When is spina bifida diagnosed
Spina Bifida Fact Sheet | National Institute of Neurological Disorders and Stroke
What is spina bifida?
What are the types of spina bifida?
How does folic acid help?
How is spina bifida diagnosed?
How is spina bifida treated?
What research is being done?
How can I help with research?
Where can I get more information?
What is spina bifida?
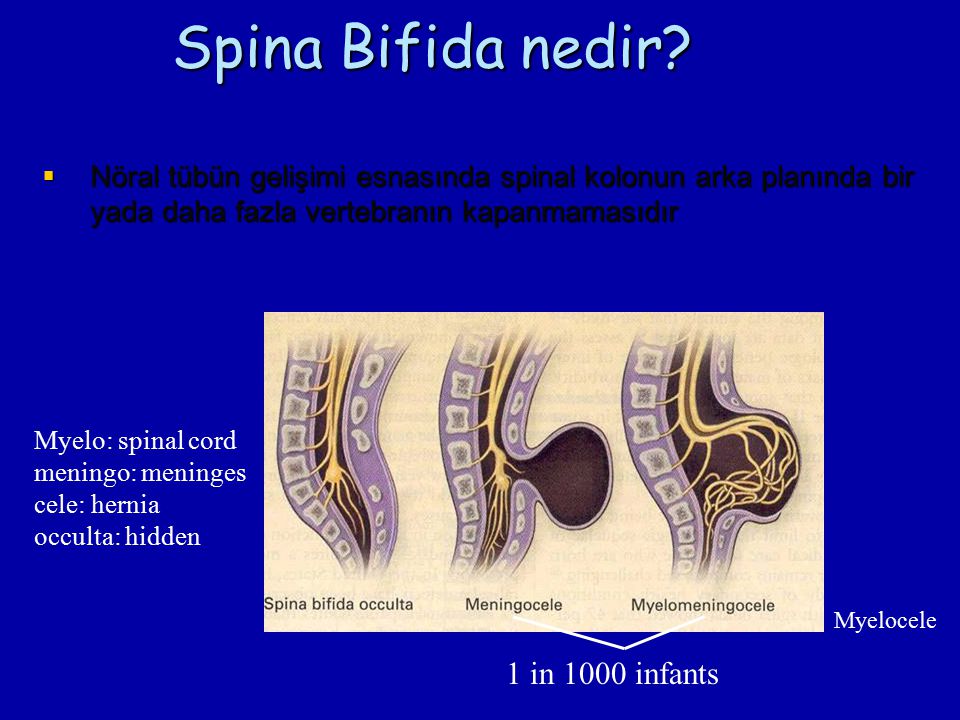
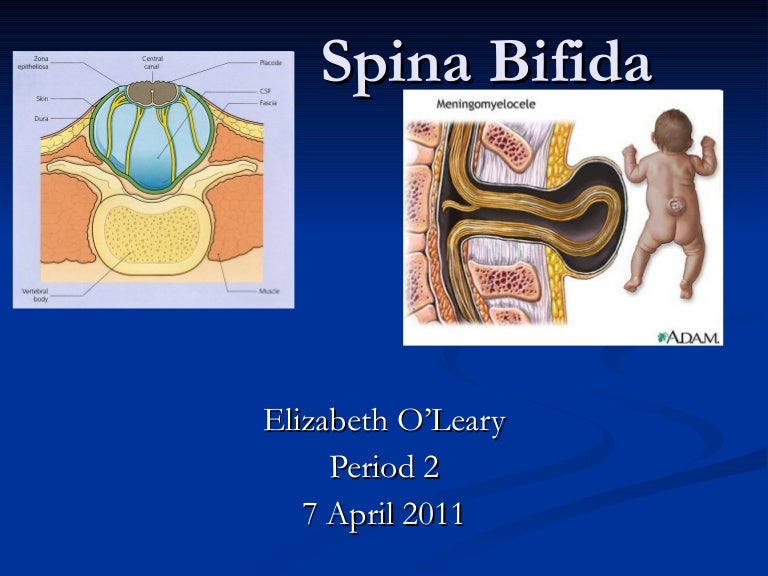
Spina bifida is a birth defect that mainly affects the spine. Normally in the first month of pregnancy, a special set of cells forms the “neural tube.” The top of the tube becomes the brain and the remainder becomes the spinal cord and structures around it. In spina bifida, the neural tube doesn’t close all the way and some of the bones of the spine don’t close in the back.
Often, abnormalities of the brain (such as hydrocephalus, described below) accompany abnormalities of the spine because the neural tube closes first in the middle and then closure proceeds both upward and downward—meaning that if something happens that prevents normal formation of the spine, it may also prevent normal formation of the part of the brain that is forming (closing) at the same time.
The term neural tube defect describes a group of conditions, including spina bifida, that occur when the neural tube does not close all the way.
Each year approximately 1,400 babies born in the United States have spina bifida, according to the U.S. Centers for Disease Control and Prevention. The exact cause of spina bifida is unknown. There is no cure but most people with spina bifida lead long and productive lives. Scientists suspect genetic, nutritional, and environmental factors all play a role in spina bifida. People with spina bifida have different abilities and medical issues.
top
What are the types of spina bifida?
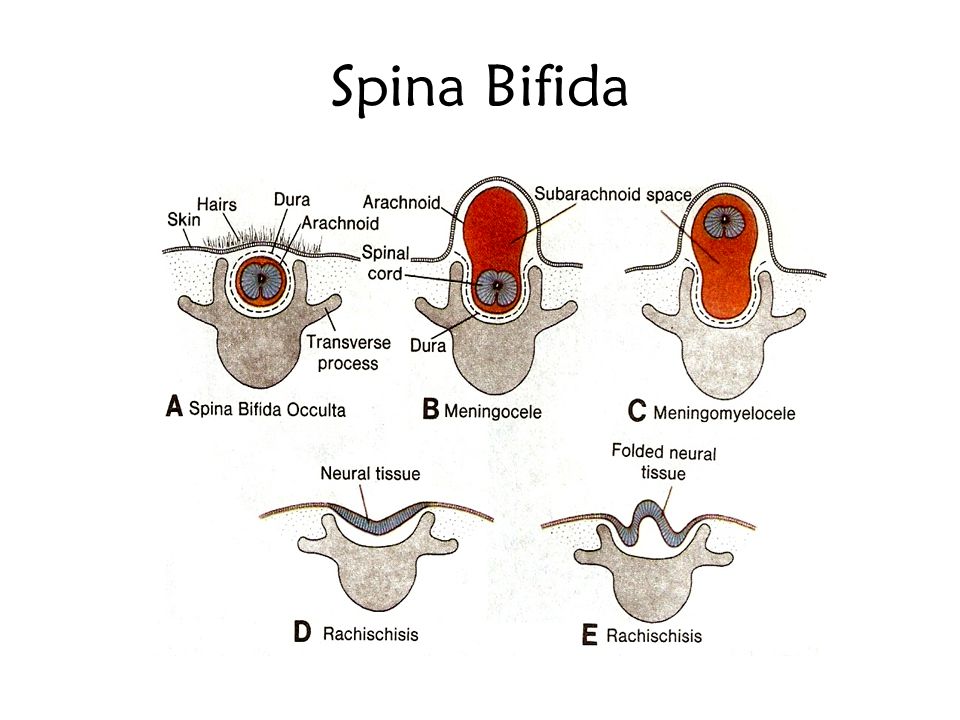
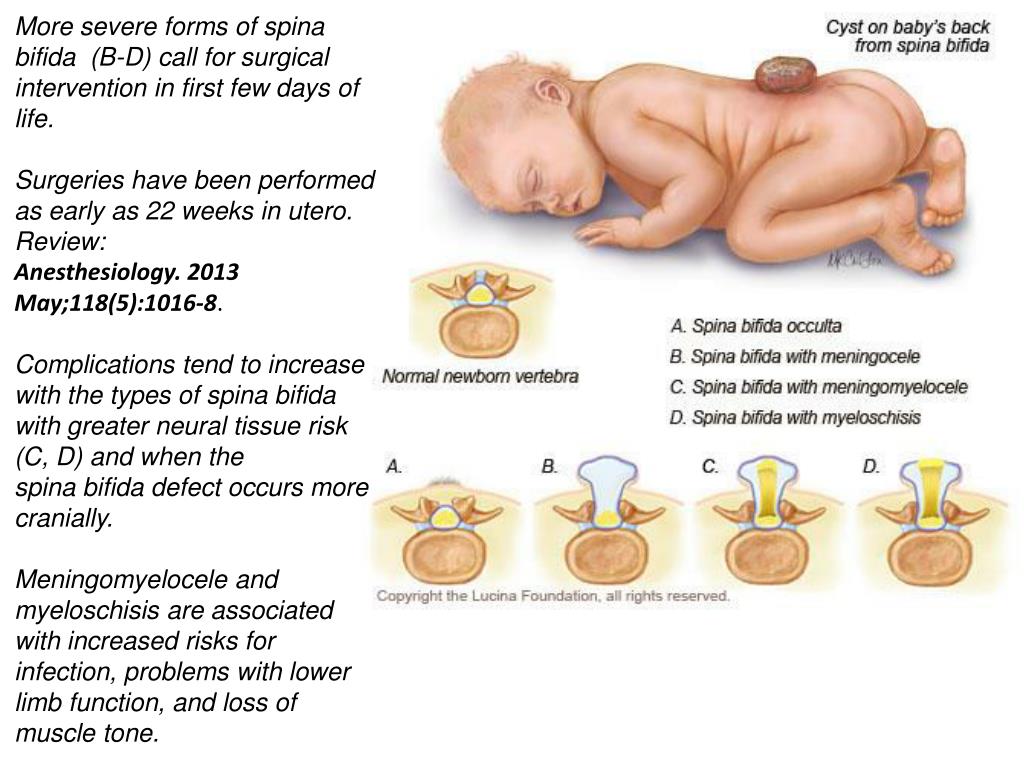
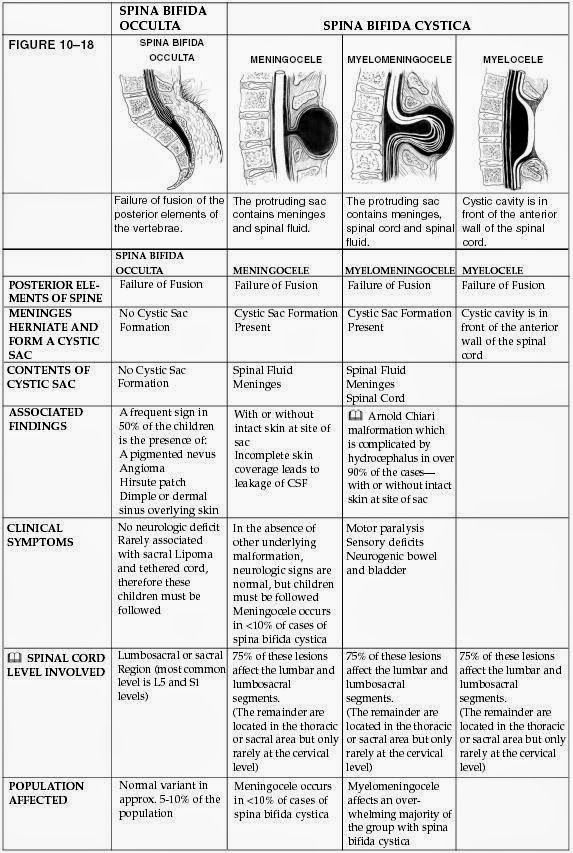
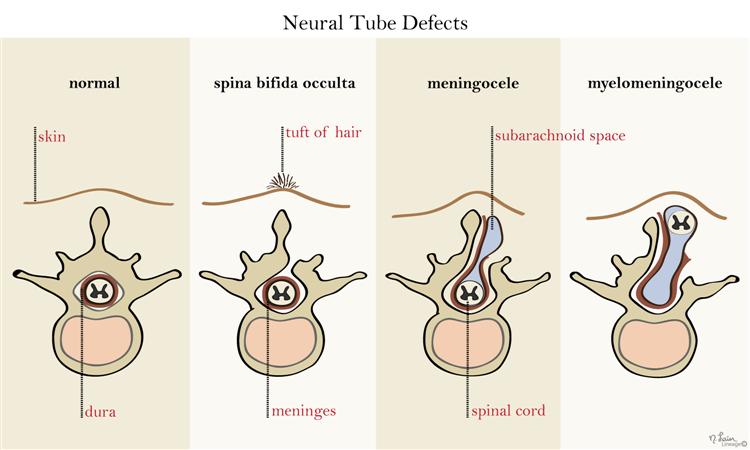
There are four types of spina bifida: occulta, closed neural tube defects, meningocele, and myelomeningocele. The symptoms of spina bifida vary from person to person, depending on the type and level of involvement.
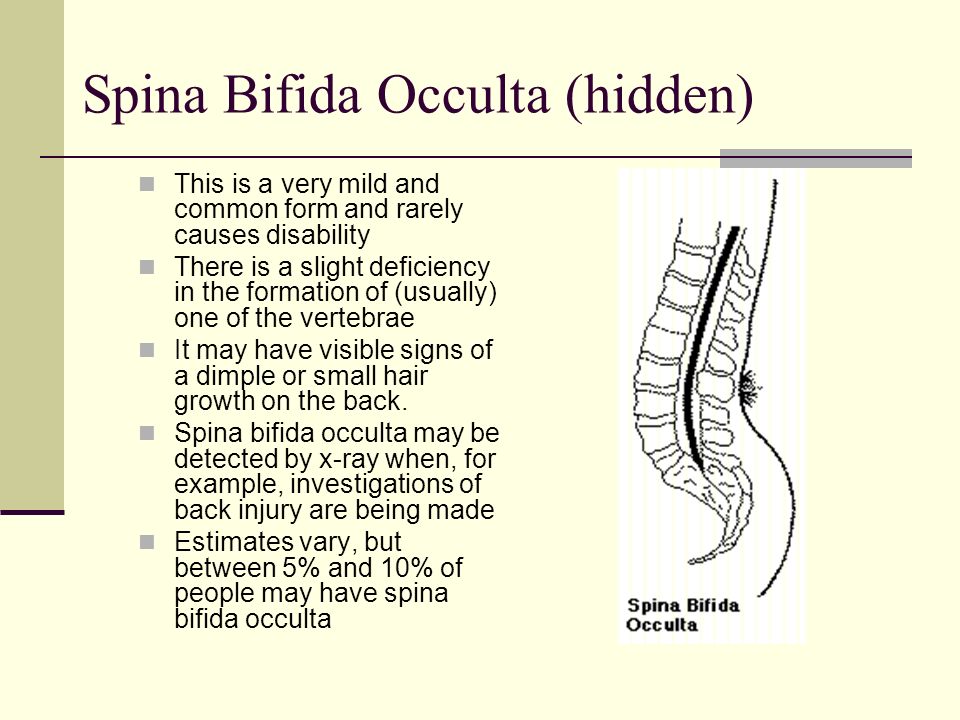
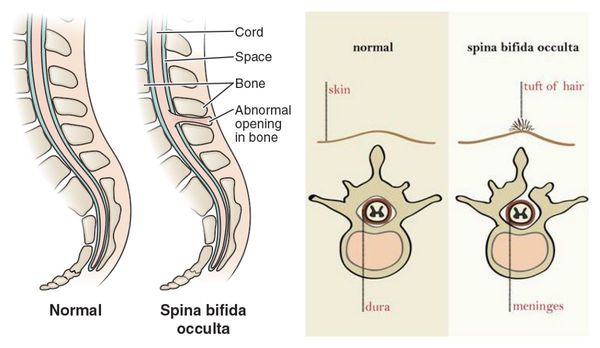
- Occulta is the mildest and most common form in which one or more bones of the spinal column (called vertebrae) are malformed.
 The name “occulta,” which means “hidden,” indicates that a layer of skin covers the opening in the bones of the spine. It is often found by accident on an x-ray or similar test. This form of spina bifida very rarely causes disabilities or symptoms.
The name “occulta,” which means “hidden,” indicates that a layer of skin covers the opening in the bones of the spine. It is often found by accident on an x-ray or similar test. This form of spina bifida very rarely causes disabilities or symptoms. - Closed neural tube defects are a diverse group of defects in which the spine may have malformations of fat, bone, or the membranes (called the meninges) that cover the spinal cord. Many of these neural tube defects require surgery in childhood. People with this type of spina bifida may have weakness of the legs and trouble with bowel and bladder control. These issues may change or progress as children grow. It is important to have close follow-up with doctors to minimize these changes as much as possible.
- Meningocele occurs when a sac of spinal fluid pokes through the spine. This fluid is normally only around the brain and spine, but a problem with the bony covering over the spine allows it to poke out in this case.
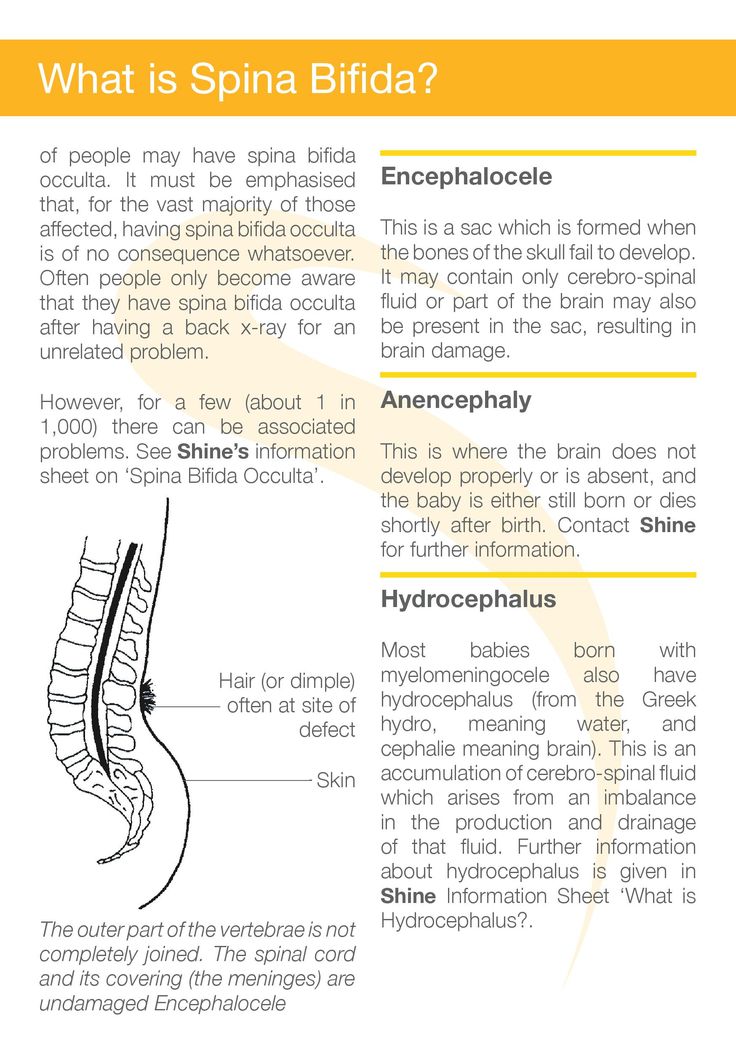 The malformation contains no nerves and may or may not be covered by a layer of skin. Individuals with meningocele may have minor symptoms.
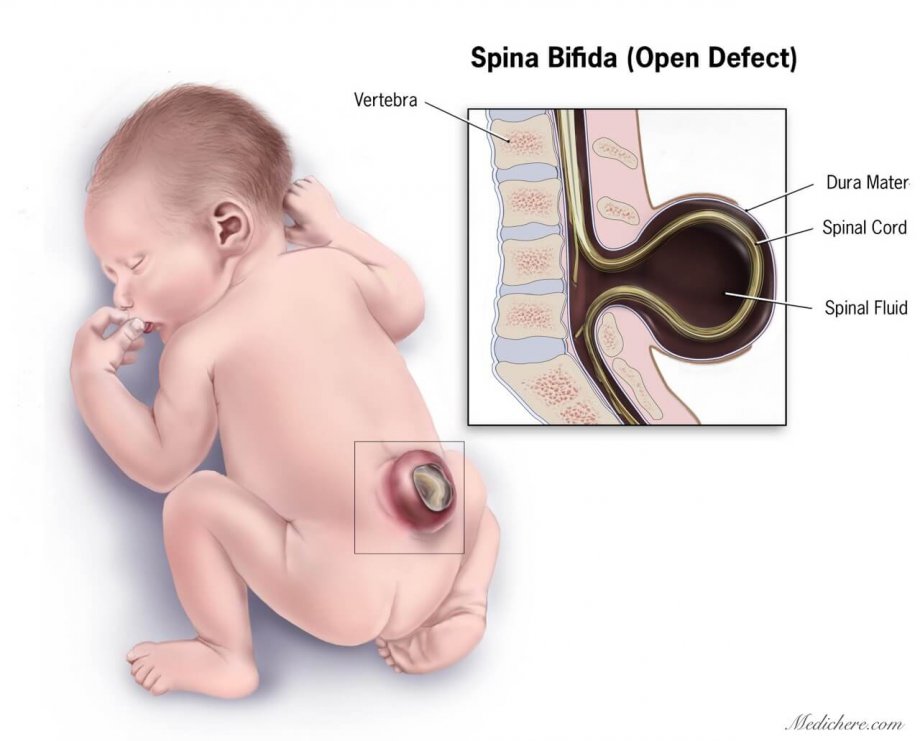
The malformation contains no nerves and may or may not be covered by a layer of skin. Individuals with meningocele may have minor symptoms. - Myelomeningocele is the most severe form of spina bifida. A portion of the spinal cord or nerves is exposed in a sac through an opening in the spine that may or may not be covered by the meninges. The opening can be closed by surgeons while the baby is in utero or shortly after the baby is born. Most people with myelomeningocele have changes in their brain structure, leg weakness, and bladder and bowel dysfunction. Myelomeningocele is often called a snowflake condition because no two people with the condition are the same. Typically, the lower in the spine the opening occurs relates to less symptoms in the person. People with myelomeningocele require close follow-up with physicians throughout their childhood and lifespan to maximize their function and prevent complications such as kidney failure.
top
How does folic acid help?
Folic acid, also called folate, is an important vitamin for the development of a healthy fetus.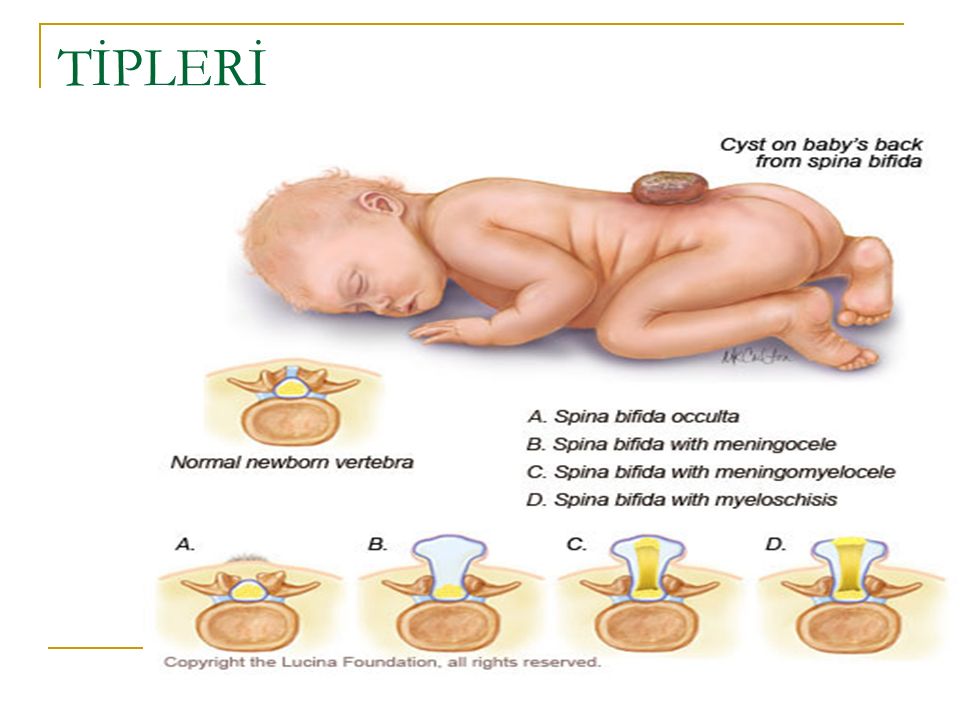 Although taking this vitamin cannot guarantee having a healthy baby, it can help. Studies show that women of childbearing age who add folic acid to their diets can significantly reduce the risk of having a child with a neural tube defect. Therefore, it is recommended that all women of childbearing age take a daily vitamin supplement with 400 micrograms of folic acid before and during early pregnancy.
Although taking this vitamin cannot guarantee having a healthy baby, it can help. Studies show that women of childbearing age who add folic acid to their diets can significantly reduce the risk of having a child with a neural tube defect. Therefore, it is recommended that all women of childbearing age take a daily vitamin supplement with 400 micrograms of folic acid before and during early pregnancy.
Foods high in folic acid include dark green vegetables, egg yolks, and some fruits. Many foods—such as some breakfast cereals, enriched breads, flours, pastas, rice, and other grain products—are now fortified with folic acid. Many multivitamins contain the recommended dosage of folic acid as well.
Women who already have a child with spina bifida, who have spina bifida themselves, or who have already had a pregnancy affected by any neural tube defect are at greater risk of having another child with a neural tube defect. These women should take a higher prescription dose of folic acid before and early in pregnancy.
Spina Bifida Complications
Spina bifida’s impact is determined by the type of defect and in the case of myelomeningocele and closed neural tube defects the size and location of the malformation.
Spina bifida complications may include:
- Abnormal sensation or paralysis, which mostly occurs with closed neural tube defects and myelomeningocele. People with these conditions typically have some degree of leg and core muscle weakness and loss of feeling in the groin and feet or legs. The sensation can be more significant on one side of the body. Typically, the lower in the spine where the condition occurs results in less weakness and loss of feeling. The strength and feeling do not improve with age due to nerve damage. People with these types of spina bifida may lose strength and sensation as they grow and mobility can become more difficult with age. People with these conditions may walk independently or use some combination of leg braces, walkers, crutches, or wheelchairs.
 As they age, they may require more of these supports.
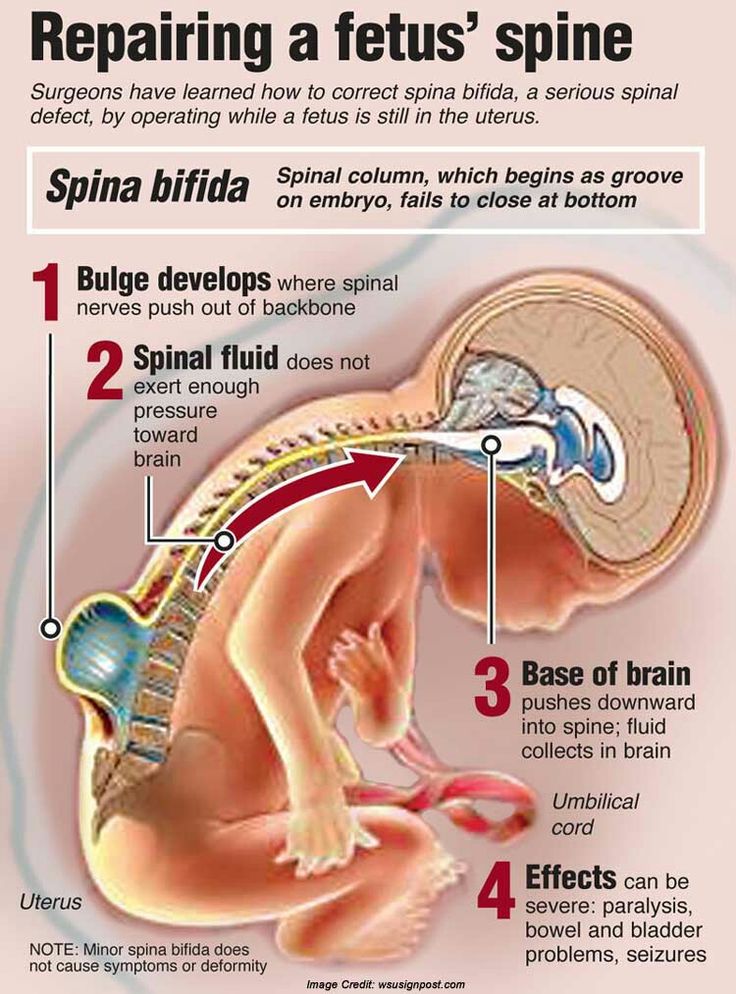
As they age, they may require more of these supports. - Chiari II malformation, in which parts of the brain called the brain stem and the cerebellum (hindbrain) protrude downward into the spinal canal or neck area. It is almost always seen on advanced imagining of the brain in people with myelomeningocele, but it rarely causes symptoms. When it does, this condition can press on the spinal cord and cause a variety of symptoms including difficulty breathing, swallowing, and arm weakness. Surgery is sometimes required to reduce pressure in this area.
- Blockage of cerebrospinal fluid, causing a condition called hydrocephalus. Hydrocephalus is the abnormal buildup of the fluid that surrounds the brain. Most people with myelomeningocele have this condition, which is not seen in the other types of spina bifida. This buildup can put damaging pressure on the brain. Hydrocephalus is commonly treated by surgically implanting a shunt—a hollow tube—in the brain which allows drainage of the excess fluid into the abdomen where it is absorbed by the body.
 The tube is tunneled under the skin and not very noticeable to others. Another treatment option is an endoscopic third ventriculostomy or ETV, a procedure that creates a new path for the fluid to flow.
The tube is tunneled under the skin and not very noticeable to others. Another treatment option is an endoscopic third ventriculostomy or ETV, a procedure that creates a new path for the fluid to flow. - Meningitis, an infection in the meninges covering the brain. It can sometimes be associated with shunts. Meningitis may cause brain injury and can be life-threatening.
- Tethered cord syndrome can occur with all forms of spina bifida, although it is very rare in individuals with spina bifida occulta. Usually the spinal cord and nerves float freely. A tethered cord means that there is some type of tissue attached to and pulling the cord down. This can cause damage to the nerves and decrease feeling and strength, as well as problems with bowel and bladder control. It is surgically treated if a person has symptoms.
- Bowel and bladder incontinence affect most individuals with myelomeningocele and closed neural tube defects.
 The nerves at the very bottom of the spine control bowel and bladder function and don’t usually work properly in people with these types of spina bifida. Most people with myelomeningocele and some types of closed neural tube defects need a regimen or other assistance to drain their bladders periodically or to have regularly scheduled bowel movements.
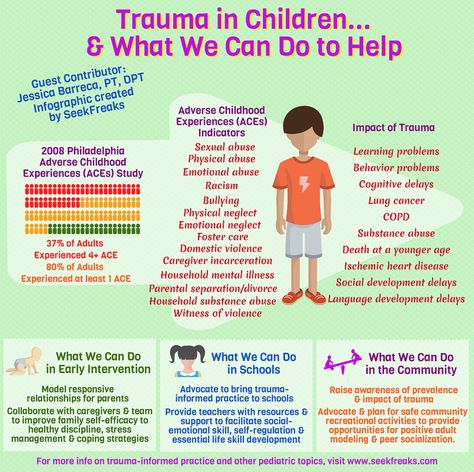
The nerves at the very bottom of the spine control bowel and bladder function and don’t usually work properly in people with these types of spina bifida. Most people with myelomeningocele and some types of closed neural tube defects need a regimen or other assistance to drain their bladders periodically or to have regularly scheduled bowel movements. - Learning disabilities, including difficulty paying attention, understanding concepts, impaired motor skills, impaired memory, and difficulty with organization and problem solving are commonly seen in children with myelomeningocele. People with strength lower down in their legs tend to have less difficulty than those with more leg weakness. Evaluation for an individualized education plan is recommended for all children with myelomeningocele.
- Other complications such as skin ulcers, low bone mineral density, impaired male fertility, obesity, and kidney failure can be seen in people with myelomeningocele and neural tube defects as they age.
 Additionally, people with myelomeningocele are at risk for precocious puberty (when changes to that of an adult occur too soon), sleep apnea, and depression.
Additionally, people with myelomeningocele are at risk for precocious puberty (when changes to that of an adult occur too soon), sleep apnea, and depression.
top
How is spina bifida diagnosed?
In most cases, spina bifida is diagnosed before birth (prenatal). However, some mild cases may go unnoticed until after birth (postnatal). Very mild forms of spinal bifida are found when doing tests for other conditions or may never be detected.
Prenatal Diagnosis
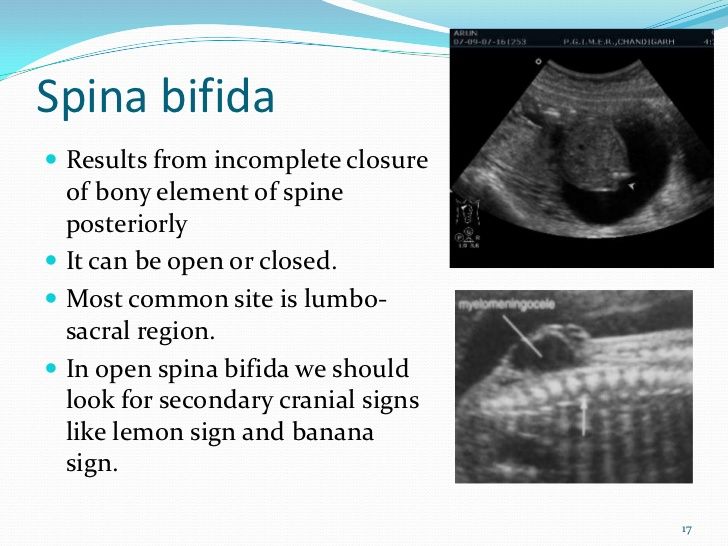
The most common screening methods used to look for spina bifida during pregnancy are maternal serum alpha fetoprotein (MSAFP) screening and fetal ultrasound. A doctor can also perform an amniocentesis test.
- Maternal serum alpha fetoprotein (MSAFP) screen. At 16 to 18 weeks of pregnancy, a sample of the mother’s blood is taken to measure the level of a protein called alpha-fetoprotein (AFP), which is made naturally by the fetus and placenta.
 During pregnancy, a small amount of AFP normally crosses the placenta and enters the mother’s bloodstream. Abnormally high levels of AFP may indicate that the fetus has spina bifida or other neural tube defect. This test is not specific for spina bifida and cannot definitively determine that there is a problem with the fetus. This means that a high AFP level alone is not enough to be sure the fetus has a neural tube defect. If a high level of AFP is detected, the doctor may request additional testing, such as an ultrasound or amniocentesis.
During pregnancy, a small amount of AFP normally crosses the placenta and enters the mother’s bloodstream. Abnormally high levels of AFP may indicate that the fetus has spina bifida or other neural tube defect. This test is not specific for spina bifida and cannot definitively determine that there is a problem with the fetus. This means that a high AFP level alone is not enough to be sure the fetus has a neural tube defect. If a high level of AFP is detected, the doctor may request additional testing, such as an ultrasound or amniocentesis.
The second trimester MSAFP screen may be performed alone or as part of a larger, multiple-marker screen. Multiple-marker screens can look for neural tube defects and other birth defects, including Down syndrome and other chromosomal abnormalities. First trimester screens for chromosomal abnormalities also exist but signs of spina bifida are not evident until the second trimester when the MSAFP screening is performed.
- Ultrasound.
 A fetal ultrasound uses high-frequency sound waves to create a picture of the developing baby inside the womb. It is highly accurate in diagnosing some birth defects during pregnancy, including spina bifida. Fetal ultrasound can be performed during the first trimester (usually between 11-14 weeks) and the second trimester (usually at 18-22 weeks), and diagnosis is more accurate during the second trimester.
A fetal ultrasound uses high-frequency sound waves to create a picture of the developing baby inside the womb. It is highly accurate in diagnosing some birth defects during pregnancy, including spina bifida. Fetal ultrasound can be performed during the first trimester (usually between 11-14 weeks) and the second trimester (usually at 18-22 weeks), and diagnosis is more accurate during the second trimester. - Amniocentesis. In this test, a doctor removes a sample of the amniotic fluid that surrounds the fetus and tests it for protein levels that may indicate a neural tube defect and genetic disorders.
Postnatal Diagnosis
Closed neural tube defects are often recognized at birth due to an abnormal fatty mass, tuft or clump of hair, or a small dimple or birthmark on the skin at the site of the spinal malformation. Spina bifida occulta is usually found when x-rays are done for another reason.
In rare cases, myelomeningocele and meningocele are not diagnosed during routine prenatal tests. The baby will be diagnosed when they are born with a bubble on their back. Babies with myelomeningocele and closed neural tube defects may have muscle weakness in their feet, hips, and legs that result in joint deformities first noticed at birth. Mild cases of spina bifida (occulta, closed neural tube defects) not diagnosed during prenatal testing may be detected postnatally using ultrasound or X-ray imaging to look at the spine.
The baby will be diagnosed when they are born with a bubble on their back. Babies with myelomeningocele and closed neural tube defects may have muscle weakness in their feet, hips, and legs that result in joint deformities first noticed at birth. Mild cases of spina bifida (occulta, closed neural tube defects) not diagnosed during prenatal testing may be detected postnatally using ultrasound or X-ray imaging to look at the spine.
Doctors may use magnetic resonance imaging (MRI) or a computed tomography (CT) scan to get a clearer view of the spinal cord and vertebrae. To evaluate for hydrocephalus, the doctor will request a head ultrasound, CT or MRI to look for extra cerebrospinal fluid inside the brain.
top
How is spina bifida treated?
Treatment depends on the type of spina bifida a person has. Myelomeningocele and meningocele require a surgery to close the bubble shortly after birth to prevent infection such as meningitis. Most people with myelomeningocele have hydrocephalus and most of them will need a shunt placed as an infant.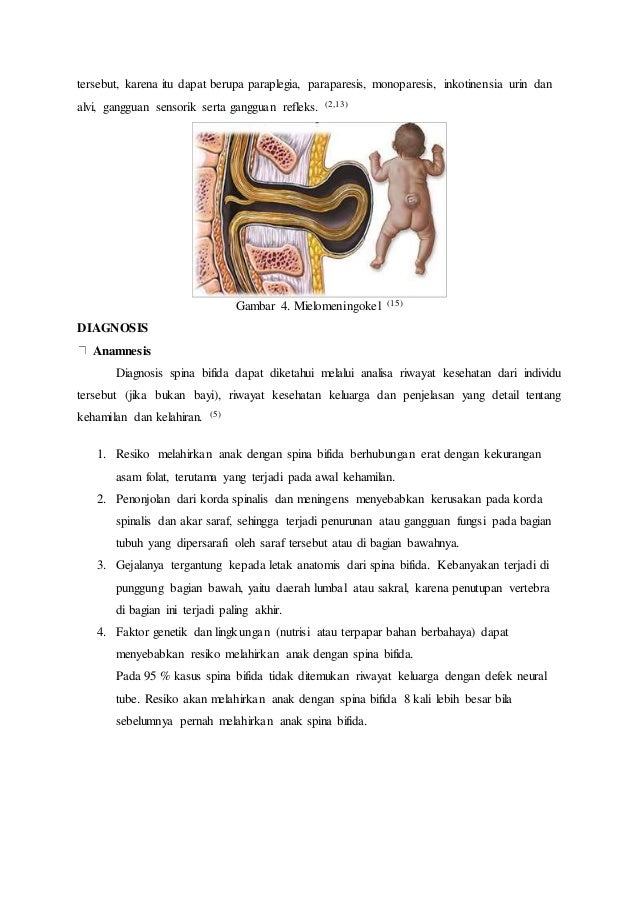 Children with a closed neural tube defect may need surgery to prevent further complications such as weakness and bowel and bladder function. Generally, people with spina bifida occulta will not need any treatment.
Children with a closed neural tube defect may need surgery to prevent further complications such as weakness and bowel and bladder function. Generally, people with spina bifida occulta will not need any treatment.
Prenatal Surgery
Prenatal (before birth) surgery involves opening the mother’s abdomen and uterus (or womb) and sewing shut the abnormal opening over the developing baby’s spinal cord. This is thought to protect the baby’s spinal cord from ongoing damage in the uterus. The Management of Myelomeningocele Study (MOMS) showed that prenatal surgery to close the defect in the spinal cord improved outcomes compared to children who had postnatal surgery for spina bifida. Data from the 2012 study showed that prenatal surgery reduced the need to drain fluid from the brain, improved mobility, and increased the chances that a child will be able to walk independently early on. This study was funded by the National Institutes of Health's Eunice Kennedy Shriver National Institute of Child Health and Human Development.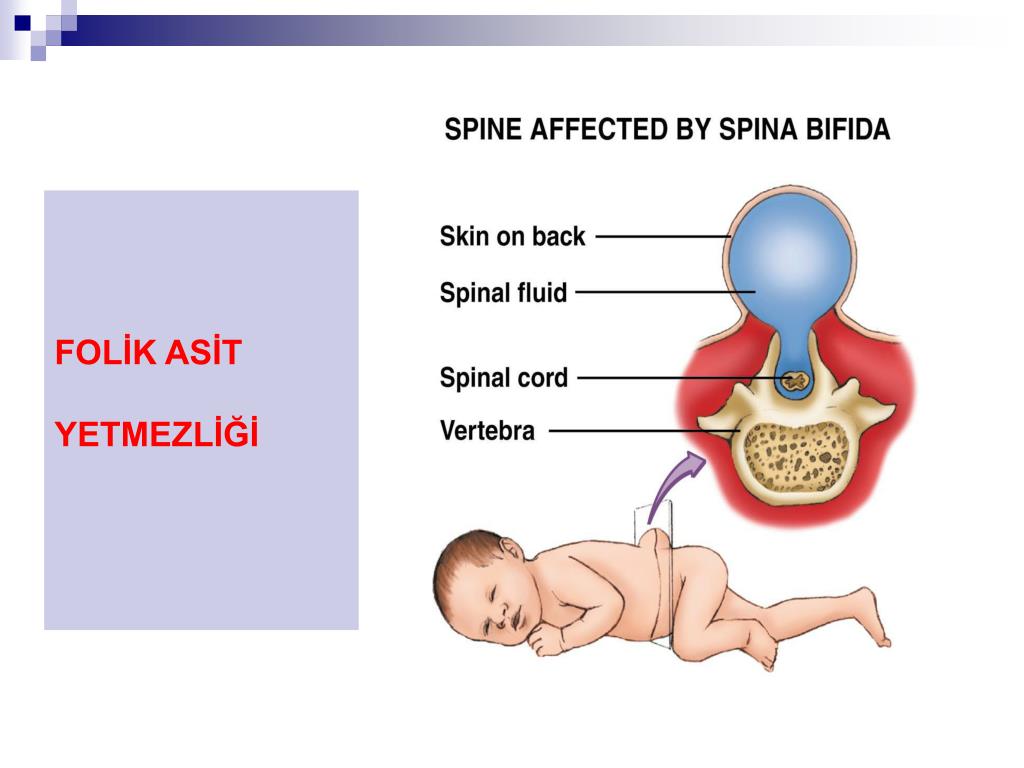
The procedure does not restore lost neurological function that happened before the surgery, but may prevent additional damage from occurring during the rest of the pregnancy. Although prenatal surgery poses some risk to the fetus as well as to the mother, the benefits are promising and are still being studied.
Postnatal Surgery
In treating myelomeningocele and meningocele, the key priorities are to prevent infection from developing in the exposed nerves and spinal cord through the spinal defect, and to protect the exposed nerves and spinal cord from additional trauma. Therefore, a child born with these types of spina bifida who has not undergone prenatal surgery will have surgery to close the defect and minimize the risk of infection or further trauma within the first few days of life.
Treatments for Complications
Some children with myelomeningocele and closed neural tube defects will need surgery to improve the alignment of their feet, legs, or spine.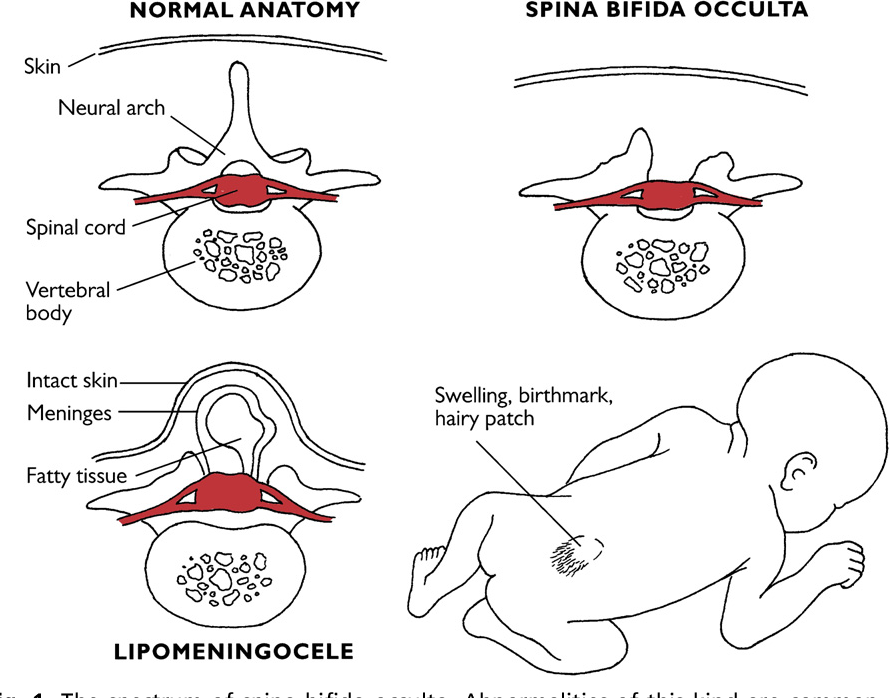 Children with myelomeningocele usually have hydrocephalus and may require surgery to help drain fluid in the brain, such as the placement of a shunt or ETV. Multiple surgeries may be required to replace the shunt, which may become clogged, infected, or disconnected.
Children with myelomeningocele usually have hydrocephalus and may require surgery to help drain fluid in the brain, such as the placement of a shunt or ETV. Multiple surgeries may be required to replace the shunt, which may become clogged, infected, or disconnected.
Some individuals with myelomeningocele or closed neural tube defects require assistive devices for mobility such as braces, walkers, crutches, or wheelchairs. The location of the defect on the spine often determines the type of assistive devices needed. Children with a defect high on the spine will have little movement of the legs and will use a wheelchair for mobility. Children with a defect lower on the spine usually have more strength in the legs. They may be able to walk independently, or they may use crutches, leg braces, walkers, and wheelchairs depending on the activity. Children with myelomeningocele usually have some degree of delayed mobility, so they are referred to physical therapists early on to maximize their strength and function.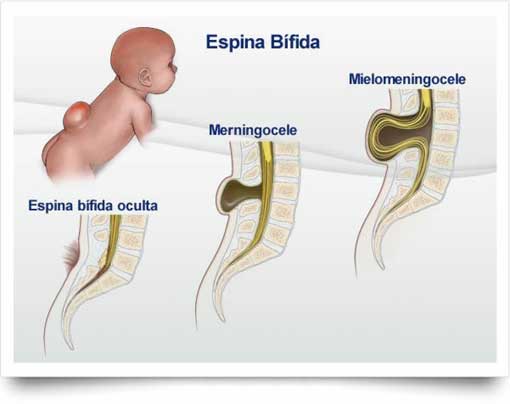
Treatment for bladder and bowel dysfunction typically begins soon after birth. Children with myelomeningocele and some closed neural tube defects have damage to the lowest spinal nerves which control typical bowel and bladder function. Some children may be able to urinate typically, but most will need to drain their bladders with a catheter or thin tube 4-6 times a day to remain dry in between and to prevent kidney damage. Kidneys are monitored closely so that medications or surgeries can be performed to prevent renal failure. To prevent bowel accidents many people with myelomeningocele and closed neural type defects will use rectal medications or large volume enemas to have planned bowel movements. Close follow-up with a spina bifida specialty clinic is recommended to develop a safe bowel and bladder program.
Treatment for progressive tethering of the spinal cord (called tethered cord syndrome) can be treated with surgery to help prevent further neurological deterioration.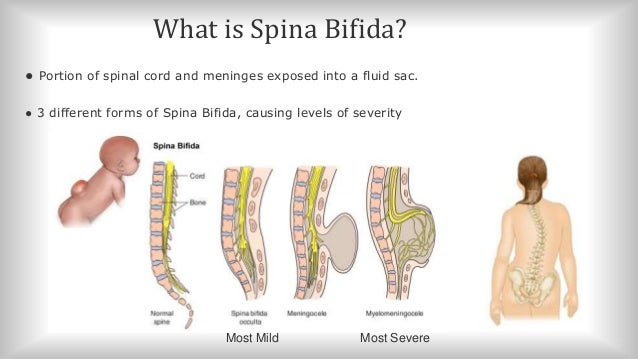
top
What research is being done?
The National Institute of Neurological Disorders and Stroke (NINDS), one of the National Institutes of Health (NIH), is the primary federal supporter of research on brain and nervous system disorders. NINDS conducts research in its laboratories at the NIH in Bethesda, Maryland, and supports research through grants to major medical institutions across the country. In addition to NINDS, other NIH Institutes support research on spina bifida and neural tube defects.
Genetic studies. In one study supported by NINDS, scientists are looking at the hereditary basis of neural tube defects and hope to find the genetic factors that make some children more likely to have a neural tube defect. These researchers are also studying gene expression during the process of normal neural tube closure, which will provide information on the human nervous system during development. Findings may lead to ways to prevent these disorders.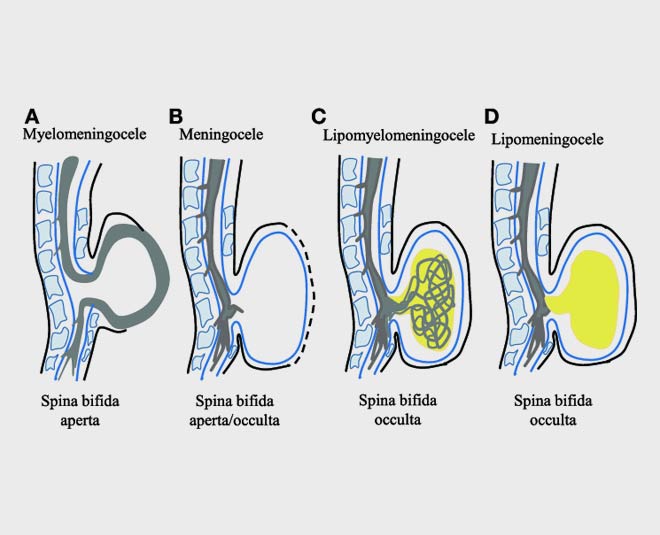
In addition, NINDS-supported scientists are working to identify, characterize, and evaluate genes involved in neural tube defects. The goal is to understand the genetics of neural tube closure and to develop information that will lead to improved clinical care, treatment, and genetic counseling.
Other scientists are studying genetic risk factors for spina bifida, especially those that reduce the effectiveness of folic acid in preventing spina bifida. This study will shed light on how folic acid prevents spina bifida and may lead to improved forms of folate supplements.
Developmental studies. NINDS supports and conducts a wide range of basic research studies to understand how the brain and nervous system develop. These studies contribute to a greater understanding of neural tube defects such as spina bifida and offer hope for new ways to treat and potentially prevent these disorders as well as other birth defects.
Surgery. Results of the Management of Myelomeningocele Study (MOMS) (see Prenatal Surgery) showed significant benefit to the developing baby.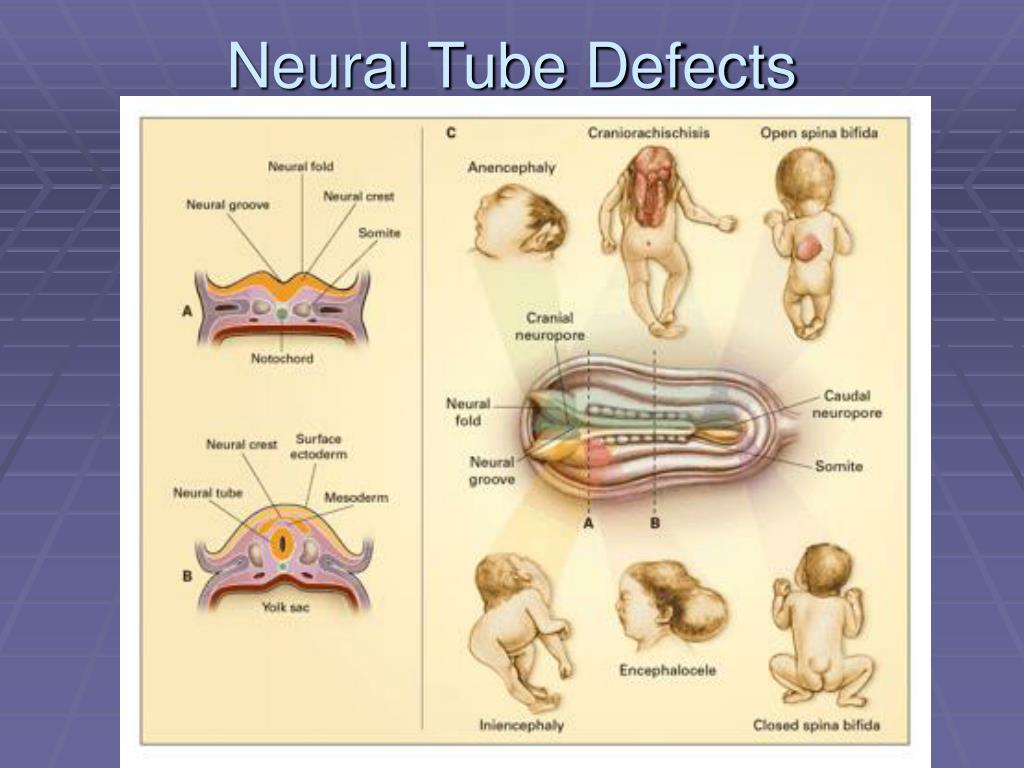 Because fetal surgery has shown promise, NINDS-funded researchers are also developing new methods, such as stem cell patches and tissue engineering, to add to the prenatal repair of spinal defects.
Because fetal surgery has shown promise, NINDS-funded researchers are also developing new methods, such as stem cell patches and tissue engineering, to add to the prenatal repair of spinal defects.
Other NIH research efforts. More information about research on spina bifida supported by NINDS and other NIH Institutes and Centers can be found using NIH RePORTER, a searchable database of current and past research projects supported by NIH and other federal agencies. RePORTER also includes links to publications and resources from these projects. Enter “spina bifida” to start your search.
top
How can I help with research?
Consider joining a clinical study. Both healthy individuals and those with a disease or condition can participate in medical research studies (sometimes called clinical trials or protocols) to help researchers better understand a disease and perhaps develop new treatments. For information about clinical studies on disorders including spina bifida and how to participate in one, please contact the NIH’s Patient Recruitment and Public Liaison office at 800-411-1222 or visit the Clinicaltrials.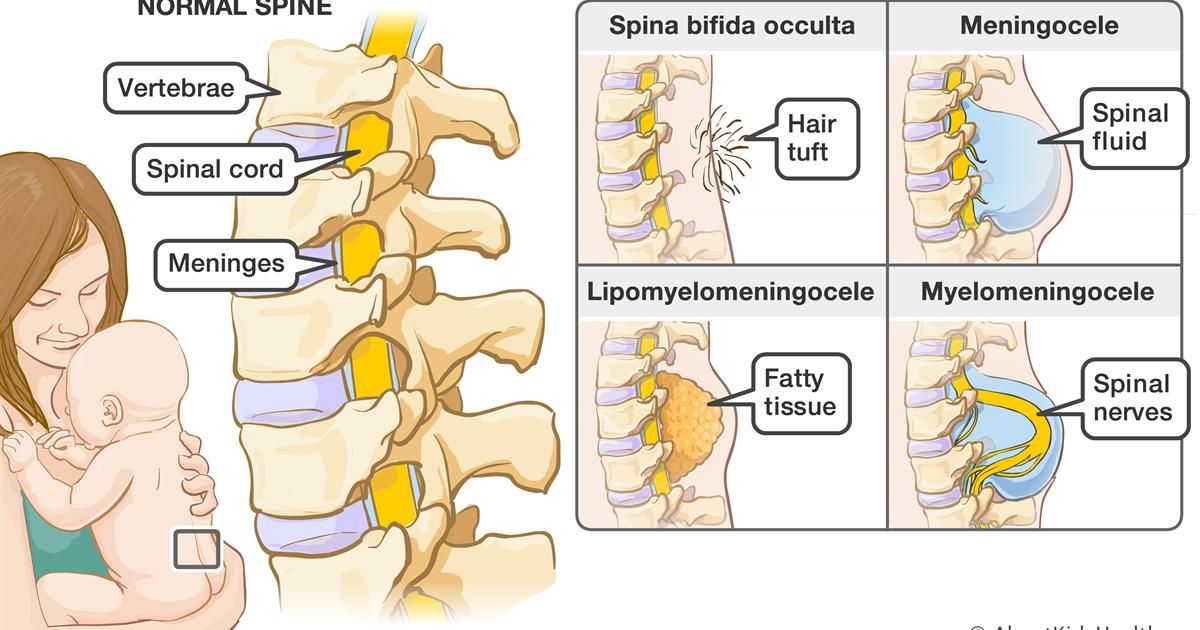 gov website.
gov website.
top
Where can I get more information?
For more information on neurological disorders or research programs funded by the National Institute of Neurological Disorders and Stroke, contact the Institute's Brain Resources and Information Network (BRAIN) at:
BRAIN
P.O. Box 5801
Bethesda, MD 20824
800-352-9424
Information also is available from the following organizations:
Eunice Kennedy Shriver National Institute of Child Health and Human Development
Information Resource Center
P.O. Box 3006
Rockville, MD 20847
800-370-2943 or 888-320-6942 (TTY)
Spina Bifida Association
4590 MacArthur Blvd. NW
Suite 250
Washington, DC 20007-4266
[email protected]
Tel: 202-944-3285; 800-621-3141
Fax: 202-944-3295
March of Dimes
1275 Mamaroneck Avenue
White Plains, NY 10605
[email protected]
Tel: 914-997-4488; 888-MODIMES (663-4637)
Fax: 914-428-8203
MedlinePlus
National Library of Medicine
National Institutes of Health
"Spina Bifida Fact Sheet", NINDS, Publication date January 2021
NIH Publication No.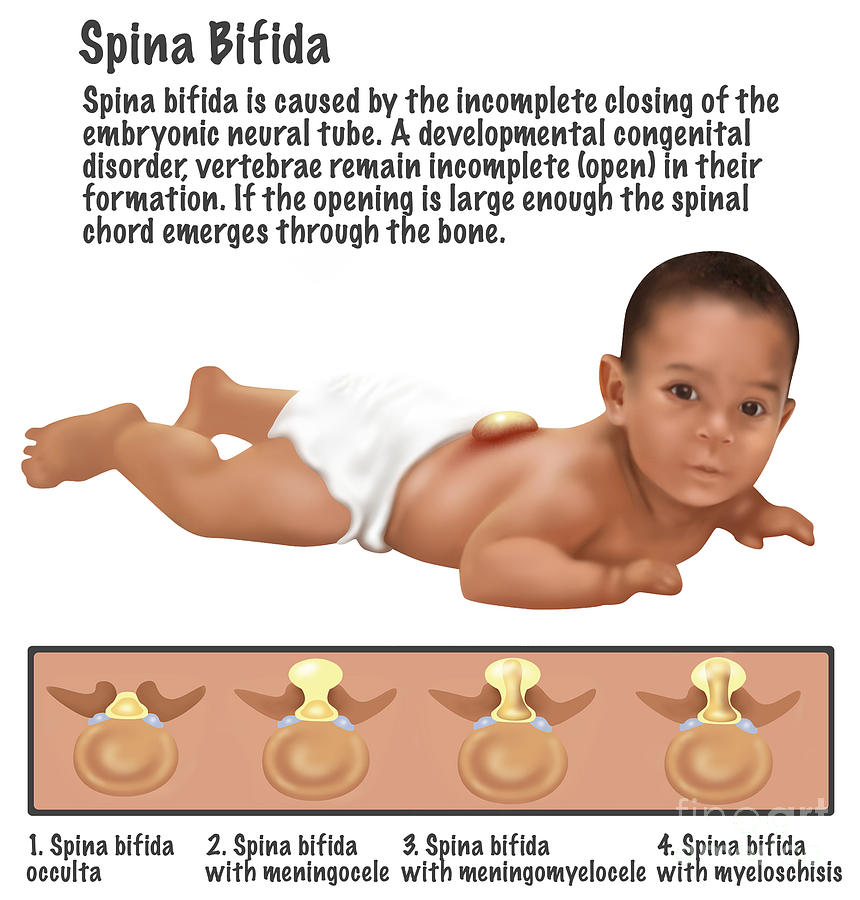 21-NS-309
21-NS-309
Back to Spina Bifida Information Page
See a list of all NINDS disorders
Publicaciones en Español
Espina Bífida
Prepared by:
Office of Neuroscience Communications and Engagement
National Institute of Neurological Disorders and Stroke
National Institutes of Health
Bethesda, MD 20892
NINDS health-related material is provided for information purposes only and does not necessarily represent endorsement by or an official position of the National Institute of Neurological Disorders and Stroke or any other Federal agency. Advice on the treatment or care of an individual patient should be obtained through consultation with a physician who has examined that patient or is familiar with that patient's medical history.
All NINDS-prepared information is in the public domain and may be freely copied. Credit to the NINDS or the NIH is appreciated.
Spina bifida - Diagnosis and treatment
Diagnosis
If you're pregnant, you'll be offered prenatal screening tests to check for spina bifida and other birth defects. The tests aren't perfect. Some mothers who have positive blood tests have babies without spina bifida. Even if the results are negative, there's still a small chance that spina bifida is present. Talk to your doctor about prenatal testing, its risks and how you might handle the results.
The tests aren't perfect. Some mothers who have positive blood tests have babies without spina bifida. Even if the results are negative, there's still a small chance that spina bifida is present. Talk to your doctor about prenatal testing, its risks and how you might handle the results.
Blood tests
Spina bifida can be screened with maternal blood tests, but typically the diagnosis is made with ultrasound.
- Maternal serum alpha-fetoprotein (MSAFP) test. For the MSAFP test, a sample of the mother's blood is drawn and tested for alpha-fetoprotein (AFP) — a protein produced by the baby. It's normal for a small amount of AFP to cross the placenta and enter the mother's bloodstream. But unusually high levels of AFP suggest that the baby has a neural tube defect, such as spina bifida, though high levels of AFP don't always occur in spina bifida.
- Test to confirm high AFP levels. Varying levels of AFP can be caused by other factors — including a miscalculation in fetal age or multiple babies — so your doctor may order a follow-up blood test for confirmation. If the results are still high, you'll need further evaluation, including an ultrasound exam.
- Other blood tests. Your doctor may perform the MSAFP test with two or three other blood tests. These tests are commonly done with the MSAFP test, but their objective is to screen for other conditions, such as trisomy 21 (Down syndrome), not neural tube defects.
Ultrasound
Fetal ultrasound is the most accurate method to diagnose spina bifida in your baby before delivery. Ultrasound can be performed during the first trimester (11 to 14 weeks) and second trimester (18 to 22 weeks).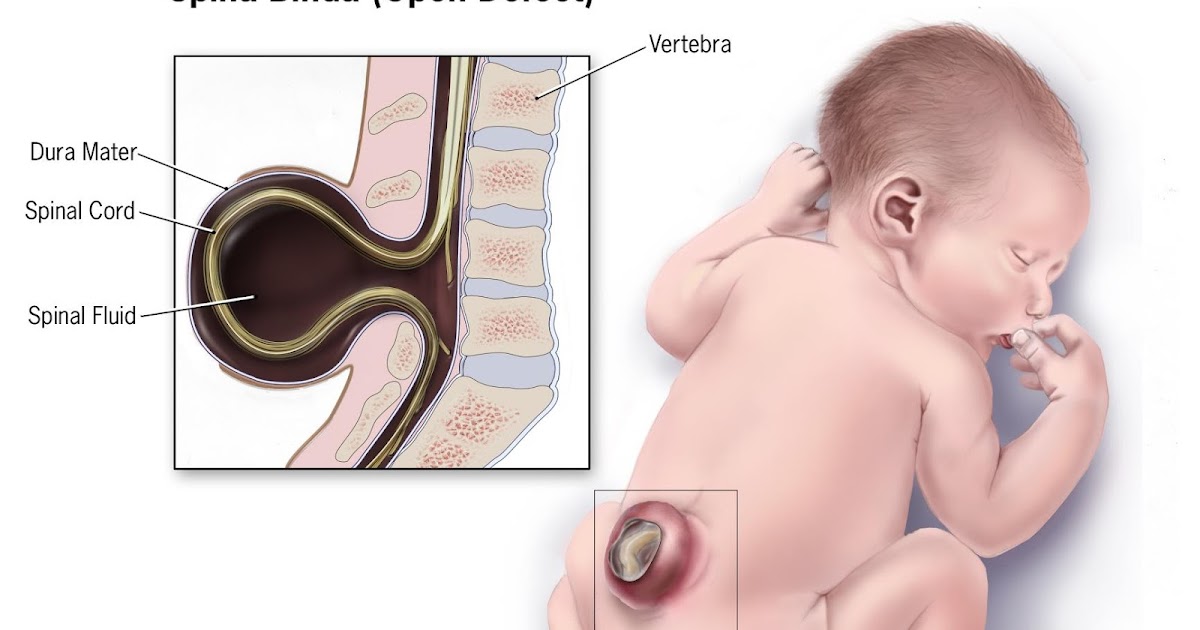 Spina bifida can be accurately diagnosed during the second trimester ultrasound scan. Therefore, this examination is crucial to identify and rule out congenital anomalies such as spina bifida.
Spina bifida can be accurately diagnosed during the second trimester ultrasound scan. Therefore, this examination is crucial to identify and rule out congenital anomalies such as spina bifida.
An advanced ultrasound also can detect signs of spina bifida, such as an open spine or particular features in your baby's brain that indicate spina bifida. In expert hands, ultrasound is also effective in assessing severity.
Amniocentesis
If the prenatal ultrasound confirms the diagnosis of spina bifida, your doctor may request amniocentesis. During amniocentesis, your doctor uses a needle to remove a sample of fluid from the amniotic sac that surrounds the baby.
This examination may be important to rule out genetic diseases, despite the fact that spina bifida is rarely associated with genetic diseases.
Discuss the risks of amniocentesis, including a slight risk of loss of the pregnancy, with your doctor.
Care at Mayo Clinic
Our caring team of Mayo Clinic experts can help you with your spina bifida-related health concerns Start Here
More Information
- Spina bifida care at Mayo Clinic
- Amniocentesis
- Ultrasound
Treatment
Spina bifida treatment depends on the severity of the condition. Spina bifida occulta often doesn't require any treatment at all, but other types of spina bifida do.
Spina bifida occulta often doesn't require any treatment at all, but other types of spina bifida do.
Surgery before birth
Nerve function in babies with spina bifida can worsen after birth if spina bifida isn't treated. Prenatal surgery for spina bifida (fetal surgery) takes place before the 26th week of pregnancy. Surgeons expose the pregnant mother's uterus surgically, open the uterus and repair the baby's spinal cord. In select patients, this procedure can be performed less invasively with a special surgical tool (fetoscope) inserted into the uterus.
Research suggests that children with spina bifida who had fetal surgery may have reduced disability and be less likely to need crutches or other walking devices. Fetal surgery may also reduce the risk of hydrocephalus. Ask your doctor whether this procedure may be appropriate for you. Discuss the potential benefits and risks, such as possible premature delivery and other complications, for you and your baby.
It's important to have a comprehensive evaluation to determine whether fetal surgery is feasible.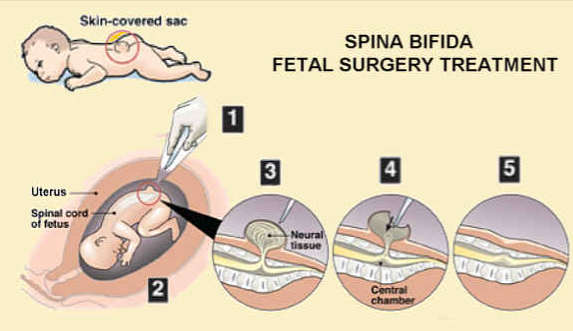 This specialized surgery should only be done at a health care facility that has experienced fetal surgery experts, a multispecialty team approach and neonatal intensive care. Typically the team includes a fetal surgeon, pediatric neurosurgeon, maternal-fetal medicine specialist, fetal cardiologist and neonatologist.
This specialized surgery should only be done at a health care facility that has experienced fetal surgery experts, a multispecialty team approach and neonatal intensive care. Typically the team includes a fetal surgeon, pediatric neurosurgeon, maternal-fetal medicine specialist, fetal cardiologist and neonatologist.
Cesarean birth
Many babies with myelomeningocele tend to be in a feet-first (breech) position. If your baby is in this position or if your doctor has detected a large cyst or sac, cesarean birth may be a safer way to deliver your baby.
Surgery after birth
Myelomeningocele requires surgery to close the opening in the baby's back within 72 hours of birth. Performing the surgery early can help minimize the risk of infection associated with the exposed nerves. It may also help protect the spinal cord from more trauma.
During the procedure, a neurosurgeon places the spinal cord and exposed tissue inside the baby's body and covers them with muscle and skin. At the same time, the neurosurgeon may place a shunt in the baby's brain to control hydrocephalus.
At the same time, the neurosurgeon may place a shunt in the baby's brain to control hydrocephalus.
Treatment for complications
In babies with myelomeningocele, irreparable nerve damage has likely already occurred and ongoing care from a multispecialty team of surgeons, physicians and therapists is usually needed. Babies with myelomeningocele may need more surgery for a variety of complications. Treatment for complications — such as weak legs, bladder and bowel problems, or hydrocephalus — typically begins soon after birth.
Depending on the severity of spina bifida and the complications, treatment options may include:
- Walking and mobility aids. Some babies may start exercises to prepare their legs for walking with braces or crutches when they're older. Some children may need walkers or a wheelchair. Mobility aids, along with regular physical therapy, can help a child become independent. Even children who need a wheelchair can learn to function very well and become self-sufficient.

- Bowel and bladder management. Routine bowel and bladder evaluations and management plans help reduce the risk of organ damage and illness. Evaluations include X-rays, kidney scans, ultrasounds, blood tests and bladder function studies. These evaluations will be more frequent in the first few years of life but less often as children grow. A specialist in pediatric urology with experience in evaluating and performing surgery on children with spina bifida may offer the most effective management options.
- Bowel management may include oral medications, suppositories, enemas, surgery or a combination of these approaches.
- Bladder management may include medications, using catheters to empty the bladder, surgery or a combination of treatments.
- Surgery for hydrocephalus. Most babies with myelomeningocele will need a surgically placed tube that allows fluid in the brain to drain into the abdomen (ventricular shunt).
 This tube might be placed just after birth, during the surgery to close the sac on the lower back or later as fluid accumulates. A less invasive procedure, called endoscopic third ventriculostomy, may be an option. But candidates must be carefully chosen and meet certain criteria. During the procedure, the surgeon uses a small video camera to see inside the brain and makes a hole in the bottom of or between the ventricles so cerebrospinal fluid can flow out of the brain.
This tube might be placed just after birth, during the surgery to close the sac on the lower back or later as fluid accumulates. A less invasive procedure, called endoscopic third ventriculostomy, may be an option. But candidates must be carefully chosen and meet certain criteria. During the procedure, the surgeon uses a small video camera to see inside the brain and makes a hole in the bottom of or between the ventricles so cerebrospinal fluid can flow out of the brain. - Treatment and management of other complications. Special equipment such as bath chairs, commode chairs and standing frames may help with daily functioning. Whatever the issue — orthopedic complications, tethered spinal cord, GI issues, skin problems or others — most spina bifida complications can be treated or at least managed to improve quality of life.
Ongoing care
Children with spina bifida need close follow-up care and observation.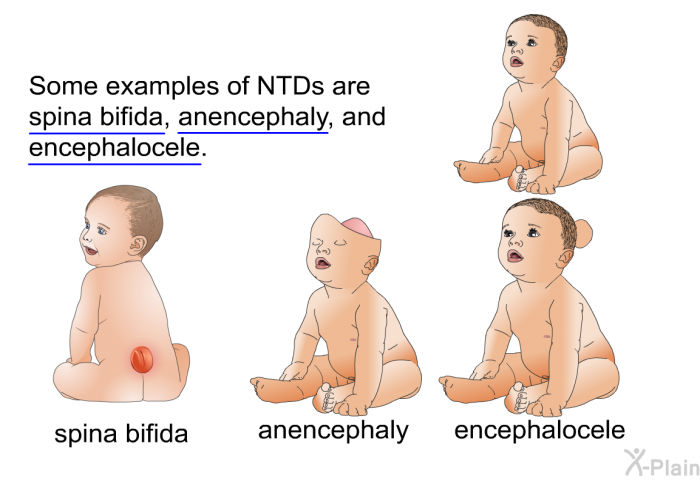 Their primary care doctors evaluate growth, the need for vaccinations and general medical issues, and they coordinate medical care.
Their primary care doctors evaluate growth, the need for vaccinations and general medical issues, and they coordinate medical care.
Children with spina bifida also often need treatment and ongoing care from:
- Physical medicine and rehabilitation
- Neurology
- Neurosurgery
- Urology
- Orthopedics
- Physical therapy
- Occupational therapy
- Special education teachers
- Social workers
- Dietitians
Parents and other caregivers are a key part of the team. They can learn how to help manage a child's condition and how to encourage and support the child emotionally and socially.
More Information
- Spina bifida care at Mayo Clinic
- C-section
- Fetal surgery
Request an Appointment at Mayo Clinic
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.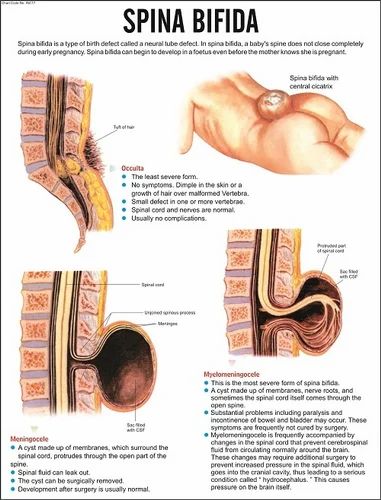
Coping and support
News that your newborn child has a condition such as spina bifida can naturally cause you to feel grief, anger, frustration, fear and sadness. There's good reason for hope, however, because most people with spina bifida live active, productive and full lives — especially with encouragement and support from loved ones. Children with spina bifida can go on to college, hold jobs and have families.
Special accommodations may be necessary along the way, but encourage your child to be as independent as possible.
Independent mobility is an important and appropriate goal for all children with spina bifida. This may mean walking with or without braces, using walking aids (such as canes or crutches), or exclusively using a wheelchair. Encouraging children to participate in activities with their peers can be beneficial, and caregivers can help adjust activities to accommodate physical limitations.
Caregivers of children with spina bifida can help adjust activities to accommodate physical limitations.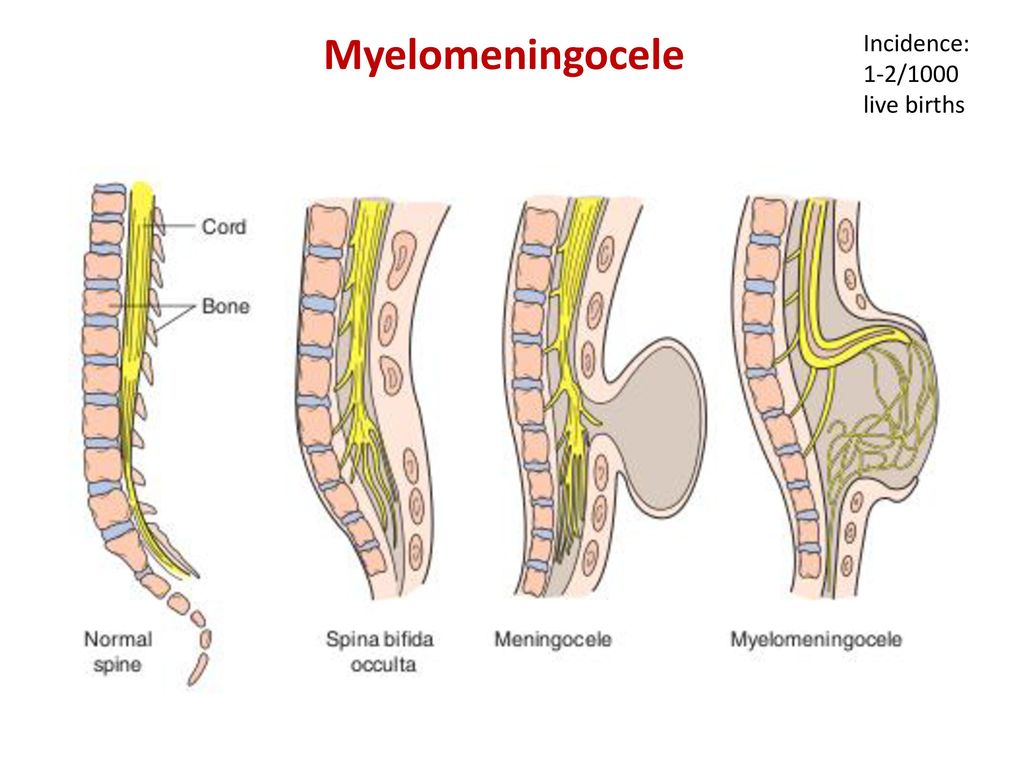
Note: This content was created prior to the coronavirus disease 2019 (COVID-19) pandemic and does not demonstrate proper pandemic protocols. Please follow all recommended Centers for Disease Control and Prevention guidelines for masking and social distancing.
Many children with spina bifida have typical intelligence, but some may need educational intervention for learning problems. Some children experience difficulty with attention, concentration or language that requires treatment from professionals outside of school.
As for any child with a chronic medical condition, children with spina bifida may benefit from meeting with mental health professionals, such as a child psychologist, to assist with adjustment and coping. Most children with spina bifida are resilient and adapt to their challenges with support from their parents, teachers and other caregivers.
If your child has spina bifida, you may benefit from finding a support group of other parents who are dealing with the condition.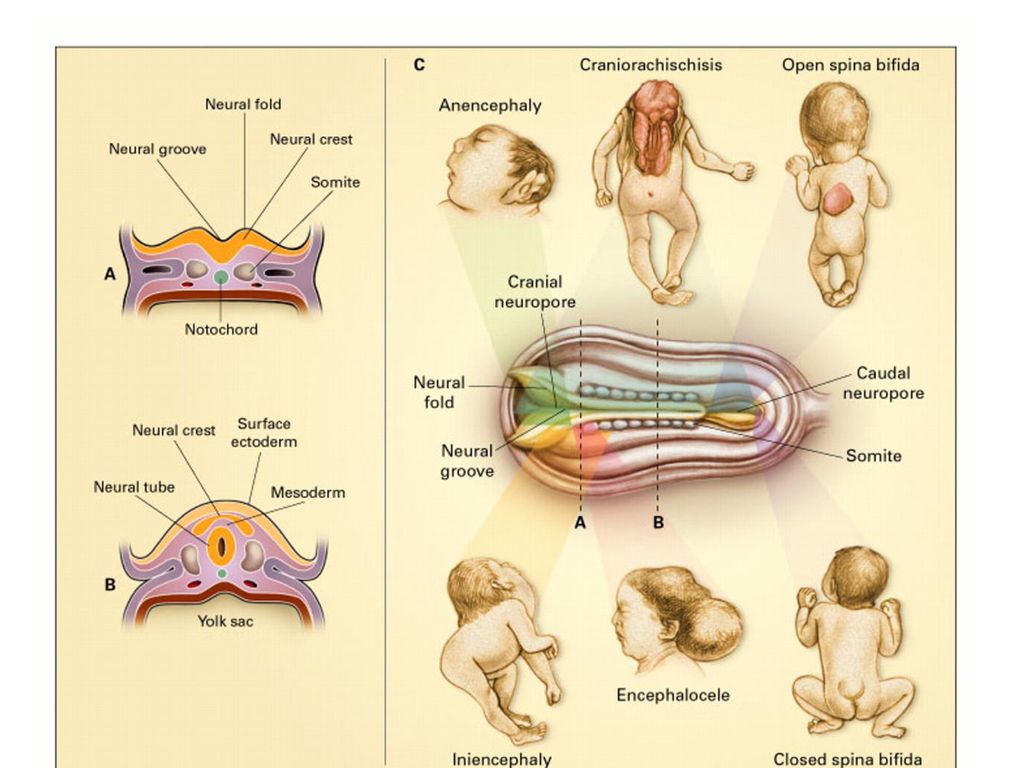 Talking with others who understand the challenges of living with spina bifida can be helpful.
Talking with others who understand the challenges of living with spina bifida can be helpful.
Preparing for your appointment
Your doctor will likely suspect or diagnose your baby's condition during your pregnancy. If that's the case, you'll likely consult with a multispecialty team of physicians, surgeons and physical therapists at a center that specializes in spina bifida treatment.
Here's some information to help you get ready for your appointment and know what to expect from your health care providers if there are suspicions that your baby may have spina bifida.
What you can do
To prepare for the appointment:
- Be aware of any pre-appointment instructions. At the time you make the appointment, be sure to ask if there's anything you need to do in advance, such as drink extra water before an ultrasound.
- Make a list of all medications, vitamins, herbs and supplements that you took before and during your pregnancy, and the dosages.
- Ask a family member or friend to come with you, if possible. Sometimes it can be difficult to remember all the information provided to you during an appointment. Someone who accompanies you may remember something that you missed or forgot.
- Create a list of questions to ask your doctor, starting with the most important in case time runs out.
For spina bifida, some basic questions to ask include:
- Is spina bifida present and how severe is it?
- Is there evidence of accumulation of fluid on the brain (hydrocephalus)?
- Can my baby be treated during pregnancy?
- What will be done for my baby immediately after birth?
- Will the treatment cure my child?
- Will there be any lasting effects?
- Who can I contact to find out about community resources that may be able to help my child?
- What is the likelihood of this happening again in future pregnancies?
- How can I keep this from happening again in the future?
- Are there any brochures or other printed material that I can have? What websites do you recommend?
In addition to the questions that you've prepared, don't hesitate to ask other questions during your appointment.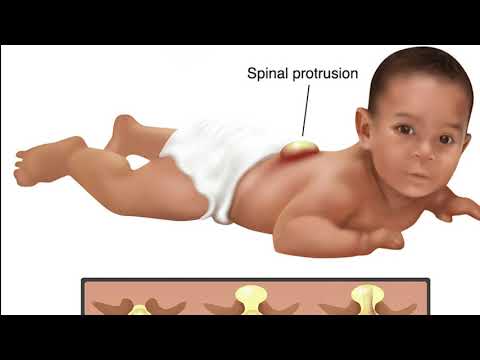
What to expect from your doctor
Being ready to answer questions from your doctor may reserve time to go over any points you want to focus on. Your doctor may ask, for example:
- Have you ever had a child with spina bifida or other birth defects?
- Is there a family history of spina bifida?
- Did you take folic acid (vitamin B-9) before and during your pregnancy?
- Are you taking any anti-seizure medications, or were you taking them at the beginning of your pregnancy?
- If necessary, are you able to travel to a facility that offers specialized care?
By Mayo Clinic Staff
Spina bifida (spina bifida) - treatment, symptoms, causes, diagnosis
Spina bifida (spina bifida) is a complex congenital defect in the development of the spinal cord and spine. This is a type of open neural tube defect in which there is an abnormal development of the back of the spine, the spinal cord, the surrounding nerves, and/or the fluid-filled sac that surrounds the spinal cord.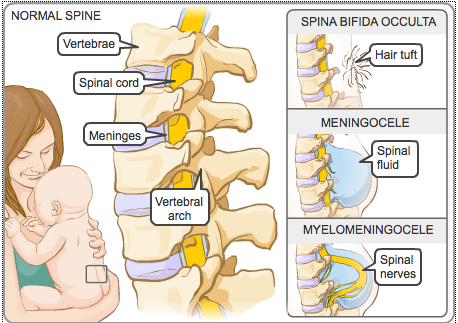
Spina bifida (back bifida) is an incurable, life-long condition that affects the neuromuscular and musculoskeletal systems. nine0003
This defect varies by type and ranges from moderate to severe.
Children with this defect may need corsets as the body grows, and in severe cases, a wheelchair.
Treatment is mainly aimed at slowing down the deformity and maintaining motor activity.
The defect may occur along the entire length of the spine and may present as part of the spinal cord and surrounding tissues protruding outward rather than inward. Approximately 85 percent of defects occur in the lower back and 15 percent in the neck and thoracic region. Surgically, it is possible to restore the integrity of the spinal column, but nerve damage cannot be restored, and if they are pronounced, then patients have various degrees of paresis of the lower extremities. The higher the defect on the spinal column, the more severe the nerve damage and movement disorders (paresis and paralysis). nine0003
nine0003
According to studies, this developmental anomaly occurs in 7 cases per 10,000 newborns. There are several types of spina bifida that have varying degrees of severity.
- Latent spina bifida (spina bifida occulta) - the most moderate form, in which there are no obvious signs of malformation and changes in the skin. In this form, at least one vertebra changes, but the nerves and spinal cord do not bulge. A child at birth may have a spot or depression in the area of the anomaly. And usually, the baby will not have symptoms. With this form of anomaly (as well as with others), there may be an anomaly in the development of the spinal cord, characterized by attachment of the spinal cord to the spine to the end of the lumbar region, when normally the spinal cord ends at the level of the first lumbar vertebrae and sags freely without attachment to the spine. nine0018
- Meningocele is a moderate (and the most common) anomaly in which the spinal canal is not properly closed and the meninges (membranes that cover the spinal cord) bulge outside the bony structures of the spinal canal, but the spinal cord itself remains intact.
 The cystic mass is covered with skin. Most children with meningocele have normal limb function, but may have partial paresis or abnormalities of the bladder or bowel. With this anomaly, there is often underdevelopment of the spinal cord. Almost all patients with this anomaly require surgery to close the defect and free the spinal cord. nine0018
The cystic mass is covered with skin. Most children with meningocele have normal limb function, but may have partial paresis or abnormalities of the bladder or bowel. With this anomaly, there is often underdevelopment of the spinal cord. Almost all patients with this anomaly require surgery to close the defect and free the spinal cord. nine0018 - Lipomeningocele is an anomaly in which fatty tissue is attached to the spinal cord and puts pressure on it. Children with this form of anomaly may not have severe nerve damage, but bladder and bowel function may be impaired. In these cases, surgical treatment is also often used.
- Myelomeningocele: the most severe common form and associated with spina bifida. The spinal canal is not closed, and the bulging mass consists of the meninges, pathologically altered spinal cord, and nerves. In addition, in this area the skin is also underdeveloped. In children with this form of spinal cord splitting, paresis below the defect and dysfunction of the pelvic organs are observed in whole or in part.
 In addition, nerve damage and other pathologies are observed. nine0018
In addition, nerve damage and other pathologies are observed. nine0018
Symptoms
The symptoms of spina bifida vary greatly, depending on the form and severity of the individual child. For example, at birth:
- In latent splitting (spina bifida occulta) there may be no obvious signs or symptoms—only a small spot, depression, or birthmark.
- With a meningocele, there will be a sac-like protrusion that will be located on the back in the spinal region. nine0018
- With myelomeningocele, there will also be a protrusion, but with altered skin, there will be a release of nerves and spinal cord.
In severe spina bifida with localization in the lumbar spine, the following symptoms may occur: paralysis of the lower extremities, dysfunction of the bladder, intestines. In addition, these patients usually have other developmental anomalies:
- Hydrocephalus occurs in 75 percent of myelomeningocele cases and this condition requires operative endoscopic treatment in order to restore normal CSF flow or a shunt to drain excess fluid from the brain.
 nine0018
nine0018 - Chiari anomaly (displacement of the brain into the upper cervical vertebrae) can cause pressure on the brainstem, which can manifest as impaired speech, swallowing, and motor disorders in the limbs.
- Underdevelopment of the spinal cord Orthopedic problems including scoliosis, kyphosis, hip dysplasia (congenital dislocation), combined deformities, clubfoot, etc.
- Precocious puberty (especially in girls with spina bifida and hydrocephalus). nine0017 depression and other neurotic conditions
- obesity
- dermatological problems
- developmental anomalies of the urinary tract.
- heart disease
- vision problems
Diagnosis
Diagnosis may be performed during pregnancy to evaluate the fetus for spina bifida. These include:
- Amniocentesis: A procedure in which a long, thin needle is inserted through the mother's abdomen into the amniotic sac to remove a small amount of amniotic fluid for examination.
 The fluid is analyzed to determine the presence or absence of an open neural tube defect. Although the analysis is very reliable, it does not allow diagnosing small or closed defects. nine0018
The fluid is analyzed to determine the presence or absence of an open neural tube defect. Although the analysis is very reliable, it does not allow diagnosing small or closed defects. nine0018 - Prenatal ultrasound: this technique, being absolutely harmless, allows you to non-invasively assess the condition and visualize the internal organs, vessels, tissues of the fetus. Sometimes it is possible to diagnose not only spina bifida, but also other anomalies.
- Blood tests: It is recommended that blood tests be performed between 15 and 20 weeks of gestation for all women who have not previously had a child with an open neural tube defect and who have no family history of the condition. A blood test for alpha-fetoprotein and other biochemical parameters can determine how high the risk of developing spinal anomalies is. nine0018
- At birth, severe cases of spina bifida are evident by the presence of a fluid-filled sac bulging on the back of the newborn. Visual indicators of mild forms (spina occulta) may be a hairy patch on the skin or a depression along the spine.
 Unusual weakness or lack of coordination in the lower extremities also suggests spina bifida. In children and adults, this anomaly is often diagnosed during routine studies or, if necessary, to differentiate neurological symptoms using instrumental research methods (MRI, CT, radiography). nine0018
Unusual weakness or lack of coordination in the lower extremities also suggests spina bifida. In children and adults, this anomaly is often diagnosed during routine studies or, if necessary, to differentiate neurological symptoms using instrumental research methods (MRI, CT, radiography). nine0018
Causes
During pregnancy, the human brain and spinal column begin to form as a flat sheet of cells that folds into a tube called the neural tube. If all or part of the neural tube fails to close, then the open area is called an open neural tube defect. An open neural tube is open in 80 percent of cases, and is covered by bone or skin in 20 percent of cases. The cause of spina bifida (spina bifida and other defects) remains unknown, but is most likely the result of a combination of genetic, nutritional, and environmental factors, such as: nine0003
- maternal dietary deficiency of folic acid (vitamin B) during pregnancy (sufficient folic acid intake during pregnancy may reduce the risk of this anomaly).
- maternal uncontrolled diabetes
- Certain medicines (antibiotics, anticonvulsants).
- A genetic factor is usually only relevant in 10 percent of cases.
- Mother's age
- What kind of births on the account (firstborns are more at risk). nine0018
- Socioeconomic status (children born in lower socioeconomic families are at higher risk).
- ethnicity
- obesity or excessive consumption of alcohol by a pregnant woman
- When exposed to pregnant hyperthermia in the early stages (sauna, jacuzzi).
Treatment
Spina bifida can be treated immediately after birth. If this defect is diagnosed prenatally, then a caesarean section is recommended in order to reduce possible damage to the spinal cord during the passage of the birth canal. Newborns with meningocele or myelomeningocele are recommended to have surgery within 24 hours of birth. With such an operation, the bone defect is closed and it is possible to preserve the function of the intact part of the spinal cord.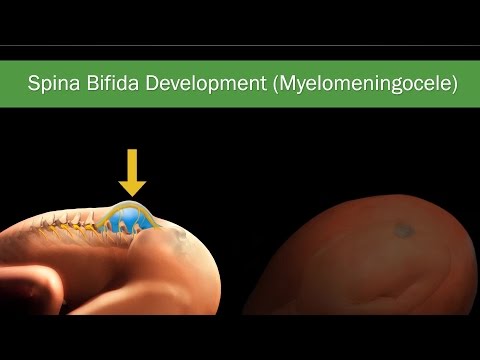 Unfortunately, surgical treatment cannot restore the function of damaged nerves as they are irreversible. nine0003
Unfortunately, surgical treatment cannot restore the function of damaged nerves as they are irreversible. nine0003
Currently, there are clinics that perform prenatal surgery to close the defect, but the techniques have not yet found wide application. The main task of treatment, both in a non-severe form and in the postoperative period, is to preserve the functions of both the musculoskeletal system and the functions of the bladder and intestines. If necessary, orthoses, therapeutic exercises, physiotherapy are used.
In cases where spina bifida is detected by chance during X-ray (MRI, CT) examination, measures must be taken to reduce the risk of spinal cord injury in the area of the spine where this defect exists. nine0003
Operative treatment in adults is used only in the presence of complications. Basically, treatment in adults is aimed only at preventing possible complications (exercise therapy, physiotherapy, wearing a corset).
Spina bifida. What is spina bifida?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment.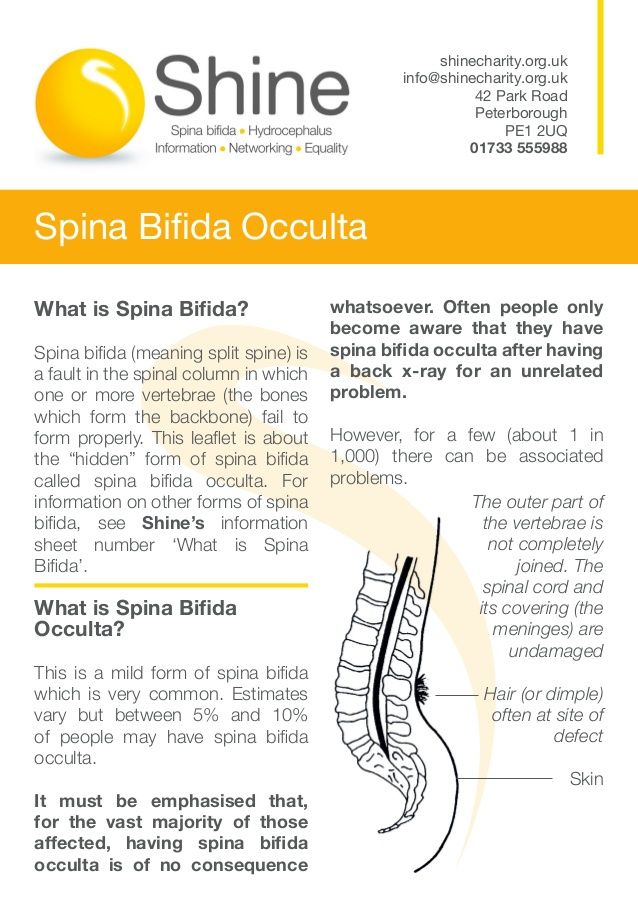 In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor. nine0003
In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor. nine0003
Spina bifida is a malformation of the spinal column, which consists in the underdevelopment of the arches and / or bodies of one or more vertebrae with the formation of a defect in the wall of the spinal canal, through which the membranes and tissues of the spinal cord can prolapse with the formation of congenital spinal hernia. Clinical manifestations are observed in the formation of a hernia or compression of the spinal cord by connective tissue and fatty growths. It is diagnosed clinically, as well as with the help of radiography, CT and MRI of the spine. Treatment is surgical only. The operation is aimed at eliminating the existing defect, but in no way can affect the existing congenital pathology of the spinal cord itself. nine0003
- Causes of spina bifida
- Classification of spina bifida
- Symptoms of spina bifida
- Complications of spina bifida
- Spina bifida diagnostics
- Treatment and prognosis of spina bifida
- Prices for treatment
General
Spina bifida is a congenital anomaly of the spinal column, in which a defect in the bone tissues that form the spinal canal is formed at the level of one or more vertebrae.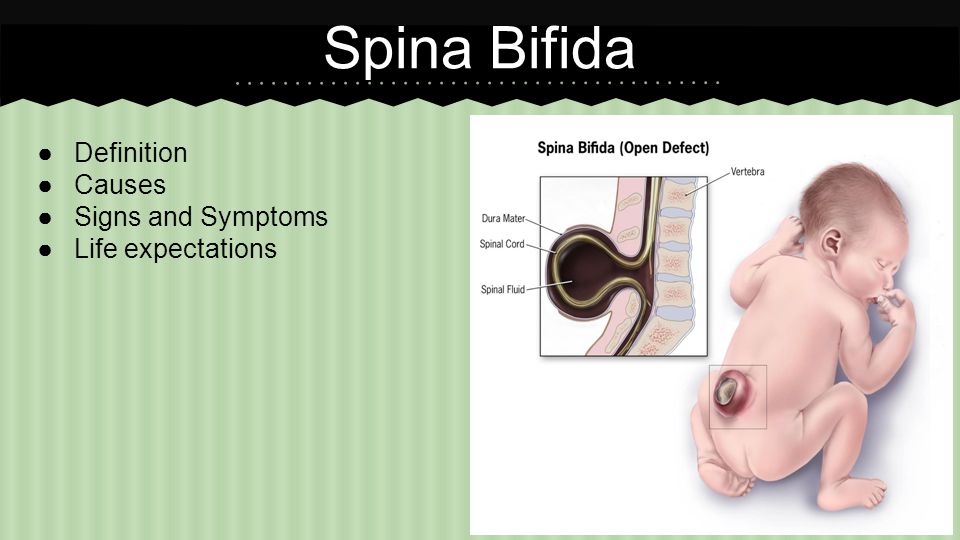 The spinal cord passes through the canal, which can prolapse at the level of the formed defect, forming a congenital spinal hernia. In modern neurology and neonatology, spina bifida is also referred to by the Latin term spina bifida. The prevalence of this anomaly in the development of the spine among the population, according to some data, is up to 20%. At the same time, the incidence of congenital spinal hernia does not exceed 1 case per 3000 newborns. Most often, the anomaly is localized in the lumbosacral spine. nine9% of congenital hernias of the spinal cord are formed in the back of the spinal canal. The contents of the hernia may vary. An exit to the hernial sac of the tissues of the spinal cord is observed in 75% of cases.
The spinal cord passes through the canal, which can prolapse at the level of the formed defect, forming a congenital spinal hernia. In modern neurology and neonatology, spina bifida is also referred to by the Latin term spina bifida. The prevalence of this anomaly in the development of the spine among the population, according to some data, is up to 20%. At the same time, the incidence of congenital spinal hernia does not exceed 1 case per 3000 newborns. Most often, the anomaly is localized in the lumbosacral spine. nine9% of congenital hernias of the spinal cord are formed in the back of the spinal canal. The contents of the hernia may vary. An exit to the hernial sac of the tissues of the spinal cord is observed in 75% of cases.
Spina bifida
Causes of spina bifida
Spina bifida is caused by disorders in the formation of the neural tube, which occurs at the 3rd week of pregnancy and ends by the 23rd day of gestation.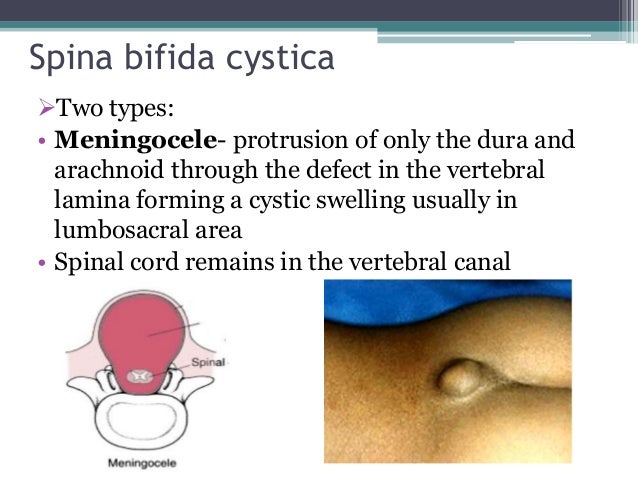 Spina bifida is a multifactorial pathology. Hereditary mechanisms, spontaneous mutations and exposure to teratogenic factors may play a role in its development. nine0003
Spina bifida is a multifactorial pathology. Hereditary mechanisms, spontaneous mutations and exposure to teratogenic factors may play a role in its development. nine0003
The latter include intrauterine infections (cytomegaly, measles, rubella, herpes), hyperglycemia in diabetes mellitus, constant overheating of the body of a pregnant woman (insolation, hot baths, sauna), taking pregnant pharmaceuticals with a teratogenic side effect (for example, antibiotics, anticonvulsants), folate deficiency acids, intoxication (drug addiction, alcoholism, substance abuse, occupational hazards), radiation. The situation is aggravated by the fact that often at such early stages of gestation, a woman does not know about her pregnancy and does not comply with the necessary protective regime aimed at excluding possible teratogenic effects as much as possible. nine0003
Classification of spina bifida
Allocate hidden and open spina bifida. Hidden (spina bifida occulta) is a small bone defects (for example, non-closure of the vertebral arches) without the formation of a spinal hernia.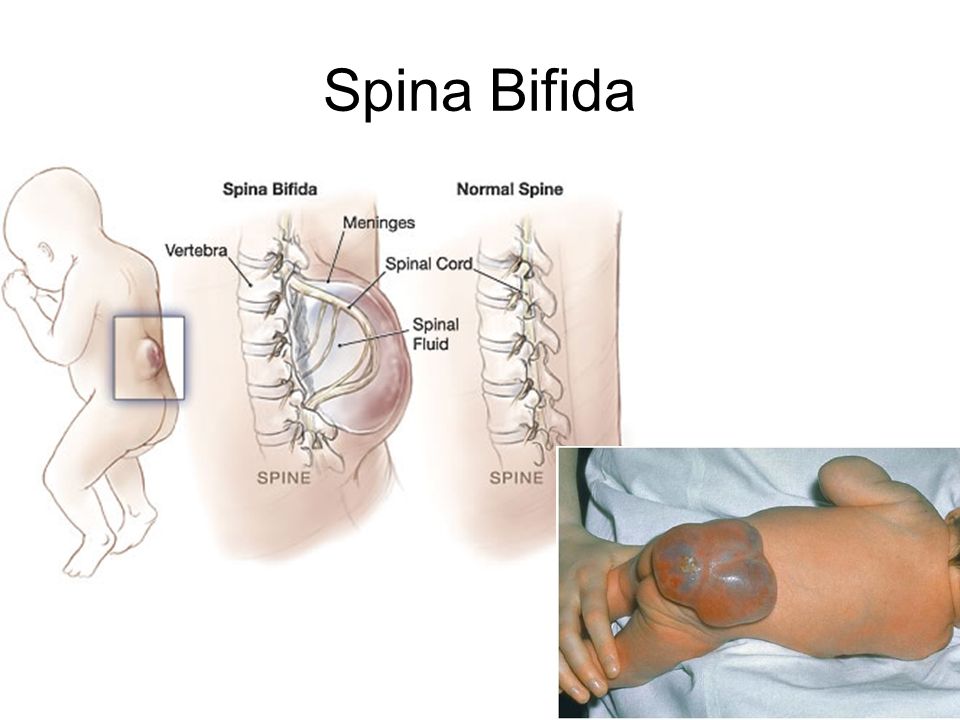 Open spina bifida (spina bifida aperta) includes rachischisis and herniated spinal cord. Any type of spina bifida can be accompanied by the growth of fibro-adipose tissue, which fills bone defects, penetrates into the subarachnoid space and causes compression of the spinal cord. nine0003
Open spina bifida (spina bifida aperta) includes rachischisis and herniated spinal cord. Any type of spina bifida can be accompanied by the growth of fibro-adipose tissue, which fills bone defects, penetrates into the subarachnoid space and causes compression of the spinal cord. nine0003
Depending on the contents of the hernial sac, there are 4 forms of congenital spinal hernias. With meningocele, only cerebrospinal fluid (CSF) is in the hernial sac. Meningoradiculocele, in addition to cerebrospinal fluid, contains the membranes of the spinal cord. In myelomeningocele, the hernia consists of cerebrospinal fluid, membranes, and tissues of the spinal cord. Myelocystocele is a complete prolapse of a segment of the spinal cord with membranes, accompanied by eversion and expansion of the spinal canal. Rakhishizis is a spina bifida in the most severe form, when a bone defect of great length is combined with non-fusion of the membranes of the spinal cord and skin. In this case, the spinal cord is visible through a gaping hole in the spine. This pathology leads to death. nine0003
This pathology leads to death. nine0003
Symptoms of spina bifida
Latent spina bifida is usually asymptomatic. Clinical manifestations manifest in cases of proliferation of fibro-adipose tissue with compression of the roots and other structures of the spinal cord. Most often, the debut of the clinic falls on adolescence. Characterized by radicular pain of the type of sciatica, which the patients themselves describe as a sensation of the passage of an electric current. On the skin in the area of a bone defect, as a rule, there is a tuft of hair and / or a pigment spot, sometimes a papilloma. nine0003
A meningocele is characterized by a visible bulge on the spine covered by a thin layer of skin. Such spina bifida occurs without the development of a neurological deficit. Meningoradiculocele is a protrusion that occupies the area from 4 to 5 vertebrae. The nature of neurological disorders depends on the number of roots involved in the hernial sac and the location of the hernia. The clinic can vary from mild paresis to a pronounced decrease in muscle strength, sensory and pelvic disorders. Myelomeningocele and myelocystocele involve 6 to 8 vertebrae and are not covered by skin, characterized by severe paralysis, lack of sensation, urinary incontinence, and encopresis. nine0003
The clinic can vary from mild paresis to a pronounced decrease in muscle strength, sensory and pelvic disorders. Myelomeningocele and myelocystocele involve 6 to 8 vertebrae and are not covered by skin, characterized by severe paralysis, lack of sensation, urinary incontinence, and encopresis. nine0003
Spina bifida is often accompanied by hydrocephalus. It can be combined with other malformations: Chiari anomaly, curvature of the spine (scoliosis, kyphosis), clubfoot, congenital limb deformities, hip dysplasia, congenital heart defects, multiple dermatofibromas, lipomas, teratomas.
Complications of spina bifida
Spina bifida with the formation of a hernia is dangerous by infection of the hernial sac. As a rule, such a complication occurs in the absence of the skin over the hernial protrusion. In addition, infection can occur with ruptures and other damage to the thinned skin covering the hernia. In such cases, reddening of the tissues of the hernial sac and surrounding skin is observed.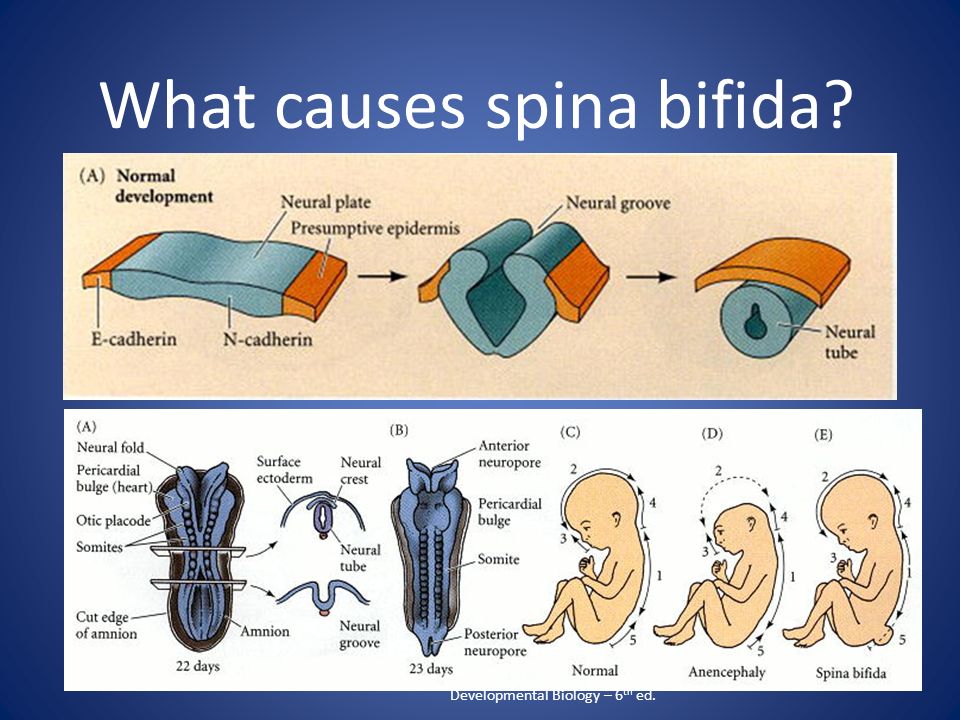 Infection is dangerous by the spread of inflammation to the meninges with the development of meningitis, the infection enters the bloodstream with the onset of sepsis. nine0003
Infection is dangerous by the spread of inflammation to the meninges with the development of meningitis, the infection enters the bloodstream with the onset of sepsis. nine0003
Another complication of congenital spinal hernias can be a rupture of the hernial sac with the outflow of cerebrospinal fluid (liquorrhea), which leads to a drop in cerebrospinal fluid pressure and also opens the gate for infection. In addition, spina bifida can be complicated by increasing compression of the spinal cord, which eventually leads to irreversible changes in the spinal tissues.
Spina bifida diagnostics
Hidden spina bifida is often not diagnosed during life. The diagnosis of congenital spinal hernia is established by a neonatologist together with a neurologist according to the clinic and the results of palpation - palpation of the bone defect of the spine. Clarification of the diagnosis is carried out using CT and MRI of the spine. CT of the spine to a greater extent allows you to identify existing bone defects and deformities, MRI - to obtain information about the state of the spinal cord and its membranes, to establish the contents of the hernial sac.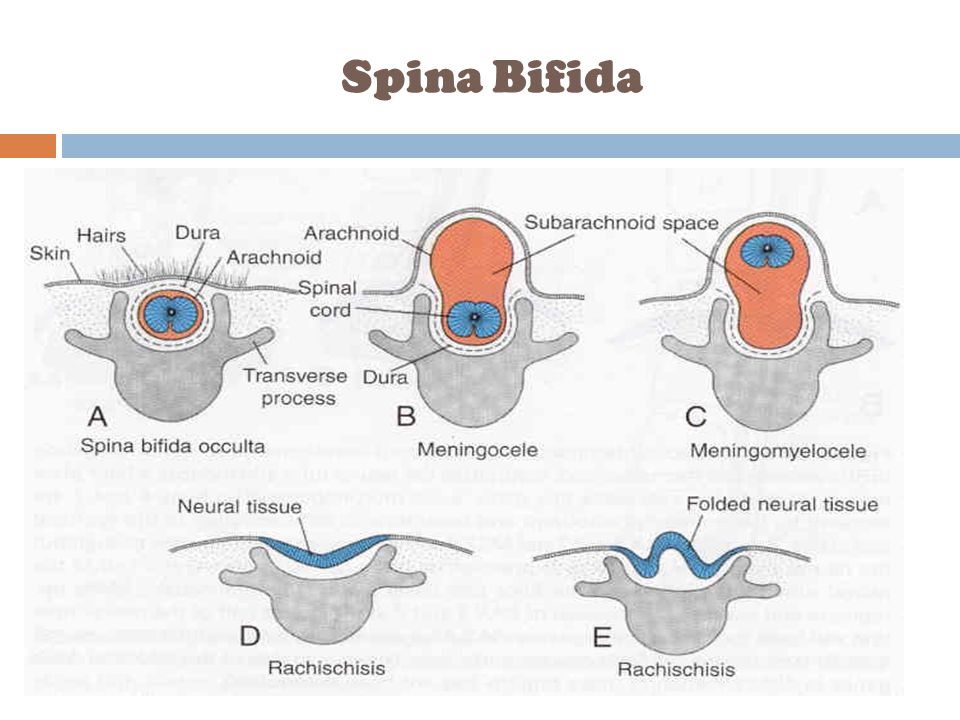 In younger children, CT is not performed due to high radiation exposure. In the absence of the possibility of a tomographic examination, an X-ray of the spine is used. nine0003
In younger children, CT is not performed due to high radiation exposure. In the absence of the possibility of a tomographic examination, an X-ray of the spine is used. nine0003
CT scan of the lumbar spine. Absence of complete fusion of the L5 arch (Spina bifida)
It is mandatory to conduct a study of somatic organs to identify concomitant congenital pathology. For this purpose, a biochemical analysis of blood and urine, urography, CT scan of the kidneys, chest x-ray, ultrasound of the heart, ultrasound of the abdominal cavity, MSCT of the abdominal cavity, radiography of bones and joints are prescribed. Specialists of various profiles can be involved in the diagnosis as necessary: nephrologist, cardiologist, gastroenterologist, etc. nine0003
In some cases, prenatal diagnosis is possible. Spina bifida can be suspected according to obstetric ultrasound, amniocentesis, followed by a study of the concentration of acetylcholinesterase and α-fetoprotein in the amniotic fluid.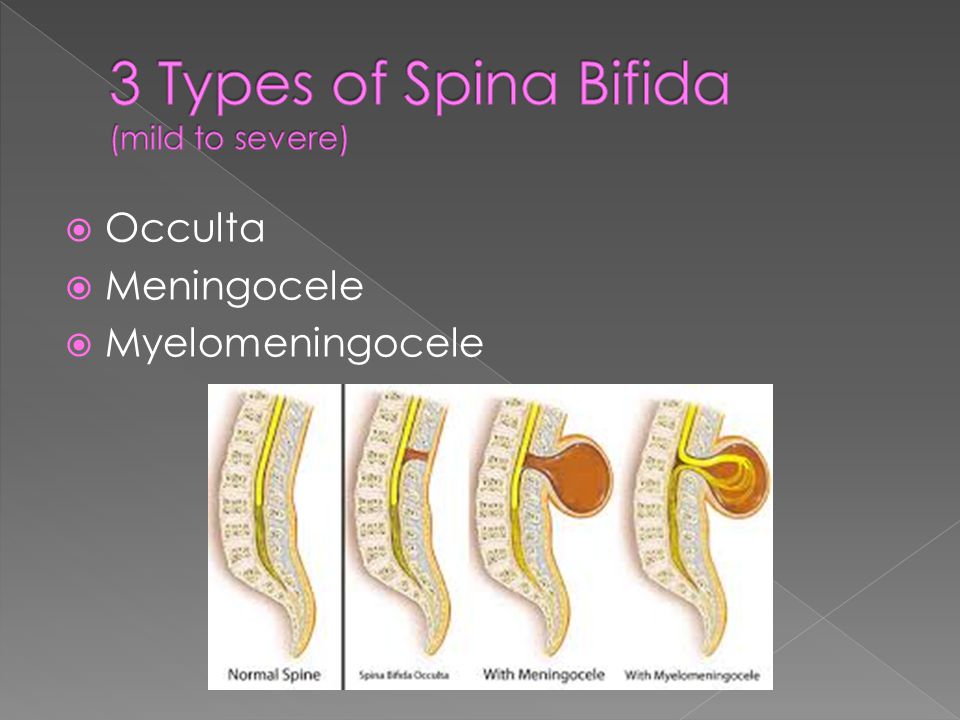 Prenatally diagnosed spina bifida is an indication for caesarean section, which helps to prevent injury to the spinal hernia during natural childbirth.
Prenatally diagnosed spina bifida is an indication for caesarean section, which helps to prevent injury to the spinal hernia during natural childbirth.
Treatment and prognosis of spina bifida
Open spina bifida needs surgical treatment. The operation is carried out by neurosurgeons in a planned manner in the first days of a newborn's life. It helps to prevent the development of complications and the growth of neurological deficit, to eliminate the existing cosmetic defect. In case of violation of the integrity of the hernial sac and liquorrhea, the operation is performed in an urgent manner. Contraindications to surgical treatment may be severe disorders of the somatic organs due to concomitant congenital pathology. nine0003
The operation is performed using general anesthesia. Its essence is to close the existing defect. An incision is made along the surface of the hernial protrusion. Nerve formations are carefully separated and retracted inside behind the spinal membranes.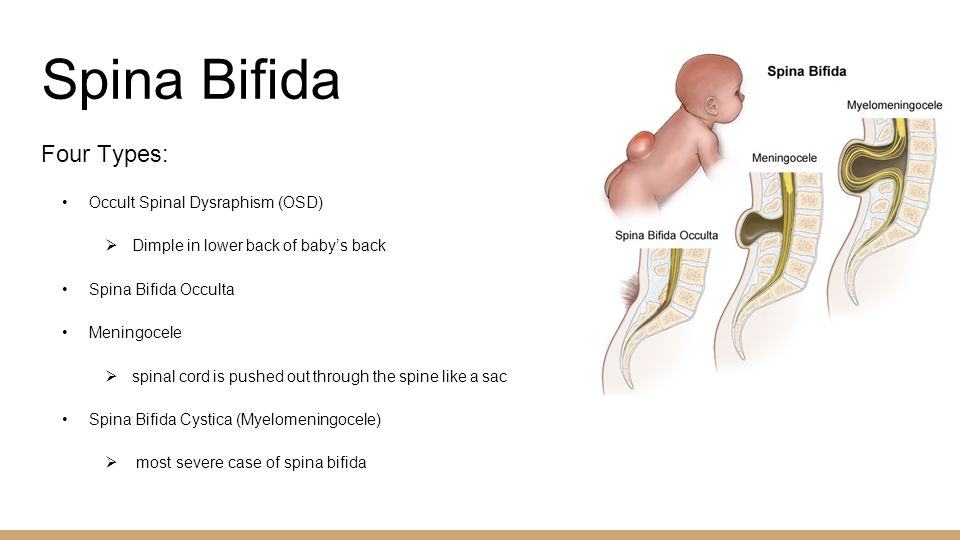 The membranes are sutured in layers, the skin defect is closed. Complications of surgical intervention can be increasing hydrocephalus, infection of the wound, divergence of its edges, trophic disorders in the area of the postoperative wound that interfere with its healing. A lumboperitoneal shunt may be used to prevent hydrocephalus. nine0003
The membranes are sutured in layers, the skin defect is closed. Complications of surgical intervention can be increasing hydrocephalus, infection of the wound, divergence of its edges, trophic disorders in the area of the postoperative wound that interfere with its healing. A lumboperitoneal shunt may be used to prevent hydrocephalus. nine0003
In the postoperative period, rehabilitation treatment is carried out, aimed at increasing muscle strength and range of motor activity, preventing joint contractures. Various methods of physiotherapy, physiotherapy exercises, massage are used. The outcome of the operation largely depends not on the skills of the neurosurgeon, but on the form of the spinal hernia. If spina bifida is not accompanied by the involvement of spinal cord tissues in the hernial sac, then after the operation there is a complete or significant restoration of neurological functions. With myelomeningocele and myelocystocele, the existing neurological deficit persists after surgery, since surgical intervention is not able to restore the altered tissues of the spinal cord.