Signs of kidney infection when pregnant
Pyelonephritis: kidney infection in pregnancy | Pregnancy, Worries and discomforts articles & support
It can cause premature births and hospitalisation during pregnancy so it’s definitely worth knowing about a type of urinary tract infection called pyelonephritis
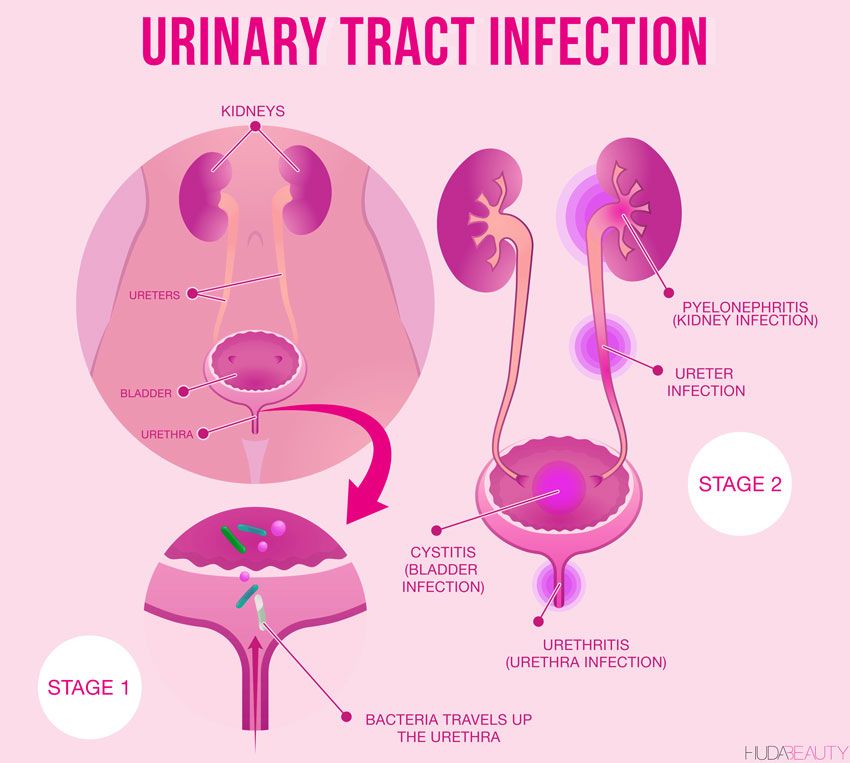
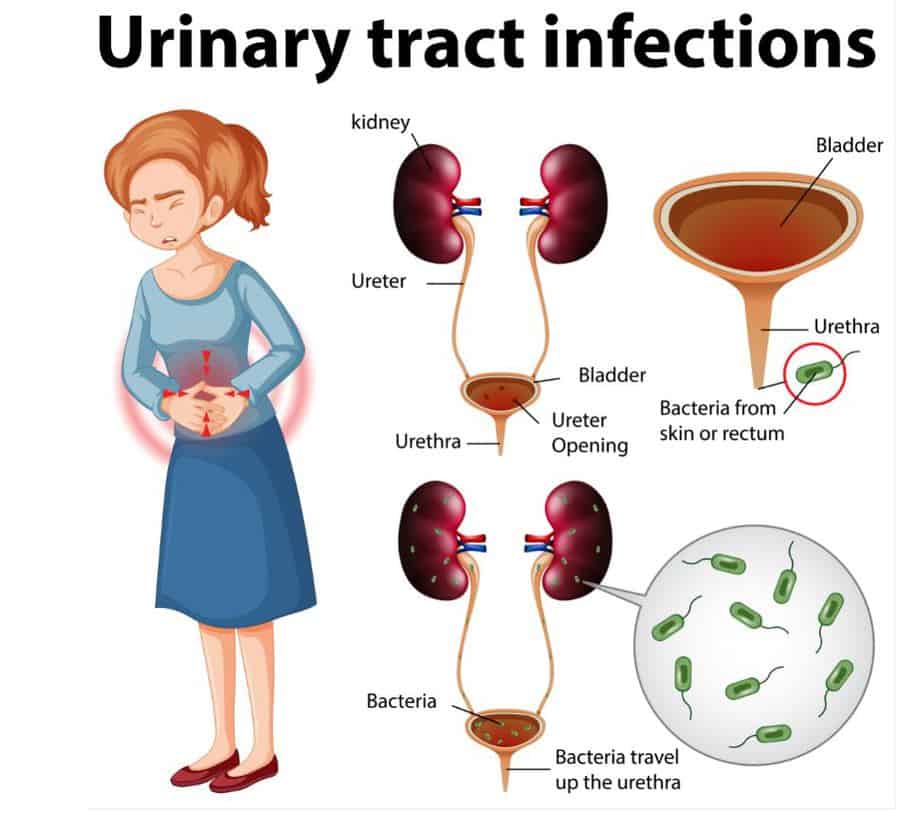
Urinary tract infections (UTIs) are more common during pregnancy. This is mostly because there are a whole load of changes going on around there at this time.
Pyelonephritis is one of the most serious types of UTIs and one of the ones most likely to get you admitted to hospital. As well as affecting the upper urinary tract, pyelonephritis affects the kidneys (Goumi et al, 2015).
Pyelonephritis usually happens if you’ve had cystitis (a lower urinary tract infection) and the bacteria then travels up into the kidneys (Goumi et al, 2015; NHS Choices, 2018).
Pyelonephritis symptoms
Symptoms of pyelonephritis usually start within a few hours (NHS Choices, 2018). Some of the symptoms in pregnancy are:
- fever
- pain and discomfort on back or side
- nausea
- vomiting
- pain in your side
- painful, frequent or an urgent need to wee.
(Goumi et al, 2015; NHS Choices, 2018).
Pyelonephritis causes
E.coli bacteria is the usual cause of pyelonephritis. This bacteria causes pyelonephritis by travelling up to the bladder, causing cystitis, then continuing up into the kidneys. Both of which are the last things you need when you’re pregnant.
E. coli normally live in the bowel where they cause no harm. But they can be transferred into the vagina during sex or when you wipe after you go to the toilet (NHS Choices, 2018). And that’s when you have a problem.
Pyelonephritis is more common in women as their urethras are shorter, so it’s easier for bacteria to reach the kidneys. It’s also more likely in younger women who are sexually active as frequent sex increases the chances of a kidney infection (NHS Choices, 2018).
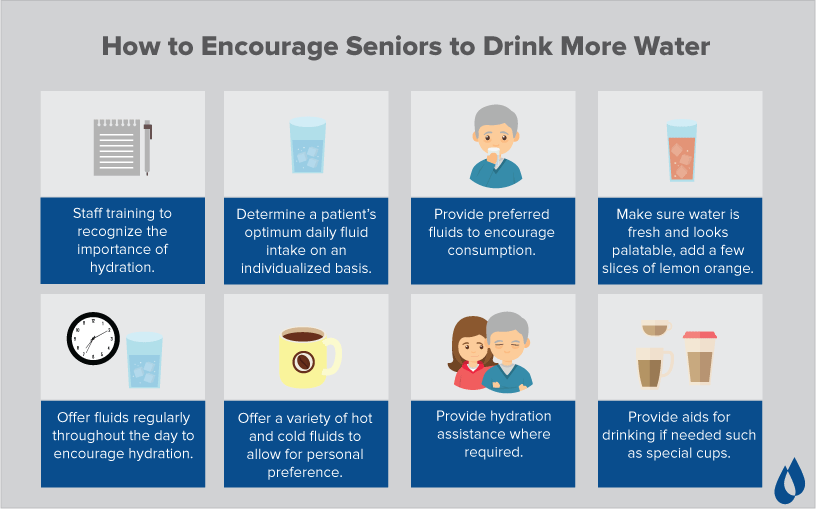
The best way to avoid pyelonephritis is to:
- drink plenty of fluids
- go to the loo as soon as you need it
- go to the loo after sex
- wipe from front to back after going to the loo
- wash down below every day, and if possible before having sex
- treat any constipation as this can increase your risk of pyelonephritis.
(NHS Choices, 2018)
When to see your GP
Pregnancy isn’t a time to be taking health risks so see your GP if:
- you feel feverish
- you have pain in your back, tummy or down below that won’t go away
- your symptoms haven’t improved after a few days
- you have blood in your wee.
(NHS Choices, 2018).
Pyelonephritis diagnosis
When they’re diagnosing pyelonephritis, your GP will ask:
- if you have had a kidney infection before
- what symptoms you’ve been having
- for a urine sample.
(NHS Choices, 2018)
Will this UTI affect my baby?
If you have pyelonephritis in pregnancy, you are more likely to have your baby prematurely or to have a low birthweight baby (Goumi et al, 2015).
You’re also more likely to have complications in your kidneys (NICE, 2013). The risks are higher if you don’t have any symptoms (Goumi et al, 2015).
Pyelonephritis treatment and antibiotics in pregnancy
Pyelonephritis needs quick treatment with antibiotics to stop it from damaging the kidney or spreading to the bloodstream (NHS Choices, 2018).
If you’re pregnant and have pyelonephritis, you’ll more than likely be admitted to hospital so doctors can take regular urine and blood samples. Your doctor can speak to you about which antibiotics are safe in pregnancy and you’ll probably be given them intravenously (NICE, 2013).
This page was last reviewed in February 2018.Further information
Our support line offers practical and emotional support with feeding your baby and general enquiries for parents, members and volunteers: 0300 330 0700. We also offer antenatal courses which are a great way to find out more about birth, labour and life with a new baby.
You might find attending one of our Early Days groups helpful as they give you the opportunity to explore different approaches to important parenting issues with a qualified group leader and other new parents in your area.
Make friends with other parents-to-be and new parents in your local area for support and friendship by seeing what NCT activities are happening nearby.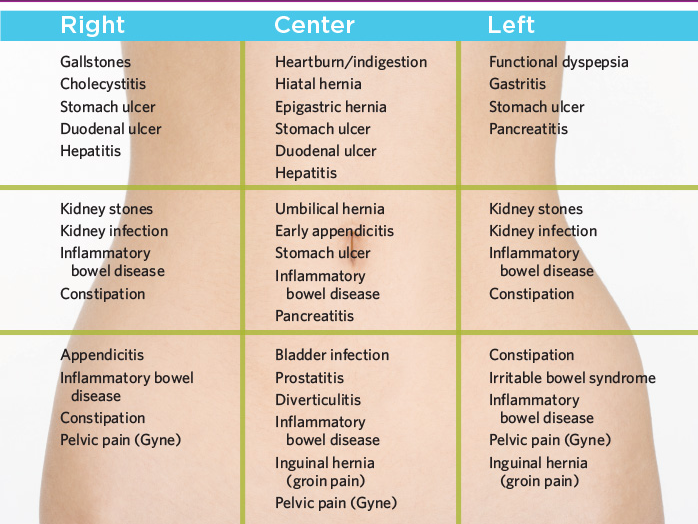
References
Goumi H, Goto Y, Laopaiboon M, Usui R, Mori R. (2015) Routine blood cultures in the management of pyelonepthritis in pregnancy for improving outcomes. Cochrane Database Systematic Review. (2):CD009216 Available from: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD009216.pub2/full [Accessed 1st February 2018]
NHS Choices. (2018) Kidney infection. Available from: https://www.nhs.uk/conditions/kidney-infection/ [Accessed 1st February 2018]
NICE (The National Institute for Health and Care Excellence). (2013) Clinical Knowledge Summaries. Pyelonephritis – acute. Available from: https://cks.nice.org.uk/pyelonephritis-acute#!scenario [Accessed 1st February 2018]
Information you can trust from NCT
When it comes to content, our aim is simple: every parent should have access to information they can trust.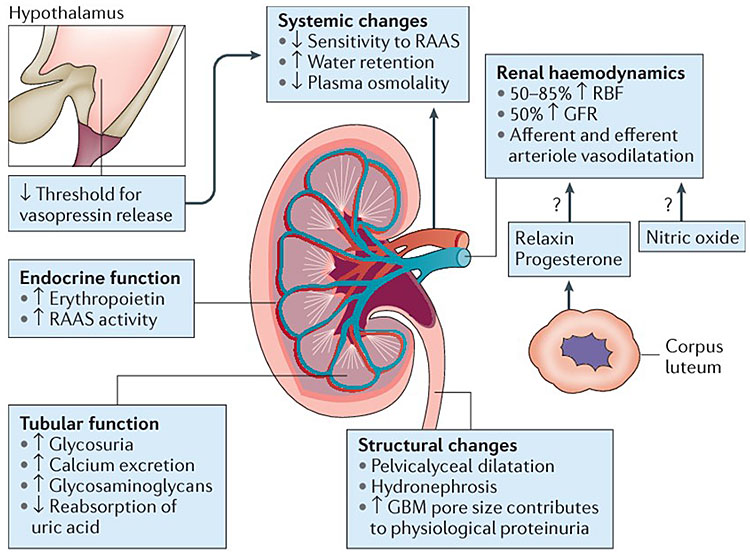
All of our articles have been thoroughly researched and are based on the latest evidence from reputable and robust sources. We create our articles with NCT antenatal teachers, postnatal leaders and breastfeeding counsellors, as well as academics and representatives from relevant organisations and charities.
Read more about our editorial review process.
Infections in Pregnancy: Acute Pyelonephritis
What is acute pyelonephritis?
Acute pyelonephritis is a bacterial infection of the kidneys that affects up to 2 percent of pregnant women. In most cases, the infection first develops in the lower urinary tract. If it’s not diagnosed and treated properly, the infection may spread from the urethra and genital area to the bladder and then to one or both kidneys.
Pregnant women are more likely to develop pyelonephritis than women who aren’t pregnant. This is due to physiological changes during pregnancy that can interfere with the flow of urine.
Normally, the ureters drain urine from the kidney into the bladder and out of the body through the urethra.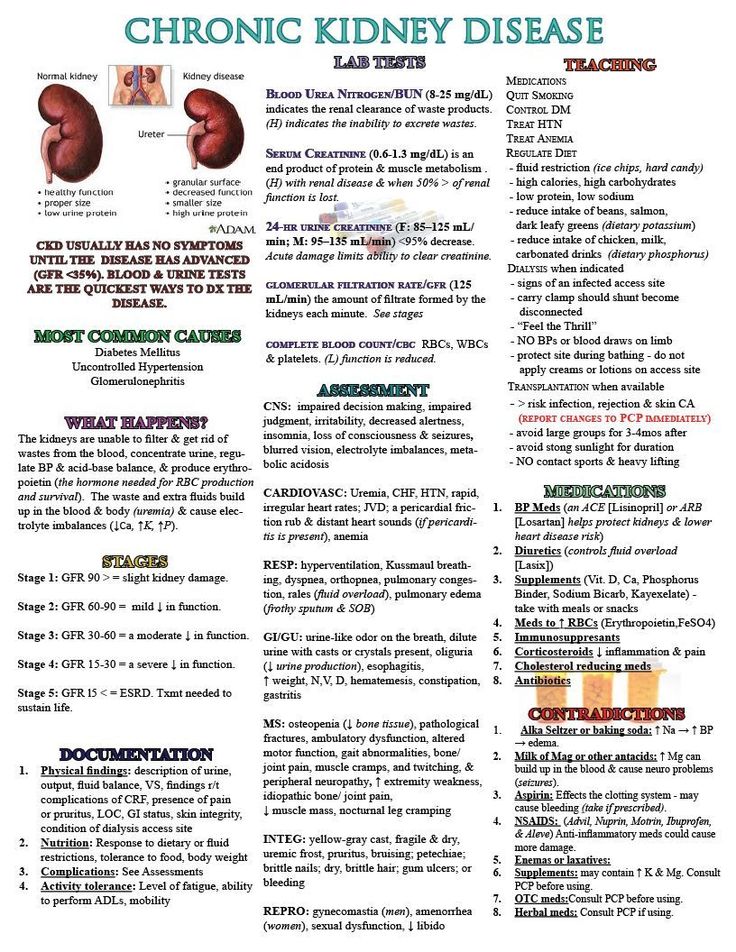 During pregnancy, the high concentration of the hormone progesterone can inhibit contraction of these drainage ducts. Also, as the uterus becomes enlarged during pregnancy, it can compress the ureters.
During pregnancy, the high concentration of the hormone progesterone can inhibit contraction of these drainage ducts. Also, as the uterus becomes enlarged during pregnancy, it can compress the ureters.
These changes can lead to problems with proper drainage of urine from the kidneys, causing the urine to remain stagnant. As a result, bacteria in the bladder may migrate to the kidneys rather than being flushed out of the system. This causes an infection. The bacteria Escherichia coli (E. coli) is the usual cause. Other bacteria, like Klebsiella pneumoniae, the Proteus species, and Staphylococcus, can also cause kidney infections.
What are the symptoms of pyelonephritis?
Typically, the first symptoms of pyelonephritis are a high fever, chills, and pain on both sides of the lower back.
In some cases, this infection causes nausea and vomiting. Urinary symptoms are also common, including:
- urinary frequency, or the need to urinate often
- urinary urgency, or the need to urinate immediately
- dysuria, or painful urination
- hematuria, or blood in the urine
What are the complications of pyelonephritis?
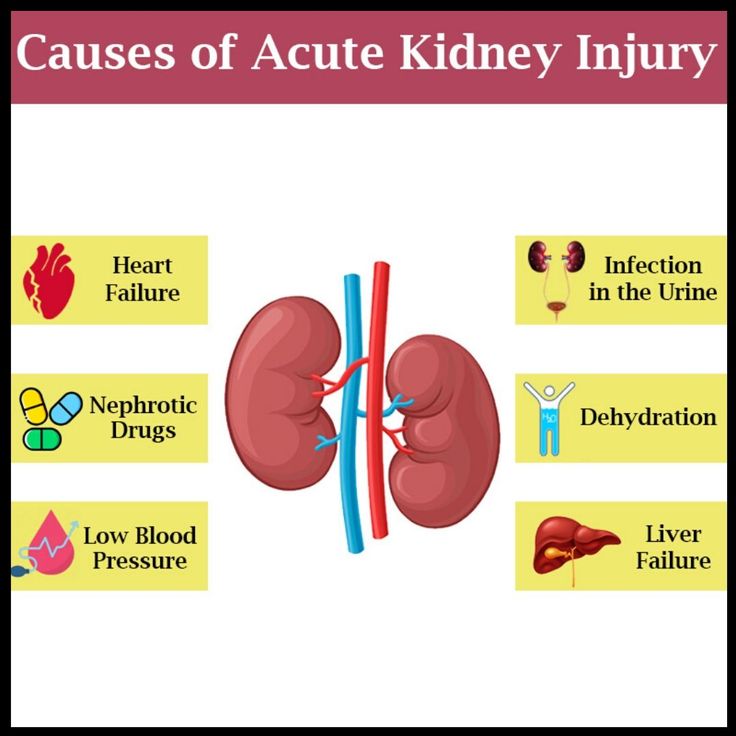
Proper treatment of pyelonephritis may prevent serious problems.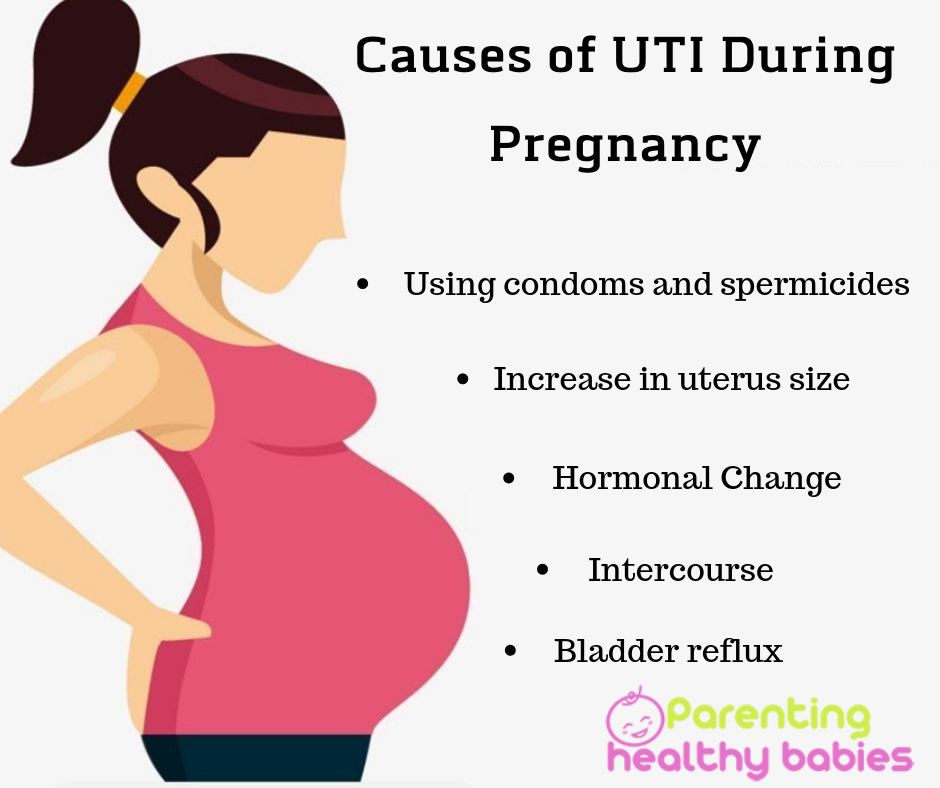 If untreated, it can lead to a bacterial infection in the bloodstream called sepsis. This can then spread to other parts of the body and cause serious conditions requiring emergency treatment.
If untreated, it can lead to a bacterial infection in the bloodstream called sepsis. This can then spread to other parts of the body and cause serious conditions requiring emergency treatment.
Untreated pyelonephritis can also result in acute respiratory distress as fluid accumulates in the lungs.
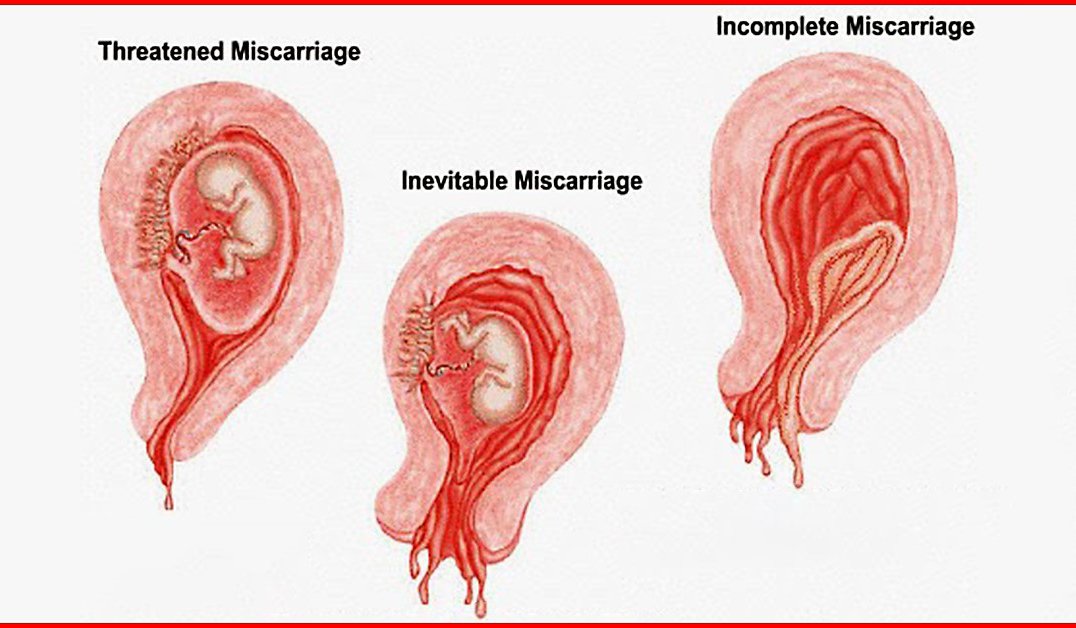
Pyelonephritis during pregnancy is a leading cause of preterm labor, which puts the baby at high risk for serious complications and even death.
How is pyelonephritis diagnosed?
A urine test can help your doctor determine whether your symptoms are the result of a kidney infection. The presence of white blood cells and bacteria in urine, which can be viewed under a microscope, are both signs of infection. Your doctor can make a definitive diagnosis by taking bacterial cultures of your urine.
How should pyelonephritis be treated?
As a general rule, if you develop pyelonephritis during pregnancy, you’ll be hospitalized for treatment. You’ll be given intravenous antibiotics, probably cephalosporin drugs such as cefazolin (Ancef) or ceftriaxone (Rocephin).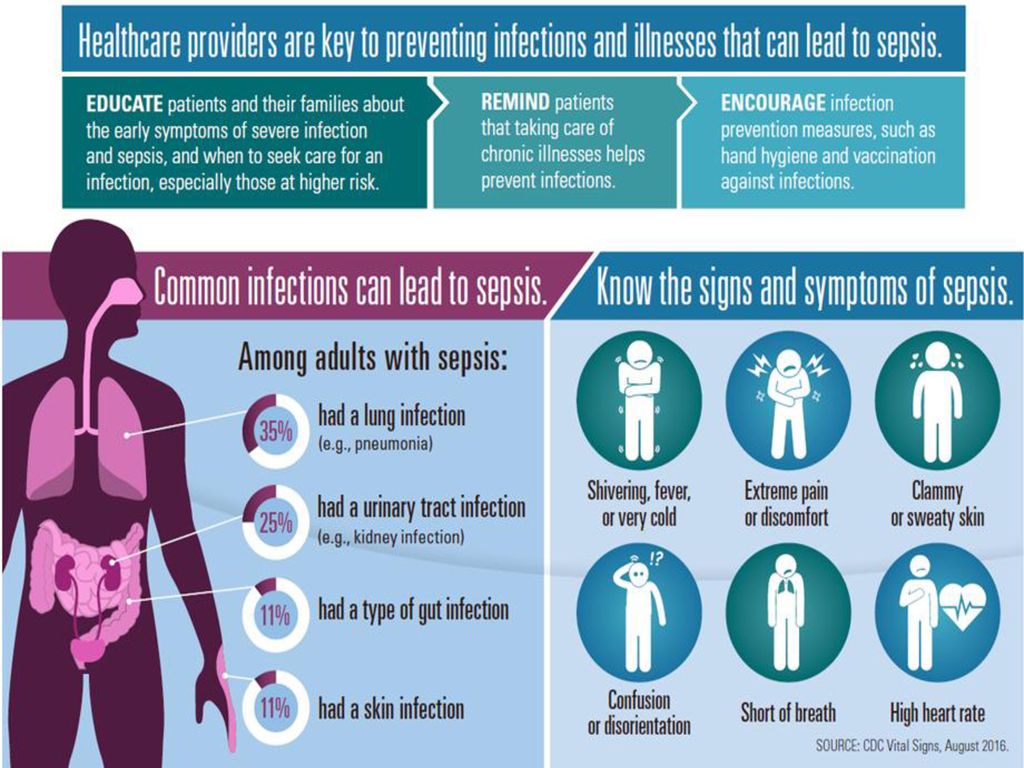
If your symptoms don’t improve, it may be that the bacteria causing the infection are resistant to the antibiotic you’re taking. If your doctor suspects that the antibiotic isn’t able to kill the bacteria, they may add a very strong antibiotic called gentamicin (Garamycin) to your treatment.
Blockage within the urinary tract is the other main cause of treatment failure. It’s typically caused by a kidney stone or physical compression of the ureter by the growing uterus during pregnancy. Urinary tract obstruction is best diagnosed through an X-ray or an ultrasound of your kidneys.
Once your condition begins to improve, you may be allowed to leave the hospital. You’ll be given oral antibiotics for 7 to 10 days. Your doctor will choose your medication based on its effectiveness, toxicity, and cost. Drugs such as trimethoprim-sulfamethoxazole (Septra, Bactrim) or nitrofurantoin (Macrobid) are often prescribed.
Recurrent infections later in pregnancy aren’t uncommon. The most cost-effective way to lower your risk of recurrence is to take a daily dose of an antibiotic, such as sulfisoxazole (Gantrisin) or nitrofurantoin monohydrate macrocrystals (Macrobid), as a preventive measure.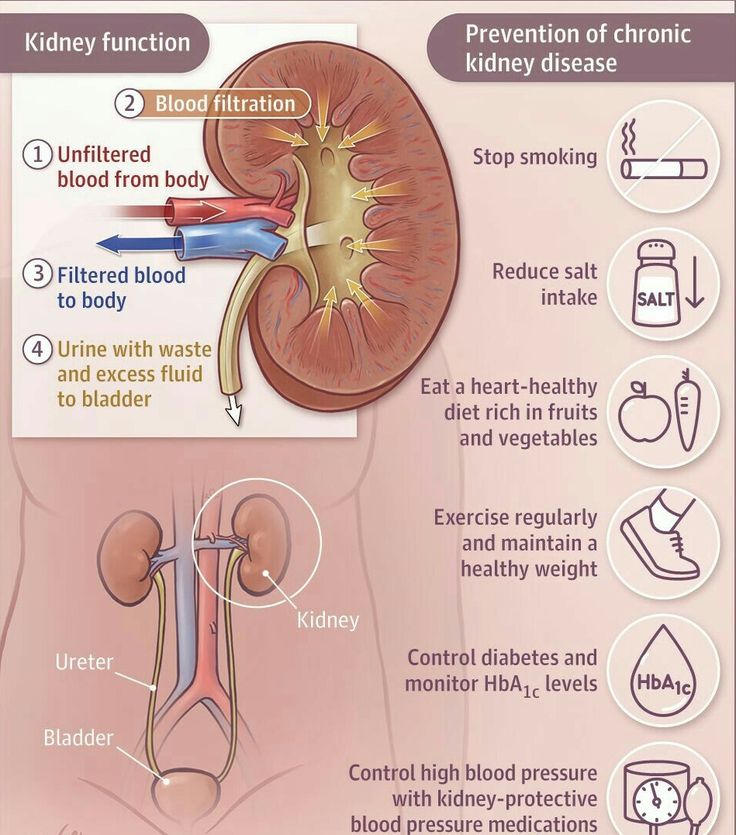 Remember that drug dosages may vary. Your doctor will prescribe what’s right for you.
Remember that drug dosages may vary. Your doctor will prescribe what’s right for you.
If you’re taking preventive medication, you should also have your urine screened for bacteria each time you see your doctor. As well, be sure to tell your doctor if any symptoms return. If the symptoms return or if a urine test shows the presence of bacteria or white blood cells, your doctor may recommend another urine culture to determine if treatment is necessary.
Pyelonephritis and pregnancy: causes and treatment
Consultation with a specialist:
Types of pyelonephritis during pregnancy
Gestational pyelonephritis is classified according to different criteria:
-
By pathogenesis: primary and secondary. Pyelonephritis is considered primary if the inflammatory process initially develops in a healthy kidney. Secondary pyelonephritis occurs against the background of anomalies in the development of the kidney and urinary tract, urodynamic disorders.
 nine0003
nine0003 -
Downstream: acute and chronic. Acute inflammation has a pronounced symptomatology, and is more often diagnosed in primiparas. Chronic is formed gradually, and is observed with repeated gestations.
-
By period: exacerbation, partial remission and remission. For exacerbation, active symptoms are characteristic, for partial remission - a gradual fading of symptoms, for remission - the absence of clinical and laboratory signs of pyelonephritis. nine0003
-
According to the preservation of kidney function: without impaired renal function, with impaired renal function and chronic renal failure.
-
By the number of affected kidneys: unilateral (more often the right kidney is affected) and bilateral.
Depending on the nature of pathological changes, acute pyelonephritis has several stages of development: nine0003
-
serous inflammation;
-
purulent inflammation;
-
apostematous pyelonephritis - a purulent-inflammatory process with the formation of multiple small pustules in the medulla of the organ;
-
kidney carbuncle - purulent-necrotic process;
- nine0006 kidney abscess - the formation of a purulent focus, delimited by a pseudocapsule, in the cortical and medulla of the kidney.
The acute form has two outcomes - complete recovery or chronic inflammation. The outcome of chronic pyelonephritis is structural and functional changes in the renal tissue of varying degrees.
Call right now
+7 (495) 215-56-90
Sign up
Causes of pyelonephritis during pregnancy
During the gestation period, pyelonephritis is found even in healthy women with normal function and structure of the kidneys. The reason for this is the presence of any purulent-inflammatory process in the body. Conditionally pathogenic microorganisms enter the kidney with blood or urine from the underlying organs, initiate inflammatory changes in the kidney tissue.
The most common causative agent of pyelonephritis in pregnant and non-pregnant women is a bacterium of the Enterobacteriaceae family (E. coli). Saprophytic Staphylococcus aureus, Klebsiella, Candida, Chlamydia, Streptococcus, Proteus, Mycoplasma and viruses are sown less frequently. nine0003
nine0003
Risk factors for the development of gestational pyelonephritis:
-
Inflammatory diseases of the female genital organs. Infection of the kidney occurs with vulvitis (external inflammation of the genital organs), colpitis (inflammation in the vagina), bacterial vaginosis. Pathogens from the foci of infection by the hematogenous route enter the kidney tissue.
-
Asymptomatic bacteriuria. In the urine of patients, a monoinfection is sown, while there are no clinical symptoms. Since urine is a favorable environment for the reproduction of opportunistic microflora, under conditions of stagnation and reverse reflux of urine, saprophytic microorganisms are activated, and pyelonephritis develops. The presence of a history of urological pathologies contributes to the more rapid development of latent chronic bacteriuria. nine0003
-
urodynamic changes. In pregnant women, against the background of an increase in the level of progesterone, the pelvicalyceal system expands, hypotension of the bladder develops (impaired urine outflow).
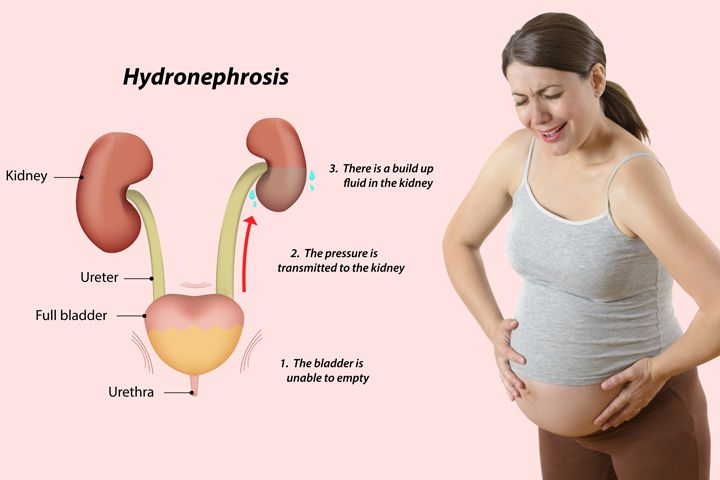 At the late stage of pregnancy, the situation is aggravated by the relaxation of the urethral sphincter, accelerated glomerular filtration, squeezing of the urinary organs by the growing uterus.
At the late stage of pregnancy, the situation is aggravated by the relaxation of the urethral sphincter, accelerated glomerular filtration, squeezing of the urinary organs by the growing uterus.
The likelihood of inflammation of the kidney tissue increases in the presence of urolithiasis, congenital malformations of the urinary system, kidney stones, diabetes mellitus. nine0003
Symptoms of pyelonephritis during pregnancy
Clinical manifestations of pyelonephritis in different gestational periods has typical features. In the first trimester, a constant symptom is a sharp, intense pain in the lumbar region. The pain spreads to the groin, genitals, lower abdomen.
Help! Usually, in primigravida, the first signs of pyelonephritis occur at 4-6 weeks, with repeated gestation - at 6-8 weeks. nine0094
Nonspecific symptom of acute pyelonephritis - intoxication syndrome:
In the II and III trimester pain in the lumbar region is less intense. The clinical picture is dominated by dysuric disorders: frequent urination, pain when emptying the bladder.
The clinical picture is dominated by dysuric disorders: frequent urination, pain when emptying the bladder.
Chronic pyelonephritis can occur with exacerbations (active phase of acute inflammation), be replaced by a latent (asymptomatic) phase or go into remission. nine0003
Diagnosis of pyelonephritis in pregnancy
The complexity of diagnosing gestational pyelonephritis is associated with a limited number of research methods that are safe during pregnancy. It is not recommended to carry out x-ray diagnostics, cystoscopy (examination of the bladder with an endoscopic device), bladder catheterization, as there is a possibility of infection.
When collecting an anamnesis, a nephrologist or urologist finds out the presence of foci of chronic infection, congenital malformations of the organs of the urinary system and other diseases that can cause a violation of the outflow of urine. In the course of the survey, he clarifies the duration of pregnancy and the features of its course.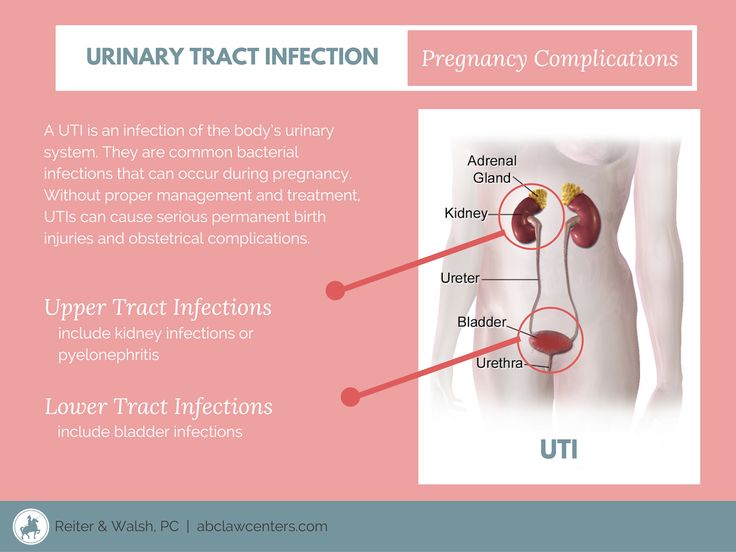 nine0003
nine0003
The plan for examining a pregnant woman includes laboratory and non-invasive techniques:
-
Clinical blood test. The level of neutrophils and leukocytes is increased, ESR is increased, a neutrophilic shift of the leukocyte formula to the left is detected.
-
Blood chemistry. Increased concentration of sialic acids, urea, creatinine, determine a positive reaction to C-reactive protein. nine0003
-
General urine analysis. During the period of acute inflammation, a large amount of protein and bacteria are found in the urine.
-
Rehberg's test. Filtration is impaired in case of severe kidney damage.
-
Microbiological examination of urine. Allows you to identify the pathogen to select adequate antibiotic therapy.
nine0009
Ultrasound of the kidneys. It makes it possible in real time to determine the structural changes in the kidney, the expansion of the pelvicalyceal system and assess the severity of the inflammatory process.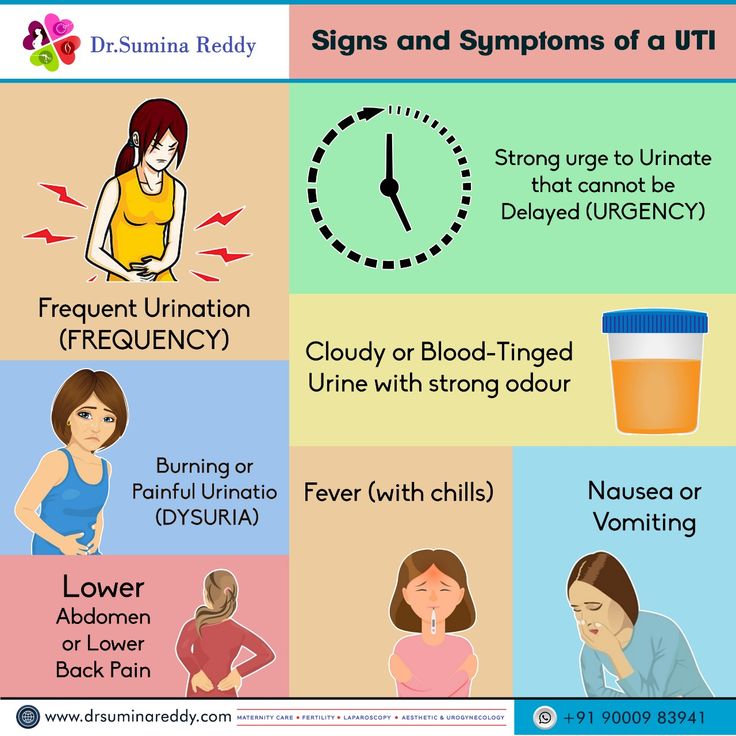 During the study, tumors, malformations of the organs of the genitourinary system, and stones can be detected.
During the study, tumors, malformations of the organs of the genitourinary system, and stones can be detected.
In the process of diagnosing pyelonephritis, it is necessary to exclude diseases with similar symptoms: appendicitis, acute cholecystitis (inflammation of the walls of the gallbladder), renal colic, toxoplasmosis and respiratory tract infections. nine0003
Treatment of pyelonephritis in pregnancy
Therapy of acute pyelonephritis is aimed at stopping the infectious and inflammatory process, normalizing the outflow of urine and eliminating stagnation, and restoring the functions of the urinary system. Treatment is selected taking into account the duration of pregnancy, the severity of the disease and the presence of complications.
Medical treatment
To treat the infection that provoked inflammation, antibiotic therapy is carried out. Before obtaining the results of a bacteriological analysis of urine, broad-spectrum antimicrobials are prescribed.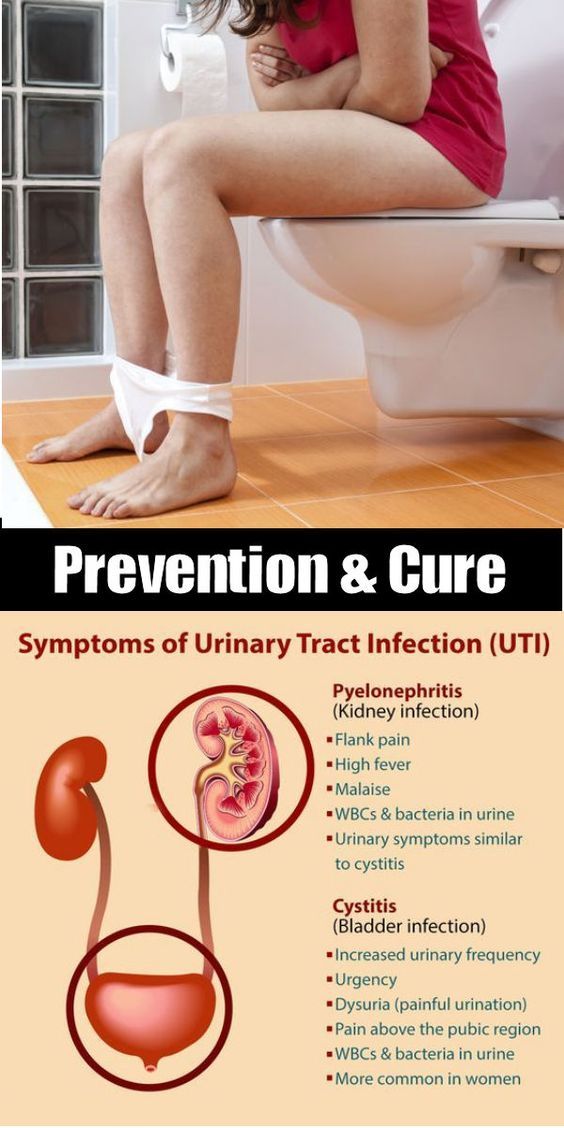 In the first trimester of gestation, inhibitor-protected aminopenicillins are recommended, from the second trimester macrolides and cephalosporins are used, in the third trimester - sulfonamides. After receiving a bacteriological analysis with the identification of the pathogen and determining its sensitivity to antibiotics, the therapy is corrected. nine0003
In the first trimester of gestation, inhibitor-protected aminopenicillins are recommended, from the second trimester macrolides and cephalosporins are used, in the third trimester - sulfonamides. After receiving a bacteriological analysis with the identification of the pathogen and determining its sensitivity to antibiotics, the therapy is corrected. nine0003
Against the background of antibiotic therapy, detoxification therapy is necessary. To remove toxic products from the body, albumin, aqueous solutions of salts and organic acids are administered intravenously. At the same time, antihistamines and desensitizing drugs are taken, which prevent and weaken the possible manifestations of an allergy to antibiotics.
In the treatment of pyelonephritis, antispasmodics, herbal uroantiseptics, saluretics to remove sodium and chlorine ions, non-steroidal anti-inflammatory drugs to reduce pain are actively used. nine0003
14 days after the end of the antibiotic, a repeated microscopic examination of the urine is performed. In the absence of infection and an increased dose of protein, dynamic monitoring of the pregnant woman is continued.
In the absence of infection and an increased dose of protein, dynamic monitoring of the pregnant woman is continued.
To consolidate the therapeutic effect, non-drug methods are practiced:
-
plentiful drink;
-
sleep in a knee-elbow position to activate the outflow of urine; nine0003
-
taking diuretics and herbal antiseptics;
-
the use of fortified decoctions and fruit drinks from rose hips, lingonberries, cranberries.
In the absence of positive clinical and laboratory dynamics, a ureteral catheter, nephrostomy or stent is installed for normal urine outflow and elimination of stagnation.
nine0006 Important! In the process of treatment, carefully monitor the condition of the fetus, prevent hypoxia. If developmental delay is detected, appropriate therapy is indicated.Surgical treatment
Acute secondary pyelonephritis, purulent-destructive processes in the kidney are indications for surgical treatment.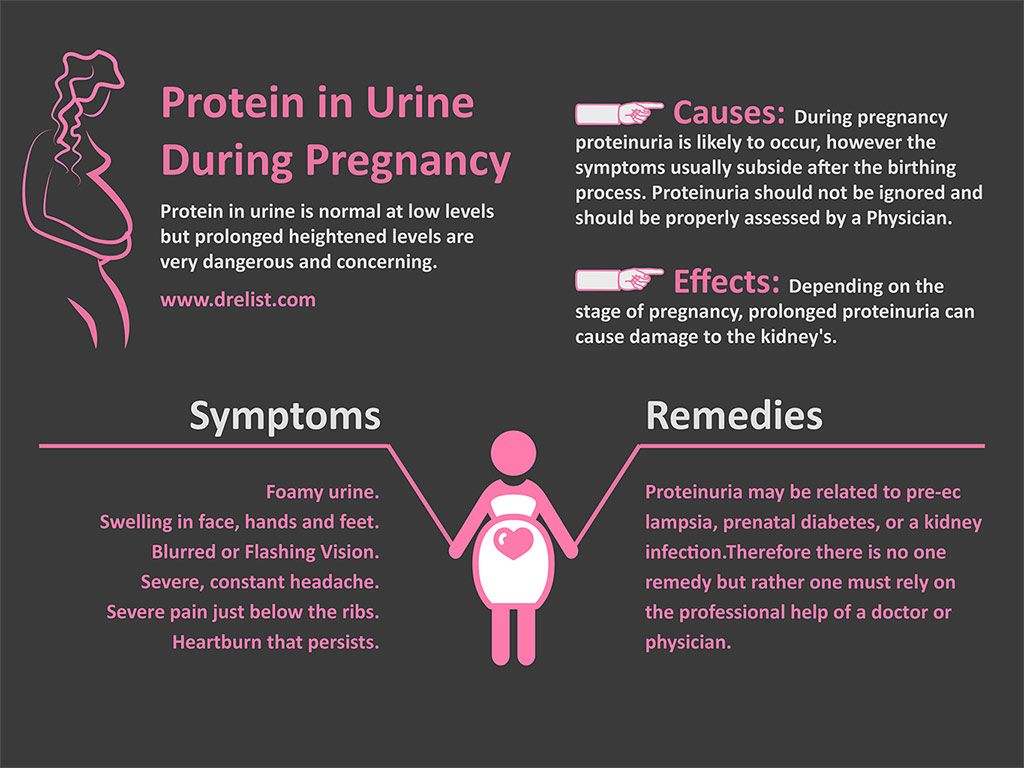
Preference is given to organ-preserving operations:
-
excision of purulent-necrotic areas of the renal tissue; nine0003
-
decapsulation - removal of the renal capsule to reduce pressure inside the renal parenchyma;
-
puncture drainage of a kidney abscess;
-
opening of purulent foci;
-
lumbotomy - opening of the retroperitoneal space.
With a high risk of infectious complications, purulent destruction of more than 2/3 of the renal parenchyma, nephrectomy is performed - complete removal of the kidney. nine0003
In most cases, gestational pyelonephritis occurs without destructive changes in the kidney, so it can be successfully treated with conservative methods. In most pregnant women with acute pyelonephritis, childbirth occurs spontaneously with the use of antispasmodic drugs. Artificial delivery is necessary for chronic complicated pyelonephritis and a high likelihood of obstetric complications.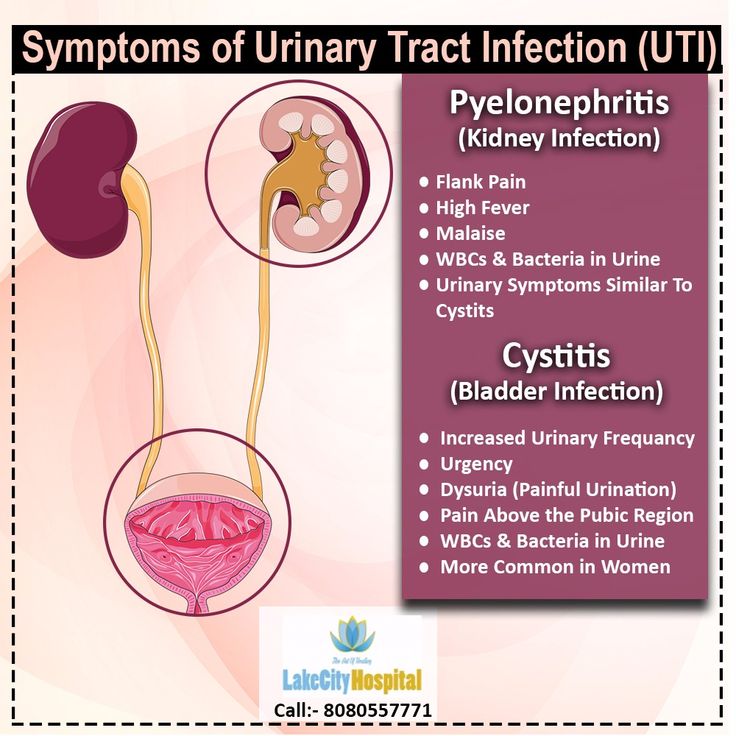
Prevention of pyelonephritis in pregnancy
nine0006 Prevention of gestational pyelonephritis is aimed at eliminating the factors that contribute to the occurrence of an infectious and inflammatory process in the kidney:-
early registration in the antenatal clinic,
-
diagnosis of asymptomatic bacteriuria and urodynamic disorders,
-
balanced diet, nine0003
-
moderate physical activity in order to prevent stagnation of urine,
-
quitting smoking and alcohol.
Pregnant women at risk are recommended to take uroantiseptic drugs to prevent pyelonephritis.
Share:
Call now
+7 (495) 215-56-90
Enroll
Pregnancy and kidney disease - Academic Medical Center (AMC)
Kidney and urinary tract diseases in pregnant women are the second most common after cardiovascular pathologies.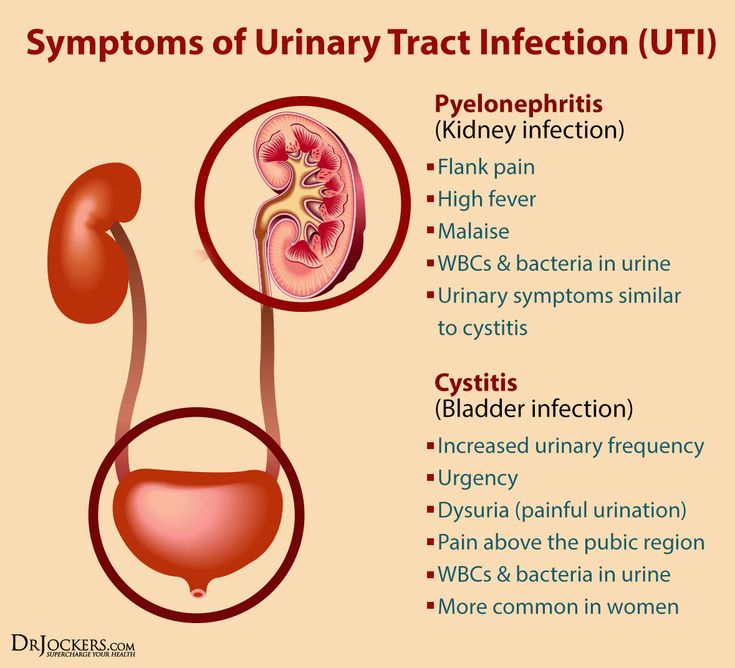 During pregnancy, a woman's body undergoes a number of physiological changes, due to which the load on all organs and systems, including the kidneys and bladder, increases. With an increase in the size of the uterus, squeezing of the ureters occurs and the outflow of urine from the kidneys becomes more difficult. All this increases the likelihood of the spread of bacteria and the development of the disease. Most often, complications occur when there were infections or inflammatory diseases in the woman's body that were not cured before pregnancy. nine0094
During pregnancy, a woman's body undergoes a number of physiological changes, due to which the load on all organs and systems, including the kidneys and bladder, increases. With an increase in the size of the uterus, squeezing of the ureters occurs and the outflow of urine from the kidneys becomes more difficult. All this increases the likelihood of the spread of bacteria and the development of the disease. Most often, complications occur when there were infections or inflammatory diseases in the woman's body that were not cured before pregnancy. nine0094
Kidney complications during pregnancy can be dangerous for both the woman and the fetus. In some cases, previous or chronic kidney disease may be a contraindication to pregnancy. How to prepare for pregnancy if there were kidney diseases, and what complications can develop in a healthy woman, said the doctor of the highest category, urologist of the Academic Medical Center Sergey Andreevich Grushko.
Sergey Andreevich, tell me how to prepare for pregnancy a woman who has had kidney disease? nine0093
— All women who have had pyelonephritis are registered at the dispensary.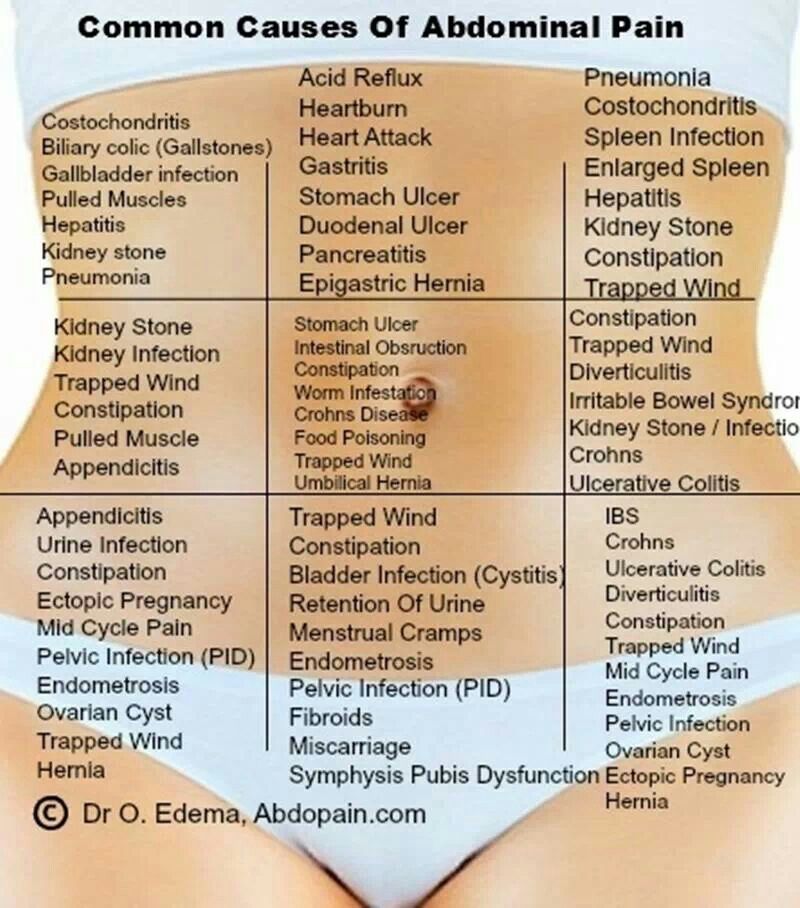 Before pregnancy, they must undergo all the necessary examinations, and after receiving their results, decide with the doctor whether the woman is now ready to carry the pregnancy. If there are any inflammatory processes in the body, they must be treated. In the second half of pregnancy, as a rule, the outflow of urine from the kidneys, especially from the right one, is disturbed. If a woman had an infection before pregnancy, obstructive pyelonephritis may develop at this point. This usually ends with kidney stenting or percutaneous nephrostomy. In severe cases, there may be a risk of abortion. nine0003
Before pregnancy, they must undergo all the necessary examinations, and after receiving their results, decide with the doctor whether the woman is now ready to carry the pregnancy. If there are any inflammatory processes in the body, they must be treated. In the second half of pregnancy, as a rule, the outflow of urine from the kidneys, especially from the right one, is disturbed. If a woman had an infection before pregnancy, obstructive pyelonephritis may develop at this point. This usually ends with kidney stenting or percutaneous nephrostomy. In severe cases, there may be a risk of abortion. nine0003
In what cases can pregnancy be contraindicated?
— Pregnancy is contraindicated in chronic pyelonephritis accompanied by renal insufficiency.
How likely is a healthy woman to develop kidney complications?
— All women are advised to prepare for pregnancy, as during the bearing of the fetus, a double burden is placed on the body. The presence of infections in the body or anomalies in the development of the kidneys during pregnancy can lead to the development of pyelonephritis and other complications.