10 month old flu
Influenza (flu) and your baby
What is the flu?
Influenza (also called flu) is a virus that can cause serious illness. It’s more than just a runny nose and sore throat. It’s really important to protect babies and young children from the flu because it can make them very sick. In rare cases, flu can cause death. In 2017, the flu caused a record number of deaths in children. Most of the children who died didn’t get a flu vaccine.
How does the flu spread?
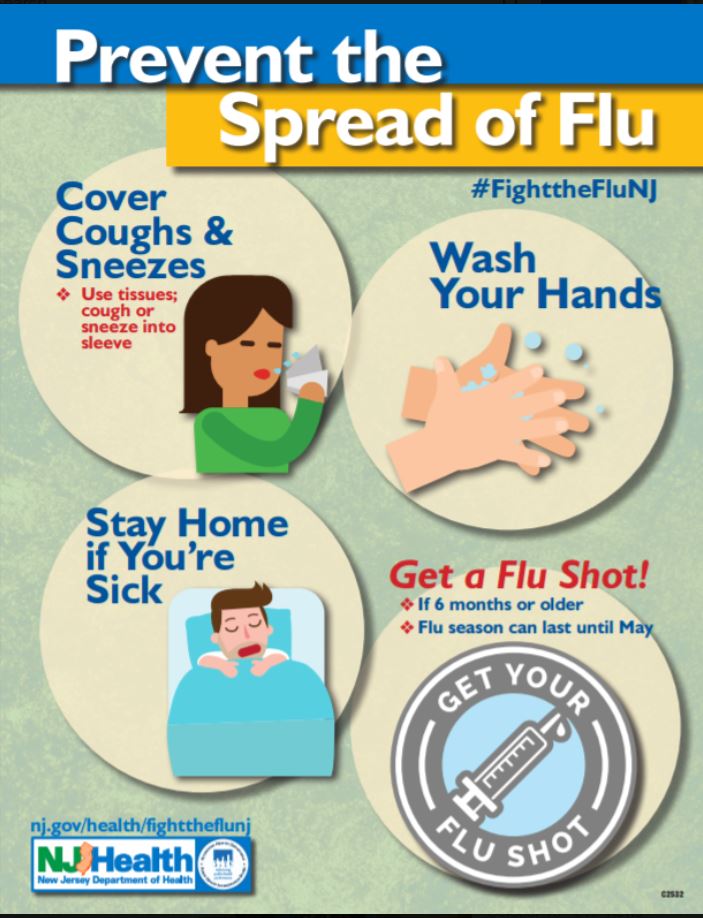
The flu spreads easily from person to person. When someone with the flu coughs, sneezes or speaks, the virus spreads through the air. Your baby can get infected with the flu if she breathes the virus in or if she touches something (like a toy) that has the flu virus on it and then touches her nose, eyes or mouth.
People with the flu may be able to infect others from 1 day before they get sick up to 5 to 7 days after. People who are very sick with the flu or young children may be able to spread the flu longer, especially if they still have symptoms.
Does your child need a flu vaccine every year?
Yes. The Centers for Disease Control and Prevention (also called CDC) and the American Academy of Pediatrics (also called AAP) recommend that everyone 6 months and older get the flu vaccine each year. It’s especially important for children younger than 5 to get it because they’re more likely than older kids to have serious health problems caused by the flu. The flu can be dangerous for all children, even healthy children.
The best way to protect your child from the flu is to make sure he gets a flu vaccine each year before flu season (October through May). Even though your child’s more likely to get the flu during flu season, he can get it any time of year.
There are two ways for your child to get the flu vaccine:
- Flu shot. Children 6 months and older can get the flu shot.
- Flu nasal spray. This is a spray your child’s provider puts in your child’s nose. Most children 2 years or older can get the flu nasal spray.
 But it’s not recommended for children who have certain health conditions, like asthma, heart and lung problems, or a weak immune system that doesn’t protect him well from infection. The flu nasal spray also isn’t recommended for children who take certain medicines for a long time, like aspirin (called long-term aspirin therapy).
But it’s not recommended for children who have certain health conditions, like asthma, heart and lung problems, or a weak immune system that doesn’t protect him well from infection. The flu nasal spray also isn’t recommended for children who take certain medicines for a long time, like aspirin (called long-term aspirin therapy).
The first time your baby gets the flu vaccine, he gets two doses to give him the best protection from the flu. Your child gets one dose of the vaccine every year after.
If you’re not sure which vaccine is best for your child, ask his health care provider. Visit flu.gov to learn more about flu vaccines.
The flu vaccine is safe for most children, even babies born prematurely (before 37 weeks of pregnancy). But if your child had a bad reaction to the flu vaccine in the past, tell his provider. The provider may want to watch your child closely after getting the vaccine to check for a reaction. If your child is allergic to eggs, talk to his provider to decide if it’s OK to get the flu vaccine. Some flu vaccines are made from eggs.
Some flu vaccines are made from eggs.
There are many different flu viruses, and they’re always changing. Each year a new flu vaccine is made to protect against three or four flu viruses that are likely to make people sick during the upcoming flu season. With the vaccine, protection from the flu lasts about a year, so it’s important to get your child vaccinated each year. You get the vaccine from his provider or from other places, like pharmacies, that offer it. Use the HealthMap Vaccine Finder to find out where you can get a flu vaccine for your child.
Are some children more likely to have serious health problems caused by flu than others?
Yes. Babies and children younger than 5 years old—and especially those younger than 2 years old-- are more likely than older children to have complications from the flu. Premature babies also are at increased risk of serious complications from flu. The CDC recommends that premature babies get most vaccines, including the flu vaccine, according to their chronological age (the time since birth). Even if a baby is born small or with a low birthweight, she can get her vaccine at the same time as other babies who are the same age. If you have a premature baby, talk your baby’s provider to make sure your baby gets the flu vaccine on time. Children with chronic health conditions, like asthma, heart disease or blood disorders, also are at high risk of flu complications.
Even if a baby is born small or with a low birthweight, she can get her vaccine at the same time as other babies who are the same age. If you have a premature baby, talk your baby’s provider to make sure your baby gets the flu vaccine on time. Children with chronic health conditions, like asthma, heart disease or blood disorders, also are at high risk of flu complications.
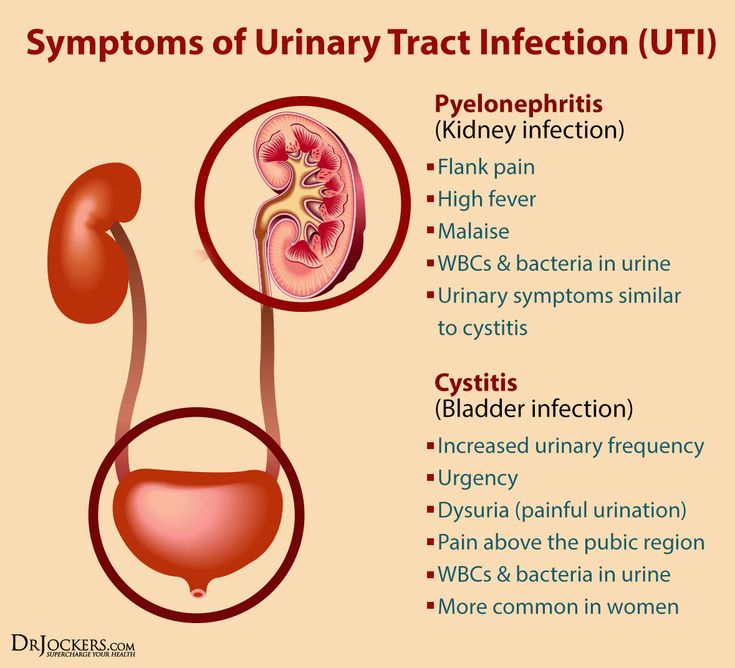
What health problems can flu cause in children?
Complications from flu in children younger than 5 years old include:
- Making chronic health conditions, like heart disease or asthma, worse
- Brain problems, like encephalopathy. Encephalopathy is any brain disease that affects the brain’s structure or how the brain works.
- Dehydration. This means not having enough water in your body.
- Pneumonia. This is an infection in one or both lungs.
- Sinus problems and ear infections. Sinuses are hollow air spaces within the bones around the nose. Sinus infections can happen when fluid builds up in the sinuses.

- Death. Flu complications can sometimes lead to death, but this is rare.
What are signs and symptoms that your baby has the flu?
Signs of a condition are things someone else can see or know about you, like you have a rash or you’re coughing. Symptoms are things you feel yourself that others can’t see, like having a sore throat or feeling dizzy. If your baby has any of these signs and symptoms of the flu, call his health care provider right away or take him to see his provider:
- Being very tired or sleepy (also called fatigue)
- Cough
- Fever (100 F or above), chills or body shakes. Not everyone who has the flu has a fever.
- Headache, or muscle or body aches
- Runny or stuffy nose
- Sore throat
- Vomiting (throwing up) or diarrhea
The flu often comes on quickly. Fever and most other signs and symptoms can last a week or longer. While your baby can’t tell you how she’s feeling, babies who have the flu often are sicker, fussier and seem more uncomfortable and unhappy than babies with a common cold. If you think your baby has the flu even if she got a flu vaccine, call her health care provider.
If you think your baby has the flu even if she got a flu vaccine, call her health care provider.
If your baby has any of these signs or symptoms, take her to a hospital emergency room:
- Being so fussy that she doesn’t want to be held
- Bluish color of lips or face
- Chronic health conditions, like asthma, get worse
- Fast breathing, trouble breathing, chest pain or ribs pulling in with each breath
- Fever in a baby younger than 12 weeks old, fever above 104 F in older babies or children, or fever with a rash
- Fever or cough that gets better but then returns and gets worse
- Having seizures. A seizure is when the whole body or parts of the body move without control.
- Not drinking enough fluids or not making as much urine as she normally does. If your baby doesn’t make urine for 8 hours, has a dry mouth or doesn’t make tears when crying, she may be dehydrated.
- Not waking up, or not being alert or interacting with you when she is awake
- Severe muscle pain.
 It may be so severe your child can’t walk.
It may be so severe your child can’t walk. - Vomiting (throwing up) that’s severe or doesn’t stop
How is flu treated in babies and children?
Your baby’s provider may prescribe an antiviral medicine to prevent or treat the flu. An antiviral is a medicine that kills infections caused by viruses. Antivirals can make your baby’s flu milder and help your baby feel better faster. Antivirals also can help prevent serious flu complications, like a lung infection called pneumonia. For flu, antivirals work best if used within 2 days of having signs or symptoms.
If your baby is at high risk for flu, his provider may prescribe an antiviral as soon as he begins to have flu symptoms. All children younger than 5 are at high risk for flu, especially children younger than 2. Children who were born prematurely or who have chronic health conditions, like asthma or sickle cell disease, also are at high risk.
Three medicines are approved in the United States for preventing or treating the flu in children:
- Oseltamivir (Tamiflu®) for children as young as 2 weeks.
 This medicine comes as a capsule or liquid.
This medicine comes as a capsule or liquid. - Zanamivir (Relenza®) for children at least 5 years old. This medicine is a powder that your child breathes in by mouth. It isn’t recommended for people with breathing problems, like asthma.
- Peramivir (Rapivab®) for children at least 2 years old. This medicine is given through a needle into a vein (also called IV) by a health care provider.
If your child has the flu, help him get lots of rest and drink plenty of fluids. He may not want to eat much. Try giving him small meals to help his body get better.
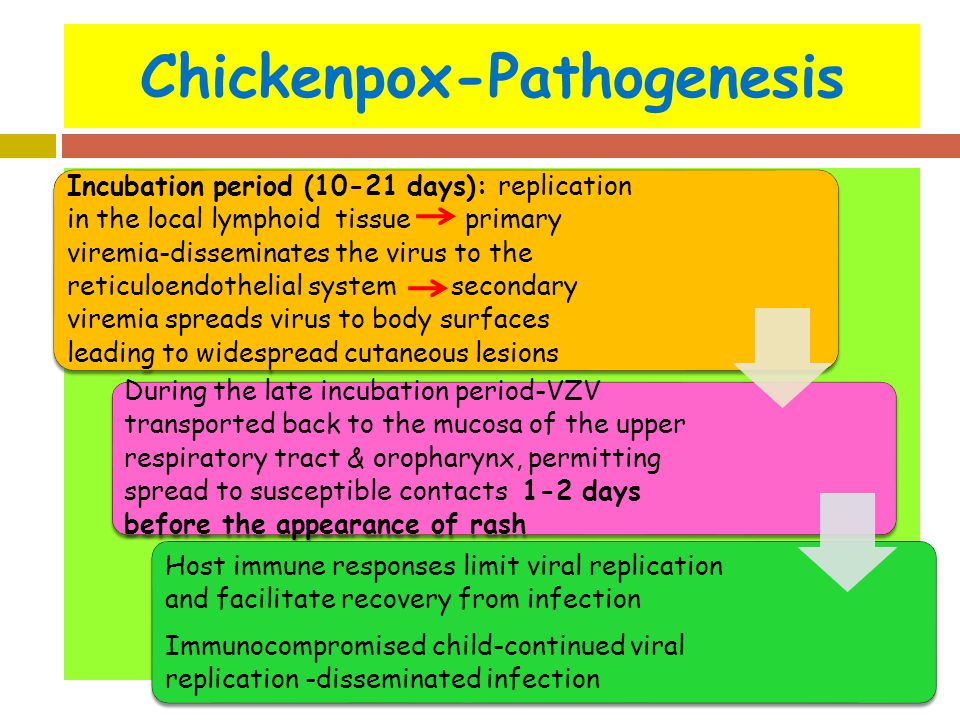
If your baby seems uncomfortable from a fever, ask her provider if you can give her infant’s or children’s acetaminophen (Tylenol®) or ibuprofen (Motrin® or Advil®). Don’t give her aspirin without checking with her health care provider. Aspirin can cause a rare but life-threatening liver disorder called Reye syndrome in children with certain illnesses, such as colds, the flu and chickenpox.
If your baby has a cough or a cold, don’t give her over-the-counter cough and cold medicine. These are medicines you can buy without a prescription from a health care provider. AAP says these medicines can cause serious health problems for children. Talk to your baby’s provider before you give your baby any kind of medicine.
These are medicines you can buy without a prescription from a health care provider. AAP says these medicines can cause serious health problems for children. Talk to your baby’s provider before you give your baby any kind of medicine.
How can you stop the flu from spreading?
Everyone 6 months and older needs to get a flu vaccine. This means you, especially if you have or take care of a baby younger than 6 months. Getting a flu vaccine can help keep you from spreading the flu.
If you or your child has the flu, you can spread it to others. Here’s how to help prevent the flu from spreading:
- Keep your child home from day care, school or camp for at least 24 hours after her fever (100 F or higher) is gone. The fever should be gone without using a medicine that lowers fever.
- Avoid contact with other people.
- Don’t kiss your baby and avoid touching your eyes, nose and mouth.
- Teach your child to cough or sneeze into a tissue or his arm.
 Throw used tissues in the trash.
Throw used tissues in the trash. - Wash your hands with soap and water before and after caring for your baby. You also can use alcohol-based hand sanitizers. Use enough hand sanitizer so that it takes at least 15 seconds for your hands to dry.
- Clean surfaces and toys that may have the flu virus on them.
- Use hot, soapy water or a dishwasher to clean your baby’s dishes and utensils.
- Don’t share any of your baby’s dishes, glasses, utensils or his toothbrush.
More information
Flu.gov
See also: Flu and pregnancy, Your baby’s vaccinations
Last reviewed: September, 2019
Flu Symptoms: When To Bring Your Child Into The Emergency Center
COVID-19 Updates: Get the latest on vaccine information, in-person appointments, video visits and more. Learn More >>
Latest Blog Posts
Swimming with the Sharks….!
Young Woman’s Battle With Autoimmune Disease Inspires her to be a Voice for Others
Doing What He Loves To Do
Standing Tall: Toddler Takes First Steps While Fighting Cancer
Young Cancer Patient Runs Past Milestones at Texas Children’s Hospital
- Home
- Texas Children's Blog
We are in the midst of one of the most severe flu seasons in a decade. Texas Children’s alongside hospitals across the nation have seen a major jump in flu-related emergency center visits over the past several weeks. It’s important for parents to understand when they should or shouldn’t bring their child into an emergency center with flu-like symptoms. The flu can cause a variety of symptoms and effects, ranging from mild to severe. Most healthy people, including children, can recover from the flu without complications, and don't need to go to the emergency center or seek hospitalization. Symptoms of the flu can include:
Symptoms of the flu can include:
- Fever or chills
- Headaches
- Fatigue
- Coughing
- Sore throat
- Runny or stuffy nose
- Body aches
- Diarrhea
- Vomiting
A child with these regular flu-like symptoms can usually be cared for at home with fever-reducing medication, like Tylenol or Ibuprofen, clear fluids and bed rest. If diagnosed early enough, some children might benefit from Tamiflu, a medication that requires a prescription from your pediatrician. To ensure your child has fully recovered from the flu, he/she should stay home for at least 24 hours after the fever is gone. If your child's flu-like symptoms return and worsen, or if your child is at high risk for developing flu-related complications (he/she is younger than 2 years old or has a chronic condition like asthma, epilepsy, lung disease, heart disease, sickle cell disease, cancer, etc.), call your child’s pediatrician to seek evaluation.
Click here to schedule an appointment online.
You should seek immediate medical care in an emergency center if your child exhibits any of these core warning signs:
- Return of flu-like symptoms with worsened fever, cough
- Fast or troubled breathing
- Cyanosis, a bluish discoloration of the skin
- Dehydration, a lack of fluid consumption (no tears with crying, dry lips and mouth, no urination in more than eight hours)
- Severe lethargy
- Irritability
In adults, core warning signs signaling a need for urgent medical attention include:
- Return of flu-like symptoms with worsened fever, cough
- Difficulty breathing, or shortness of breath
- Pain or pressure in the chest or abdomen
- Sudden dizziness
- Confusion or altered mental state
- Severe or persistent vomiting
Just remember: Although most flu-related illnesses can be treated at home, please seek immediate medical care if you're especially concerned about your child’s health, or if your child exhibits any of the core warning signs. The flu vaccine is the best way to protect yourself and your family from flu infection. It isn't too late to get your flu shot!
The flu vaccine is the best way to protect yourself and your family from flu infection. It isn't too late to get your flu shot!
Why I give my kids the flu shot
Flu symptoms? Where to go, and when
10 common myths regarding the influenza (flu) vaccine
Author
Katherine Leaming-Van Zandt, MD
Influenza in children
Children get the flu 4-5 times more often than adults. This is because their immune system is imperfect. Children of the first 3 years of age have the most severe course and a high risk of complications at any time from the onset of the disease. Children of large cities attending children's organized groups (kindergartens, schools, sports clubs) are at particular risk. In children living in big cities, immunity can be reduced due to polluted air and malnutrition.
Influenza is an acute, highly contagious infectious disease that affects the upper and lower respiratory tract and is caused by a virus.
The influenza virus is transmitted by airborne droplets through coughing, sneezing and talking and is highly contagious. It is very easily transmitted when children are in the same room for a long time.
The incubation period (the period from the moment of infection to the onset of the first symptoms) is from 1 to 5 days.
Flu symptoms :
- The disease develops rapidly, acutely with the onset of chills and fever from 38.5 to 40 gr. during the first day
- In children of the first year of life at the peak of fever, convulsions may occur
- Headache
- Pain and pain in the eyeballs
- Pain in the joints, muscles
- Decreased appetite
- Severe weakness In young children
- marbling of the skin, pallor
- May present with catarrhal symptoms such as runny nose, sore throat, dry cough
- Breastfeeding, restlessness, sleep and wake disturbances may occur in infants.

Risk groups:
- Children of the neonatal period
- Children of the first six months of life
- Children attending preschool institutions
.
- From 6 months to 5 years the course of the disease can be very severe with the development of encephalitis.
Complications
Most often influenza is complicated by inflammation of the lungs (pneumonia), bronchitis, and damage to the nervous system. Otitis, sinusitis, inflammation of the heart muscle (myocarditis). In the worst case, inflammation of the brain and its membranes may develop.
It is not uncommon for children to develop laryngotracheitis, which can lead to false croup (an attack of suffocation that causes the airways to close). False croup can be fatal.
Joint complications such as rheumatoid arthritis are also possible, which leads to limited mobility and deformity of the joints.
Treatment of influenza in children
If a child is ill, the first thing to do is to see a doctor. During treatment for influenza, the following guidelines should be followed:
During treatment for influenza, the following guidelines should be followed:
- Follow your doctor's instructions
- Take medication
- Stay in bed
- Drink plenty of water (liquid speeds up the elimination of toxins that are formed during the vital activity of viruses)
- Don't force your child to eat if he doesn't want to. Appetite decreases during the flu. It is necessary to follow a diet (light meals in small portions)
- Do not wrap the child
- It is necessary to ventilate the children's room as often as possible.
Most often, influenza is treated at home, but sometimes it becomes necessary to hospitalize the child in a hospital in case of a severe course of the disease or the development of a complication.
Prevention of influenza in children:
The main type of influenza prevention in children is vaccination. It is indicated for children attending preschool institutions, children who often suffer from colds, children with chronic diseases of the cardiovascular and respiratory systems. Vaccination is carried out from the beginning of autumn. Vaccination helps to develop immunity against the influenza virus. Even if a vaccinated child becomes ill, he will have a mild illness, and the chance of complications in such children is small. Vaccination can be used in children from 6 months. Vaccination should be done annually.
Vaccination is carried out from the beginning of autumn. Vaccination helps to develop immunity against the influenza virus. Even if a vaccinated child becomes ill, he will have a mild illness, and the chance of complications in such children is small. Vaccination can be used in children from 6 months. Vaccination should be done annually.
In addition to vaccination, there are other methods of prevention aimed at improving immunity, such as walking in the fresh air. Physical development, hardening.
Before visiting schools, kindergartens, polyclinics, it is recommended to lubricate the nose with oxolin ointment.
It is recommended to avoid crowded places.
Hands should be washed frequently and thoroughly. Do not touch your face with dirty hands, there may be virus particles on your hands.
If there is a sick person in the house, it is necessary:
- Isolate the patient with influenza in a separate room
- Regularly ventilate the room where the patient is located
- When caring for the sick, use a medical mask
- Wash hands with soap after each contact
- Perform wet cleaning daily.

Dear parents, watch your child's health! At the slightest sign of a viral infection - consult a doctor!
A cold in a child: how to treat it correctly
Many parents are ready for their babies to catch common infections, including seasonal infections, which is typical for childhood. Some parents study the methods of treating ARVI and colds in advance, read about it from experienced mothers in blogs and diaries, consult with doctors they know, and watch medical programs. But even despite the fact that the child's body from birth has a powerful immune system, this protection is imperfect. Therefore, no matter how informed the mother is, when the child becomes ill, she has a lot of questions that require qualified answers.
What is ARI and ARVI
Most often, children are faced with acute respiratory diseases, abbreviated as acute respiratory infections or colds. This is especially evident when visiting children's groups, where they come into contact with other kids, and actually exchange various pathogens. The mothers of "kindergarten" children are very familiar with the phrase: "We go for 2 days, then 2 weeks - on sick leave."
This is especially evident when visiting children's groups, where they come into contact with other kids, and actually exchange various pathogens. The mothers of "kindergarten" children are very familiar with the phrase: "We go for 2 days, then 2 weeks - on sick leave."
A cold can be both viral and bacterial, even fungal and of a different nature, in 70-80% of cases it is of a viral nature. It is impossible to establish the origin of a cold with accuracy on a pediatric examination, as well as “by eye” to distinguish one infection from another. However, there are certain signs that indicate the action of viruses, harmful bacteria and other pathogens. For example, nasal mucus is indicative of an acute respiratory viral infection, which usually begins with mild malaise, decreased appetite, moodiness, and sleep disturbance in a child. This is a prodromal period, it lasts from several hours to 1-2 days. And such a viral infection as the flu begins acutely, immediately with a very high temperature, intoxication, there is almost no prodromal period, dry cough appears in the late stages of the disease. Often SARS passes with catarrhal symptoms: nasal congestion, change in tone of voice, "circles", "blue" under the eyes, runny nose, discharge from the nose, cough, sore throat and swallowing.
Often SARS passes with catarrhal symptoms: nasal congestion, change in tone of voice, "circles", "blue" under the eyes, runny nose, discharge from the nose, cough, sore throat and swallowing.
What to do?
First of all, you need to remember that parents should not panic if the child has a fever and other unpleasant symptoms of a cold. Any mood of the mother is transmitted to the baby. A cold with a competent approach is simply MUST pass in 5-7 days without complications. And it is important to know that the treatment of a cold is complex, which includes the main drugs - antiviral, antibacterial, etc., as well as symptomatic therapy. You should not rely on just one medicine as a panacea, a magic pill from advertising or the advice of a pharmacy worker.
How to treat?
Antivirals. Now there is a lot of false information regarding antiviral drugs. They are credited with mythical side effects and actions. If this comes from a doctor, then he must provide data confirming his point of view in official sources, which are state medical institutions, major scientific journals.
Antibiotics. As for antibiotics, their use is currently limited by very clear indications, contraindications, age of the patient, etc. In addition, antibiotics, especially with uncontrolled, frequent use, contribute to the formation of new strains of harmful bacteria that are difficult to treat. Usually, against the background of antibiotic treatment, it is customary to prescribe biological products - live microbes that make up the human intestinal microflora. But there is an opinion that the antibiotic has a detrimental effect on these bacteria, and such therapy does not bring the desired result.
Auxiliaries . In the treatment of colds of any origin, symptomatic therapy is used, the action of which is directed against the symptoms of the disease. They are called auxiliary, as they help to alleviate the course of a cold. They do not get rid of the cause of ARVI, but the child's own antibodies work against viruses.
How to treat a runny nose? In case of a runny nose, a nasal toilet with saline solutions is performed. The procedure is simple, but requires certain skills and care. To do this, you should seat the child with his back to him, first clean his nose. In babies, this can be done with cotton buds (in children under six months old, only with ordinary cotton turundas), and at an older age, children can already blow their nose. After that, you need to raise the chin, holding the child's face with his palm in a raised position. Using a pipette, drip saline solution into both nasal passages, lower the child's head forward. Part of the medicine may spill out of the nose, but the result of such a procedure will still be achieved. If there are no special recommendations from the pediatrician of the sick child, you can use a pipette and normal saline. But preferably a sterile solution based on sea water. It is a delusion to think that washing a child's nose will be addictive or the snot will flow out on its own. Part, of course, can leak out, but if you do not clean your nose, there is a high risk of infection spreading to the lower respiratory tract, the development of complications such as inflammation of the trachea, bronchi, and lungs.
The procedure is simple, but requires certain skills and care. To do this, you should seat the child with his back to him, first clean his nose. In babies, this can be done with cotton buds (in children under six months old, only with ordinary cotton turundas), and at an older age, children can already blow their nose. After that, you need to raise the chin, holding the child's face with his palm in a raised position. Using a pipette, drip saline solution into both nasal passages, lower the child's head forward. Part of the medicine may spill out of the nose, but the result of such a procedure will still be achieved. If there are no special recommendations from the pediatrician of the sick child, you can use a pipette and normal saline. But preferably a sterile solution based on sea water. It is a delusion to think that washing a child's nose will be addictive or the snot will flow out on its own. Part, of course, can leak out, but if you do not clean your nose, there is a high risk of infection spreading to the lower respiratory tract, the development of complications such as inflammation of the trachea, bronchi, and lungs.
If the runny nose is profuse, watery, painful, accompanied by nasal congestion, vasoconstrictor drugs (based on oxymetazoline, xylometazoline) are used in the form of drops at bedtime, before walking with the child. This helps the baby to have a good rest in a dream without waking up, and on a walk it is normal to breathe through the nose without taking cold air into the mouth. It should not be instilled into the nose of a child in a supine state, since there is a high probability of a change in pressure during such manipulation and there is a risk of otitis media. All instillations must be done while sitting. The use of special preparations in the form of soft (spray with limited jet pressure) should be carried out with great care, since there is also a risk of promoting the spread of infection under pressure.
Antipyretics . Often there are questions about the use of antipyretics, for children - these are drugs based on paracetamol or ibuprofen, for babies - in syrup, suppositories. It should be noted that if there are no special recommendations in this regard, it is necessary to reduce the temperature above 38.3 - 38.5 ° С. If the child feels well, plays, has an appetite, and, in general, tolerates temperature well, antipyretic drugs can not be used. If the parents see that the child's condition is bad, he refuses to eat and drink, becomes lethargic, vomiting occurs, headache, the temperature rises further, you can start giving antipyretics even at a low temperature.
It should be noted that if there are no special recommendations in this regard, it is necessary to reduce the temperature above 38.3 - 38.5 ° С. If the child feels well, plays, has an appetite, and, in general, tolerates temperature well, antipyretic drugs can not be used. If the parents see that the child's condition is bad, he refuses to eat and drink, becomes lethargic, vomiting occurs, headache, the temperature rises further, you can start giving antipyretics even at a low temperature.
How to treat a cough? Questions about cough are the most frequent and sometimes the most difficult at pediatric appointments for SARS. It is best if the doctor dynamically observes the coughing child. In this case, the specialist can distinguish changes in the tone of the voice, a barking component, a dry or wet cough, wheezing, localization of wheezing. If the pediatrician recommends taking an x-ray, you should not refuse such an examination, this will help to make the correct diagnosis and prescribe adequate treatment. Currently, in the treatment of cough, inhalation drugs are widely used - through a special device - an inhaler. This tactic reduces the systemic effect of the drug on the child's body, where the drug reaches the point of its application - large and medium bronchi, and even alveoli. Inhalers can be used from the very birth of a child, but it is necessary to pay attention to the type of device, the medicinal substances recommended for it, their dosages and the frequency of use.
Currently, in the treatment of cough, inhalation drugs are widely used - through a special device - an inhaler. This tactic reduces the systemic effect of the drug on the child's body, where the drug reaches the point of its application - large and medium bronchi, and even alveoli. Inhalers can be used from the very birth of a child, but it is necessary to pay attention to the type of device, the medicinal substances recommended for it, their dosages and the frequency of use.
Activities before the doctor arrives
Sometimes, especially during the season of high incidence of flu and colds, there are difficulties with a doctor's visit, you have to wait for an appointment, the doctor does not have time to come as quickly as parents would like. There are steps that can be taken before the arrival of a specialist. It is necessary to measure the temperature of the child and write down the data on the thermometry performed in a diary, which is then shown to the doctor.