormonal background. nine0005
Your baby is still just a tiny "ball", consisting of several hundred cells, the number of which is multiplying at an insane pace. As soon as the “ball” of cells (these cells are called blastocysts) is located in the uterus, the part of it, from which the placenta will develop later, begins to produce the pregnancy hormone hCG (human chorionic gonadotropin). HCG "instructs" the ovaries to stop producing eggs, and also provides the synthesis of progesterone and estrogens necessary to maintain pregnancy. HCG stimulates the growth of the placenta, supports the existence of the corpus luteum until the "fetus-placenta" complex acquires the ability to independently form the necessary hormonal background. nine0005  In the third week of pregnancy, your little baby receives oxygen and nutrients (and eliminates waste) through the primitive circulatory systems that connect the developing baby to the blood vessels in the uterine wall. The placenta is not yet developed enough to take on this task until the end of next week. nine0005
In the third week of pregnancy, your little baby receives oxygen and nutrients (and eliminates waste) through the primitive circulatory systems that connect the developing baby to the blood vessels in the uterine wall. The placenta is not yet developed enough to take on this task until the end of next week. nine0005  Allocations are very meager and few of the pregnant women notice them. nine0005
Allocations are very meager and few of the pregnant women notice them. nine0005  It occurs even more often than cravings for certain foods during pregnancy. You may suddenly find that certain foods, even your favorites, disgust you. nine0084
It occurs even more often than cravings for certain foods during pregnancy. You may suddenly find that certain foods, even your favorites, disgust you. nine0084