How painful is the epidural
Epidurals: Meaning and Side Effects of Anesthesia During Labor
An epidural is the most common type of anesthetic used for pain relief during labor. Here’s what you should know before having an epidural, including information that dispels some common myths.
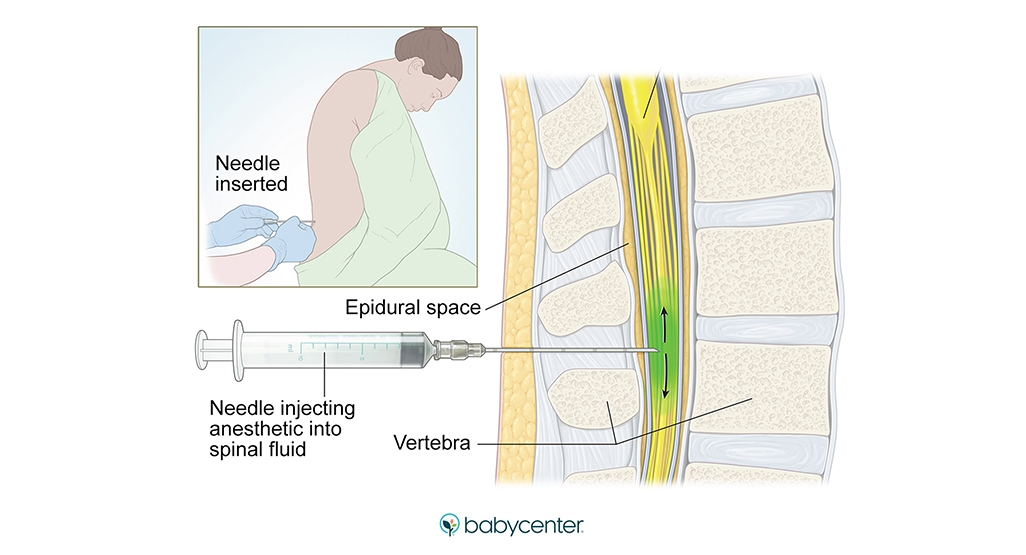
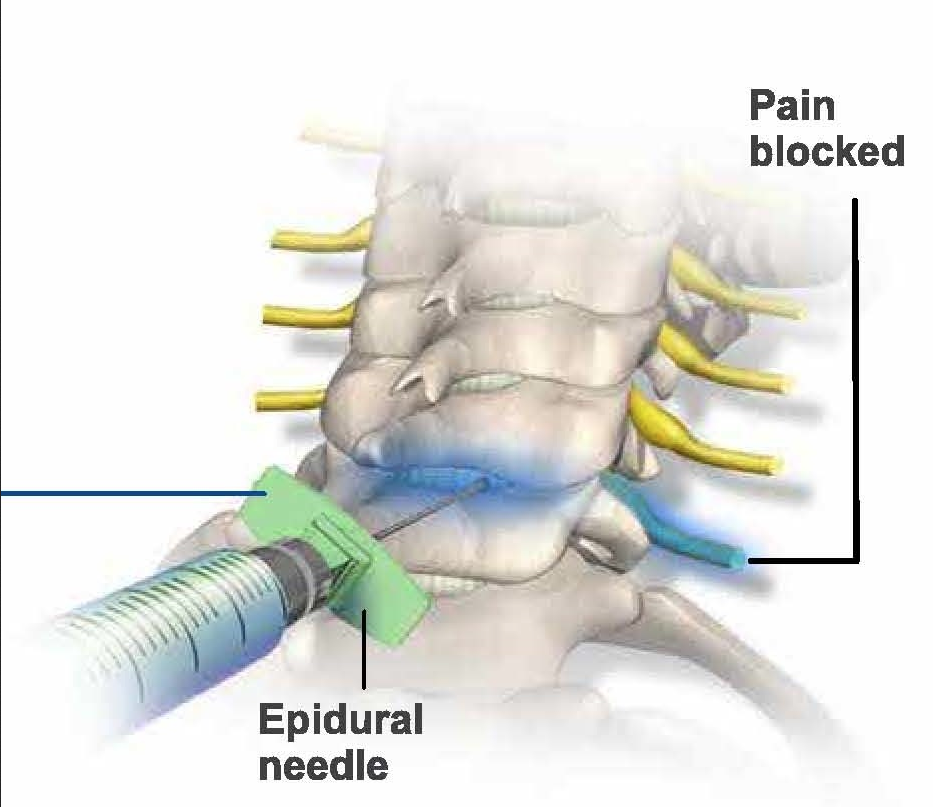
How and when is an epidural for labor pain administered?If you choose to have an epidural, an anesthesiologist will insert a needle and a tiny tube, called a catheter, in the lower part of your back. The needle is removed and the catheter left in place for delivery of the medication through the tube as needed. You can begin an epidural at any time during your labor — in the beginning, in the middle, or even toward the end — in consultation with your physician.
Does it hurt when the epidural is administered?The anesthesiologist will numb the area where the epidural is administered, which may cause a momentary stinging or burning sensation. But because of this numbing, there is very little pain associated with an epidural injection. Instead, most patients will feel some pressure as the needle is inserted.
An epidural provides anesthesia that creates a band of numbness from your bellybutton to your upper legs. It allows you to be awake and alert throughout labor, as well as to feel pressure. The ability to feel second-stage labor pressure enables you to push when it’s time to give birth to your baby. It can take about 15 minutes for the pain medication to work.
How long does the pain relief last?You can continue to receive pain relief through an epidural for as long as you need it. The amount of medication you receive through the epidural can be increased or decreased as necessary.
Can an epidural slow labor or lead to a cesarean delivery (C-section)?There is no credible evidence that it does either. When a woman needs a C-section, other factors usually are at play, including the size or position of the baby or slow progression of labor due to other issues.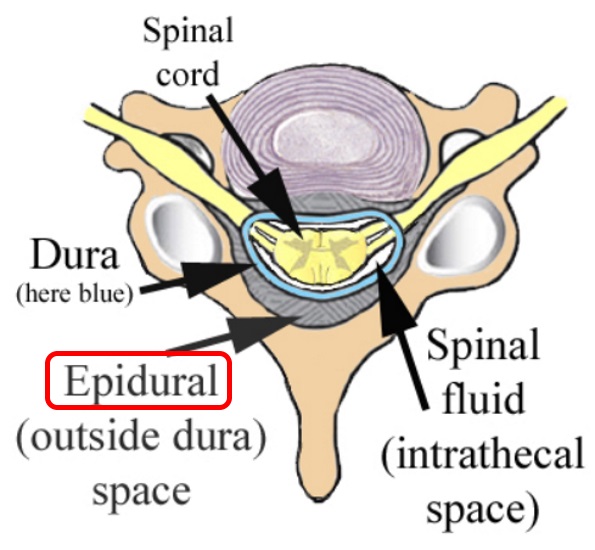 With an epidural, you might be able to feel contractions — they just won’t hurt — and you’ll be able to push effectively. There is some evidence that epidurals can speed the first stage of labor by allowing the mother to relax.
With an epidural, you might be able to feel contractions — they just won’t hurt — and you’ll be able to push effectively. There is some evidence that epidurals can speed the first stage of labor by allowing the mother to relax.
The amount of medication that reaches the baby from the epidural is very small, and there is no evidence that it causes any harm.
Are there risks and side effects?Epidurals are very safe; serious complications are extremely rare. However, as with all medications and medical procedures, there are potential side effects:
- Decrease in blood pressure – The medication may lower your blood pressure, which may slow your baby’s heart rate. To make this less likely, you will be given extra fluids through a tube in your arm (IV), and you may need to lie on your side. Sometimes, your anesthesiologist will give you a medication to maintain your blood pressure.
- Sore back – Your lower back may be sore where the needle was inserted to deliver the medication. This soreness should last no more than a few days. There is no evidence that an epidural can cause permanent back pain.
- Headache – On rare occasions, the needle pierces the covering of the spinal cord, which can cause a headache that may last for a few days if left untreated. If this situation arises, discuss the treatment options with your anesthesiologist.
A spinal block is sometimes used in combination with an epidural during labor to provide immediate pain relief. A spinal block, like an epidural, involves an injection in the lower back. While you sit or lie on your side in bed, a small amount of medication is injected into the spinal fluid to numb the lower half of the body. It brings good relief from pain and starts working quickly, but it lasts only an hour or two and is usually given only once during labor.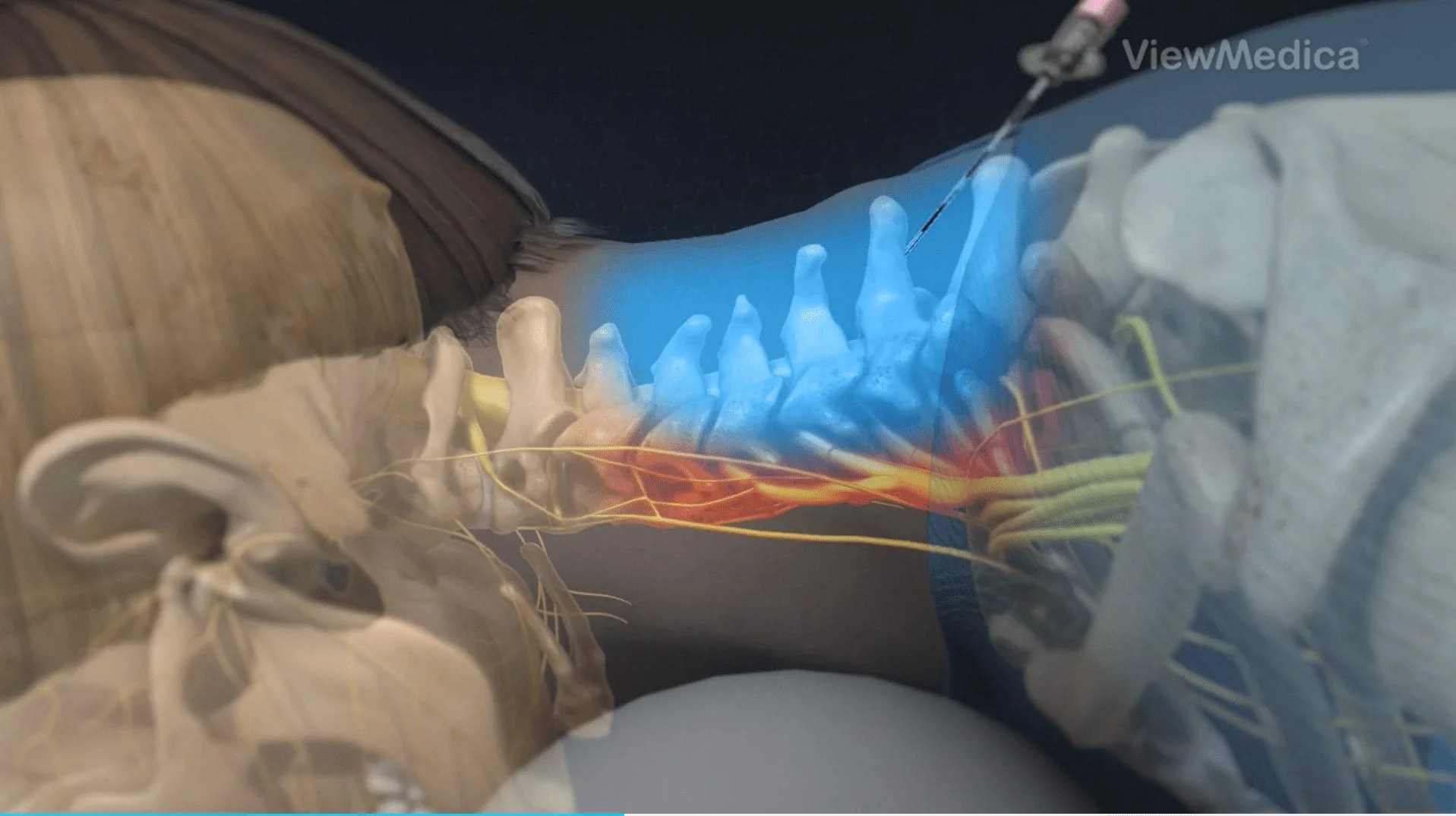 The epidural provides continued pain relief after the spinal block wears off.
The epidural provides continued pain relief after the spinal block wears off.
Anesthesiologists are committed to patient safety and high-quality care, and have the necessary knowledge to understand and treat the entire human body.
What Does an Epidural Feel Like?
The CDC reports that around 61% of women opt for epidural or spinal anesthesia during vaginal birth, and it's not a surprise why. Labor can be painful! As the American Society of Anesthesiologists and American College of Obstetricians and Gynecologists have said, "There is no other circumstance where it is considered acceptable for an individual to experience untreated severe pain, amenable to safe intervention, while under a physician's care." While some mothers may opt for drug-free births using lamaze, acupuncture, or massage, many mothers chose epidurals — pain medication delivered through a catheter inserted near your spine — to manage their labor pains.
Dr. Edna Ma, an anesthesiologist and mother of two who also had two labor epidurals as a patient, explains that epidurals usually happen when a patient is about 4 cm dilated during labor.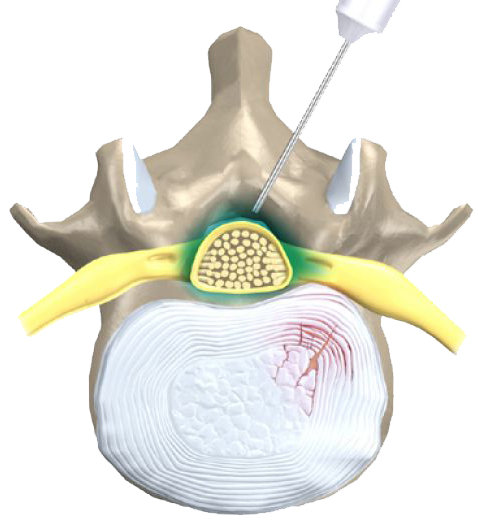 "From the patient perspective, the numbing medicine feels like a bee-sting," she explains. Once you've been numbed, you won't feel the epidural needle inserted into your back. You may feel pressure as the epidural needle is inserted into the right spot, but you shouldn't feel the actual needle. Once the needle is in place, the anesthesiologist will insert a catheter and remove the needle. Dr. Ma says that the whole process shouldn't take more than ten minutes.
"From the patient perspective, the numbing medicine feels like a bee-sting," she explains. Once you've been numbed, you won't feel the epidural needle inserted into your back. You may feel pressure as the epidural needle is inserted into the right spot, but you shouldn't feel the actual needle. Once the needle is in place, the anesthesiologist will insert a catheter and remove the needle. Dr. Ma says that the whole process shouldn't take more than ten minutes.
Here, eight women who went through labor epidurals describe their experiences.
1. "I had an epidural after 15 hours of labor. I knew it was something that I wanted the second I found out I was pregnant. Who wants to go through the worst pain of your life? I have scoliosis so the administrator had to put the needle in both my left and right sides of my spine. It was awful. I had to hold still for 15 minutes with contractions happening every two minutes. They say you forget everything about labor after you have a baby, but that is not true.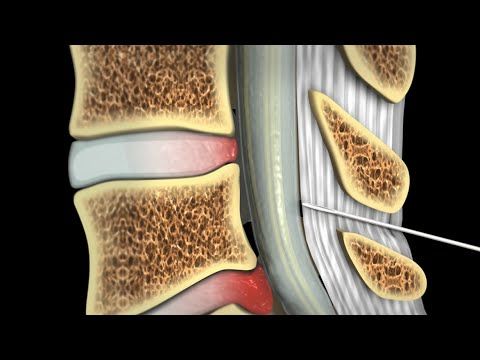 I remember every single detail. I loved my epidural and would pre-order it for my next baby if I could."— Rosalin, 37
I remember every single detail. I loved my epidural and would pre-order it for my next baby if I could."— Rosalin, 37
2. "I got my first epidural in 2016 and it was not as scary or painful as most women make it seem. Yes, you are getting a getting a small tube inserted near your spine via a not-so-tiny needle, but that is not the worst part. Getting an epidural feels like being a sock puppet, and the anesthesiologist is the puppeteer. You feel the poking and prodding, and the tube threading down your back initially, but once the medicine begins to work, it feels like the puppet strings have been cut, and you're dancing away like Pinocchio... figuratively, not literally. You can't move once the epidural is administered. "— Brittany, 24
3. "With my first, I wanted to try to have a drug-free birth if possible. But, real talk, I just couldn’t do it! After being awake [during labor] for more than 30 hours, I needed a break.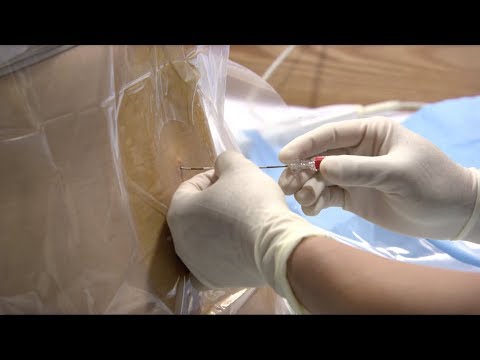 The worst part of an epidural is the numbing before the epidural is administered — though the needle injection in your back is no joke either. The numbing was awful because it felt like a terrible burning sensation down my back. It was also nerve-wracking because while you're getting the epidural you’re also going through contractions, but you need to stay perfectly still while it happens. It took a few minutes for the epidural to work but, to me, it was totally worth it. I had relief very quickly and didn’t feel pain again until after it wore off post-birth. With the epidural, I was able to finally sleep before a long night of pushing. With my second child, as soon as I was admitted, I asked for the epidural right away because I knew what to expect. I knew I needed my 'nap' before my life was going to change all over again."— Stephanie, 34
The worst part of an epidural is the numbing before the epidural is administered — though the needle injection in your back is no joke either. The numbing was awful because it felt like a terrible burning sensation down my back. It was also nerve-wracking because while you're getting the epidural you’re also going through contractions, but you need to stay perfectly still while it happens. It took a few minutes for the epidural to work but, to me, it was totally worth it. I had relief very quickly and didn’t feel pain again until after it wore off post-birth. With the epidural, I was able to finally sleep before a long night of pushing. With my second child, as soon as I was admitted, I asked for the epidural right away because I knew what to expect. I knew I needed my 'nap' before my life was going to change all over again."— Stephanie, 34
4. "I'm a fairly "crunchy" gal, gravitating to holistic wellness. As such, I was prepared for an unmedicated pregnancy. I exercised throughout my pregnancy, ate well (mostly), and engaged in hypnobirthing with my husband who, bless him, didn't pass out during one special day of class when at least six voluminous vaginas were featured in a water-birthing video. I'm a brain tumor survivor and have an incredibly high pain threshold. At just shy of 42 weeks, I hit about 22 hours of laboring when I was told our daughter was in the occiput posterior position [Editor's note: this means the baby is head down, with their head facing their mother's belly button, as opposed to the "more favorable" position of head down, facing mom's butt.], which makes for a painful labor and delivery and often leads to c-section. At that point, I was exhausted and my doula even recommended an epidural. I consented and this crunchy mama's perception of "medicated pregnancy" vastly changed. As soon as I was given the epidural, I slept until I was told it was time to push. After about an hour of pushing mightily — like I wasn't given an epidural, my beautiful baby was born, looking straight up! And I had a little extra energy to enjoy our early time together.
I exercised throughout my pregnancy, ate well (mostly), and engaged in hypnobirthing with my husband who, bless him, didn't pass out during one special day of class when at least six voluminous vaginas were featured in a water-birthing video. I'm a brain tumor survivor and have an incredibly high pain threshold. At just shy of 42 weeks, I hit about 22 hours of laboring when I was told our daughter was in the occiput posterior position [Editor's note: this means the baby is head down, with their head facing their mother's belly button, as opposed to the "more favorable" position of head down, facing mom's butt.], which makes for a painful labor and delivery and often leads to c-section. At that point, I was exhausted and my doula even recommended an epidural. I consented and this crunchy mama's perception of "medicated pregnancy" vastly changed. As soon as I was given the epidural, I slept until I was told it was time to push. After about an hour of pushing mightily — like I wasn't given an epidural, my beautiful baby was born, looking straight up! And I had a little extra energy to enjoy our early time together. All that matters is that these precious little beings are born healthy. My daughter Madeleine is my favorite human and, by far, one of the highlights of my life. I will never naysay any woman who elects to use an epidural."—Brook, 37
All that matters is that these precious little beings are born healthy. My daughter Madeleine is my favorite human and, by far, one of the highlights of my life. I will never naysay any woman who elects to use an epidural."—Brook, 37
5. "The anesthesiologist came in and asked me to lay with my legs across the side of the bed and hold the pillow on my stomach so I would be in a hunched over position and lay very still. He put numbing cream on my back before he inserted the needle, and I barely felt it going in. I was so scared of the needle, but was even more scared of the pain of childbirth, so I just went with it! I intentionally did not want to see the needle before it went into my back so I asked them not to show it to me. It took about 20 minutes, from start to finish. It felt like a small shot going into my back — similar to getting blood drawn. I couldn't feel anything below my waist after it kicked in, so the nurses had to empty my bladder using a tube in my urethra since I couldn't feel below my waist. Overall it was a great experience. Why feel that torturous pain if you don't have to? I truly believe the epidural aided in making my birthing experience a joyous one."—Demia, 31
Overall it was a great experience. Why feel that torturous pain if you don't have to? I truly believe the epidural aided in making my birthing experience a joyous one."—Demia, 31
6. "I was very nervous about getting a needle in my back but I was scared of the pain [of unmedicated birth] even more. They put something on my spine to numb the area before the epidural went in. You feel a pinch when they insert it and it felt very warm going in, but I didn't feel anything after that. It wasn't painful but it did take the entire day to wear off, which was very uncomfortable. Once the epidural kicked in I was completely numb from the waist down and I couldn't feel anything. At one point, one side of the epidural had worn off but my other side was still completely numb. The nurse tried to get me up to walk around but I ended up passing out because I couldn't feel my legs, and they put one of those smelling salts under my nose. During my second pregnancy I was very nervous to get the epidural because of what happened during the first pregnancy. After my first experience, I was careful not to get up until I was sure the epidural wore off."—Yolanda, 35
After my first experience, I was careful not to get up until I was sure the epidural wore off."—Yolanda, 35
7. "I remember it was frightening. The anesthesiologist walked in to explain the legal jargon, the side effects, and the description of the length of the needle. He walked behind me and counted down. My thoughts raced, and then I felt the needle pierce my skin and go deeper. The injection felt like a splash of ice cubes gently melting inside my lower back after feeling the injection sting for five seconds. I kept trying to breathe and sit still because I did not want the needle wiggling around out of place. Afterwards, I had an epidural button to administer more of it, but did not use it. My legs were already completely numb. The epidural was so strong that pushing with my legs numb felt confusing and was difficult for me. Physiologically, it just seemed like my legs did not exist. I did not know if I was even pushing or making progress. I had to tell by the way the nurses and my sister answered.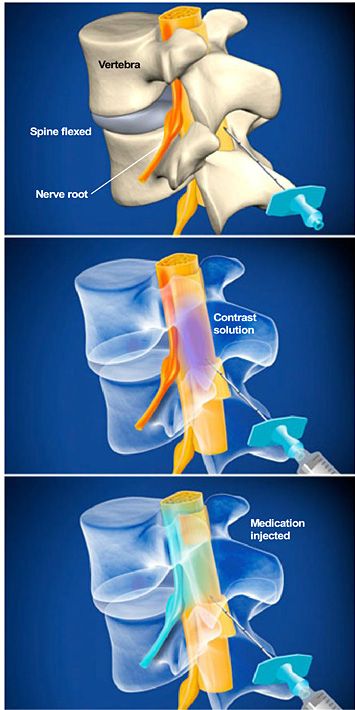 I asked for a mirror or a video so I could see my own progress."—Adriana, 27
I asked for a mirror or a video so I could see my own progress."—Adriana, 27
8. "With my first child, I was in so much pain from contractions that I barely noticed the pain from the injection. I was, however, very scared to move. We've all been warned about potential risks from an epidural and although that was very unlikely, trying not to move while having contraction makes the whole thing very scary. First, they numbed the area of my back and then injected the epidural. I felt the stinging when the drugs went in but shortly after felt nothing below my boobs. I could feel the liquid entering my back and I felt a stream of coolness enter my back with the stinging and then a sense of warmth as the lower half of my body went fairly numb. It did take some time to find the exact spot for the epidural — I gave birth at a teaching hospital so there were a few people looking at the spot and going over how to do it. I would guess 20-30 minutes. The epidural made it possible to get some rest before my daughter arrived.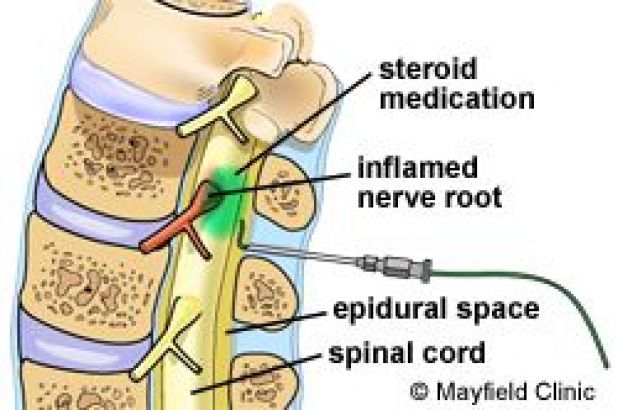 I slept for a little before pushing began. When I woke up, I was only numb on one side, so I let the doctors know that and they pumped more in. It almost worked too well and I was completely numb, so when the doctor told me to 'push right here' I had to ask him to describe exactly where, because I couldn't feel his finger!"—Stephanie, 36
I slept for a little before pushing began. When I woke up, I was only numb on one side, so I let the doctors know that and they pumped more in. It almost worked too well and I was completely numb, so when the doctor told me to 'push right here' I had to ask him to describe exactly where, because I couldn't feel his finger!"—Stephanie, 36
Answers have been lightly edited for clarity.
Follow Carina on Twitter.
Carina Hsieh Sex & Relationships Editor Carina Hsieh lives in NYC with her French Bulldog Bao Bao — follow her on Instagram and Twitter • Candace Bushnell once called her the Samantha Jones of Tinder • She enjoys hanging out in the candle aisle of TJ Maxx and getting lost in Amazon spirals.
Epidural versus non-epidural or no analgesia for labor pain management
What is the problem?
We set out to evaluate the effectiveness of all types of epidural anesthesia (including combined spinal-epidural anesthesia) for mother and child, compared with non-epidural anesthesia or its absence during childbirth.
Why is this important?
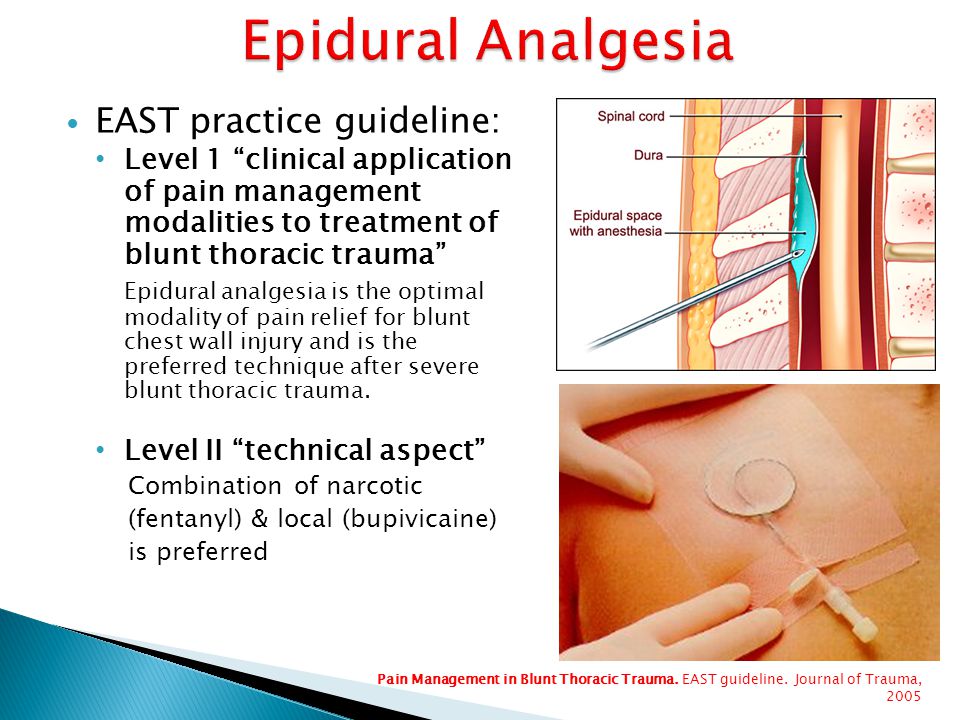
Pain relief is important for women in labour. Pharmacological methods of pain relief include inhaled nitrous oxide, opioid injections, and local analgesia with epidural anesthesia to provide central blockade. Epidural anesthesia is widely used to relieve the pain of childbirth and involves injecting a local anesthetic into the lower back in close proximity to the nerves that transmit pain. Solutions for epidural anesthesia are administered by bolus injection (large, rapid injection), continuous infusion, or using a pump (pump) controlled by the patient. When combined with opiates, lower concentrations of local anesthetic are required, which allows women to maintain the ability to move during childbirth and actively participate in them. Combined spinal-epidural anesthesia involves a single injection of a local anesthetic or opiate into the cerebrospinal fluid for rapid onset of pain relief, and insertion of an epidural catheter for long-term pain relief.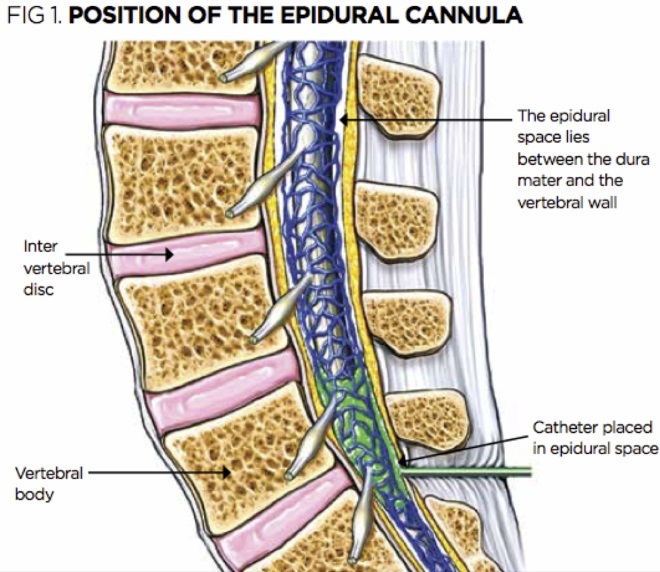 There are reports of side effects such as itching, drowsiness, chills and fever. Rare but potentially serious adverse effects of epidural anesthesia may also occur, such as severe prolonged headache after injection, or nerve damage.
There are reports of side effects such as itching, drowsiness, chills and fever. Rare but potentially serious adverse effects of epidural anesthesia may also occur, such as severe prolonged headache after injection, or nerve damage.
What evidence did we find?
We searched for evidence in April 2017 and identified 40 trials involving over 11,000 women who contributed to this review. Clinical trials have been distinguished by the quality of their methods.
All but six studies compared epidural analgesia with the administration of opioid analgesics. An epidural can relieve labor pain more effectively than opioids, and most women can be satisfied with an epidural. In general, women who have used epidurals are more likely to require forceps or vacuum extraction to assist in labor compared to opioid analgesics. However, we did not see this effect in studies conducted after 2005, which more frequently used lower local anesthetic concentrations and more modern epidural techniques such as patient-controlled epidural analgesia (PCEA). Epidural anesthesia, compared with opioids, may have little or no effect on the rate of caesarean section, prolonged back pain, impact on the baby at birth, or number of infants requiring transfer to the neonatal intensive care unit.
Epidural anesthesia, compared with opioids, may have little or no effect on the rate of caesarean section, prolonged back pain, impact on the baby at birth, or number of infants requiring transfer to the neonatal intensive care unit.
Women who have had an epidural may have trouble urinating and may have a fever. There are highly variable outcomes such as longer labor, very low blood pressure, and inability to move for a period of time after delivery (motor block), likely due to the higher concentration of local anesthetic used in the epidural or due to the use of an epidural. infusions instead of dosed epidural administration of anesthetic at regular intervals. However, women who received opioid analgesics experienced some side effects, such as breathing so slow that they required oxygen masks, and severe nausea and vomiting. More babies whose mothers received opioids received antidotes to counteract the effects of opioids. There was no difference between women who received epidurals or opioid analgesics in terms of postpartum depression, headache, itching, chills, or drowsiness.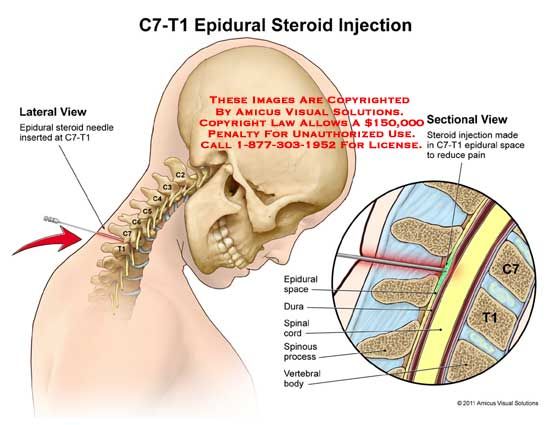
Women who received epidurals reported less pain than women who received placebo or no treatment or acustimulation. There were no reports of pain in trials that compared epidurals with inhaled analgesia or continuous support.
What does this mean?
Epidurals may reduce labor pain more effectively than any other form of pain relief and may increase maternal satisfaction with pain relief. However, some women who received epidurals instead of opioid analgesics were more likely to have assisted vaginal delivery, but this result probably reflects the higher concentrations of local anesthetics used traditionally instead of the low concentrations of modern local anesthetics for epidural anesthesia. Further research will be useful, with more consistent measures to reduce adverse outcomes associated with epidural anesthesia.
Translation notes:
Translation: Tashtanbekova Cholpon Bolotbekovna. Editing: Ziganshina Lilia Evgenievna. Project coordination for translation into Russian: Cochrane Russia - Cochrane Russia (branch of the Northern Cochrane Center on the basis of Kazan Federal University). For questions related to this translation, please contact us at: [email protected]; [email protected]
For questions related to this translation, please contact us at: [email protected]; [email protected]
Anesthesiology and resuscitation - Spinal anesthesia (SMA) close to home
Recording in 1 click
What is spinal anesthesia?
During spinal anesthesia, the pain-conducting nerves in certain areas are temporarily switched off. To do this, pain medication is injected at a specific location in the spine near these nerves.
How is spinal anesthesia performed?
- You can discuss in more detail how the spinal anesthesia is performed (if you wish) with the anesthesiologist before the operation.
- To perform this procedure, use one of the positions of the patient - sitting or lying on his side.
- The anesthesiologist selects the position required for spinal anesthesia. The anesthesiologist and his assistant will explain to you how to assume the required body position.
- In order to perform this type of anesthesia quickly and safely, please do not move or change your body position during the doctor's manipulations.
- After cleaning the injection site with a special disinfectant solution (which feels like a touch of something cold), the doctor gives an anesthetic injection of the puncture site.
- The manipulation itself is then carried out.
How will I feel?
- Spinal anesthesia is usually not uncomfortable and takes 10 to 15 minutes.
- After spinal anesthesia is performed and pain medication is administered, you may feel a slight tingling sensation in the legs (soles of the feet, lower legs), a feeling of “overflowing” heat. This is fine. And you should not be afraid of these sensations. Then there may be (but not necessarily) a feeling that your legs have become heavy and "naughty". Following these sensations, the sensation of pain disappears when touched by sharp objects in the area where the operation is planned to be performed.
- In some cases, when performing spinal anesthesia, you may feel some painful tingling, which some patients describe as "a little jolt of current." If this happens, tell the anesthesiologist about it without changing the position of the body and without turning the head.
Why Spinal Anesthesia?
Benefits of this type of anesthesia:
- Reduces the amount of blood lost during surgery. 2
- Less risk of postoperative complications such as thrombosis, pulmonary embolism.
- Less associated with surgery, unwanted effects and anesthesia on the heart and lungs.
- No pain at the end of the operation.
- Absence of weakness, feelings of nausea, vomiting.
- There are no such strict restrictions on the intake of drinks and food in the postoperative period.
- With spinal anesthesia, you can communicate with the anesthetist and surgeon before, during and after the operation.
If you wish, the anesthesiologist can make you sleep-like by injecting additional medication into your vein. But We do not recommend using this feature.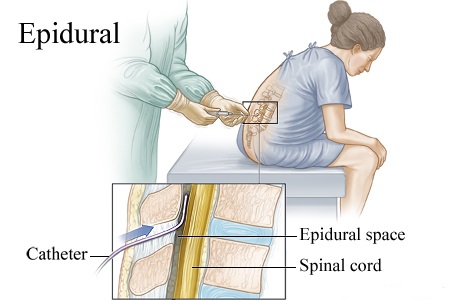
When may I need general anesthesia?
However, in some cases, despite spinal anesthesia, general anesthesia (anesthesia) may be required:
- If your anesthesiologist feels that the level of pain relief received is not sufficient to perform the operation
- Spinal anesthesia "does not work"
- The operation was more difficult than expected
At the end of spinal anesthesia
Full recovery of sensation in your body occurs within 1.5 to 4 hours (depending on the type of pain medication used).
Ask the people around you, the medical staff to help you at the first attempt to get up after the end of anesthesia on the first day (dizziness is possible).
After 30 - 60 minutes after the end of the operation, you can drink drinks, take easily digestible food in the evening - in agreement with the surgeon.
Side effects and adverse reactions
Regional anesthesia generally has less effect on the body than general anesthesia. Complications during spinal anesthesia are extremely rare. With anesthesia, the risk of complications depends on the individual case. The type and severity of the disease, as well as concomitant diseases, general condition, age, and bad habits matter. All activities in anesthesiology (eg, infusions ("droppers"), blood transfusions, placement of a catheter in a central vein, and subsequent treatment in the intensive care unit, etc.) carry risks. But the risk of developing complications does not mean that complications will definitely come. When we cross a road, we run the risk of being hit by a car, but not all pedestrians get into traffic accidents.
Please note!
- Do not eat or drink anything 6-8 hours before the operation!
- Do not smoke 6 hours before surgery!
- Remove removable dentures and contact lenses before surgery.
 If you have ocular prostheses, be sure to warn the anesthesiologist about this!
If you have ocular prostheses, be sure to warn the anesthesiologist about this! - Do not wear cosmetics or paint your nails before surgery.
- Remove earrings, rings, chains, other jewelry and wigs!
- For believers, it is allowed to leave a simple pectoral cross on a braid (not on a chain).
Failure to follow these rules greatly increases the risk of possible complications.
Please inform your anesthesiologist about all your chronic illnesses, surgeries, injuries, allergic reactions, intolerance to any medications, and any medications you have recently taken. This information can be very useful in preventing possible complications during anesthesia.