Leg pain symptoms of pregnancy
Treatment, Home Remedies, and Prevention
Pregnancy isn’t always a cakewalk. Sure, we hear how beautiful it is (and it is!), but your first months may have been filled with morning sickness and heartburn. And just when you think you’re out of the woods, leg cramps come along.
Leg cramps are a common pregnancy symptom that usually occurs in the second and third trimester. In fact, nearly half of all pregnant women report muscle spasms by the third trimester.
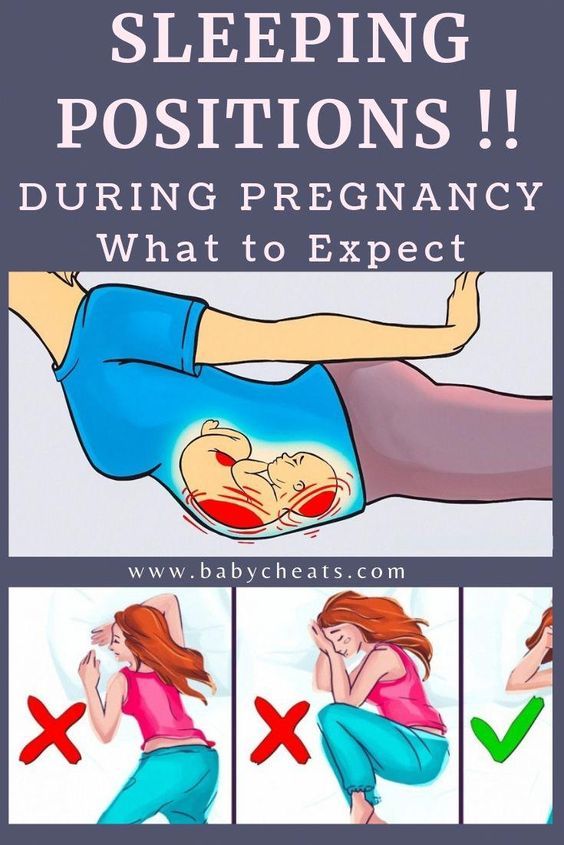
You may experience these cramps mainly at night — just when you’d like to get the sleep you’re probably craving — and feel tightness in your calf, foot, or both areas. Some women also experience them after sitting in one position for an extended amount of time.
It may not be possible to entirely prevent leg cramps. But preventative and relief measures like stretching, staying active, and drinking plenty of water may help ease your symptoms and get your mind back on the true joys of pregnancy.
Let’s start by talking about what causes these cramps, because knowledge is power when it comes to getting relief.
Circulation changes
During pregnancy, circulation slows — this is totally normal and not a reason to worry. It’s due in part to overactive hormones. (You probably know by now that hormones are gifts that keep on giving for the whole 40 weeks — and beyond.)
During later trimesters, your body also experiences an increase in blood volume, which also contributes to slow circulation. This can lead to swelling and cramping in your legs.
Tips for improving circulation while pregnant
- Try sleeping on your left side.
- Elevate your legs as often as possible — literally, find the time to put your feet up and relax if you can.
- At night, place a pillow under or between your legs.
- During the day, stand up and walk around every hour or two — especially if you have a job that keeps you at a desk all day.
Dehydration
Quick check: Are you drinking enough water?
During pregnancy, you’re ideally drinking 8 to 12 cups of water each day. Watch out for symptoms of dehydration, like dark yellow pee (it should be clear or nearly clear).
Watch out for symptoms of dehydration, like dark yellow pee (it should be clear or nearly clear).
Dehydration can cause and worsen leg cramps. If you’re experiencing them, try upping your daily water intake.
Weight gain
The pressure from your growing baby can take a toll on your nerves and blood vessels, including the ones that go to your legs. This is why you’re more likely to experience leg cramps as your pregnancy progresses, especially in the third trimester.
Gaining a healthy amount of weight and staying active during your pregnancy may help prevent leg cramps. Talk to your healthcare provider if you’re concerned.
Fatigue
It’s the norm to feel tired during pregnancy — you’re growing a tiny human! — and this is especially true as you gain more weight in the second and third trimester. As your muscles get fatigued from the added pressure, too, it can lead to leg cramps.
Try drinking plenty of water, going for a walk during the day, and stretching before bed to prevent leg cramps due to muscle fatigue.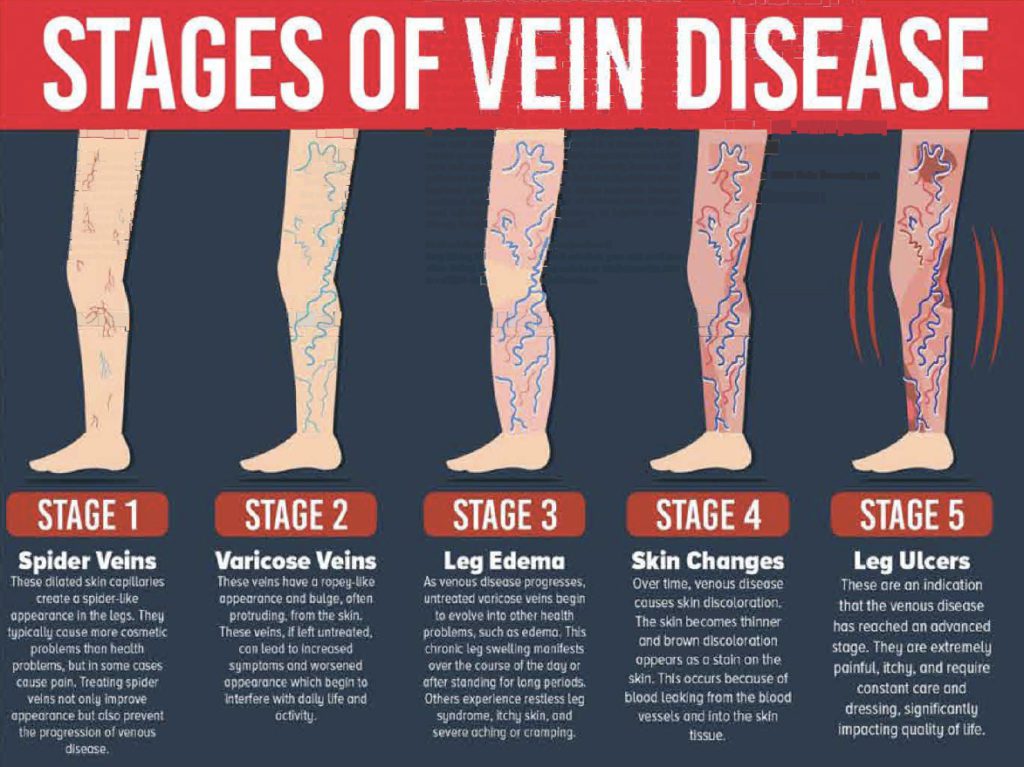
Calcium or magnesium deficiency
Having too little calcium or magnesium in your diet may contribute to leg cramps.
But if you already take a prenatal vitamin, you likely don’t need to take an additional supplement. A 2015 review of studies of 390 pregnant women found that taking magnesium or calcium supplements made little to no difference when it came to experiencing leg cramps.
If you’re concerned you aren’t getting enough of these nutrients, speak to your doctor. You’re probably getting labs done occasionally anyway, so it doesn’t hurt to have these levels checked.
DVT blood clot
A deep vein thrombosis (DVT) blood clot can occur in the legs, thigh, or pelvis. Pregnant women are 5 to 10 times more likely to develop a DVT than non-pregnant women. While there’s no need to panic that you’ll get one — it’s pretty uncommon to start with — we can’t say enough that knowledge is power.
Bottom line: Keep moving. We’re not talking marathons here, but the best way to prevent DVT during pregnancy is to avoid hours at a time of inactivity.
If your job requires a lot of sitting, you could set a quiet alarm on your phone to go off every hour to remind you to get up and walk — perhaps to the water cooler to add to your water intake for the day! Two birds, one stone.
Also take extra care to get up during long flights. You may want to check with your doctor before flying while pregnant.
Symptoms of a blood clot are similar to leg cramps, but a DVT blood clot is a medical emergency. Seek medical care right away if you experience symptoms like:
- a lot of pain in your legs when you’re standing or moving around
- severe swelling
- warm-to-the-touch skin near the affected area
Stretching before bed
Performing a calf stretch before getting into bed at night may help prevent or ease leg cramps. Follow these steps:
- Stand facing a wall, an arm’s length away.
- Place your hands on the wall in front of you.
- Step your right foot back. Keep your heels on the floor the whole time and bend your left knee while keeping your right leg straight.
 Keep your left knee bent as so you feel the stretch in your right calf muscle.
Keep your left knee bent as so you feel the stretch in your right calf muscle. - Hold for up to 30 seconds. Switch legs, if needed.
Staying hydrated
Drinking plenty of water during pregnancy is important to prevent dehydration — and dehydration can also lead to those awful leg cramps.
Try to drink 8 to 12 cups of water each day during pregnancy. Easier said than done, sure — but super important for a lot of good reasons.
Applying heat
Try applying heat to your cramping muscle. It may help loosen up the cramp. No need to buy a fancy heating pad: You can also use a microwave-safe cloth bag (or a sock) filled with rice.
Massaging the area
When you get a leg cramp, performing a self-massage may help ease your pain. Use one hand to gently massage your calf or wherever your leg is cramping. Perform this self-massage for 30 seconds to a minute to ease your cramp.
You can also get a prenatal massage, which can be a positively divine experience. Look for an experienced therapist in your area who specializes in working with pregnant women.
Look for an experienced therapist in your area who specializes in working with pregnant women.
Exercising
It’s a smart idea to stay active throughout your pregnancy, even though you don’t want to overdo it.
With your doctor’s OK, pregnancy-safe activities like prenatal yoga, walking, and swimming can benefit you and your baby-to-be.
Staying active can prevent excess weight gain, promote circulation, and yes — help prevent leg cramps. Always stretch and warm up before and after exercising so your muscles don’t cramp up afterward, though.
Avoiding inactivity
So, perhaps you don’t have the time or energy for a challenging hike or run. That is more than OK — you need to listen to your body and know your limits, especially during pregnancy.
But sitting for long periods of time can lead to leg and muscle cramps. To avoid this, make sure you stand up and walk around every hour or two. Set a timer on your phone or watch if you tend to forget to get up during the day.
Leg cramps are a common pregnancy symptom. (That doesn’t make having them any easier, but hopefully it turns down the stress dial a bit.)
If you’re concerned about your pain or they’re causing too much lost shut-eye, mention it at your next prenatal checkup.
Also call your doctor and let them know if your leg cramps are severe, persistent, or worsening. You may need supplements or medication.
Seek medical help immediately if you experience severe swelling in one or both legs, pain walking, or enlarged veins. These may be symptoms of a blood clot.
The straight answer here is that there is no straight answer. (Great.)
Leg cramps are most common in the second and third trimester of pregnancy, not the first. But changing symptoms are a valid reason to wonder if you’re pregnant.
Some women do report aches and pains during the first trimester. This is likely due to your hormonal changes and your expanding uterus.
Leg cramps alone can’t tell you if you’re pregnant. If you suspect you’re pregnant or miss your period, take an at-home pregnancy test or see your doctor to confirm.
If you suspect you’re pregnant or miss your period, take an at-home pregnancy test or see your doctor to confirm.
To prevent leg cramps, try the following:
- Drink between 8 and 12 cups of water per day.
- Stay active throughout your pregnancy.
- Stretch out your calf muscles.
- Wear comfortable shoes — leave the heels at home!
- Eat a balanced diet with calcium- and magnesium-rich foods like yogurt, leafy greens, whole grains, dried fruit, nuts, and seeds
Experiencing leg cramps during pregnancy isn’t pleasant. But it’s a common symptom, especially at night. Try our tips — we think they’ll help.
And as always, let your doctor know if you have any related worries. Never feel bad or self-conscious about phoning or emailing your clinic — helping you through a healthy pregnancy is the number one concern of OB doctors and nurses.
Treatment, Home Remedies, and Prevention
Pregnancy isn’t always a cakewalk. Sure, we hear how beautiful it is (and it is!), but your first months may have been filled with morning sickness and heartburn. And just when you think you’re out of the woods, leg cramps come along.
And just when you think you’re out of the woods, leg cramps come along.
Leg cramps are a common pregnancy symptom that usually occurs in the second and third trimester. In fact, nearly half of all pregnant women report muscle spasms by the third trimester.
You may experience these cramps mainly at night — just when you’d like to get the sleep you’re probably craving — and feel tightness in your calf, foot, or both areas. Some women also experience them after sitting in one position for an extended amount of time.
It may not be possible to entirely prevent leg cramps. But preventative and relief measures like stretching, staying active, and drinking plenty of water may help ease your symptoms and get your mind back on the true joys of pregnancy.
Let’s start by talking about what causes these cramps, because knowledge is power when it comes to getting relief.
Circulation changes
During pregnancy, circulation slows — this is totally normal and not a reason to worry. It’s due in part to overactive hormones. (You probably know by now that hormones are gifts that keep on giving for the whole 40 weeks — and beyond.)
It’s due in part to overactive hormones. (You probably know by now that hormones are gifts that keep on giving for the whole 40 weeks — and beyond.)
During later trimesters, your body also experiences an increase in blood volume, which also contributes to slow circulation. This can lead to swelling and cramping in your legs.
Tips for improving circulation while pregnant
- Try sleeping on your left side.
- Elevate your legs as often as possible — literally, find the time to put your feet up and relax if you can.
- At night, place a pillow under or between your legs.
- During the day, stand up and walk around every hour or two — especially if you have a job that keeps you at a desk all day.
Dehydration
Quick check: Are you drinking enough water?
During pregnancy, you’re ideally drinking 8 to 12 cups of water each day. Watch out for symptoms of dehydration, like dark yellow pee (it should be clear or nearly clear).
Dehydration can cause and worsen leg cramps. If you’re experiencing them, try upping your daily water intake.
Weight gain
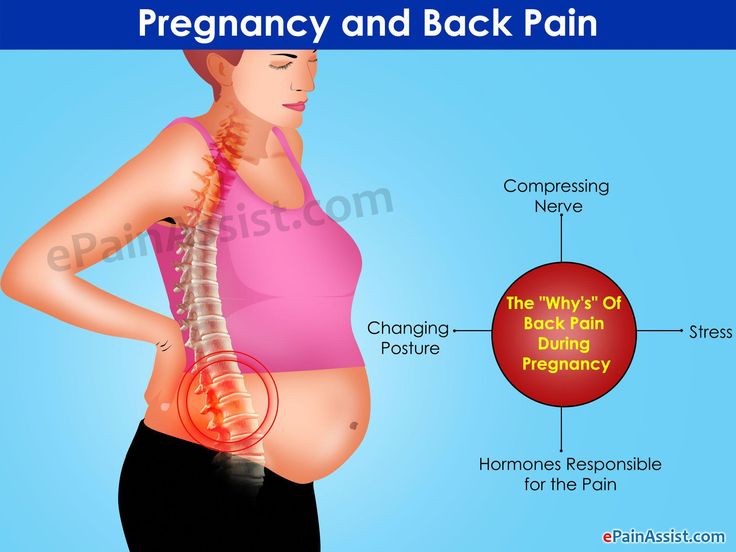
The pressure from your growing baby can take a toll on your nerves and blood vessels, including the ones that go to your legs. This is why you’re more likely to experience leg cramps as your pregnancy progresses, especially in the third trimester.
Gaining a healthy amount of weight and staying active during your pregnancy may help prevent leg cramps. Talk to your healthcare provider if you’re concerned.
Fatigue
It’s the norm to feel tired during pregnancy — you’re growing a tiny human! — and this is especially true as you gain more weight in the second and third trimester. As your muscles get fatigued from the added pressure, too, it can lead to leg cramps.
Try drinking plenty of water, going for a walk during the day, and stretching before bed to prevent leg cramps due to muscle fatigue.
Calcium or magnesium deficiency
Having too little calcium or magnesium in your diet may contribute to leg cramps.
But if you already take a prenatal vitamin, you likely don’t need to take an additional supplement. A 2015 review of studies of 390 pregnant women found that taking magnesium or calcium supplements made little to no difference when it came to experiencing leg cramps.
If you’re concerned you aren’t getting enough of these nutrients, speak to your doctor. You’re probably getting labs done occasionally anyway, so it doesn’t hurt to have these levels checked.
DVT blood clot
A deep vein thrombosis (DVT) blood clot can occur in the legs, thigh, or pelvis. Pregnant women are 5 to 10 times more likely to develop a DVT than non-pregnant women. While there’s no need to panic that you’ll get one — it’s pretty uncommon to start with — we can’t say enough that knowledge is power.
Bottom line: Keep moving. We’re not talking marathons here, but the best way to prevent DVT during pregnancy is to avoid hours at a time of inactivity.
If your job requires a lot of sitting, you could set a quiet alarm on your phone to go off every hour to remind you to get up and walk — perhaps to the water cooler to add to your water intake for the day! Two birds, one stone.
Also take extra care to get up during long flights. You may want to check with your doctor before flying while pregnant.
Symptoms of a blood clot are similar to leg cramps, but a DVT blood clot is a medical emergency. Seek medical care right away if you experience symptoms like:
- a lot of pain in your legs when you’re standing or moving around
- severe swelling
- warm-to-the-touch skin near the affected area
Stretching before bed
Performing a calf stretch before getting into bed at night may help prevent or ease leg cramps. Follow these steps:
- Stand facing a wall, an arm’s length away.
- Place your hands on the wall in front of you.
- Step your right foot back. Keep your heels on the floor the whole time and bend your left knee while keeping your right leg straight. Keep your left knee bent as so you feel the stretch in your right calf muscle.
- Hold for up to 30 seconds. Switch legs, if needed.
Staying hydrated
Drinking plenty of water during pregnancy is important to prevent dehydration — and dehydration can also lead to those awful leg cramps.
Try to drink 8 to 12 cups of water each day during pregnancy. Easier said than done, sure — but super important for a lot of good reasons.
Applying heat
Try applying heat to your cramping muscle. It may help loosen up the cramp. No need to buy a fancy heating pad: You can also use a microwave-safe cloth bag (or a sock) filled with rice.
Massaging the area
When you get a leg cramp, performing a self-massage may help ease your pain. Use one hand to gently massage your calf or wherever your leg is cramping. Perform this self-massage for 30 seconds to a minute to ease your cramp.
You can also get a prenatal massage, which can be a positively divine experience. Look for an experienced therapist in your area who specializes in working with pregnant women.
Exercising
It’s a smart idea to stay active throughout your pregnancy, even though you don’t want to overdo it.
With your doctor’s OK, pregnancy-safe activities like prenatal yoga, walking, and swimming can benefit you and your baby-to-be.
Staying active can prevent excess weight gain, promote circulation, and yes — help prevent leg cramps. Always stretch and warm up before and after exercising so your muscles don’t cramp up afterward, though.
Avoiding inactivity
So, perhaps you don’t have the time or energy for a challenging hike or run. That is more than OK — you need to listen to your body and know your limits, especially during pregnancy.
But sitting for long periods of time can lead to leg and muscle cramps. To avoid this, make sure you stand up and walk around every hour or two. Set a timer on your phone or watch if you tend to forget to get up during the day.
Leg cramps are a common pregnancy symptom. (That doesn’t make having them any easier, but hopefully it turns down the stress dial a bit.)
If you’re concerned about your pain or they’re causing too much lost shut-eye, mention it at your next prenatal checkup.
Also call your doctor and let them know if your leg cramps are severe, persistent, or worsening. You may need supplements or medication.
You may need supplements or medication.
Seek medical help immediately if you experience severe swelling in one or both legs, pain walking, or enlarged veins. These may be symptoms of a blood clot.
The straight answer here is that there is no straight answer. (Great.)
Leg cramps are most common in the second and third trimester of pregnancy, not the first. But changing symptoms are a valid reason to wonder if you’re pregnant.
Some women do report aches and pains during the first trimester. This is likely due to your hormonal changes and your expanding uterus.
Leg cramps alone can’t tell you if you’re pregnant. If you suspect you’re pregnant or miss your period, take an at-home pregnancy test or see your doctor to confirm.
To prevent leg cramps, try the following:
- Drink between 8 and 12 cups of water per day.
- Stay active throughout your pregnancy.
- Stretch out your calf muscles.
- Wear comfortable shoes — leave the heels at home!
- Eat a balanced diet with calcium- and magnesium-rich foods like yogurt, leafy greens, whole grains, dried fruit, nuts, and seeds
Experiencing leg cramps during pregnancy isn’t pleasant. But it’s a common symptom, especially at night. Try our tips — we think they’ll help.
But it’s a common symptom, especially at night. Try our tips — we think they’ll help.
And as always, let your doctor know if you have any related worries. Never feel bad or self-conscious about phoning or emailing your clinic — helping you through a healthy pregnancy is the number one concern of OB doctors and nurses.
Early pregnancy | Shchelkovsky perinatal center
Pregnancy is a wonderful period! However, the changes taking place in the body at this time can greatly frighten you. The phenomena characteristic of pregnancy are different for all women, and will not necessarily be repeated during each subsequent gestation. Let's analyze the most common symptoms, their causes and possible methods of correction.
1. Frequent urination.
Frequent, painless (!) urge to urinate is one of the signs of pregnancy. This is due to increased secretion of progesterone (pregnancy hormone), changes in metabolism and pressure from the growing uterus on the bladder.
Be sure to see a doctor if:
- painful urination (this may be a sign of an infection)
- urine of strange color (stained with blood, brown)
- the amount of urine excreted per day is much less than the liquid drunk per day
Life hack! Under no circumstances should fluid intake be restricted! To alleviate the condition and reduce the frequent urge to urinate, it is necessary to exclude products that have a diuretic effect: tea, coffee, zucchini, watermelon; as well as salty, spicy and fried foods. It is better to drink water or juice. Wear comfortable cotton underwear that does not squeeze the lower abdomen.
2. Nausea, vomiting, heartburn, increased susceptibility to smells.
Nausea is one of the common symptoms of early pregnancy. The range of issues related to nausea and vomiting during pregnancy is quite wide. From "it's good, I don't even feel sick" (with relief), "I don't feel sick, what's wrong with me?" (with anxiety) to "when will this nausea pass" (with hope). Indeed, these symptoms are not at all a mandatory accompaniment of gestation, they can manifest at 7-8 weeks and last up to 12-14 weeks. The duration of this condition can sometimes be delayed, but rarely persists throughout pregnancy.
Indeed, these symptoms are not at all a mandatory accompaniment of gestation, they can manifest at 7-8 weeks and last up to 12-14 weeks. The duration of this condition can sometimes be delayed, but rarely persists throughout pregnancy.
Life hack! For nausea, eat before feeling hungry. Solid, non-hot food and drinks at a cool temperature are best. With heartburn, you should eat small portions of food and often, and most importantly, sit, stand or walk for at least 30 minutes after eating, but do not lie down.
You should definitely consult a doctor if:
- vomiting occurs even after drinking water
- vomiting is exhausting, accompanied by dizziness, weakness
- dryness, jaundice and flaking of the skin appear
- Nausea and vomiting interfere with proper nutrition, accompanied by weight loss
To reduce nausea and vomiting in the morning, try eating something before you get out of bed. It can be a cracker, a cookie, a piece of hard cheese. And salty food is preferable to sweet. You can have a snack in the same way at night when you get up to go to the toilet. Do not lie down immediately after eating, this will only increase nausea. Vitamins for pregnant women with nausea should be taken in the evening after meals. Cool water with lemon, ginger, mint tea, or ginger or mint candies can alleviate the condition. It is necessary to exclude those foods, drinks and smells that are unpleasant to you. Brushing your teeth and rinsing your mouth often can also reduce nausea.
It can be a cracker, a cookie, a piece of hard cheese. And salty food is preferable to sweet. You can have a snack in the same way at night when you get up to go to the toilet. Do not lie down immediately after eating, this will only increase nausea. Vitamins for pregnant women with nausea should be taken in the evening after meals. Cool water with lemon, ginger, mint tea, or ginger or mint candies can alleviate the condition. It is necessary to exclude those foods, drinks and smells that are unpleasant to you. Brushing your teeth and rinsing your mouth often can also reduce nausea.
3. Pain or cramps in the lower abdomen, constipation, pain in the lumbar region.
The simplest and most easily controlled cause of pain is delayed and incomplete bowel movements. An increase in the concentration of progesterone relaxes the smooth muscles, which are located not only in the uterus, but also in other hollow organs. In this case, the correction of the diet and the restoration of the passage of feces will help. If the measures are ineffective, the doctor may prescribe safe drugs for you. A special type of pain that occurs during exclusivity in pregnant women is pain in the round ligament of the uterus. This acute, rather intense pain occurs, as a rule, on the one hand with a sharp change in body position (for example, when getting up from a chair or leaving a car). This pain occurs due to stretching, and then a sharp contraction, like a spring, of the round uterine ligaments. The pain quickly passes if you immediately take a comfortable position and does not require special treatment.
If the measures are ineffective, the doctor may prescribe safe drugs for you. A special type of pain that occurs during exclusivity in pregnant women is pain in the round ligament of the uterus. This acute, rather intense pain occurs, as a rule, on the one hand with a sharp change in body position (for example, when getting up from a chair or leaving a car). This pain occurs due to stretching, and then a sharp contraction, like a spring, of the round uterine ligaments. The pain quickly passes if you immediately take a comfortable position and does not require special treatment.
You should definitely consult a doctor if:
- pain is accompanied by spotting bloody discharge from the external genitalia
- increasing duration and intensity of pain
- abdominal pain accompanied by dizziness, fever, loss of consciousness
Life hack! To normalize bowel movements, eat more vegetables and fruits, drink water and move more during the day. Try to eat often and in small portions.
Try to eat often and in small portions.
4. Enlargement and soreness of the mammary glands.
Hormonal restructuring of the body during gestation is accompanied, among other things, by an increase in the size of the mammary glands and an increase in their sensitivity. By the end of the first trimester, the soreness usually disappears, no additional methods of treatment are needed.
Life hack! Choose comfortable supportive underwear (it should not leave marks on the skin at the end of the day). You may need a larger size or a sports bra. Pain in the mammary glands is relieved by a warm shower at the end of the day.
You should definitely see a doctor if:
- the pain is intense
- mammary glands are very dense with redness and body temperature is increased
- discharge from the nipples appears (purulent, bloody)
5. Increased body temperature.
In early pregnancy, an increase in body temperature to 37.5 ° C is not necessary, but is possible due to the peculiarities of the action of progesterone. Because of this, it is difficult for pregnant women to endure stuffy, hot rooms. Self-medication is dangerous: an attempt to bring down the temperature even with a seemingly harmless folk method - tea with raspberries - can mask the true cause of hyperthermia and delay the diagnosis. Due to the increased body temperature, pregnant women should dress in layers and avoid stuffy and hot rooms and spaces so that they can always “adjust” their temperature on their own.
- temperature above 37.5 °C
- along with fever, any pain occurs
- runny nose, cough, body aches appear
6. Nasal congestion, difficulty breathing, nosebleeds.
These symptoms can be explained by the individual reaction of the vascular system to the increase in blood volume that occurs during pregnancy. Another possible reason is dry air in the room, the operation of central heating batteries.
Another possible reason is dry air in the room, the operation of central heating batteries.
Life hack! The easiest way to deal with nasal congestion is to use a humidifier. If you don't have one, you can put a damp towel on the battery - less effective, but better than nothing. It is possible to use sprays with sea salt, but you need to carefully read the instructions and especially the "Indications" section, it should contain information about the safety of the product during pregnancy.
You should definitely see a doctor if:
- symptoms of a cold occur
- nasal congestion accompanied by ear congestion
- These symptoms appeared after exposure to the allergen known to you
7. Blood pressure fluctuations.
An ideal option for the course of any pregnancy is the stability of the blood pressure throughout the gestation. However, this is extremely rare. A small (up to 10 units) increase in pressure from the usual reference may be due to an increase in the load on the cardiovascular system as a result of changes in body weight, hormonal changes, and uterine pressure on the vessels. Normal pressure: systolic below 130 mm Hg, diastolic no more than 85 mm Hg. Blood pressure in the range of 130–139/ 85–89 mm Hg considered high to be normal. High numbers are often observed in patients of older reproductive age, suffering from diabetes mellitus and kidney disease, obesity, etc. However, it is imperative to tell the doctor about all these concomitant pathological conditions at the first appointment and, if necessary, consult a neurologist, cardiologist, endocrinologist and other related specialists . Reasonable physical activity, adherence to sleep and wakefulness, a balanced diet, and the rejection of coffee and strong tea allow you to keep pressure within limits. Of the completely exotic for our days, but no less significant - the prevention of stress.
Normal pressure: systolic below 130 mm Hg, diastolic no more than 85 mm Hg. Blood pressure in the range of 130–139/ 85–89 mm Hg considered high to be normal. High numbers are often observed in patients of older reproductive age, suffering from diabetes mellitus and kidney disease, obesity, etc. However, it is imperative to tell the doctor about all these concomitant pathological conditions at the first appointment and, if necessary, consult a neurologist, cardiologist, endocrinologist and other related specialists . Reasonable physical activity, adherence to sleep and wakefulness, a balanced diet, and the rejection of coffee and strong tea allow you to keep pressure within limits. Of the completely exotic for our days, but no less significant - the prevention of stress.
Life hack! If you first discovered that you have high normal pressure, repeat the measurement after 15 minutes. If the pressure remains elevated, see a doctor.
Be sure to see a doctor if:
- your blood pressure is above 140/90 mmHg.
- pressure increased by more than 10 mm Hg. relative to your usual
- an increase in the pressure indicator is accompanied by edema, the appearance of "flies" before the eyes
NB! You should also pay attention to lowering blood pressure. Numbers less than 90/60 mmHg - an excuse to see a doctor.
Life hack! Keep a blood pressure diary, especially if you are prone to hypertension. Show your diary to your doctor at every appointment.
8. Heaviness and pain in the legs.
Heaviness and pain in the legs, especially in the evening, are frequent companions of pregnancy. There is an explanation for the occurrence of symptoms: an increase in load due to growing weight and a shift in the center of gravity of the body.
Life hack! Ask your partner/husband to give you a foot massage, relax with your limbs elevated (not too much!) A therapeutic pedicure, dousing the legs with cool water, a contrast shower, a cream or gel for legs with cooling components (menthol, essential oils), as well as compression stockings or stockings of the lightest degree of compression will help.
You should always see a doctor if:
- one or both legs are very swollen or discolored
- previously diagnosed varicose veins, family history of thrombosis
9. Skin changes.
During pregnancy, you may notice dark spots on your skin. Especially often such darkening (hyperpigmentation) is observed in the nipple area, along the white line of the abdomen. Stretch marks (stretch marks) may appear on the skin of the abdomen and thighs. These are normal signs and do not require any treatment. In most cases, skin color will return to normal after breastfeeding ends, and stretch marks will shrink and fade. Itching can be associated with stretching of the skin, especially in the abdomen and mammary glands. This symptom occurs infrequently and is usually successfully stopped by the use of special products to moisturize and soften the skin. By the way, these same remedies usually help in the fight against stretch marks.
Life hack! Oils and moisturizing creams to increase skin elasticity, contrast showers, massage with a hard brush will help reduce the likelihood of skin changes.
You should definitely consult a doctor if:
- along with itching there are areas of redness, spots, peeling
- itching increases
10. Bleeding gums.
Changes in the characteristics of blood circulation in the body of a pregnant woman can cause bleeding gums. The appearance of minor blood impurities during brushing your teeth, when eating solid foods (for example, an apple) is acceptable. However, the key provision is "insignificant". If you find it difficult to assess your own condition, consult a specialist.
You should definitely consult a doctor if:
- you have loose teeth, sore gums, bad breath
- bleeding in the gum area increases
11. Fatigue, mood instability.
Fatigue, mood instability.
Tearfulness, lack of strength, forgetfulness, distraction, the whole palette of feelings "here and now"... The list can be continued, and there is only one explanation for this - pregnancy. The most common early symptom is severe fatigue. There is no universal recipe, just as there is no single picture of these states. The main recommendation for all pregnant women is to rest often, relax and even sleep during the day. Most importantly, you need to remember: pregnancy is not a disease, but a great time to prepare for motherhood.
Pain in the legs | Dikul Center
Minor pains in the leg muscles are quite common. Foot problems most often occur when playing sports, during work related to stress on the legs or household chores. In addition, injuries are a common cause of pain in the legs. Leg problems can be minor or serious and manifest with symptoms such as pain, swelling, cramps, numbness, tingling, muscle weakness, or changes in temperature or skin color.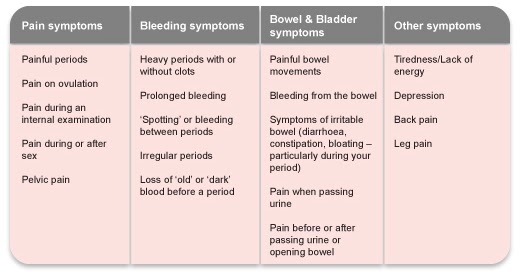 Symptoms often appear after exercise, daily routine and overuse. People in the older age group are more prone to foot problems in the same way that muscle loss occurs over the years. In childhood, foot problems can be caused by similar factors as in adults, or be specific.
Symptoms often appear after exercise, daily routine and overuse. People in the older age group are more prone to foot problems in the same way that muscle loss occurs over the years. In childhood, foot problems can be caused by similar factors as in adults, or be specific.
The causes of pain in the legs are divided into two groups: traumatic and non-traumatic.
According to localization - pain in the thigh, buttocks, pain in the lower leg and pain in the foot.
The main and most common causes of pain in the legs.
- Injuries associated with excessive load or repetitive movements (bursitis, tendonitis, plantar fasciitis).
- Muscle cramps.
- Schlatter-Osgood disease
- Juvenile idiopathic arthritis
- Growing pains
- Medicines (side effect)
- Restless legs syndrome
- Transient ischemic attacks or stroke
- Obliterating diseases of peripheral arteries
- Venous thrombosis.

- Pregnancy
- Muscle strain
- Muscle tear
- Injury to muscle or lower limb
- Bone lesions
- Rupture of popliteal cyst (Baker's cyst)
- Diseases of the joints (osteoarthritis, systemic lupus erythematosus, rheumatoid arthritis, arthrosis)
- Varicose disease
- Obesity
- Night cramps
- Fibromyalgia
- Infections
- Neurogenic pain (herniated disc, stenosis, protrusion of the disc, sciatica)
- Diabetic polyneuropathy
Muscle cramps
Muscle cramps (cramps) are severe, painful contractions and tightness of a muscle that occur suddenly, lasting from a few seconds to a few minutes. Muscle soreness may persist for several hours after the episode of constriction (convulsions) has ended. They usually resolve on their own and do not require special treatment.
The cause of seizures is not always known. Muscle cramps can occur with various conditions or types of physical activity, such as:
- Exercise, injury or overuse of the muscles.
 A muscle with overwork, with poor elasticity or an incorrect load vector, can give a cramp.
A muscle with overwork, with poor elasticity or an incorrect load vector, can give a cramp. - Dehydration associated with exercise during hot weather may be a cause of heat cramps. In addition, in various conditions (vomiting, diarrhea or lack of water), there may also be convulsions.
- Pregnancy. Pregnancy cramps can occur due to a decrease in the amount of minerals in the body, such as calcium and magnesium, especially in the last months of pregnancy (when the formation of the musculoskeletal system of the fetus is completed).
- Exposure to low temperatures, especially when immersed in cold water.
- Certain diseases (occlusive peripheral arterial disease, kidney disease, thyroid disease) multiple sclerosis, etc.
- Medications - some drugs may cause seizures (neuroleptics, diuretics). In any case, if there are recurring episodes of seizures, you should consult a doctor.
Osgood-Schlatter's disease
Osgood-Schlatter's disease (sometimes also called Schlatter's disease or osteochondrosis of the tibial tuberosity) is an inflammation in the upper part of the tibia where the patellar tendons attach to a tubercle called the tibial tuberosity. This disease is often the cause of knee pain in adolescence (10 to 15 years), is associated with the growth of the musculoskeletal system, and as the growth is completed, the symptoms may disappear.
This disease is often the cause of knee pain in adolescence (10 to 15 years), is associated with the growth of the musculoskeletal system, and as the growth is completed, the symptoms may disappear.
Osgood-Schlatter disease may present with pain, swelling, and tenderness in the anterior part of the knee, below the kneecap. As a rule, one knee is affected (sometimes it happens on both sides). Symptoms worsen with stress on the tendon attached to the tibial tuberosity (eg, jumping). The diagnosis is made on the basis of radiography. The main task of treatment is aimed at the prevention of symptoms (reduction of certain types of load, immobilization during exacerbation, physiotherapy). Surgical treatments are rarely used.
Juvenile idiopathic arthritis
Juvenile idiopathic arthritis, often referred to as juvenile rheumatoid arthritis or juvenile chronic arthritis, is a childhood disease characterized by inflammation of the joints that become swollen and painful (respectively, with impaired mobility in the joint). It manifests itself in children with pain in the joints, impaired gait, due to decreased mobility in the joints and stiffness in the joints, usually in the first half of the day, with regression within 1-1.5 hours and after normal physical activity. The causes of this disease are not completely clear. Most researchers believe that the disease is due to a combination of factors that cause excessive activation of the immune system. There are several types of juvenile arthritis. The division into types is based on the number of joints involved in the process during the first 6 months from the onset of the disease, the area of the body where the disease manifested itself, the presence of other symptoms. Types of juvenile arthritis: oligoarthritis (affecting no more than 4 joints) polyarthritis (affecting 5 or more joints), rheumatic positive and rheumatic negative (depending on the presence of rheumatic factor in the blood), systemic (accompanied by rashes on the body, temperature and lesions eye).
It manifests itself in children with pain in the joints, impaired gait, due to decreased mobility in the joints and stiffness in the joints, usually in the first half of the day, with regression within 1-1.5 hours and after normal physical activity. The causes of this disease are not completely clear. Most researchers believe that the disease is due to a combination of factors that cause excessive activation of the immune system. There are several types of juvenile arthritis. The division into types is based on the number of joints involved in the process during the first 6 months from the onset of the disease, the area of the body where the disease manifested itself, the presence of other symptoms. Types of juvenile arthritis: oligoarthritis (affecting no more than 4 joints) polyarthritis (affecting 5 or more joints), rheumatic positive and rheumatic negative (depending on the presence of rheumatic factor in the blood), systemic (accompanied by rashes on the body, temperature and lesions eye).
Growing pains
Leg pains are associated with growing pains and are not uncommon in children and adolescents. Most likely, pain manifestations are associated with uneven growth of muscles, bones and soft tissues. Pain, as a rule, is localized in the thighs or calf muscles and usually appears in the afternoon. The duration of pain can be 1-2 hours. Growth pain is not accompanied by other symptoms (fever, swelling). Over time, the symptoms disappear by themselves. massage and sometimes paracetamol. Aspirin under 20 years of age is not recommended due to the possibility of developing Reye's syndrome.
Medicines
Some medicines can cause problems in the legs due to side effects. Combining with smoking or drinking alcohol increases the risk of drug side effects. Main groups of drugs that can cause problems in the legs:
- Drugs that cause blood clots (for example, contraceptives)
- Antipsychotics (chlorpromazine, haloperidol)
- Beta-2 receptor agonists (terbutaline or albuterol)
- Antihypertensive drugs (nifedipine, amlodipine or nicardipine)
- Statins are cholesterol-lowering drugs (simvastatin or atorvastatin).

- Estrogens
- Lithium preparations
- Diuretics (Lasix and others)
- Opiates
- Steroids
If you are on medication (especially long-term), tell your doctor if you experience pain or cramps in your legs.
Restless Leg Syndrome
Restless Leg Syndrome is a condition in which the patient experiences discomfort with the position of the legs and sometimes an overwhelming urge to move the legs. This syndrome can disrupt sleep and interfere with daily life.
Patients describe their sensations as needles in the legs, sometimes as drawing pains. Changing the position of the legs brings temporary relief. Most often, these sensations occur in the evening, when a person is trying to relax or go to bed. The cause of this syndrome is not known. Certain medications (such as antidepressants) pregnancy or iron deficiency (anemia) can cause this syndrome. Restless legs syndrome is treated with drugs that increase dopamine levels in the brain (levodopa) or anti-seizure drugs (gabapentin) to control leg movements and improve sleep. Opiates are rarely used.
Opiates are rarely used.
Transient ischemic attacks
Transient ischemic attacks are temporary interruptions in the blood supply to the brain. They are harbingers of a stroke. The only difference from a stroke is that the symptoms gradually disappear. The following symptoms should alert:
- Sudden numbness, tingling and weakness in half of the body or limb
- Gait disorder
- Violation of the perception of reality
- Speech disorder
- Severe headache.
If these symptoms appear, seek emergency medical attention
Obliterating peripheral arterial disease
PAD is a permanent narrowing or blockage of the arteries that supply oxygen-rich blood to various organs, including the lower extremities.
The main cause of occlusive lesions of the peripheral vessels of the lower extremities is the accumulation of cholesterol, calcium and other substances on the walls of the arteries (atherosclerosis).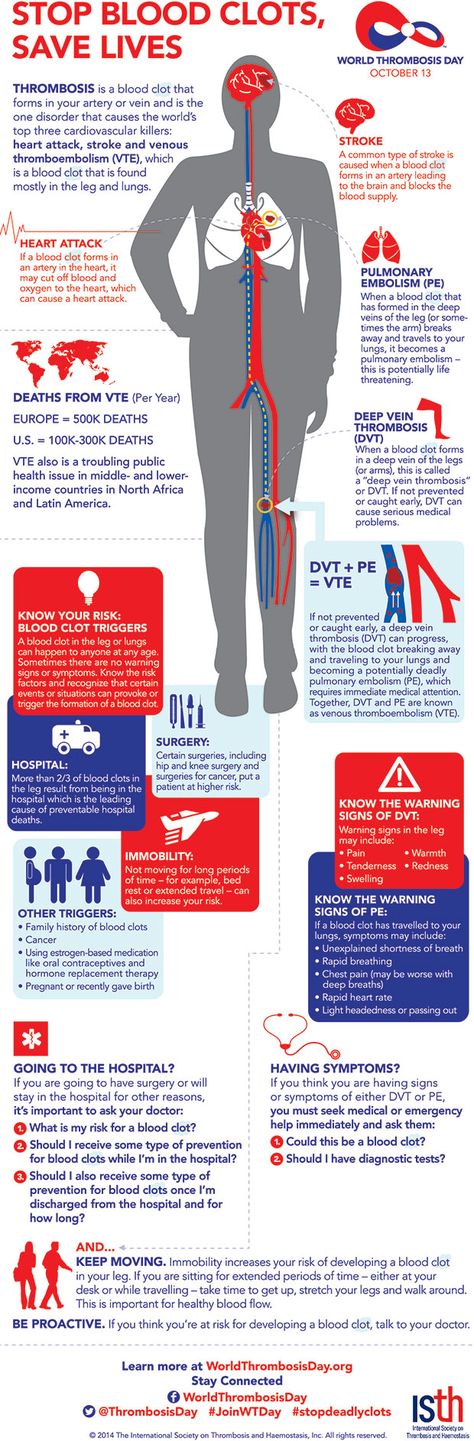 The narrowing of the lumen of the artery leads to a decrease in the flow of arterial blood to the muscles of the legs, which is especially evident during exercise. When the muscle is at rest, the blood supply may be adequate.
The narrowing of the lumen of the artery leads to a decrease in the flow of arterial blood to the muscles of the legs, which is especially evident during exercise. When the muscle is at rest, the blood supply may be adequate.
The main symptom of obliterating disease of the leg arteries is pain in the calf muscles, thighs and buttocks, which appear after physical activity (such as climbing a hill or stairs, running, walking). This pain is called intermittent claudication. This usually occurs after a certain amount of movement and disappears after rest. As the disease progresses, symptoms appear with minimal exercise. In addition to pain, patients are often concerned about: decreased muscle strength in the legs and balance, standing, numbness of one leg or two, the appearance of ulcers that heal slowly. Treatment is usually conservative. With a pronounced violation of the blood supply, surgical methods of treatment are indicated.
Venous thrombosis
Thrombosis pain (blockage of a vein by a blood clot) is caused by inflammation of the vessel wall or surrounding tissues. In addition, a violation of the outflow can lead to swelling, discoloration of the skin (pallor, cyanosis, redness). Paleness can be detected in the early stages of iliofemoral vein thrombosis. Cyanosis is caused by congestive hypoxia and usually occurs with obstruction of the proximal veins of the leg. Pain during thrombosis can be aching, sharp or dull, intense and moderate. Often the pain is aggravated by walking, carrying weights. Reduction of pain, possibly in the supine position with legs raised. With superficial vein thrombosis, diagnosis is not difficult. If there is a suspicion of deep vein thrombosis, then objective research methods are needed.
In addition, a violation of the outflow can lead to swelling, discoloration of the skin (pallor, cyanosis, redness). Paleness can be detected in the early stages of iliofemoral vein thrombosis. Cyanosis is caused by congestive hypoxia and usually occurs with obstruction of the proximal veins of the leg. Pain during thrombosis can be aching, sharp or dull, intense and moderate. Often the pain is aggravated by walking, carrying weights. Reduction of pain, possibly in the supine position with legs raised. With superficial vein thrombosis, diagnosis is not difficult. If there is a suspicion of deep vein thrombosis, then objective research methods are needed.
Pregnancy
Pain and soreness in the lower leg (rarely in the thigh) may occur during pregnancy. In pregnant women, pain may be accompanied by swelling of the lower leg and thigh (both one and both limbs). The causes of pain in the legs in pregnant women are not entirely clear. On the one hand, this is due to a violation of the outflow from the venous network of the lower extremities due to the fetus. On the other hand, a decrease in electrolytes in the blood contributes to the appearance of muscle cramps, which serve as one of the sources of pain. Unilateral swelling and pain in the limb may be associated with compression of the iliac artery by an enlarged uterus.
On the other hand, a decrease in electrolytes in the blood contributes to the appearance of muscle cramps, which serve as one of the sources of pain. Unilateral swelling and pain in the limb may be associated with compression of the iliac artery by an enlarged uterus.
Muscle strain
Pain in the muscles may appear after fast walking, running, playing sports, walking in ill-fitting shoes. As a rule, discomfort occurs immediately after exercise or after 12-24 hours. Most often, pain occurs in the legs, sometimes in the hips. There may be pain on palpation. Sometimes there is swelling of the leg. If there is a clear connection with physical activity and bilateral pain, then the diagnosis is beyond doubt. In cases where the pain is unilateral, it is necessary to exclude possible vein thrombosis using objective diagnostic methods.
Muscle rupture
Muscle rupture most often occurs in the lower leg (possible also in the thigh). Rupture occurs as a result of a sharp stretching or contraction of the muscle. As a rule, a small section of the muscle is torn at the junction with the tendon. But there are also large gaps, up to the separation of the muscle from the tendon or the detachment of the tendon. Rupture of the muscle occurs mainly with a sharp bending of the limb in the opposite direction to the acting force. The rupture is accompanied by acute pain, immediately after excessive load. For some time, the pain may subside, but as the hematoma grows, the pain will gradually increase. There is swelling in the area of the damaged muscle and limited range of motion.
As a rule, a small section of the muscle is torn at the junction with the tendon. But there are also large gaps, up to the separation of the muscle from the tendon or the detachment of the tendon. Rupture of the muscle occurs mainly with a sharp bending of the limb in the opposite direction to the acting force. The rupture is accompanied by acute pain, immediately after excessive load. For some time, the pain may subside, but as the hematoma grows, the pain will gradually increase. There is swelling in the area of the damaged muscle and limited range of motion.
Damage to bones
Damage to the bone tissue of the lower extremities (tumors, subperiosteal hematomas, fractures) may be accompanied by pain, tenderness to the touch, swelling of the extremity. Clinical manifestations may be similar to venous thrombosis. It is especially difficult to diagnose a hip fracture in the elderly (often the fracture is accompanied by swelling of the lower limb). Given the involutional changes in the CNS (cerebrovascular sclerosis), it is sometimes difficult to collect an anamnesis in this category of patients. In addition, older people often have a combination of a hip fracture with venous thrombosis.
In addition, older people often have a combination of a hip fracture with venous thrombosis.
Rupture of a popliteal cyst (Baker's cyst)
Fluid contained in a Baker's cyst, when ruptured (in case of trauma, arthritis, or surgery in the knee joint), can descend into the intermuscular space and cause an inflammatory reaction. This can be manifested by pain, swelling in the lower leg, pain on palpation and resemble a picture of venous thrombosis. Rupture of a Baker's cyst can occur without provoking causes. The diagnosis can be made on the basis of radiography. But the possible combination of cyst rupture and venous thrombosis requires, first of all, the exclusion of thrombosis.
Diagnosis
First of all, to diagnose the cause of pain, the doctor needs to get answers to a number of questions:
- Pain localization
- Presence of pain in one or both limbs
- Nature of pain (acute, dull)
- Dependence of pain on the time of day
- Dependence of pain intensity on physical activity
- Ability to reduce pain when lifting legs
- Presence of other symptoms (fever, weakness, back pain).