How to gain weight during pregnancy second trimester
How to Know If You're Not Gaining Enough
Many women struggle with gaining too much weight during pregnancy. But what happens when the opposite is true, and you’re not gaining enough weight during pregnancy? Here’s what you need to know about weight gain during pregnancy.
If you’d like to learn more about this topic in a visual way, check out my Google web stories for 6 tips to help you gain weight during pregnancy.
There may be several reasons that you’re not gaining enough weight during pregnancy—it could be due to excessive nausea, loss of appetite, food aversions, or other digestive concerns. If you’re concerned that you’re not gaining enough weigh, don’t worry. I’ve got you covered. Plus, check this out if you’re looking for the ultimate guide to pregnancy nutrition.
In this post you’ll learn:
- How to figure out how much weight you should gain
- Calorie intake during pregnancy (how do I know how much to eat?)
- How to choose calorie and nutrient-dense foods
- Why Smaller more frequent meals might help
- Why you might want to skip the salad
- Why you shouldn’t turn towards junk food for extra calories
- How to combat nausea
- How to notice food aversions
How to know whether you’re gaining the right amount of weight during pregnancy
First of all, it’s important to understand what healthy pregnancy weight gain looks like. A common way to calculate your target weight gain during pregnancy is by using your pre-pregnancy Body Mass Index (BMI).
Now, I really don’t want to get stuck on the numbers here—especially when it comes to your body mass index (BMI)—because what’s defined as “healthy” according to BMI charts can be a little deceiving or unfair. For example, someone who has lots of muscle may have a higher BMI than what’s considered “healthy,” but may be in great shape and very healthy. Or someone who has a “healthy” BMI due to their genetics may have an unvaried diet and never move their body. BMI is just one assessment tool you can use, but it’s imperfect. Don’t get stuck on it! But for those of you who like numbers, here they are:
To calculate your pre-pregnancy BMI, multiply your weight in kilograms by your height in meters squared. Or if you want a shortcut, just google “BMI calculator” and plug your numbers in. The recommended weight gain during pregnancy depends on which category the pre-pregnancy BMI lands in.
Pregnancy Weight Gain
| Prepregnancy BMI | Weight category | Weight gain for full-term pregnancy | Weight gain for full-term pregnancy with twins |
| Below 18.5 | Underweight | 28 to 40 pounds | No set guidelines |
| 18.5 to 24.9 | Normal weight | 25 to 35 pounds | 37 to 54 pounds |
| 25.0 to 29.9 | Overweight | 15 to 25 pounds | 31 to 50 pounds |
| 30.0 and above | Obese | 11 to 20 pounds | 25 to 42 pounds |
Calorie intake during pregnancy
I’m not keen on overemphasizing calorie goals or ranges because I really want to encourage you to listen to your body when it comes to the amount of food you eat at any given meal or snack. And quite frankly, counting calories sucks and takes the enjoyment out of eating! But here’s what I will tell you:
- During your first trimester, it’s not necessary to eat any more than normal.
 So just eat like you normally would!
So just eat like you normally would! - During the second trimester, it makes sense that you’re hungrier than normal, because your energy and nutrient needs are rising. It’s good to eat a little more: about 300 to 350 extra calories. That’s like an extra snack each day.
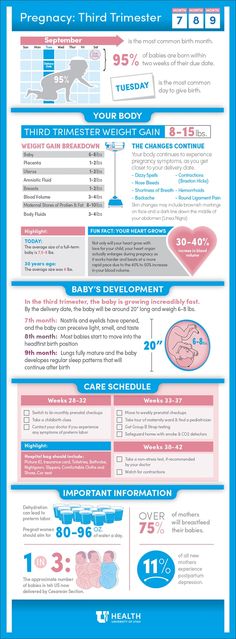
- During the third trimester is when your nutrient and energy needs are the highest throughout your pregnancy, and it’s advised to eat an extra 400 to 450 calories per day. That could be an extra snack (Greek yogurt, berries, and granola) or maybe a little more at each meal.
How many extra calories do I need (assuming that you’re starting out at a healthy BMI)?
| Stage of pregnancy | Calorie intake |
| First trimester | No additional calories |
| Second trimester | Add 300 to 350 calories per day |
| Third trimester | Add 400 to 450 calories per day |
Any additional calories that you take in should come from nutrient-dense foods such as lean protein, vegetables, fruits, and whole grains. Limit foods that are overly processed with a lot of added sugar, salt, or fat to only once in a while. But do give yourself permission to indulge once a day on something that you absolutely love and can’t live without.
Limit foods that are overly processed with a lot of added sugar, salt, or fat to only once in a while. But do give yourself permission to indulge once a day on something that you absolutely love and can’t live without.
I’m having trouble gaining enough
If you’re having trouble gaining enough weight during pregnancy, know that you’re not alone. This is a common concern and something that can be managed with a little bit of extra knowledge and even some help from a registered dietitian if you and/or your doctor are concerned. Lack of weight gain can happen because of many reasons, including:
- excessive nausea
- loss of appetite
- food aversions
- other digestive concerns
- you might be a small or particular eater to begin with, and may need to pay a little bit more attention to what and how much you’re eating.
To help ensure that you are gaining enough weight throughout your pregnancy, and in a healthy way, here are my top 6 tips:
1.
 Choose calorie-dense (and nutrient-dense) foods
Choose calorie-dense (and nutrient-dense) foodsIf you have a small appetite, it’s crucial to make every bite count! That means you want to get the most nutrition (protein, vitamins, minerals etc.)in the foods you choose. Even if you get full quickly or have a small appetite, you know you took in some great nutrition. Foods that are high in calories and chock-full of nutrients are:
- Nuts, seeds, and nut butters
- Avocados
- Olive oil as a topping or dressing
- Whole grain pasta, oats, brown rice, and other whole grains
- Legumes like lentils, chickpeas, and beans
- Fatty fish like salmon
If you’re needing some recipe inspiration for nutrient-dense meals and snacks, check out one of my fave cookbooks, Nourish. On top of this, you should be making sure that you’re taking a prenatal multivitamin, vitamin D and perhaps even an Omega-3 supplement too. Here are some nutrients (and foods) that you should be paying extra attention to during pregnancy.
2. Try smaller, more frequent meals
You may be turned off of larger portion sizes of foods, and eating might feel overwhelming if your plate is too full (which can actually decrease your appetite). Instead, try having five or six smaller more snack-sized, lighter meals that aren’t so overwhelming. For example, instead of having a big spaghetti dinner, have a piece of French toast with greek yogurt and berries. Or make a batch of homemade protein-rich muffins or energy bites that you can snack on throughout the day or on-the-go. These snack-sized meals can still pack a nutritional punch and provide the calories that you need, but might be less overwhelming and more appealing (meaning, you’ll eat more!).
3. Salads are great but may be too low in calories
Wait, what? Did a dietitian just advise you to skip a salad? While vegetables are super-healthy, they are not calorically-dense and high in fiber. A big bowl of lettuce with cucumber can make you feel full quickly, but is too low in calories. That’s not enough to meet your needs! If you really have a low appetite and can eat only a small amount, it’s better to have more calories with every bite. For example, try whole grain toast with peanut butter and banana slices (yes, you CAN and SHOULD eat peanuts when you’re pregnant), or a pasta salad with avocado, nuts, meat and cooked veggies which would have more calories than a light green salad.
That’s not enough to meet your needs! If you really have a low appetite and can eat only a small amount, it’s better to have more calories with every bite. For example, try whole grain toast with peanut butter and banana slices (yes, you CAN and SHOULD eat peanuts when you’re pregnant), or a pasta salad with avocado, nuts, meat and cooked veggies which would have more calories than a light green salad.
Look at the numbers to see what I mean:
- Whole grain toast with 1 tablespoon peanut butter and a banana: 220 calories
- 1½ cups romaine lettuce and cucumbers: 20 calories
- 1½ cups romaine lettuce, cucumbers, and 1 teaspoon dressing: 60 calories
If you ARE craving salad, what can you add to it? Maybe it means adding a tablespoon of dressing to your lettuce, and topping it with nuts, seeds, chickpeas, quinoa, avocado, or any other calorie-dense foods.
4. Energy dense foods are fine in moderation
We know what you’re thinking: “I need to eat more calories! I can have all of the ice cream I’ve ever wanted!” If only it were that easy! Yes, you need more calories. BUT. You also don’t need tons of sugar and fat. You want the calories to come from nutritious foods (see list above). Of course, you can enjoy ice cream mindfully, but please don’t get your day’s worth of calories from pint after pint of creamy goodness.
BUT. You also don’t need tons of sugar and fat. You want the calories to come from nutritious foods (see list above). Of course, you can enjoy ice cream mindfully, but please don’t get your day’s worth of calories from pint after pint of creamy goodness.
5. Combat nausea in pregnancy
Morning sickness can sometimes turn into all-day-sickness. Luckily, by the time you enter your second trimester, when weight gain starts to ramp up, nausea usually starts to wind down. If you’re one of the unlucky (approximately half of all pregnant women) who feels pregnancy-related nausea, here are some tricks that may help:
- Keep a snack on your night table. Have a bite before bed and in the morning. Soda crackers are a popular option!
- Avoid getting too hungry – that can lead to nausea. It might be your first instinct to avoid food when you feel nauseous, but that is the opposite of what you should do. Eating every two to three hours will help keep nausea at bay! Keep high calorie snack options (like nuts) with you throughout the day.
- Don’t take your nutrition supplements on an empty stomach–make sure you combine with a meal or snack.
- Try ginger. This age old-remedy is backed by science too. Try making tea with fresh ginger. You can use ginger in cooking and baking. Ginger snaps anyone?
- Stay hydrated, especially if nausea is accompanied by vomiting. Try drinking your fluids before or after meals, as opposed to with your meal. This is my favourite water bottle (that I carry around always!) to help me remember to stay hydrated.
If none of these tips help and you really can’t keep any food down, you may have hyperemesis gravidarum, and should discuss it with your doctor. They can prescribe medication to help.
6. Notice food aversions in pregnancy
There may be certain smells or flavors that turn your stomach when you’re pregnant – and often they are foods you used to love. Common food aversions are to strong flavors, such as garlic, onion, spice and coffee. If you can’t stand the taste or smell of certain foods, simply avoid them. Know that it’s totally normal, it’s common, and it will pass!
Know that it’s totally normal, it’s common, and it will pass!
Commonly Asked Questions About Pregnancy Weight Gain
How much weight should you gain while pregnant?
The weight gain ranges below are for a full-term pregnancy:
• Underweight: 28 to 40 pounds
• Normal: 25 to 35 pounds
• Overweight: 15 to 25 pounds
• “Obese”: 11 to 20 pounds
How fast do you gain weight when pregnant?
On average, people gain 1 to 4 pounds in the first trimester — but it can vary. Expect to gain ½ a pound to one pound (. 23 to . 45 kg) per week during the rest of your pregnancy. Ultimate guide to pregnancy nutrition.
How soon do you gain weight when pregnant?
Some initial weight gain will happen in the first 12 weeks of pregnancy. The majority of weight gain will occur during the second and third trimester. How much is too much?
How much is too much?
If you need some personalized guidance on your nutrition during pregnancy, contact us to book an appointment with our dietitian team (most people have coverage for our services through their health benefits plan).
Food to Grow On
Food to Grow On is the definitive guide to childhood nutrition, packed with practical advice to support you through pregnancy, and up until your little one starts school.
Laid out in an easy-to-navigate question and answer style, this book provides practical advice and support from Sarah Remmer and Cara Rosenbloom, two trusted registered dietitians (and moms). Food to Grow On is packed with hard-earned parenting wisdom and the very latest research in pediatric nutrition, so you will feel supported, understood, and ready to help your child thrive.
Buy Food to Grow On Now!
Managing your weight gain during pregnancy: MedlinePlus Medical Encyclopedia
Most women should gain somewhere between 25 and 35 pounds (11. 5 to 16 kilograms) during pregnancy. Most will gain 2 to 4 pounds (1 to 2 kilograms) during the first trimester, and then 1 pound (0.5 kilogram) a week for the rest of the pregnancy. The amount of weight gain depends on your situation.
5 to 16 kilograms) during pregnancy. Most will gain 2 to 4 pounds (1 to 2 kilograms) during the first trimester, and then 1 pound (0.5 kilogram) a week for the rest of the pregnancy. The amount of weight gain depends on your situation.
- Overweight women need to gain less (15 to 25 pounds or 7 to 11 kilograms or less, depending on their pre-pregnancy weight).
- Underweight women will need to gain more (28 to 40 pounds or 13 to 18 kilograms).
- You should gain more weight if you are having more than 1 baby. Women having twins need to gain 37 to 54 pounds (16.5 to 24.5 kilograms).
A balanced, nutrient-rich diet, along with exercise, is the basis for a healthy pregnancy. For most pregnant women, the right amount of calories is:
- 1,800 calories per day in the 1st trimester
- 2,200 calories per day in the 2nd trimester
- 2,400 calories per day in the 3rd trimester
Much of the weight that you gain during pregnancy is not fat, but is related to the baby. Here is a breakdown of how 35 pounds (16 kilograms) adds up:
Here is a breakdown of how 35 pounds (16 kilograms) adds up:
- Baby: 8 pounds (3.5 kilograms)
- Placenta: 2 to 3 pounds (1 to 1.5 kilograms)
- Amniotic fluid: 2 to 3 pounds (1 to 1.5 kilograms)
- Breast tissue: 2 to 3 pounds (1 to 1.5 kilograms)
- Blood supply: 4 pounds (2 kilograms)
- Fat stores: 5 to 9 pounds (2.5 to 4 kilograms)
- Uterus growth: 2 to 5 pounds (1 to 2.5 kilograms)
Some women are already overweight when they get pregnant. Other women gain weight too quickly during their pregnancy. Either way, a pregnant woman should not go on a diet or try to lose weight during pregnancy.
It is better to focus on eating the right foods and staying active. If you do not gain enough weight during pregnancy, you and your baby may have problems.
Still, you can make changes in your diet to get the nutrients you need without gaining too much weight. Talk to your health care provider to get help with planning a healthy diet.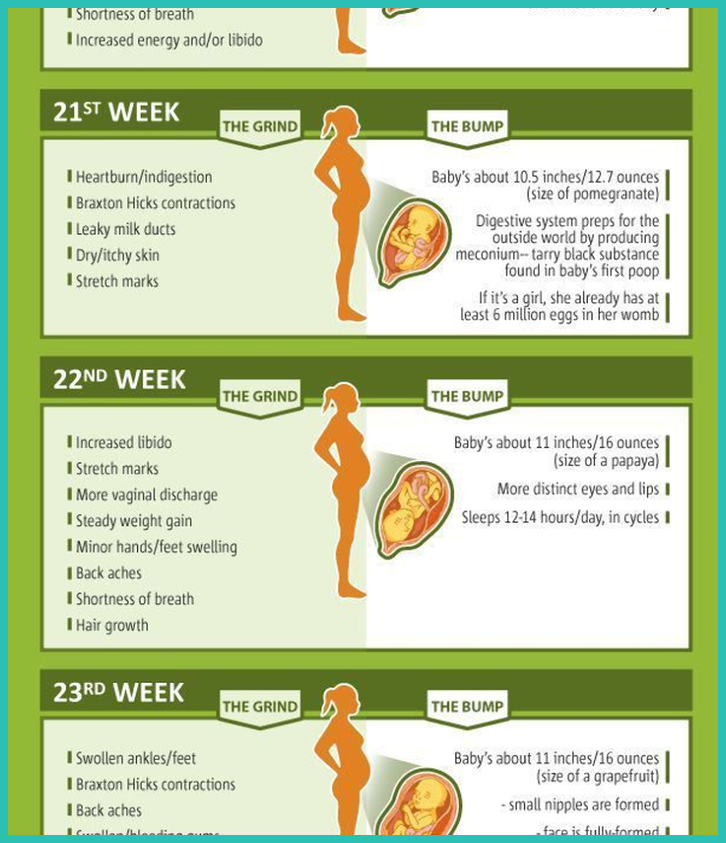
Below are some healthy eating tips to help you get started.
Healthy choices:
- Fresh fruits and vegetables make good snacks. They are full of vitamins and low in calories and fat.
- Eat breads, crackers, and cereals made with whole grains.
- Choose reduced-fat dairy products. You need at least 4 servings of milk products every day. However, using skim, 1%, or 2% milk will greatly reduce the amount of calories and fat you eat. Also choose low-fat or fat-free cheese or yogurt.
Foods to avoid:
- Naturally sweetened is better than foods and drinks with added sugar or artificial sweeteners.
- Food and drinks that list sugar or corn syrup as one of the first ingredients are not good choices.
- Many sweetened drinks are high in calories. Read the label and watch out for drinks that are high in sugar. Substitute water for sodas and fruit drinks.
- Avoid junk-food snacks, such as chips, candy, cake, cookies, and ice cream.
 The best way to keep from eating junk food or other unhealthy snacks is to not have these foods in your house.
The best way to keep from eating junk food or other unhealthy snacks is to not have these foods in your house. - Go light on fats. Fats include cooking oils, margarine, butter, gravy, sauces, mayonnaise, regular salad dressings, lard, sour cream, and cream cheese. Try the lower-fat versions of these foods.
Eating out:
- Knowing the amount of calories, fat, and salt in your food can help you eat healthier.
- Most restaurants have menus and nutrition facts on their websites. Use these to plan ahead.
- In general, eat at places that offer salads, soups, and vegetables.
- Avoid fast food.
Cooking at home:
- Prepare meals using low-fat cooking methods.
- Avoid fried foods. Frying foods in oil or butter will increase the calories and fat of the meal.
- Baking, broiling, grilling, and boiling are healthier, lower-fat methods of cooking.
Exercise:
- Moderate exercise, as recommended by your provider, can help burn extra calories.

- Walking and swimming are generally safe, effective exercises for pregnant women.
- Be sure to talk to your provider before starting an exercise program.
If you have struggled with your weight in the past, it may be hard to accept that it is OK to gain weight now. It is normal to feel anxious as the numbers on the scale edge up.
Keep in mind that you need to gain weight for a healthy pregnancy. The extra pounds will come off after you have had your baby. However, if you gain a lot more weight than is recommended, your baby will also be bigger. That can sometimes lead to problems with delivery. A healthy diet and regular exercise are your best ways to ensure a healthy pregnancy and baby.
Prenatal care - managing your weight
Berger DS, West EH. Nutrition during pregnancy. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe’s Obstetrics: Normal and Problem Pregnancies. 8th ed. Philadelphia, PA: Elsevier; 2021:chap 6.
Bodnar LM, Himes KP. Maternal nutrition. In: Resnik R, Lockwood CJ, Moore TR, Greene MF, Copel JA, Silver RM, eds. Creasy and Resnik's Maternal-Fetal Medicine: Principles and Practice. 8th ed. Philadelphia, PA: Elsevier; 2019:chap 12.
Maternal nutrition. In: Resnik R, Lockwood CJ, Moore TR, Greene MF, Copel JA, Silver RM, eds. Creasy and Resnik's Maternal-Fetal Medicine: Principles and Practice. 8th ed. Philadelphia, PA: Elsevier; 2019:chap 12.
Updated by: John D. Jacobson, MD, Professor of Obstetrics and Gynecology, Loma Linda University School of Medicine, Loma Linda Center for Fertility, Loma Linda, CA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Browse the Encyclopedia
Weight gain during pregnancy - how not to gain weight?
Contents:
- What are the optimal weight limits?
- Pregnancy Weight Chart
- How to weigh yourself correctly during pregnancy
- Why does weight gain occur?
During pregnancy, it is important for a woman to eat a varied diet so as not to deprive the unborn baby of essential minerals and nutrients. Both excessive weight gain and weight loss are equally dangerous. But evidence suggests that more than half of European and American women gain more weight during pregnancy than recommended 1 . So now is the time to give up what does not bring any benefit, but only extra pounds: sweet, fatty, fast food. Being overweight can cause problems during pregnancy and childbirth.
But evidence suggests that more than half of European and American women gain more weight during pregnancy than recommended 1 . So now is the time to give up what does not bring any benefit, but only extra pounds: sweet, fatty, fast food. Being overweight can cause problems during pregnancy and childbirth.
What are the optimal weight limits?
The average weight gain during pregnancy is about 10-12.5 kilograms 2 . But a child is born weighing 3-4 kilograms, where does everything else come from and when does the excess go away?
In addition to the fetus itself, the uterus and breasts become larger in preparation for feeding. Muscle and fat increase - the body stores energy.
This is how the weight gained by a woman during pregnancy is distributed on the eve of feeding,
0.9 kg - amniotic fluid,
1.4–1.8 kg - blood and organic fluids, thanks to which the child receives the necessary oxygen,
0.9 kg - uterus (20 times more than normal weight),
0. 7 kg - placenta, the main element through which the fetus receives nutrients.
7 kg - placenta, the main element through which the fetus receives nutrients.
Add the weight of the unborn baby, and you will get the approximate weight that a woman gains in nine months.
Doctors say that everything is individual and there are no uniform standards for how many kilograms to gain during pregnancy. But let things take their course, there is something horrible and you can’t completely forget about the scales. Watch your weight - you will avoid many problems during pregnancy and childbirth and easily return to your previous weight. You will have "strategic reserves" for feeding the baby. Don't worry, those extra pounds will go away as quickly as they appeared. But only on the condition that you eat right during pregnancy and lactation.
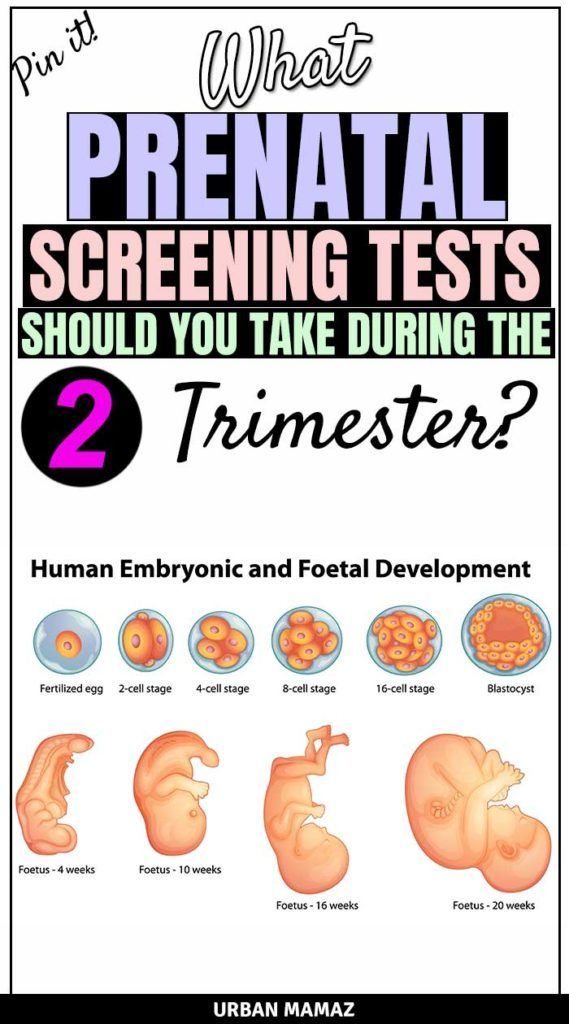
Pregnancy weight chart
The recommended weight gain during pregnancy for women with a normal body mass index is 11.5-16 kilograms. Those who are overweight during pregnancy are advised to gain a little less - from 7 to 11. 5 kilograms. Those who are expecting twins or triplets, on the contrary, should score more. For example, in a multiple pregnancy with twins for a woman of normal weight, the recommended weight gain is from 16.8 to 24.5 kilograms 3 .
5 kilograms. Those who are expecting twins or triplets, on the contrary, should score more. For example, in a multiple pregnancy with twins for a woman of normal weight, the recommended weight gain is from 16.8 to 24.5 kilograms 3 .
Trimester weight gain during pregnancy varies 3 . A woman gains the least during the first trimester - from 1.6 to 2.3 kg. Nausea in the first trimester usually causes loss of appetite and some weight loss may occur.
In the second and third trimesters, a woman gains an average of 200 to 500 g per week.
Pregnancy weight gain: weekly chart, weight in kilograms
| Week | Minimum | Average weight | Maximum |
|---|---|---|---|
| 14 | 1.1 | 1.5 | 1.9 |
| 15 | 1.6 | 2 | 2. 4 4 |
| 16 | 1.9 | 2.3 | 2.8 |
| 17 | 2.2 | 2.8 | 3.4 |
| 18 | 2.5 | 2.8 | 3.4 |
| 19 | 3 | 3.7 | 4.5 |
| 20 | 3.5 | 4.2 | 5 |
| 21 | 3.9 | 4.7 | 5.6 |
| 22 | 4.2 | 5.2 | 6.2 |
| 23 | 4.6 | 5.7 | 6.9 |
| 24 | 4.9 | 6.1 | 7.4 |
| 25 | 5.3 | 6.6 | 8 |
| 26 | 5.6 | 7 | 8.5 |
| 27 | 6 | 7.5 | 9 |
| 28 | 6.3 | 7.9 | 9.5 |
| 29 | 6.7 | 8.3 | 9.9 |
| 30 | 7 | 8. 7 7 | 10.4 |
| 31 | 7.3 | 9 | 10.8 |
| 32 | 7.5 | 9.4 | 11.3 |
| 33 | 7.8 | 9.7 | 11.7 |
| 34 | 8.1 | 10.1 | 12.1 |
| 35 | 8.4 | 10.5 | 12.6 |
| 36 | 8.6 | 10.8 | 13 |
| 37 | 9 | 11.2 | 13.5 |
| 38 | 9.3 | 11.6 | 14 |
| 39 | 9.4 | 11.7 | 14.1 |
| 40 | 9.5 | 11.8 | 14.2 |
How to weigh yourself correctly during pregnancy
Doctors do not recommend weighing yourself daily, it is not always informative, fluctuations are not always noticeable, the error is large, and in general this can lead to unnecessary worries.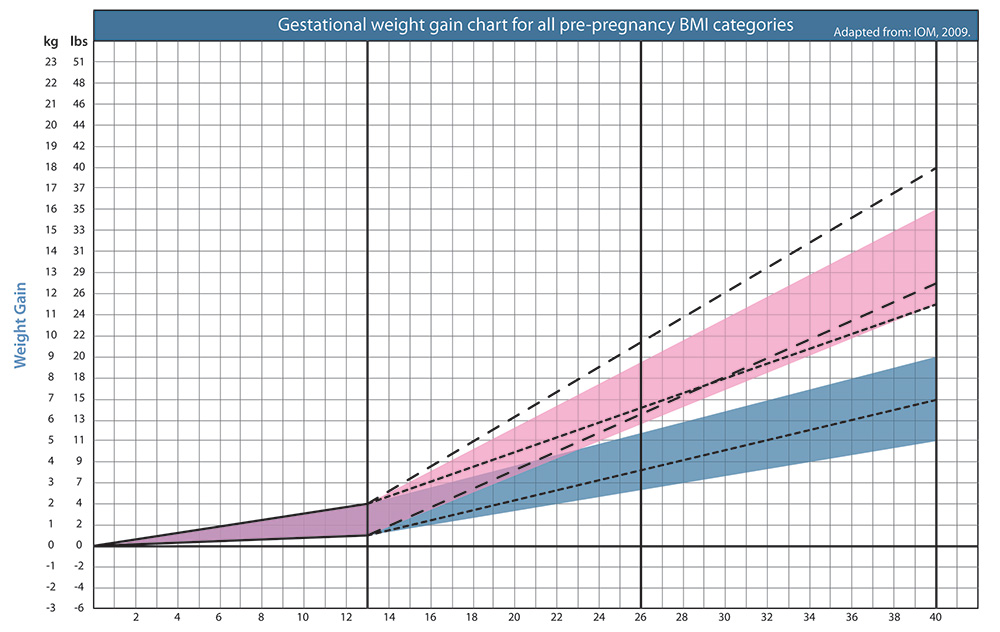 The correct option: control the weight once a week, in the morning, on an empty stomach. It is important to use the same scales, now the priority is “dynamics”. Weigh yourself only at home or in the office of your gynecologist.
The correct option: control the weight once a week, in the morning, on an empty stomach. It is important to use the same scales, now the priority is “dynamics”. Weigh yourself only at home or in the office of your gynecologist.
Why does weight gain occur?
Excess weight is caused by hormonal changes in the body, which makes the expectant mother constantly feel hungry. Many pregnant women decide that now they need to eat for two. No need. Just eat twice as good - more varied, more correct, but not more.
Sources:
* Not a drug. dietary supplement. There are contraindications. ** Estimated period of use within the Elevit line of vitamin and mineral complexes. According to the instructions, Elevit Pronatal can be used at the stage of pregnancy planning, during pregnancy, after childbirth and during breastfeeding.
- Healthy maternal nutrition: a better start to life report WHO, Regional Office for Europe 2016.
- https://www.nhs.uk/common-health-questions/pregnancy/how-much-weight-will-i-put-on-during-my-pregnancy/
- Poston L.
 Gestational weight gain // https://www.uptodate.com/contents/gestational-weight-gain, accessed 07.10.2018.
Gestational weight gain // https://www.uptodate.com/contents/gestational-weight-gain, accessed 07.10.2018.
CH-20220504-32
Weight during pregnancy. What increase is considered optimal?
Why is excessive weight gain during pregnancy particularly harmful? What should be the calorie content of the diet? How to build your diet so that you can eat varied (and tasty), but at the same time not gain too much? Let's figure it out.
What makes up weight gain during pregnancy?
An increase in the subcutaneous fat layer during pregnancy is a normal and natural process.
While the baby is growing inside you, he needs energy and external protection. But during pregnancy, weight increases not only and not so much due to the adipose tissue of the mother: there is more fluid in the body, the uterus grows, the fetus and placenta develop, and the breasts increase in preparation for the feeding process.
Interestingly, weight loss during the period of toxicosis can later provoke its increase: the body will try to regain what was lost.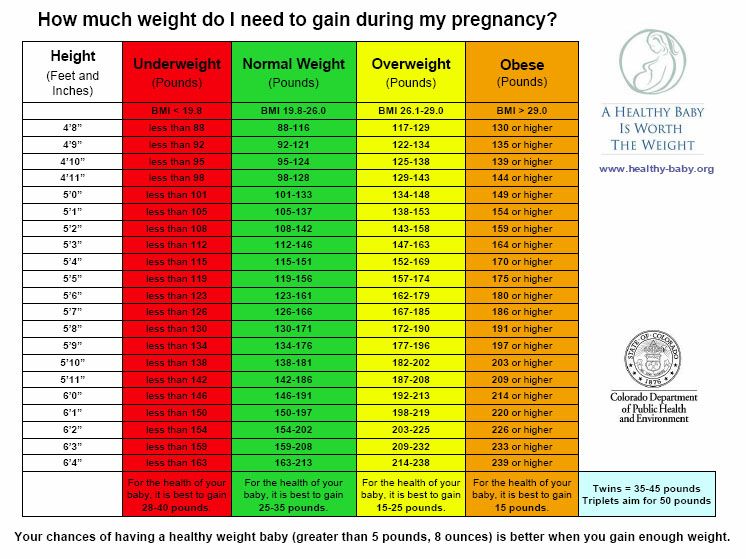
Expectant mothers especially actively gain weight in the second trimester and the beginning of the third, but closer to childbirth, a pregnant woman can even lose 1-2 kilograms.
As long as the weight grows more or less evenly and does not go beyond the upper limit of the norm, there is nothing to worry about. But if your weight is rapidly going up, you should be wary.
How to correctly calculate the weight, and what increase is considered optimal?
In Russian obstetric practice, it is generally accepted that the total increase should not exceed 12 kg. for the entire pregnancy. Of these 12 kg. 5-6 accounts for the fetus, placenta, amniotic fluid, another 1.5-2 - for an increase in the uterus and mammary glands, and only 3-3.5 - for the fat mass of a woman.
But this is a general indicator, a kind of "average temperature in the hospital." The optimal increase is calculated individually and depends on the initial weight of the pregnant woman, her age, the number of fetuses and the size of the child (children), physical activity.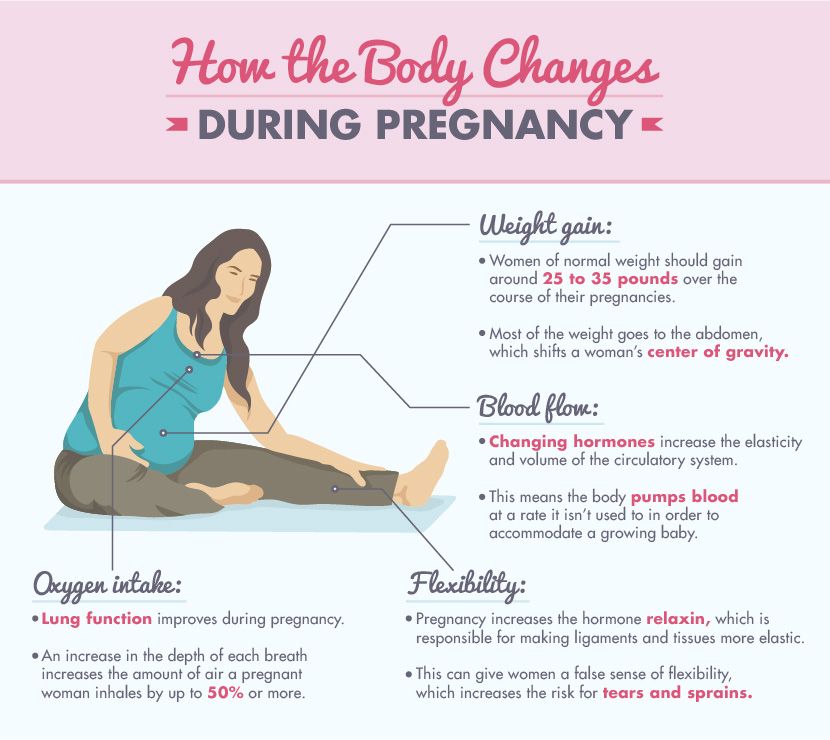
WHO recommends that optimal weight gain be calculated based on Body Mass Index (BMI).
It is determined by the formula: body weight (kg) / height squared (m).
| BMI | Recommended weight gain |
|---|---|
| 19.8-26 (normal body weight) | 12.5-15 kg |
| 26.1-29 (overweight) | 11.5 - 14 kg |
| over 29 (obese) | 7-9 kg |
How to calculate the optimal weight gain?
To do this, use the following chart:
- Calculate your BMI: Divide your initial weight in kg. for height in meters squared.
For example, your “pre-pregnancy” weight was 60 kg with a height of 170 cm.
BMI = 60: (170 x 170) = 20.76.
- A BMI of less than 18.5 indicates underweight. Indicators from 18.5 to 25 are within the norm, from 25 to 30 are above the norm, and a figure greater than 30 indicates obesity.
- Now that you know your BMI, find the optimal weekly increase in the table and compare it with yours.
| Week of pregnancy | Underweight before pregnancy (BMI less than 18.5) | Normal pre-pregnancy weight (BMI 18.5 to 24.9) | Overweight before pregnancy (BMI over 30) |
|---|---|---|---|
| 4 | 0-0.9 kg | 0-0.7 kg | 0-0.5 kg |
| 6 | 0-1.4 kg | 0-1 kg | 0-0.6 kg |
| 8 | 0-1.6 kg | 0-1.2 kg | 0-0.7 kg |
| 10 | 0-1.8 kg | 0-1.3 kg | 0-0.8 kg |
| 12 | 0-2 kg | 0-1.5 kg | 0-1 kg |
| 14 | 0.5-2.7 kg | 0.5-2 kg | 0.5-1.2 kg |
| 16 | up to 3.6 kg | up to 3 kg | up to 1. 4 kg 4 kg |
| 18 | up to 4.6 kg | up to 4 kg | up to 2.3 kg |
| 20 | up to 6 kg | up to 5.9 kg | up to 2.9 kg |
| 22 | up to 7.2 kg | up to 7 kg | up to 3.4 kg |
| 24 | up to 8.6 kg | up to 8.5 kg | up to 3.9 kg |
| 26 | up to 10 kg | up to 10 kg | up to 5 kg |
| 28 | up to 13 kg | up to 11 kg | up to 5.4 kg |
| 30 | up to 14 kg | up to 12 kg | up to 5.9 kg |
| 32 | up to 15 kg | up to 13 kg | up to 6.4 kg |
| 34 | up to 16 kg | up to 14 kg | up to 7.3 kg |
| 36 | up to 17 kg | up to 15 kg | up to 7.9 kg |
| 38 | up to 18 kg | up to 16 kg | up to 8. 6 kg 6 kg |
| 40 | up to 18 kg | up to 16 kg | up to 9.1 kg |
Recently, doctors are increasingly talking about an individual approach and urge not to panic if the increase is slightly beyond the normal range. When assessing the state of health of a pregnant woman, the doctor focuses not only on weight, but also takes into account the results of tests and examinations and other important indicators.
Why is excessive weight gain dangerous?
Gaining extra pounds can lead to gestational diabetes, hypertension, preeclampsia, or cause a caesarean section.
In addition, excessive weight gain during pregnancy may increase the risk of obesity and associated cardiovascular disease.
What can I do to keep my weight within normal limits during pregnancy?
First of all, consult a nutritionist. If there is no such doctor in the antenatal clinic, it makes sense to contact a specialist on a commercial basis.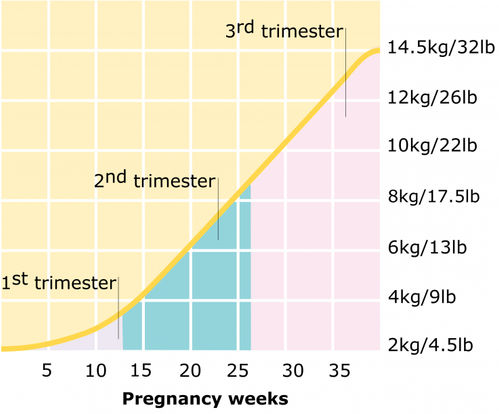 He will develop an individual diet, which will contain all the useful elements, and will offer to keep a food diary. It will also tell you how to eat right and weigh yourself.
He will develop an individual diet, which will contain all the useful elements, and will offer to keep a food diary. It will also tell you how to eat right and weigh yourself.
To prevent excessive weight gain during pregnancy, it is enough to follow simple rules of a healthy diet:
- Eat often and in small portions;
- Always have a “healthy snack” on hand: fresh apple wedges, unsweetened crackers, dried fruit, or sugar-free yogurt;
- Refuse soda, chips, sausages and sausages;
- Minimize the consumption of sweets;
- Avoid fast food;
- Limit the use of seasonings, especially salt, which retains water in the body;
- Choose steamed dishes;
- Eat more fiber-rich foods such as whole grain bread, bran, vegetables;
The diet of a pregnant woman should be varied. Include grains, vegetables, fruits, dairy products, meat and fish, legumes, or nuts.
It must be remembered that expectant mothers should never starve and adhere to extreme diets.
How many calories do you need per day during pregnancy?
It is difficult to calculate the energy value per day on your own, and then strictly adhere to a certain number of calories, and it is not necessary if it is not recommended by a nutritionist or endocrinologist. On average, you can aim for 2000-2500 calories per day, but it is important to understand that the need for calories depends on many factors: age, initial weight, health status and level of physical activity.
When should I be on the alert?
Strictly speaking, it is better for a pregnant woman not to worry and entrust her condition to a doctor who will monitor the development of pregnancy, analyzes and monitor weight. It is important to take tests to determine the level of fasting blood glucose once a trimester. The appearance of glucosuria, an increase in fasting blood glucose (more than 5.5 mmol / l) or an hour after a meal (more than 7.7 mmol / l) indicate the possible development of "diabetes in pregnancy", in connection with which the doctor will prescribe appropriate treatment .