How to tell if your child is dehydrated when sick
Dehydration (for Parents) - Nemours KidsHealth
Reviewed by: Amy W. Anzilotti, MD
en español Deshidratación
What Is Dehydration?
Dehydration is when there is not enough water in the body.
What Causes Dehydration?
Dehydration in children usually is caused by vomiting, diarrhea, or both. It also can happen when children don't want to drink because they have mouth sores or a sore throat. Kids also can get dehydrated in hot weather or when they are very active.
What Are the Signs & Symptoms of Dehydration?
Signs of dehydration include:
- a dry or sticky mouth
- few or no tears when crying
- eyes that look sunken
- in babies, the soft spot (fontanelle) on top of the head looks sunken
- peeing less or fewer wet diapers than usual
- crankiness
- drowsiness or dizziness
How Is Dehydration Treated?
Treatment for dehydration depends on how severe it is. Kids with mild dehydration can get extra liquids at home. Kids with more severe dehydration may need treatment in the ER or hospital.
Mild dehydration is treated with oral (by mouth) rehydration. This usually includes giving oral rehydration solution (such as Pedialyte, Enfalyte, or a store brand). It has the right amounts of water, sugar, and salt to help with dehydration. You can buy it without a prescription at drugstores or supermarkets. If you can’t get oral rehydration solution, talk to your doctor. There are other fluids that can help with dehydration.
If your child has mild dehydration and your doctor says it’s OK to start treatment at home:
- Give your child small sips of oral rehydration solution as often as possible, about 1 or 2 teaspoons (5 or 10 milliliters) every few minutes.
- Babies can continue to breastfeed or take formula, as long as they are not vomiting repeatedly.
- Older children also can have electrolyte ice pops.
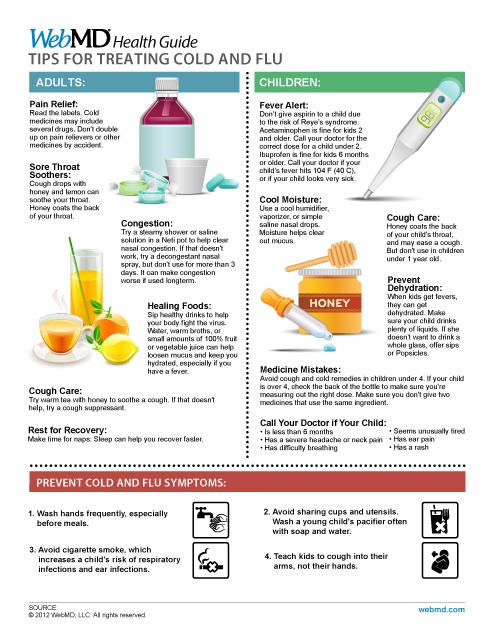
- Kids can keep eating their regular diet, unless the doctor recommends a change. They may not want to eat at first but as long they are drinking, it’s OK if they aren’t eating much solid foods.
- Don't give babies plain water instead of oral rehydration solution. It doesn't have the right nutrients for babies with dehydration.
- Don't give sports drinks, soda, or full-strength (undiluted) juice. They have too much sugar and can make some symptoms worse.
- As your child starts to feel better and have a better appetite, you can give less oral rehydration solution and more of their usual food and drink.
- Don’t give medicines for diarrhea or vomiting unless the doctor recommends it.
When Should I Call the Doctor?
Call your doctor if your child:
- won't take anything to drink for more than a few hours
- is under 1 year old and is drinking only oral rehydration solution (no breastmilk or formula) for 24 hours
- vomits more than a few times in 24 hours
- has vomit that's bright green, red, or brown
- hasn’t started eating some food within 3-4 days
- has signs of dehydration like a dry mouth, peeing less often (or fewer wet diapers in babies), fewer tears, or sunken soft spot (in babies)
- doesn’t seem to be getting better
Go to the ER if your child is very sleepy or isn’t responding to you.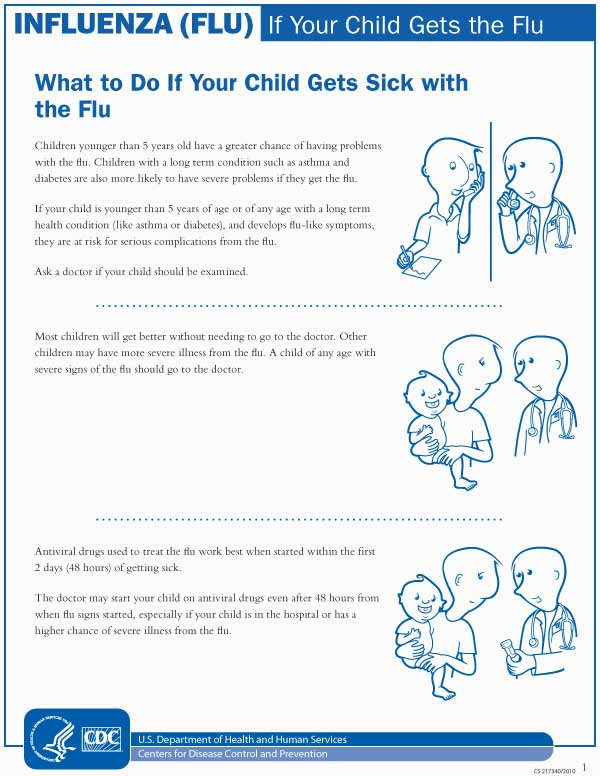
How Can We Prevent Dehydration?
Whenever your child gets sick, give extra fluids or oral rehydration solution. Give small amounts often, especially if your child is vomiting.
Kids need to drink often during hot weather. Those who play sports or are very physically active should drink extra fluids beforehand, and then take regular drink breaks (about every 20 minutes) during the activity.
Reviewed by: Amy W. Anzilotti, MD
Date reviewed: March 2020
Signs of Dehydration in Toddlers: Warning Signs
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission. Here’s our process.
Intro
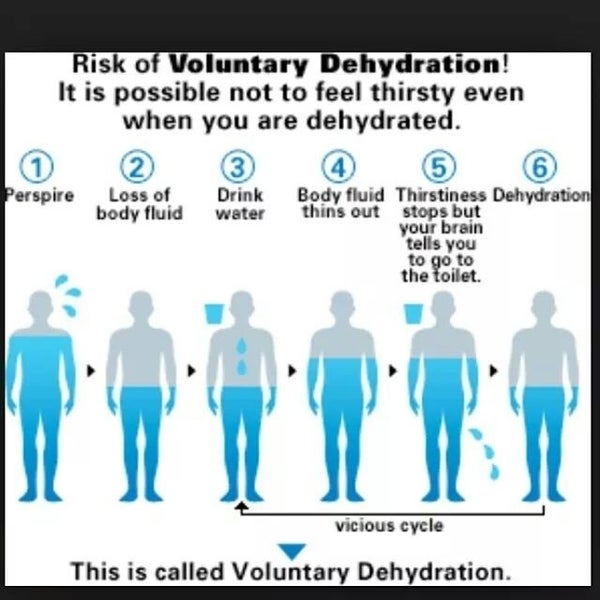
All kids and adults lose water constantly throughout the day. Water evaporates from the skin and leaves the body when you breathe, cry, sweat, and use the toilet.
Most of the time, a toddler gets enough water from eating and drinking to replace the fluids they lose. But in some cases, kids can lose more water than normal. Fevers, stomach flus, being out in hot weather, or too much exercise, for example, may result in too much fluid loss. This can lead to dehydration.
But in some cases, kids can lose more water than normal. Fevers, stomach flus, being out in hot weather, or too much exercise, for example, may result in too much fluid loss. This can lead to dehydration.
Dehydration isn’t something to take lightly. When it happens, the body doesn’t have enough fluids and water to function properly. In severe cases, this could lead to brain damage or even death.
Read on to learn the warning signs of dehydration in your toddler, and tips for how to prevent it.
Is my toddler at risk for dehydration?
Dehydration happens when more fluid is leaving the body than entering it. Children are more susceptible to dehydration than older teens and adults because they have smaller bodies. They have smaller reserves of water.
Some toddlers become dehydrated because they don’t drink enough water. Certain factors can also put your toddler at a higher risk of dehydration. These include:
- fever
- vomiting
- diarrhea
- excessive sweating
- poor fluid intake during an illness
- chronic illnesses like diabetes or a bowel disorder
- exposure to hot and humid weather
Diarrhea may be caused by an infection (viral, bacterial, or parasite), food allergy or sensitivity, a medical condition such as inflammatory bowel disease, or a reaction to a medication.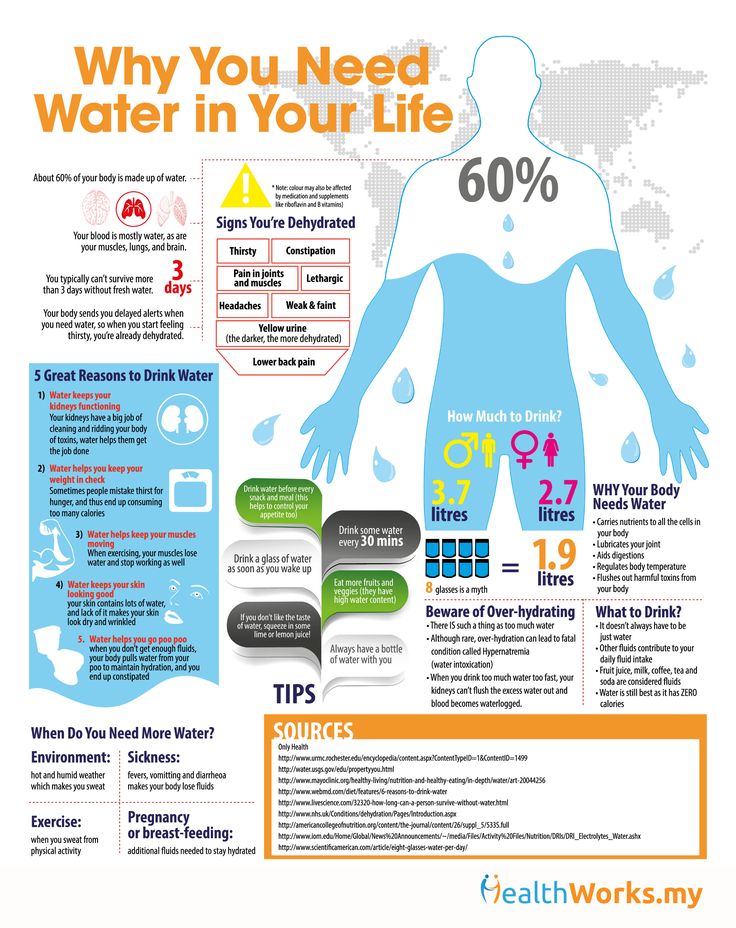 If your toddler is vomiting, has watery stools, or is unable or unwilling to drink because of an illness, monitor them for signs of dehydration. Be ready to respond.
If your toddler is vomiting, has watery stools, or is unable or unwilling to drink because of an illness, monitor them for signs of dehydration. Be ready to respond.
Warning signs of dehydration in toddlers
Dehydration can happen very slowly over time, or it can happen suddenly. Toddlers with an illness, especially stomach flu, should be monitored closely for signs of dehydration. The warning signs aren’t always obvious.
Don’t wait until your toddler is excessively thirsty. If they’re really thirsty, they may already be dehydrated. Instead, look out for these warning signs:
- dry, cracked lips
- dark-colored urine
- little or no urine for eight hours
- cold or dry skin
- sunken eyes or sunken soft spot on the head (for babies)
- excessive sleepiness
- low energy levels
- no tears when crying
- extreme fussiness
- fast breathing or heart rate
In the most serious cases, your toddler can become delirious or unconscious.
Treating dehydration in toddlers
The only way to effectively treat dehydration is to replenish the lost fluids. Mild dehydration can be managed at home. If your toddler has diarrhea, vomiting, or fever, or is showing signs of dehydration, take the following steps.
- Give your toddler an oral rehydration solution like Pedialyte. You can purchase Pedialyte online. These solutions contain water and salts in precise proportions and are easy to digest. Plain water won’t usually be enough. If you don’t have an oral rehydration solution available, you can try milk or diluted juice until you are able to get some.
- Keep giving your toddler liquids slowly until their urine is clear. If your toddler is vomiting, give them only a small amount at a time until they’re able to keep it down. They may only be able to tolerate a spoonful at a time, but anything is better than nothing. Gradually increase the frequency and amount. Giving too much too fast will often cause vomiting to return.
- If you are still breast-feeding, continue to do so. You can also give your baby a rehydration solution in their bottle.
Preventing dehydration in toddlers
It’s important for parents to learn the warning signs of dehydration. If your toddler is excessively thirsty, it may already be too late. Here are some steps to take to prevent dehydration.
Have an oral rehydration solution on hand at all times. These are available in liquids, popsicles, and powders.
- If your toddler gets sick, be proactive about their fluid intake. Start giving them extra water and a rehydration solution at the first sign of an illness.
- Toddlers who won’t eat or drink due to a sore throat may need to ease the pain with acetaminophen (Tylenol) or ibuprofen (Advil). Shop for acetaminophen or ibuprofen at Amazon.
- Make sure your toddler is up-to-date on vaccinations, including the rotavirus vaccine. Rotavirus causes one-third of all diarrhea-related hospitalizations in kids under 5.
 Talk to your doctor if you have any concerns or questions about the rotavirus vaccine.
Talk to your doctor if you have any concerns or questions about the rotavirus vaccine. - Teach your toddler how to wash their hands before eating or drinking and after using the bathroom to avoid contracting infections.
- Encourage children to drink plenty of water before, during, and after exercise.
- If you’re outside on a hot summer day, allow your toddler to enjoy a pool, sprinkler, or rest in a cool, shaded environment, and offer them plenty of water.
When to see a doctor if your toddler is dehydrated
Bring your child to the doctor if:
- your child doesn’t appear to be recovering or is becoming more dehydrated
- there’s blood in your toddler’s stool or vomit
- your child refuses to drink or have an oral rehydration solution
- your toddler’s vomiting or diarrhea is persistent and severe and they can’t drink enough fluid to keep up with how much they’re losing
- the diarrhea is lasting more than a few days
A doctor can check for dehydration and replenish your child’s fluids and salts quickly intravenously (through a vein) if needed.
Next steps
Dehydration in your toddler can’t always be prevented, but there are actions you can take right now to help. Learn to recognize the warning signs. Contact your pediatrician if you’re concerned your toddler might be dehydrated.
Share on Pinterest
Children from 0 to 5 years old. When should you urgently take your child to the doctor?
We are all very worried when a child gets sick; including the fear that he will certainly be sent to the hospital. And the children's hospital, as you know, is like this: you get in with one, you leave with another. That is why mothers often refuse hospitalization or postpone a visit to the doctor, hoping that the disease will recede on its own, others prefer online consultations on forums and advice from grandmothers and girlfriends.
Fortunately for all mothers, in most cases, modern medicine makes it possible to diagnose and provide the necessary assistance very quickly, resorting to hospitalization only as a last resort.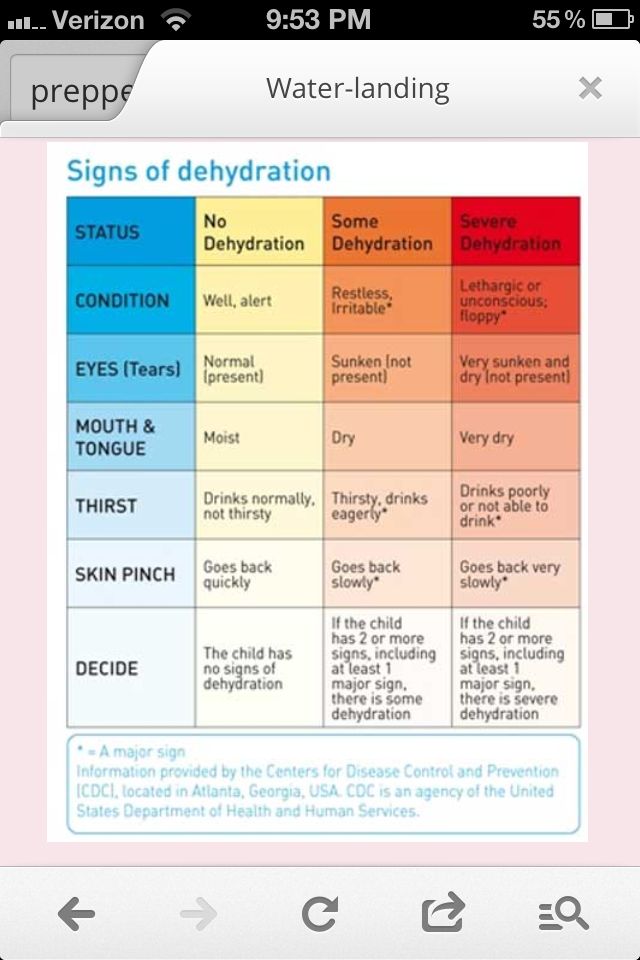 Something like in the famous series with Hugh Laurie - and MRI, and all the necessary tests, and CT scans, and, most importantly, competent pediatricians and highly specialized specialists. Unfortunately, not all polyclinics have such a set, but in one place in Moscow they definitely have it - in the department of emergency pediatrics of the Federal State Autonomous Institution "NMIC for Children's Health" of the Ministry of Health of Russia, where doctors usually need no more than 2 hours to establish an accurate diagnosis, taking all the necessary analyzes and quickly receive their results, stabilize the child and send him home if there is no threat to life and indications for emergency hospitalization.
Something like in the famous series with Hugh Laurie - and MRI, and all the necessary tests, and CT scans, and, most importantly, competent pediatricians and highly specialized specialists. Unfortunately, not all polyclinics have such a set, but in one place in Moscow they definitely have it - in the department of emergency pediatrics of the Federal State Autonomous Institution "NMIC for Children's Health" of the Ministry of Health of Russia, where doctors usually need no more than 2 hours to establish an accurate diagnosis, taking all the necessary analyzes and quickly receive their results, stabilize the child and send him home if there is no threat to life and indications for emergency hospitalization.
If you understand that your child needs a prompt consultation with a specialist, but for some reason you postpone the visit to the doctor, if you are afraid that the child will be immediately sent to the hospital ward “to clarify the diagnosis”, or he will not be given due Attention, just come to the pediatric emergency department of the Federal State Autonomous Institution "NMIC of Children's Health" of the Ministry of Health of Russia. Here they immediately do all the necessary research and provide the child with assistance as efficiently and quickly as possible. Every year, more than 3,000 children receive care in the department, and only 2% of them are hospitalized by doctors in a round-the-clock hospital. The rest are sent home after all the necessary procedures with appropriate recommendations, or will be observed for several days in a day hospital. The department accepts children without an appointment, works on CHI, VHI and on a commercial basis.
Here they immediately do all the necessary research and provide the child with assistance as efficiently and quickly as possible. Every year, more than 3,000 children receive care in the department, and only 2% of them are hospitalized by doctors in a round-the-clock hospital. The rest are sent home after all the necessary procedures with appropriate recommendations, or will be observed for several days in a day hospital. The department accepts children without an appointment, works on CHI, VHI and on a commercial basis.
If your child is between 0 and 5 years old, do not neglect visits to the doctor because your child is at risk. It is this age that accounts for most of the serious diseases that are well studied by medicine, are well treated, but require prompt medical intervention. Tatyana Vladimirovna Kulichenko, Head of the Department of Emergency Pediatrics, FGAU "NMIC of Children's Health" of the Ministry of Health of Russia, Doctor of Medical Sciences, pediatrician of the highest category, WHO expert, spoke about the cases in which it is worth immediately contacting specialists for young children (we are talking about children first 5 years of life).
High temperature (fever)
First, it is important to define what a fever is from a doctor's point of view. Fever is an increase in body temperature greater than 38°C if measured rectally (preferred as this is the most reliable way to determine body temperature in any person) and greater than 37.5°C if measured axillary depression.
Not every fever is a very bad sign, but with children under three years old it is better to play it safe and see a doctor as soon as possible. There are no legislative "terms of patience"; there is no need to wait three days, as pediatricians usually say: all the most severe infections develop very quickly and can be threatening from the first hours of the illness. The sooner you contact a specialist, the better. Examination of the child, instrumental and laboratory studies will help to understand the cause of the fever and quickly stabilize the child's condition.
If just a high temperature seems to you not enough reason to see a doctor, then pay attention to the symptoms of intoxication:
- The child refuses to drink (not to eat, namely to drink).
- There is lethargy and drowsiness, it is difficult to establish eye contact with the child (some pediatricians say about such patients "the child looks into himself").
If a child develops a rash on the skin along with an increase in body temperature, then you should go to the doctor immediately.
Cough
Cough is a fairly common symptom in children. Precisely because it seems to be a common, “understandable” sign of illness, parents often miss the moment of timely visit to the doctor. Cough can be caused not only by problems with the organs of the respiratory system. It can signal a malfunction in the cardiovascular or digestive systems. It can even be caused by a sulfur plug in the ear. Until you eliminate the cause, the symptom will not disappear!
Take your child to the doctor immediately if:
- The child is less than 6 months old (whether or not he has a fever or other symptoms).
- The child has a nocturnal cough.

- The child has a cough to the point of vomiting.
- Cough does not go away for more than 3 weeks.
- Barking cough, often accompanied by hoarseness and noisy breathing.
Difficulty breathing
Any difficulty in breathing can be a life-threatening symptom, especially in infants. How to understand that breathing is difficult in an infant: when inhaled, retraction is visible along the edge of the costal arch (the child, as it were, strongly draws in the stomach when breathing). Difficulty in breathing in older children can be noticed if there is no fluency of speech: the child cannot speak in long sentences (as a rule, these are obstructive bronchitis or asthmatic conditions).
Take your child to the doctor immediately if you notice signs of difficulty breathing, especially if the breath is grunting, groaning or you hear wheezing or whistling when breathing even from a distance.
Vomiting, diarrhea (diarrhea, loose stools)
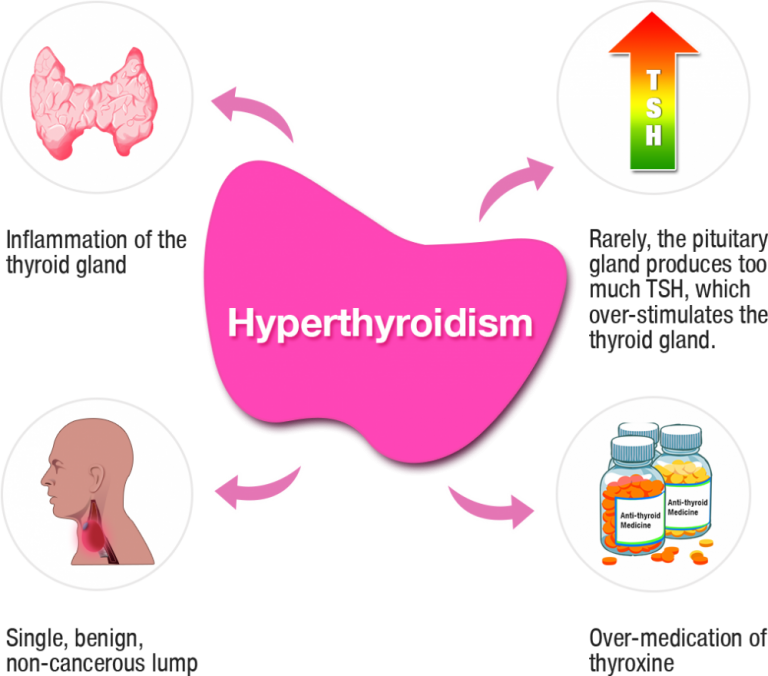
These symptoms are often associated with simple and well-known conditions that are caused by extremely unpleasant, but in modern conditions, with proper treatment, non-life-threatening intestinal infections.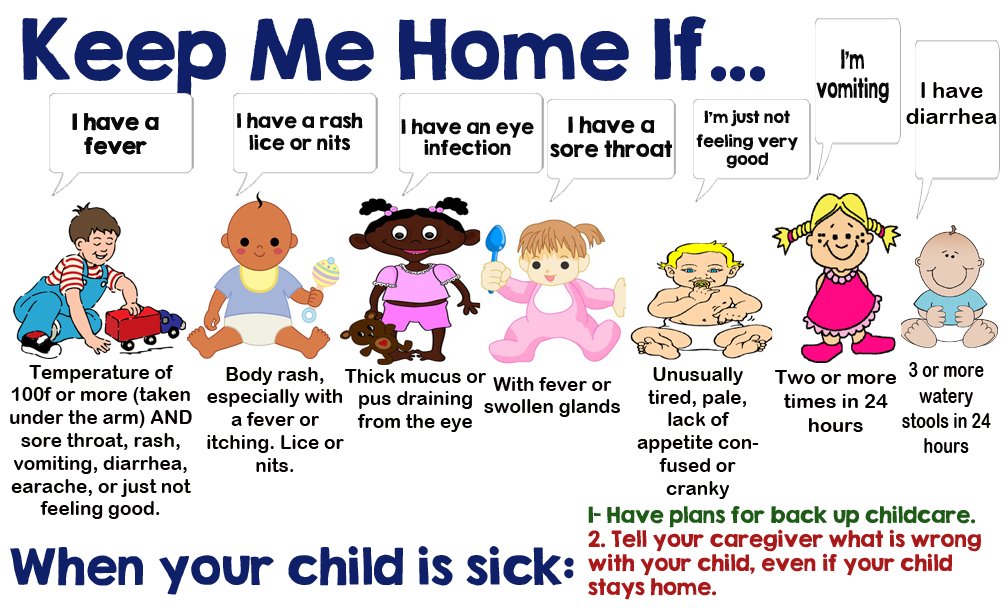 But if the child is not fed with special solutions for rehydration, if the volume of fluid losses is not replenished correctly, then vomiting and liquefied stools are dangerous because they lead to rapid dehydration and electrolyte disturbances due to loss of water and salts.
But if the child is not fed with special solutions for rehydration, if the volume of fluid losses is not replenished correctly, then vomiting and liquefied stools are dangerous because they lead to rapid dehydration and electrolyte disturbances due to loss of water and salts.
It happens that loose stools are not a serious problem if it happened, for example, once. If you observe it more often 3 times a day, this is a reason to sound the alarm, especially if you notice the first signs of dehydration:
- Decreased frequency and volume of urination. If your child has not peed for 5 hours, see a doctor immediately!
- Dryness of the skin and mucous membranes: there were fewer tears, saliva, the skin became dry and unusually flabby.
- Thirst.
When to take the child to the doctor immediately:
- The child refuses to drink (does not want to drink despite being very dehydrated).
- The child stops urinating (break more than 5 hours).
- The child is lethargic, capricious, not interested in toys (even if there is no temperature).
- "Sink" eyes or fontanel (this is rare, but it is a formidable symptom).
- There is blood in the stool (even if there is no diarrhea).
Skin rashes
Skin rashes are not always normal. If the rash is accompanied by fever, this is always a reason for urgent medical attention. There are children diagnosed with skin diseases (for example, atopic dermatitis or psoriasis), in which case the parents are usually already trained on how to behave when the rash increases or the skin process worsens. Then you need to go to the doctor if the measures taken previously recommended to you turn out to be ineffective - and you will most likely go to an allergist or dermatologist, i.e. to a specialist you know. But if the rash appeared for the first time, if the rashes are not associated with understandable provoking factors, this is an occasion to consult a doctor. Not all rashes are a sign of a serious illness, but a clear diagnosis by a specialist will calm you down and allow you to quickly deal with the problem.
Not all rashes are a sign of a serious illness, but a clear diagnosis by a specialist will calm you down and allow you to quickly deal with the problem.
Pain
Pain is always a symptom of anxiety, which the human body signals about danger. An intense and growing pain symptom is always a reason to consult a specialist. Remember that if a child is "teething" - this may be the cause of the child's capriciousness and irritability, but in the vast majority of cases it does not cause a temperature rise above 37.5 * C or severe pain. Therefore, you should not write off the symptoms that have appeared on teething.
How to understand that a child is in pain:
- The child cries, does not calm down.
- Unmotivated excitability.
- Anxiety (the child cannot find peace, a comfortable position).
Head injuries and loss of consciousness
Very often, parents go to the doctor only when the injury leaves traces (hematoma, swelling).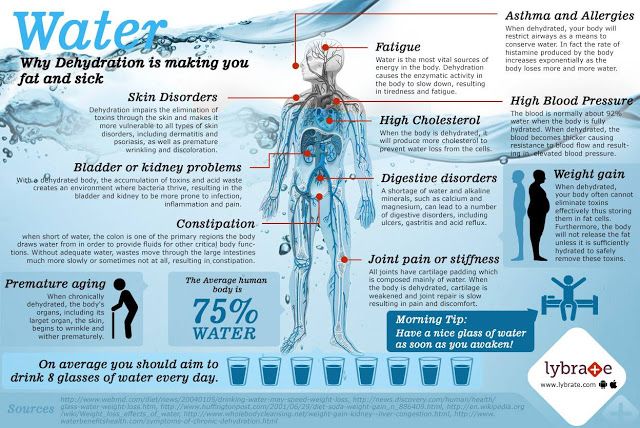 If the child fell from a certain height (even if you did not see what exactly he hit), or he hit his head, do not be too lazy to immediately go to a specialist. Not every head injury can pass without a trace, and, most importantly, you may not see the internal damage that occurred during the injury.
If the child fell from a certain height (even if you did not see what exactly he hit), or he hit his head, do not be too lazy to immediately go to a specialist. Not every head injury can pass without a trace, and, most importantly, you may not see the internal damage that occurred during the injury.
An episode of loss of consciousness, "slackness" or convulsions is always a cause for immediate medical attention.
You can read more about the Department of Emergency Pediatrics of the National Medical Research Center for Children's Health on the official website >>>
Dehydration in a child: symptoms and prevention
home
reference Information
Resources for Parents
Dehydration in a child: symptoms and prevention
Dehydration is a pathological condition in which the body loses fluid and, along with it, salts and minerals. Infants and young children are especially at risk of dehydration because they lose fluid faster than adults.
Causes of dehydration
1. Difficulty in the flow of fluid into the body. This situation is rare. This may be the refusal of the child to drink liquid, for example, due to pain when swallowing. Or these are severe pathological conditions in which the child cannot swallow on his own.
2. Increased excretion of water and minerals by the body, when the loss of fluid exceeds its intake. This situation is observed in acute infections, food poisoning, parasitic damage, overheating, burns.
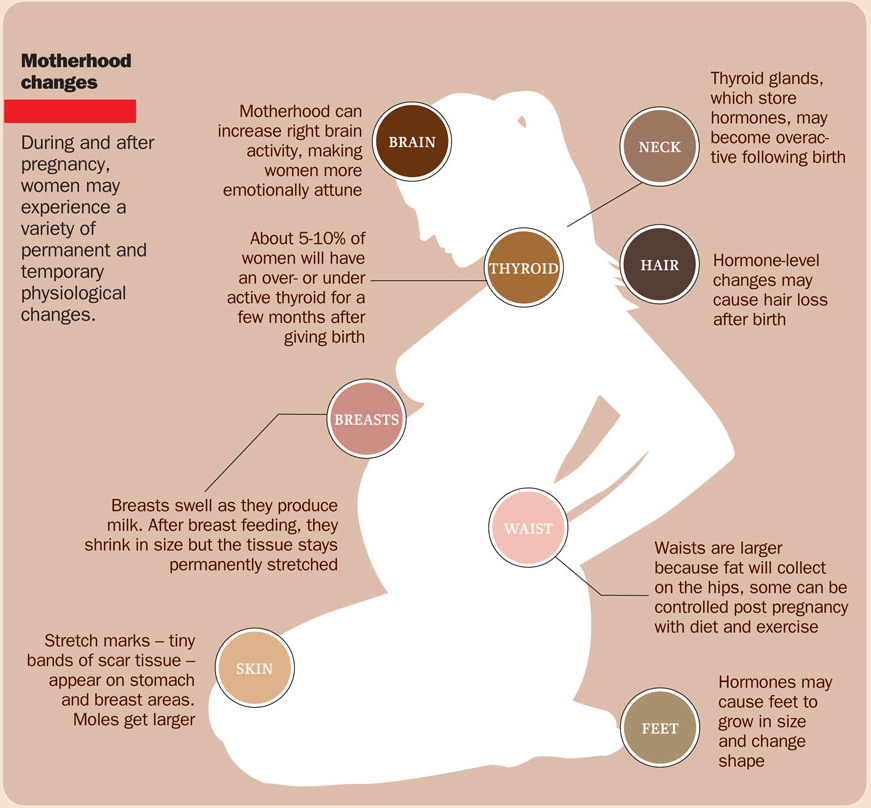
Signs of dehydration in a child: dry mucous membranes, shallow breathing, rapid pulse, low blood pressure, lethargy and irritability; decreased frequency of urination, deformation of the fontanel, lack of tears when crying.
Dehydration is a very dangerous condition, especially for children. Its most common cause is a viral infection with the following manifestations: high fever, loss of appetite, loose stools, vomiting.
In many cases, the infection is caused by rotaviruses.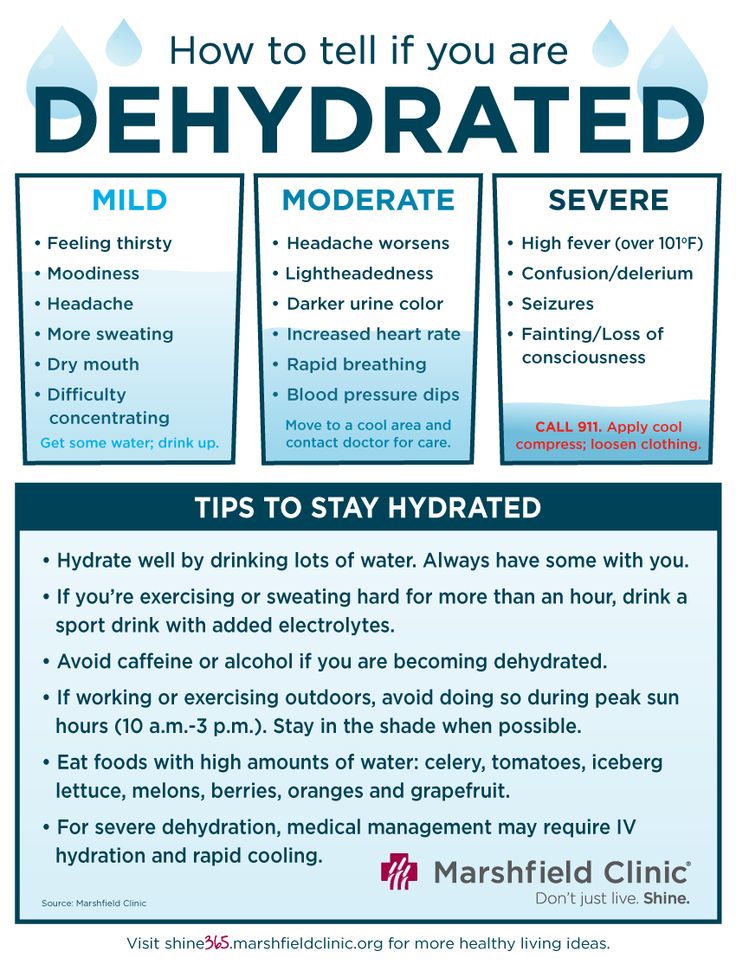
Dehydration can also be the result of the formation of wounds in the child's mouth, because they are also the result of the entry of the virus into the body. Painful mouth ulcers make it difficult for a child to eat and drink normally. Dehydration can also occur as a result of intense sweating, so on hot days you should make sure that the child consumes more fluids than usual. Always carry a bottle of water with you.
2. Symptoms of dehydration in children
The first symptoms of dehydration in infants and children are as follows: chills, weakness, crying without tears, dry mouth. In severe cases, symptoms include dry skin, a change in the smell and color of urine, and a decrease in the amount of urination. Having recognized these symptoms, it is worth thinking about how to restore the water balance of the body as soon as possible.
How to quench a child's thirst?
Water
Pediatricians always recommend water to quench your thirst. Drinking water will not cause a child to lose their appetite and will not have problems with tooth decay and obesity in the future, unlike the consequences of drinking sugary drinks.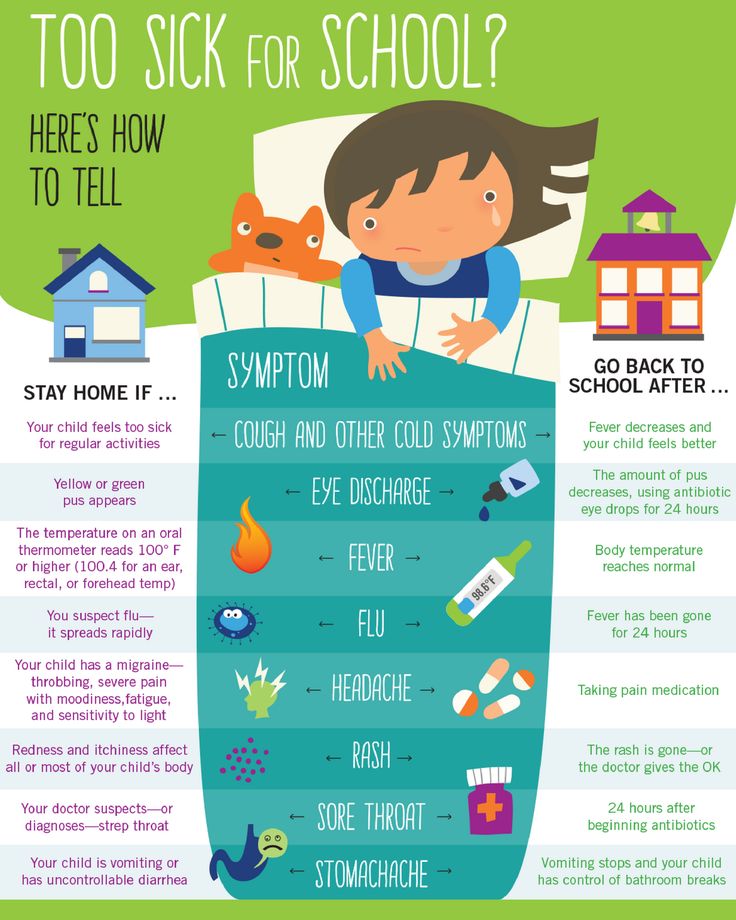
A baby only needs a few teaspoons of water a day. When he shows that he is no longer thirsty, stop the process and give the next dose in a few hours.
The water given to the child should be boiled and cooled. Even tap water filtered with special filters is not suitable for direct consumption by a child, as it contains many chemicals and metals that can be harmful to health.
Teas
Teas are also recommended for children, but only in small amounts, as babies often like the sweetened drink. You can also give your child juices, preferably diluted 1:1 with water. The most useful are low-sugar juices containing pulp, without dyes and preservatives. They are meant to be safe for children to consume.
How to avoid dehydration?
If you have already experienced the annoying problem of dehydration in your child, do not rush to panic! Read the detailed description of actions on how to avoid this phenomenon.
Give your child a small amount of water several times a day
Breastfeed your baby more often, especially in hot weather
Use drinking water, chamomile tea and light fruit infusions
Check the temperature of drinks before serving it to the child - it should be at room temperature
Remember that hot days can be dangerous not only for your baby, but also for you. At this time, be sure to have a bottle of water with you separately for yourself and your baby. When a child's dehydration is so severe that he looks visibly weak and lethargic, see a doctor as soon as possible.
At this time, be sure to have a bottle of water with you separately for yourself and your baby. When a child's dehydration is so severe that he looks visibly weak and lethargic, see a doctor as soon as possible.
In extreme cases of dehydration (accompanied by fever and diarrhoea), we are talking about inpatient treatment and the installation of a drip under the supervision of doctors
What Diet Should You Follow During Dehydration?
The most important rule during dehydration is the constant filling of the body with fluid. Not only oral rehydration fluids, but also some dietary changes play a key role in solving this problem.
Fruits and vegetables are best for consumption. Liquid products are also ideal.
It is very important to provide the child's body with the necessary nutrients that enter it with food. Your baby's diet should be free of complex carbohydrates (potatoes, rice, whole wheat bread, cereals), lean meats, and yogurt. The diet should be appropriate for the age of the child.