Safe supplements pregnancy
What’s Safe and What’s Not
If you’re pregnant, you may think that feeling overwhelmed and confused comes with the territory. But it doesn’t have to be so confusing when it comes to vitamins and supplements.
If you did your extra credit work, we bet you already know that high mercury seafood, alcohol, and cigarettes are off-limits during pregnancy. What may surprise you is that some vitamins, minerals, and herbal supplements should be avoided as well.
Information on which supplements are safe and which aren’t varies and can make things feel even more complicated. We’ve got you, though.
This article breaks down which supplements are believed to be safe to take during pregnancy and why some supplements should be avoided.
Getting the right nutrients is important at every stage of life, but it’s especially critical during pregnancy, as you’ll need to nourish both yourself and your growing babe.
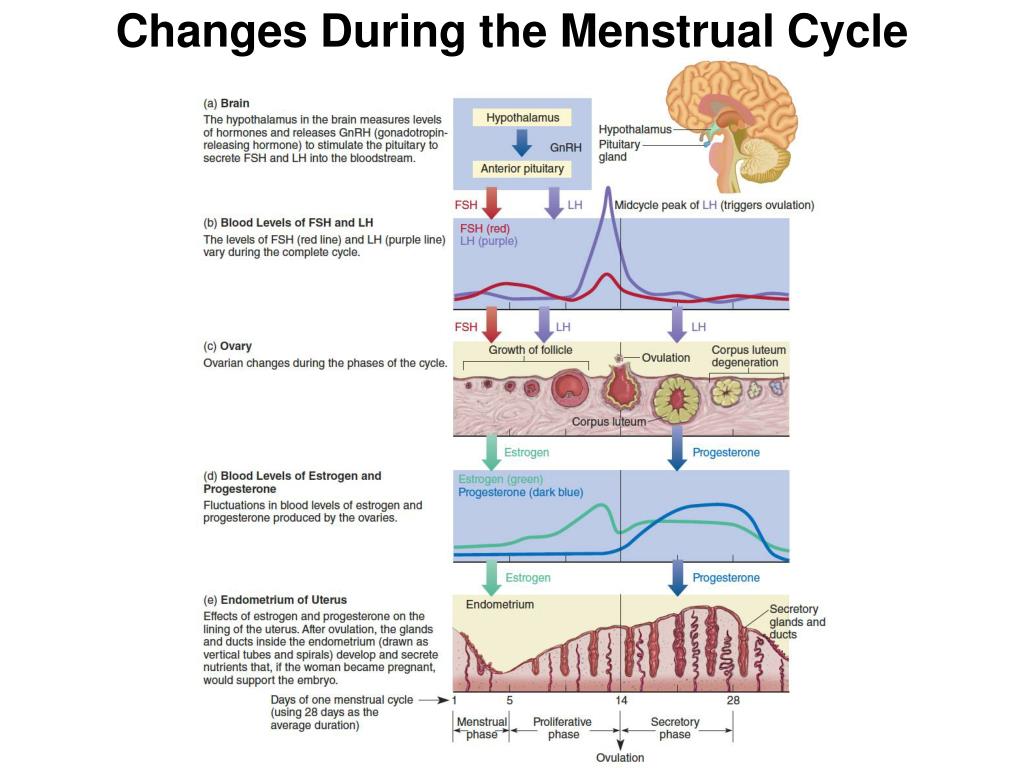
Pregnancy increases the need for nutrients
During pregnancy, macronutrient intake needs grow significantly. Macronutrients include carbohydrates, proteins, and fats.
For example, protein intake needs to increase from the recommended 0.36 grams per pound (0.8 grams per kg) of body weight for non-pregnant women to 0.5 grams per pound (1.1 grams per kg) of body weight for pregnant women.
You’ll want to be including protein in every meal and snack to meet your needs.
The requirement for micronutrients, which include vitamins, minerals, and trace elements, increases even more than the need for macronutrients.
While some people are able to meet this growing demand through a well-planned, nutrient-dense eating plan, it can be a challenge for others.
You may need to take vitamin and mineral supplements for various reasons, including:
- Nutrient deficiencies: Some people may need a supplement after a blood test reveals a deficiency in a vitamin or mineral. Correcting deficiencies is critical, as a shortage of nutrients like folate has been linked to birth defects.

- Hyperemesis gravidarum: This pregnancy complication is characterized by severe nausea and vomiting. It can lead to weight loss and nutrient deficiencies.
- Dietary restrictions: Women who follow specific diets, including vegans and those with food intolerances and allergies, may need to supplement with vitamins and minerals to prevent micronutrient deficiencies
- Smoking: Although it’s critical for mothers to avoid cigarettes during pregnancy, those who continue to smoke have an increased need for specific nutrients like vitamin C and folate.
- Multiple pregnancies: Women carrying more than one baby have higher micronutrient needs than women carrying one baby. Supplementing is often necessary to ensure optimal nutrition for both the mother and her babies.
- Genetic mutations like MTHFR: Methylenetetrahydrofolate reductase (MTHFR) is a gene that converts folate into a form that the body can use.
 Pregnant women with this gene mutation may need to supplement with a specific form of folate to avoid complications.
Pregnant women with this gene mutation may need to supplement with a specific form of folate to avoid complications. - Poor nutrition: Women who under eat or choose foods that are low in nutrients may need to supplement with vitamins and minerals to avoid deficiencies.
In addition, experts like those at the American College of Obstetricians and
Gynecologists (ACOG) recommend that all pregnant people take a prenatal vitamin and folic acid supplement. This is advised to fill nutritional gaps and prevent developmental abnormalities at birth like spina bifida.
Depending on your personal circumstances, be prepared to take on the task of adding supplements to your daily routine if directed by your healthcare provider.
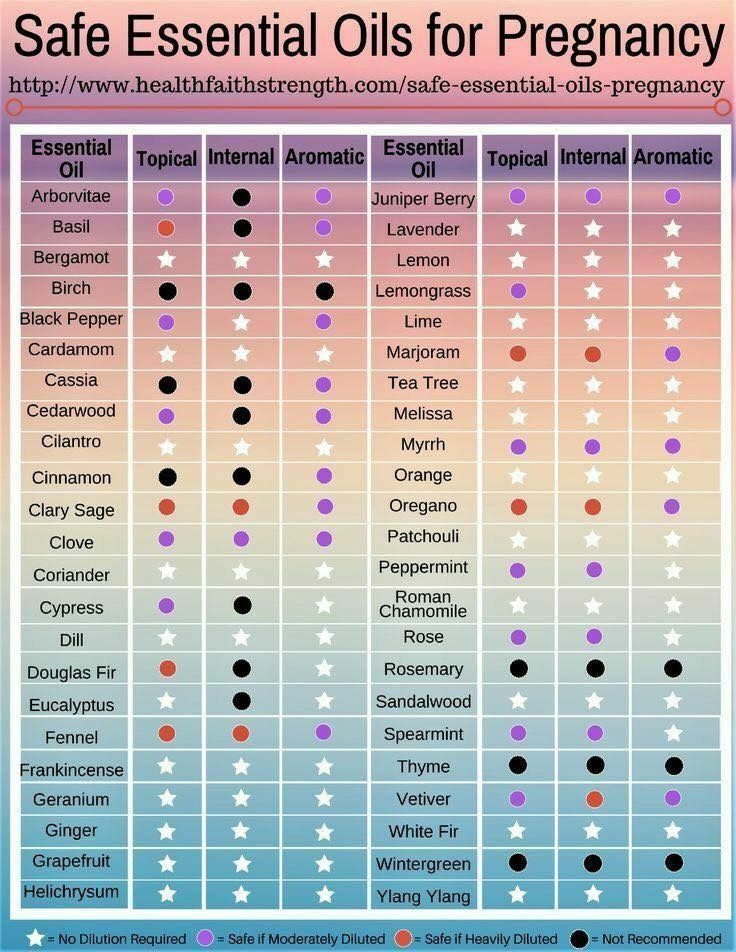
Herbal supplements can help with ailments — with caution
In addition to micronutrients, herbal supplements are popular.
One 2019 study found that 15.4 percent of pregnant women in the United States use herbal supplements. However not all disclose to their physicians they’re taking them. (A 2017 study found about 25 percent of herbal supplement users in the United States don’t tell their docs.)
However not all disclose to their physicians they’re taking them. (A 2017 study found about 25 percent of herbal supplement users in the United States don’t tell their docs.)
While some herbal supplements may be safe to take during pregnancy, there are far more that might not be.
Although some herbs can help with common pregnancy ailments like nausea and upset stomach, some may be harmful to both you and baby.
Unfortunately, there isn’t much research regarding the use of herbal supplements by pregnant people, and much is unknown about how the supplements can affect you.
The safest bet? Keep your doctor in the know about any and all changes to your eating plan and supplements.
Just as with medications, your doctor should approve and supervise all micronutrient and herbal supplements to ensure that they’re necessary and taken in safe amounts.
Always purchase vitamins from a reputable brand that has their products evaluated by third-party organizations like the United States Pharmacopeia (USP).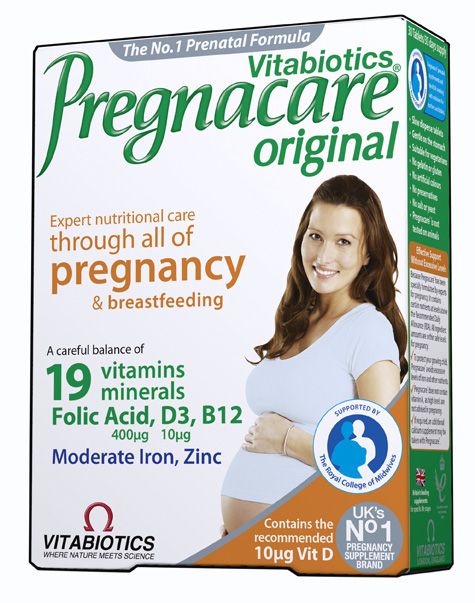
This ensures that the vitamins adhere to specific standards and are generally safe to take. Not sure which brands are reputable? Your local pharmacist can be a lot of help.
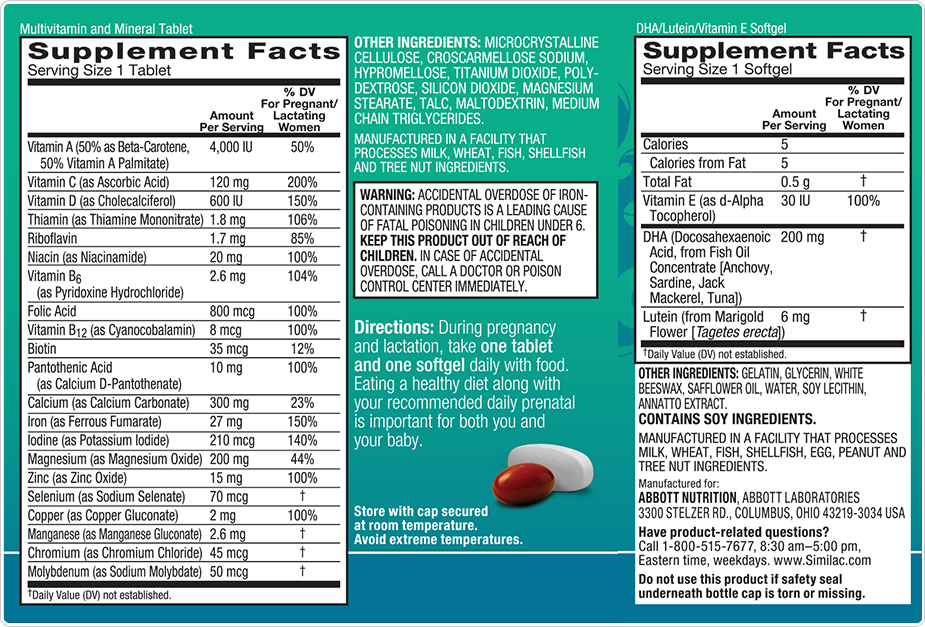
1. Prenatal vitamins
Prenatal vitamins are multivitamins that are specially formulated to meet the increased demand for micronutrients during pregnancy.
They’re intended to be taken before conception and during pregnancy and breastfeeding.
Observational studies have shown that supplementing with prenatal vitamins reduces the risk of preterm birth and preeclampsia. Preeclampsia is a potentially dangerous complication characterized by high blood pressure and possibly protein in the urine.
While prenatal vitamins aren’t meant to replace your healthy eating plan, they may help prevent nutritional gaps by providing extra micronutrients that are in high demand during pregnancy.
Since prenatal vitamins contain the vitamins and minerals that you’ll need, taking additional vitamin or mineral supplements may not be necessary unless suggested by your doctor.
Prenatal vitamins are often prescribed by doctors and available over-the-counter.
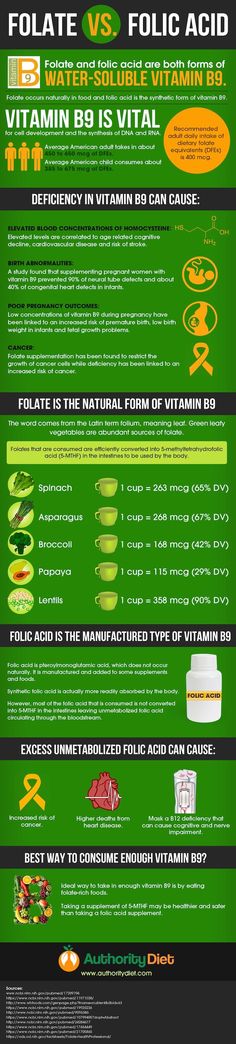
2. Folate
Folate is a B vitamin that plays an integral role in DNA synthesis, red blood cell production, and fetal growth and development.
Folic acid is the synthetic form of folate found in many supplements. It gets converted into the active form of folate — L-methylfolate — in the body.
It’s recommended to take at least 600 micrograms (mcg) of folate or folic acid per day to reduce the risk of neural tube defects and congenital abnormalities like cleft palate and heart defects.
In a review of five randomized studies including 6,105 women, supplementing with folic acid daily was associated with a reduced risk of neural tube defects. No negative side effects were noted.
Although adequate folate can be obtained through diet, many women don’t eat enough folate-rich foods, making supplementation necessary.
Additionally, the Centers for Disease Control and Prevention (CDC) recommends that all women of childbearing age consume at least 400 mcg of folate or folic acid per day.
This is because many pregnancies are unplanned, and birth abnormalities due to a folate deficiency can occur very early in pregnancy, even before most women know they’re pregnant.
It may be wise for pregnant women, especially those with an MTHFR genetic mutation, to choose a supplement that contains L-methylfolate to ensure maximum uptake.
3. Iron
The need for iron increases significantly during pregnancy, as maternal blood volume increases by about 45 percent.
Iron is critical for oxygen transport and healthy growth and development of your baby and the placenta.
In the United States, the prevalence of iron deficiency in pregnant women is around 18 percent, and 5 percent of these women have anemia.
Anemia during pregnancy has been associated with preterm delivery, maternal depression, and infant anemia.
The recommended intake of 27 milligrams (mg) iron per day can be met through most prenatal vitamins. However, if you have iron deficiency or anemia, you’ll need higher doses of iron, managed by your doctor.
If you aren’t iron deficient, you shouldn’t take more than the recommended intake of iron to avoid adverse side effects. These may include constipation, vomiting, and abnormally high hemoglobin levels.
4. Vitamin D
This fat-soluble vitamin is important for immune function, bone health, and cell division.
Vitamin D deficiency during pregnancy has been linked to an increased risk of cesarean section, preeclampsia, preterm birth, and gestational diabetes.
The current recommended intake of vitamin D during pregnancy is 600 IU or 15 mcg per day. However, some experts suggest that vitamin D needs during pregnancy are much higher.
Check in with your doctor regarding screening for vitamin D deficiency and proper supplementation.
5. Magnesium
Magnesium is a mineral involved in hundreds of chemical reactions in your body. It plays critical roles in immune, muscle, and nerve function.
Deficiency in this mineral during pregnancy may increase the risk of chronic hypertension and premature labor.
Some studies suggest that supplementing with magnesium may reduce the risk of complications like fetal growth restriction and preterm birth.
6. Ginger
Ginger root is commonly used as a spice and herbal supplement.
In supplement form, you may have heard of it used to treat nausea caused by motion sickness, pregnancy, or chemotherapy.
A review of four studies suggested that ginger is both safe and effective for treating pregnancy-induced nausea and vomiting.
Nausea and vomiting are common during pregnancy, with up to 80 percent of women experiencing them in the first trimester of pregnancy.
Though ginger may help reduce this unpleasant pregnancy complication, more research is needed to identify the maximum safe dosage. Double check with your doctor to see if you need it.
7. Fish oil
Fish oil contains docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA), two essential fatty acids that are important for baby’s brain development.
Supplementing with DHA and EPA in pregnancy might boost post-pregnancy brain development in your baby and decrease maternal depression, though research on this topic isn’t conclusive.
Although observational studies have shown improved cognitive function in the children of women who supplemented with fish oil during pregnancy, several controlled studies have failed to show a consistent benefit.
For example, one 2010 study involving 2,399 women found no difference in the cognitive function of infants whose mothers had supplemented with fish oil capsules containing 800 mg of DHA per day during pregnancy, compared with infants whose mothers did not.
This study also found that supplementing with fish oil did not affect maternal depression.
However, the study did find that supplementing with fish oil protected against preterm delivery, and some evidence suggests that fish oil may benefit fetal eye development.
Maternal DHA levels are important for proper fetal development and supplementing is considered safe.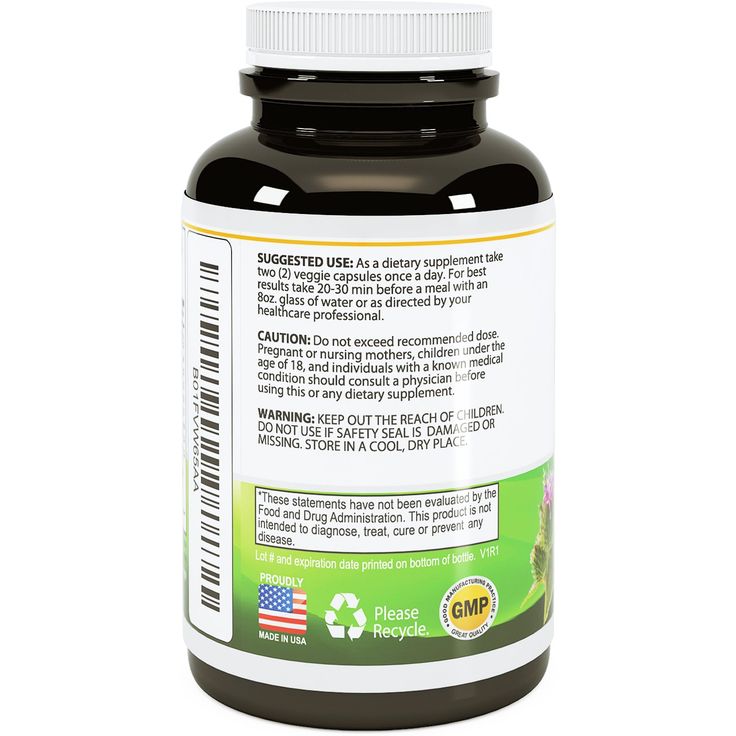 The jury is still out on whether taking fish oil during pregnancy is necessary.
The jury is still out on whether taking fish oil during pregnancy is necessary.
To get DHA and EPA through food, it’s encouraged to consume two to three servings of low-mercury fish like salmon, sardines, or pollock per week.
8. Probiotics
Given increased general awareness of gut health, many parents-to-be turn to probiotics.
Probiotics are living microorganisms that are thought to benefit digestive health.
Many studies have shown that probiotics are safe to take during pregnancy, and no harmful side effects have been identified, aside from an extremely low risk of probiotic-induced infection.
Additionally, several studies have shown that supplementing with probiotics may reduce the risk of gestational diabetes, postpartum depression, and infant eczema and dermatitis.
Research on probiotic use in pregnancy is ongoing, and more about the role of probiotics in maternal and fetal health is sure to be discovered.
9. Choline
Choline plays a vital role in baby’s brain development and helps to prevent abnormalities of the brain and spine.
The current recommended daily allowance of choline during pregnancy (450 mg per day) has been thought to be inadequate and that an intake closer to 930 mg per day is optimal instead.
Note that prenatal vitamins often don’t contain choline. A separate choline supplement may be recommended by your doctor.
While supplementing with some micronutrients and herbs is safe for pregnant women, many of them should be avoided, or avoided in high amounts.
Always check with your doctor before adding any additional supplements outside of any prenatal vitamins you may be taking.
1. Vitamin A
You’ll often find vitamin A in your prenatal vitamins since it’s so important. Although this vitamin is extremely important for fetal vision development and immune function, too much vitamin A can be harmful.
Given that vitamin A is fat soluble, your body stores excess amounts in the liver.
This accumulation can have toxic effects on the body and lead to liver damage. It can even cause birth defects.
It can even cause birth defects.
For example, excessive amounts of vitamin A during pregnancy has been shown to cause congenital birth abnormalities.
Between prenatal vitamins and foods, you should be able to get enough vitamin A, and additional supplementation outside of your prenatal vitamins is not advised.
2. Vitamin E
This fat-soluble vitamin plays many important roles in the body and is involved in gene expression and immune function.
While vitamin E is very important for health, it’s recommended that you don’t supplement with it.
Extra supplementation with vitamin E has not been shown to improve outcomes for either mothers or babies and may instead increase the risk of abdominal pain and premature rupture of the amniotic sack.
3. Black cohosh
A member of the buttercup family, black cohosh is a plant used for a variety of purposes, including controlling hot flashes and menstrual cramps.
It’s unsafe to take this herb during pregnancy, as it can cause uterine contractions, which could induce preterm labor.
Black cohosh has also been found to cause liver damage in some people.
4. Goldenseal
Goldenseal is a plant that’s used as a dietary supplement to treat respiratory infections and diarrhea, although there’s very little research on its effects and safety.
Goldenseal contains a substance called berberine, which has been shown to worsen jaundice in infants. It can lead to a condition called kernicterus, a rare type of brain damage that can be fatal.
For these reasons, definitely avoid goldenseal.
5. Dong quai
Dong quai is a root that has been used for over 1,000 years and is popular in traditional Chinese medicine.
Though it’s used to treat everything from menstrual cramps to high blood pressure, evidence regarding its efficacy and safety is lacking.
You should avoid dong quai, as it may stimulate uterine contractions, raising the risk of miscarriage.
6. Yohimbe
Yohimbe is a supplement made from the bark of a tree native to Africa.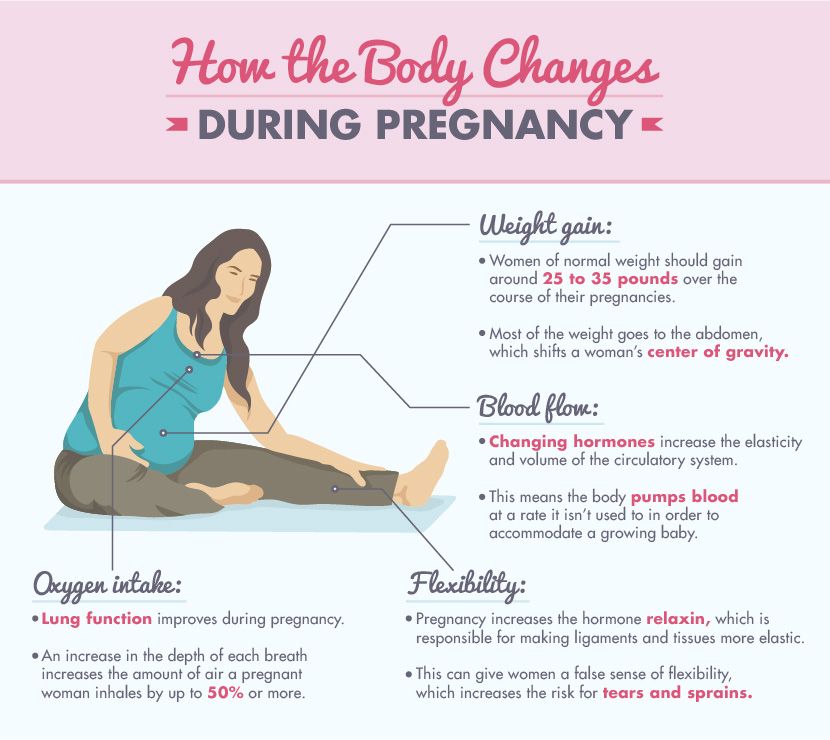
It’s used as an herbal remedy to treat a range of conditions from erectile dysfunction to obesity.
This herb should never be used during pregnancy, as it has been associated with dangerous side effects like high blood pressure, heart attacks, and seizures.
7. Other herbal supplements considered unsafe during pregnancy
It’s best to avoid the following:
- saw palmetto
- tansy
- red clover
- angelica
- yarrow
- wormwood
- blue cohosh
- pennyroyal
- ephedra
- mugwort
Pregnancy is a time of growth and development, making health and nutrition a top priority. Taking the best care of that little one is the goal.
While some supplements can be helpful during pregnancy, many can cause dangerous side effects in both you and your baby.
Importantly, while supplementing with certain vitamins and minerals may help fill nutritional gaps, supplements are not meant to replace a healthy eating plan and lifestyle.
Nourishing your body with nutrient-dense foods, as well as getting enough exercise and sleep and minimizing stress, is the best way to ensure a healthy pregnancy for you and your baby.
Although supplements can be necessary and helpful in certain circumstances, always check with your doctor regarding doses, safety, and potential risks and benefits.
Vitamins and other nutrients during pregnancy
During pregnancy your baby gets all necessary nutrients from you. So you may need more during pregnancy than you did before pregnancy.
Taking prenatal vitamins and eating healthy foods can help give you all the nutrients you and your baby need during pregnancy.
Make sure your prenatal vitamin has folic acid, iron and calcium in it. Most have the right amount of each of these.
Talk to your provider to make sure you get enough vitamin D, DHA and iodine each day.
Don’t take any supplements without your provider’s OK.
What are prenatal vitamins?
Prenatal vitamins are multivitamins for pregnant women or women who are trying to get pregnant. Compared to a regular multivitamin, they have more of some nutrients that you need during pregnancy. Your health care provider may prescribe a prenatal vitamin for you, or you can buy them over the counter without a prescription. Take a prenatal vitamin every day during pregnancy. If you’re planning to get pregnant, start taking prenatal vitamins before you get pregnant.
Your body uses vitamins, minerals and other nutrients in food to strong and healthy. During pregnancy, your growing baby gets all necessary nutrients from you. So you may need more during pregnancy than you did before. If you’re pregnant with multiples (twins, triplets or more), you may need more nutrients than if you’re pregnant with one baby. Your prenatal vitamin contains the right amount of nutrients you need during pregnancy.
If you’re a vegetarian, have food allergies or can’t eat certain foods, your provider may want you to take a supplement to help you get more of certain nutrients. A supplement is a product you take to make up for certain nutrients that you don’t get enough of in foods you eat. For example, your provider may recommend that you take a vitamin supplement to help you get more vitamin D, iron or calcium.
A supplement is a product you take to make up for certain nutrients that you don’t get enough of in foods you eat. For example, your provider may recommend that you take a vitamin supplement to help you get more vitamin D, iron or calcium.
Which nutrients are most important during pregnancy?
All nutrients are important, but these six play a key role in your baby’s growth and development during pregnancy:
- Folic acid
- Iron
- Calcium
- Vitamin D
- DHA
- Iodine
What is folic acid?
Folic acid is a B vitamin that every cell in your body needs for healthy growth and development. Taking folic acid before and during early pregnancy can help prevent birth defects of the brain and spine called neural tube defects (also called NTDs). Some studies show that taking folic acid may help prevent heart defects and birth defects in your baby’s mouth (called cleft lip and palate).
- Before pregnancy take a vitamin supplement with 400 mcg of folic acid every day.
- Take a vitamin supplement with 400 mcg of folic acid each day, even if you’re not trying to get pregnant.
- During pregnancy, take a prenatal vitamin each day that has 600 mcg of folic acid in it.
Check the product label to see how much folic acid is in it.
If you’re at high risk for having a baby with an NTD, talk to your provider about how you can safely take 4,000 mcg of folic acid each day to help prevent an NTD. Start taking 4,000 mcg at least 3 months before you get pregnant and through the first 12 weeks of pregnancy. You’re at high risk if:
- You’ve had a pregnancy with an NTD in the past.
- You or your partner has an NTD.
- Your partner has a child with an NTD.
Don’t take several multivitamins or prenatal vitamins. You can get too much of other nutrients, which may be harmful to your health. Your provider can help you figure out the best and safest way for you to get the right amount of folic acid.
You can also get folic acid from food. Citrus fruits, green leafy vegetables and beans are all excellent sources of folic acid. Some foods are also enriched with folic acid, such as cereals, bread, rice and pasta.
Citrus fruits, green leafy vegetables and beans are all excellent sources of folic acid. Some foods are also enriched with folic acid, such as cereals, bread, rice and pasta.
What is iron?
Iron is a mineral. Your body uses iron to make hemoglobin, a protein that helps carry oxygen from your lungs to the rest of your body. You need twice as much iron during pregnancy than you did before pregnancy. Your body needs this iron to make more blood so it can carry oxygen to your baby. Your baby needs iron to make his own blood.
During pregnancy you need 27 milligrams of iron each day. Most prenatal vitamins have this amount. You also can get iron from food. Good sources of iron include:
- Lean meat, poultry and seafood
- Cereal, bread and pasta that has iron added to it (check the package label)
- Leafy green vegetables
- Beans, nuts, raisins and dried fruit
Foods containing vitamin C can increase the amount of iron your body absorbs. It's a good idea to eat foods like orange juice, tomatoes, strawberries and grapefruit every day.
It's a good idea to eat foods like orange juice, tomatoes, strawberries and grapefruit every day.
Calcium (in dairy products like milk) and coffee, tea, egg yolks, fiber and soybeans can block your body from absorbing iron. Try to avoid these when eating iron-rich foods.
If you don’t get enough iron during pregnancy, you may be more likely to experience:
- Infections.
- Anemia. This means you have too little iron in your blood.
- Fatigue. This means you feel really tired or exhausted.
- Premature birth. This means your baby is born too soon, before 37 weeks of pregnancy.
- Low birthweight. This means your baby is born weighing less than 5 pounds, 8 ounces.
What is calcium?
Calcium is a mineral that helps your baby’s bones, teeth, heart, muscles and nerves develop. During pregnancy, you need 1,000 milligrams of calcium each day. You can get this amount by taking your prenatal vitamin and eating food that has a lot of calcium in it. Good sources of calcium include:
Good sources of calcium include:
- Milk, cheese and yogurt
- Broccoli and kale
- Orange juice that has calcium added to it (check the package label)
If you don’t get enough calcium during pregnancy, your body takes it from your bones and gives it to your baby. This can cause health conditions, such as osteoporosis, later in life. Osteoporosis causes your bones become thin and break easily.
What is vitamin D?
Vitamin D helps your body absorb calcium. It also helps your body’s nerves, muscles and immune system work. Your immune system protects your body from infection. Vitamin D helps your baby’s bones and teeth grow.
During pregnancy, you need 600 IU (international units) of vitamin D each day. You can get this amount from food or your prenatal vitamin. Good sources of vitamin D include:
- Fatty fish, like salmon
- Milk and cereal that has vitamin D added to it (check the package label)
What is DHA?
Docosahexaenoic acid (DHA) is a kind of fat (called omega-3 fatty acid) that helps with growth and development. During pregnancy, you need DHA to help your baby’s brain and eyes develop. Not all prenatal vitamins contain DHA, so ask your provider if you need to take a DHA supplement.
During pregnancy, you need DHA to help your baby’s brain and eyes develop. Not all prenatal vitamins contain DHA, so ask your provider if you need to take a DHA supplement.
During pregnancy, it is recommended that women eat 8 to 12 ounces of seafood low in mercury each week. Good sources of DHA include:
- Herring, salmon, trout, anchovies, halibut, catfish, shrimp and tilapia
- Orange juice, milk and eggs that have DHA added to them (check the package label)
What is iodine?
Iodine is a mineral your body needs to make thyroid hormones, which help your body use and store energy from food. You need iodine during pregnancy to help your baby’s nervous system develop. The nervous system (brain, spinal cord and nerves) helps your baby move, think and feel.
During pregnancy, you need 220 micrograms of iodine every day. Not all prenatal vitamins contain iodine, so make sure you eat foods that have iodine in them. Ask your provider if you need to take an iodine supplement.
Good sources of iodine include:
- Fish
- Milk, cheese and yogurt
- Enriched or fortified cereal and bread (check the package label)
- Iodized salt (salt with iodine added to it; check the package label)
Last reviewed September, 2020
What nutritional supplements are useful for pregnant women to take
From the moment of conception, a woman is no longer alone, and the amount of calories consumed, the volume of vitamins and minerals is not enough to provide them for an adult and a second developing organism. Of course, you do not need to eat for two and enter the sick leave, because you can easily continue the normal rhythm of life. But during pregnancy, your body already needs additional nourishment in order to pass on all the most valuable and important to the unborn baby.
Need more nutrients
The period of gestation causes a woman's need for macronutrients to increase. We are talking about increased consumption of proteins, carbohydrates and fats.
With a normal rhythm of life, the protein norm is 0.8 grams per 1 kilogram of body weight, and during pregnancy this figure increases to 1.1 grams.
The norm of substances enriched with vitamins, minerals and microelements increases significantly. These components are important for maintaining maternal growth and proper fetal development at every stage of pregnancy, thereby ensuring the proper functioning of all systems, cell signaling.
With a correct and varied diet, you can fully meet your needs for all the necessary micronutrients.
Among the main reasons why women take nutritional supplements and vitamin complexes during pregnancy are the following:
- nutritional deficiency - if a blood test reveals a lack of specific minerals or vitamins, then special supplements are prescribed. This is necessary, especially if there is a deficiency of folate, as it can cause birth defects for the baby born;
- Hyperemesis gravidarum - a complication during pregnancy, accompanied by vomiting and nausea.
 Often results in weight loss and nutritional deficiencies;
Often results in weight loss and nutritional deficiencies; - limited nutrition and strict diet - if you are a vegan, have an allergy or intolerance to certain foods, follow a strict diet, then the body needs to be saturated with minerals and vitamins in order to protect itself from unforeseen deviations and health disorders in the future;
- smoking - despite the fact that this bad habit is not combined with pregnancy, there are many women who allow themselves to smoke. In this case, you need to saturate the body with vitamin C and folate;
- multiple pregnancy - if you are carrying more than one baby, but several, then the body's need for micronutrients increases already several times. Mothers need to provide good nutrition so that future children are healthy;
- gene mutations, in particular MTHFR - this gene converts folate into the form that is used by the body. If a pregnant woman has such a mutation, care should be taken to supplement her intake of folate to protect herself from the risks of complications;
- poor diet, malnutrition - when malnourished and consuming foods poor in vitamins, the body experiences a lack of them, and then it is necessary to compensate for the needs through nutritional supplements.

Representatives of the American Congress of Obstetricians and Gynecologists, as well as experts who share their views and positions, advise all pregnant women to take vitamins, especially folic acid. You also need to review your diet and adjust the foods you eat to prevent birth defects in a child. One of the most common pathologies is spina bifida.
All of the above reasons encourage expectant mothers to take vitamin and mineral supplements.
Herbal Pregnancy Supplements
Natural herbal supplements are becoming increasingly popular. They can be combined with minerals.
A study found that 15.4 percent of pregnant women in the United States take herbal supplements. However, 25 percent of this population never told their gynecologist that they were taking drugs.
Only some types of herbal products are safe and harmless to the fetus, and there are many substances that are fraught with danger and harm to the mother's body.
There are herbs that are effective for complications during pregnancy, such as relieving nausea, relieving indigestion, but most other herbs pose a threat to the mother's body and to the health of the fetus.
Research aimed at studying herbal supplements and their effect on the pregnant body, so many aspects remain unexplored, which does not allow us to confidently declare the benefits of herbal preparations for pregnant women.
The Safest Supplements for Women During Pregnancy
Like medicines and medicines, all micronutrients and vitamin or herbal supplements must be reviewed and approved by your gynecologist to prescribe the correct dosage and determine if it is appropriate and appropriate to take them in a particular situation.
If you're buying your own vitamin supplements, be sure to go for a well-known brand that submits their products to testing and independent labs. In particular, there must be a quality mark from the United States Pharmacopoeia Convention (USP). Thus, it can be understood that the product meets the declared quality and safety standards for use.
Thus, it can be understood that the product meets the declared quality and safety standards for use.
This ensures that the vitamins meet quality standards and are generally safe to consume.
Prenatal Vitamins
These substances are multivitamins designed specifically to meet the micronutrient needs of the female body to ensure a smooth and smooth pregnancy.
They can be taken during pregnancy planning, during fetal development and further after childbirth during lactation.
Observational studies have shown that taking vitamins helps mothers-to-be avoid the risk of preterm birth and preeclampsia. The latter is a very dangerous complication, accompanied by an increase in pressure and a splash of protein into the urine.
Despite the fact that prenatal vitamins cannot be a full-fledged replacement for proper and healthy food, they nevertheless prevent the lack of important trace elements and saturate the body with all the substances that are important during pregnancy.
Prenatal vitamins contain many minerals and vitamins that are difficult for pregnant women to do without, but there is no need for additional preparations, unless they are prescribed by a doctor.
Prenatal vitamins are available over the counter but are prescribed by your gynecologist.
Folate
Folate is a substance from the B vitamin group that is involved in DNA synthesis, helps produce red blood cells, and promotes the development and growth of the fetus.
Folic acid is an artificial form of folate found in many dietary supplements. In the body, it is converted into an active form called L-methylfolate and has a beneficial effect on the body.
The recommended amount of folic acid for pregnant women is 600 micrograms per day. The trace element reduces the risk of damage to the neural tube and prevents congenital anomalies, for example, protects against heart defects and cleft palate.
Scientists conducted five randomized trials on a group of 6105 women. Folic acid was required to reduce the risk of neural tube defects. At the end of the experiment, the researchers found no side effects.
Folic acid was required to reduce the risk of neural tube defects. At the end of the experiment, the researchers found no side effects.
The modern diet, even the healthiest, does not meet the daily requirement for folate. But with the usual rhythm of life, this is not felt and does not affect health in any way, but during pregnancy, when a woman keeps a new life in herself, care must be taken to ensure that the body receives the entire dose of the trace element.
Experts at the various Centers for Disease Control and Prevention recommend that all pregnant and expecting women take at least 400 micrograms of folate each day.
This is due to the fact that many conceptions are not planned, and birth defects of the fetus can appear very early, even before the woman knows about her condition.
If a woman has an MTHFR mutation, it is best to choose supplements with the active form of L-methylfolate, as this is the best absorption of micronutrients.
Iron
Due to the fact that the volume of blood in women during periods of gestation increases by 50 percent, the body's need for such an element as iron increases. This component is used for the development of the fetus, as well as for transporting oxygen to the internal organs.
This component is used for the development of the fetus, as well as for transporting oxygen to the internal organs.
Today, approximately 18 percent of women in the United States are iron deficient, and another 8 percent are anemic. The latter disease most often occurs due to preterm birth, depression after the birth of a child and the occurrence of this disease in the fetus.
The daily rate of iron in the body, which is 27 mg, can be replenished by using specialized vitamin complexes for pregnant women. However, it should be borne in mind that during pregnancy this rate increases, due to which a larger volume may be prescribed by a doctor.
To exclude the possibility of side effects, women during the period of gestation, if they do not have a deficiency of this trace element, are not recommended to exceed the daily intake. If this recommendation is not followed, a gag reflex, a violation of the stool and an increase in hemoglobin levels may occur. Vitamin D
Vitamin D
To normalize the immune system, strengthen bones and restore cell division, it is recommended to consume vitamin D.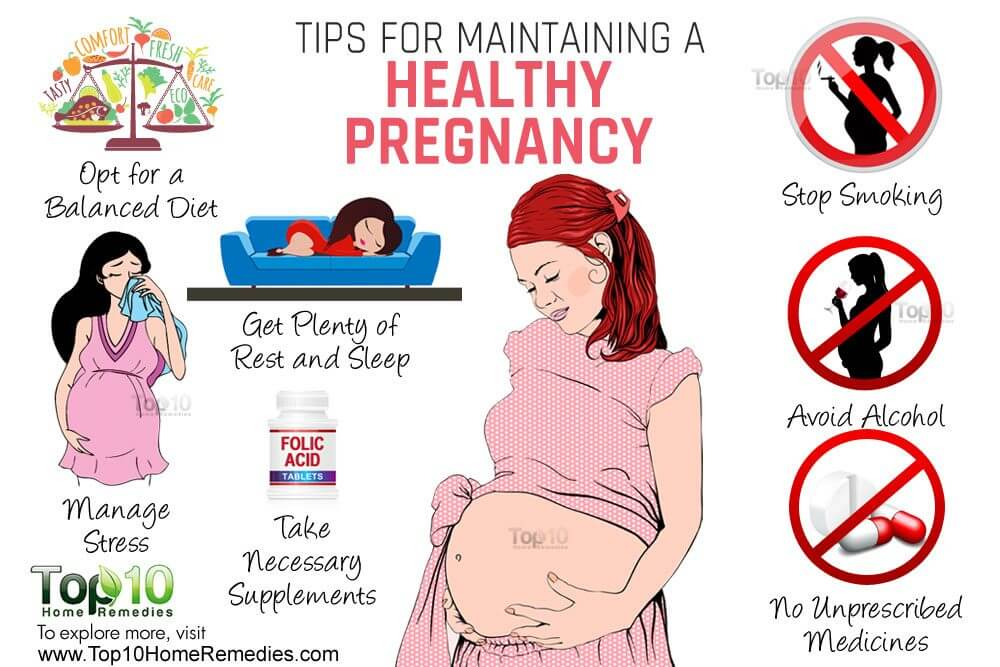 An acute shortage of this element in pregnant women can lead to the need for a caesarean section, to premature birth or to the development of gestational diabetes.
An acute shortage of this element in pregnant women can lead to the need for a caesarean section, to premature birth or to the development of gestational diabetes.
Women during pregnancy are recommended to consume up to 600 IU per day. However, according to experts, some pregnant women may have a much higher need for this element.
Before taking this vitamin, it is recommended that you consult your doctor and test for vitamin D deficiency.
Magnesium
Magnesium is used by the human body to carry out a wide variety of chemical processes. It is used to normalize the functioning of the nervous and immune systems, as well as to maintain muscle function. Under the condition of an acute shortage of this mineral in the body of pregnant women, the likelihood of premature birth and the development of chronic hypertension increases significantly.
The use of appropriate nutritional supplements can reduce the risk of preterm birth and ensure the proper development of the fetus.
Ginger
In most cases, ginger root is used as a spice. However, it can also be used as a remedy for nausea, which can be caused by intoxication, chemotherapy, or motion sickness.
So, during research, scientists were able to find out that the root of this plant can be used as a remedy for nausea and vomiting during pregnancy, which in 80 percent of cases are observed in the first trimester.
Despite this effect, more research is needed to determine the safe dosage of ginger and prevent negative effects on the mother and fetus.
Fish oil
The main components of fish oil recommended during pregnancy are DHA and EPA, which are necessary for the normal development of the brain of the unborn child. Moreover, the use of these trace elements can prevent the development of depression in pregnant women.
Although pregnant women have seen improvements in cognitive function and brain development in the fetus during fish oil intake, scientists have not been able to confirm that this effect is not temporary, but permanent.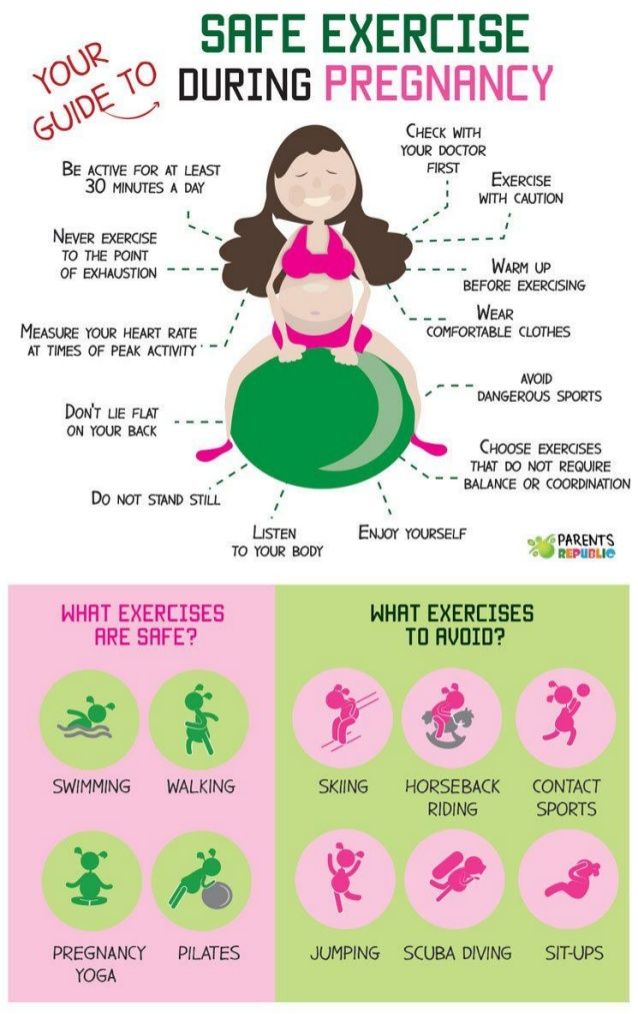
For example, one study of 2,400 women found no difference in brain development between children whose mothers took 800 mg of DHA per day and children whose mothers did not take these supplements. This study also demonstrated that this micronutrient has no effect on the development of depression in pregnant women.
However, despite this, the use of fish oil can reduce the risk of preterm birth and significantly improve the development of the eye in the fetus.
Scientists have also noted that DHA is safe for pregnant women. It can be obtained not only through supplements, but also through the consumption of fatty fish such as salmon, pollock and sardines.
Probiotics
Most pregnant women are actively interested in probiotics - microorganisms that improve the digestive process. In this regard, several studies have been conducted demonstrating that the consumption of these substances is absolutely safe for the body.
For example, in one study, scientists found that the consumption of probiotics can significantly reduce the risk of developing diabetes, depression, and skin diseases in the fetus.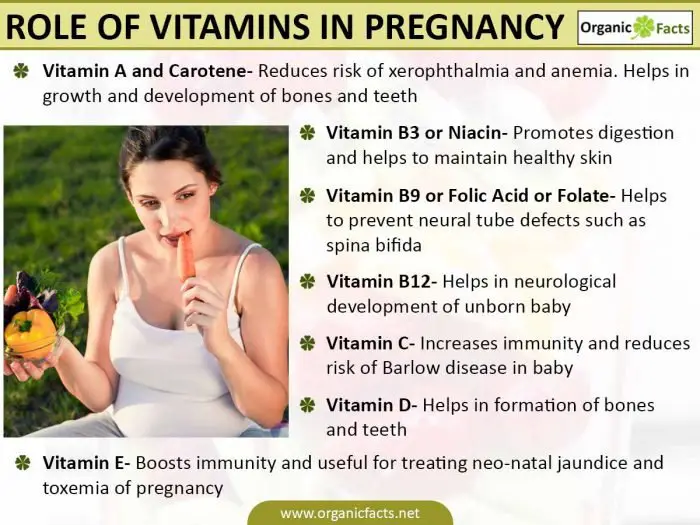
Researchers are currently continuing to study the effect of probiotics on the body of pregnant women, which will soon allow them to identify a number of other positive aspects of taking these substances.
Which dietary supplements are not recommended for pregnant women
Although most nutritional supplements are recommended for pregnant women, some of them can adversely affect the health of the mother and fetus. Consider the main substances and products that are not recommended for pregnant women.
Vitamin A
Although vitamin A is important for the development of fetal vision during embroidery, taking it as a dietary supplement can be extremely harmful. An excessive amount of this trace element can lead to disruption of the liver and damage to this organ in the mother, which in turn can cause the development of birth defects in the baby.
Therefore, during pregnancy, it is recommended to consume foods rich in this vitamin rather than supplements.
Vitamin E
This fat-soluble vitamin helps to strengthen the immune system and improve the transmission of heredity to the child. Despite the fact that this substance is important for the body, its use is highly discouraged during gestation. This is due to the fact that an excessive amount of the nutrient component can increase pain in the abdomen and lead to rupture of the amniotic sac.
Black cohosh
Black cohosh is a herb that belongs to the buttercup family and is used to relieve menstrual pain. Due to the fact that this herb promotes uterine contractions, which can lead to premature birth, its use during pregnancy is highly undesirable.
In addition, scientists have found that this plant can cause liver dysfunction and destruction of this organ.
Hydrastis
Hydrastis, more commonly known as Goldenseal, is a plant whose extract is used to treat diarrhea and respiratory infections. It contains a substance called berberine, which increases the symptoms of jaundice in children.
The use of this herb or supplements containing it can cause damage to brain cells and even death. In this regard, its use is not recommended for pregnant women.
Dong Quai
Dong Quai root has been used in Chinese traditional medicine for 1,000 years to relieve menstrual discomfort and normalize blood pressure. However, despite its benefits, the effectiveness of this plant is highly questionable.
Due to the fact that the root of this plant stimulates uterine contractions, which can lead to miscarriage or premature birth, its use is not recommended during gestation.
Yohimbe
Yohimbe is a food supplement made from the bark of specialized trees native to West Africa. This supplement is used to treat a range of conditions ranging from prostate problems to obesity.
Yohimbe is highly discouraged during pregnancy as it can increase blood pressure, cause heart failure and muscle spasms.
Other herbs not recommended for pregnant women
Other herbs not recommended during pregnancy include:
- Saw palmetto;
- clover;
- yarrow;
- pennyroyal;
- wormwood;
- ephedra;
- angelica;
- blue cohosh.

Conclusion
Pregnancy is the time of gestation and growth of the fetus in the womb, during which proper nutrition is the main factor on which the health of the child depends.
Although some nutritional supplements can be very beneficial for pregnant women, there are many that can still harm the health of both the mother and the unborn child. It is worth paying attention to the fact that nutritional supplements are only an addition to the main diet, and are not a replacement for it.
Eating wholesome foods, minimizing stress, exercising in the morning, and getting good sleep are the keys to having a healthy baby. While supplements may be necessary in some cases, a doctor should be consulted before taking them.
Research links
1. Protein and Amino Acid Requirements during Pregnancy
pregnancy worldwide: health effects and prevention
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4927329/
3. Periconceptional Folate Deficiency and Implications in Neural Tube Defects
Periconceptional Folate Deficiency and Implications in Neural Tube Defects
https://www. ncbi.nlm.nih.gov/pmc/articles/PMC3415073/
what is safe and what is not - Drink-Drink
If you are pregnant, you might think that feeling overwhelmed and confused comes with territory. But it doesn't have to be so confusing when it comes to vitamins and supplements.
If you've done your extra work, we're sure you already know that high-mercury seafood, alcohol, and cigarettes are prohibited during pregnancy. What may surprise you is that certain vitamins, minerals, and herbal supplements should also be avoided.
Information about which supplements are safe and which are not varies and can make things even more complicated. But we have you.
This article explains which supplements are considered safe to take during pregnancy and why certain supplements should be avoided.
Why take supplements during pregnancy?
Getting the right nutrients is important at every stage of life, but it's especially important during pregnancy as you need to feed both yourself and your growing baby.
Pregnancy increases the need for nutrients
During pregnancy, the need for macronutrients increases significantly. Macronutrients include carbohydrates, proteins and fats.
For example, protein intake should be increased from the recommended 0.36 g per pound (0.8 g per kg) of body weight for non-pregnant women to 0.5 g per pound (1.1 g per kg) of body weight for pregnant women.
You will want to include protein in every meal and snack to meet your needs.
The need for micronutrients, which include vitamins, minerals and trace elements, is increasing even more than the need for macronutrients.
While some people can meet this growing demand with a well-planned, nutrient-dense meal plan, it can be a challenge for others.
You may need to take vitamin and mineral supplements for a variety of reasons, including:
- Nutrient deficiencies: Some people may need a supplement after a blood test reveals a vitamin or mineral deficiency.
 Correcting the deficiency is critical, as deficiencies in nutrients such as folic acid have been linked to birth defects.
Correcting the deficiency is critical, as deficiencies in nutrients such as folic acid have been linked to birth defects. - Hyperemesis pregnant: This complication of pregnancy is characterized by severe nausea and vomiting. This can lead to weight loss and nutritional deficiencies.
- dietary restrictions: Women on certain diets, including vegans and those with food intolerances and allergies, may need vitamin and mineral supplements to prevent micronutrient deficiencies.
- Smoking: While it is essential for mothers to avoid smoking during pregnancy, those who continue to smoke have an increased need for certain nutrients such as vitamin C and folic acid.
- multiple pregnancies: Women with more than one child have higher micronutrient requirements than women with one child. Supplementation is often necessary to ensure optimal nutrition for both the mother and her baby.
- Genetic mutations such as MTHFR: Methylenetetrahydrofolate reductase (MTHFR) is the gene that converts folic acid into a form usable by the body. Pregnant women with this gene mutation may need to take a specific form of folic acid to avoid complications.
- Poor nutrition: Women who are malnourished or choose foods low in nutrients may need vitamin and mineral supplements to avoid deficiency.
In addition, experts such as the American College of Obstetricians and
Gynecologists (ACOG) recommend prenatal vitamin and folic acid supplements for all pregnant women. It is recommended to fill nutritional gaps and prevent birth defects such as spina bifida.
Depending on your personal circumstances, be prepared to take on the task of adding supplements to your daily routine if directed by your healthcare professional.
Herbal Supplements Can Help Treat Diseases—With Caution
In addition to micronutrients, herbal supplements are popular.
One 2019 study found that 15.4 percent of pregnant women in the United States use herbal supplements. However, not everyone tells their doctors that they are taking them. (A 2017 study found that about 25 percent of herbal supplement users in the United States don't tell their doctors.)
While some herbal supplements may be safe to take during pregnancy, there are others that may be safe.
While some herbs can help with common pregnancy ailments such as nausea and indigestion, some can be harmful to both you and your baby.
Unfortunately, there is not much research on the use of herbal supplements during pregnancy, and much is not known about how supplements can affect you.
The safest bet? Keep your doctor updated on any changes to your nutrition plan and supplements.
Supplements Considered Safe During Pregnancy
As with medications, your doctor must approve and monitor all micronutrients and herbal supplements to ensure they are needed and taken in safe amounts.
Always buy vitamins from well-known brands that are evaluated by third parties, such as the United States Pharmacopeia (USP).
This ensures that the vitamins meet certain standards and are generally safe to take. Not sure which brands deserve respect? Your local pharmacist can be of great help.
1. Prenatal vitamins
Prenatal vitamins are multivitamins specially formulated to meet the increased demand for micronutrients during pregnancy.
They are intended for use before conception and during pregnancy and lactation.
Observational studies have shown that prenatal vitamins reduce the risk of preterm birth and preeclampsia. Preeclampsia is a potentially dangerous complication characterized by high blood pressure and possibly protein in the urine.
While not meant to replace your healthy eating plan, prenatal vitamins can help prevent nutritional deficiencies by providing additional micronutrients that are in high demand during pregnancy.
Because prenatal vitamins contain the vitamins and minerals you will need, you may not need to take extra vitamin or mineral supplements unless your doctor tells you to.
Prenatal vitamins are often prescribed by doctors and sold without a prescription.
2. Folate
Folate is a B vitamin that plays an important role in DNA synthesis, red blood cell production, and fetal growth and development.
Folic acid is a synthetic form of folic acid found in many supplements. In the body, it is converted to the active form of folic acid, L-methylfolate.
At least 600 mcg (mcg) of folic acid or folate per day is recommended to reduce the risk of neural tube defects and congenital anomalies such as cleft palate and heart defects.
In a review of five randomized trials including 6,105 women, daily folic acid supplementation was associated with a reduced risk of neural tube defects. No negative side effects were noted.
Although sufficient folic acid can be obtained through diet, many women do not eat enough folate-rich foods, so supplements are needed.
In addition, the Centers for Disease Control and Prevention (CDC) recommends that all women of childbearing age consume at least 400 micrograms of folic acid or folate per day.
This is because many pregnancies are unintended, and congenital anomalies due to folic acid deficiency can occur very early in pregnancy, even before most women know they are pregnant.
Pregnant women, especially those with an MTHFR genetic mutation, may benefit from choosing L-methylfolate supplements to ensure maximum absorption.
3. Iron
The need for iron increases significantly during pregnancy, as maternal blood volume increases by about 45 percent.
Iron is critical for oxygen transport and the healthy growth and development of your baby and placenta.
In the United States, the prevalence of iron deficiency in pregnant women is about 18 percent, and 5 percent of these women are anemic.
Anemia during pregnancy is associated with preterm birth, maternal depression and childhood anemia.
Recommended Intake 27 milligrams (mg) of iron per day can be obtained with most prenatal vitamins. However, if you are iron deficient or anemic, you will need higher doses of iron as prescribed by your doctor.
If you are not iron deficient, you should not take more than the recommended amount of iron to avoid adverse side effects. These may include constipation, vomiting, and abnormally high hemoglobin levels.
4. Vitamin D
This fat-soluble vitamin is important for immune function, bone health and cell division.
Vitamin D deficiency during pregnancy has been associated with an increased risk of caesarean section, preeclampsia, preterm birth, and gestational diabetes.
The current recommended dose of vitamin D during pregnancy is 600 IU or 15 micrograms per day. However, some experts suggest that vitamin D requirements are much higher during pregnancy.
Consult your doctor about vitamin D deficiency screening and proper supplementation.
5. Magnesium
Magnesium is a mineral involved in hundreds of chemical reactions in your body. It plays an important role in immune, muscle and nerve function.
Deficiency of this mineral during pregnancy may increase the risk of chronic hypertension and preterm birth.
Some studies show that magnesium supplementation may reduce the risk of complications such as fetal growth retardation and preterm labor.
6. Ginger
Ginger root is commonly used as a spice and herbal supplement.
In supplement form, you may have heard that it is used to treat nausea caused by motion sickness, pregnancy, or chemotherapy.
A review of four studies found ginger to be safe and effective in treating nausea and vomiting associated with pregnancy.
Nausea and vomiting often occur during pregnancy. up to 80 percent of women experiencing them in the first trimester of pregnancy.
Although ginger may help reduce this unfortunate pregnancy complication, more research is needed to determine the maximum safe dosage. Check with your doctor twice to see if you need it.
Check with your doctor twice to see if you need it.
7. Fish oil
Fish oil contains docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA), two essential fatty acids that are important for a child's brain development.
DHA and EPA supplementation during pregnancy may speed up your baby's brain development and reduce maternal depression, although research on this topic is not conclusive.
Although observational studies have shown improvement in cognitive function in the children of women who took fish oil supplements during pregnancy, several controlled studies have failed to show a sustained benefit.
For example, one 2010 study of 2,399 women found no difference in the cognitive function of infants whose mothers took a fish oil capsule supplement containing 800 mg of DHA per day during pregnancy compared with infants whose mothers did not.
This study also showed that fish oil supplementation had no effect on maternal depression.
However, research has shown that fish oil supplements protect against preterm labor, and some evidence suggests that fish oil may promote fetal eye development.
Maternal DHA levels are important for proper fetal development and supplements are considered safe. The question of the need to take fish oil during pregnancy has not yet been clarified.
To get DHA and EPA through your diet, it is recommended that you consume two to three servings of low-mercury fish such as salmon, sardines or pollock per week.
8. Probiotics
With increased general awareness of gut health, many parents-to-be are turning to probiotics.
Probiotics are live microorganisms believed to be beneficial for digestive health.
Many studies have shown that probiotics are safe to take during pregnancy and no harmful side effects have been identified, except for an extremely low risk of probiotic infection.
In addition, several studies have shown that probiotic supplementation may reduce the risk of gestational diabetes, postpartum depression, childhood eczema, and dermatitis.
Research into the use of probiotics during pregnancy is ongoing and more information is likely to be uncovered about the role of probiotics in maternal and fetal health.
9. Choline
Choline plays a vital role in baby's brain development and helps prevent brain and spinal anomalies.
The current recommended daily intake of choline during pregnancy (450 mg per day) is considered inadequate and that an intake closer to 930 mg per day is instead optimal.
Please note that prenatal vitamins often do not contain choline. Your doctor may recommend a separate choline supplement for you.
Supplements to Avoid During Pregnancy
While some micronutrient and herbal supplements are safe for pregnant women, many should be avoided or avoided in large amounts.
Always check with your doctor before adding any supplements other than prenatal vitamins you are taking.
1. Vitamin A
You will often find vitamin A in your prenatal vitamins as it is very important. While this vitamin is extremely important for the development of fetal vision and immune function, too much vitamin A can be harmful.
Because vitamin A is fat soluble, your body stores excess amounts in the liver.
This buildup can be toxic to the body and lead to liver damage. It can even cause birth defects.
For example, excess vitamin A during pregnancy has been shown to cause birth defects.
Between prenatal vitamins and food, you should be getting enough vitamin A, and additional supplements other than prenatal vitamins are not recommended.
2. Vitamin E
This fat-soluble vitamin plays many important roles in the body and is involved in gene expression and immune function.
Although vitamin E is very important for health, it is recommended not to supplement it.
Vitamin E supplementation does not improve outcomes for either mother or child, and instead may increase the risk of abdominal pain and premature rupture of the amniotic sac.
3. Black cohosh
A member of the buttercup family, cimicifuga is a herb used for a variety of purposes, including controlling hot flashes and menstrual cramps.
It is not safe to take this herb during pregnancy as it can cause uterine contractions which can cause premature labour.
Black cohosh has also been found to cause liver damage in some people.
4. Goldenseal
Goldenseal is an herb that is used as a dietary supplement to treat respiratory infections and diarrhea, although there is very little research on its effects and safety.
Goldenseal contains a substance called berberine that has been shown to worsen jaundice in babies. This can lead to a condition called kernicterus, a rare type of brain damage that can be fatal.
For these reasons, definitely avoid Goldenseal.
5. Dong Quay
Angelica root has been used for over 1,000 years and is popular in traditional Chinese medicine.
Although it is used to treat everything from menstrual cramps to high blood pressure, there is no evidence of its effectiveness or safety.
You should avoid angelica as it can stimulate uterine contractions, increasing the risk of miscarriage.