Pregnancy and pcos
Polycystic ovarian syndrome (PCOS) and pregnancy – symptoms and treatments
Polycystic ovarian syndrome (PCOS) and pregnancy – symptoms and treatments | Pregnancy Birth and Baby beginning of content7-minute read
Listen
What is PCOS?
Polycystic ovarian syndrome, or PCOS, is a common condition.
People with PCOS can have:
- higher than normal levels of androgens (male-type hormones)
- problems with ovulation (the release of eggs from the ovaries)
- multiple cysts on the ovaries
This can affect your menstrual cycle, fertility and appearance.
If you have PCOS you may struggle to become pregnant and may be at higher risk of developing some pregnancy complications.
Illustration showing a normal ovary and a polycystic ovary.What are the symptoms of PCOS?
There are many signs and symptoms that are associated with PCOS. These can include:
- irregular menstrual periods
- cysts on the ovaries
- infertility
- weight gain
- acne
- depression
- excessive face and body hair
- thinning or balding head hair
- insulin resistance (where your cells don't respond to insulin and your blood sugar levels rise)
Some of these symptoms (such as acne, excess face and body hair, and scalp hair loss) are due to increased levels of the hormones called androgens. These hormones are found in all females, but those with PCOS have slightly higher amounts.
CHECK YOUR SYMPTOMS — If you are feeling unwell and not sure what to do next, check your symptoms using the healthdirect Symptom Checker tool.
How is PCOS diagnosed?
It often takes a while to get a PCOS diagnosis.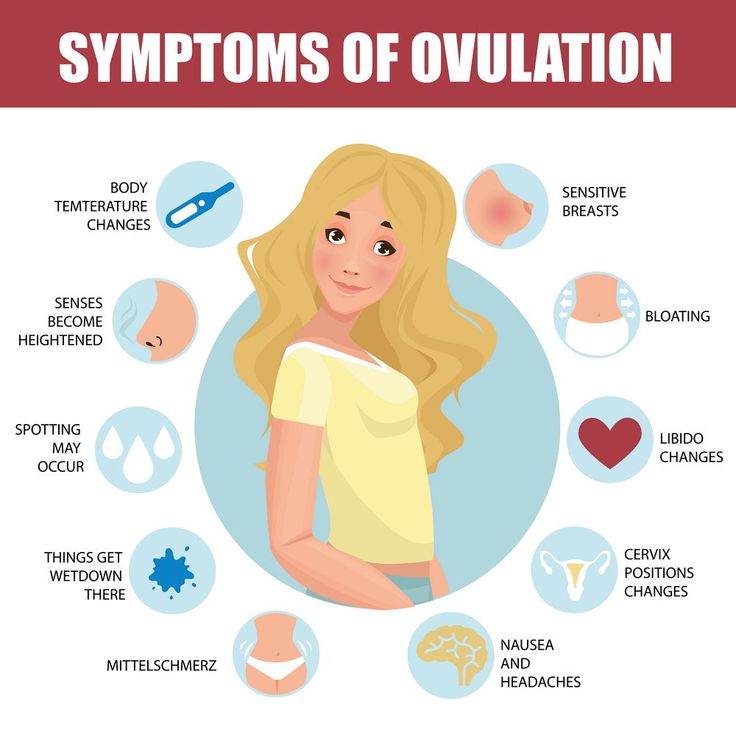 This is because the condition can mimic other problems. Sometimes, people only find out that they have PCOS when they have tests to find out why they are having trouble getting pregnant.
This is because the condition can mimic other problems. Sometimes, people only find out that they have PCOS when they have tests to find out why they are having trouble getting pregnant.
If you think you might have PCOS, see your doctor. Early diagnosis means that your symptoms can be treated early.
At your appointment, your doctor will:
- ask about your symptoms
- ask for your medical history
- examine you
Your doctor may also recommend blood tests and an ultrasound scan to look for any cysts in the ovaries.
In general, to be diagnosed with PCOS, you need to have 2 out of 3 of the following;
- irregular periods, or no periods
- symptoms due to increased levels of androgen hormones, or a blood test showing you have increased levels of androgen hormones
- an ultrasound scan showing multiple cysts on your ovary or ovaries
FIND A HEALTH SERVICE — The Service Finder can help you find doctors, pharmacies, hospitals and other health services.
Will PCOS affect my fertility?
If you have PCOS, you might struggle to get pregnant.
Fortunately, with lifestyle changes or infertility treatment, most people with PCOS can become pregnant. Talk to your doctor or fertility specialist for individual advice for your situation.
Can PCOS increase my risk of complications during pregnancy?
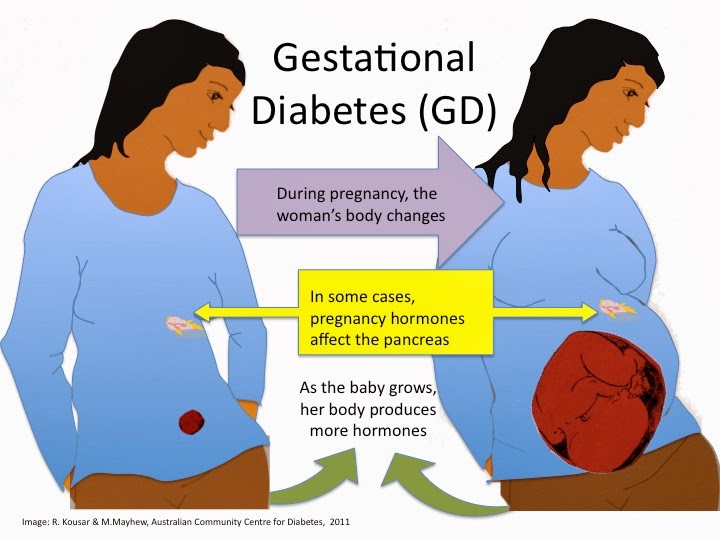
Having PCOS can increase your risk of some complications during pregnancy, such as:
- high blood pressure
- gestational diabetes
- premature birth
If you have PCOS, you are also at increased risk of having a baby larger than expected for their gestational age. This comes with a higher risk of needing a caesarean delivery.
Babies born to people with PCOS have a higher chance of being admitted to a newborn intensive care unit.
Pregnant women with PCOS may have a higher risk of miscarriage and stillbirth. However, more research is needed in this area.
If you have PCOS and are pregnant, it is important you talk with your doctor. The risk of these complications can be reduced by monitoring your PCOS symptoms and taking extra care during your pregnancy.
The risk of these complications can be reduced by monitoring your PCOS symptoms and taking extra care during your pregnancy.
What steps can I take to look after my health?
You can make lifestyle changes to manage your PCOS and look after your health. These include:
- maintaining a healthy weight
- eating healthily
- exercising
- managing stress
- getting enough sleep
These lifestyle changes can reduce the symptoms of PCOS and improve your chance of falling pregnant.
If you are overweight, a 5% to 10% loss in weight can increase your fertility.
Speak to your doctor for guidance on how to make effective lifestyle changes.
How is PCOS treated?
Treatment for PCOS depends on each person. Speak to your doctor about the best treatment for you.
If you are trying to fall pregnant, your PCOS treatment will focus on:
- restoring regular ovulation
- weight loss
- improving your general health and wellbeing
If you have made lifestyle changes and are still struggling to fall pregnant, your doctor may order fertility tests. They may also prescribe fertility medicines to help you ovulate. In some cases, they may recommend surgery.
They may also prescribe fertility medicines to help you ovulate. In some cases, they may recommend surgery.
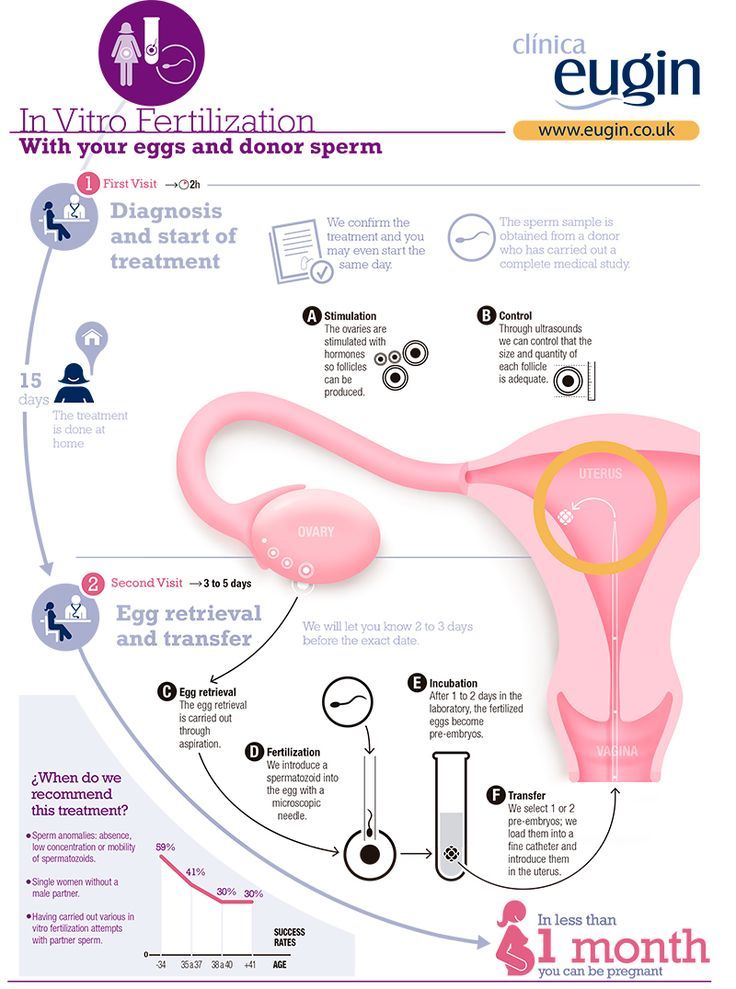
Another possibility is in vitro fertilisation (IVF), which offers the best chance of conception. However, this can be expensive and is usually only considered when all other options have been unsuccessful.
If you are not trying to fall pregnant, your PCOS treatment will focus on:
- reducing your symptoms
- reducing your risk of long-term health issues, including heart disease and type 2 diabetes
Speak to your doctor. They can help you manage your PCOS symptoms by providing:
- weight loss management strategies
- treatment for sleeping problems
- acne treatment
- medicines, including hormonal contraception (birth control) to manage irregular menstruation
Dealing with infertility and PCOS symptoms can be difficult. You may experience feelings of depression and anxiety. Your doctor can refer you to a counsellor or psychologist for your mental health.
Resources and support
Visit the Jean Hailes website for more information on PCOS and its complications.
Hormones Australia also supplies information on PCOS, including questions to ask your doctor.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
Australian Family Physician (Polycystic ovary system), Jean Hailes (PCOS), Royal Australian College of General Practitioners (Polycystic ovary system - clinical guidelines), The Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Long-term consequences of PCOS - statement)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: July 2022
Back To Top
Need more information?
Polycystic Ovary Syndrome (PCOS) | Your Fertility
PCOS can be associated with a range of symptoms including irregular periods and difficulties getting pregnant
Read more on Your Fertility website
Fact sheets | Your Fertility
Polycystic ovary syndrome (PCOS) is the most common hormonal condition affecting women in their reproductive years
Read more on Your Fertility website
What is PCOS?
Polycystic ovary syndrome (PCOS) is the most common hormonal condition affecting women in their reproductive years.
Read more on Your Fertility website
Polycystic ovarian syndrome (PCOS) - Better Health Channel
Polycystic ovarian syndrome is a hormonal condition associated with irregular menstrual cycles, excess hair growth, acne, reduced fertility, and increased risk of diabetes and mood changes.
Read more on Better Health Channel website
Polycystic ovary syndrome (PCOS) | Dietitians Australia
PCOS is a common hormonal condition of the ovaries that can cause problems such as an irregular menstrual cycle, weight gain, impaired fertility and poor mental health. Diet and lifestyle changes are the first steps to manage PCOS, and an Accredited Practising Dietitian specialising in PCOS is the most qualified professional to help.
Read more on Dietitians Australia website
Fertility explained | VARTA
Fertility is the ability to conceive a child. Most of us take our fertility for granted but the process of reproduction is complex, so some people may experience difficulties when trying for a baby. There are a range of factors that can affect fertility. Taking care of your preconception health by modifying your lifestyle can improve your chance of a pregnancy and the health of your future child. Medical conditions such as polycystic ovary syndrome (PCOS) and endometriosis can reduce fertility, however it may just take longer to get pregnant. In some cases, medical procedures can be used to preserve fertility. Fertility preservation (freezing of gametes for later use) is used by people who are not ready to have a baby during their most fertile years or for those facing medical treatment that might impair their fertility. Understanding reproduction It is useful to understand how eggs and sperm are normally formed, and how conception occurs to understand the causes of infertility and how they are targeted in fertility treatment. The hormones which control the production of sperm and eggs are called gonadotrophins.
Most of us take our fertility for granted but the process of reproduction is complex, so some people may experience difficulties when trying for a baby. There are a range of factors that can affect fertility. Taking care of your preconception health by modifying your lifestyle can improve your chance of a pregnancy and the health of your future child. Medical conditions such as polycystic ovary syndrome (PCOS) and endometriosis can reduce fertility, however it may just take longer to get pregnant. In some cases, medical procedures can be used to preserve fertility. Fertility preservation (freezing of gametes for later use) is used by people who are not ready to have a baby during their most fertile years or for those facing medical treatment that might impair their fertility. Understanding reproduction It is useful to understand how eggs and sperm are normally formed, and how conception occurs to understand the causes of infertility and how they are targeted in fertility treatment. The hormones which control the production of sperm and eggs are called gonadotrophins. There are two types of gonadotrophins: follicle-stimulating hormone (FSH) and luteinising hormone (LH). In men, they stimulate the testicles to produce sperm and testosterone. In women, they act on the ovaries where the eggs develop. The female sex hormones, oestrogen and progesterone, are produced by the ovaries when eggs mature and are released (ovulation). For women, the production of sex hormones and the release of an egg is known as the menstrual cycle. It is counted from the first day of the period until the day before the start of the next period. In an average cycle of 28 days, ovulation happens on day 14. However, cycle length varies between women, and it is important to note that ovulation occurs earlier in women with shorter cycles and later in women with longer cycles. Sperm are produced at the rate of about 300 million per day. They take some 80 days to mature. Each sperm has a head, which contains the genetic material, and a tail, which propels it up through the vagina, uterus, and fallopian tubes where the egg is fertilised.
There are two types of gonadotrophins: follicle-stimulating hormone (FSH) and luteinising hormone (LH). In men, they stimulate the testicles to produce sperm and testosterone. In women, they act on the ovaries where the eggs develop. The female sex hormones, oestrogen and progesterone, are produced by the ovaries when eggs mature and are released (ovulation). For women, the production of sex hormones and the release of an egg is known as the menstrual cycle. It is counted from the first day of the period until the day before the start of the next period. In an average cycle of 28 days, ovulation happens on day 14. However, cycle length varies between women, and it is important to note that ovulation occurs earlier in women with shorter cycles and later in women with longer cycles. Sperm are produced at the rate of about 300 million per day. They take some 80 days to mature. Each sperm has a head, which contains the genetic material, and a tail, which propels it up through the vagina, uterus, and fallopian tubes where the egg is fertilised. Conception occurs when an egg and a sperm come together. At ovulation, an egg is released from the ovary into the fallopian tube. If sperm is present at that time, the egg can be fertilised. The fertilised egg then starts to divide and becomes an embryo. After ovulation, the ovary produces progesterone which prepares the lining of the uterus - the endometrium - for the growing embryo. A few days after implantation, the embryo starts to produce human chorionic gonadotrophins (HCG) - the hormone that gives a positive pregnancy test reading. If an embryo does not form or attach to the endometrium (implantation), the level of progesterone drops and the next period starts.
Conception occurs when an egg and a sperm come together. At ovulation, an egg is released from the ovary into the fallopian tube. If sperm is present at that time, the egg can be fertilised. The fertilised egg then starts to divide and becomes an embryo. After ovulation, the ovary produces progesterone which prepares the lining of the uterus - the endometrium - for the growing embryo. A few days after implantation, the embryo starts to produce human chorionic gonadotrophins (HCG) - the hormone that gives a positive pregnancy test reading. If an embryo does not form or attach to the endometrium (implantation), the level of progesterone drops and the next period starts.
Read more on Victorian Assisted Reproductive Treatment Authority website
Good fertility health
Your age and your health can affect your chances of falling pregnant. Maintaining a healthy lifestyle may help you improve your fertility.
Read more on Pregnancy, Birth & Baby website
All about Polycystic Ovary Syndrome (PCOS) | Jean Hailes
Read about causes, signs and symptoms of PCOS, as well as diagnosis and treatments available to help. Jean Hailes is Australia's leader in women's health.
Read more on Jean Hailes for Women's Health website
Ovulation and fertility - Better Health Channel
The female body shows several signs of ovulation and you may experience some or all of these signs.
Read more on Better Health Channel website
The Pink Elephants Support Network - Female Fertility Issues - Pink Elephants
The Pink Elephants Support Network are a not for profit charity, formed to support women through miscarriage, pregnancy loss and beyond.
Read more on Pink Elephants Support Network website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.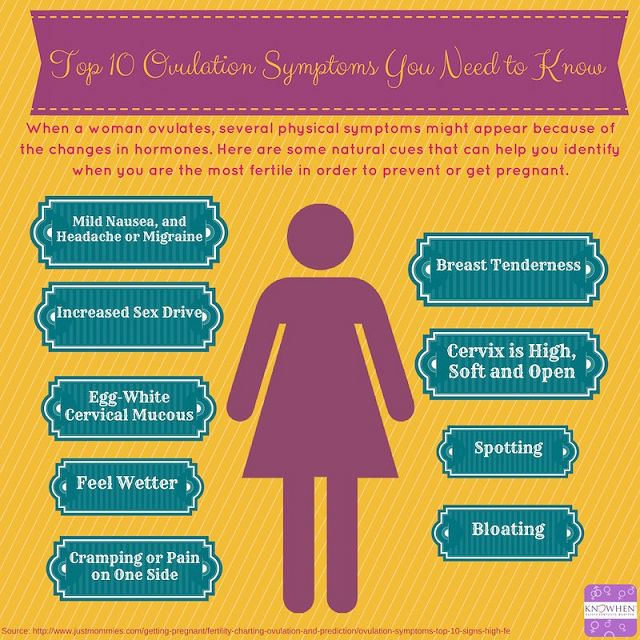
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Pregnancy in polycystic ovary syndrome
1. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril. 2004;81:19–25. [PubMed] [Google Scholar]
2. Azziz R, Carmina E, Dewailly D, Diamanti-Kandarakis E, Escobar-Morreale HF, Futterweit W, et al. Positions statement: Criteria for defining polycystic ovary syndrome as a predominantly hyperandrogenic syndrome: An androgen excess society guideline. J Clin Endocrinol Metab. 2006;91:4237–45. [PubMed] [Google Scholar]
J Clin Endocrinol Metab. 2006;91:4237–45. [PubMed] [Google Scholar]
3. Kumarapeli V, Seneviratne Rde A, Wijeyaratne CN, Yapa RM, Dodampahala SH. A simple screening approach for assessing community prevalence and phenotype of polycystic ovary syndrome in a semi-urban population in Sri Lanka. Am J Epidemiol. 2008;168:321–8. [PubMed] [Google Scholar]
4. Mehrabian F, Khani B, Kelishadi R, Ghanbari E. The prevalence of polycystic ovary syndrome in Iranian women based on different diagnostic criteria. Endokrynol Pol. 2011;62:238–42. [PubMed] [Google Scholar]
5. Barbour LA, Shao J, Qiao L, Pulawa LK, Jensen DR, Bartke A, et al. Human placental growth hormone causes severe insulin resistance in transgenic mice. Am J Obstet Gynecol. 2002;186:512–7. [PubMed] [Google Scholar]
6. Catalano PM, Huston L, Amini SB, Kalhan SC. Longitudinal changes in glucose metabolism during pregnancy in obese women with normal glucose tolerance and gestational diabetes mellitus. Am J Obstet Gynecol.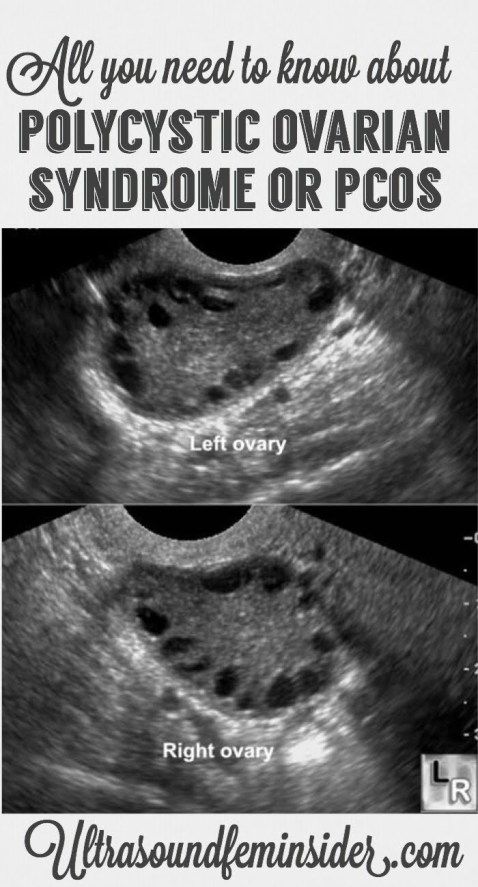 1999;180:903–16. [PubMed] [Google Scholar]
1999;180:903–16. [PubMed] [Google Scholar]
7. Okuno S, Akazawa S, Yasuhi I, Kawasaki E, Matsumoto K, Yamasaki H, et al. Decreased expression of the GLUT4 glucose transporter protein in adipose tissue during pregnancy. Horm Metab Res. 1995;27:231–4. [PubMed] [Google Scholar]
8. Friedman JE, Ishizuka T, Shao J, Huston L, Highman T, Catalano P. Impaired glucose transport and insulin receptor tyrosine phosphorylation in skeletal muscle from obese women with gestational diabetes. Diabetes. 1999;48:1807–14. [PubMed] [Google Scholar]
9. Roos N, Kieler H, Sahlin L, Ekman-Ordeberg G, Falconer H, Stephansson O. Risk of adverse pregnancy outcomes in women with polycystic ovary syndrome: Population based cohort study. BMJ. 2011;343:d6309. [PMC free article] [PubMed] [Google Scholar]
10. Boomsma CM, Eijkemans MJ, Hughes EG, Visser GH, Fauser BC, Macklon NS. A meta-analysis of pregnancy outcomes in women with polycystic ovary syndrome. Hum Reprod Update. 2006;12:673–83. [PubMed] [Google Scholar]
11. Kjerulff LE, Sanchez-Ramos L, Duffy D. Pregnancy outcomes in women with polycystic ovary syndrome: A metaanalysis. Am J Obstet Gynecol. 2011;204:558. e1-6. [PubMed] [Google Scholar]
Kjerulff LE, Sanchez-Ramos L, Duffy D. Pregnancy outcomes in women with polycystic ovary syndrome: A metaanalysis. Am J Obstet Gynecol. 2011;204:558. e1-6. [PubMed] [Google Scholar]
12. Jakubowicz DJ, Iuorno MJ, Jakubowicz S, Roberts KA, Nestler JE. Effects of metformin on early pregnancy loss in the polycystic ovary syndrome. J Clin Endocrinol Metab. 2002;87:524–9. [PubMed] [Google Scholar]
13. Gray RH, Wu LY. Subfertility and risk of spontaneous abortion. Am J Public Health. 2000;90:1452–4. [PMC free article] [PubMed] [Google Scholar]
14. Homburg R. Pregnancy complications in PCOS. Best Pract Res Clin Endocrinol Metab. 2006;20:281–92. [PubMed] [Google Scholar]
15. Regan L, Owen EJ, Jacobs HS. Hypersecretion of luteinising hormone, infertility, and miscarriage. Lancet. 1990;336:1141–4. [PubMed] [Google Scholar]
16. Homburg R, Levy T, Berkovitz D, Farchi J, Feldberg D, Ashkenazi J, et al. Gonadotropin-releasing hormone agonist reduces the miscarriage rate for pregnancies achieved in women with polycystic ovarian syndrome. Fertil Steril. 1993;59:527–31. [PubMed] [Google Scholar]
Fertil Steril. 1993;59:527–31. [PubMed] [Google Scholar]
17. Balen AH, Tan SL, MacDougall J, Jacobs HS. Miscarriage rates following in vitro fertilization are increased in women with polycystic ovaries and reduced by pituitary desensitization with buserelin. Hum Reprod. 1993;8:959–64. [PubMed] [Google Scholar]
18. Clifford K, Rai R, Watson H, Franks S, Regan L. Does suppressing luteinising hormone secretion reduce the miscarriage rate. Results of a randomised controlled trial? BMJ. 1996;312:1508–11. [PMC free article] [PubMed] [Google Scholar]
19. Rai R, Backos M, Rushworth F, Regan L. Polycystic ovaries and recurrent miscarriage-a reappraisal. Hum Reprod. 2000;15:612–5. [PubMed] [Google Scholar]
20. Aksoy S, Celikkanat H, Senöz S, Gökmen O. The prognostic value of serum estradiol, progesterone, testosterone and free testosterone levels in detecting early abortions. Eur J Obstet Gynecol Reprod Biol. 1996;67:5–8. [PubMed] [Google Scholar]
21. Tulppala M, Stenman UH, Cacciatore B, Ylikorkala O. Polycystic ovaries and levels of gonadotrophins and androgens in recurrent miscarriage: Prospective study in 50 women. Br J Obstet Gynaecol. 1993;100:348–52. [PubMed] [Google Scholar]
Polycystic ovaries and levels of gonadotrophins and androgens in recurrent miscarriage: Prospective study in 50 women. Br J Obstet Gynaecol. 1993;100:348–52. [PubMed] [Google Scholar]
22. Okon MA, Laird SM, Tuckerman EM, Li TC. Serum androgen levels in women who have recurrent miscarriages and their correlation with markers of endometrial function. Fertil Steril. 1998;69:682–90. [PubMed] [Google Scholar]
23. Apparao KBC, Lovely LP, Gui Y, Lininger RA, Lessey BA. Elevated endometrial androgen receptor expression in women with polycystic ovarian syndrome. Biol Reprod. 2002;66:297–304. [PubMed] [Google Scholar]
24. Cermik D, Karaca M, Taylor HS. HOXA10 expression is repressed by progesterone in the myometrium: Differential tissue-specific regulation of HOX gene expression in the reproductive tract. J Clin Endocrinol Metab. 2001;86:3387–92. [PubMed] [Google Scholar]
25. Glueck CJ, Wang P, Fontaine RN, Sieve-Smith L, Tracy T, Moore SK. Plasminogen activator inhibitor activity: An independent risk factor for the high miscarriage rate during pregnancy in women with polycystic ovary syndrome. Metab Clin Exp. 1999;48:1589–95. [PubMed] [Google Scholar]
Metab Clin Exp. 1999;48:1589–95. [PubMed] [Google Scholar]
26. Palomba S, Orio F, Jr, Falbo A, Russo T, Tolino A, Zullo F. Plasminogen activator inhibitor 1 and miscarriage after metformin treatment and laparoscopic ovarian drilling in patients with polycystic ovary syndrome. Fertil Steril. 2005;84:761–5. [PubMed] [Google Scholar]
27. Glueck CJ, Sieve L, Zhu B, Wang P. Plasminogen activator inhibitor activity, 4G5G polymorphism of the plasminogen activator inhibitor 1 gene, and first-trimester miscarriage in women with polycystic ovary syndrome. Metab Clin Exp. 2006;55:345–52. [PubMed] [Google Scholar]
28. Dunaif A. Insulin resistance and the polycystic ovary syndrome: Mechanism and implications for pathogenesis. Endocr Rev. 1997;18:774–800. [PubMed] [Google Scholar]
29. Dunaif A, Segal KR, Futterweit W, Dobrjansky A. Profound peripheral insulin resistance, independent of obesity, in polycystic ovary syndrome. Diabetes. 1989;38:1165–74. [PubMed] [Google Scholar]
30. Chi MM, Schlein AL, Moley KH. High insulin-like growth factor 1 (IGF-1) and insulin concentrations trigger apoptosis in the mouse blastocyst via down-regulation of the IGF-1 receptor. Endocrinology. 2000;141:4784–92. [PubMed] [Google Scholar]
Chi MM, Schlein AL, Moley KH. High insulin-like growth factor 1 (IGF-1) and insulin concentrations trigger apoptosis in the mouse blastocyst via down-regulation of the IGF-1 receptor. Endocrinology. 2000;141:4784–92. [PubMed] [Google Scholar]
31. Hinck L, Thissen JP, De Hertogh R. Identification of caspase-6 in rat blastocysts and its implication in the induction of apoptosis by high glucose. Biol Reprod. 2003;68:1808–12. [PubMed] [Google Scholar]
32. Mioni R, Chiarelli S, Xamin N, Zuliani L, Granzotto M, Mozzanega B, et al. Evidence for the presence of glucose transporter 4 in the endometrium and its regulation in polycystic ovary syndrome patients. J Clin Endocrinol Metab. 2004;89:4089–96. [PubMed] [Google Scholar]
33. Lessey BA. Adhesion molecules and implantation. J Reprod Immunol. 2002;55:101–12. [PubMed] [Google Scholar]
34. Lee C-L, Lam KKW, Koistinen H, Seppala M, Kurpisz M, Fernandez N, et al. Glycodelin-A as a paracrine regulator in early pregnancy. J Reprod Immunol. 2011;90:29–34. [PubMed] [Google Scholar]
2011;90:29–34. [PubMed] [Google Scholar]
35. Jakubowicz DJ, Essah PA, Seppälä M, Jakubowicz S, Baillargeon JP, Koistinen R, et al. Reduced serum glycodelin and insulin-like growth factor-binding protein-1 in women with polycystic ovary syndrome during first trimester of pregnancy. J Clin Endocrinol Metab. 2004;89:833–9. [PubMed] [Google Scholar]
36. Metwally M, Ong KJ, Ledger WL, Li TC. Does high body mass index increase the risk of miscarriage after spontaneous and assisted conception. A meta-analysis of the evidence? Fertil Steril. 2008;90:714–26. [PubMed] [Google Scholar]
37. Sandhu MS, Gibson JM, Heald AH, Dunger DB, Wareham NJ. Association between insulin-like growth factor-I: Insulin-like growth factor-binding protein-1 ratio and metabolic and anthropometric factors in men and women. Cancer Epidemiol Biomarkers Prev. 2004;13:166–70. [PubMed] [Google Scholar]
38. Kelly CJ, Stenton SR, Lashen H. Insulin-like growth factor binding protein-1 in PCOS: A systematic review and meta-analysis. Hum Reprod Update. 2011;17:4–16. [PubMed] [Google Scholar]
Hum Reprod Update. 2011;17:4–16. [PubMed] [Google Scholar]
39. Wang JX, Davies MJ, Norman RJ. Polycystic ovarian syndrome and the risk of spontaneous abortion following assisted reproductive technology treatment. Hum Reprod. 2001;16:2606–9. [PubMed] [Google Scholar]
40. Veltman-Verhulst SM, van Haeften TW, Eijkemans MJC, de Valk HW, Fauser BC, Goverde AJ. Sex hormone-binding globulin concentrations before conception as a predictor for gestational diabetes in women with polycystic ovary syndrome. Hum Reprod. 2010;25:3123–8. [PubMed] [Google Scholar]
41. Urman B, Sarac E, Dogan L, Gurgan T. Pregnancy in infertile PCOD patients. Complications and outcome. J Reprod Med. 1997;42:501–5. [PubMed] [Google Scholar]
42. Li G, Fan L, Zhang L, Liu XW, Sun CJ, Zhang WY, et al. Clinical characteristics and perinatal outcomes of non-overweight/obese pregnant women with polycystic ovary syndrome. Zhonghua Yi Xue Za Zhi. 2011;91:2753–6. [PubMed] [Google Scholar]
43. Haakova L, Cibula D, Rezabek K, Hill M, Fanta M, Zivny J. Pregnancy outcome in women with PCOS and in controls matched by age and weight. Hum Reprod. 2003;18:1438–41. [PubMed] [Google Scholar]
Pregnancy outcome in women with PCOS and in controls matched by age and weight. Hum Reprod. 2003;18:1438–41. [PubMed] [Google Scholar]
44. Mikola M, Hiilesmaa V, Halttunen M, Suhonen L, Tiitinen A. Obstetric outcome in women with polycystic ovarian syndrome. Hum Reprod. 2001;16:226–9. [PubMed] [Google Scholar]
45. Turhan NO, Seçkin NC, Aybar F, Inegöl I. Assessment of glucose tolerance and pregnancy outcome of polycystic ovary patients. Int J Gynaecol Obstet. 2003;81:163–8. [PubMed] [Google Scholar]
46. Toulis KA, Goulis DG, Kolibianakis EM, Venetis CA, Tarlatzis BC, Papadimas I. Risk of gestational diabetes mellitus in women with polycystic ovary syndrome: A systematic review and a meta-analysis. Fertil Steril. 2009;92:667–77. [PubMed] [Google Scholar]
47. Roberts JM, Pearson G, Cutler J, Lindheimer M. Summary of the NHLBI Working Group on Research on Hypertension During Pregnancy. Hypertension. 2003;41:437–45. [PubMed] [Google Scholar]
48. Diamant YZ, Rimon E, Evron S. High incidence of preeclamptic toxemia in patients with polycystic ovarian disease. Eur J Obstet Gynecol Reprod Biol. 1982;14:199–204. [PubMed] [Google Scholar]
High incidence of preeclamptic toxemia in patients with polycystic ovarian disease. Eur J Obstet Gynecol Reprod Biol. 1982;14:199–204. [PubMed] [Google Scholar]
49. Radon PA, McMahon MJ, Meyer WR. Impaired glucose tolerance in pregnant women with polycystic ovary syndrome. Obstet Gynecol. 1999;94:194–7. [PubMed] [Google Scholar]
50. de Vries MJ, Dekker GA, Schoemaker J. Higher risk of preeclampsia in the polycystic ovary syndrome: A case control study. Eur J Obstet Gynecol Reprod Biol. 1998;76:91–5. [PubMed] [Google Scholar]
51. Ghazeeri GS, Nassar AH, Younes Z, Awwad JT. Pregnancy outcomes and the effect of metformin treatment in women with Polycystic Ovary Syndrome: An overview. Acta Obstet Gynecol Scand. 2012;91:658–78 [Epub ahead of print]. [PubMed] [Google Scholar]
52. Sir-Petermann T, Hitchsfeld C, Maliqueo M, Codner E, Echiburú B, Gazitúa R, et al. Birth weight in offspring of mothers with polycystic ovarian syndrome. Hum Reprod. 2005;20:2122–6. [PubMed] [Google Scholar]
53. Glueck CJ, Phillips H, Cameron D, Sieve-Smith L, Wang P. Continuing metformin throughout pregnancy in women with polycystic ovary syndrome appears to safely reduce first-trimester spontaneous abortion: A pilot study. Fertil Steril. 2001;75:46–52. [PubMed] [Google Scholar]
Glueck CJ, Phillips H, Cameron D, Sieve-Smith L, Wang P. Continuing metformin throughout pregnancy in women with polycystic ovary syndrome appears to safely reduce first-trimester spontaneous abortion: A pilot study. Fertil Steril. 2001;75:46–52. [PubMed] [Google Scholar]
54. Glueck CJ, Wang P, Goldenberg N, Sieve-Smith L. Pregnancy outcomes among women with polycystic ovary syndrome treated with metformin. Hum Reprod. 2002;17:2858–64. [PubMed] [Google Scholar]
55. Orio F, Jr, Palomba S, Cascella T, De Simone B, Manguso F, Savastano S, et al. Improvement in endothelial structure and function after metformin treatment in young normal-weight women with polycystic ovary syndrome: Results of a 6-month study. J Clin Endocrinol Metab. 2005;90:6072–6. [PubMed] [Google Scholar]
56. Jakubowicz DJ, Seppälä M, Jakubowicz S, Rodriguez-Armas O, Rivas-Santiago A, Koistinen H, et al. Insulin reduction with metformin increases luteal phase serum glycodelin and insulin-like growth factor-binding protein 1 concentrations and enhances uterine vascularity and blood flow in the polycystic ovary syndrome. J Clin Endocrinol Metab. 2001;86:1126–33. [PubMed] [Google Scholar]
J Clin Endocrinol Metab. 2001;86:1126–33. [PubMed] [Google Scholar]
57. Eng GS, Sheridan RA, Wyman A, Chi MM, Bibee KP, Jungheim ES, et al. AMP kinase activation increases glucose uptake, decreases apoptosis, and improves pregnancy outcome in embryos exposed to high IGF-I concentrations. Diabetes. 2007;56:2228–34. [PubMed] [Google Scholar]
58. Glueck C, Wang P, Kobayashi S, Phillips H, Sieve-Smith L. Metformin therapy throughout pregnancy reduces the development of gestational diabetes in women with polycystic ovary syndrome. Fertil Steril. 2002;77:520–5. [PubMed] [Google Scholar]
59. Vanky E, Salvesen KA, Heimstad R, Fougner KJ, Romundstad P, Carlsen SM, et al. Metformin reduces pregnancy complications without affecting androgen levels in pregnant polycystic ovary syndrome women: Results of a randomized study. Hum Reprod. 2004;19:1734–40. [PubMed] [Google Scholar]
60. Vanky E, Stridsklev S, Heimstad R, Romundstad P, Skogoy K, Kleggetveit O, et al. Metformin versus placebo from first trimester to delivery in polycystic ovary syndrome: A randomized, controlled multicenter study. J Clin Endocrinol Metab. 2010;95:E448–55. [PubMed] [Google Scholar]
J Clin Endocrinol Metab. 2010;95:E448–55. [PubMed] [Google Scholar]
61. Rowan JA, Gao W, Hague WM, McIntyre HD. Glycemia and its relationship to outcomes in the metformin in gestational diabetes trial. Diabetes Care. 2010;33:9–16. [PMC free article] [PubMed] [Google Scholar]
62. Khattab S, Mohsen IA, Aboul Foutouh I, Ashmawi HS, Mohsen MN, van Wely M, et al. Can metformin reduce the incidence of gestational diabetes mellitus in pregnant women with polycystic ovary syndrome. Prospective cohort study? Gynecol Endocrinol. 2011;27:789–93. [PubMed] [Google Scholar]
63. Fauser BCJM, Tarlatzis BC, Rebar RW, Legro RS, Balen AH, Lobo R, et al. Consensus on women's health aspects of polycystic ovary syndrome (PCOS): The Amsterdam ESHRE/ASRM-Sponsored 3 rd PCOS Consensus Workshop Group. Fertil Steril. 2012;97:28–38. [PubMed] [Google Scholar]
How to get pregnant with polycystic ovaries?
Polycystic disease is a common hormonal disease that affects a woman's ovaries. The dangers of PCOS include irregular menstrual periods, excessive hair growth, acne, weight gain, and other problems. Left untreated, PCOS can even lead to infertility. In this article we will tell you more about causes of polycystic , polycystic ovaries and pregnancy , and also give an answer to the question: “ Is it possible to give birth with polycystic ovaries? ".
The dangers of PCOS include irregular menstrual periods, excessive hair growth, acne, weight gain, and other problems. Left untreated, PCOS can even lead to infertility. In this article we will tell you more about causes of polycystic , polycystic ovaries and pregnancy , and also give an answer to the question: “ Is it possible to give birth with polycystic ovaries? ".
What is polycystic ovary syndrome?
Polycystic ovary syndrome (PCOS) is a hormonal disorder common among women of reproductive age. Women with PCOS may have menstrual irregularities and elevated levels of male hormones (androgens). Numerous small collections of fluid (follicles) may form in the ovaries, and an egg may not be released regularly. This condition should not be confused with multifollicular ovaries, because with multifollicular ovaries, ovulation and a normal menstrual cycle can persist, unlike polycystic disease. nine0019
50-75% of cases of endocrine infertility. 20-22% of marital infertility. It is detected in 5-16% of women of reproductive age. These are the figures for the diagnosis of "Polycystic Ovary".
20-22% of marital infertility. It is detected in 5-16% of women of reproductive age. These are the figures for the diagnosis of "Polycystic Ovary".
Symptoms of polycystic ovary syndrome
Polycystic ovary syndrome is accompanied by characteristic symptoms, upon noticing which it is necessary to seek advice from an endocrinologist or gynecologist. For some women, symptoms begin around the time of their first menstrual period. Others discover symptoms of PCOS only after they have gained a lot of weight or have trouble getting pregnant. In some cases, PCOS may be asymptomatic. nine0019
The most common symptoms of PCOS:
- Irregular periods. Lack of ovulation prevents the lining of the uterus from falling off every month. Some women with PCOS have fewer than eight periods a year, or none at all.
- Severe bleeding. The lining of the uterus builds up over a longer period of time, so menstruation may be heavier than usual.

- Hair growth . More than 70 percent of women with this condition grow hair on their face and body, including on their back, abdomen, and chest. Excess hair growth is called hirsutism.
- Acne . Male hormones can make the skin more oily than normal and cause breakouts on areas such as the face, chest, and upper back.
- Weight gain. Up to 80 percent of women with PCOS are overweight or obese.
- Male pattern baldness. nine0039 The hair on the scalp becomes thinner and may fall out.
- Darkening of the skin. Dark patches of skin may develop in body folds, such as the neck, groin area, and under the breasts.
- Headaches. Hormonal changes may cause headaches in some women.
Irregular periods
Infrequent, irregular periods, long or no periods are the most common symptom of PCOS. For example, with PCOS, you may have fewer than nine periods a year, more than 35 days between periods, and abnormally heavy periods. nine0019
nine0019
Hyperandrogenism
Hyperandrogenism is a disease characterized by high levels of androgens. It is more common in women than in men. Symptoms of hyperandrogenism may include acne, seborrhea (inflammation of the skin), hair loss on the scalp, increased body or facial hair, and infrequent or absent periods.
Hyperandrogenism is a defining feature of women and young girls with PCOS. Polycystic disease causes a malfunction of the ovaries or adrenal glands, which leads to the production of excess androgens (male sex hormones). nine0019
Anovulation
Anovulation occurs when an egg is not released from the ovary during the menstrual cycle. The egg is essential for pregnancy. Since several hormones are involved in ovulation, there are many causes of anovulation, one of which is PCOS. Chronic anovulation is a common cause of infertility.
Diagnosis
There is no test to definitively diagnose polycystic ovary syndrome (PCOS). The doctor will likely begin by discussing your medical history, including menstrual periods and weight changes.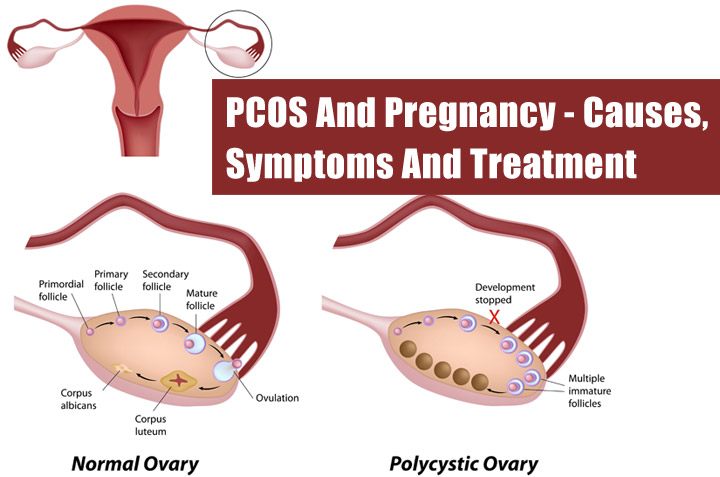 A physical exam will include checking for signs of excessive hair growth, acne, and weight gain. nine0019
A physical exam will include checking for signs of excessive hair growth, acne, and weight gain. nine0019
Your doctor may recommend:
- Gynecological examination. A physician visually and manually examines the reproductive organs for growths or other abnormalities.
- Blood tests. A blood test is given to determine the level of hormones. This will help rule out possible causes of menstrual irregularities or excess androgens that mimic PCOS. An additional blood test may also be needed to measure insulin resistance as well as fasting cholesterol and triglyceride levels. nine0041
- Ultrasound examination (ultrasound). The doctor will check the appearance of the ovaries and the thickness of the lining of the uterus. A rod-shaped device (sensor) (transvaginal ultrasound) is inserted into the vagina, which emits sound waves and converts them into images on a computer screen.
Is it possible to get pregnant with PCOS
How to get pregnant with PCOS? Getting pregnant with PCOS can be difficult, but that doesn't mean it's impossible. While PCOS can affect your hormones and therefore your fertility, there are medical treatments and lifestyle changes you can make to improve your chances of pregnancy. nine0019
While PCOS can affect your hormones and therefore your fertility, there are medical treatments and lifestyle changes you can make to improve your chances of pregnancy. nine0019
Is it possible to get pregnant with polycystic ovaries? To get pregnant, you must ovulate, which PCOS most often prevents. Women who do not ovulate regularly with PCOS do not release enough eggs for fertilization. Pregnancy with PCOS is further complicated by the fact that PCOS causes a hormonal imbalance that changes the quality of cervical fluid, making it difficult for sperm to survive.
It is impossible to say categorically that PCOS is infertility, but PCOS is one of the main causes of infertility in women. nine0019
Is it possible to get pregnant with PCOS? And although there are no exact statistics on the chances of pregnancy, 70 to 80 percent of women with PCOS have fertility problems. PCOS disrupts the normal menstrual cycle and makes it difficult to conceive.
Is it possible to get pregnant with PCOS? Polycystic ovary syndrome is not a sentence and it is possible to get pregnant, albeit problematic. However, if PCOS is left untreated, the chances of getting pregnant decrease with age.
However, if PCOS is left untreated, the chances of getting pregnant decrease with age.
It is possible to get pregnant with polycystic disease, but most often pregnancy with polycystic disease is difficult. This condition can increase the risk of pregnancy complications. Women with PCOS are twice as likely to have a preterm birth than women without. They are also at greater risk of miscarriage, high blood pressure, and gestational diabetes. However, by managing the symptoms, many women with PCOS can become pregnant and have a healthy baby.
How to get pregnant with PCOS? Women with PCOS can become pregnant using fertility treatments that improve ovulation. Losing weight and lowering your blood sugar can increase your chances of a healthy pregnancy. nine0019
Planning pregnancy with PCOS
How to get pregnant with PCOS? While your chances of getting pregnant with PCOS may be lower, there are a few things you can do to increase those chances.
- Call your doctor.
 How to get pregnant with polycystic ovaries? Normalization of hormones and menstruation is the first step. Your doctor may prescribe medications to help your body deal with insulin better and regulate your menstrual cycle. nine0039
How to get pregnant with polycystic ovaries? Normalization of hormones and menstruation is the first step. Your doctor may prescribe medications to help your body deal with insulin better and regulate your menstrual cycle. nine0039 - Maintain a healthy weight. Is it possible to get pregnant with PCOS? Weight loss can lower insulin levels, androgen levels, and restore ovulation. Ask your doctor about a weight management program and meet with a nutritionist regularly for help with your weight loss goals.
- Eat right. Polycystic Ovarian Diet includes sugary foods, simple carbohydrates and unhealthy fats. Add to your menu: fresh and cooked fruits and vegetables, whole grains such as brown rice, oats and barley, beans and lentils, chicken, fish. nine0041
- Be active. Exercise helps lower blood sugar levels. How to get pregnant with insulin resistance? If you have PCOS, increasing daily activity such as walking, exercising, walking can help treat or even prevent insulin resistance, control your weight, and avoid developing diabetes.
- Lead a healthy lifestyle. Follow a healthy lifestyle with PCOS, give up bad habits, unhealthy diet, lack of sports and irregular sleep. nine0041
Treatment for PCOS
Treatment for PCOS focuses on your individual problems such as infertility, acne or obesity. Also, the direction of PCOS treatment largely depends on whether a woman is planning a pregnancy or not. Specific treatment may include lifestyle changes or medications.
How to treat PCOS?
Lifestyle changes
Your doctor may recommend weight loss through a low-calorie diet combined with moderate exercise. Even small weight loss - like losing 5 percent of your body weight - can improve your condition. Can you get pregnant with PCOS? Losing weight can also increase the effectiveness of medications your doctor recommends to treat PCOS and help with infertility. nine0019
Treatment with drugs for polycystic ovaries
To regulate the menstrual cycle, the doctor may recommend:
Combination birth control pills. Estrogen and progestin tablets reduce androgen production and regulate estrogen. Hormone regulation can reduce the risk of endometrial cancer and correct abnormal bleeding, excess hair growth, and acne. Instead of pills, you can use a skin patch or vaginal ring containing a combination of estrogen and progestin. nine0019
Estrogen and progestin tablets reduce androgen production and regulate estrogen. Hormone regulation can reduce the risk of endometrial cancer and correct abnormal bleeding, excess hair growth, and acne. Instead of pills, you can use a skin patch or vaginal ring containing a combination of estrogen and progestin. nine0019
Progestin therapy. Daily progestin may: restore normal hormonal balance, regulate ovulation, stop excessive hair growth, protect against endometrial cancer, and help get pregnant with sleep deprivation.
How to induce ovulation in PCOS? To help induce ovulation in PCOS, your doctor may recommend:
Clomiphene is a fertility medication that can help women with PCOS get pregnant.
Metformin is a drug used to treat type 2 diabetes. It also treats PCOS by increasing insulin levels.
Operation
How to get pregnant with PCOS? Surgery may be an option to improve fertility if other treatments don't work. Ovarian drilling is a procedure in which tiny holes are made in the ovary using a laser or a thin, heated needle to restore normal ovulation and the possibility of pregnancy with PCOS. nine0019
Ovarian drilling is a procedure in which tiny holes are made in the ovary using a laser or a thin, heated needle to restore normal ovulation and the possibility of pregnancy with PCOS. nine0019
Important! To determine the right treatment and choose the right drug, you need to consult a doctor!
Help Doc.ua: you can make an appointment with a gynecologist-endocrinologist on the website.
PCOS and pregnancy - how does polycystic ovary syndrome reduce the chance of getting pregnant?
PCOS is one of the most common causes of female infertility. Patients with polycystic ovary syndrome may have difficulty getting pregnant and have trouble carrying a pregnancy. The treatment of PCOS and the choice of appropriate therapy largely depend on the severity of the events that have occurred. nine0019
Pregnancy in women with PCOS
The main obstacle to getting pregnant in women struggling with PCOS is:
- the occurrence of anovulatory cycles.
The diagnosis of PCOS does not mean that a woman has no chance of getting pregnant naturally. A lot depends on the degree and type of disorder. Many women with mild PCOS require no special treatment and, despite less frequent ovulation, become mothers without any problems. At the same time, there are patients with a more severe form of this disease who already need pharmacotherapy or the use of medical insemination methods in order to achieve the desired pregnancy. nine0019
Do you have any questions? Contact us!
PCOS and pregnancy
A woman with PCOS has a higher risk of miscarriage as well as gestational diabetes, which can pose health risks to mother and baby. In the presence of cysts in the ovaries, changes in their size should also be systematically checked. Cysts are usually harmless, but large cysts can pose a potential threat during pregnancy, as rupture can lead to threatened preterm labor or miscarriage. nine0019
Diagnosis and treatment of PCOS
Polycystic ovary syndrome can worsen over the years, which is why correct, early diagnosis is so important to effectively prevent the development and symptoms of the disease. The age factor is also important, therefore, if possible, it is advisable not to postpone pregnancy plans for later years. Standards have been developed for the treatment of PCOS. Sometimes all it takes to improve fertility is:
The age factor is also important, therefore, if possible, it is advisable not to postpone pregnancy plans for later years. Standards have been developed for the treatment of PCOS. Sometimes all it takes to improve fertility is:
- lifestyle changes,
- healthy eating,
- exercise.
Some patients need pharmacological support. Properly selected drugs are aimed at regulating the monthly circus and restoring ovulation, without which fertilization cannot occur. In the event that a woman with PCOS fails to conceive after using various treatments, medical insemination methods may be used.
Testing for other causes of infertility
If a woman with PCOS is unsuccessfully trying to conceive, it is also important to check for other disorders that can lead to infertility besides PCOS, such as:
- poor sperm parameters for the partner.
A complete couples diagnosis, both for men and women, is necessary if there are problems with the onset of pregnancy.