How can i induce labor at 37 weeks
Ways to induce labor: Medical and natural options
Most pregnancies that involve just one baby last about 40 weeks from the first day of the woman’s last menstrual period. Multiple gestation pregnancies may vary in their duration.
It is usually best to maintain a pregnancy for as long as it is safely possible to allow for continued growth and weight gain as well as fetal brain, liver, and lung development. All of these processes are essential for the health of a newborn.
Infants who are born before 39 weeks are more likely to experience complications, such as breathing difficulties, vision and hearing problems, being unable to stay warm, and feeding difficulties, among other health problems.
However, if a baby is born after 42 weeks, other problems can arise. For this reason, a doctor will sometimes recommend inducing labor.
The American College of Obstetricians and Gynecologists (ACOG) recommend classifying full-term pregnancies in one of four ways.
The categories are:
- Early-term: Delivery occurs between 37 weeks and 38 weeks and 6 days.
- Full-term: Delivery takes place after 39 weeks but before 40 weeks and 6 days.
- Later-term: Delivery is within 6 days after 41 weeks.
- Post-term: Delivery happens at any time after week 42.
Doctors do not know why some women have post-term deliveries, but a 2012 study suggests that possible reasons may include:
- hormonal factors
- obesity, possibly because fatty tissue affects the balance of hormones in the body
- genetic factors, as parents who were born post term appear to be more likely to have a post-term delivery
- having a baby for the first time
Preventing the risks of a post-term delivery
Post-term pregnancies may carry a higher risk of delivery complications.
Risks to the baby include:
- increased fetal size, which can make injury more likely during delivery
- inhaling fecal waste, which can lead to lung problems in the newborn
- the aging of the placenta and low pH levels in the umbilical cord, leading to neonatal acidemia (low blood pH)
- issues arising from growth restriction in the womb, such as wrinkled, peeling skin and a thin body due to malnourishment
Risks to the woman include:
- the need for a cesarean delivery
- a higher chance of tearing when giving birth
- an obstructed, slow, or delayed labor
- a negative emotional effect, as waiting tends to increase anxiety
In some situations, a doctor may recommend inducing, or bringing on, labor. However, they will first consider the risks, benefits, and necessity of the intervention.
However, they will first consider the risks, benefits, and necessity of the intervention.
A doctor may recommend inducing labor in instances in which:
- they have concerns about the health of the woman or baby
- the post-term date is approaching
- there is an infection in the uterus
- there is delayed fetal growth
- the levels of amniotic fluid are low
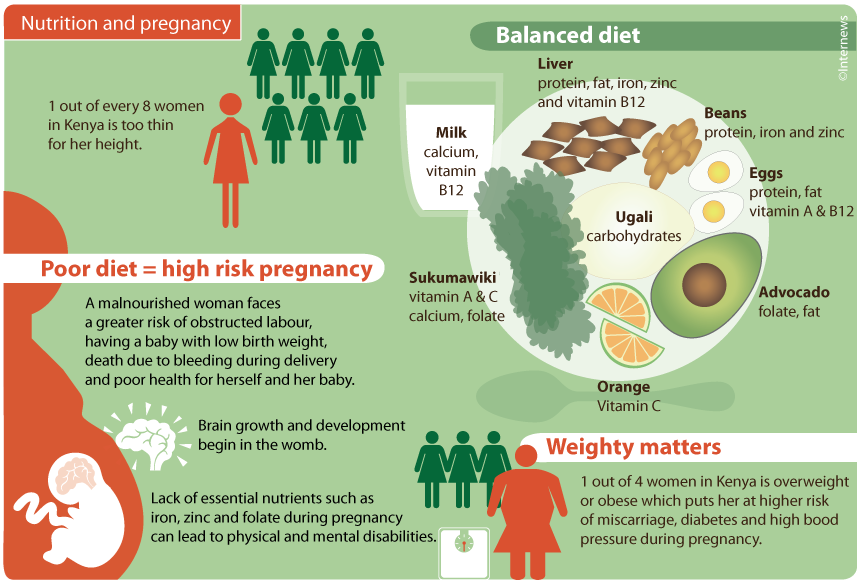
Certain medical conditions may pose a risk to the woman or baby, including:
- high blood pressure
- preeclampsia
- diabetes
- kidney disease
- blood problems due to rhesus (Rh) factor issues
Rh factor is a protein that is sometimes present on the surface of red blood cells. People with this protein in their blood have Rh-positive blood, while those who do not have this protein have Rh-negative blood.
Problems can arise if the fetus has Rh-positive blood, but the woman’s blood is Rh-negative.
Typically, maternal blood does not mix with fetal blood during pregnancy. However, this can sometimes occur during a medical procedure, such as amniocentesis, or if the woman experiences trauma to the abdomen.
However, this can sometimes occur during a medical procedure, such as amniocentesis, or if the woman experiences trauma to the abdomen.
If it does happen, the woman will develop antibodies against the Rh factor of the fetus, and her body will fight against the unborn baby’s blood. This attack can be life-threatening for the unborn child, and it can also result in complications with subsequent pregnancies.
If it is necessary to induce labor, a healthcare professional will use certain medications and procedures to cause labor to start.
These procedures include:
Cervical ripening
It is possible to ripen, or dilate, the cervix by inserting a catheter with a small balloon-type device on the end or by introducing a substance that absorbs water.
Amniotomy
A healthcare professional may burst the amniotic sac that surrounds the baby inside the uterus to start labor or to progress labor that has already begun. They can only perform this procedure if the cervix has dilated enough to make the amniotic sac accessible.
Hormones
Doctors may use naturally occurring chemicals called prostaglandins to try to soften and thin out the cervix and encourage cervical dilation. They deliver prostaglandins to the cervix through the vagina. In some cases, they may administer the hormone oxytocin to induce labor by stimulating contractions.
Stripping the membranes
This method can help release prostaglandins to induce labor, according to ACOG. A doctor or midwife will use a finger to “sweep” over the membranes connecting the amniotic sac to the uterine wall.
According to one source, this may be uncomfortable for some women and is only possible following the dilation of the cervix.
As with any medical procedure, labor induction involves some risks.
These include:
- strong, frequent contractions that can lead to fetal complications, such as an increased heart rate and umbilical cord problems
- maternal or fetal infections
- torn uterus
- increased likelihood of a cesarean delivery
- fetal death
Some women may seek out natural or nonmedical ways to induce labor at home. However, some of these methods may not be safe.
However, some of these methods may not be safe.
It is essential to discuss any thoughts of induction with a healthcare professional. There are several factors to consider before deciding on any method of induction. These include the gestational age of the fetus, the fetal position, and any pregnancy complications.
Some natural methods of inducing labor that people have tried include:
Nipple stimulation
Nipple rolling or gentle rubbing may lead to a release of oxytocin, which could help induce labor.
Exercise
Exercise is advisable during pregnancy unless a doctor specifies otherwise. However, there is no evidence that it can induce labor.
Sex
Having sex could help induce labor because orgasms cause uterine contractions, nipple stimulation triggers the release of oxytocin, and semen contains high levels of prostaglandins.
An Iranian study of 120 women concluded that sex during the last week of pregnancy “might be associated with the onset of labor” and could be a natural way to induce this process.
However, a 2012 study of almost 1,200 women in Malaysia found no difference in labor and delivery whether or not the women had sex with the aim of inducing pregnancy.
It is generally safe to have sex during pregnancy, but it is not advisable:
- after labor has started
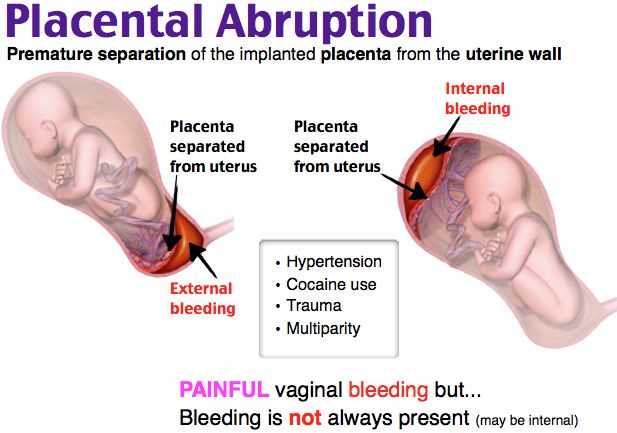
- if the woman has a low-lying placenta
- if there is vaginal bleeding
In some cases, sex during pregnancy could lead to bleeding, putting the health of both the woman and baby at risk. Women should talk with their doctor if they have any concerns about having sex during pregnancy.
Homeopathy and herbs
Some people recommend herbs and homeopathic remedies to induce labor. The authors of a study that BMJ Open published in 2018 concluded that even though some herbs may be effective, there is a lack of evidence to confirm that they are safe to use.
It is vital to discuss the safety of using herbs to induce labor with a doctor or midwife before trying this method.
Castor oil
Some people have recommended taking castor oil to trigger contractions. Doing this may cause a stomach upset, but it is unlikely to initiate labor.
The authors of a 2012 review concluded that castor oil and evening primrose oil are not likely to induce labor and may increase the risk of complications.
Food
Anecdotal evidence suggests that some foods, including spicy foods and pineapple, may induce labor.
However, there is a lack of scientific evidence to support these claims, and these foods may worsen acid reflux, which is already a common problem in the later stages of pregnancy.
Some have argued that because pineapple contains an enzyme called bromelain, which people use to tenderize meat, eating it might cause the cervix to soften.
However, stomach acids break down any enzymes in food, so they will not travel directly to the cervix.
In some cases, a doctor may decide that it is necessary to induce labor to try to ensure the safety of the woman and baby.
Several medical procedures can help encourage labor to start, and people can also try a variety of natural methods at home with the approval of their doctor or midwife.
It is important that people speak with their doctor or midwife about any methods of labor induction and the associated risks and benefits.
How to induce labor naturally
Around 38 weeks into their pregnancies, I start to see a shift in my expecting patients. The excitement of being pregnant has worn off. They are sore, uncomfortable and often feeling a great deal of pregnancy fatigue.
This is also usually when I start getting questions about natural ways to induce labor.
“Is it true that eating spicy food will get things going?” “Does drinking castor oil really work?”
Some of my expecting moms are willing to try just about anything at this point, and the internet provides endless ideas. However, I always caution that very few methods have been proven effective in getting labor started. And some methods can actually be dangerous for both mom and baby.
And some methods can actually be dangerous for both mom and baby.
Here are six natural ways to induce labor that I get questions about from my patients, and the advice I share with them. I recommend that you first get your doctor’s permission before trying any of these methods as a way to induce labor.
1. Exercise
Walking and exercise often make it to the top of the list of things to try. While there’s no research that says it will induce labor, 30 minutes of moderate exercise at least five times a week can be helpful in any stage of pregnancy. And, it’s safe to use a birthing or exercise ball to stretch and help relieve some of the pressure in your pelvis, hips and back (unless you’ve been instructed otherwise by your doctor). Staying fit can help improve sleep and your mood. It can also decrease your risk of cesarean delivery and gestational diabetes.
2. Spicy foods
Spicy foods can make you sweat, but they won’t induce labor. That’s an old wives’ tale. Research has shown that eating spicy food can trigger heartburn and indigestion, but as for labor, there has been no documented research to prove this theory.
Research has shown that eating spicy food can trigger heartburn and indigestion, but as for labor, there has been no documented research to prove this theory.
3. Sexual intercourse
You might be wondering “How would sex induce labor?” For starters, it can release oxytocin from the brain – the same chemical that causes contractions. And it can also release prostaglandins, which help the cervix naturally soften and prepare for labor. Be sure to ask your doctor whether you have the go-ahead to give sex at this time a try. If you’re given the okay, it’s certainly one of the more fun ways to try and get labor going.
4. Acupuncture and acupressure
Using acupuncture, acupressure or massage to induce labor is somewhat controversial. The belief is that stimulating certain pressure points in the body can release oxytocin and induce labor. While the effectiveness of this method is still up for debate, a foot massage is still enjoyable, especially at the end of pregnancy. And massage therapy can help treat the hip, back, ligament and musculoskeletal pain you might feel while pregnant. Both are very safe as long as the care professional has experience in taking care of pregnant women. Here at Park Nicollet, we’re lucky to have massage therapists specifically trained to work with pregnant women and their much more loose and relaxed muscles and joints.
And massage therapy can help treat the hip, back, ligament and musculoskeletal pain you might feel while pregnant. Both are very safe as long as the care professional has experience in taking care of pregnant women. Here at Park Nicollet, we’re lucky to have massage therapists specifically trained to work with pregnant women and their much more loose and relaxed muscles and joints.
5. Nipple stimulation to induce labor – discouraged
Some of my patients ask me whether using a breast pump can help start labor. Similar to sex, nipple stimulation can lead to oxytocin release. However, there is no research that shows using a breast pump to induce labor is safe or effective, so I discourage my patients from trying this method.
6. Castor oil to induce labor – highly discouraged and potentially dangerous
Castor oil can cause uterine contractions. But, the contractions may or may not be labor. The theory is that castor oil stimulates the bowels, which irritates the uterus and causes contractions. This can lead to side effects like diarrhea, nausea and vomiting – all of which can lead to dehydration. I highly discourage my patients from trying this method.
This can lead to side effects like diarrhea, nausea and vomiting – all of which can lead to dehydration. I highly discourage my patients from trying this method.
Be patient, and remember these methods for later
At the end of the day, your baby will come when they are ready. But once you’re in labor, some of the things listed above may actually help it progress. Walking, acupuncture, massage and more can also be used as natural ways to manage labor and delivery pains.
Until then, try to stay comfortable and be patient. And know that, if needed, your doctor can help you get your labor started safely and effectively.
Induction of labor in women with normal pregnancies of 37 weeks or more
Does a policy of inducing labor at 37 weeks or more of gestation reduce the risks for infants and their mothers compared with a policy of waiting until a later gestational age or until Will there be indications for labor induction?
This review was originally published in 2006 and subsequently updated in 2012 and 2018.
What is the problem?
The average pregnancy lasts 40 weeks from the start of a woman's last menstrual period. Pregnancies lasting more than 42 weeks are described as "post-term" and therefore the woman and her doctor may decide to give birth by induction. Factors associated with postnatal pregnancy and delayed delivery include obesity, first birth, and maternal age over 30 years.
Why is this important?
Protracted (term) pregnancy may increase risks for infants, including greater risk of death (before or shortly after birth). However, induction (stimulation or induction) of labor can also pose risks to mothers and their babies, especially if the woman's cervix is not ready for delivery. Current diagnostic methods cannot predict risks to babies or their mothers per se, and many hospitals have specific policies regarding how long a pregnancy can last.
What evidence did we find?
We searched for evidence (July 17, 2019) and identified 34 randomized controlled trials in 16 different countries involving more than 21,500 women (mostly at low risk of complications). The trial compared a policy of induction of labor after 41 completed weeks of gestation (>287 days) with a policy of waiting (expectant management).
The trial compared a policy of induction of labor after 41 completed weeks of gestation (>287 days) with a policy of waiting (expectant management).
Labor induction policies were associated with fewer perinatal deaths (22 trials, 18 795 babies). Four perinatal deaths occurred in the induction policy group compared with 25 perinatal deaths in the expectant management group. Fewer stillbirths occurred in the induction group (22 trials, 18,795 infants): two in the induction group and 16 in the expectant management group.
Women in the induction of labor groups in the included studies were probably less likely to deliver by caesarean section than in the expectant management groups (31 studies, 21,030 women), and there was probably little or no difference when compared with assisted vaginal delivery (22 studies, 18,584 women).
Fewer infants were admitted to the neonatal intensive care unit (NICU) in the induction policy group (17 trials, 17,826 infants; high-certainty evidence). A simple test of the baby's health status (Apgar score) at five minutes after birth was likely to be more favorable in the induction groups than expectant management (20 trials, 18,345 infants).
A simple test of the baby's health status (Apgar score) at five minutes after birth was likely to be more favorable in the induction groups than expectant management (20 trials, 18,345 infants).
An induction policy may make little or no difference for women who have had a perineal injury, and likely has little or no effect on the number of women with postpartum hemorrhage or breastfeeding at hospital discharge. We are uncertain about the effect of induction or expectant management on length of stay in the maternity hospital due to the very low certainty of the evidence.
Among newborns, the number of children with trauma or encephalopathy was similar in both groups (moderate and low-certainty evidence, respectively). None of the studies reported the development of neurodevelopmental problems during follow-up of children and postpartum depression in women. Only three trials reported some measure of maternal satisfaction.
What does this mean?
An induction policy compared to expectant management is associated with fewer infant deaths and probably fewer caesarean sections; and probably has little or no effect on assisted vaginal delivery. Determining the best time to offer induction of labor to women at 37 weeks' gestation or more requires further study, as well as further study of women's risk profiles and their values and preferences. Discussing the risks of induction of labor, including benefits and harms, can help women make an informed choice between induction of labor, especially if the pregnancy lasts more than 41 weeks, or expectant management—waiting and/or waiting until labor is induced. Women's understanding of induction, procedures, their risks and benefits is important to influence their choice and satisfaction.
Determining the best time to offer induction of labor to women at 37 weeks' gestation or more requires further study, as well as further study of women's risk profiles and their values and preferences. Discussing the risks of induction of labor, including benefits and harms, can help women make an informed choice between induction of labor, especially if the pregnancy lasts more than 41 weeks, or expectant management—waiting and/or waiting until labor is induced. Women's understanding of induction, procedures, their risks and benefits is important to influence their choice and satisfaction.
Translation notes:
Translation: Alekseeva Lada Igorevna. Editing: Prosyukova Ksenia Olegovna and Ziganshina Lilia Evgenievna. Russian translation project coordination: Cochrane Russia - Cochrane Russia, Cochrane Geographic Group Associated to Cochrane Nordic. For questions related to this translation, please contact us at: [email protected]
Induction of labor or induction of labor
The purpose of this informational material is to familiarize the patient with the induction of labor procedure and to provide information on how and why it is performed.
In most cases, labor begins between the 37th and 42nd weeks of pregnancy. Such births are called spontaneous. If drugs or medical devices are used before the onset of spontaneous labor, then the terms "stimulated" or "induced" labor are used in this case.
Labor should be induced when further pregnancy is for some reason unsafe for the mother or baby and it is not possible to wait for spontaneous labor to begin.
The purpose of stimulation is to start labor by stimulating uterine contractions.
When inducing labor, the patient must be in the hospital so that both mother and baby can be closely monitored.
Labor induction methods
The choice of labor induction method depends on the maturity of the cervix in the patient, which is assessed according to the Bishop scale (when viewed through the vagina, the position of the cervix, the degree of its dilatation, consistency, length, position of the presenting part of the fetus in the area pelvis). Also important is the medical history (medical history) of the patient, for example, a past caesarean section or operations on the uterus.
Also important is the medical history (medical history) of the patient, for example, a past caesarean section or operations on the uterus.
The following methods are used to induce labor:
- Oral misoprostol is a drug that is a synthetic analogue of prostaglandins found in the body. It prepares the body for childbirth, under its action the cervix becomes softer and begins to open.
- Balloon Catheter – A small tube is placed in the cervix and the balloon attached to the end is filled with fluid to apply mechanical pressure to the cervix. When using this method, the cervix becomes softer and begins to open. The balloon catheter is kept inside until it spontaneously exits or until the next gynecological examination.
- Amniotomy or opening of the fetal bladder - in this case, during a gynecological examination, when the cervix has already sufficiently dilated, the fetal bladder is artificially opened. When the amniotic fluid breaks, spontaneous uterine contractions will begin, or intravenous medication may be used to stimulate them.

- Intravenously injected synthetic oxytocin - acts similarly to the hormone of the same name produced in the body. The drug is given by intravenous infusion when the cervix has already dilated (to support uterine contractions). The dose of the drug can be increased as needed to achieve regular uterine contractions.
When is it necessary to induce labor?
Labor induction is recommended when the benefits outweigh the risks.
Induction of labor may be indicated in the following cases:
- The patient has a comorbid condition complicating pregnancy (eg, high blood pressure, diabetes mellitus, preeclampsia, or some other condition).
- The duration of pregnancy is already exceeding the norm - the probability of intrauterine death of the fetus increases after the 42nd week of pregnancy.
- Fetal-related problems, eg, problems with fetal development, abnormal amount of amniotic fluid, changes in fetal condition, various fetal disorders.

- If the amniotic fluid has broken and uterine contractions have not started within the next 24 hours, there is an increased risk of inflammation in both the mother and the fetus. This indication does not apply in case of preterm labor, when preparation of the baby's lungs with a special medicine is necessary before delivery.
- Intrauterine fetal death.
What are the risks associated with labor induction?
Labor induction is not usually associated with significant complications.
Occasionally, after receiving misoprostol, a patient may develop fever, chills, vomiting, diarrhea, and too frequent uterine contractions (tachysystole). In case of too frequent contractions to relax the uterus, the patient is injected intravenously relaxing muscles uterus medicine. It is not safe to use misoprostol if you have had a previous caesarean section as there is a risk of rupture of the uterine scar.