39 weeks pregnant c section
C-sections - everything you need to know
Tommy's PregnancyHub
A caesarean section (c-section) may be planned or unplanned. Find out why you may need a c-section and what to do if you would like to have one.
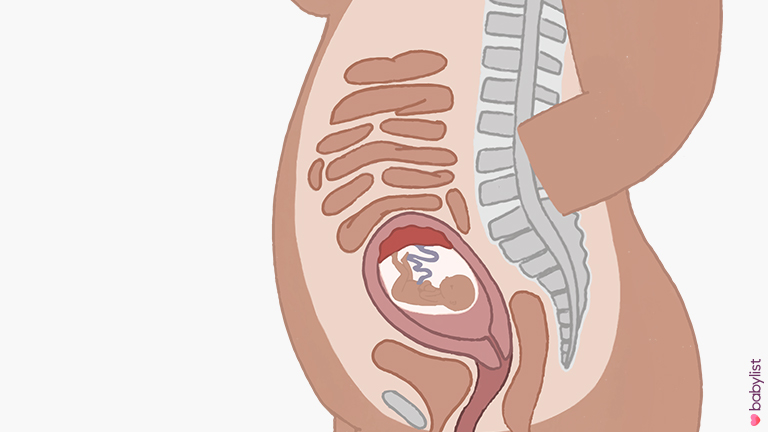
A caesarean section (c-section) is an operation to deliver your baby. A doctor makes a cut just below your bikini line, through your abdomen and womb, and lifts your baby out through it.
You may have a planned (elective) c-section if you know you will need a c-section before you go into labour.
You may have an unplanned (emergency) c-section if this is the safest way to deliver your baby.
About 1 in 4 women who give birth in the UK have a c-section. Most of these are emergency c-sections.
What is a planned c-section?
Sometimes, a c-section may be safer for you or your baby than a vaginal birth. For example, your doctor or midwife may offer you a planned c-section if:
- there are problems with the placenta, such as a low-lying placenta (placenta praevia)
- your baby is lying in a difficult position for labour, such as bottom down (breech)
- you are expecting twins who share a placenta or if either baby is lying in a difficult position for labour
- you are expecting more than 2 babies.
If you have HIV or genital herpes, your doctor will explain your birth options. Some women may need a c-section to reduce the risk of passing the virus to the baby.
“Don’t be afraid to ask your consultant for more information. I wasn’t well informed about my placenta praevia and unfortunately was one of the small minority of women whose placenta haemorrhages. I felt this wasn’t clearly explained enough as a risk and I could have been better prepared.”
Emily
If you are offered a c-section because of medical reasons, it is your choice whether to have one or not. You do not have to have one if you don’t want one.
You may want to have a c-section, even if there’s no medical need. Read more about your options for giving birth.
If you decide to have a planned c-section, you will see an obstetrician. This is a doctor who specialises in care during pregnancy, labour and after birth. They will explain the benefits and risks of a c-section and your other birth options. You will also see a midwife at your antenatal appointments where you can discuss your options.
You will also see a midwife at your antenatal appointments where you can discuss your options.
You will usually have a planned c-section at 39 weeks of pregnancy. The aim is to do the c-section before you go into labour. Babies born earlier than 39 weeks are more likely to need help with their breathing. Sometimes there’s a medical reason for delivering the baby earlier than this. For example, if you’re expecting more than 1 baby.
What is an emergency c-section?
You may have an unplanned emergency c-section if your baby needs to be delivered quickly. This may happen if your labour is not progressing or there’s any concern about your or your baby’s wellbeing.
The word ‘emergency’ makes it sound rushed, but there’s often time to decide whether you want a c-section. Your doctor and midwife will explain what your options are. If your or your baby’s health is at risk, you may need to have a c-section more quickly.
"Everything I had ever heard about c-sections had been negative and scary.
So, when I was told I needed an emergency c-section, I was very anxious. But it went well and I had a good experience, which I hadn’t thought was possible."
C-section myths
There’s no strong evidence that any of these things affect your chances of needing a c-section:
- walking around during labour
- not lying on your back during labour
- being in water during labour
- drinking raspberry leaf tea
- the midwife or doctor breaking your waters early
- having an epidural.
There is no evidence that your height or the size of your baby can predict whether you will need a c-section. Being short or having a small pelvis or small feet does not affect whether you can have a vaginal birth. But you may be more likely to have a c-section if you’re overweight or over the age of 40.
You may be less likely to have a c-section if you:
- give birth in a midwife-led unit, or
- have continuous support during labour from a midwife or someone trained to support you, such as a doula.
Read about what happens during a c-section.
Read about preparing for a c-section.
Read about your options for giving birth.
Review dates
Reviewed: 16 July 2021 | Next review: 16 July 2024
Tags
- Mum
- Dad
- Singleton
- Multiple
- During pregnancy
Back to top
‘Elective caesarean section at 38–39 weeks gestation compared to > 39 weeks on neonatal outcomes: a prospective cohort study | BMC Pregnancy and Childbirth
- Research article
- Open Access
- Published:
- Reihaneh Pirjani1,2,
- Motahareh Afrakhteh3,
- Mahdi Sepidarkish4,
- Shahin Nariman5,
- Mahboobeh Shirazi6,
- Ashraf Moini7,8 &
- …
- Ladan Hosseini9
BMC Pregnancy and Childbirth volume 18, Article number: 140 (2018) Cite this article
-
92k Accesses
-
11 Citations
-
2 Altmetric
-
Metrics details
Abstract
Background
This study was conducted to compare neonatal complications in scheduled cesarean sections (CS) between 38 and 39 gestational weeks with CS performed after 39 gestational weeks in Iranian low -risk pregnant women.
Methods
In this cohort study, 2086 patients were enrolled based on the inclusion and exclusion criteria. The neonates were evaluated in terms of the following items: transient tachypnea of the newborn (TTN), respiratory distress syndrome (RDS), sepsis, need for NICU hospitalization, birth weight, birth height, head circumference, and the first minute and fifth minute Apgar score. Several multiple logistic regression models were performed for each response variable (adverse outcome) separately.
Results
The incidence of NICU admission was significantly higher in neonates born at 38–39 gestational weeks than those who were born after 39 gestational weeks. No significant differences were found in the incidence of neonatal sepsis, TTN, and RDS between the two groups.
Conclusion
According to our study results, elective CS at 38–9 weeks’ gestation is associated with a higher rate of TTN and NICU admission in comparison with elective CS performed after 39 completed gestational weeks.
Peer Review reports
Background
The appropriate gestational age for scheduled cesarean section (CS) has become a topic of interest in prenatal care [1]. For the past four decades, obstetricians and pediatricians, assuming that fetal maturity could be completed at the end of 37 gestational weeks, have defined “the term pregnancy” from that time onwards [2]. However, it has now become clear that even in “the term pregnancy” (37 gestational weeks), neonatal respiratory complications will decrease with an increase in the gestational age to 39 weeks. These findings have challenged the old definition of “theterm pregnancy” [3]. Recently, the definition of “the term pregnancy” has changed to cover three categories of premature term (37–38 weeks + 6 days), full term (39–40 weeks and 6 days), and late term (41-41 weeks + 6 days) [4].
Experts recommend that scheduled cesarean delivery be conducted from 39 weeks onwards [5], so that fetal maturity is complete. Some studies have shown discrepancies in respiratory complications according to the gestational age pattern between Asian and Caucasian ethnicities. The lowest complication rate was observed in 39–40 gestational weeks in the Caucasians and in 38 gestational weeks in Asians [1]. Accordingly, this study aimed to compare neonatal complications in scheduled CS between 38 and 39 gestational weeks with scheduled CS performed after 39 gestational weeks in Iranian pregnant women.
Some studies have shown discrepancies in respiratory complications according to the gestational age pattern between Asian and Caucasian ethnicities. The lowest complication rate was observed in 39–40 gestational weeks in the Caucasians and in 38 gestational weeks in Asians [1]. Accordingly, this study aimed to compare neonatal complications in scheduled CS between 38 and 39 gestational weeks with scheduled CS performed after 39 gestational weeks in Iranian pregnant women.
Method and materials
This prospective cohort study was conducted at a university hospital (Arash Hospital, Tehran, Iran) from April 2013 to April 2015. All term singleton pregnancies (≥38 gestational weeks) scheduled for elective CS were enrolled in this study. The research protocol of the study was approved by the Ethical Research Committee of Tehran University of Medical Sciences. The informed consent was obtained from all pregnant women. The inclusion criteria were singleton pregnancy and elective CS scheduled for 38 complete gestational weeks or later. The exclusion criteria were gestational age below 38 completed gestational weeks, multiple pregnancy, maternal chronic diseases, gestational diabetes, preeclampsia, CS due to fetal distress, intra uterine growth restriction, meconium defecation, placenta previa or accreta, fetal abnormalities, CS during the active phase of labor, repeated CS after beginning of uterine contracture, and any other cause of emergency CS.
The exclusion criteria were gestational age below 38 completed gestational weeks, multiple pregnancy, maternal chronic diseases, gestational diabetes, preeclampsia, CS due to fetal distress, intra uterine growth restriction, meconium defecation, placenta previa or accreta, fetal abnormalities, CS during the active phase of labor, repeated CS after beginning of uterine contracture, and any other cause of emergency CS.
All patients had two ultrasonography reports in the first trimester, one at 6–9 gestational weeks and the other at 11–14 gestational weeks. Gestational age was determined based on the date of the last menstrual period (LMP). If the difference was more than 5 days, gestational age was estimated based on ultrasound criterion at 6–9 gestational weeks provided that it was confirmed by ultrasound at 11–14 weeks. In our practice, at least two ultrasound examinations are routinely performed in the first trimester in all pregnant women, one at 6–9 gestational weeks and the other at 11–14 gestational weeks. All ultrasound examinations were performed by a perinatologist or radiologist experienced in obstetric sonography. Gestational age (GA) was determined by measuring of the fetal crown-rump-length (CRL) at 6–9 and 11–14 gestational weeks. The average CRL measurement in mm was derived from three satisfactory images. CRL was converted to the equivalent number of gestational days according to Hadlock et al. (1992). All pregnant women received their antenatal care at our hospital.
All ultrasound examinations were performed by a perinatologist or radiologist experienced in obstetric sonography. Gestational age (GA) was determined by measuring of the fetal crown-rump-length (CRL) at 6–9 and 11–14 gestational weeks. The average CRL measurement in mm was derived from three satisfactory images. CRL was converted to the equivalent number of gestational days according to Hadlock et al. (1992). All pregnant women received their antenatal care at our hospital.
The collected data were maternal age, parity, neonatal weight, and neonatal complications. The following items were considered to evaluate the neonatal outcomes: transient tachypnea of the newborn (TTN) defined as the presence of tachypnea within hours after birth; respiratory distress syndrome (RDS) defined as the signs of respiratory distress (radiological features and oxygen therapy), sepsis, need for NICU hospitalization, and first minute and fifth minute Apgar scores.
Statistical analysis and sample size
The sample size was calculated on the assumption that the incidence of TTN would be 3% in women with a delivery time between 38 and 39 gestational weeks and 1% in women with a delivery time ≥ 39 gestational weeks. The estimated sample size was 866 women in each group (α = 0.05; 1 - β = 0.80).
The estimated sample size was 866 women in each group (α = 0.05; 1 - β = 0.80).
Categorical and continuous variables are expressed as number (percentage) and mean ± (standard deviation), respectively. Chi-square test was applied to compare categorical variables. Student’s t-test was used to compare parametric continuous variables. In order to control the potential confounders, a multiple logistic regression model was fitted for each dependent outcome variable (TTN, RDS, sepsis and need for NICU hospitalization). Explanatory variables were considered into the model for adjustment in the following order: maternal age, parity, neonatal weight, first minute Apgar, and fifth minute Apgar. The results are presented as odds ratios (OR) with 95% confidence intervals. Data analysis was undertaken using the Stata statistical software, released 13.0 (Stata Corp, College Station, Tex, USA).
Results
Totally, 4892 CS were performed in our hospital during the study period, and based on the inclusion and exclusion criteria, 2086 patients were enrolled. In our study, 1002 (48%) women delivered between 38 and 39 gestational weeks and 1084 (52%) women delivered after 39 gestational weeks. Indications for elective caesarean delivery were prior caesarean section in 54.5% (1137 women), breech presentation in 7.2% (150 women), suspected cephalopelvic disproportion in 4.6% (96 women), maternal requested CS in 28.8% (601 women), and other causes such as retinopathy or myopathy and a history of infertility in 4.9% (102 women).
In our study, 1002 (48%) women delivered between 38 and 39 gestational weeks and 1084 (52%) women delivered after 39 gestational weeks. Indications for elective caesarean delivery were prior caesarean section in 54.5% (1137 women), breech presentation in 7.2% (150 women), suspected cephalopelvic disproportion in 4.6% (96 women), maternal requested CS in 28.8% (601 women), and other causes such as retinopathy or myopathy and a history of infertility in 4.9% (102 women).
The mean ± (SD) age of the mothers who delivered between 38 to 39 gestational weeks was 27.77 ± (5.29) years, which was significantly higher than the mean (SD) age of mothers who delivered at > 39 gestational weeks (27.27 ± 5.74 years) (P = 0.041) (Table 1).
Table 1 Comparison of demographic characteristics of participantsFull size table
As shown in Table 1, repeated caesarean was more frequent in mothers who delivered between 38 and 39 gestational weeks compared to mothers who delivered after 39 gestational weeks (64. 7% vs. 45.1%, P < 0.001). Inversely, the frequency of breech presentation (10% vs. 4.2%), Cephalopelvic Disproportion (CPD) (5.4% vs. 3.8%), and maternal request (35.4% vs. 21.7%) were higher in mothers who delivered after 39 weeks’ gestation compared to mothers who delivered between 38 and 39 gestational weeks (P < 0.001).
7% vs. 45.1%, P < 0.001). Inversely, the frequency of breech presentation (10% vs. 4.2%), Cephalopelvic Disproportion (CPD) (5.4% vs. 3.8%), and maternal request (35.4% vs. 21.7%) were higher in mothers who delivered after 39 weeks’ gestation compared to mothers who delivered between 38 and 39 gestational weeks (P < 0.001).
The weight of neonates born after 39 gestational weeks was significantly higher than neonates born between 38 and 39 gestational weeks (mean difference: 136.76, 95% CI: 103.61 to 169.91, P < 0.001). Also, the one-minute Apgar score was significantly different between the two groups (mean difference: 0.02, 95% CI: 0.002 to 0.04, P = 0.029). There was no statistical significant difference in other characteristics between the two groups .
No significant differences were found in the incidence of neonatal sepsis between the two groups (0.6 and 0.4% in neonates born between 38 and 39 and after 39 gestational weeks respectively, adjusted OR: 1. 60, 95% CI: 0.48 to 5.31, P = 0.440). The incidence of respiratory distress syndrome (RDS) was 0.7% (7 neonates) and 0.3% (3 neonates) in group 1 and 2, respectively. (Adjusted OR: 2.07, 95%CI: 0.56 to 7.56, P = 0.270).
60, 95% CI: 0.48 to 5.31, P = 0.440). The incidence of respiratory distress syndrome (RDS) was 0.7% (7 neonates) and 0.3% (3 neonates) in group 1 and 2, respectively. (Adjusted OR: 2.07, 95%CI: 0.56 to 7.56, P = 0.270).
The incidence of NICU admission was 2.2% (22 people) in neonates born between 38 and 39 gestational weeks and 0.7% (8 people) in those born after 39 gestational weeks. The difference was statistically significant (adjusted OR: 2.59, 95%CI: 1.16 to 5.79, P = 0.020).
The incidence of TTN was 1.5% (15 neonates) in neonates born between 38 and 39 gestational weeks (95% CI: 0.74 to 2.25) and 0.5% (5 people) in neonates born after 39 gestational weeks (95% CI: 0.05–0.08). The adjusted odds ratio of the association between TTN and time of delivery was 2.91 (95%CI: 1.09–7.76) (P = 0.032) using multiple logistic regression analysis, indicating that the minimal risk of TTN in neonates born between 38 and 39 gestational weeks was 9% higher compared to neonates born after 39 gestational weeks. Table 2 shows crude and adjusted odds ratio of the association between adverse outcomes and time of delivery.
Table 2 shows crude and adjusted odds ratio of the association between adverse outcomes and time of delivery.
Full size table
Discussion
This study showed that elective CS delivery between 38 to 39 gestational weeks is associated with a higher rate of TTN and NICU admission in comparison with elective CS performed after 39 completed gestational weeks. Other major complications and more serious disorders such as respiratory distress syndrome (RDS) and sepsis were not significantly different between the two groups.
Matsuo et al. reported severe neonatal respiratory complications (RDS and TTN) that were similar in 415 Japanese pregnant women who underwent scheduled cesarean delivery in 38 and 39 gestational weeks [6]. In a study of 442,596 South Asian and Black women, Balchin et al. found that the rate of respiratory dysfunction was the lowest in white infants whose mothers underwent C-section after 39 gestational weeks and in South Asian infants whose mothers underwent C-section at 38 gestational weeks [7].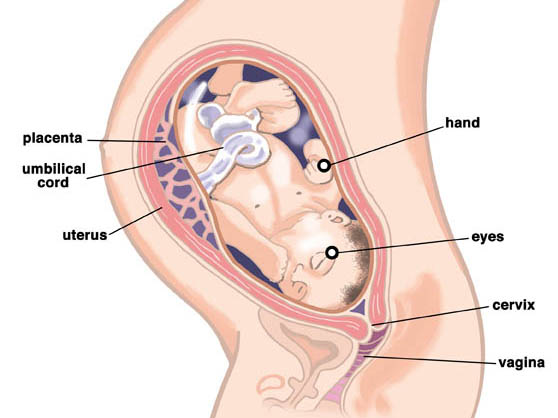 Moreover, Trata et al. examined 1951 cases of elective cesarean delivery in Japan and reported that elective cesarean should be performed at 38 weeks and two days or later in order to avoid respiratory complications [8].
Moreover, Trata et al. examined 1951 cases of elective cesarean delivery in Japan and reported that elective cesarean should be performed at 38 weeks and two days or later in order to avoid respiratory complications [8].
A retrospective study of 1221 singleton pregnant women in Taiwan and Southeast Asia with scheduled cesarean delivery at 38 gestational weeks compared to 39 weeks revealed no statistically significant difference in severe neonatal complications including TTNB, RDS and NICU admission [1]. In contrast, the rate of NICU admission was higher in our study at 38 gestational weeksthan 39 gestational weeks. This difference may be attributed to differences in the hospital strategy to admit infants to NICU or high frequency of TTN.
Furthermore, most studies on Caucasian and mainly white women have emphasized the improved neonatal outcome in scheduled cesarean deliveries at 39 gestational weeks [9, 10]. It has been suggested that difference in the prevalence of respiratory dysfunction at different gestational ages in white and Asian infants can be due to genetic differences when the fetus matures in the uterine [7, 11]. Black and Asian infants have mostly shown meconium-stained amniotic fluid, indicating prematurity [11].
Black and Asian infants have mostly shown meconium-stained amniotic fluid, indicating prematurity [11].
On the other hand, a multicentre clinical trial in Denmark showed that NICU admission was higher in scheduled cesarean delivery at 38 gestational weeks than those born at 39 gestational weeks,even though the difference was not significant [5]. It can be concluded that race alone cannot determine neonatal complications at different pregnancy ages. The difference of these studies conducted in the Caucasian and Asian communities in terms of the gestational age at the time of scheduled cesarean delivery can be due to differences in the sample size, failure to control confounding variables, or race.
In this study, the main reason for NICU admission was TTN, not other serious complications including RDS and sepsis. NICU admissions may lead to a large financial burden. Christopher J. Robinson et al. reported that waiting until 39 gestational weeks to perform an elective CS is cost effective [12]. However, the likelihood of emergency cesarean delivery and its maternal complications should also be taken into account. As suggested by some studies, the mean gestational age in Asian and black populations is less than the whites, which can be due to fetal prematurity [11]. Emergency cesarean can be followed by complications for mothers and infants [13]. Thus, in our study, we cannot draw a definite conclusion that delivery should be performed after 39 gestational weeks. Further studies are required to compare the rate and complications of emergency and scheduled cesarean delivery in Iranian population at 38 and 39 gestational weeks.
However, the likelihood of emergency cesarean delivery and its maternal complications should also be taken into account. As suggested by some studies, the mean gestational age in Asian and black populations is less than the whites, which can be due to fetal prematurity [11]. Emergency cesarean can be followed by complications for mothers and infants [13]. Thus, in our study, we cannot draw a definite conclusion that delivery should be performed after 39 gestational weeks. Further studies are required to compare the rate and complications of emergency and scheduled cesarean delivery in Iranian population at 38 and 39 gestational weeks.
One of the concerns that causes scheduled cesarean delivery at 38 gestational weeks is prevention of unexpected fetal death. In this study, we did not have any cases of stillbirth. The risk of unexplained stillbirth at 38 gestational weeks was reported to be about 0.05 per 1000 births among women with the history of cesarean delivery in a Scottish and a Canadian cohort study [14, 15]. To measure the prevalence of 0.01–1% with sufficient accuracy and confidence, as many as 20,000 cases are needed [16]. Therefore, a small size of the sample may be the reason.
To measure the prevalence of 0.01–1% with sufficient accuracy and confidence, as many as 20,000 cases are needed [16]. Therefore, a small size of the sample may be the reason.
In this study, the most common causes of cesarean delivery in the two groups were a previous history of CS and maternal request. However, the frequency of repeated cesarean delivery was higher at 38–39 gestational weeks than its frequency after 39 gestational weeks. Two-thirds of births were done at 38–39 gestational weeks for this reason. Moreover, 56% of all repeated cesarean deliveries were performed before 39 gestational weeks. A multicentric cohort in the United States showed that one-third of cesarean deliveries are performed before 39 gestational weeks. The rate is between 50 and 80% in some European countries. The reason for this concern is maternal complications in pregnancy associated with previous CS [17]. In this study, other reasons, including maternal request, breech presentation, and CPD, were more prevalent at 39 gestational weeks.
In our study, almost half of elective caesarean sections were performed before 39 gestational weeks. Wilmink et al. reported that more than 50% of the elective cesarean sections were done before 39 gestational weeksin the Netherlands (8.3% at 37 gestational weeks and 48.3% at 38 gestational weeks [10]. Zanardo V. et al. reported that about 60% of elective cesarean sections in their hospital were performed before 38 weeks and 6 days [18] It seems that physicians, regardless of the existing documents, perform a large percentage of CS deliveries before 39 gestational weeks. It may be due to the physician’s opinion or practice patterns, maternal request for early CS, birth certificate data, or any other reason.
The strong points of this study were excluding the cases of emergency cesarean delivery and a large sample size. The limitations of this study were evaluating neonatal complications only up to 28 days after birth not beyond 28 days.
Conclusion
According to our study findings, scheduled CS delivery between 38 and 39 gestational weeks is associated with a higher rate of NICU admission in comparison with scheduled CS performed after 39 gestational weeks. The main reason for NICU admission was TTN, not other serious complications. Although no cases of intrauterine fetal death occurred in women who underwent CS delivery after 39 gestational weeks, we did not have any information on the incidence and complications of emergency CS in those who delivered after 39 weeks’ gestation.Therefore, based on the results of this study, it cannot be concluded that scheduled caesarean section should be performed after 39 gestational weeks. We suggest that the above issue be examined in the future studies to determine the time of scheduled CS more accurately.
The main reason for NICU admission was TTN, not other serious complications. Although no cases of intrauterine fetal death occurred in women who underwent CS delivery after 39 gestational weeks, we did not have any information on the incidence and complications of emergency CS in those who delivered after 39 weeks’ gestation.Therefore, based on the results of this study, it cannot be concluded that scheduled caesarean section should be performed after 39 gestational weeks. We suggest that the above issue be examined in the future studies to determine the time of scheduled CS more accurately.
Abbreviations
- CPD:
-
Cephalopelvic Disproportion
- CRL:
-
Fetal crown-rump-length
- CS:
-
Cesarean sections
- GA:
-
Gestational age
- LMP:
-
The last menstrual period
- OR:
-
Odds ratios
- RDS:
-
Respiratory distress syndrome
- TTN:
-
Transient tachypnea of the newborn
References
Phaloprakarn C, Tangjitgamol S, Manusirivithaya S. Timing of elective cesarean delivery at term and its impact on maternal and neonatal outcomes among Thai and other Southeast Asian pregnant women. J Obstet Gynaecol Res. 2016;42(8):936–43.
Article PubMed Google Scholar
Glavind J, Uldbjerg N. Elective cesarean delivery at 38 and 39 weeks: neonatal and maternal risks. Curr Opin Obstet Gynecol. 2015;27(2):121–7.
Article PubMed Google Scholar
Doan E, Gibbons K, Tudehope D. The timing of elective caesarean deliveries and early neonatal outcomes in singleton infants born 37–41 weeks' gestation. Aust N Z J Obstet Gynaecol. 2014;54(4):340–7.
Article PubMed Google Scholar
Spong CY. Defining “term” pregnancy: recommendations from the defining “term” pregnancy workgroup.
 JAMA. 2013;309(23):2445–6.
JAMA. 2013;309(23):2445–6.Article CAS PubMed Google Scholar
Glavind J, et al. Elective caesarean section at 38 weeks versus 39 weeks: neonatal and maternal outcomes in a randomised controlled trial. BJOG Int J Obstet Gynaecol. 2013;120(9):1123–32.
Article CAS Google Scholar
Matsuo K, et al. Is 38 weeks late enough for elective cesarean delivery? Int J Gynecol Obstet. 2008;100(1):90–1.
Article CAS Google Scholar
Balchin I, et al. Timing of planned cesarean delivery by racial group. Obstet Gynecol. 2008;111(3):659–66.
Article PubMed Google Scholar
Terada K, et al. Timing of Elective Cesarean Singleton Delivery and Neonatal Respiratory Outcomes at a Japanese Perinatal Center.
 Journal of Nippon Medical School. 2014;81(4):285–8.
Journal of Nippon Medical School. 2014;81(4):285–8.Article PubMed Google Scholar
Chiossi G, et al. Timing of delivery and adverse outcomes in term singleton repeat cesarean deliveries. Obstet Gynecol. 2013;121(3):561.
Article PubMed PubMed Central Google Scholar
Wilmink FA, et al. Neonatal outcome following elective cesarean section beyond 37 weeks of gestation: a 7-year retrospective analysis of a national registry. American journal of obstetrics and gynecology. 2010;202(3):250. e1–8.
Article Google Scholar
Patel RR, et al. Does gestation vary by ethnic group? A London-based study of over 122 000 pregnancies with spontaneous onset of labour. Int J Epidemiol. 2004;33(1):107–13.
Article PubMed Google Scholar
Robinson CJ, et al. Timing of elective repeat cesarean delivery at term and neonatal outcomes: a cost analysis. American journal of obstetrics and gynecology. 2010;202(6):632. e1–6.
Article Google Scholar
Daniel S, et al. Comparison of fetal outcomes of emergency and elective caesarean sections in a teaching hospital in Kerala. Academic medical journal of India. 2014;2(1):32–6.
Google Scholar
Smith GC, Pell JP, Bobbie R. Caesarean section and risk of unexplained stillbirth in subsequent pregnancy. Lancet. 2003;362(9398):1779–84.
Article PubMed Google Scholar
Wood S, et al. The risk of unexplained antepartum stillbirth in second pregnancies following caesarean section in the first pregnancy. BJOG Int J Obstet Gynaecol. 2008;115(6):726–31.

Article CAS Google Scholar
Tita AT, et al. Timing of elective repeat cesarean delivery at term and neonatal outcomes. N Engl J Med. 2009;360(2):111–20.
Article CAS PubMed PubMed Central Google Scholar
Tita AT, Lai Y, Landon MB, Spong CY, Leveno KJ, Varner MW, et al. Timing of elective repeat cesarean delivery at term and maternal perioperative outcomes. Obstet Gynecol. 2011;117(2 Pt 1):280–6.
Article PubMed PubMed Central Google Scholar
Zanardo V, et al. Neonatal respiratory morbidity risk and mode of delivery at term: influence of timing of elective caesarean delivery. Acta Paediatr. 2004;93(5):643–7.
Article CAS PubMed Google Scholar
Download references
Acknowledgements
We would like to thank the research development center of Arash women’s hospital for their contributions in the process of preparing this article.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate:
Research protocol of the study was confirmed in ethical research committee of Tehran University of medical sciences. All of pregnant women sign informed consents for participating into the study.
Author information
Authors and Affiliations
Obstetrics and Gynecology Department, Arash Women’s Hospital, Tehran University of Medical Sciences, Tehran, Iran
Reihaneh Pirjani
Research development center, Arash Women’s Hospital, Tehran University of Medical Sciences, Tehran, Iran
Reihaneh Pirjani
School of medicine, Tehran University of Medical Sciences, Tehran, Iran
Motahareh Afrakhteh
Department of Epidemiology and Reproductive Health, Reproductive Epidemiology Research Center, Royan Institute for Reproductive Biomedicine, ACECR, Tehran, Iran
Mahdi Sepidarkish
Department of Pediatrics, Arash women’s Hospital, Tehran University of Medical Sciences, Tehran, Iran
Shahin Nariman
Maternal, Fetal and Neonatal Research Center, Tehran University of Medical Sciences, Tehran, Iran
Mahboobeh Shirazi
Obstetrics and Gynecology Department, Arash Women’s Hospital, Tehran University of Medical Sciences, Tehran, Iran
Ashraf Moini
Department of Endocrinology and Female Infertility, Reproductive Biomedicine Research Center, Royan Institute for Reproductive Biomedicine, ACECR.
 , Tehran, Iran
, Tehran, IranAshraf Moini
Research development center, Arash Women’s Hospital, Tehran University of Medical Sciences, Tehran, Iran
Ladan Hosseini
Authors
- Reihaneh Pirjani
View author publications
You can also search for this author in PubMed Google Scholar
- Motahareh Afrakhteh
View author publications
You can also search for this author in PubMed Google Scholar
- Mahdi Sepidarkish
View author publications
You can also search for this author in PubMed Google Scholar
- Shahin Nariman
View author publications
You can also search for this author in PubMed Google Scholar
- Mahboobeh Shirazi
View author publications
You can also search for this author in PubMed Google Scholar
- Ashraf Moini
View author publications
You can also search for this author in PubMed Google Scholar
- Ladan Hosseini
View author publications
You can also search for this author in PubMed Google Scholar
Contributions
RP designed the study. RP,MA, SHN,AM, LH and MSH contributed in participants selection and data collection and revised the manuscript. RP and LH wrote the manuscript. MS helped in the analysis of the data. All authors read and approved the final manuscript.
RP,MA, SHN,AM, LH and MSH contributed in participants selection and data collection and revised the manuscript. RP and LH wrote the manuscript. MS helped in the analysis of the data. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Ladan Hosseini.
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.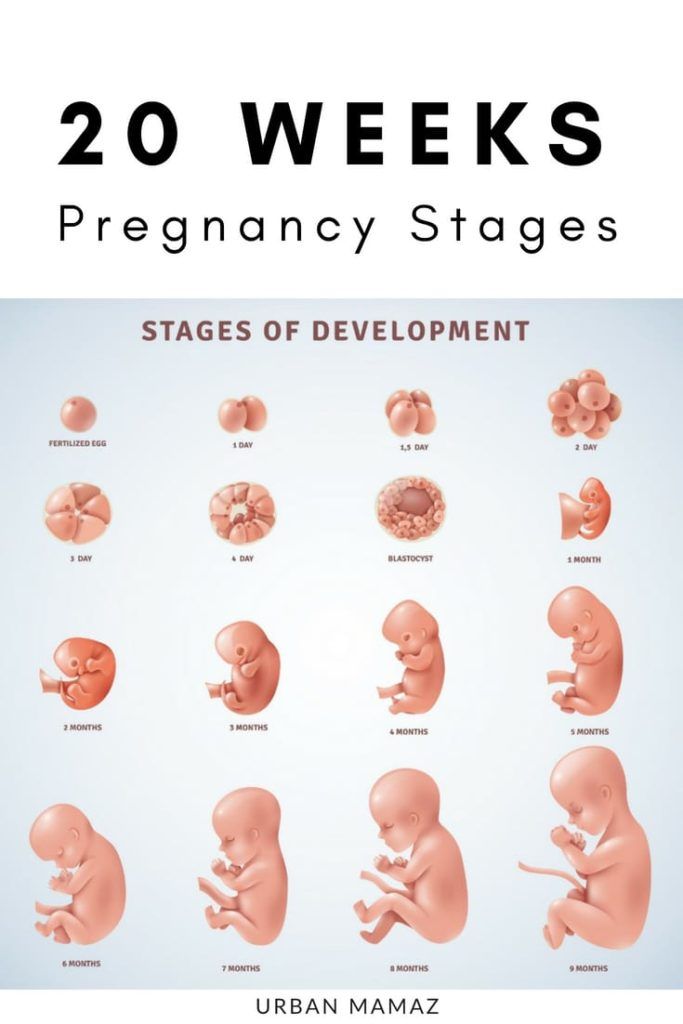 The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
Reprints and Permissions
About this article
Planned caesarean section: what you need to know
On-demand caesarean section? Not necessary. Elective caesarean section is primarily intended to make the operation of maternity hospitals more predictable and reliable, when it can be foreseen that natural childbirth is impossible or complicated.
Share this information
What to expect during a planned caesarean section
Few pregnant women want to think about the process of caesarean section, since most are set for a natural birth. However, the number of caesarean sections in the world increased by 20 percent from 2006 to 2017. One of the reasons for this is the increase in the number of elective caesarean sections, which are performed as a precautionary measure to avoid emergency caesarean sections and complications during childbirth. We answer the most frequently asked questions about "caesarean section at will" and medically necessary birth interventions.
We answer the most frequently asked questions about "caesarean section at will" and medically necessary birth interventions.
If I want to have a caesarean, can I decide whether to have a baby naturally or by caesarean?
First of all: Elective caesarean section is not the same as voluntary caesarean section, which is also a misleading term. Every mother can decide for herself which birth she needs. However, you should discuss the pros and cons of natural birth, vaginal delivery, and caesarean section with your doctor or midwife. nine0003
It is important to remember that there are strong indications for a planned caesarean section. If there is a foreseeable risk to the mother or baby during childbirth, the gynecologist will advise a caesarean section by prior arrangement. For example, if the placenta overlaps the cervix - the so-called placenta praevia - a planned caesarean section will avoid damage to the placenta and life-threatening bleeding.
How is the preparation for a caesarean section carried out?
During your birth planning consultation at the clinic, you will talk to your attending physicians about preparing for a planned caesarean section. Since the consultation is usually done well in advance, there is still a lot that can happen before delivery. If your gynecologist recommends that you have a caesarean section, he or she will make a note in the referral to hospital for a consultation.
This appointment will have ultrasound to reassess the size and weight of the baby , the cervix was examined and CTG was done . If a caesarean section is to be performed due to a transverse or breech presentation, then at the 37th or 38th week of pregnancy, a recheck will likely be performed to see if the position of the baby in the womb has changed. An elective caesarean section does not have to remain an elective one: if a mother decides to have a normal birth after her baby turns in the womb again, the decision can be changed. nine0003
nine0003
How is a planned caesarean section performed?
Together with your doctor, you will decide whether you need general anesthesia or regional (local) anesthesia for your operation. Regional anesthesia for caesarean section has the advantage that after caesarean section you can immediately take the baby in your arms and breastfeed.
Once the anesthesia has worn off, the bladder catheter is inserted and the operation begins. Doctors usually open the abdominal wall using the Misgava-Ladakh method. The top layer of the skin is cut off and the deeper layers of tissue are carefully opened by hand, which ensures a slight loss of blood. The baby is then removed from the uterus, and the wound on the uterus and abdominal tissues is carefully closed. nine0003
When is the right time for a planned caesarean section at what time?
The timing of the caesarean section affects the outcome for the baby, as does the timing of a natural birth. "People are now trying to have caesarean section as close as possible to the estimated due date of , that is, from the end of the 39th week of gestation," explains Prof. MD Dimpfl. At this stage, the development of the child is completed, and he is ready to be born - by caesarean section or by natural means. If there is no medical reason for an earlier delivery, your doctor will advise you to have a planned caesarean section from the beginning of the 40th week. nine0003
MD Dimpfl. At this stage, the development of the child is completed, and he is ready to be born - by caesarean section or by natural means. If there is no medical reason for an earlier delivery, your doctor will advise you to have a planned caesarean section from the beginning of the 40th week. nine0003
indications, how they do it, for how long the planned one is done and how it differs from the emergency
In 2016, I had an emergency caesarean section.
Veronika Vysotina
went through a caesarean section
All five days before the discharge, doctors called me and other women who needed an operation “cesareans”, and our babies were called “cesareans”.
I was not at all ready for the operation: the pregnancy was going well. For almost half a year after the cesarean, I struggled with various thoughts, went through the stages of "I'm not a real mother" and "I'm ashamed in front of the child", I envied my friends who gave birth themselves. Fortunately, now all this is behind us. nine0003
nine0003
In the article I will tell you what a caesarean section is, how it is done and how the recovery goes.
What is a caesarean section
What is it. Caesarean section is also childbirth, only operational. And efficiency here is not about time, but about surgical intervention. Unlike natural childbirth, when a woman gives birth to a child herself through attempts, during a cesarean, the doctor makes an incision in the abdomen with a scalpel and takes the child out of the uterus through it.
Caesarean section - Medscape
Initially, a caesarean section was performed to save the baby if the mother died in childbirth. This operation is mentioned even in Greek and Roman myths - even the name itself came, according to one version, from the Roman law, according to which a pregnant woman could be buried only after the child was taken out of her stomach.
Caesarean section - Britannica
In the 17th century, caesarean sections were performed on living women, but almost always the patient died due to blood loss or infection. mid 19For centuries, doctors came up with the idea of removing the uterus, and a little later they began to put stitches on it, leaving a chance for the next pregnancy.
mid 19For centuries, doctors came up with the idea of removing the uterus, and a little later they began to put stitches on it, leaving a chance for the next pregnancy.
Methodical letter of the Ministry of Health of the Russian Federation on the classification of caesarean sectionPDF, 2.98 MB
Nowadays, caesarean section has become a fairly common situation: in Russia, about every third birth ends like this.
This is a medieval engraving depicting a caesarean section. It is believed that almost the birth of Gaius Julius Caesar is depicted here. But this is a historical myth: Caesar's mother survived after giving birth. Source: The History Blog Which is better: caesarean or natural childbirth. The term "natural birth" is a little outdated: childbirth cannot be artificial. A caesarean section is carried out according to indications from the mother or fetus - often otherwise the woman cannot give birth or there is a risk to the health and even the life of the child.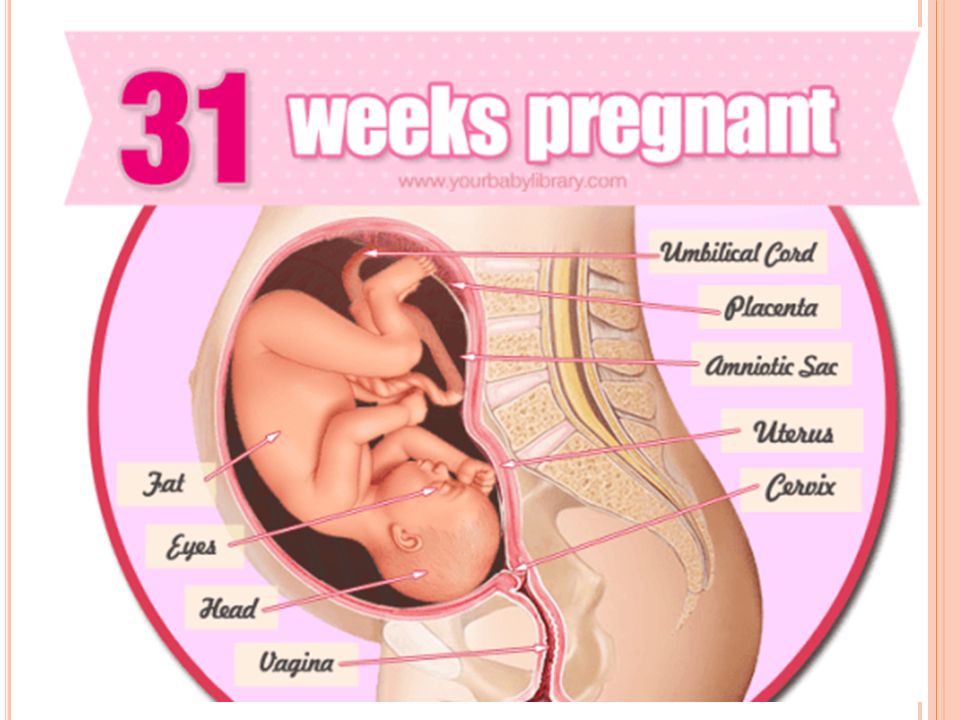
It cannot be said that some way to give birth is definitely better: doctors recommend the method of delivery that will be the safest in a particular situation.
What week is the caesarean section. nine0012 If a caesarean section was planned in advance, then it is usually done starting from the 39th week of pregnancy.
Types of cesarean section
Elective. It is so called because the woman and the doctor know about it in advance, while agreeing on a specific date for the operation.
Caesarean section - NHS
Emergency. This is when the need for operative delivery arises unexpectedly, usually already in the process of childbirth. For example, when a woman suddenly stops labor and this creates a danger to the child, or heavy bleeding begins. nine0003
In addition, there are several types of operations in obstetrics, but in general they can be divided into two large types.
Transverse or horizontal. In this case, the incision is made horizontally across the lower abdomen. Doctors prefer this method if the caesarean section is planned and the patient's life is not in danger. Such an incision takes a little longer, but it is less dangerous in terms of infections. The scar from the horizontal incision is subsequently less noticeable. nine0003
In this case, the incision is made horizontally across the lower abdomen. Doctors prefer this method if the caesarean section is planned and the patient's life is not in danger. Such an incision takes a little longer, but it is less dangerous in terms of infections. The scar from the horizontal incision is subsequently less noticeable. nine0003
Longitudinal or vertical. In this case, a large vertical incision is made almost from the navel to the pelvic bone. This allows you to quickly remove the child in an emergency.
A horizontal incision for caesarean section is better at least cosmetically: it can be hidden under underwearWho is having a caesarean section
Cesarean section can be elective or emergency. Planned is so called because the woman and the doctor know about it in advance, while agreeing on a specific date. nine0003
Clinical guidelines for caesarean section in Russia
There are many reasons for surgery. Here are some of them.
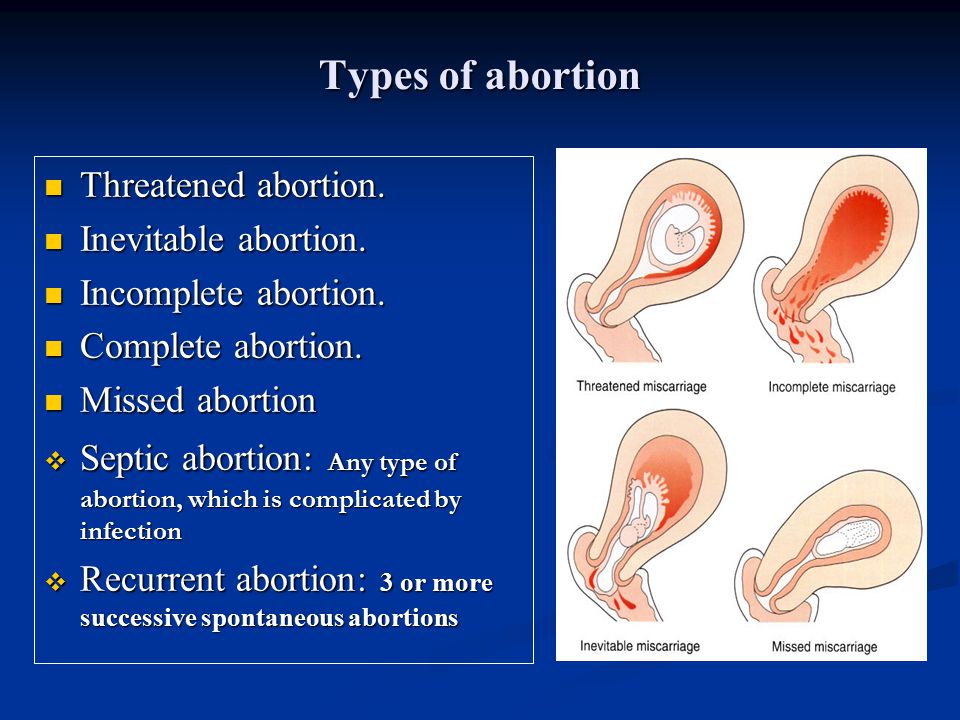
Breech presentation of the child. This is a situation where the fetus in the mother's abdomen lies with its legs or buttocks down and cannot roll over in any way. The Russian clinical guidelines state that a breech presentation of a fetus weighing more than 3600 g is a direct indication for a caesarean section.
Of course, natural childbirth in such cases is possible, but the risks for mother and child are too great, so doctors prefer to do caesarean. There are other incorrect positions of the fetus, which serve as indications for surgery. nine0003
Mother's health problems. These include, for example, cardiovascular disease or spinal problems. In such situations, the period of attempts can become deadly for a woman. Also, an indication for caesarean section may be fibroids, a neoplasm on the cervix or its deformation after plastic surgery - for example, after suturing severe tears during previous births.
Anatomically narrow pelvis. This is a situation where the size of the pelvic bones in a woman is smaller than necessary for normal childbirth. In ordinary life, this does not cause inconvenience, but in childbirth it can become a serious problem: the baby's head will not go through a strong narrowing. That is why, already when registering pregnant women, gynecologists must measure the external dimensions of the pelvis and calculate the internal ones using a special formula. nine0003
This is a situation where the size of the pelvic bones in a woman is smaller than necessary for normal childbirth. In ordinary life, this does not cause inconvenience, but in childbirth it can become a serious problem: the baby's head will not go through a strong narrowing. That is why, already when registering pregnant women, gynecologists must measure the external dimensions of the pelvis and calculate the internal ones using a special formula. nine0003
This also includes other situations that are called “fetal-pelvic disproportions” in the clinical guidelines: for example, deformity of the pelvic bones or a mismatch between the size of the pelvis of the mother and fetus.
/life/kontrakt-beremennost/
How much does pregnancy management cost?
Placenta previa. In some women, the placenta is located in the lower part of the uterus and covers the internal os - in other words, blocks the "exit" for the child.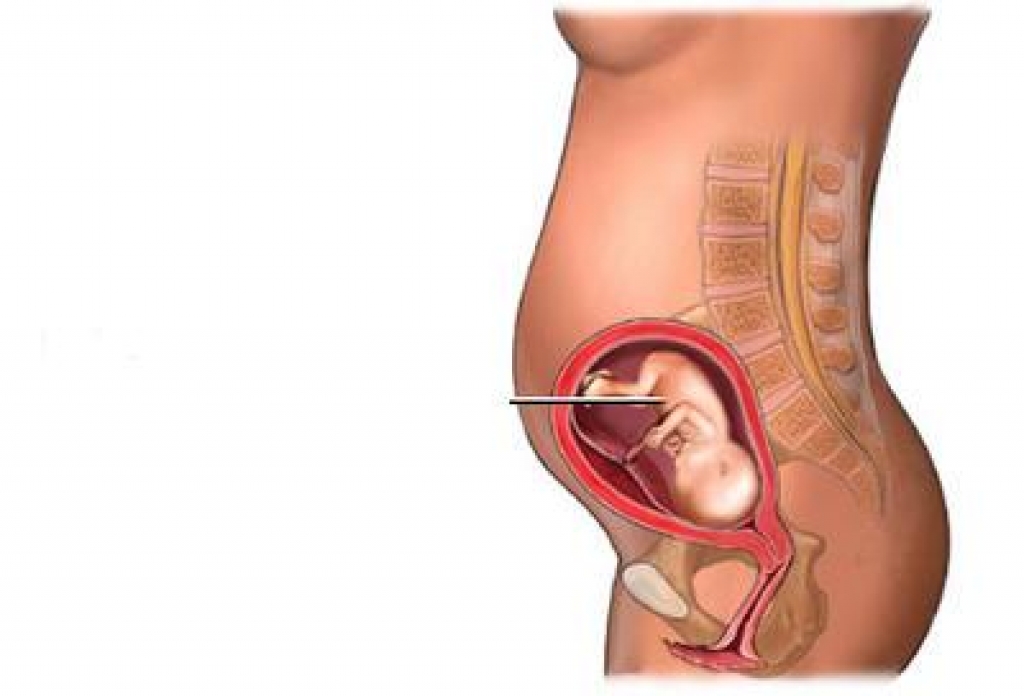 nine0003
nine0003
Previous cesarean. In general, there are quite a lot of situations when, after a caesarean section, a woman gives birth to a child in a natural way. However, this may not always be the case.
With regard to emergency caesarean section, everything that threatens the life of a woman and a child serves as a reason. These are, for example, placental abruption, car and other accidents, lack of oxygen in a child, stopping labor after it begins.
My experience. I had an emergency caesarean section at 41 weeks of pregnancy, at that time I was already a week and a half ahead of the planned date of delivery. The reason for the operation was a clinically narrow pelvis: its dimensions were normal, but the child still could not pass. As the doctor later explained, my son decided to rest his forehead against the bones of the pelvis, while usually children are born with the back of the head forward, while pressing the chin to the chest. nine0003
nine0003
My friend had an emergency c-section at 37 weeks due to eclampsia, a serious complication that often presents with swelling and very high blood pressure, threatening two lives at once. The reasons for this condition are still poorly understood - in Germany, where my friend lives, eclampsia is even called "pregnancy poisoning".
/german-birth/
How much does it cost to give birth in Germany
Can a woman have a caesarean at her request?
Oksana Bogdashevskaya
gynecologist of the Fomina Clinic network
In some countries, for example in the USA, operative delivery can be performed without taking into account medical indications - simply at the request of the woman. The local association of obstetricians and gynecologists asks that decisions be made carefully, but such births account for about 2.5% of all cases of caesarean sections.
As with any operation, risks and complications must be considered. A caesarean section requires a longer hospital stay and has its own risks associated with pain relief, bleeding, thrombosis, bowel or bladder injury. A scar on the uterus complicates the course of the next pregnancy, creating a threat of uterine rupture during pregnancy and childbirth. nine0003
A caesarean section requires a longer hospital stay and has its own risks associated with pain relief, bleeding, thrombosis, bowel or bladder injury. A scar on the uterus complicates the course of the next pregnancy, creating a threat of uterine rupture during pregnancy and childbirth. nine0003
Although vaginal delivery after a previous cesarean is possible, in practice there is a “domino effect”: a cesarean gives rise to a cesarean, and two cesareans lead to a third cesarean. Each time, the risks increase more and more, so "caesarean at will" is not the best option for women who want to have many children.
In Russia, you can't officially have a cesarean just because you want to. The list of indications for it is strictly defined by federal clinical guidelines. nine0003
How to prepare for surgery
Caesarean section, like any other abdominal surgery, is performed on an empty stomach. With a planned caesarean, at least eight hours must pass after eating and two hours after drinking water. In Russia, they still often give an enema to cleanse the intestines, although I found a study that this is not necessary before a planned caesarean.
In Russia, they still often give an enema to cleanse the intestines, although I found a study that this is not necessary before a planned caesarean.
On the eve of the operation, a general blood test is performed, its group, Rh factor and coagulation are assessed. It is imperative to get tested for HIV, syphilis, and hepatitis B. Also the day before, an anesthesiologist comes to the woman's room. He asks the patient in detail about injuries, illnesses, allergies to drugs and more. This information is needed by a specialist in order to choose the safest type of anesthesia. nine0003
/analyz/
You have the right to free analyzes under compulsory health insurance
After the conversation, the doctor signs a voluntary informed consent for medical intervention with the patient. This document does not relieve doctors of responsibility, but only confirms that the patient understood the essence of the procedures - anesthesia and the operation itself - and agrees with them.
In my emergency caesarean situation, there was no preparation at all. When my water broke at ten in the evening, the nurse took blood tests and gave me an enema. During the contractions, the doctor examined him several times and put CTG sensors. Either the problems were not visible, or they were not reported to me, but until seven in the morning I was still preparing for a natural birth. Then the head of the department came, conducted an examination, studied the CTG data and, as a result, announced: “I give the child three hours. If it doesn’t turn around as it should, we will have a Caesarean.” nine0003
How to be healthy and rich
We tell you how to choose a good doctor and not pay for unnecessary tests. Twice a week - in your mail along with other articles about money. Subscribe, it's free
What kind of anesthesia is used for caesarean section
There are two types of anesthesia for caesarean section: general and regional. The doctor is obliged to find out the presence of contraindications to both: if the patient has contraindications to the general one, they make a regional one - and vice versa.
Labor pain relief - Medscape
Anesthesia. At the same time, the patient is asleep and does not know what is happening. And the effect of regional anesthesia extends only to part of the body, that is, the woman is conscious during the operation and can immediately see the child. General anesthesia is usually used in emergencies or when the patient is unconscious. There are almost no contraindications to anesthesia, but recovery from it can be long and difficult, it is often accompanied by nausea, muscle pain and confusion. nine0003
Regional anesthesia. It is divided into two subtypes - epidural and spinal. In both cases, the doctor uses a thin needle to make an injection in the area of the spine. They differ in where exactly the needle goes: into the epidural space or into the cerebrospinal fluid. Epidural anesthesia begins to work within about 20 minutes, spinal anesthetic works faster.
Regional anesthesia has more contraindications than general anesthesia: these include spinal injuries or pressure problems in the mother, oxygen starvation of the fetus. Nevertheless, it is used much more often for cesarean delivery: local anesthesia is safer for the patient and is recommended by numerous protocols around the world. For example, only in the USA at 95% of births use this option.
Nevertheless, it is used much more often for cesarean delivery: local anesthesia is safer for the patient and is recommended by numerous protocols around the world. For example, only in the USA at 95% of births use this option.
/american-girl/
How to go to give birth in the USA
In epidural anesthesia, the doctor leaves a catheter at the injection site through which the anesthetic can be added. Spinal anesthesia is a one-time procedure, its effect cannot be extended. Sometimes doctors combine both optionsCan a woman choose the type of anesthesia herself
Alexander Ronenson
Head of the Department of Anesthesiology and Resuscitation of the Perinatal Center named after E. M. Bakunina
In short, maybe. However, if there are no contraindications, the doctor will first of all recommend spinal anesthesia to the patient - she has the lowest risks of complications.
If a patient, for some personal reasons, refuses spinal anesthesia and chooses general anesthesia, she has every right to do so in accordance with Art. 20 of the Federal Law of the Russian Federation "On the fundamentals of protecting the health of citizens" (No. 323). At the same time, a woman must understand all possible risks and complications, and is also obliged to sign an informed voluntary consent for general anesthesia and refusal of spinal anesthesia. nine0003
20 of the Federal Law of the Russian Federation "On the fundamentals of protecting the health of citizens" (No. 323). At the same time, a woman must understand all possible risks and complications, and is also obliged to sign an informed voluntary consent for general anesthesia and refusal of spinal anesthesia. nine0003
How is a cesarean performed and how long does the operation take?
The operation usually takes about 40 minutes. It involves several obstetrician-gynecologists with assistants, a team of anesthesiologists, a pediatrician or neonatologist - a doctor who assesses the condition of the newborn.
The nurse inserts a urinary catheter, a special bag with a hose that prevents fluid from accumulating in the bladder. A full bladder can interfere with surgeons during surgery, and if accidentally cut, creates a high risk of infection in the abdominal cavity. nine0003
The anesthesiologist performs anesthesia, after which the operating team can start working.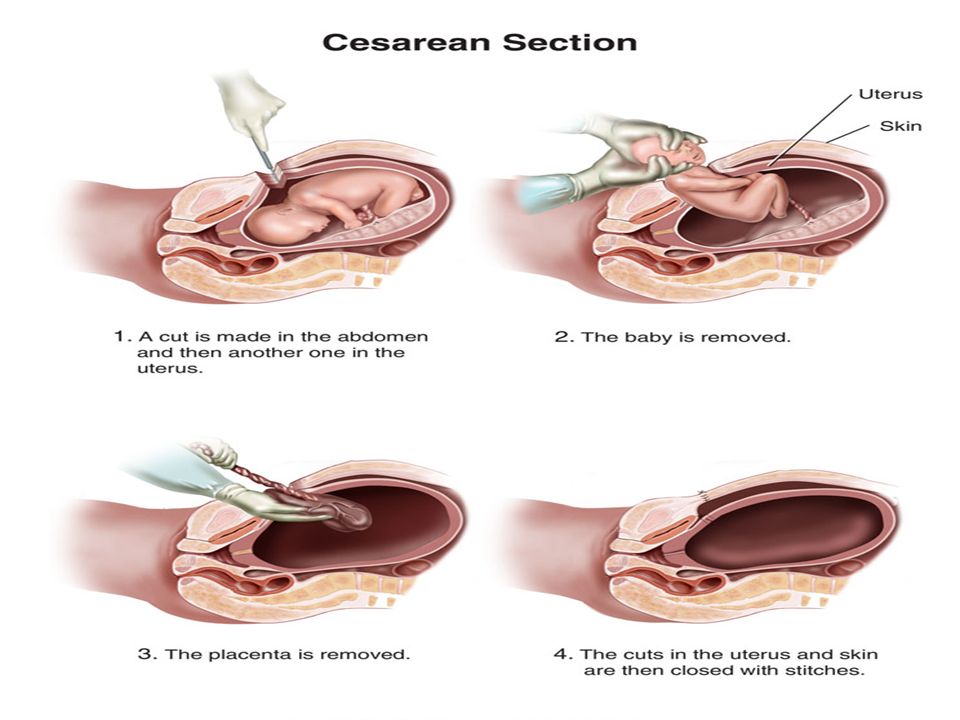 The skin is treated with an antiseptic and the first external incision is made along the abdominal wall.
The skin is treated with an antiseptic and the first external incision is made along the abdominal wall.
Then the skin and all layers of abdominal tissue underneath are pulled apart and an incision is made on the uterus. The child is removed, the umbilical cord is cut off and transferred to a neonatologist for examination.
Surgeons continue their work during this time. If during natural childbirth the placenta is born by itself after a while, then during caesarean delivery it has to be removed by doctors. If even a small piece of the placenta remains inside the uterus, there is a high probability of postpartum hemorrhage and inflammation. nine0003
/platnie-rodi/
How much does it cost to give birth in Moscow
After successful removal of the baby and placenta, the uterus and all subsequent layers up to the skin are sutured in reverse order, using self-absorbable threads or special surgical glue. Sometimes the skin can be held together with metal staples or non-absorbable threads, but then they will have to be removed separately. And some studies say that the use of staples is sometimes fraught with the risk of wound complications. nine0003
And some studies say that the use of staples is sometimes fraught with the risk of wound complications. nine0003
/where-babies-born/
5 Moscow maternity hospitals where it is not scary to give birth to a child
Sometimes a woman is only shown a baby, sometimes she is allowed to hold or attach to her breast right away in the operating room: it all depends on the internal rules of a particular maternity hospital.
Is a caesarean section safe for a child? For example, premature babies are removed from the uterus in the whole fetal bladder - this is a very complex and delicate procedure. nine0003
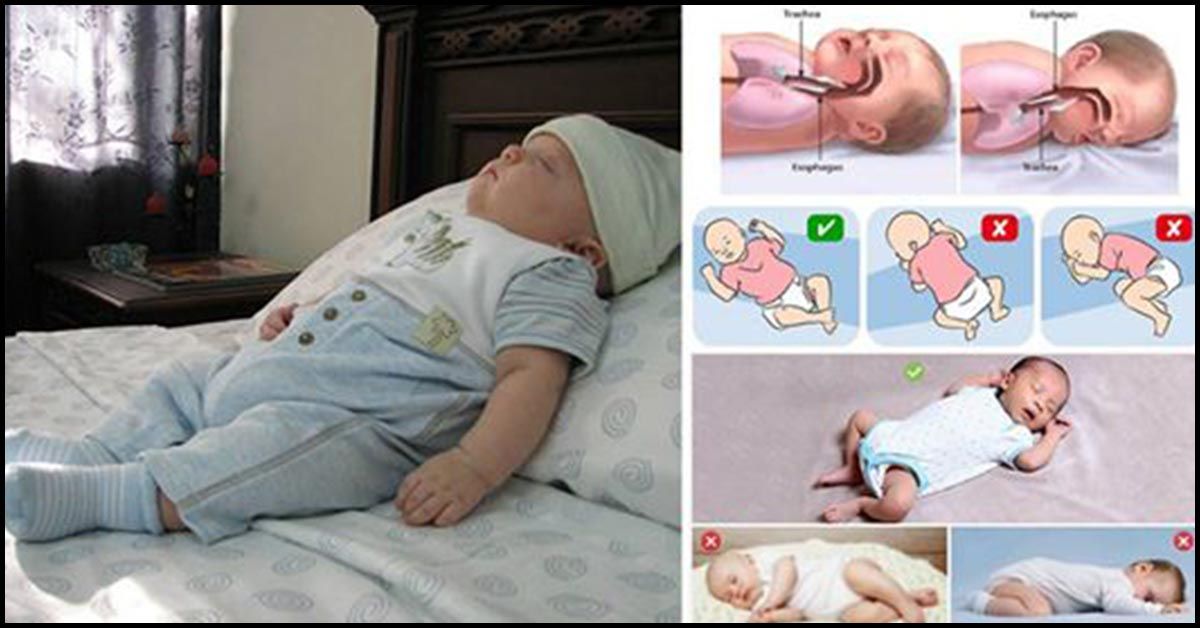
In other cases, it is important for the baby to go through birth stress: this increases his adaptive abilities. That is why it is now recommended to carry out planned operations only after the onset of labor activity - in order to allow the baby to "be born".
When passing through the birth canal of the mother, the child's body is colonized with maternal lactoflora. Research is even being carried out now: is it worth lubricating newborns born by caesarean section with the mother's vaginal secretions, how adequate this imitation is. nine0003
Research is even being carried out now: is it worth lubricating newborns born by caesarean section with the mother's vaginal secretions, how adequate this imitation is. nine0003
Are children born after caesarean different from those born vaginally? There is an opinion that the heads of children who were born in different ways are different. It's not exactly like that. In newborns born naturally, at first a really characteristic shape of the head is called a birth tumor. However, these changes pass quickly, and in the future, the heads of babies do not differ.
How I had a caesarean section
I had an emergency caesarean section, they didn't warn me about it in advance. Although even so, the preparation stage turned out to be the same as during a planned operation. Blood tests, ultrasound and CTG were standard. Dinner the day before was at 5:00 pm, then around 9:00 pm I drank a cup of tea with a small cookie — by the time of the operation I had not eaten anything for 13 hours. nine0003
nine0003
The anesthetist, who came to see me on the day of delivery, quickly interviewed me and said that the anesthesia would be spinal. He immediately gave me some paper to sign - apparently, consent to the operation and anesthesia. I honestly don’t remember what happened there: after ten hours of contractions, it seemed to me that I was ready to sign a donation for an apartment, if only all this would end soon.
In the operating room, I had to completely undress and climb onto the table. The anesthesiologist ordered me to lie on my side and drew something on my spine - apparently, he marked the place of the future injection. I did not feel the injection itself, there was only a slight tingling sensation. nine0003
Then I was allowed to lie on my back, and my hands were fixed on special stands on the left and right. The anesthetist connected a pulse oximeter to my finger, put a blood pressure cuff on my arm, and put oxygen tubes in my nose to make it easier for me to breathe. The nurse inserted a urinary catheter into the urethra.
The nurse inserted a urinary catheter into the urethra.
I was very scared, most of all I did not want to watch how the operation would go. She closed her eyes and immediately received a scolding from the anesthesiologist: "I must see your condition." At this time, the nurse put a curtain in the chest area - just so that I could not see anything. nine0003
The legs became very warm - the anesthesiologist said that the anesthesia had begun to take effect, and gave the command to the surgeons that "we are ready." Now, when I am writing this article, I read that they can check the readiness with a piece of ice or with clamps that lightly pinch the skin.
During the operation, for some reason I really wanted to talk-talk-talk. It seems that I told the anesthesiologist my entire biography. The doctor at that time looked at the values of the devices and told me about the actions of the surgeons: “Now, now they will get the baby. Now scream. You have a boy!" nine0003
Now I don't remember the baby's first cry.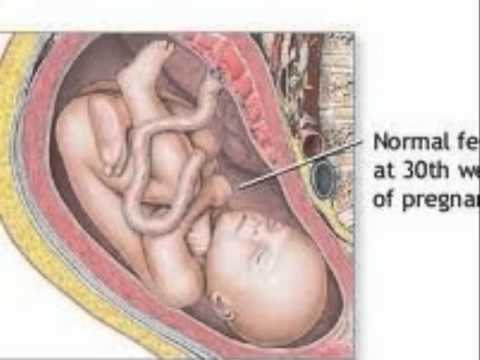 But I clearly remembered him outwardly: they carried my son past - for some reason, his skin was blue-violet. Later, the baby was washed, shown to me and given a kiss on the forehead. They didn’t offer to put it on the chest, and then I didn’t know that it was possible at all.
But I clearly remembered him outwardly: they carried my son past - for some reason, his skin was blue-violet. Later, the baby was washed, shown to me and given a kiss on the forehead. They didn’t offer to put it on the chest, and then I didn’t know that it was possible at all.
How was the day in the intensive care unit
Immediately after the operation, I was taken to the intensive care unit. My son was taken to the neonatal unit - I already found out a few hours later, when a neonatologist came to me and asked for consent to vaccinations.
I remember that my head was very foggy: apparently, fatigue from ten-hour contractions and the effect of anesthesia had an effect. I did not ask where my child was and where they took him. It was important for me to know only one thing: did I forget my slippers in the antenatal ward. Now it seems funny and scary at the same time. nine0003
It was important for me to know only one thing: did I forget my slippers in the antenatal ward. Now it seems funny and scary at the same time. nine0003
/life/sumka-v-roddom/
How much does it cost to pack a bag for the maternity hospital? I didn't argue. Or did not have time - fell asleep.
Waking up in intensive care, I took this photo and sent it to my husband with the caption: “No stomach! I lie down and see my feet!”What can I eat after a caesarean section
When I woke up after the operation, I realized that I was terribly hungry, but the doctor did not allow me to. You could only drink low-fat chicken broth with white meat, and even then only a few sips. My husband unknowingly gave me a two-liter jar filled to the neck. The nurse then laughed: “Is this what they brought for the whole resuscitation, or what?” nine0003
I also had to drink a lot of water, probably to make up for the loss of blood. My relatives also gave me water. The doctor advised me to buy bottles of 0.25 liters: it is difficult and uncomfortable to drink lying down from a "one and a half" bottle. The resuscitation nurse approached each patient in the ward once every 40 minutes and reminded them to drink. At the end of the day, she wrote down in a notebook the amount of alcohol she drank and how full the urinal bag was.
The doctor advised me to buy bottles of 0.25 liters: it is difficult and uncomfortable to drink lying down from a "one and a half" bottle. The resuscitation nurse approached each patient in the ward once every 40 minutes and reminded them to drink. At the end of the day, she wrote down in a notebook the amount of alcohol she drank and how full the urinal bag was.
Later doctors allow solid food. It is important to eat so that there is no constipation, in particular, eat vegetables and drink plenty of water. nine0003
How was the recovery
On the first day after the operation, the lights out was announced at about ten in the evening. I clearly remembered that the thought then flashed through my head: “This is my last good night for the coming year. You need to sleep." The next morning, I was already transferred to the postpartum ward. I felt great, I was ready to jump around the ward.
I spent five days in the maternity hospital after the caesarean: I was operated on on Friday and discharged on Tuesday. Starting on Saturday, they gave injections of oxytocin, a hormone that helps the uterus contract and at the same time stimulates milk production. The injections were very painful - the buttock then hurt for another three weeks. nine0003
Starting on Saturday, they gave injections of oxytocin, a hormone that helps the uterus contract and at the same time stimulates milk production. The injections were very painful - the buttock then hurt for another three weeks. nine0003
Back in the maternity hospital, I had a dressing done once. In the operating room, of course, they put a bandage on the wound, but after all, the caesarean was an emergency, so I didn’t have good postoperative plasters. The bandage was a gauze soaked in something pink. It was not very pleasant to remove such a seam: the fabric stuck to the seam.
I had all the sutures made with self-absorbable threads, they did not need to be removed. On the day of discharge, only an ultrasound was done to make sure everything was healing well and not bleeding. nine0003
How to recover quickly after caesarean section
Suture after caesarean section. As a rule, a bandage is applied to the suture after a caesarean section for 24-48 hours. After its removal, the wound is treated. If the sutures need to be removed, this is usually done on the sixth, seventh or eighth day after the operation.
After its removal, the wound is treated. If the sutures need to be removed, this is usually done on the sixth, seventh or eighth day after the operation.
C-section Recovery - NHS
How and with what to treat a stitch. It is enough to gently clean and dry the wound every day, and also monitor the appearance of signs of infection - this is redness, swelling, increased soreness, a feeling of heat in the suture area, a change in the color of the discharge. The maternity hospital will give recommendations on the treatment of seams, which should be followed at home. nine0003
C-section recovery - Mayo Clinic
How long does the uterus and suture heal after caesarean. Recovery after surgery takes four to six weeks. A scar gradually forms on the skin: at first it will be bright and noticeable, but after a few months it will brighten and will not stand out so much.
How much does the uterus shrink after cesarean. Uterine contractions may be felt during the first few days after surgery. They remind menstrual cramps. nine0003
They remind menstrual cramps. nine0003
These contractions may be uncomfortable, but they help prevent excessive bleeding by constricting the blood vessels in the uterus. An over-the-counter pain reliever, such as ibuprofen, can be taken to relieve pain.
Exercise after caesarean section. After the operation, you should start moving as soon as possible, but the physical activity should be moderate. Any exercises can be done only after the permission of the doctor.
They can usually be started three to four weeks after the caesarean if everything went without complications. It is important not to do exercises that lead to abdominal tension: abdominal exercises, squats, straight leg raises from a prone position, and others. nine0003
Massage after caesarean section. Body massage can be done after complete healing of postoperative sutures. Massage of the hands and feet is allowed, and there is evidence that it can alleviate the discomfort associated with the operation.
Period after caesarean section. The operation does not affect the restoration of the menstrual cycle after pregnancy. When breastfeeding, menstruation will return after it stops or when the woman becomes less likely to put the baby to the breast. If a woman is not breastfeeding, then her periods will return on average two months after the birth of the baby. nine0003
Bandage is an elastic bandage that is worn over the waistband to support fabrics. It is believed that the bandage helps to relieve pain after surgery, especially during movement. There is evidence to support this, although other studies show that wearing a brace has little effect on discomfort.
How to wear a bandage after a caesarean section. The bandage should fit snugly enough to the body, but not squeeze. It needs to be fastened so that support is felt, but the bandage does not interfere with breathing and does not cause discomfort. nine0003
Before using the bandage, you should consult your doctor. Also, it should not be worn if there are signs of infection or inflammation in the suture area.
Also, it should not be worn if there are signs of infection or inflammation in the suture area.
How long to wear a bandage after a caesarean section. It should not be worn all the time without taking it off. The brace is usually worn four to eight hours a day. You can’t sleep in it, as it is uncomfortable, it can make breathing and blood circulation difficult.
Wear a brace, as a rule, from six to twelve weeks after childbirth - after this time the body will recover sufficiently. nine0003 Postpartum bandage costs an average of 1000 R. Sometimes it helps to relieve pain after surgery. Source: Yandex Market
What are the restrictions on sexual life and subsequent pregnancy
Oksana Bogdashevskaya
gynecologist of the Fomina Clinic network
If everything went well, discharge from the hospital after cesarean occurs already on the fourth or fifth day. The first postpartum visit to the antenatal clinic should be planned within two weeks after discharge. nine0003
nine0003
Sex after cesarean. Sexual activity can be resumed four to six weeks after the operation, but it is better to see a doctor again before that and discuss contraceptive issues.
If you are planning a new pregnancy, then do not forget about the safe interval. The optimal interval between births should be about two and a half years - different protocols give slightly different numbers. However, these data are similar to recommendations for natural childbirth.
If less than six months have elapsed from delivery by caesarean to a new conception, then the next pregnancy is at risk of uterine rupture. If less than 12 months, there are high chances of placenta previa and abruption. nine0003
When can I exercise after a caesarean section
For at least four weeks after surgery, you should avoid exercises that directly affect the abs, and during the recovery period, you should not lift weights, run, do weight training. The load should only be light.
Sports activities are usually not possible until eight weeks after surgery. From that point on, it is usually safe to return to swimming, Pilates, yoga, light jogging, and low-resistance gym activities. nine0003
Aerobics, running, strength training are usually possible 12 weeks after surgery. In any case, you should consult a doctor before resuming sports.
When does milk come after caesarean and is it possible to breastfeed
After caesarean section, you can immediately breastfeed, just like after a normal birth. Sometimes breastfeeding takes longer after surgery. For example, milk production may start a little slower. nine0003
Breastfeeding after caesarean section - Australian Breastfeeding Association
Babies born by caesarean section may not breastfeed as actively. This can be solved by trying to feed the baby more often.
Complications after caesarean
Although caesarean has become commonplace, it is wrong to think that this is just an “easy way to give birth”. This is a real abdominal operation, which is much more dangerous than natural childbirth.
This is a real abdominal operation, which is much more dangerous than natural childbirth.
It happens that after a caesarean section, a woman develops complications. One of them is endomyometritis, an inflammation of the lining of the uterus.
Women after cesarean have a high risk of leg thrombosis. This is due to the fact that anesthesia weakens and expands the vascular walls, the blood flow slows down. That is why doctors recommend wearing special compression stockings for a planned caesarean, they maintain the desired level of blood flow.
Sometimes, after a caesarean, women have problems with the onset of lactation - this is due to the fact that hormones in such a situation begin to work a little differently than during natural childbirth. Fortunately, I didn’t have such a problem: the milk came already on the third day. nine0003
Babies delivered by cesarean may have slightly different gut microflora. When a child is born naturally, he receives some of the microorganisms from the mother's birth canal. This does not happen with a caesarean, so these babies may develop colic earlier.
This does not happen with a caesarean, so these babies may develop colic earlier.
/colic/
How to help a newborn with colic
Even after a normal birth, a woman is not recommended to lift weights of more than five to six kilograms for the first few months - the approximate weight of a baby in winter overalls. In the postpartum period, this can lead to bleeding, and in the case of a caesarean, even to rupture of the sutures. nine0003
A month and a half after giving birth, I noticed that three red pustules appeared near the suture. Wildly frightened, I made an appointment with the first gynecologist I came across. Ultrasound of the soft tissues showed that everything was in order with the suture, and later small pieces of threads came out of the pustules, which had not yet had time to resolve. The doctor said that this sometimes happens and you should not be afraid - the seam will not open. And so it happened, everything quickly healed.
But I had enough worries. The fact is that during the operation, my son accidentally made a large cut a centimeter from his eye and another one on his head. Fortunately, they healed within a month and a half and are now completely invisible. nine0003 I'm afraid to imagine what would happen if the cut was closer to the eye
Psychological pressure and depression after caesarean
Somehow I came across a comparison of women who gave birth by caesarean with those who leave children in maternity hospitals. Some people stigmatize such mothers as “not a real mother” and reproach them: “I couldn’t even give birth, how are you going to educate?”
"No, it's okay: don't feel guilty about a caesarean birth" - NEN
Such words, to put it mildly, do not add self-confidence. Some women are already feeling ashamed that they allegedly "lost control" and that they "got the child already ready." nine0003
Not far from postpartum depression. Here are its main signs: depression, lack of interest in the child or too strong feelings for him, inability and unwillingness to enjoy life, tearfulness, impaired appetite. Postpartum depression is extremely dangerous and should not be ignored, especially if the symptoms recur regularly.
Postpartum depression is extremely dangerous and should not be ignored, especially if the symptoms recur regularly.
Postpartum Depression - Medscape
If you notice these signs in yourself or a woman you know who has recently given birth, it is important to see a psychologist or psychotherapist. The specialist will do tests to determine the level of depression, possibly send them for tests, and in emergency cases even offer medical treatment in a hospital setting. Alas, there are stories on the Internet about the suicide of women who have recently given birth. nine0003
/psychotherapy-search/
How to choose a psychotherapist
Fortunately, I was able to cope with my feelings on my own, even though they came to me periodically for six months. The switch was the idea that the birth went well and that it is not clear how the situation would have developed if the doctors had not performed a caesarean. My son got an Apgar score of 8/8, which is a good and high number.
Apgar score - Medscape
How to get sick leave after cesarean
Caesarean section is considered a complication of childbirth. Because of it, maternity leave is extended by two weeks. At the same time, an additional code 020 is put on the sick leave.
I was issued a sick leave at the maternity hospital before discharge. It indicated this additional code and a new deadline for starting work. On the new sick leave they wrote that it was a continuation of the previous one.
This is my first sick leave. Code 05 is simply written here - maternity leave. Theoretically, I was supposed to go to work on September 13. This sick leave was issued at the maternity hospital. They wrote the number of the first sheet in the header, put an additional code 020. Now I had to go to work on 29September The statement for the newborn also indicated about the caesarean sectionHow much does a caesarean section cost
I didn’t pay anything for a caesarean section. This operation is included in the list of those that are performed under compulsory health insurance. However, if a woman enters into a paid contract for childbirth, surgery is paid separately, such programs are more expensive. Here are some examples.
This operation is included in the list of those that are performed under compulsory health insurance. However, if a woman enters into a paid contract for childbirth, surgery is paid separately, such programs are more expensive. Here are some examples.
How much does a contract for operative delivery cost in different clinics
| Clinic | Contract price for operative delivery |
|---|---|
| Mother and Child | From 222 000 R |
| Maternity hospital No. 25 | 135 000 Р |
| Maternity hospital No. 8 | Complicated childbirth program — 120,000 R |
| Center. V. I. Kulakova | From 85 000 R |
| Regional Clinical Perinatal Center. E. M. Bakunin | From 27 600 R |
"Mother and Child"
From 222 000 R
Maternity hospital No. 25
135,000 R
Maternity hospital No.