Sharp pain in boob breastfeeding
Common Breastfeeding Problems & Solutions
If you’re new to breastfeeding, common pains-in-the-boobs can get you down. And maybe even challenge your breastfeeding goals. But a little information—and some helpful tips—can go a long way in staying the course. (Spoiler alert: an incorrect latch is often the root of the problem and a lactation consultant can help with that).
Problem: Clogged milk ductsSymptoms: A small reddish lump in your breast that feels sore or tender to the touch is likely a clogged milk duct.
Solution: Breastfeeding (or pumping) is the best remedy. Apply warm compresses before you nurse (or stand in a hot shower), give yourself a breast massage, and try a different nursing position (the dangle lets gravity works for you). If you’re prone to clogged ducts, talk to your doctor about lecithin supplements (which may make your breast milk less sticky). There’s a lack of clinical research on their efficacy, but many moms swear by them.
Good-to-know: Some moms recommend using a (clean) vibrator or electric toothbrush to massage the clogged duct. (True story.) Blocked ducts can turn into mastitis—an infection that usually requires antibiotics—so it’s important to treat them before they do.
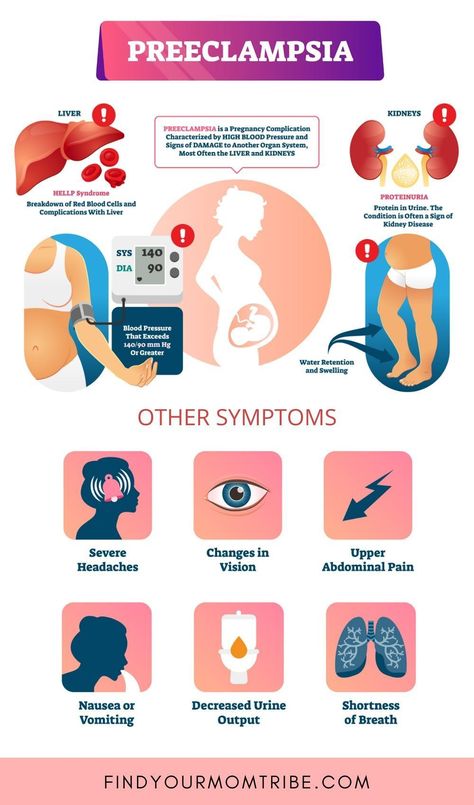
Problem: Mastitis
Symptoms: If you experience breast pain, breast swelling, or a burning sensation during breastfeeding, accompanied by a fever or chills, you could have lactation mastitis—a bacterial infection that needs to be treated with antibiotics.
Solution: To avoid developing mastitis, stick to a regular nursing/pumping schedule and completely empty your breasts every time. If your symptoms last more than 24 hours, you spike a high fever (101 or higher), or you notice pus or blood in your breast milk, consult your doctor.
Good-to-know: Breast massage and probiotics may help reduce the risk of developing mastitis, but more research is needed.
Problem: Engorged + painful breastsSymptoms: Breasts feel rock hard, tight, and heavy.
Solution: Breastfeeding or pumping—and completely emptying your breasts of milk—is the best treatment. If your breasts are still painful after a nursing session, apply a cold compress for 15 minutes every hour as needed.
Good-to-know: Putting chilled green cabbage leaves on your breasts—not your nipples—may help reduce pain and engorgement. Pro-mom tip: tuck the leaves inside your bra and leave on for 20 minutes or until they’re no longer cool.
Problem: A stabbing pain in breasts or nipplesSymptoms: Breast or nipple pain that’s stabbing, burning, or feels like pins and needles—both during and after nursing—can be the result of a vasospasm, when contracting blood cells reduces blood flow to a particular area. You may also notice your nipples turning white, then blue or red. Nipple vasospasms are related to Raynaud’s phenomenon—which affects 20 percent of women. (Some moms develop it when they’re pregnant!)
You may also notice your nipples turning white, then blue or red. Nipple vasospasms are related to Raynaud’s phenomenon—which affects 20 percent of women. (Some moms develop it when they’re pregnant!)
Solution: Dress warmly and breastfeed in a warm environment. As soon as your babe comes off your breast, place your hand over your nipple to keep it warm as you readjust your nursing bra. It also helps to place a heating pad—over your clothes—on your breast.
Good-to-know: Avoid caffeine as it can restrict blood vessels.
Problem: Sore or cracked nipplesSymptoms: Tender, sore, or chafed nipples that can develop into cracks or open wounds.
Solution: Ice your nipples (with ice cubes wrapped in a soft towel) right before you nurse to help ease the pain. After nursing, pat your nipples dry, apply breast milk or a 100% lanolin nipple cream, and keep your nipples exposed to air to help them heal. Be sure to change your (cotton!) nipple pads after each feeding. An incorrect or shallow latch is the leading cause of nipple pain, so work with a lactation consultant to ensure your baby has a good one. Persistent nipple pain is one of the main reasons moms prematurely end their breastfeeding journey, but most nipple pain subsides after the first 7-10 days postpartum. If the pain persists, see your doctor.
Be sure to change your (cotton!) nipple pads after each feeding. An incorrect or shallow latch is the leading cause of nipple pain, so work with a lactation consultant to ensure your baby has a good one. Persistent nipple pain is one of the main reasons moms prematurely end their breastfeeding journey, but most nipple pain subsides after the first 7-10 days postpartum. If the pain persists, see your doctor.
Good-to-know: Continued nursing with cracked nipples can increase your chance of developing mastitis as bacteria enter an open wound.
Problem: Milk blebsSymptoms: A small white spot on your nipple that looks like a pimple. Milk blebs—also called milk or nipple blisters—develop when skin grows over a nipple pore and creates a backlog of blocked milk.
Solution: Soak your nipples (or your whole body!) in an epsom-salt bath to help open the pore. Then apply a hot compress directly to the blister for 15 minutes. Once you've opened your pores with heat, try gentle massage to release the clogged milk or apply a little breast milk. Continue breastfeeding as your baby’s sucking helps remove milk blockages. Call your doctor if the bleb persists, you see pus, or you develop a fever.
Then apply a hot compress directly to the blister for 15 minutes. Once you've opened your pores with heat, try gentle massage to release the clogged milk or apply a little breast milk. Continue breastfeeding as your baby’s sucking helps remove milk blockages. Call your doctor if the bleb persists, you see pus, or you develop a fever.
Good-to-know: Applying a cotton ball soaked in olive oil directly on the milk bleb can help soften the skin.
Problem: ThrushSymptoms: Itchy or burning nipples, shiny or flaky skin around your nipples and areola, and shooting pain in your breasts could be a sign of thrush, an overgrowth of the yeast fungus Candida albicans.
Solution: The common treatment for thrush is a prescription antifungal medication. It also helps to wash your hands, sterilize everything that comes into contact with your babe’s mouth (as you and your babe can pass thrush back and forth—good times!), wear cotton bras (which are less likely to trap moisture), drink plenty of water, and let your nipples dry completely between nursing sessions.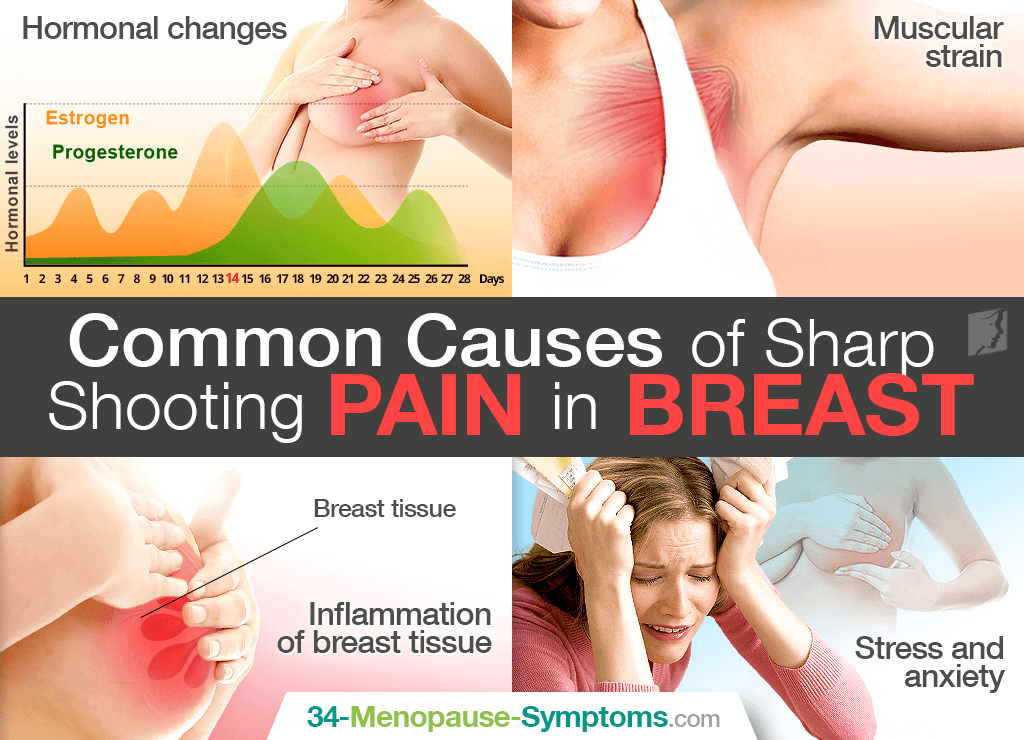
Good-to-know: Taking antibiotics and oral contraceptives can put you at higher risk for developing thrush.
More parent resources
Breastfeeding
A Pumping Guide for Breastfeeding People
Breastfeeding
Returning to work? Here’s a primer to get the pump party started.
Breastfeeding
Breastfeeding
7 Things That Can Make Breastfeeding Hard
Breastfeeding
These situations may require professional breastfeeding support.
Breastfeeding
Breastfeeding
How to Store, Freeze, and Thaw Breast Milk
Breastfeeding
The info you need to store, freeze, and thaw your liquid gold with confidence.
Breastfeeding
Breastfeeding
Fast Fixes for Common Breastfeeding Problems
Breastfeeding
Common pains-in-the-boobs can get you down and challenge your breastfeeding goals.
Breastfeeding
Breastfeeding
Breastfeeding in the Age of Coronavirus: What You Need to Know
Breastfeeding
Don’t panic. Do continue breastfeeding.
Do continue breastfeeding.
Breastfeeding
Breastfeeding
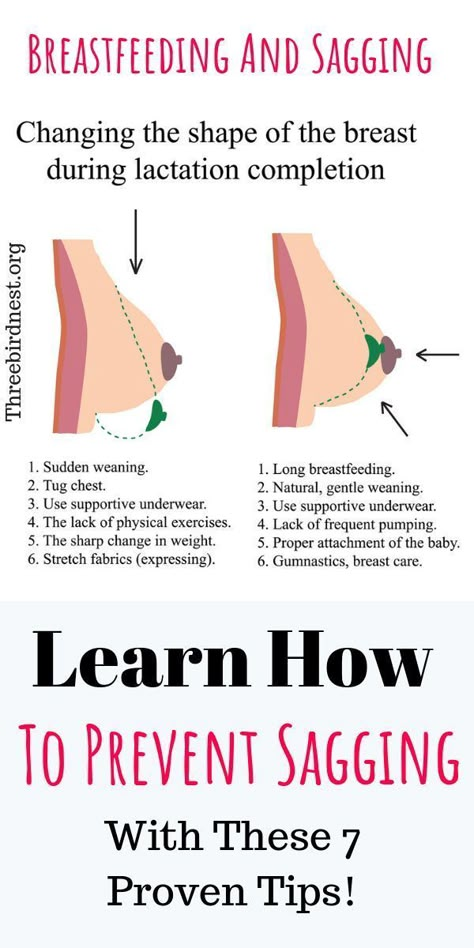
How to Wean
Breastfeeding
Your go-to guide to weaning when you’re ready.
Breastfeeding
Breastfeeding
Top Breastfeeding Tips for New and Expecting Moms
Breastfeeding
Experienced moms share their top breastfeeding tips for new (and expecting) moms.
Breastfeeding
Breastfeeding
The Worst-Case Scenario Guide for Breastfeeding
Breastfeeding
How to breastfeed with confidence, no matter what sticky situation you find yourself in.
Breastfeeding
Breastfeeding
The Best Breastfeeding Positions for New Moms
Breastfeeding
The eight best breastfeeding positions (according to moms).
Breastfeeding
Breastfeeding
How Much Do You Know About Breastfeeding?
Breastfeeding
Rumor, fact, or folklore? Test your breastfeeding know-how with this quiz.
Breastfeeding
Breastfeeding
The History of Breastfeeding
Breastfeeding
A brief history of human infant feeding—breast, bottles, and formula—through the ages.
Breastfeeding
Breastfeeding
Before You Buy a Breast Pump, Read This
Breastfeeding
Every breastfeeding mom on the go needs a breast pump. Here’s how to get one.
Breastfeeding
Breastfeeding
Top Breastfeeding Myths Busted
Breastfeeding
Stop Googling! Here are three breastfeeding myths we can bust right now.
Breastfeeding
Breastfeeding
Breastfeeding and Preemies
Breastfeeding
Five practices that help moms with preterm babies breastfeed.
Breastfeeding
Breastfeeding
Fasting and Breastfeeding: What Moms Need to Know
Breastfeeding
A breastfeeding mom’s guide to fasting for religious observance.
Breastfeeding
Breastfeeding
Breast, Bottle, Pump: Mamava’s 2019 Survey Results
Breastfeeding
Four thousands moms weigh in on how they feed their baby.
Breastfeeding
Breastfeeding
Words of Support From Breastfeeding Moms Who Get It
Breastfeeding
Seventeen breastfeeding moms share their hard-earned wisdom and messages of support for new moms.
Breastfeeding
Breastfeeding
Gloriously Nerdy Facts About Your Milk Supply
Breastfeeding
Five facts about breast milk to delight your inner nerd (and help you breastfeed).
Breastfeeding
Breastfeeding
5 Tips From a Lactation Consultant
Breastfeeding
Mamava’s boob whisperer and certified lactation consultant can help when the flowing gets tough.
Breastfeeding
Breastfeeding
Hoops and Boobs: The Breastfeeding Mama's Playbook
Breastfeeding
Breastfeeding and basketball have more in common than you think.
Breastfeeding
Breastfeeding
How to Set Yourself Up for Breastfeeding Success
Breastfeeding
Every mama, and every baby, is different, so keep the breast and leave the rest.
Breastfeeding
Breastfeeding
5 Benefits of Breastfeeding
Breastfeeding
Breastfeeding benefits babies and their mamas.
Breastfeeding
BreastfeedingMegan FulwilerBreastfeeding
Breastfeeding FAQs: Pain and Discomfort (for Parents)
Breastfeeding is natural, but it takes practice to get it right. Here's how to handle pain and discomfort during nursing.
Is It Normal to Have Cramps While Breastfeeding?
Yes. During the first few days to weeks after delivery, you may feel strong, menstrual-like cramps in your uterus when your milk “lets down” (starts to flow). This is your uterus shrinking back to a smaller size.
Is It Normal for My Breasts to Get Engorged?
During the first 2–5 days after birth, it’s normal to have engorged (very full) breasts as your milk supply increases. But if your baby nurses (or you pump) every 2–3 hours, your breasts should not feel engorged.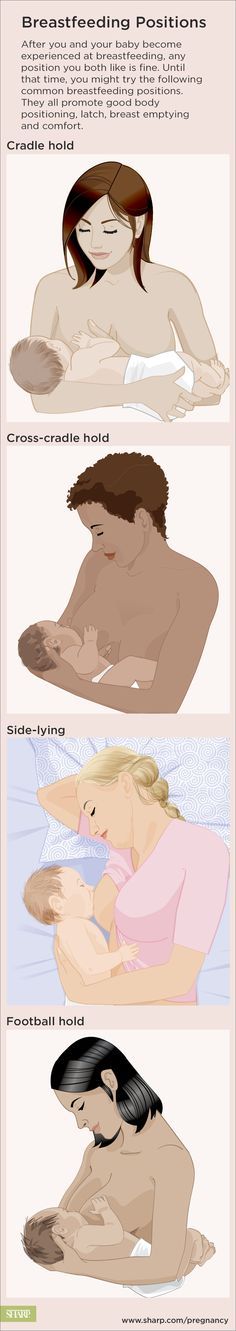
Engorgement can lead to sore, painful breasts or a breast infection. So it’s best to try to avoid it. The longer you wait to breastfeed or pump, the more uncomfortable and engorged your breasts may get.
If you can't feed your baby right away, use warm compresses and try to pump or manually express your milk. One way to express milk is to put your thumb on top of your areola and a finger below it. Gently but firmly press your thumb and fingers back against your chest wall. Then compress your fingers together to express (push out) your milk.
Is It Normal to Feel Pain During or After Breastfeeding?
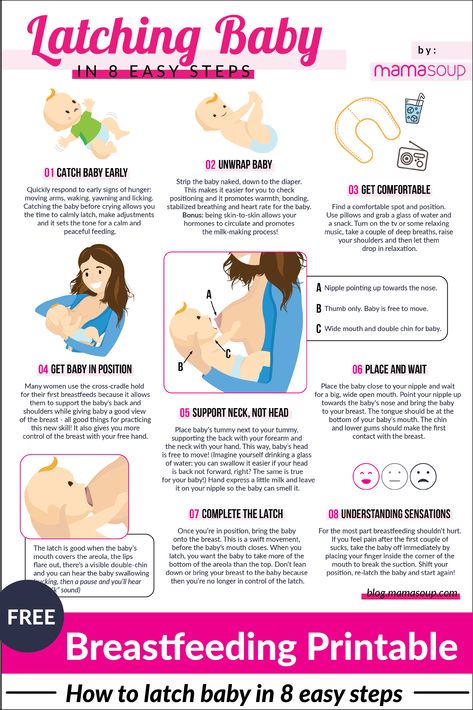
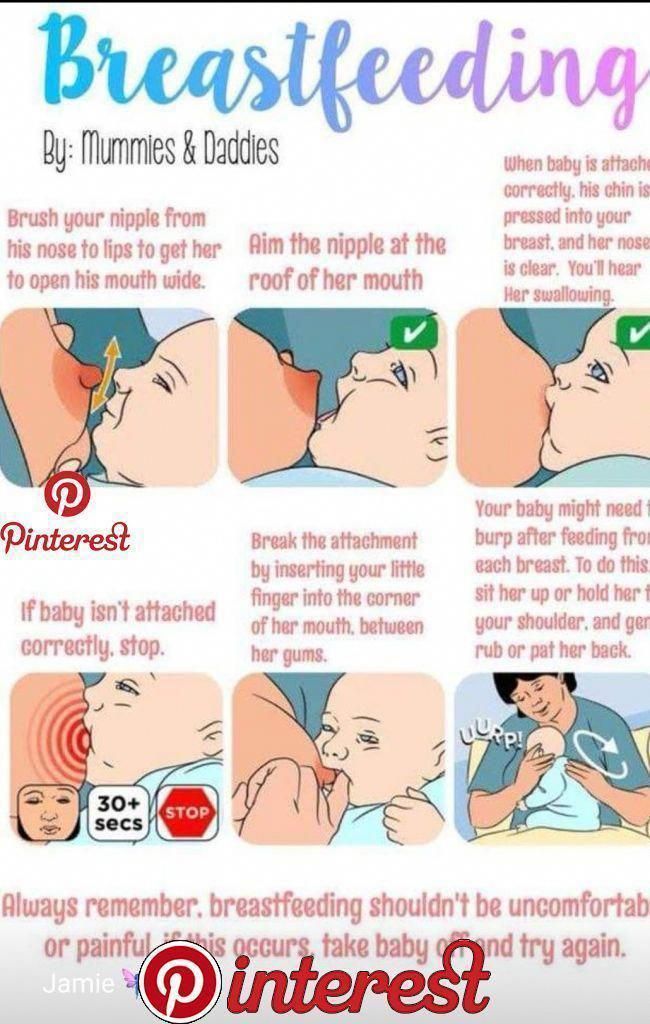
When babies latch on properly, some moms feel a few moments of discomfort at the very beginning of a nursing session. After that, discomfort should ease. You may feel a gentle tug on your breasts while your baby feeds, but it shouldn’t hurt.
If you feel discomfort during nursing, stop nursing and reposition your baby to get a better latch. Your nipple areola (the ring around the nipple) should be mostly in your baby’s mouth. When babies are latched on wrong, it can hurt or feel like a pinch each time your baby sucks. Over time, this can lead to painful, sore, cracked nipples.
When babies are latched on wrong, it can hurt or feel like a pinch each time your baby sucks. Over time, this can lead to painful, sore, cracked nipples.
If you have pain during breastfeeding, talk to your doctor or lactation consultant to make sure your baby is properly latched or that something else isn't going on.
What Else Can Cause Breast Pain?
The most common causes of breast pain include:
A plugged milk duct. Sometimes milk ducts get plugged. You may feel pain in an area of your breast or a lump may form under the skin where the duct is plugged. To help unclog the duct and ease pain:
- Take warm showers or use warm compresses on the area. Massage the area several times a day. Then, breastfeed your baby right away.
- Position your baby’s chin so that it points toward the clogged area during feeding. This will help that area of the breast empty sooner.
- Gently massage the lump while your baby feeds. It may take 2 to 3 feedings for the lump to go away.
 You also can use a manual (hand) or electric pump for a few minutes to help draw out the clogged milk while gently massaging the area.
You also can use a manual (hand) or electric pump for a few minutes to help draw out the clogged milk while gently massaging the area. - Apply cold compresses (ice wrapped in a thin towel) between feedings.
- If the lump doesn't go away within a couple of days, or if you have a fever, chills, aches, or red streaking, call your doctor.
Mastitis. This is an inflammation of the breast. If your breasts are sore; have red streaks; or have a hard, red area, you may have mastitis. Some women also get a fever and chills. If you think you have mastitis, call your doctor. In the meantime, continue to breastfeed or pump to drain the milk from your breasts. Switch between warm compresses and gentle massage right before breastfeeding and then apply cold compresses after a session. Mastitis caused by an infection may need treatment with antibiotics.
Oral thrush. Sometimes babies develop a yeast infection in the mouth called oral thrush. Babies with this have cracked skin in the corners of the mouth, and whitish or yellowish patches on the lips, tongue, or inside the cheeks. The infection can spread to your breast and cause:
Babies with this have cracked skin in the corners of the mouth, and whitish or yellowish patches on the lips, tongue, or inside the cheeks. The infection can spread to your breast and cause:
- shooting or burning breast pain either during or after feedings
- pain deep within your breast
- strong pain in the breasts or nipples that doesn't get better after your baby properly latches on or you reposition your baby
- nipples that are cracked, itchy, burning, or are pink, red, shiny, flaky, or have a rash with little blisters
Call your doctor if you or your baby have any of these symptoms.
Inverted or flat nipples. Women who have inverted nipples (nipples that turn in rather than stick out) or flat nipples (that don't become as erect as they should when a baby is nursing) may have a harder time breastfeeding or have nipple pain. If either is the case, talk to your doctor or a lactation consultant about ways to make nursing easier and reduce any pain.
How Can I Ease Breast or Nipple Pain?
During Feedings
- Nurse first on the side that's less sore and vary breastfeeding positions.
- Make sure your baby latches onto your breasts correctly. If breastfeeding is too painful, it may be more comfortable to drain your breasts by pumping the milk.
- If you have sore nipples, ask a lactation consultant or your health care provider if a nipple shield is a good idea. Nipple shields go over the areola and nipple during a feeding to protect sore or cracked nipples. They should only be used when recommended by your care team as they can sometimes affect milk supply.
- Gently break the suction when removing your baby from your breast. Slip your finger in the side of your baby's mouth, between the gums, and then turn your finger a quarter turn to do so.
- At the end of a feeding, massage some breast milk onto your nipples, and then let them air dry.
Between Feedings
- Gently massage the sore area before nursing.

- Use wet or dry heat on your breasts (a warm shower, water bottle, heating pad, or warm washcloth) right before feeding. But if you have a yeast infection in your breast, you'll need to keep your nipples dry because yeast thrives on moisture. Get plenty of rest and fluids.
- Put ice packs or cool compresses on engorged breasts after feedings.
- Make the area where you feed your baby comfortable. Sit in a glider or a cozy chair with armrests. Footstools and pillows can give extra support. Some women like wraparound nursing pillows or "husband" back pillows with arms on each side for nursing in bed.
If breastfeeding is painful or uncomfortable for you, callyour doctor or lactation consultant for help.
Solving nine breastfeeding problems in the first month
Expert advice on solving major breastfeeding problems in the first month.
Share this information
Cathy Garbin, child health nurse, midwife and lactation consultant:
Cathy, a mother of two, was a research fellow at the renowned Human Lactation Research Institute, founded by Peter Hartmann, for seven years, providing support to breastfeeding mothers in clinics and at home. Today, she still works as a family counselor, and also conducts seminars for attending physicians and speaks at international conferences.
Today, she still works as a family counselor, and also conducts seminars for attending physicians and speaks at international conferences.
Breastfeeding is as much a skill as driving a car, and in the first month mother and baby may encounter some obstacles along the way. It takes time and experience to make it familiar to both of you. Solving breastfeeding problems in the first month helps to establish good milk production and increase the duration of breastfeeding in the future. Below you will find tips on how to overcome the main breastfeeding challenges that mothers often face from the end of the first week to the end of the first month after giving birth.
Problem #1. A painful lump appeared in the breast
Lumps and lumps in the breast of a nursing woman can appear for various reasons. One of the most common is blockage of the milk ducts, which results in a hard and painful lump that can become inflamed.
Solutions 1-3
- Massage the inflamed area, especially while breastfeeding or expressing, to clear the blockage.
- Gently apply warm flannel to your breasts or take a warm shower before feeding to relieve discomfort.
- Continue breastfeeding as usual to avoid milk accumulation that can cause mastitis.
- Try to express milk from the inflamed breast after feeding to ensure that it is completely emptied. This will help to remove the blockage and restore the patency of the duct. See what breast pumps* Medela has to offer and choose the right one for you.
- Try ultrasound therapy. If you have repeated blocked ducts, your lactation consultant or healthcare professional may suggest this procedure to help restore milk flow. The procedure is performed by a physiotherapist.
- Call your healthcare provider, if you notice signs of infection (breast redness and tenderness or flu-like symptoms such as fever, aches, malaise and headache), or if you think the lump is not related to breastfeeding .
Problem #2. The breast is red and sore
If one or both mammary glands are red and sore, and this is not due to blockage of the ducts, mastitis, that is, inflammation of the breast tissue, is not excluded. Mastitis is characterized by redness, burning, and soreness of the breasts, combined with flu-like symptoms: You feel hot and cold, your joints ache, and your temperature rises above 38.5 °C (101.3 °F). Seek medical attention immediately if you experience these symptoms. Mastitis needs to be treated as soon as possible, as your condition can worsen in just a few hours. 3
Mastitis can be caused by the following causes:
- untreated blocked ducts,
- Bacteria entering the breast through cracked and damaged nipples,
- incorrect attachment of the child to the breast,
- long periods between feedings,
- breasts too full,
- wearing a bra that is too tight or that cuts into the skin,
- Abrupt weaning,
- excess milk.

Solutions 3
In addition to seeking medical attention:
- Continue to breastfeed or express milk frequently. Your milk is still safe for your baby. Its release will help eliminate blockage of the ducts and prevent painful accumulation of milk. Sudden cessation of feeding or pumping may exacerbate symptoms. After feeding, it is advisable to express any remaining milk.
- Give the child the inflamed breast first. This way the child can empty it completely. If it hurts too much, start feeding on the healthy breast, and when milk begins to flow, go back to the first one.
- Have a good rest, drink and eat. You need to get enough fluids and good nutrition.
- Massage the sore area under a warm shower or apply a warm flannel or warm pack to clear the blockage and relieve symptoms before feeding or pumping.
- Apply a cooling pack after feeding, , to reduce inflammation.
Problem #3. My strength is running out
Breastfeeding in the first weeks can be very tiring and seem endless. The baby will ask for a breast every few hours, day and night, and you have not yet grown stronger after giving birth.
Solutions
- Take care of yourself. This may be easier said than done when you have a newborn in your arms, but still try to get as much rest as possible, eat healthy and regular meals, and drink plenty of water. Do not refuse the help of your partner, relatives and friends, or even hire an assistant if you can afford it.
- Feed lying down. This will allow you to relax and reduce stress on sore spots, stitches or c-section scars.
- Do not skip feedings. Your partner may offer to bottle feed your baby while you are resting. However, despite this temptation, it should be remembered that milk production is best established in the first four weeks through breastfeeding.
 When breastfeeding is well established, you can give your baby expressed milk, but before that, ask family or friends to help you with other things so you can fully focus on breastfeeding.
When breastfeeding is well established, you can give your baby expressed milk, but before that, ask family or friends to help you with other things so you can fully focus on breastfeeding.
Problem #4. How can I increase breast milk production?
It's easy to question whether you're making enough breast milk, especially when your baby has developmental spikes between the third and fourth weeks. It may seem to you that the child asks for breasts more often because he does not have enough milk. However, if the number of wet and soiled diapers doesn't change—see Breastfeeding: What to Expect in the First Month—the baby is likely to breastfeed more often to calm down. The baby is surrounded by many new sounds and images that are easy to get tired of, and at the breast he feels safe. 4
Solutions 4.5
- Do not try to supplement your baby with formula, unless doctors are worried about weight gain or fluid loss.
 Continue breastfeeding your baby. This will help naturally increase breast milk production.
Continue breastfeeding your baby. This will help naturally increase breast milk production. - Do not feed on a schedule. Feed your baby on demand. Thus, the production of breast milk will adapt to his needs.
- Use the breast pump, , to help increase breast milk production while continuing to breastfeed.
Problem #5. I have too much milk
Hyperlactation, or too much milk, can also be difficult for you and your baby. You may experience discomfort from swollen and leaking breasts, and your baby may have difficulty latch-on, choke on the milk flowing too fast, and be unable to empty the breast properly. 6
Solutions
- Express some breast milk at the start of a feed to reduce the force of the flush. Don't pump too much as this can aggravate the situation - pump only as much as needed to ease the discomfort. Try hand pumping or use a breast pump (check out the Medela* breast pump range and choose the right one for you).

- Use towel or pad to soak up excess milk, or place the Milk Collection Pad** on the other breast while you breastfeed first.
- The child must feel supported. Hold him firmly (this gives a sense of security) and in a comfortable position so that he can turn his head. Talk to the baby during the first rapid flush, then he will not be frightened by surprise and will not push the breast.
- Contact a lactation consultant or health care professional who will monitor you and suggest single-sided feedings or hourly breast changes (“breast duty”) to normalize your milk supply.
- Be patient . Problems with milk production usually go away after a few weeks.
Problem #6. I have different breasts!
You have noticed that the baby has a preference for one breast, or that one breast produces more milk than the other, and as a result, the mammary glands have become of different sizes and shapes. This happens quite often and does not pose any problems for breastfeeding. If this does not bother you or your baby, you can leave everything as it is. If this makes you uncomfortable, try the following tricks.
This happens quite often and does not pose any problems for breastfeeding. If this does not bother you or your baby, you can leave everything as it is. If this makes you uncomfortable, try the following tricks.
Solutions
- During feeding, offer the less demanded breast first as babies usually suckle more vigorously at the beginning of feeding.
- Use the breast pump to increase breast milk production in the smaller breast.
- Don't give up on bigger breasts. Breastfeeding should continue with fuller breasts to avoid blocked ducts and mastitis.
- See a doctor. Sometimes an ear infection is the reason for a baby to latch on only one side. However, some positions may cause him discomfort, so try to keep the child more upright. In addition, a breast infection can change the taste of milk and cause milk to be rejected as well.
Problem #7.
 A blister has appeared on the nipple
A blister has appeared on the nipple With frequent feeding, sometimes painful friction occurs, and a blood bubble may appear on the breast,
nipple or areola. 7
Solutions
- Ask a lactation consultant or specialist to check the baby's latch on. A shallow grip can cause blistering of the nipples and areolas.
- Talk to your doctor about what medicine you can take to relieve pain if needed.
- Try other feeding positions to avoid pressure on the painful area.
- Lubricate inflammation with pure lanolin.
- Use Breast Pads** to avoid rubbing your blister with clothing and help it heal faster with air circulation, or try cooling hydrogel pads** to help relieve pain and promote healing.
- Try expressing milk. Using a breast pump can be an alternative way to get breast milk without bladder irritation.
 Choose the correct funnel size so that the nipple can move freely and the bubble does not rub against the walls of the tunnel.
Choose the correct funnel size so that the nipple can move freely and the bubble does not rub against the walls of the tunnel. - Do not pierce the vial as this may lead to infection.
- Seek medical attention, if the problem persists and causes you pain.
Problem #8. Painful white spot on nipple
When the orifice of the milk duct becomes blocked with milk or a thin layer of skin grows over it, a small white or yellowish spot may appear on the tip of the nipple. For some, these blocked ducts, sometimes called milk vesicles or blisters, cause pinpoint pain, especially during feeding or pumping. Others do not experience any discomfort. White blisters may persist for several days or weeks until the skin breaks and hardened milk comes out. 8
Solutions
- Follow the tips above to solve friction bubble problems.
- Remove the blockage, if you see that the milk cork is starting to bulge.
 Try to squeeze it out very gently with clean nails.
Try to squeeze it out very gently with clean nails. - Continue breastfeeding or pumping, to clear the milk duct. If the milk duct clears during feeding, it will not harm the baby in any way.
- Apply hot wet flannel to the vial just before feeding or pumping. This will help open the blocked duct. You can also try rubbing the area quickly with a clean, damp cloth.
- Manually express some milk before feeding, trying to push out hardened milk clots. If this does not help, feed the baby or express milk as usual. Repeat several times a day.
- Soak a cotton swab with olive oil and place it in the bra, pressing it against the bubble nipple. This will help soften the skin.
- Seek medical attention, if problem persists. Your doctor may remove the plug with a sterile needle. This should be done immediately after feeding, when the bubble is as inflated as possible.

Issue #9. My nipples hurt while breastfeeding
At the start of breastfeeding, my nipples may become more tender, sore, and even inflamed, but this usually goes away after a few days. If your baby's latch is checked by a specialist and the inflammation persists or the nipples hurt with every feeding, you may need medical attention to resolve this problem. 2.7
The following symptoms and signs that appear on one or both breasts during or after feeding may indicate a bacterial infection or thrush:
- burning, itching or moderate to severe pain in the nipples
- pain in nipples aggravated by contact with clothing,
- nipple pain persists despite attempts to attach baby differently,
- nipples hurt to touch,
- stitching, shooting, burning or deep aching pain,
- chest pain during feeding and almost an hour after,
- hot pink nipples,
- discoloration and texture of the areola (hot pink, darkening, dryness or peeling),
- white rash on chest or areola.

Also check if your child has the following symptoms and signs:
- hard white patches or coating on the tongue,
- white indelible spots on the cheeks,
- bright red spotted rash on buttocks not helped by diaper rash creams.
Solutions 7
- Seek medical attention. He will most likely suggest testing for infections to make a diagnosis. Bacterial and fungal (yeast) infections are treated differently, so appropriate treatment should be started as soon as possible. There are other reasons that can cause similar nipple pain, such as eczema, psoriasis or vasospasm (narrowing of the blood vessels) in the mother and problems with latch or tongue frenulum in the child. Therefore, it is very important to make an accurate diagnosis.
- Strict hygiene. Wash hands before and after feeding and applying any medication, and after changing diapers. Change bra pads regularly, wash bras, tank tops and towels in high temperature water, thoroughly wash breast cups and anything your baby puts in her mouth, such as nipples.

- Let the nipples dry after feeding, as all infections love a warm and humid environment.
- See your doctor again if there is no improvement after a few days. Do not let the problem run its course, otherwise the situation may worsen.
Related materials. Breastfeeding: what to expect in the first month
Breastfeeding: what to expect after the first month
Breastfeeding problems after the first month
Literature
1 Academy of Breastfeeding Medicine Protocol Committee. ABM clinical protocol # 20: Engorgement. Breastfeed Med. 2009;4(2):111-113.- Breastfeeding Academy Protocol Committee, "AVM Clinical Protocol #20: Breast engorgement." Brestfeed Med (Breastfeeding Medicine). 2009;4(2):111-113.
2 Jacobs A et al. S3-guidelines for the treatment of inflammatory breast disease during the lactation period. Geburtshilfe and Frauenheilkunde . 2013;73(12):1202-1208. - Jacobs A. et al., "Recommendations 2014;9(5):239-243.
2013;73(12):1202-1208. - Jacobs A. et al., "Recommendations 2014;9(5):239-243.
4 Kent JC et al. Principles for maintaining or increasing breast milk production. 2012;41(1):114-121. - Kent J.S. et al., "Principles for Maintaining and Increasing Milk Production". G Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121.
5 Amir L. Breastfeeding managing ‘supply’ difficulties. Aust fam physician . 2006;35(9):686. - - Amir L., "Breastfeeding: problems of 'supply'. Aust fam physis. 2006;35(9):686.
6 Trimeloni L, Spencer J. Diagnosis and management of breast milk oversupply Journal Am Board Fam Med . 2016;29(1):139-142. - Trimeloni L., Spencer J., "Diagnosis and correction of excess breast milk production. " Journal Am Bord Fam Med. 2016;29(1):139-142.
" Journal Am Bord Fam Med. 2016;29(1):139-142.
7 Berens P et al. Academy of Breastfeeding Medicine. ABM Clinical Protocol# 26: Persistent pain with breastfeeding. Breastfeed Med. 2016;11(2):46-53. - Behrens, P. et al., Academy of Breastfeeding Medicine, AVM Clinical Protocol #26: Persistence of Breastfeeding Pain. Brestfeed Med (Breastfeeding Medicine). 2016;11(2):46-53.
8 Australian Breastfeeding Association [Internet] White spot nipple; March 2015 [Accessed 02/08/2018]. - Australian Breastfeeding Association [Internet], "White spots on the nipples", March 2015 [visited 02/08/2018].
Read instructions before use. Consult a specialist about possible contraindications.
* RU № ФСЗ 2010/06525 of 03/17/2021
** RU ФСЗ 2010/07352 of 07/19/10
0001
“Recommend a mammologist!”
If you are a breastfeeding mother, you probably don't have much time. The child “hangs” on the chest, you get tired like never before in your life, you don’t often manage to sleep normally.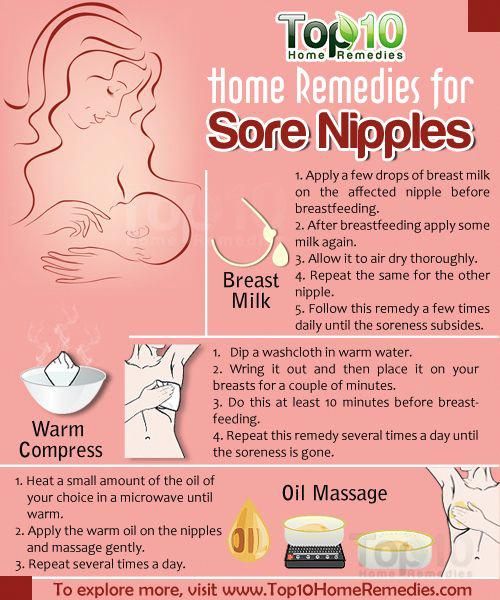 What to say about the "campaigns" to the doctors.
What to say about the "campaigns" to the doctors.
It's much easier to go to the Internet, type in a symptom in a search engine, ask for advice on the mothers' forum.
However, who guarantees that the advice will be correct and the condition will not worsen? The mammologists of our center understand your concerns and are ready to solve all the issues that arise with breastfeeding mothers.
You are breastfeeding. What's going wrong?
Not enough milk
| You think you don't have enough milk. |
| Violation of the rhythm of feeding, improper attachment, overwork. |
| The child is restless, gains or loses weight poorly. |
| Breastfeed more frequently, consult a mammologist and lactation consultant. |
Too much milk
| | You think there is too much milk. |
| Individual features, excess prolactin. |
| Too much milk is produced. |
| Change the rhythm of feeding, freeze excess milk, consult a mammologist and endocrinologist. |
Teat fissure
| Pain during feeding, skin defect, blood. |
| Heavy workload, slow recovery. |
| Limit feeding to this breast for the duration of treatment, express adequately when filling, consult a doctor for anti-inflammatories, antibiotics and physiotherapy as indicated. |
Milk stasis
| What's bothering you? | Pain and distension in the chest. |
| Possible causes? | Ejection of milk is uneven in different parts of the gland, there is no muscular wall in the milk ducts, and the outward movement of milk is also uneven. The ducts may be compressed or twisted. |
| How does it manifest itself? | Painful, tight-elastic lump in the breast, does not disappear after feeding, without fever and redness. |
| What to do? | Change position during feeding, pumping, applying ice, consult a mammologist, do ultrasound, microflora culture (bacteria culture), discharge cytology |
| What worries you? | Depends on the stage - first, a painful focus of compaction, a decrease in the amount of milk, an increase in body temperature up to 38 degrees. Further, the focus increases, there is swelling of the skin, axillary lymph nodes, high temperature, impurities in the milk. Further, redness joins, swelling increases, weakness, drowsiness, palpitations, the amount of impurities increases. |
| Possible causes | Unemptied stagnation, curdling of milk and clogging of the duct, penetration of infection through cracks leads to mastitis. |
| How does it manifest itself? | Depends on the stage - painful, stony density, swollen gland, redness of the skin, increased body temperature, symptoms of general intoxication, lactation is sharply reduced. |
| What to do? | Seek immediate medical attention, often requiring hospitalization and surgical treatment. |
There is a hardening in the chest, it does not hurt
| What worries | Abruptly appeared soft and painless mass in the mammary gland, the condition is not disturbed. |
| Possible causes | Lactocele is an acute accumulation of milk in an overdistended duct. |
| How it manifests itself | The formation is soft-elastic, painless, appeared acutely, lactation is preserved. |
| What to do | Contact a mammologist, you need ultrasound, aspiration of contents with cytology. |
Breast lump, spotting
| Painless, firm mass without clear contours in the presence of normal lactation. | |
| Possible causes? | Suspicion of an oncological process due to hormonal changes during lactation. |
| How does it manifest itself? | The formation is dense, painless, axillary lymph nodes are enlarged, lactation is preserved, there is bloody discharge from the nipple. |
| What to do? | Consult a mammologist, you need ultrasound, mammography, biopsy, cytology, histology, complex examination. |
How not to waste a breastfeeding mother's precious time? The CMC offers:
• Consultations of a competent mammologist with more than 15 years of experience with nursing mothers.
• Assistance in organizing breastfeeding - for ordinary issues we involve our consultant, in difficult situations - with the participation of our mammologist.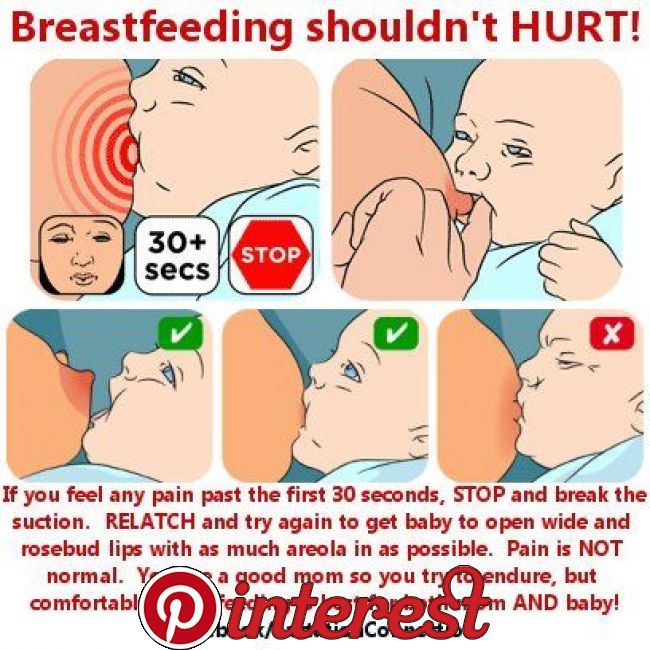
• Complete examination in 1-2 visits – we perform ultrasound, mammography, cultures, cytology and histology.
• Treatment of breastfeeding according to world standards: we perform therapeutic fine needle biopsy, therapeutic massage and pumping for lactostasis, conservative and surgical treatment.
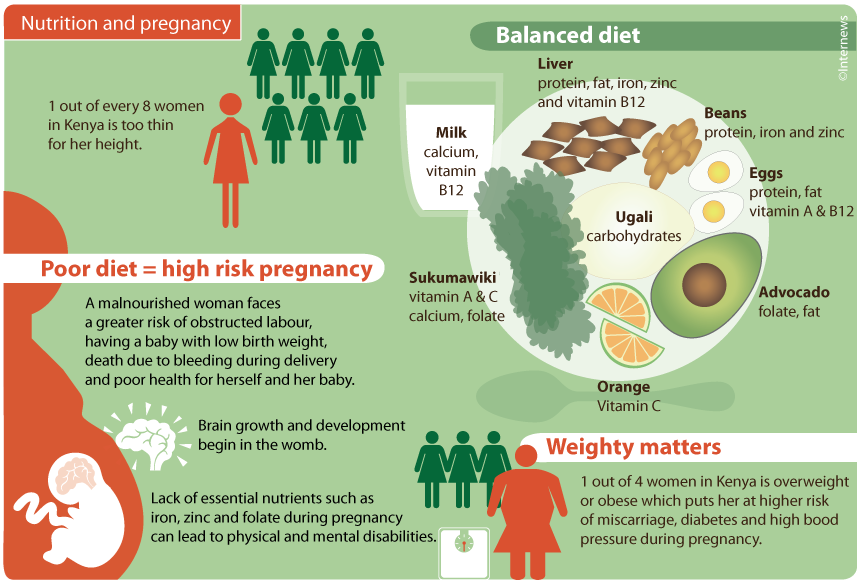
1. What should a breastfeeding mother eat?
It is best if your diet is complete, balanced in proteins, fats and carbohydrates. It is advisable to drink fluids at least 2 liters per day. Milk will come to you more actively if you drink a cup of warm tea with milk before feeding.
2. What underwear to wear?
Choose by bust size and quality. Best of all - on a wide supporting strap, you can sport a cut. Your bra should not be constricting under your armpits or tight under your bust. The composition of the fabric is cotton.
3. What should I do to avoid cracks and mastitis?
Maintain good hygiene. Apply a natural cream on the nipples with a healing and moisturizing effect after each feeding, preferably without strong odors.
 Enlarged axillary lymph nodes on one or both sides. Bloody discharge from the nipples of one or both glands.
Enlarged axillary lymph nodes on one or both sides. Bloody discharge from the nipples of one or both glands.