Group b positive
Group B strep disease - Symptoms and causes
Overview
Group B strep (streptococcus) is a common bacterium often carried in the intestines or lower genital tract. The bacterium is usually harmless in healthy adults. In newborns, however, it can cause a serious illness known as group B strep disease.
Group B strep can also cause dangerous infections in adults with certain chronic medical conditions, such as diabetes or liver disease. Older adults are at increased risk of illness due to group B strep, too.
If you're a healthy adult, there's nothing you need to do about group B strep. If you're pregnant, get a group B strep screening test during your third trimester. If you have group B strep, antibiotic treatment during labor can protect your baby.
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Symptoms
Infants
Most babies born to women carrying group B strep are healthy. But the few who are infected by group B strep during labor can become critically ill.
In infants, illness caused by group B strep can be within six hours of birth (early onset) — or weeks or months after birth (late onset).
Signs and symptoms might include:
- Fever
- Low body temperature
- Difficulty feeding
- Sluggishness, limpness or weak muscle tone
- Difficulty breathing
- Irritability
- Jitteriness
- Seizures
- Rash
- Jaundice
Adults
Many adults carry group B strep in their bodies — usually in the bowel, vagina, rectum, bladder or throat — and have no signs or symptoms.
In some cases, however, group B strep can cause a urinary tract infection or other more-serious infections. Signs and symptoms of infections that may be caused by group B strep include the following.
Urinary tract infection
- A strong, persistent urge to urinate
- A burning sensation or pain when urinating
- Passing frequent, small amounts of urine
- Urine that appears red, bright pink or cola colored — a sign of blood in the urine
- Pelvic pain
Blood infection (bacteremia)
- Fever
- Chills
- Confusion or lack of alertness
Pneumonia
- Fever
- Chills
- Cough
- Shortness of breath
- Chest pain when you breathe or cough
Skin or soft-tissue infection
- Swelling, warmth or redness in the area of the infection
- Pain in the area of the infection
- Lesions with pus or drainage
Bone or joint infection
- Fever
- Chills
- Swelling, warmth or redness over the area of the infection
- Pain in the area of the infection
- Stiffness or inability to use a limb or joint
When to see a doctor
If you have signs or symptoms of group B strep infection — particularly if you're pregnant, you have a chronic medical condition or you're older than 65 — contact your doctor right away.
If you notice your infant has signs or symptoms of group B strep disease, contact your baby's doctor immediately.
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which
information is beneficial, we may combine your email and website usage information with
other information we have about you. If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
Causes
Many healthy people carry group B strep bacteria in their bodies. You might carry the bacteria in your body for a short time — it can come and go — or you might always have it. Group B strep bacteria aren't sexually transmitted, and they're not spread through food or water. How the bacteria are spread to anyone other than newborns isn't known.
Group B strep can spread to a baby during a vaginal delivery if the baby is exposed to — or swallows — fluids containing group B strep.
Risk factors
Infants
An infant is at increased risk of developing group B strep disease if:
- The mother carries group B strep in her body
- The baby is born prematurely (earlier than 37 weeks)
- The mother's water breaks 18 hours or more before delivery
- The mother has an infection of the placental tissues and amniotic fluid (chorioamnionitis)
- The mother has a urinary tract infection during the pregnancy
- The mother's temperature is greater than 100.
 4 F (38 C) during labor
4 F (38 C) during labor - The mother previously delivered an infant with group B strep disease
Adults
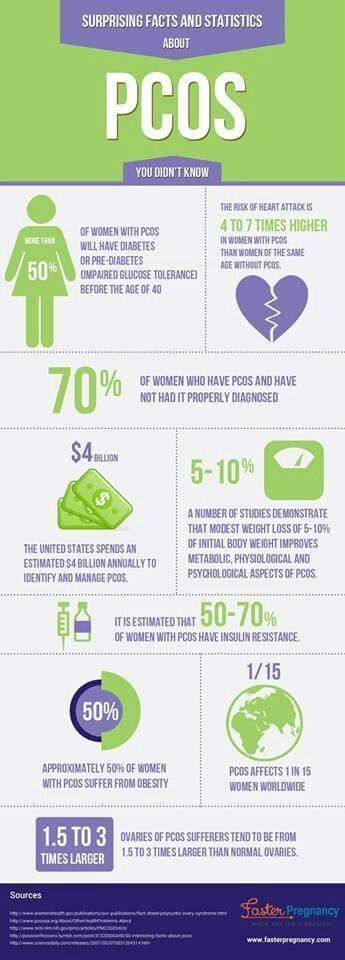
Adults age 65 and older are at increased risk of group B strep. You're also at increased risk of if you have a condition that impairs your immune system or other serious diseases, including the following:
- Diabetes
- HIV infection
- Liver disease
- Heart disease
- Cancer or history of cancer
Complications
Group B strep infection can lead to life-threatening disease in infants, including:
- Pneumonia
- Inflammation of the membranes and fluid surrounding the brain and spinal cord (meningitis)
- Infection in the bloodstream (bacteremia)
If you're pregnant, group B strep can cause the following:
- Urinary tract infection
- Infection of the placenta and amniotic fluid (chorioamnionitis)
- Infection of the membrane lining the uterus (endometritis)
- Bacteremia
If you're an older adult or you have a chronic health condition, group B strep bacteria can lead to any of the following conditions:
- Skin infection
- Bacteremia
- Urinary tract infection
- Pneumonia
- Bone and joint infections
- Infection of the heart valves (endocarditis)
- Meningitis
Prevention
If you're pregnant, the American College of Obstetricians and Gynecologists recommends a group B strep screening during weeks 36 to 37 of pregnancy. Your doctor will take swab samples from your vagina and rectum and send them to a lab for testing.
Your doctor will take swab samples from your vagina and rectum and send them to a lab for testing.
A positive test indicates that you carry group B strep. It doesn't mean that you're ill or that your baby will be affected, but that you're at increased risk of passing the bacteria to your baby.
To prevent group B bacteria from spreading to your baby during labor or delivery, your doctor can give you an IV antibiotic — usually penicillin or a related drug — when labor begins.
If you're allergic to penicillin or related drugs, you might receive clindamycin or vancomycin as an alternative. Because the effectiveness of these alternatives is not well understood, your baby will be monitored for up to 48 hours.
Taking oral antibiotics ahead of time won't help because the bacteria can return before labor begins.
Antibiotic treatment during labor is also recommended if you:
- Have a urinary tract infection
- Delivered a previous baby with group B strep disease
- Develop a fever during labor
- Haven't delivered your baby within 18 hours of your water breaking
- Go into labor before 37 weeks and haven't been tested for group B strep
Vaccine in development
Although it's not available yet, researchers are working on a group B strep vaccine that could help prevent group B strep infections in the future.
By Mayo Clinic Staff
Related
Products & Services
Group B Strep and Pregnancy (for Parents)
What Is Group B Strep?
Group B Streptococcus (group B strep, GBS) is a type of
bacteriaoften found in the urinary tract, digestive system, and reproductive tracts. The bacteria come and go from our bodies, so most people who have it don't know that they do. GBS usually doesn't cause health problems.
What Problems Can Group B Strep Cause?
Health problems from GBS are not common. But it can cause illness in some people, such as the elderly and those with some medical conditions. GBS can cause infections in such areas of the body as the blood, lungs, skin, or bones.
About 1 out of every 4 women have GBS. In pregnant women, GBS can cause infection of the urinary tract, placenta, womb, and amniotic fluid.
Even if they haven't had any symptoms of infection, pregnant women can pass the infection to their babies during labor and delivery.
How Does Group B Strep Affect Babies?
When women with GBS are treated with antibiotics during labor, most of their babies do not have any problems. But some babies can become very sick from GBS. Premature babies are more likely to be infected with GBS than full-term babies because their bodies and immune systems are less developed.
The two types of GBS disease in babies are:
- Early-onset infections, which happen during the first week of life. Babies often have symptoms within 24 hours of birth.
- Late-onset infections, which develop weeks to months after birth. This type of GBS disease is not well understood.
What Are the Signs & Symptoms of GBS Disease?
Newborns and infants with GBS disease might show these signs:
- a fever
- feeding problems
- breathing problems
- irritability or fussiness
- inactivity or limpness
- trouble keeping a healthy body temperature
Babies with GBS disease can develop serious problems, such as:
- pneumonia
- sepsis
- meningitis (infection of the fluid and lining around the brain).
 Meningitis is more common with late-onset GBS disease and, in some cases, can lead to hearing loss, vision loss, learning disabilities, seizures, and even death.
Meningitis is more common with late-onset GBS disease and, in some cases, can lead to hearing loss, vision loss, learning disabilities, seizures, and even death.
How Is Group B Strep Diagnosed?
Pregnant women are routinely tested for GBS late in the pregnancy, usually between weeks 35 and 37. The test is simple, inexpensive, and painless. Called a culture, it involves using a large cotton swab to collect samples from the vagina and rectum. These samples are tested in a lab to check for GBS. The results are usually available in 1 to 3 days.
If a test finds GBS, the woman is said to be "GBS-positive." This means only that she has the bacteria in her body — not that she or her baby will become sick from it.
GBS infection in babies is diagnosed by testing a sample of blood or spinal fluid. But not all babies born to GBS-positive mothers need testing. Most healthy babies are simply watched to see if they have signs of infection.
How Is Group B Strep Treated?
Doctors will test a pregnant woman to see if she has GBS. If she does, she will get intravenous (IV) antibiotics during labor to kill the bacteria. Doctors usually use penicillin, but can give other medicines if a woman is allergic to it.
If she does, she will get intravenous (IV) antibiotics during labor to kill the bacteria. Doctors usually use penicillin, but can give other medicines if a woman is allergic to it.
It's best for a woman to get antibiotics for at least 4 hours before delivery. This simple step greatly helps to prevent the spread of GBS to the baby.
Doctors also might give antibiotics during labor to a pregnant woman if she:
- goes into labor prematurely, before being tested for GBS
- hasn't been tested for GBS and her water breaks 18 or more hours before delivery
- hasn't been tested for GBS and has a fever during labor
- had a GBS bladder infection during the pregnancy
- had a baby before with GBS disease
Giving antibiotics during labor helps to prevent early-onset GBS disease only. The cause of late-onset disease isn't known, so no method has yet been found to prevent it. Researchers are working to develop a vaccine to prevent GBS infection.
Babies who get GBS disease are treated with antibiotics. These are started as soon as possible to help prevent problems. These babies also may need other treatments, like breathing help and IV fluids.
How Can I Help Prevent Group B Strep Infection?
Because GBS comes and goes from the body, a woman should be tested for it during each pregnancy. Women who are GBS-positive and get antibiotics at the right time during labor do well, and most don't pass the infection to their babies.
If you are GBS-positive and begin to go into labor, go to the hospital rather than laboring at home. By getting IV antibiotics for at least 4 hours before delivery, you can help protect your baby against early-onset GBS disease.
Reviewed by: Thinh Phu Nguyen, MD
Date reviewed: July 2022
About Blood Types - Blood Center
When a doctor talks about your blood type, he usually means two things: your ABO blood type and your Rh (rhesus factor).
A person's blood group is determined by antigens found on his red blood cells. An antigen is a structure on the surface of a cell. If it is foreign to the body, then the human defense system will react to it. Therefore, it is necessary to take into account blood groups when transfusing: the donor's blood group is determined at the Blood Center, and the patient's blood group is determined before transfusion. nine0003
An antigen is a structure on the surface of a cell. If it is foreign to the body, then the human defense system will react to it. Therefore, it is necessary to take into account blood groups when transfusing: the donor's blood group is determined at the Blood Center, and the patient's blood group is determined before transfusion. nine0003
AB0 system
The most important is the ABO blood group system, according to which blood is divided into groups A, B, O and AB. It is determined by two antigens located on the surface of red blood cells:
- group A - only antigen A is present on the surface of erythrocytes
- group B - only antigen B is present on the surface of erythrocytes
- group AB - both A and B antigens are present on the surface of erythrocytes
- group O - on the surface of erythrocytes there is neither antigen A nor antigen B.
If a person has blood type A, B or 0, then in his blood plasma there are also antibodies that destroy those antigens that the person himself does not have. Examples: If you have type A blood, then you cannot be transfused with type B blood, because in this case there are antibodies in your blood that fight against B antigens. If you have blood type 0, then your blood contains antibodies that fight like against antigens A and against antigens B.
Examples: If you have type A blood, then you cannot be transfused with type B blood, because in this case there are antibodies in your blood that fight against B antigens. If you have blood type 0, then your blood contains antibodies that fight like against antigens A and against antigens B.
If a person has blood type AB, then he does not have such antibodies, so he can be transfused with blood of any group. Therefore, the carrier of the AB blood group can be called universal patient.
A carrier of blood type 0 with a negative Rh factor, in turn, is called a universal donor, , since his red blood cells are suitable for all patients.
Rhesus (Rh ) accessory
Rh factor (Rh) can be positive (+) and negative (-). It depends on the presence of the D antigen on the surface of the red blood cells. If the D antigen is present, the person is considered Rh-positive, and if the D antigen is absent, then the person is Rh-negative.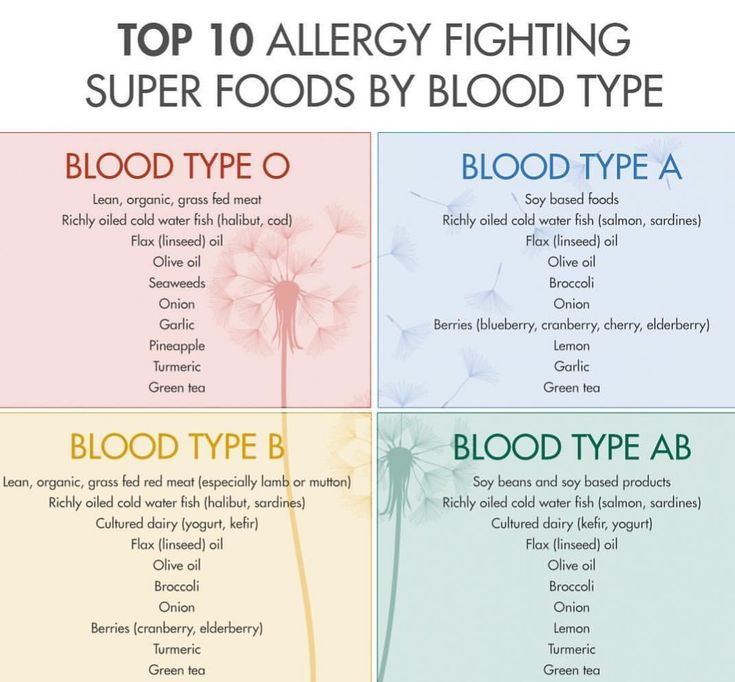 nine0003
nine0003
If a person is Rh negative, contact with Rh positive blood (for example, during pregnancy or blood transfusion) may form antibodies. These antibodies can cause pregnancy problems in an Rh-negative woman if she is carrying an Rh-positive baby.
In addition to the ABO and Rh systems, about thirty more blood group systems have been discovered to date. Clinically, the most important of these are the Kell, Kidd and Duffy systems. According to the Kell system, donor blood is also examined. nine0003
How is the blood type determined?
To determine the blood type, it is mixed with a reagent containing known antibodies.
Three drops of blood taken from one person are applied to the base: the anti-A test reagent is added to one drop, the anti-B test reagent to the other, and the anti-D test reagent to the third, i.e. Rh test reagent. If blood clots form in the first drop, i.e. erythrocytes stick together (agglutination), then the person has antigen A. If erythrocytes do not stick together in another drop, therefore the person does not have antigen B; and if agglutination occurs in the third drop, then this indicates a positive Rh factor. In this example, the donor has blood type A and is Rh positive. nine0003
If erythrocytes do not stick together in another drop, therefore the person does not have antigen B; and if agglutination occurs in the third drop, then this indicates a positive Rh factor. In this example, the donor has blood type A and is Rh positive. nine0003
Donor and recipient blood group compatibility is extremely important, otherwise the recipient may have dangerous reactions to the blood transfusion.
Inheritance of blood groups
A person inherits from his father and from his mother to the same extent. Therefore, the hereditary substance has a double structure: one part from the mother and the other from the father. Speaking about the inheritance of blood groups, it must be borne in mind that:
- Most of our genes exist in two copies
- Each parent gives (based on random selection) one of these copies to their children
- Genes occur in different versions (alleles)
- Some versions of the gene are stronger than others
| ABO system | System Rh |
In the AB0 system, antigens are presented in three versions A, B and 0. Given that the hereditary substance consists of two parts, six different combinations can occur: nine0072 Given that the hereditary substance consists of two parts, six different combinations can occur: nine0072 | |
| Genes | |
| AA | |
| A0 | |
| AB | |
| B0 | |
| BB | |
| 00 |
The stronger part appears, both equally or a combination. In the AB0 system, genes A and B are stronger than 0, which affects the formation of the blood group as follows:
| Genes | Blood type | |
| AA | A | |
| A0 | A | |
| AB | AB | |
| B0 | B | |
| BB | B | |
| 00 | 0 | |
Example: The mother has a combination of A0 genes in hereditary substance, and her blood type is A (at the same time, she is a carrier of the blood type 0 gene, and there is a possibility that she will pass it on to her child). The father's blood type has the designation 0, and in his hereditary substance there is a combination of genes 00. Accordingly, he can only pass 0 to the child, i.e. absence of antigens. Thus, their child may have an A (A0) or 0 (00) blood type. nine0003
The father's blood type has the designation 0, and in his hereditary substance there is a combination of genes 00. Accordingly, he can only pass 0 to the child, i.e. absence of antigens. Thus, their child may have an A (A0) or 0 (00) blood type. nine0003
| Genes | Blood group |
| +/+ | positive |
| +/- | positive |
| -/- | negative |
Example: if the mother has Rh positive blood, and there is a hidden negative version, that is, the allele (+/-), and the father has exactly the same combination, and they both pass the negative allele, then two Rh-positive parents can have a child with a negative Rh factor.
Blood groups
There are 4 blood types.
ABO system
Late 19th century The Australian scientist Karl Landsteiner, while conducting a study of erythrocytes, discovered a curious pattern: in the red blood cells (erythrocytes) of some people there may be a special marker, which the scientist designated with the letter A, in others - marker B, in others neither A nor B were found. Later it turned out that the markers described by Landsteiner are special proteins that determine the species specificity of cells, or antigens. In fact, these studies divided all of humanity into 3 blood groups. nine0003
The fourth group was described in 1902 by the scientists Decastello and Sturli. The joint discovery of scientists was called the ABO system.
People with the first blood group 0(I) are universal donors, since their blood, taking into account the AB0 system, can be transfused to people with any blood type.
The owners of the fourth blood group AB(IV) belong to the category of universal recipients. They can be transfused with blood of any group.
However, now physicians are striving to transfuse an identical blood type to a person. This rule is deviated only in extreme cases. nine0003
Rh factor
Unlike blood group antigens, Rh factor is an antigen found only in the erythrocyte membrane and independent of other blood factors. The Rh factor is inherited and persists throughout a person's life. 85% of people whose red blood cells contain the Rh factor have Rh-positive blood (Rh +), the blood of the rest of the people does not contain the Rh factor and is called Rh-negative (Rh-).
Kell factor
The Kell system is a blood type system that includes 25 antigens, including the most immunogenic after A, B and D, antigen K.
Based on the presence or absence of K antigen in red blood cells, all people can be divided into two groups: Kell-negative and Kell-positive. The presence of the K antigen (Kell-positive) is not a pathology and is inherited, like other human group antigens. In Russia, it occurs in 7-10% of the population.
The presence of the K antigen (Kell-positive) is not a pathology and is inherited, like other human group antigens. In Russia, it occurs in 7-10% of the population.
At present, the presence of antigen K is determined in blood service institutions as the most dangerous for the occurrence of immunological complications. Many cases of blood transfusion complications and hemolytic disease of the newborn are described, the cause of which was isoimmunization with antigen K.
Kell-negative blood should only be transfused from donors lacking the K antigen to prevent hemolysis. Kell-positive individuals are universal recipients of blood, since they do not reject its components.
In order to prevent post-transfusion complications due to the Kell system antigen, departments and blood transfusion stations issue an erythrocyte suspension or mass that does not contain this factor for transfusion to medical institutions. When transfusing all types of plasma, platelet concentrate, leukocyte concentrate, antigen K of the Kell system is not taken into account. nine0003
nine0003
Plasma donation is therefore recommended for Kell-positive donors.
Interesting facts
The Japanese are sure that a person's character is influenced by blood type. The Japanese scientist Masahito Naomi, on the basis of research, deduced such a relationship between the blood type and the character of a person.
First blood type - samurai. These people have strong leadership qualities. They are ambitious, self-confident, as a rule, occupy high positions.
Second blood type - peasants. These are perfectionists. Such people are conservative in everything, they honor traditions and are not used to changing their habits and way of life. He is quite restrained, stubborn, has his own opinion on everything.
Third blood type - merchants. Optimistic, passionate nature. They can be selfish, they always put their own interests first, they will never miss their benefits.
Fourth blood group - artisans.