Signs of bladder weakness
Overactive bladder - Symptoms and causes
Overview
Overactive bladder, also called OAB, causes a frequent and sudden urge to urinate that may be difficult to control. You may feel like you need to pass urine many times during the day and night, and may also experience unintentional loss of urine (urgency incontinence).
If you have an overactive bladder, you may feel embarrassed, isolate yourself, or limit your work and social life. The good news is that a brief evaluation can determine whether there's a specific cause for your overactive bladder symptoms.
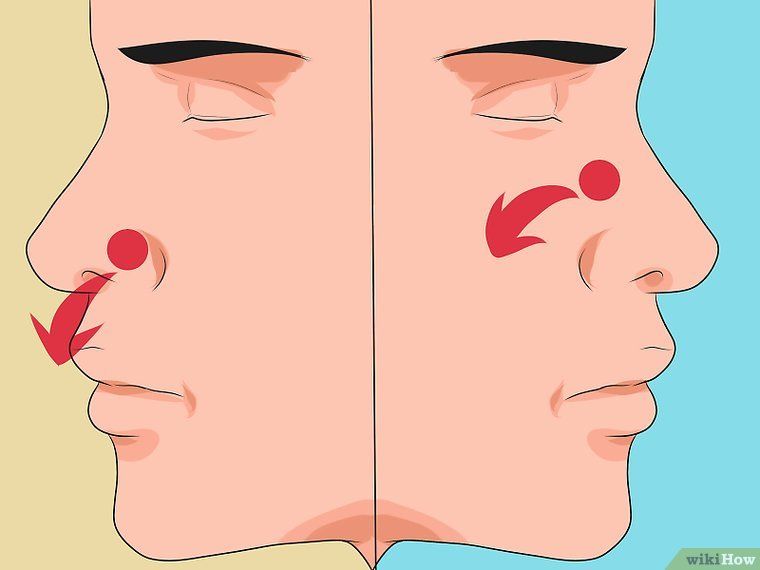
You may be able to manage symptoms of an overactive bladder with simple behavioral strategies, such as dietary changes, timed voiding and bladder-holding techniques using your pelvic floor muscles. If these initial efforts don't help enough with your overactive bladder symptoms, additional treatments are available.
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Book: Mayo Clinic on Incontinence
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Symptoms
If you have an overactive bladder, you may:
- Feel a sudden urge to urinate that's difficult to control
- Experience unintentional loss of urine immediately after an urgent need to urinate (urgency incontinence)
- Urinate frequently, usually eight or more times in 24 hours
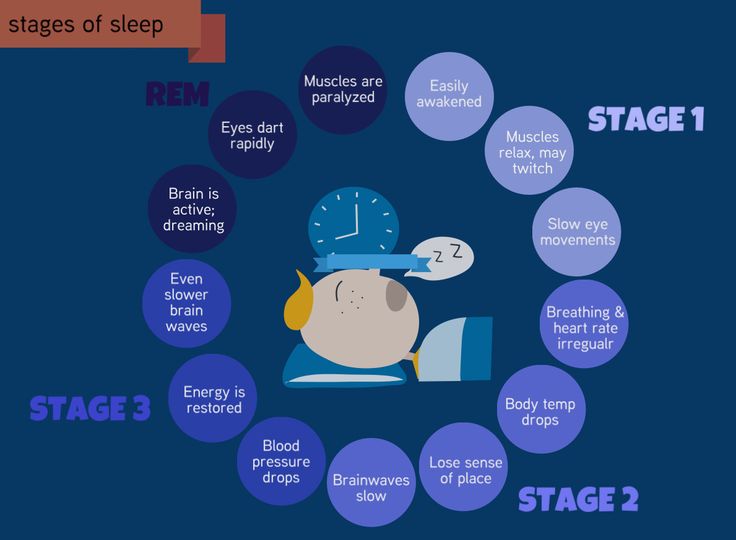
- Wake up more than two times in the night to urinate (nocturia)
Even if you are able to get to the toilet in time when you sense an urge to urinate, unexpected frequent urination and nighttime urination can disrupt your life.
When to see a doctor
Although it's not uncommon among older adults, overactive bladder isn't a typical part of aging. It might not be easy to discuss your symptoms, but if they are distressing you or disrupting your life, talk to your doctor. Treatments are available that might help you.
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which
information is beneficial, we may combine your email and website usage information with
other information we have about you. If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
Causes
How a healthy bladder works
Female urinary system
Female urinary system
Your urinary system includes the kidneys, ureters, bladder and urethra. The urinary system removes waste from the body through urine. The kidneys are located toward the back of the upper abdomen. They filter waste and fluid from the blood and produce urine. Urine moves from the kidneys through narrow tubes to the bladder. These tubes are called the ureters. The bladder stores urine until it's time to urinate. Urine leaves the body through another small tube called the urethra.
Male urinary system
Male urinary system
Your urinary system includes the kidneys, ureters, bladder and urethra. The urinary system removes waste from the body through urine. The kidneys are located toward the back of the upper abdomen. They filter waste and fluid from the blood and produce urine. Urine moves from the kidneys through narrow tubes to the bladder. These tubes are called the ureters. The bladder stores urine until it's time to urinate. Urine leaves the body through another small tube called the urethra.
The kidneys are located toward the back of the upper abdomen. They filter waste and fluid from the blood and produce urine. Urine moves from the kidneys through narrow tubes to the bladder. These tubes are called the ureters. The bladder stores urine until it's time to urinate. Urine leaves the body through another small tube called the urethra.
The kidneys produce urine, which drains into your bladder. When you urinate, urine passes from your bladder through a tube called the urethra (u-REE-thruh). A muscle in the urethra called the sphincter opens to release urine out of the body.
In women, the urethral opening is located just above the vaginal opening. In men, the urethral opening is at the tip of the penis.
As your bladder fills, nerve signals sent to your brain eventually trigger the need to urinate. When you urinate, these nerve signals coordinate the relaxation of the pelvic floor muscles and the muscles of the urethra (urinary sphincter muscles). The muscles of the bladder tighten (contract), pushing the urine out.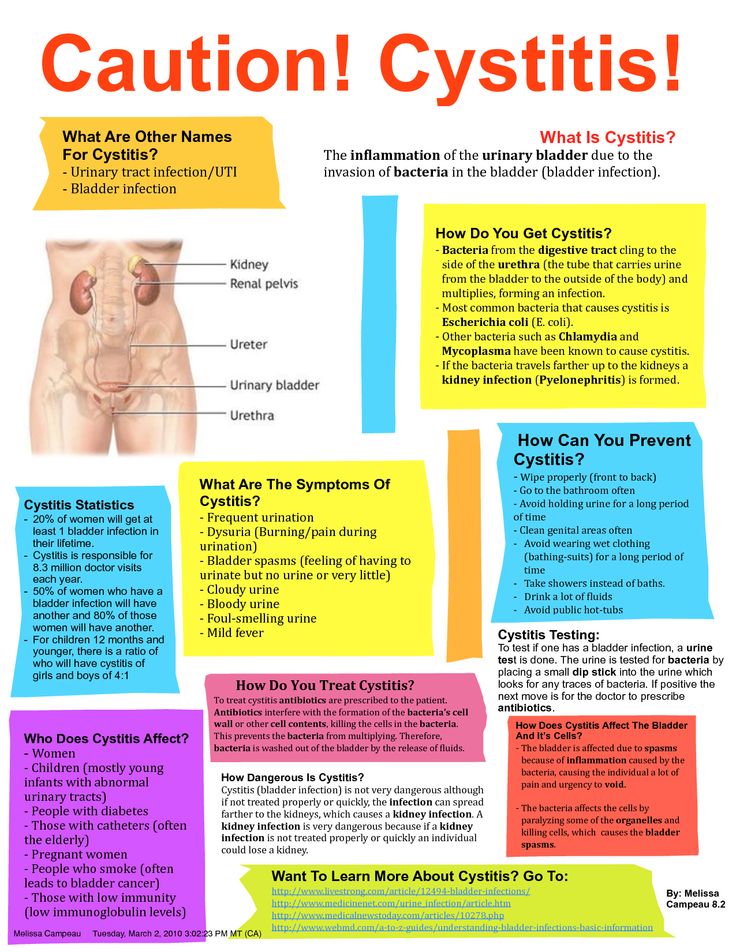
Involuntary bladder contractions
Overactive bladder happens when the muscles of the bladder start to contract on their own even when the volume of urine in your bladder is low. These are called involuntary contractions, and they create an urgent need to urinate.
Several conditions may contribute to signs and symptoms of overactive bladder, including:
- Neurological disorders, such as stroke and multiple sclerosis
- Diabetes
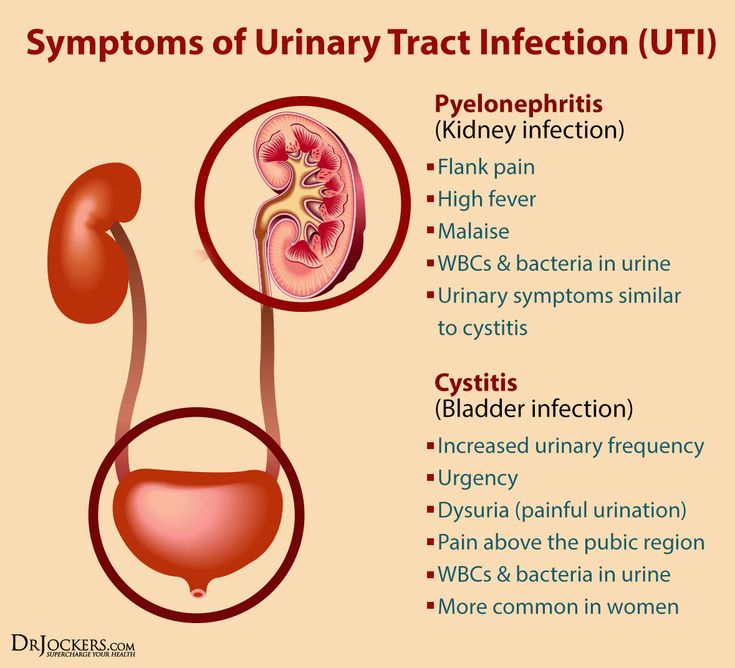
- Urinary tract infections that can cause symptoms similar to those of an overactive bladder
- Hormonal changes during menopause in women
- Conditions affecting the bladder, such as tumors or bladder stones
- Factors that get in the way of urine leaving the bladder, such as enlarged prostate, constipation or previous surgery to treat incontinence
Overactive bladder symptoms may also be associated with:
- Medications that cause your body to make a lot of urine or require that you take them with lots of fluids
- Drinking too much caffeine or alcohol
- Declining cognitive function due to aging, which may make it more difficult for your bladder to understand the signals it receives from your brain
- Difficulty walking, which can lead to bladder urgency if you're unable to get to the bathroom quickly
- Incomplete bladder emptying, which may lead to symptoms of overactive bladder, as you have little urine storage space left
The specific cause of an overactive bladder may be unknown.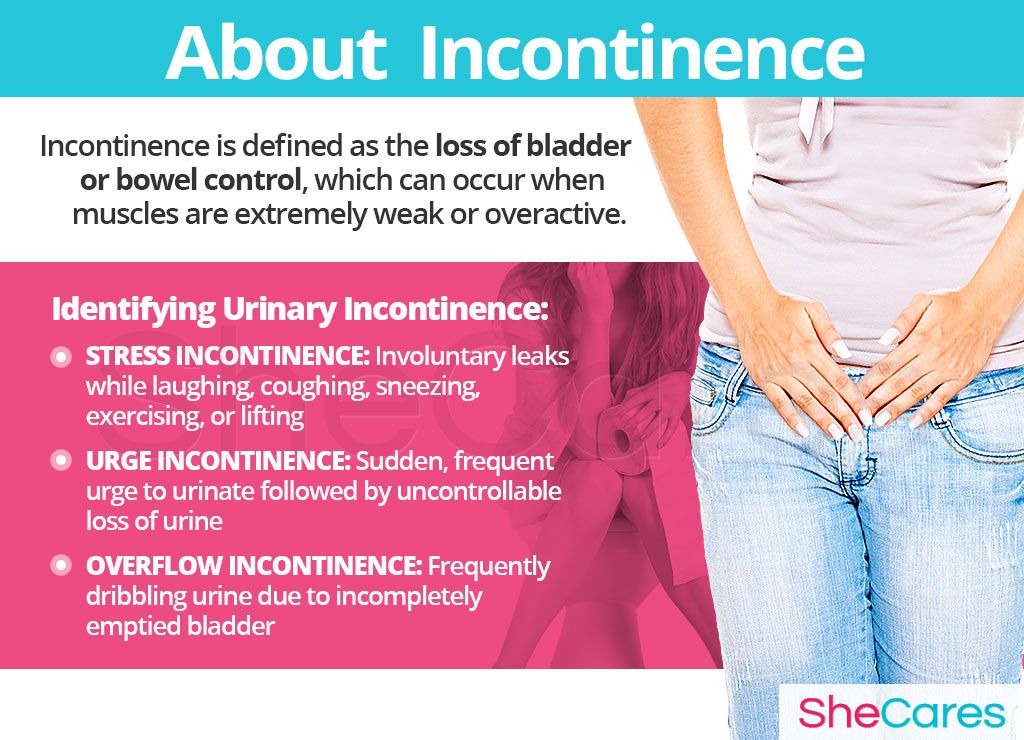
Risk factors
As you age, you're at increased risk of developing overactive bladder. You're also at higher risk of diseases and disorders, such as enlarged prostate and diabetes, which can contribute to other problems with bladder function.
Many people with cognitive decline — for instance, those who have had a stroke or have Alzheimer's disease — develop an overactive bladder. Incontinence that results from situations like this can be managed with fluid schedules, timed and prompted voiding, absorbent garments, and bowel programs.
Some people with an overactive bladder also have bowel control problems; tell your doctor if this is a problem for you.
Complications
Any type of incontinence can affect your overall quality of life. If your overactive bladder symptoms cause disruption to your life, you might also have:
- Emotional distress or depression
- Anxiety
- Sleep disturbances and interrupted sleep cycles
- Issues with sexuality
In some cases, treatment of these associated conditions may help with your urinary symptoms.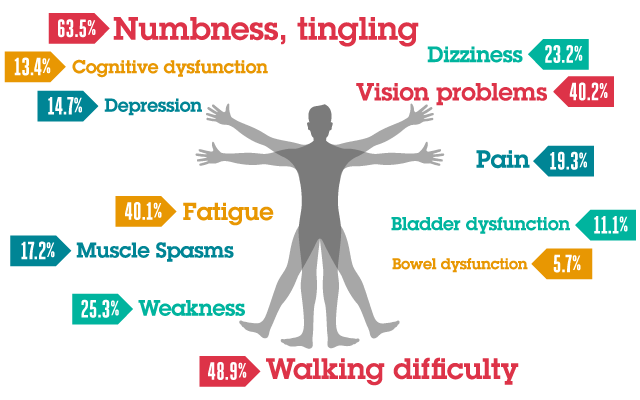
Women who have an overactive bladder may also have a disorder called mixed incontinence, when both urgency and stress incontinence occur. Stress incontinence is the unintentional loss of urine prompted by physical movement or activity that puts pressure on your bladder, such as coughing, sneezing, laughing or exercising. Treatment of stress incontinence is not likely to help overactive bladder symptoms. Similarly, treatment of overactive bladder is not likely to improve stress incontinence symptoms.
Some people may have a common combination of bladder storage problems and bladder-emptying issues. The bladder may cause a lot of urgency and even incontinence, but it doesn't empty well. A specialist may be able to help you with this combination of bladder problems.
Prevention
These healthy lifestyle choices may reduce your risk of overactive bladder:
- Maintain a healthy weight.
- Get regular, daily physical activity and exercise.
- Limit caffeine and alcohol.
- Quit smoking.
- Manage chronic conditions, such as diabetes, that might contribute to overactive bladder symptoms.
- Do exercises to make the pelvic floor muscles stronger. These exercises are called Kegel exercises.
By Mayo Clinic Staff
Related
Associated Procedures
News from Mayo Clinic
Products & Services
Symptoms & Causes of Bladder Control Problems (Urinary Incontinence)
In this section:
- What are the symptoms of bladder control problems?
- When should I see a health care professional?
- What causes bladder control problems?
- What else causes bladder control problems in women?
- What else causes bladder control problems in men?
What are the symptoms of bladder control problems?
You may have bladder control problems if you limit your activities in fear of not making it to a bathroom in time.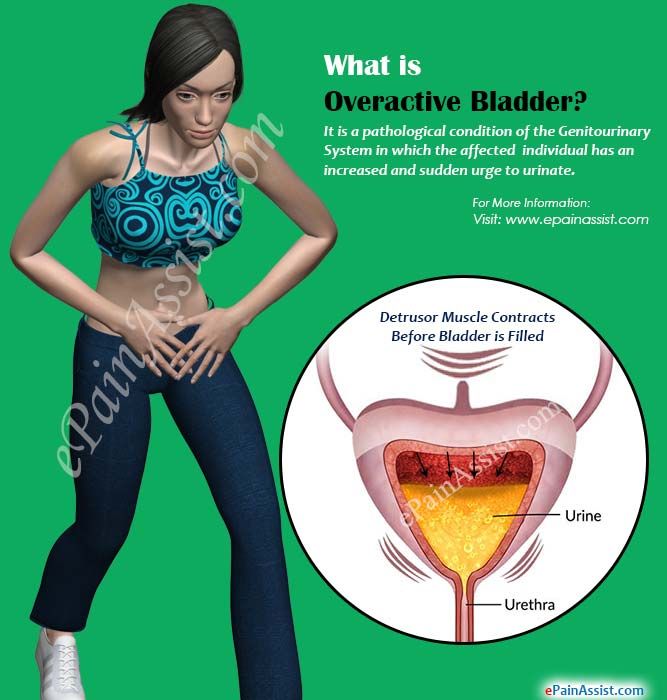
Signs and symptoms of urinary incontinence (UI) can include
- leaking urine during everyday activities, such as lifting, bending, coughing, or exercising
- being unable to hold in urine after feeling a sudden, strong urge to urinate
- leaking urine without any warning or urge
- being unable to reach a toilet in time
- wetting your bed during sleep
- leaking during sexual activity
When should I see a health care professional?
See a health care professional if you have symptoms of a bladder problem, such as trouble urinating, a loss of bladder control, waking to use the bathroom, pelvic pain, or leaking urine.
Bladder problems can affect your quality of life and cause other health problems. Your health care professional may be able to treat your UI by recommending lifestyle changes or a change in medicine.
Seek care right away
See a health care professional if you
- can’t pass urine or empty your bladder, which is a sign of urinary retention
- urinate too often—eight or more bathroom visits a day—also called frequency
- see blood in your urine, called hematuria
- have bladder infection symptoms, including painful urination
These symptoms can signal a serious health problem, including inflammation of the bladder, also called cystitis, or even bladder cancer.
What causes bladder control problems?
Health changes and problems, including those with your nervous system, and lifestyle factors can cause or contribute to UI in women and men.
Health changes and problems
Health changes and problems that can lead to UI, include
- aging
- bladder infection
- constipation
- birth defects
- blocked urinary tract—from a tumor or kidney stone
- chronic, or long-lasting, cough
- diabetes
- overweight or obesity
- genitourinary fistulas
Some health problems can be short-term, like a urinary tract infection or constipation, and can cause temporary incontinence.
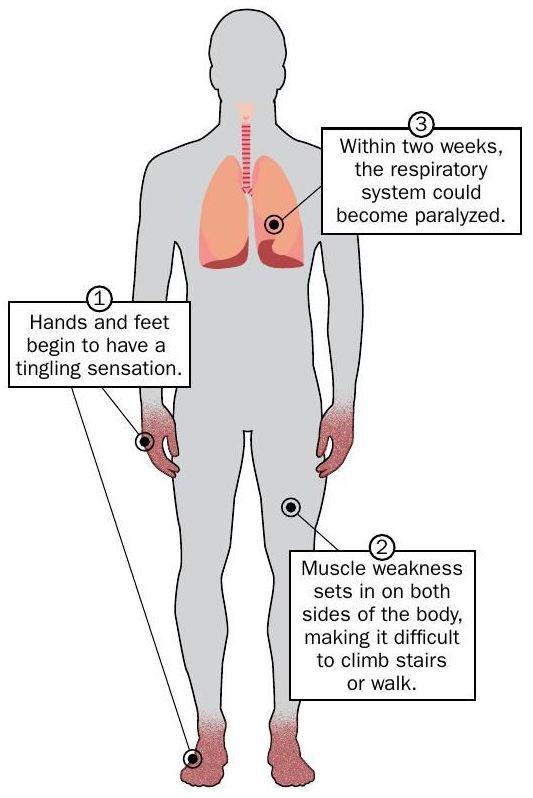
Nerve damage
Problems with the nervous system are common causes of UI. Nerves carry messages from the bladder to the brain to let it know when the bladder is full. Nerves also carry messages from the brain to the bladder, telling muscles either to tighten or release.![]() The brain decides if it’s an acceptable time to urinate. Functional incontinence can occur when there is a problem getting the messages from your brain to a part of your urinary tract—usually the bladder, the sphincters, or both.
The brain decides if it’s an acceptable time to urinate. Functional incontinence can occur when there is a problem getting the messages from your brain to a part of your urinary tract—usually the bladder, the sphincters, or both.
Nerves carry signals from your brain to your bladder and sphincter muscles.
Bladder nerves and muscles can be damaged or affected by
- diabetes
- vaginal childbirth
- surgery for prostate cancer
- stroke
- Parkinson’s disease
- multiple sclerosis
- Alzheimer’s disease
- brain or spinal cord injury
- anxiety
- heavy metal poisoning
Triggers that may cause a sudden, strong urge to urinate can include drinking or touching water, hearing running water, or being in a cold environment, such as reaching into the freezer at the grocery store.
Lifestyle factors
Lifestyle factors that make women and men more likely to experience UI include
- eating habits, such as eating foods that cause constipation
- drinking habits, such as drinking alcohol or caffeinated or carbonated beverages
- certain medicines
- physical inactivity
- smoking
Temporary incontinence is usually a side effect of a medicine or short-term health condition. Temporary incontinence can also be a result of eating and drinking habits, including using alcohol or caffeine.
Temporary incontinence can also be a result of eating and drinking habits, including using alcohol or caffeine.
What else causes bladder control problems in women?
Certain life events and health problems can lead to stress incontinence in women by weakening the pelvic floor muscles
- pregnancy and childbirth
- trauma or injury, such as sexual assault
- pelvic organ prolapse, such as a cystocele
- menopause
Weak pelvic floor muscles can make it hard for your bladder to hold urine in during stress incontinence. Stress incontinence occurs when an action—coughing, sneezing, laughing, or physical activity—puts pressure on your bladder and causes urine to leak. A weak pelvic floor can also cause fecal incontinence, or bowel control problems.
Weak pelvic floor muscles can allow your bladder to leak.
What else causes bladder control problems in men?
Men sometimes develop UI along with prostate problems.
Prostate problems
Men have a prostate gland that surrounds the opening of the bladder.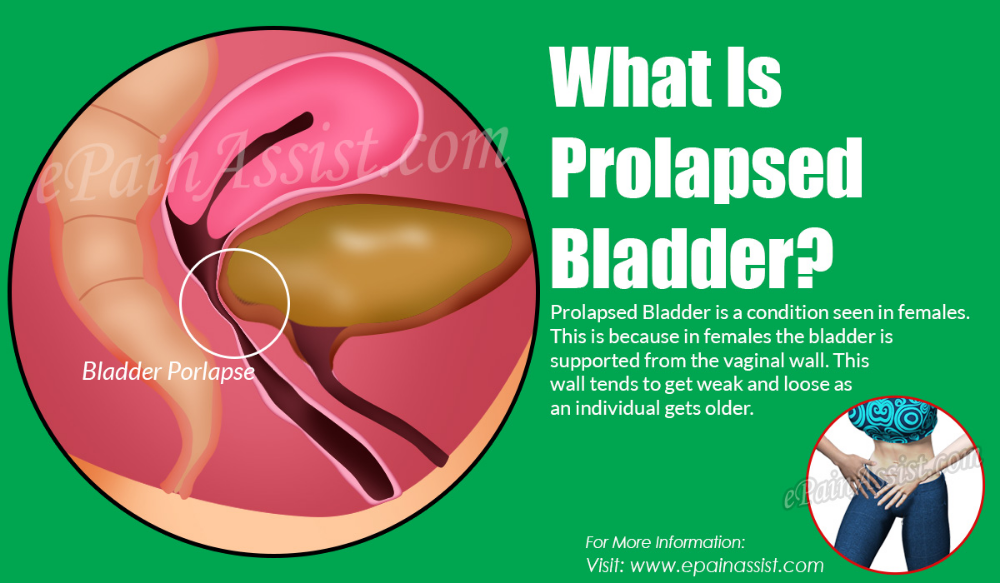 The prostate gets bigger as a man grows older. When a man’s prostate gets too big but isn’t cancerous, he has a condition called prostate enlargement, or benign prostatic hyperplasia (BPH). Men with an enlarged prostate may have
The prostate gets bigger as a man grows older. When a man’s prostate gets too big but isn’t cancerous, he has a condition called prostate enlargement, or benign prostatic hyperplasia (BPH). Men with an enlarged prostate may have
- problems starting to urinate
- a slow urine stream
- problems fully emptying the bladder
Treatment for BPH can lead to stress incontinence, but it is usually temporary.
Men who have a history of radiation or surgery for prostate cancer may have short-term or long-term UI. Surgery, radiation, or other prostate cancer treatments can lead to nerve damage, bladder spasms, or stress incontinence. Bladder control problems after prostate cancer treatment can get better over time.
When the prostate gets too big it can squeeze the urethra, making it hard to start urinating. You also may have a slow urine stream or be unable to completely empty your bladder.
Neurogenic bladder dysfunction (NDDM)
home
Diseases and treatment
Neurogenic bladder dysfunction (NDBD)
Neurogenic bladder dysfunction (NDMP)
At the N.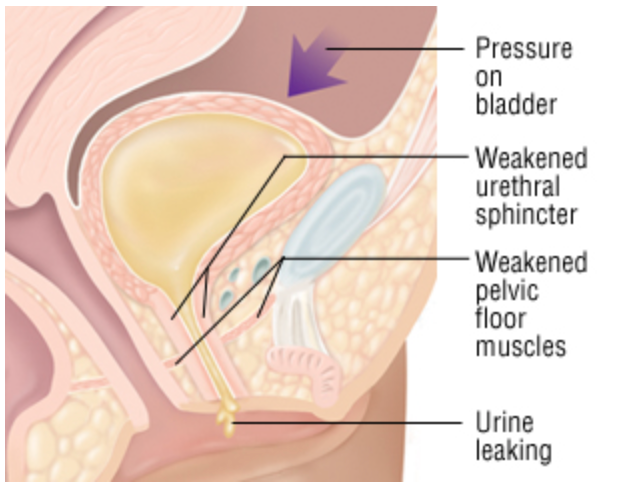 A. Lopatkin - a branch of the Federal State Budgetary Institution "NMITs Radiology" of the Ministry of Health of Russia, all modern methods of treating neurogenic bladder dysfunction are used. We bring to your attention a brief but very detailed description of this disease. It was prepared by specialists of the Department of Urolithiasis of the Research Institute of Urology and Interventional Radiology named after N.A. Lopatkina
A. Lopatkin - a branch of the Federal State Budgetary Institution "NMITs Radiology" of the Ministry of Health of Russia, all modern methods of treating neurogenic bladder dysfunction are used. We bring to your attention a brief but very detailed description of this disease. It was prepared by specialists of the Department of Urolithiasis of the Research Institute of Urology and Interventional Radiology named after N.A. Lopatkina
Neurogenic bladder dysfunction (NDDM)
- a collective term for urinary disorders in children and adults, formed in the absence of regulation of the process by the nervous system and (or) smooth muscles of the bladder and can be caused by various diseases and pathological conditions characterized by impaired nervous regulation of the lower urinary tract. The nature of NDMP largely depends on the location and severity of neurological disorders.
The overall prevalence of NDDM in the population reaches 16-23%. With various diagnosed neurological diseases, the prevalence of NDMT can reach 90%. The main manifestations of NDMP can be such types of functional disorders as: overactive bladder (OAB), hypoactive bladder, functional infravesical obstruction (FIVO) caused by spasm of the striated urethral sphincter, detrusor-sphincter dyssynergy (DSD).
With various diagnosed neurological diseases, the prevalence of NDMT can reach 90%. The main manifestations of NDMP can be such types of functional disorders as: overactive bladder (OAB), hypoactive bladder, functional infravesical obstruction (FIVO) caused by spasm of the striated urethral sphincter, detrusor-sphincter dyssynergy (DSD).
Symptoms:
- Frequent urination
- Urinary incontinence (when there is an urge to urinate)
- Non-mechanical urinary retention
- Pain in the region of the bladder and projection of the urethra
- Urgent urge to urinate
It should be noted that all the symptoms of NDMT can be combined and uncharacteristic, which is why the diagnosis of this disease requires consultation of a highly qualified narrow specialist - a neurourologist.
Risk factors:
- Cerebrovascular disease (stroke)
- Alzheimer's disease
- Parkinson's syndrome or other corticobasal degeneration
- Tumors of the brain and spinal cord
- Cerebral palsy
- Injuries of the brain and spinal cord
- Spina bifida
- Degenerative diseases of the lumbar spine
- Intervertebral disc pathology
- Degenerative diseases
- Intervertebral disc prolapse
- Lumbar spinal stenosis
- Iatrogenic injuries of the pelvic nerves
- Peripheral neuropathy
- Diabetes mellitus
- Alcohol abuse
- Herpes sacro-lumbar and genital herpes, Guillain-Barré syndrome
- Porfiria
- Sarcoidosis
- Multiple sclerosis
Diagnosis:
Diagnostic procedures used to recognize NPDM.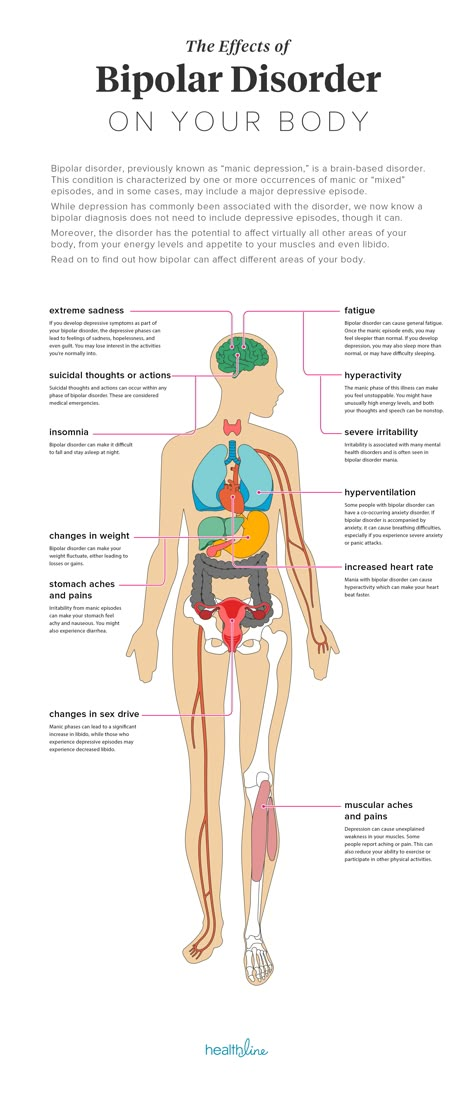
- Physical examination
- History taking
- Diagnostics of risk factors
- Urination diaries
- Profile Questionnaire Questionnaire
- Uroflowmetry with residual urine volume (UVR)
- Combined urodynamic study (CUDI)
Treatment:
Treatment of NDDM primarily depends on the variant of its manifestation. In the conditions of the Research Institute of Urology and Interventional Radiology, a branch of the Federal State Budgetary Institution "NMITs Radiology" of the Ministry of Health of Russia, there is the most modern equipment for the diagnosis and treatment of this nosology.
Main treatments for NDMT:
- Behavioral Therapy
- Physiotherapy: biofeedback, extracorporeal electromagnetic stimulation, tibial neuromodulation
- Pharmacotherapy (individual selection of the drug and its dose for each specific case)
- Botulinum therapy (injection of botulinum toxin type A into the detrusor and striated urethral sphincter)
Prophylaxis:
- S
- Regular visits to a urologist
- Active monitoring for all neurological diseases by a neurologist
Department where neurogenic bladder dysfunction (NDMP) is treated
Lopatkina !
After the consultation, it will be necessary to undergo an examination or additional examination, after which an interdisciplinary consultation of doctors will be held, at which a decision will be made on the chosen method of treatment.
Department of Urodynamics and Neuurology Research Institute of Urology and Interventional Radiology named after N.A. Lopatkina is the leading department of the institute in the treatment of patients with various disorders of urination and urinary incontinence.
Head of the department, urologist - ROMIKH Victoria Valerievna
Call us today so that we can help you!
Moscow, 8 (499) 110 - 40 - 67
COVID
19
COVID
19
+7(800)444-31-02
Physiological causes of loss of urinary control in men and women
Urinary incontinence (also known as urinary leakage) is described as involuntary and uncontrolled urination. It can happen to anyone, regardless of gender or age, although each gender has its own risks at different stages of life.
At an early age, girls usually learn to control their bladder function earlier than boys, and enuresis is much less common in girls.
In adulthood, women are much more likely than men to experience incontinence. This is mainly due to the peculiarities of the structure of the pelvic organs and the changes caused by pregnancy and childbirth.
While urinary incontinence is not an inevitable part of aging, the prevalence of the condition increases dramatically with age.
How the bladder functions
To understand what causes incontinence and why incontinence occurs in each sex, it is necessary to understand how a healthy bladder functions.
The bladder is a muscular, globular organ that sits in the pelvis and is held in place by the pelvic floor muscles. Its function is to store urine and get rid of it.
Urine is delivered to the urethra via the urethra. The muscular ring - the sphincter - pinches the urethra, preventing leakage of urine, until the appropriate command is received from the brain, while the normal hormonal background helps to maintain the urethral mucosa in a healthy state.
When the muscular sac that is the bladder fills up, the muscle tissue relaxes and a signal is sent along the nerves to the brain that it is time to urinate. The brain, in turn, sends a feedback signal to the bladder that it is possible to relax the sphincter.
In order for the excretory system to function effectively, muscles and nerves must work in sync to keep urine in the bladder and, at the right time, allow the body to empty it. If any muscle or nerve is not working properly, it can lead to incontinence.
- Weak muscles
Weak pelvic floor muscles are the cause of most urinary control problems. If the bladder sags due to muscle weakness, it becomes distended at the opening of the urethra.
- Nerve damage
Nerve damage can either send an unauthorized signal to the bladder, resulting in involuntary urination, or a complete lack of signal from the bladder to the brain, which cannot determine when the bladder is full. Nerve damage can result from injury or disease, such as Parkinson's disease, stroke, diabetes, or multiple sclerosis.
Nerve damage can result from injury or disease, such as Parkinson's disease, stroke, diabetes, or multiple sclerosis.
In addition to nerve damage and weakening of the pelvic floor muscles, incontinence can be caused by drug-induced CNS depression.
Types of incontinence
Temporary incontinence.
Functional incontinence - when the normal regulation of urination is prevented by mental or physical (inability to quickly reach the toilet) problems, despite the fact that the excretory system itself is in order. Functional incontinence is caused by Parkinson's disease, Alzheimer's disease, and other forms of dementia.
Urgent incontinence . People who leak urine after a sudden, urgent urge to urinate have urge incontinence. This is due to an increase in the tone of the muscles of the bladder, which can be the result of a large number of reasons, such as: mental stress, nerve damage (due to diabetes, stroke), infection, bladder stones, tumor. In this situation, a complete examination is necessary to identify the root cause and prescribe adequate treatment. Acute incontinence most often begins with an urgent urge to urinate when it is impossible to carry it out. This condition progresses to the point where it becomes impossible to control the process of urination. For urge incontinence, medications are indicated to help regulate bladder tone, as well as Kegel exercises to strengthen the muscles of the pelvic floor and “training” the bladder to work at a certain interval.
In this situation, a complete examination is necessary to identify the root cause and prescribe adequate treatment. Acute incontinence most often begins with an urgent urge to urinate when it is impossible to carry it out. This condition progresses to the point where it becomes impossible to control the process of urination. For urge incontinence, medications are indicated to help regulate bladder tone, as well as Kegel exercises to strengthen the muscles of the pelvic floor and “training” the bladder to work at a certain interval.
Stress incontinence. Every fifth woman over 40 knows what stress incontinence is. This is when coughing, laughing, sneezing, physical exertion (especially those that increase intra-abdominal pressure) releases a small portion of urine. Stress urinary incontinence in the vast majority of cases is characteristic of women, but does not depend on age - both young women and professional athletes are familiar with this. This is not about emotional stress, but about weakened muscles of the sphincter and pelvic floor, which leads to the fact that stress, whether it is a sudden movement or an increase in intra-abdominal pressure, leads to squeezing a portion of urine from the bladder into the urethra.