Signs of miscarriage in the second trimester
Understanding Second Trimester Loss | Obstetrics and Gynecology
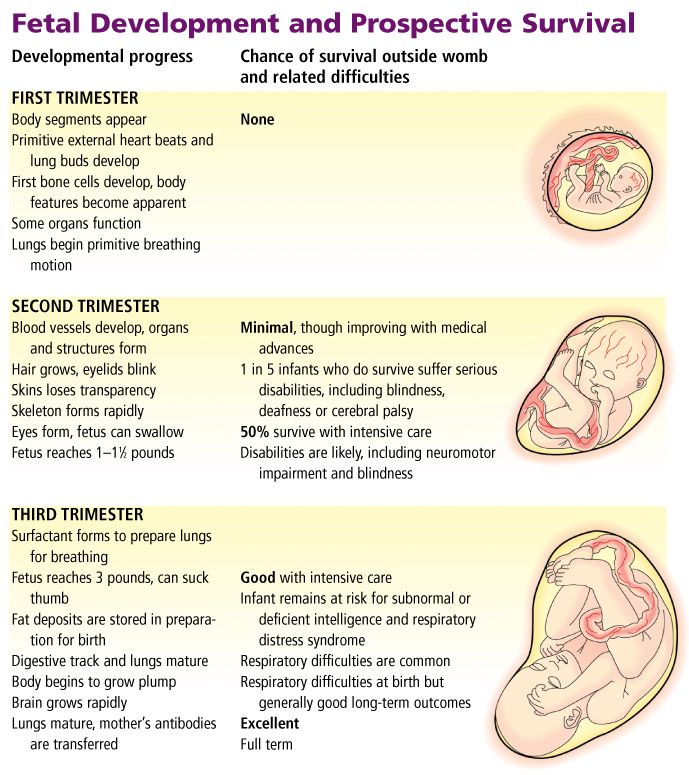
Pregnancy loss in the second trimester can be the result of a very preterm delivery (like a spontaneous miscarriage in the second trimester) or death of the fetus (called a fetal demise). About 2-3% of pregnancies will be lost in the second trimester, a rate that is much lower than in the first trimester. Once a pregnancy gets to about 20 weeks gestation, less than 0.5% will end in a fetal demise.
A loss at this time in pregnancy is most often a hard and sad experience. Many friends and family already know you are pregnant. What do you do? What do you say? For most women and their partners, the process of grieving is no different than losing a person who has been in your life for some time. You often have hopes and dreams about your child before that child is born, and losing the pregnancy in the second or third trimester is certainly a loss for a family.
Why see a UC Davis Health specialist?
Our specialists can evaluate you quickly in an office setting. Any laboratory testing or ultrasound examinations that need to be done can be performed easily and conveniently. We perform our own ultrasound examination in the office and can share the results with you immediately. Treatment of a second trimester loss is very different than early miscarriage, and our specialists can provide all options to you and your family. We understand that losses at this time require both emotional and medical support. We are happy to review all treatment options but also know that you may need some time. It is also important for you to know that a fetal demise in the second trimester is not a medical emergency so treatment is not immediately indicated.
If you are having very heavy vaginal bleeding or are feeling very sick, you should go to the Emergency Room to see our physicians.
Symptoms of a second trimester loss
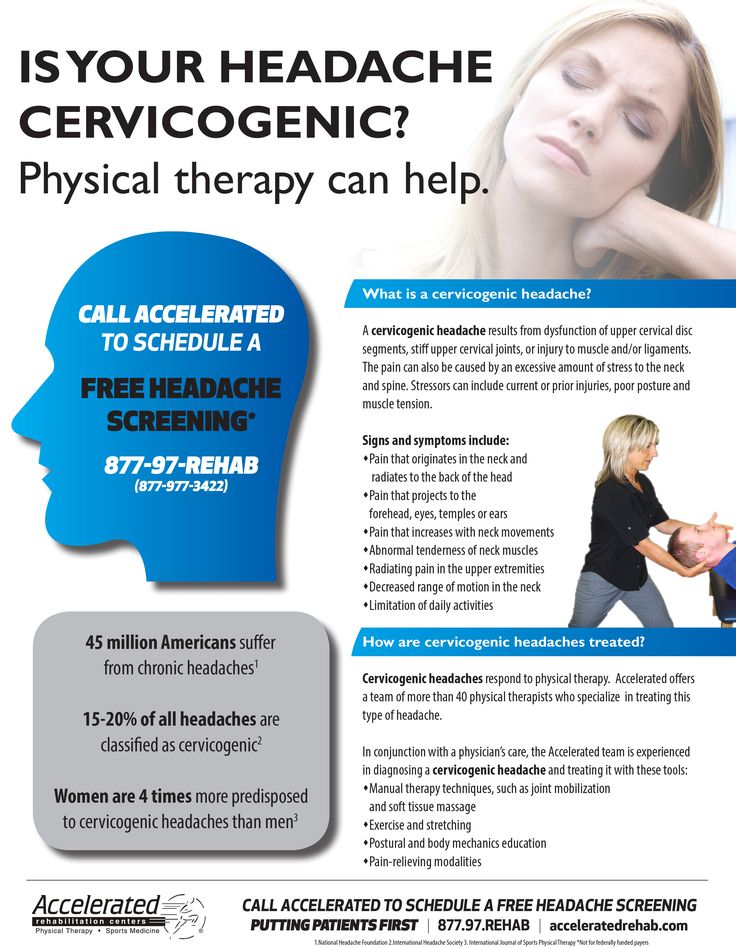
- Bleeding: Most commonly, bleeding is a sign of a problem with the placenta and does not indicate a fetal demise. But, bleeding can be a sign that the cervix is opening without labor (called cervical insufficiency).
 With cervical insufficiency, the cervix begins to open early without contractions; as the cervix opens more, contractions then follow.
With cervical insufficiency, the cervix begins to open early without contractions; as the cervix opens more, contractions then follow. - Cramping: Pregnancy losses in the second trimester can be due to early labor.
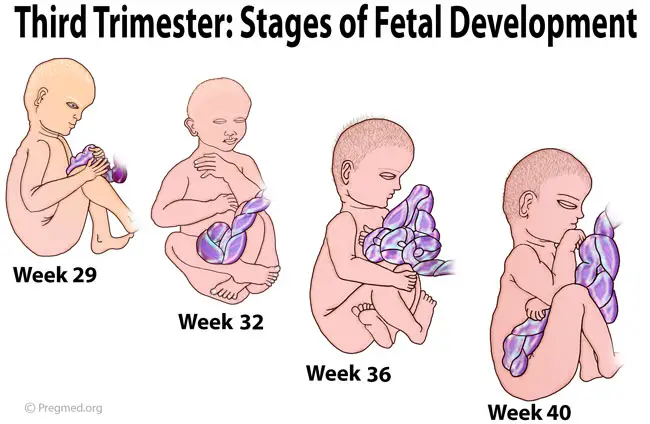
- Loss of fetal movement: This can indicate a fetal demise. Most women can feel the baby moving by the 20th week. If the baby has been moving and you no longer feel that same movement, it is important to contact the doctor’s office immediately to make sure the baby is fine. Decreased fetal movement is more commonly a sign that there is a problem with the pregnancy and only rarely does it mean the fetus has died.
Most women less than 20 weeks of pregnancy do not notice any symptoms of a fetal demise.
The test used to check for a fetal demise in the second trimester is an ultrasound examination to see if the baby is moving and growing. Fetal demise is diagnosed when the ultrasound examination shows no fetal heart activity.
What causes a second trimester loss?
The causes of a pregnancy loss in the second trimester are very different than early pregnancy loss. There are medical conditions that increase the risk for cervical insufficiency or preterm labor before viability which include:
There are medical conditions that increase the risk for cervical insufficiency or preterm labor before viability which include:
- Prior surgery to the cervix
- Use of illicit drugs, especially cocaine
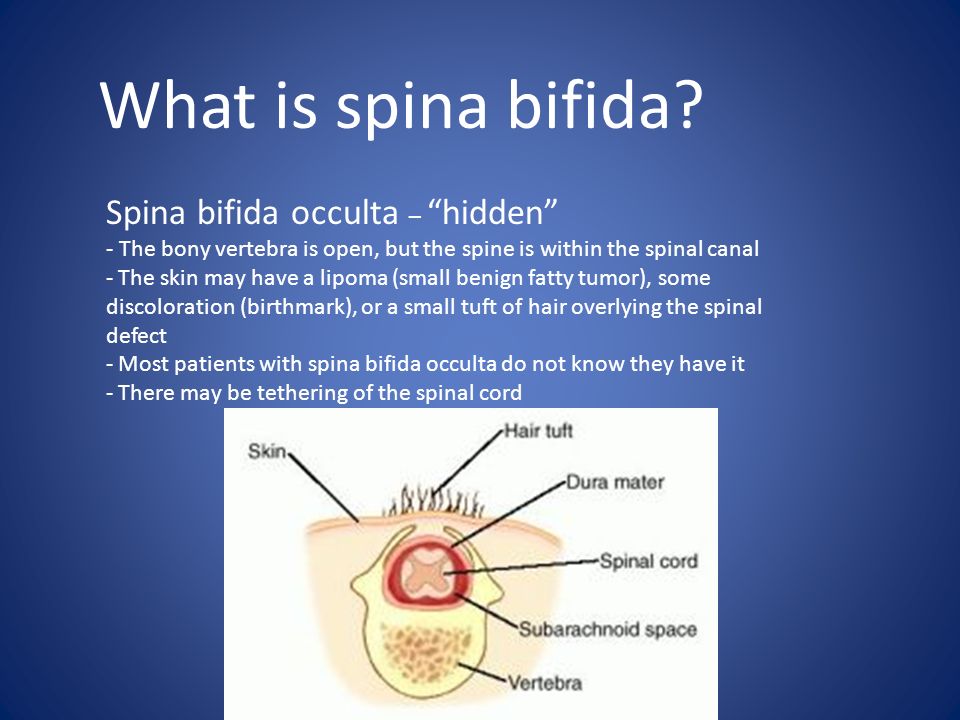
- Fetal abnormalities (genetic or structural problems)
- Uterine infection (this is more common in developing countries and less common in the United States)
- Physical problems with the uterus, including fibroids or abnormalities in the shape of the uterus
There are also some medical conditions that are associated with fetal death in the second trimester which include:
- Fetal abnormalities (genetic or structural problems)
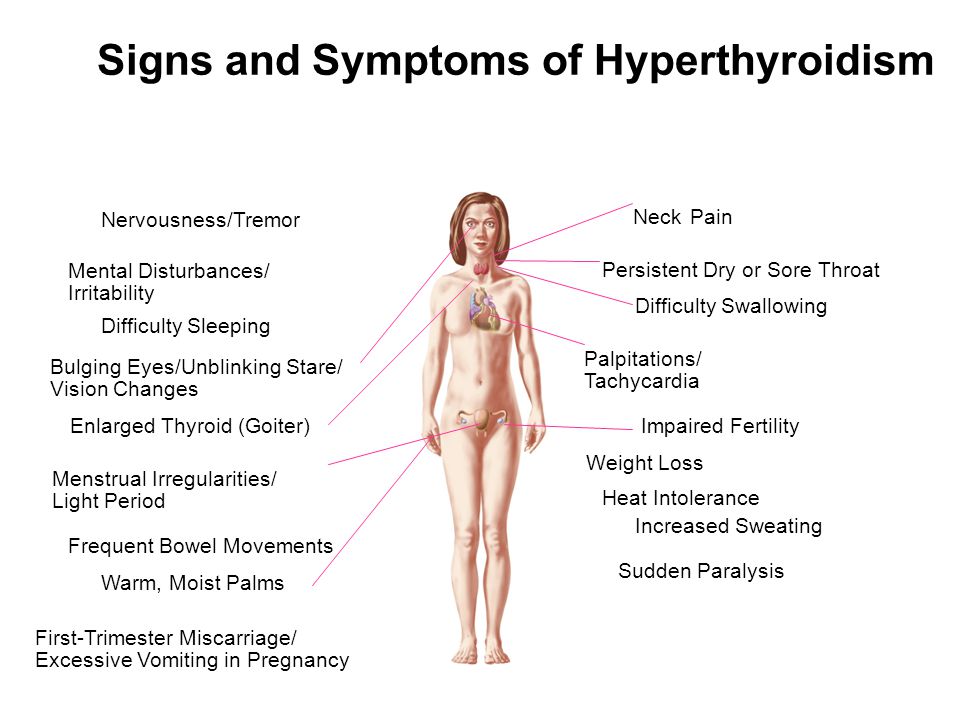
- Poorly controlled maternal cnoditions like thyroid disease, diabetes or hypertension
- Lupus (systemic lupus erythematosus)
- Autoimmune or genetic conditions that increase a woman’s risk of forming blood clots in her legs or her lungs (like antiphospholipid syndrome)
- Very early pre-eclampsia or eclampsia of pregnancy
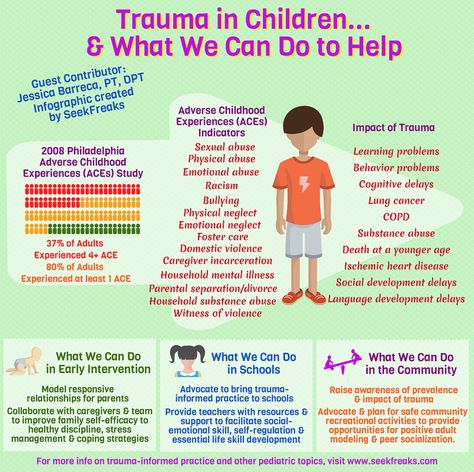
- Trauma
The specialists at UC Davis Health will review with you what testing is indicated to help learn more about why a second trimester loss occurred. Despite the testing that is available, about half of the time there is no identifiable reason for a second trimester loss. We can work with you to figure out what may be helpful with a next pregnancy or to learn more about medical issues that are important for your future.
Despite the testing that is available, about half of the time there is no identifiable reason for a second trimester loss. We can work with you to figure out what may be helpful with a next pregnancy or to learn more about medical issues that are important for your future.
Treatment of a second trimester loss
It is typically not safe for a woman to wait for the pregnancy to deliver on its own with a second trimester loss. There is a high chance of having significant bleeding when a pregnancy in the second trimester delivers on its own at home. In the case of fetal demise, a dead fetus that has been in the uterus for 4 weeks can cause changes in the body’s clotting system. These changes can put a woman at a much higher chance of significant bleeding if she waits for a long time after the fetal demise to deliver the pregnancy.
Our doctors are committed to providing all available treatment options. Testing to figure out the cause of the pregnancy loss can be performed regardless of the method a woman chooses for termination.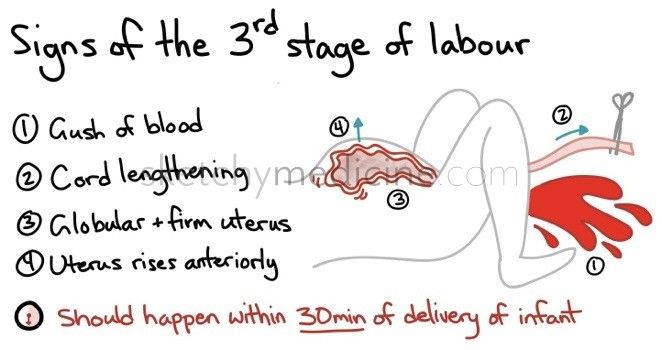
We understand that a second trimester loss is an emotional and stressful time and we want to ensure that the emotional needs of you and your family are met as well. We understand this is a time that you need support and we are sensitive to your wishes for remembrances and religious preferences. We will discuss these issues with you before any treatment.
When a diagnosis of fetal demise in the second or third trimester is made, options include:
- Surgical evacuation: This procedure, called a dilation and evacuation, can be performed in the second trimester, typically up to about 24 weeks. Surgical evacuation is the most common treatment women choose and involves removing the pregnancy through the cervix in the operating room while you are asleep. The cervix needs to be opened about 1-2 inches in diameter. The doctors can use different ways to open the cervix based on how far along the pregnancy is and your individual circumstance. The goal is to provide the safest care for each patient.
 After a surgical evacuation, normal activity can typically be resumed the following day. Opening or preparing the cervix for surgical evacuation of the pregnancy may involve:
After a surgical evacuation, normal activity can typically be resumed the following day. Opening or preparing the cervix for surgical evacuation of the pregnancy may involve: - Medicines (tablets) that are put in the vagina a few hours to one day before the procedure.
- Medicine (tablets) that you hold between your cheek and gums for 30 minutes before swallowing. You would use this medicine a few hours before the procedure.
- Placing thin sticks in your cervix, called osmotic dilators, to absorb water from the cervix which causes the dilator sticks to swell slowly over 4-24 hours. Having the osmotic dilators placed is similar to getting a Pap test.
Labor induction: This treatment uses medicines to cause the uterus to go into labor. For women with pregnancies beyond 24 weeks, this is commonly the only option. If you choose this option, you will be in the Labor and Delivery Unit at UC Davis Medical Center and will have all of the same pain treatments available to you as a woman who is naturally in labor (like IV pain medications or an epidural).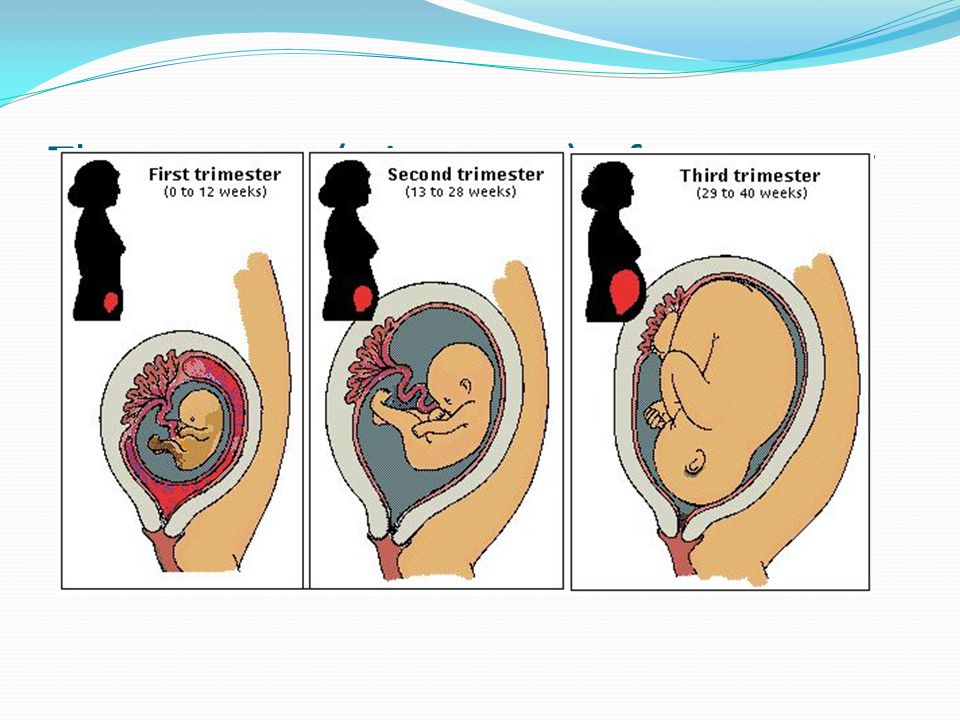 The treatment typically starts with swallowing a pill to make the uterus more sensitive to the medications to induce labor. About 24 hours later, you are admitted to the Labor and Delivery Unit and will have medicine (tablets) put in the vagina every few hours to cause labor. Sometimes, women need medicine through an IV to also help get labor started. It may take 1-2 days for the uterus to go into labor and for the delivery to be complete. Up to 5% of women in the second trimester do not go into labor and need a surgical evacuation.
The treatment typically starts with swallowing a pill to make the uterus more sensitive to the medications to induce labor. About 24 hours later, you are admitted to the Labor and Delivery Unit and will have medicine (tablets) put in the vagina every few hours to cause labor. Sometimes, women need medicine through an IV to also help get labor started. It may take 1-2 days for the uterus to go into labor and for the delivery to be complete. Up to 5% of women in the second trimester do not go into labor and need a surgical evacuation.
Your doctor will be able to explain more details about the pros and cons of each treatment.
After treatment of a second trimester loss
Bleeding may continue for several weeks after a labor induction but tends to be much lighter with a surgical evacuation. Any bleeding may change in color from bright red to pink or brown. Lower abdominal cramping in the few days after treatment is also common. You should contact a doctor right away if the bleeding gets heavier instead of lighter over time, if a fever develops, or if vaginal discharge or a strange or unpleasant vaginal odor occurs. Avoid intercourse, douching, or using tampons for one week. Regular activities can be resumed right away, based on how you feel. Importantly, if you want to delay getting pregnant, it will be very important to start an effective method of contraception.
Avoid intercourse, douching, or using tampons for one week. Regular activities can be resumed right away, based on how you feel. Importantly, if you want to delay getting pregnant, it will be very important to start an effective method of contraception.
FAQs about second trimester loss
Q: What is cervical insufficiency?
A: This diagnosis is made when a woman has dilation of the cervix during the second trimester without having any contractions or signs of a uterine infection. Some studies suggest that some types of surgeries performed when women have advanced pre-cancerous changes in the cervix can increase the risk of cervical insufficiency. These surgeries include cervical conization (also known as a “cone biopsy”) or if a patient has had multiple LEEP procedures. With these surgeries, part of the cervix is removed to get rid of the pre-cancerous changes. Having these procedures increases the risk of having a second trimester loss by about 1%. In women who have these types of procedures, the chance of having cervical insufficiency is about 1.5%.
In women who have these types of procedures, the chance of having cervical insufficiency is about 1.5%.
Q: What treatments are available if one of the tests shows I have a medical problem that increased the chance of a second trimester loss?
A: Our specialists will work with you to maximize your health status before you try to get pregnant again. For some women, this may mean treatment of a thyroid condition, improved control of diabetes, or changing medications being used for chronic illnesses. Some conditions may require blood thinners like aspirin or injectable medications that should be started early in the next pregnancy (after a normal pregnancy is seen with an early ultrasound exam).
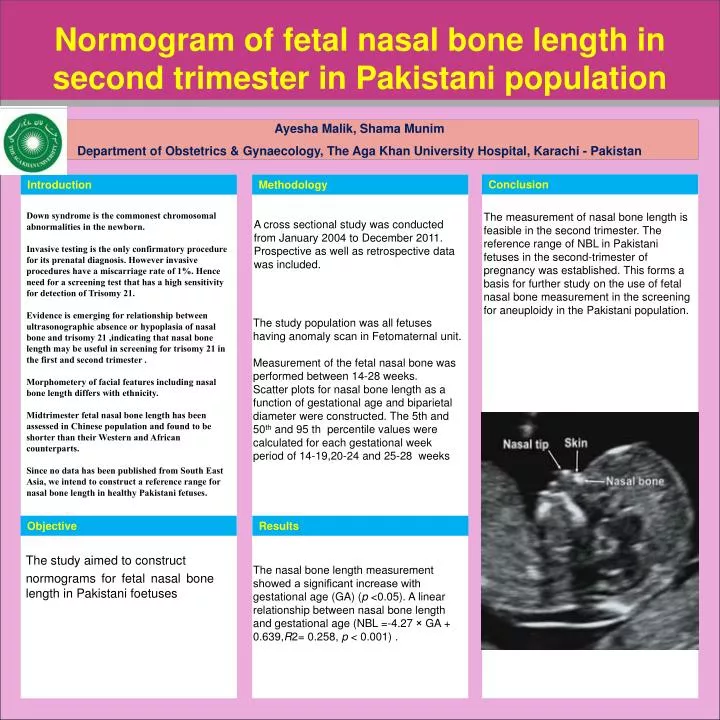
Q: In my last pregnancy, I didn’t get any genetic testing and had a second trimester demise related to a genetic abnormality. What genetic testing is available for my next pregnancy to help figure out if the pregnancy is normal so I can learn earlier if the pregnancy is genetically normal?
A: It will be important to meet with a genetic counselor, if possible, before your next pregnancy, who can also review the details of the available tests. The counselor can also talk with you more about your history and your family history to make sure no genetic or familial medical problems are missed. There are a few different tests, all of which can be performed early in pregnancy, depending on what is right for you. Screening for some of the most common chromosomal abnormalities just from your blood (called NIPT or non-invasive prenatal testing). First trimester screening can be performed between 11 and 14 weeks which involves a blood test and an ultrasound examination. In some situations, chorionic villus sampling (a biopsy of the placenta) or expanded prenatal screening may be indicated. Our specialists and genetic counselors can work with you and your family to help you understand all of these tests and figure out what approach is right for you.
The counselor can also talk with you more about your history and your family history to make sure no genetic or familial medical problems are missed. There are a few different tests, all of which can be performed early in pregnancy, depending on what is right for you. Screening for some of the most common chromosomal abnormalities just from your blood (called NIPT or non-invasive prenatal testing). First trimester screening can be performed between 11 and 14 weeks which involves a blood test and an ultrasound examination. In some situations, chorionic villus sampling (a biopsy of the placenta) or expanded prenatal screening may be indicated. Our specialists and genetic counselors can work with you and your family to help you understand all of these tests and figure out what approach is right for you.
Q: After a second trimester loss, how long should I wait before I try to conceive again?
A: There is really no good information available to show the absolute right answer to that question.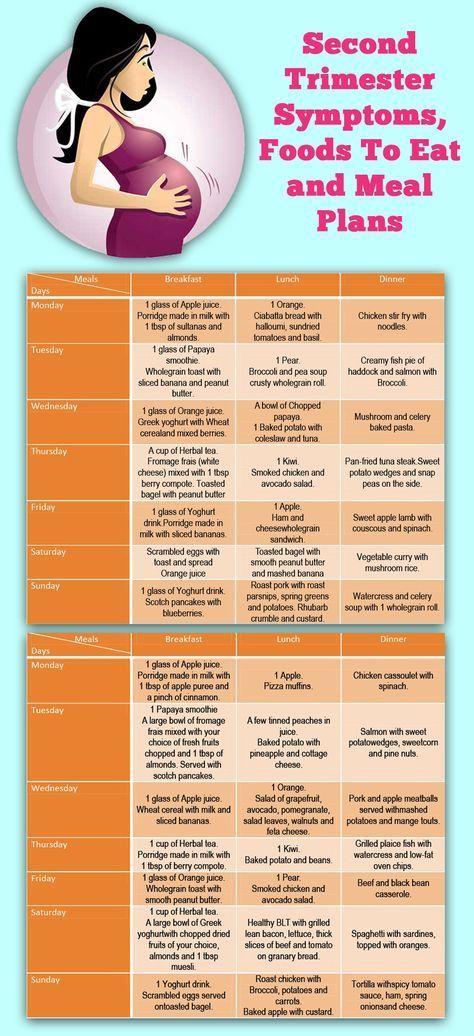 First, it may take a month or two to have any testing completed to help figure out why you had a second trimester loss. We know that it takes some time for your uterus and your body to get back to normal. The specialists at UC Davis usually recommend waiting at least 3 months after a second trimester loss before trying again to get pregnant.
First, it may take a month or two to have any testing completed to help figure out why you had a second trimester loss. We know that it takes some time for your uterus and your body to get back to normal. The specialists at UC Davis usually recommend waiting at least 3 months after a second trimester loss before trying again to get pregnant.
Miscarriage Symptoms, Causes, Diagnosis, and Treatment
Written by WebMD Editorial Contributors
In this Article
- What Is a Miscarriage?
- Miscarriage Symptoms
- Miscarriage Causes and Risk Factors
- Miscarriage Types
- Miscarriage Diagnosis
- Miscarriage Treatments
- Symptoms Following a Miscarriage
- Pregnancy Following a Miscarriage
- When to Try to Conceive After a Miscarriage
- Miscarriage Prevention
What Is a Miscarriage?
A miscarriage is the loss of a baby before the 20th week of pregnancy. The medical term for a miscarriage is spontaneous abortion.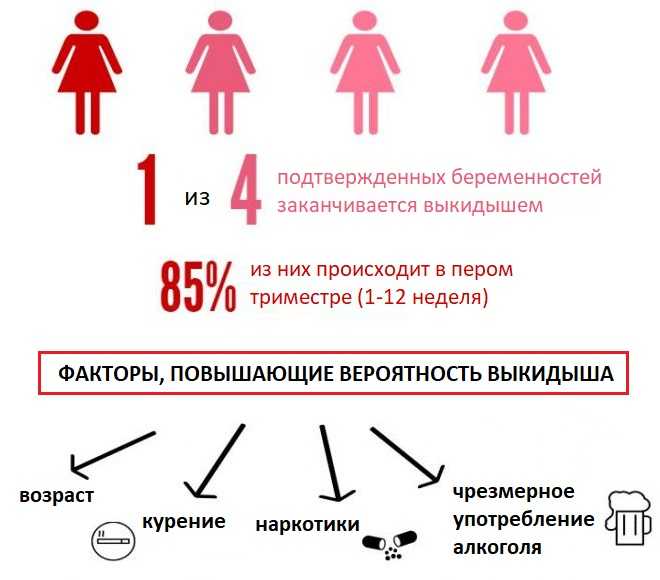 But it isn’t an abortion in the common meaning of the term.
But it isn’t an abortion in the common meaning of the term.
As many as 50% of all pregnancies end in miscarriage -- most often before a woman misses a menstrual period or even knows they’re pregnant. About 15%-25% of recognized pregnancies will end in a miscarriage.
More than 80% of miscarriages happen within the first 3 months of pregnancy. Miscarriages are less likely to happen after 20 weeks. When they do, doctors call them late miscarriages.
Miscarriage Symptoms
Symptoms of a miscarriage include:
- Bleeding that goes from light to heavy
- Severe cramps
- Belly pain
- Weakness
- Worsening or severe back pain
- Fever with any of these symptoms
- Weight loss
- White-pink mucus
- Contractions
- Tissue that looks like blood clots passing from your vagina
- Fewer signs of pregnancy
If you have these symptoms, contact your doctor right away.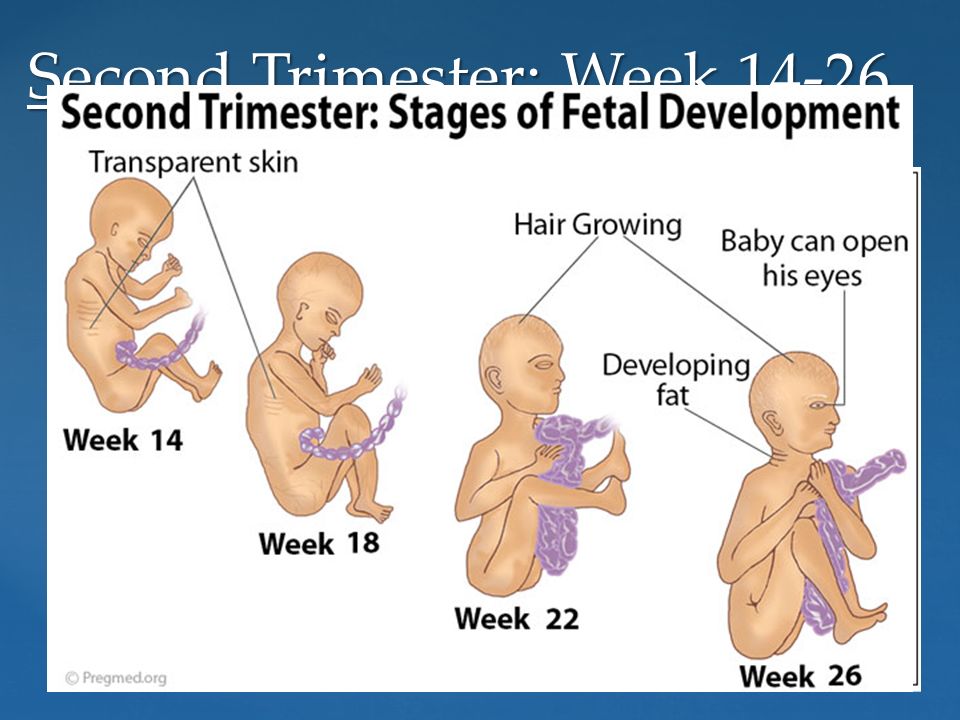 They’ll tell you whether to come to the office or go to the emergency room.
They’ll tell you whether to come to the office or go to the emergency room.
Miscarriage Causes and Risk Factors
Most miscarriages happen when the unborn baby has fatal genetic problems. Usually, these problems are not related to the mother.
Other problems that can increase the risk of miscarriage include:
- Infection
- Medical conditions in the mother, such as diabetes or thyroid disease
- Hormone problems
- Immune system responses
- Physical problems in the mother
- Uterine abnormalities
- Smoking
- Drinking alcohol
- Using street drugs
- Exposure to radiation or toxic substances
A woman has a higher risk of miscarriage if they:
- Are over age 35
- Have certain diseases, such as diabetes or thyroid problems
- Have had three or more miscarriages
Cervical insufficiency. A miscarriage sometimes happens when the mother has a weakness of the cervix. Doctors call this a cervical insufficiency. It means the cervix can’t hold the pregnancy. This type of miscarriage usually happens in the second trimester.
A miscarriage sometimes happens when the mother has a weakness of the cervix. Doctors call this a cervical insufficiency. It means the cervix can’t hold the pregnancy. This type of miscarriage usually happens in the second trimester.
There are usually few symptoms before a miscarriage caused by cervical insufficiency. You may feel sudden pressure, your water might break, and tissue from the baby and placenta could leave your body without much pain. Doctors usually treat an insufficient cervix with a "circling" stitch in the next pregnancy, usually around 12 weeks. The stitch holds your cervix closed until the doctor removes it around the time of delivery. If you never had a miscarriage but your doctor finds that you have cervical insufficiency they might add the stitch to prevent a miscarriage.
Miscarriage Types
There are different kinds of miscarriages, including:
Threatened miscarriage. You’re bleeding and there’s the threat of a miscarriage, but your cervix hasn’t dilated.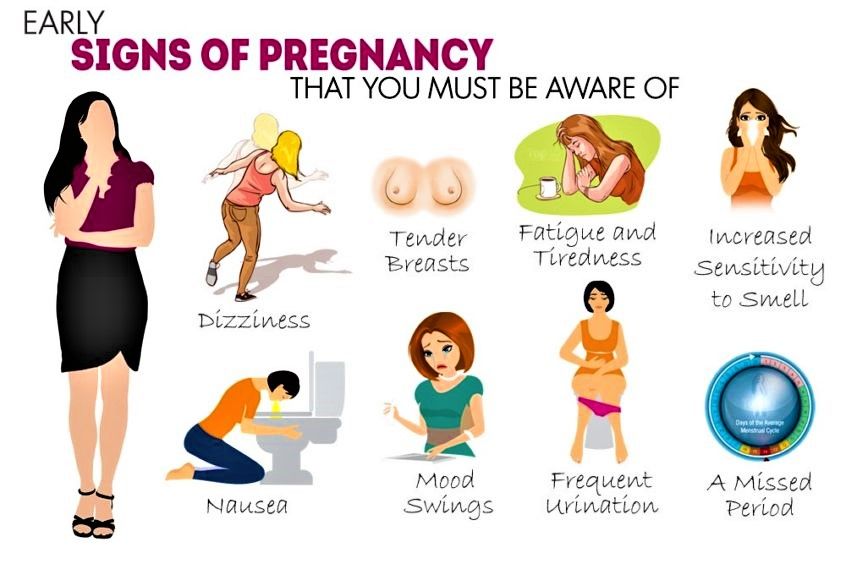 Your pregnancy will likely continue without any problems.
Your pregnancy will likely continue without any problems.
Inevitable miscarriage. You’re bleeding and cramping. Your cervix is dilated. A miscarriage is likely.
Incomplete miscarriage. Some tissue from the baby or the placenta leaves your body, but some stays in your uterus.
Complete miscarriage. All the pregnancy tissues leave your body. This type of miscarriage usually happens before the 12th week of pregnancy.
Missed miscarriage. The embryo dies or was never formed, but the tissues stay in your uterus.
Recurrent miscarriage (RM). You lose three or more pregnancies in a row during the first trimester. This type of miscarriage only affects about 1% of couples trying to have a baby.
Miscarriage Diagnosis
To check whether you've had a miscarriage, your doctor will do:
- A pelvic exam. They’ll check to see if your cervix has started to dilate.
- An ultrasound test.
 This test uses sound waves to check for a baby’s heartbeat. If the results aren’t clear, you may go back for another test in a week.
This test uses sound waves to check for a baby’s heartbeat. If the results aren’t clear, you may go back for another test in a week. - Blood tests. The doctor uses them to look for pregnancy hormones in your blood and compare it to past levels. They may also test you for anemia if you’ve been bleeding a lot.
- Tissue tests. If tissue left your body, the doctor may send it to a lab to confirm that you had a miscarriage. It can also help make sure there wasn’t another cause for your symptoms.
- Chromosome tests. If you’ve had two or more miscarriages, the doctor might do these tests to see if you or your partner’s genes are the cause.
Miscarriage Treatments
If the miscarriage is complete and your uterus is empty, you probably won’t need further treatment.
Sometimes all the tissue doesn’t come out. If that happens, your doctor might do a dilation and curettage (D&C) procedure. They’ll dilate your cervix and gently remove any remaining tissue. There are also medications you can take that cause any tissue left in your uterus to leave your body. This may be a better option if you want to avoid surgery.
There are also medications you can take that cause any tissue left in your uterus to leave your body. This may be a better option if you want to avoid surgery.
If it’s later in the pregnancy and the fetus has died in the womb, the doctor will induce labor and delivery.
When the bleeding stops, you should be able to go back to your normal activities. If your cervix dilated on its own but you’re still pregnant, you could have a condition known as incompetent cervix. Your doctor might do a procedure to close it called cerclage.
If your blood type is Rh negative, the doctor may give you a blood product called Rh immune globulin (Rhogam). This prevents you from developing antibodies that could harm your baby or any future pregnancies.
You may get blood tests, genetic tests, or medication if you’ve had more than two miscarriages in a row (recurrent miscarriage). To diagnose this condition, your doctor might use tests like:
- Pelvic ultrasound
- Hysterosalpingogram, An X-ray of the uterus and fallopian tubes
- Hysteroscopy.
 The doctor uses a thin, telescope-like device inserted through your vagina and cervix to look inside your uterus
The doctor uses a thin, telescope-like device inserted through your vagina and cervix to look inside your uterus
If you've had two miscarriages in a row, use a form of birth control and talk to your doctor about tests to find the cause
Symptoms Following a Miscarriage
Bleeding and mild discomfort are common symptoms after a miscarriage. If you have heavy bleeding with fever, chills, or pain, contact your doctor right away. These may be signs of an infection.
Besides the physical effects, you may also feel a range of emotions, from sadness and guilt to grief and worry about future pregnancies. What you’re feeling is normal. Let yourself grieve.
If you’re up to it, talk to people in your life who are supportive like your partner, a friend, or family member. You can also talk to a professional mental health counselor. Pregnancy loss support groups may also be a valuable resource to you and your partner. Ask your doctor for more information about these resources.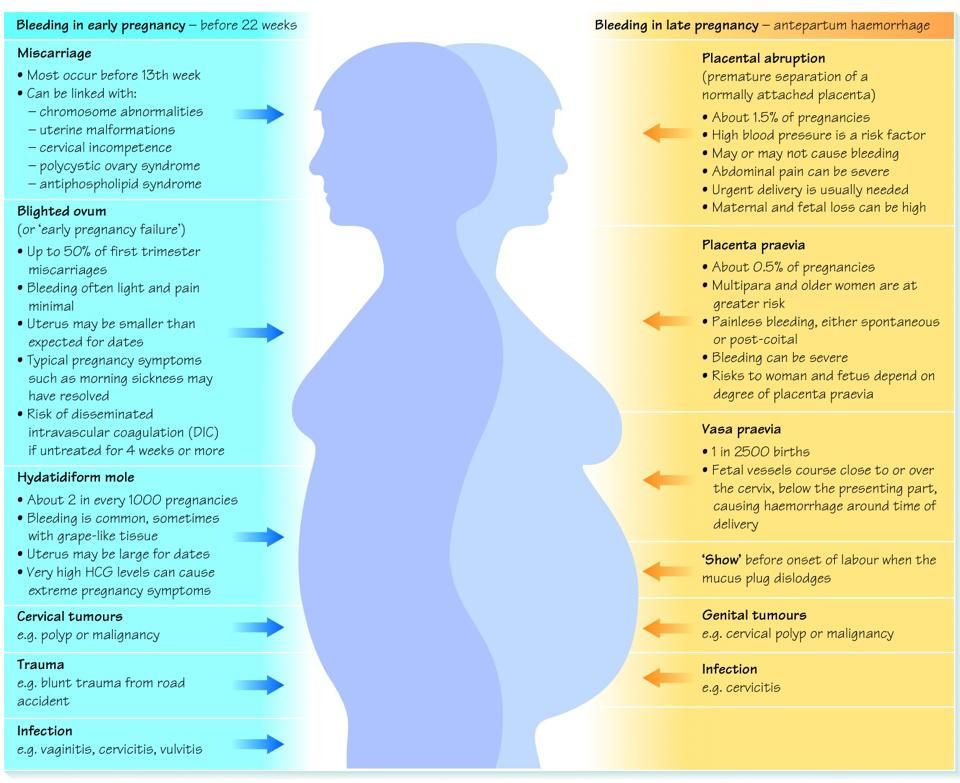 And remember that everyone heals at a different pace and in different ways.
And remember that everyone heals at a different pace and in different ways.
Pregnancy Following a Miscarriage
You can get pregnant after a miscarriage. At least 85% of women who have one go on to have normal pregnancies and births. Having a miscarriage doesn’t mean you have a fertility problem. On the other hand, about 1%-2% of women may have repeated miscarriages (three or more). Some researchers believe this is related to an autoimmune response.
If you've had two miscarriages in a row, you should stop trying to conceive, use a form of birth control, and ask your doctor to do tests to figure out what’s causing the miscarriages.
When to Try to Conceive After a Miscarriage
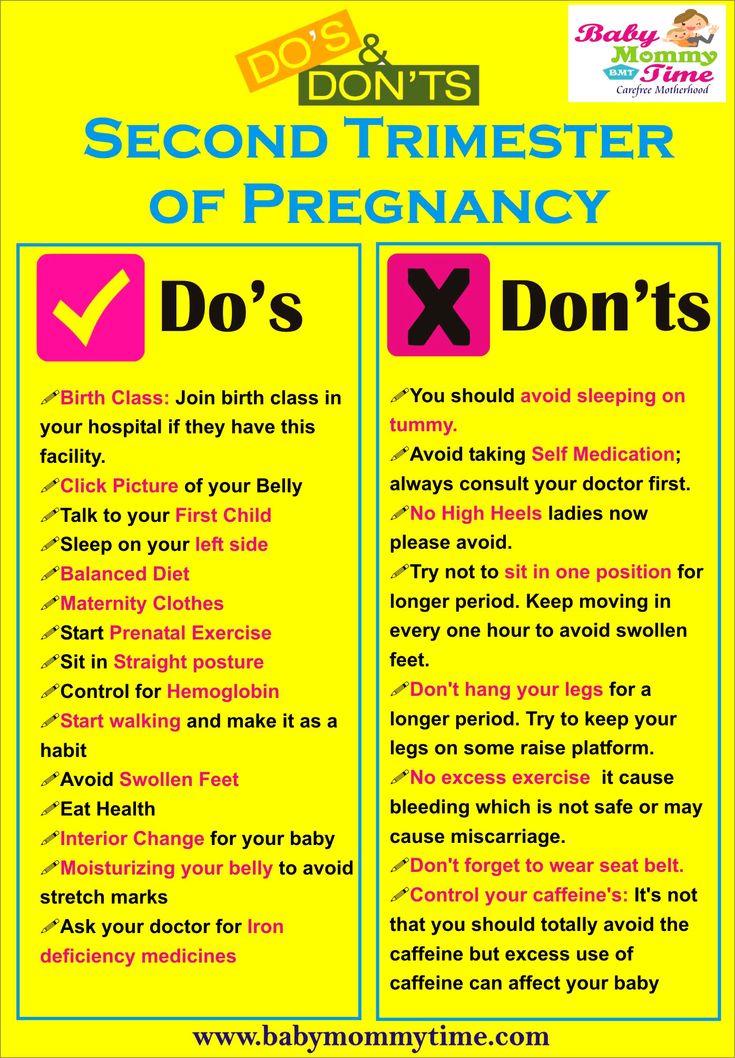
Discuss the timing of your next pregnancy with your doctor. Some experts say you should wait a certain amount of time (from one menstrual cycle to 3 months) before you try again. While this is not a widespread practice, to prevent another miscarriage the doctor may suggest treatment with progesterone, a hormone that helps the embryo implant and supports early pregnancy in your uterus.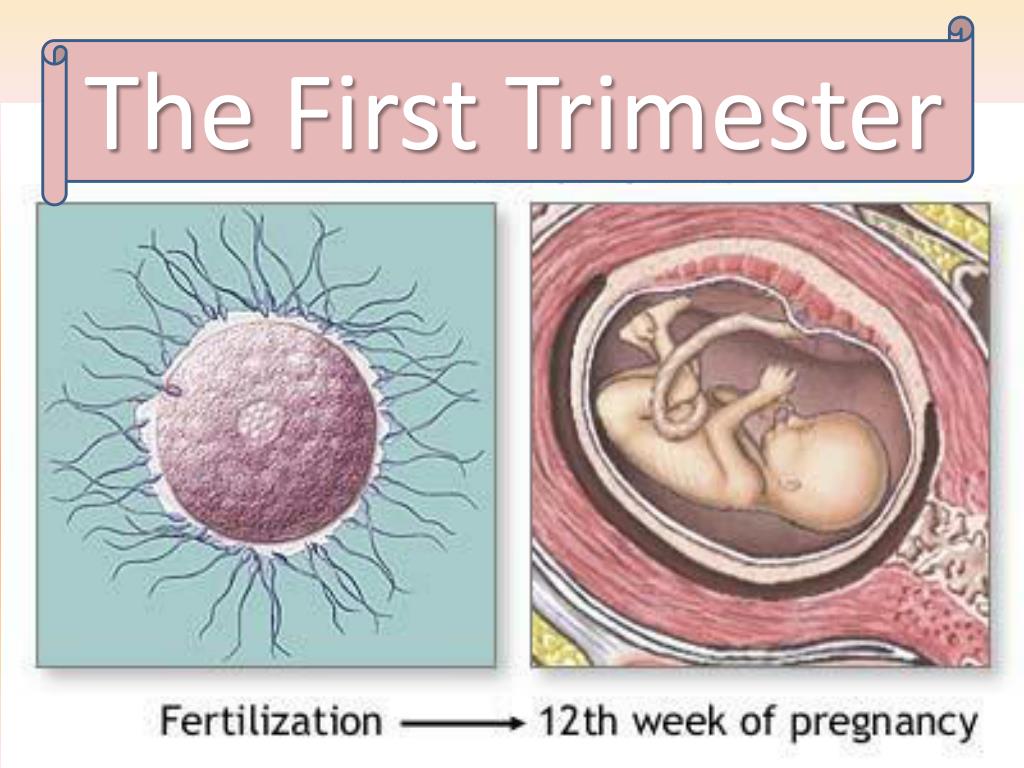
Taking time to heal both physically and emotionally after a miscarriage is important. Above all, don't blame yourself. Counseling is available to help you handle your loss.
Miscarriage Prevention
Most miscarriages happen because there’s a problem with the pregnancy. You can’t prevent them. If your doctor does testing and finds a problem, treatment options may be available.
If you have an illness, treating it can improve your chances for a successful pregnancy. One step you can take is to get as healthy as you can before you try to have a baby:
- Get regular exercise.
- Eat a healthy, well-balanced diet.
- Maintain a healthy weight.
- Avoid infections.
- Don’t smoke, drink alcohol, or take illegal drugs.
- Cut back on caffeine.
Health & Pregnancy Guide
- Getting Pregnant
- First Trimester
- Second Trimester
- Third Trimester
- Labor and Delivery
- Pregnancy Complications
- All Guide Topics
Miscarriage, symptoms - Health Clinic 365 Yekaterinburg
Causes of miscarriage
Questions to the doctor about miscarriage
Diagnosis of miscarriage
Treatment and prevention of miscarriage
According to statistics, 10 to 20% of all pregnancies end in miscarriage. Miscarriage is quite common, but this fact does not make things any easier. It is always difficult to cope with the realization that there was a pregnancy, but no child. Try to deal with the situation psychologically and understand what could be causing the miscarriage, what increases the risk of it, and what type of treatment might be needed. Miscarriage symptoms . Most miscarriages occur before 12 weeks. Signs and symptoms of a miscarriage include: It is important to consider the fact that in early pregnancy, spotting or vaginal bleeding is quite common. Some women who have a miscarriage develop an infection in the uterus. This infection, also called septic miscarriage, can cause: When to see a doctor. Call your doctor if: You can put a piece of tissue to be isolated in a clean container and take it to your doctor for examination. It is unlikely that the study will give any accurate results, but if it is determined that the fragments of the excreted tissue are from the placenta, the doctor will be able to conclude that the symptoms that appear are not associated with the presence of a tubal (ectopic) pregnancy. You can get more detailed information about miscarriage from the gynecologists of the Health 365 clinic in Yekaterinburg. Gynecologist, initial appointment 2300 i Pregnancy is a period of life that is extremely important for any woman. However, it is at this stage that the body loses most of its protective properties, becoming more vulnerable to adverse factors, especially in the case of existing health problems. According to disappointing statistics, about 15% of all clinically confirmed pregnancies end in the loss of a baby, and with a diagnosis of “ the threat of miscarriage “every second expectant mother is familiar firsthand. Miscarriage is an involuntary termination of pregnancy that occurs before 20 weeks of gestation, when the weight of the fetus does not exceed 500 grams. If the threat of miscarriage occurs after 22 weeks, then we are talking about premature birth and born babies weighing over 650 grams. can be successfully cared for thanks to the achievements of modern medicine and the experience of doctors. The fact that the pregnancy is at risk of miscarriage is indicated by the onset of vaginal bleeding. Whatever its intensity, duration and color saturation, this is a signal that you should immediately seek help from a specialist. No less alarming sign is a pulling pain that has appeared in the lower abdomen. Painful sensations radiating to the sacrum or inguinal region indicate the presence of uterine hypertonicity and an attempt by the body to get rid of the developing fetus. The causes of bleeding and discomfort may be less serious, but these symptoms should definitely not be ignored. If the expectant mother is given a disappointing diagnosis, the task of the doctors is to do everything possible to keep the pregnancy until a safe period. nine0003 The threat of miscarriage can be provoked by a number of reasons and not in every case it is possible to establish the true problem. And, nevertheless, every woman should be aware of the factors that can lead to termination of pregnancy: No woman is insured against involuntary termination of pregnancy, and yet there are a number of factors that increase the risk and require more attention from the expectant mother and additional control from the attending physician: Even with the slightest suspicion, a specialist should be contacted immediately. It is very important to maintain a sober mind and not panic. Your calmness and timely medical care in most cases help to keep the pregnancy. If you notice bloody discharge, indicating a possible detachment of the chorion - the membranes of the embryo, with which it is held on the walls of the uterus, you should lie down and call an ambulance. Trying to get to a medical facility on your own in such a state is not worth it. nine0003 If a doctor suspects a threatened miscarriage , a number of tests and examinations will help clarify the situation and identify the degree of danger. After a thorough examination and determination of the level of danger, the doctor will prescribe maintenance therapy. In the case when the risk of miscarriage is particularly high, the expectant mother is left for treatment in a hospital until her condition stabilizes and the threat of miscarriage is eliminated. If the condition does not cause serious concern, a woman can be treated at home, subject to the doctor's instructions and maintaining complete calm, for which she will be prescribed sedatives on a natural basis. nine0003 Treatment aimed at preserving pregnancy, includes the following stages: If The threat of miscarriage was caused by hormonal disorders, a pregnant woman will be prescribed by the main necessary hormone - progesterone. Taking drugs (usually "Utrozhestan" or "Dufaston") is prescribed according to a special scheme and is used until a period of 16 weeks is reached. By this time, the mature placenta begins to produce the necessary hormones on its own. nine0003 There is no need to obtain hormones artificially, but it is very important to know that the abrupt cessation of progesterone use can cause spontaneous abortion. Cancellation of the drug should occur in stages, by reducing the dose entering the body weekly. Prescribing antispasmodics can reduce uterine tone and reduce pain. The most common drugs that can be used until the pain disappears completely are papaverine (candles) and drotaverine (tablets). nine0003 The expectant mother will be required to take vitamins, which will not only strengthen the body as a whole, but also contributes to the fact that the threat of miscarriage will be minimized. Given the number of factors that affect the course of pregnancy, it is impossible to find a magic formula that reduces the risk of miscarriage to zero. And yet, some preventive measures will help reduce the risk of complications to the minimum possible: Problems. nine0024 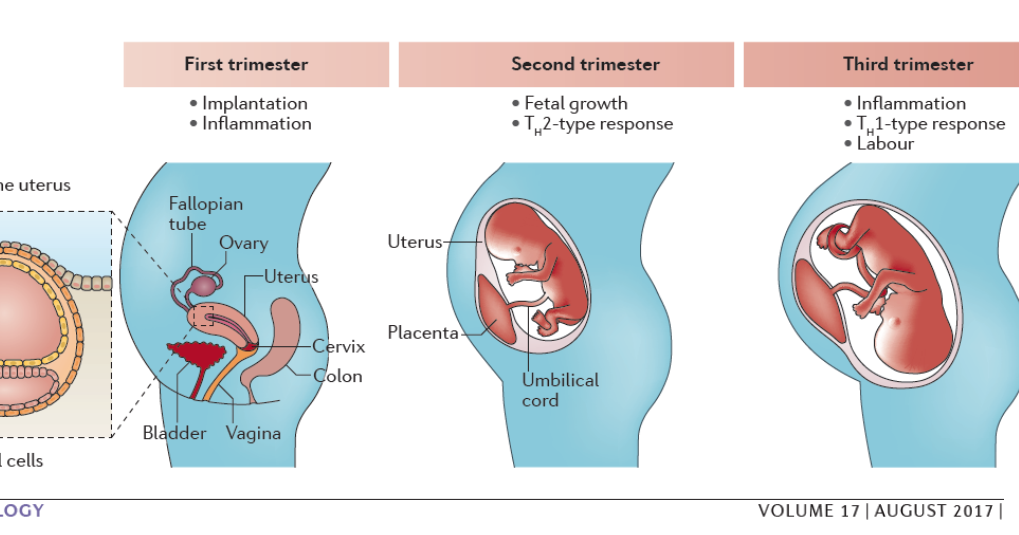 However, the real numbers could be much higher, as a large number of miscarriages happen very early, and women are not even aware of their pregnancy. Most miscarriages happen due to abnormal development of the fetus. nine0003
However, the real numbers could be much higher, as a large number of miscarriages happen very early, and women are not even aware of their pregnancy. Most miscarriages happen due to abnormal development of the fetus. nine0003
 In most cases, women who experience light bleeding during the first three months have an uneventful pregnancy thereafter. In some cases, even with heavy bleeding, the pregnancy does not end in a miscarriage. nine0003
In most cases, women who experience light bleeding during the first three months have an uneventful pregnancy thereafter. In some cases, even with heavy bleeding, the pregnancy does not end in a miscarriage. nine0003
 nine0003
nine0003 Prices
The threat of miscarriage: how to recognize and prevent
What is a miscarriage?
 More than 80% of miscarriages occur early up to 12 weeks. It is at this time that the initial laying of the organs of the fetus occurs, and therefore any impact can be negative. Often, the woman herself, not knowing about her pregnancy, perceives the bleeding that has arisen as the monthly onset of the menstrual cycle. This situation is dangerous and can cause serious complications in case of incomplete expulsion from the fetus. nine0003
More than 80% of miscarriages occur early up to 12 weeks. It is at this time that the initial laying of the organs of the fetus occurs, and therefore any impact can be negative. Often, the woman herself, not knowing about her pregnancy, perceives the bleeding that has arisen as the monthly onset of the menstrual cycle. This situation is dangerous and can cause serious complications in case of incomplete expulsion from the fetus. nine0003 Symptoms that must not be ignored
 nine0003
nine0003 The main reasons causing the threat of abortion
 The leaders who appear among the first in this list are rubella, chlamydia, hepatitis, taxoplasmosis, syphilis. Even the sore throat familiar to everyone at the initial stage can be fatal. nine0024
The leaders who appear among the first in this list are rubella, chlamydia, hepatitis, taxoplasmosis, syphilis. Even the sore throat familiar to everyone at the initial stage can be fatal. nine0024 
Who is at additional risk?
 After a series of studies, doctors say that the risk of abortion after 30 years increases by 2 times, after 40 years the probability of carrying a child decreases to 20%. Doctors attribute this problem to the aging of the eggs, which nature endows a woman at birth and lose their vitality as they get older. Past diseases, the accumulation of toxic substances adversely affect the ability of eggs to conceive. nine0024
After a series of studies, doctors say that the risk of abortion after 30 years increases by 2 times, after 40 years the probability of carrying a child decreases to 20%. Doctors attribute this problem to the aging of the eggs, which nature endows a woman at birth and lose their vitality as they get older. Past diseases, the accumulation of toxic substances adversely affect the ability of eggs to conceive. nine0024  nine0024
nine0024  However, if a woman has to constantly experience excessive loads, lift weights, then this is a serious reason to think about changing jobs or going on maternity leave as soon as possible.
However, if a woman has to constantly experience excessive loads, lift weights, then this is a serious reason to think about changing jobs or going on maternity leave as soon as possible. What should I do if I suspect a threatened miscarriage? nine0075
 First of all, the specialist will check the heartbeat of the developing fetus. Ultrasound examination will help to find out about the condition of the placenta and embryo, as well as show possible pathologies of the structure of the uterus. Examination by a gynecologist will determine the presence of tone.
First of all, the specialist will check the heartbeat of the developing fetus. Ultrasound examination will help to find out about the condition of the placenta and embryo, as well as show possible pathologies of the structure of the uterus. Examination by a gynecologist will determine the presence of tone. Methods of treatment
1.
 Hormonal therapy
Hormonal therapy 2. Decreased tone
3. Vitamin support
 The use of folic acid during the first trimester as a separate drug or as part of a vitamin complex will prevent the development of neural tube defects in the embryo.
The use of folic acid during the first trimester as a separate drug or as part of a vitamin complex will prevent the development of neural tube defects in the embryo. How to avoid the threat of miscarriage: preventive measures