Rash that comes and goes in the same spot
Skin Rash: 9 Questions That Will Help You Decode That Skin Rash
Health ConditionsChevron
Skin HealthChevron
EczemaChevron
Related Condition Centers
- Dermatology
- Psoriasis
- Allergies
Ask yourself these after wondering, “WTF is that?!”
By Korin Miller
Getty / VikiVector
Having a skin rash can feel like you’re in a bizarre, dermatological version of Invasion of the Body Snatchers. Your skin is unhappy for some reason, and instead of doing the polite thing—chilling TF out—it’s going to express its displeasure. Boldly. Meet your new rash.
A rash generally indicates that your skin is inflamed in some way, Joshua Zeichner, M.D., a New York City–based board-certified dermatologist and director of cosmetic and clinical research in dermatology at Mount Sinai Medical Center, tells SELF. Broadly, that means your skin is manifesting an immune system response to something your body thinks could harm your health. But there are so many different types of rashes that it can be hard to tell what’s going on with your skin. Dermatologists to the rescue! Here, they offer up several questions that may help you decipher what’s behind your rash—and what to do next.
1. Is your rash itchy?
Itching is a really common side effect of all sorts of rashes, so it’s unlikely that you’ll figure out what’s going on from this symptom alone, Dr. Zeichner says. But some rashes aren’t usually itchy, so this is still a good question to ask yourself.
One example is the rash that can come with angioedema. This skin condition is related to the itchy, raised welts you may know as hives, but it starts deeper under the skin, the Mayo Clinic explains. While hives are known to be maddeningly itchy, angioedema is more likely to cause large, red welts that feel painful or warm, according to the Mayo Clinic. If you’re stumped because you have “hives” that don’t itch, this could be a potential cause.
If you’re stumped because you have “hives” that don’t itch, this could be a potential cause.
Even if your rash is itchy, the specifics can help you narrow down what might be causing it. For instance, clusters of tiny, itchy bumps or pimples around hair follicles might indicate a condition known as folliculitis. If you have an itchy rash that comes and goes in the same area, Dr. Zeichner says your doctor may suspect atopic dermatitis (often simply called eczema), a common and chronic skin condition that causes itching and inflammation.
2. Does it have a clear edge?
If your rash has a clear edge, cut-off point, or pattern, the cause is pretty likely something external that is affecting your skin, Misha A. Rosenbach, M.D., associate professor of dermatology at the University of Pennsylvania’s Perelman School of Medicine, tells SELF. That’s as opposed to something internal, like an underlying medical condition, which would be less likely to create a clearly-defined rash.
This can happen due to something like irritant contact dermatitis, or when something inflames the top layer of your skin, according to the American Academy of Dermatology (AAD). Common irritants include nickel, plants like poison ivy, and harsh cleaning agents like bleach. (There’s also allergic contact dermatitis, which is when your immune system loses it in response to something that touches your skin.)
Most Popular
One really weird example of this is phytophotodermatitis, or when chemicals in a plant or plant-based substance you touch interact with sunlight and lead to a superficial skin burn, Dr. Rosenbach says. If you do something like squeeze oranges for fresh OJ then spend a day out in the sun, you might notice a painful, streaky rash on your hands that mimics where the juice touched you, possibly along with swelling and blistering.
3. Does your rash burn?
This can help narrow things down quite a bit. “There aren’t that many rashes that give a burning sensation,” Dr. Zeichner says. You’ll usually get a burning feeling if there is a break in your skin, Caroline Robinson, M.D., a dermatologist at Northwestern Medical Group, tells SELF.
Zeichner says. You’ll usually get a burning feeling if there is a break in your skin, Caroline Robinson, M.D., a dermatologist at Northwestern Medical Group, tells SELF.
If your skin is red, inflamed, and burning, first check that you don’t have some sort of cut or actual burn. If it really seems like you have a burning rash, Dr. Zeichner says you could be dealing with something like shingles.
Shingles happens due to a varicella-zoster virus infection, according to the Mayo Clinic. (This virus is also to blame for chicken pox, and it can remain dormant in your system for years.) At first, shingles usually causes unpleasant sensations like pain, burning, numbness, and tingling. After a few days, a rash of blisters bubbles up, typically on the left or right side of the abdomen, but occasionally around one eye or one small portion of the neck or face.
Herpes is another potential cause of burning rashes. When herpes shows up around your genitals, it can start as tiny red bumps or white blisters that eventually burst and leak fluid, then scab over, according to the Mayo Clinic. If it emerges around your mouth, this virus can lead to tiny patches of blisters you may know as cold sores, the Mayo Clinic explains. Either way, you can experience some serious burning, itching, tingling, pain, and other uncomfortable symptoms.
If it emerges around your mouth, this virus can lead to tiny patches of blisters you may know as cold sores, the Mayo Clinic explains. Either way, you can experience some serious burning, itching, tingling, pain, and other uncomfortable symptoms.
4. Is it blistering?
As you may know after trying to break in a pair of shoes, blisters often happen because something is rubbing your skin or otherwise putting too much pressure on your delicate epidermis, according to the U.S. National Library of Medicine. Unfortunately, they also happen because of skin conditions. In fact, blisters can often bead up due to dermatological issues, because a long list of conditions may cause this symptom.
A blister-filled rash could be due to eczema, irritant or allergic contact dermatitis, shingles, and herpes. This can also happen due to a skin infection such as cellulitis, which occurs when bacteria (often streptococcus or staphylococcus) worm their way into your body through a crack in your skin, according to the Mayo Clinic. In addition to blisters, your skin might be red, swollen, warm, painful, and otherwise sending you signs that something is wrong.
In addition to blisters, your skin might be red, swollen, warm, painful, and otherwise sending you signs that something is wrong.
5. Is your rash scaly?
In a perfect world, your skin cells will naturally bow out when their job is done, shedding in order to allow new, healthy cells to rise to the surface. (Fun fact, per the AAD: The human body typically sheds 30,000 to 40,000 old skin cells every day.) But sometimes this process doesn’t go as smoothly as it should.
Most Popular
“Certain rashes can appear scaly because this natural exfoliating process has been affected,” Dr. Robinson says. This is generally because your old skin cells aren’t shedding properly or your skin is overproducing new cells, she explains. This can happen with eczema, which we’ve discussed above, and also with psoriasis. This chronic condition can present in a few different ways, but the most common—plaque psoriasis—causes thick, raised, dry, scaly patches to form on the skin, the Mayo Clinic explains.
6. Have you had this rash before?
The answer to this question can help you and your doctor figure out what’s triggering the rash. In some cases, chronic skin conditions like eczema or psoriasis are to blame, Dr. Zeichner says. But repeated rashes can also be a sign that continued exposure to something external is setting off your skin.
For example, if you find that you’ve been getting a rash when you wear one specific necklace, you could be allergic to a metal like nickel.
7. Have you tried a new cosmetic recently?
Contact dermatitis often crops up in response to products like soap, lotion, and makeup, Dr. Robinson says. Ask yourself if you’ve added anything new to your routine, but also keep this tricky fact in mind: You can develop this reaction to certain products even if you’ve been using them for ages. Sometimes it takes many exposures for your body to begin showing signs of irritant or allergic contact dermatitis.
If you have a condition like eczema that can cause sensitive skin (or you have sensitive skin in general), you may be more prone to developing rashes in response to what you put on your face and body. If you don’t think you have any underlying skin condition and suspect that products you use are causing your rash, contact dermatitis is probably to blame.
If you don’t think you have any underlying skin condition and suspect that products you use are causing your rash, contact dermatitis is probably to blame.
8. Could it be related to the heat?
You can wind up with a heat rash from being in hotter temperatures, the Mayo Clinic explains. This happens when your sweat ducts become clogged, so moisture gets caught under your skin.
In a mild case of heat rash, you may just experience a swath of superficial, clear blisters on the top of your skin, the Mayo Clinic says. More involved cases can cause prickly, itchy red bumps, pus-filled sacs, and hard, skin-toned lesions that look a lot like goosebumps. Luckily, heat rash usually goes away after a few days of keeping your skin cool and stay out of the heat, but you should call your doctor if it lasts longer than that or seems to be getting worse, the Mayo Clinic says.
Heat can also exacerbate some skin conditions like rosacea. This health issue causes reddened facial skin and sometimes acne-like bumps.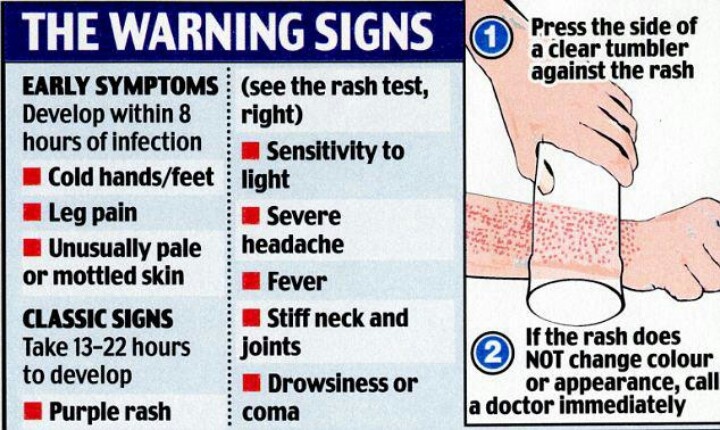 “Rosacea is a condition where the skin on the face is extra sensitive to the environment and overly reactive to triggers such as spicy foods, emotional stress, alcohol, and heat,” Dr. Zeichner says.
“Rosacea is a condition where the skin on the face is extra sensitive to the environment and overly reactive to triggers such as spicy foods, emotional stress, alcohol, and heat,” Dr. Zeichner says.
9. Do you have a fever?
If you have a fever along with your rash, it’s a good idea to get checked out by a medical professional, Dr. Rosenbach says. You could be having a serious allergic reaction to something like a medication, according to the Mayo Clinic. This combination of symptoms could also indicate an infection like shingles, mononucleosis, or even measles, according to the AAD.
Don’t hesitate to see your doctor for “just” a rash.
You know your body best. If any symptom feels concerning enough that you’re tempted to see a doctor, that’s a sign that you probably should seek medical advice.
Plus, even if you go through all of the above questions, it can be tough to decode a rash on your own. Luckily, dermatologists are well-versed in rashes. Seeing one can get you one step closer to putting your rash behind you.
Related:
- Here's What It Means If You Got a Skin Reaction From Your Makeup
- This Is How Often You Should Actually Be Exfoliating
- An Allergist Explains Why You Might Be Itchy All Over, Even Though You Don’t Have a Rash
Korin is a former New Yorker who now lives at the beach. She received a double B.A. in International Relations and Marketing from The College of William & Mary (which she doesn't use at all now) and an M.A. in Interactive Journalism from American University. Korin has been published in... Read more
SELF does not provide medical advice, diagnosis, or treatment. Any information published on this website or by this brand is not intended as a substitute for medical advice, and you should not take any action before consulting with a healthcare professional.
Topicsskinskin healthallergic reactions
More from Self8 Common Types of Rashes
Is your skin itchy, dry, blistering, or red? Do you have rashes that come and go? You may have one of these common skin conditions.
Medically Reviewed
By Moira LawlerMedically Reviewed by Ross Radusky, MD
Reviewed:
Itchy? It may be time to schedule an appointment with a dermatologist.
iStockSkin conditions can be hard to identify. Is it dermatitis or hives? A breakout or an infection? Because rashes may need to be treated a certain way, if you don't know what you have, you may inadvertently be making it worse. Whether it’s a minor nuisance or an epidermis nightmare, there are ways to soothe your skin — once you know what you’re dealing with.
“With most skin conditions, you either have a genetic predisposition to them or not,” says Ranella Hirsch, MD, a board-certified dermatologist based in Cambridge, Massachusetts. “They can be exacerbated by stress — either emotional, such as meeting your future in-laws, or environmental, such as an allergen.”
Some skin conditions (athlete’s foot, for instance) can be cured, but most are chronic or recurring. They can be triggered by anything from weather (as in the case of atopic dermatitis) to perfume (as with contact dermatitis). Many of these rashes come and go.
They can be triggered by anything from weather (as in the case of atopic dermatitis) to perfume (as with contact dermatitis). Many of these rashes come and go.
RELATED: 7 Types of Eczema and Photos of What They Look Like
Read on to learn about eight common skin conditions and their symptoms and triggers. You’ll find photos of each, to assist in identification, as well as some simple soothing tips courtesy of experts. Remember: It’s important to see a doctor if you’re dealing with a concerning skin issue, especially if lifestyle and over-the-counter treatments don’t provide relief.
202
Eczema (Atopic Dermatitis)
Sergio Azenha/AlamyThe most common type of eczema is atopic dermatitis, and the terms are often used interchangeably to describe the same skin condition. Symptoms of atopic dermatitis are often confused with those of psoriasis; but they aren’t the same. Both can cause red, raised, itchy patches of skin on the hands and scalp, but eczema tends to come with really intense itching, according to Penn Medicine.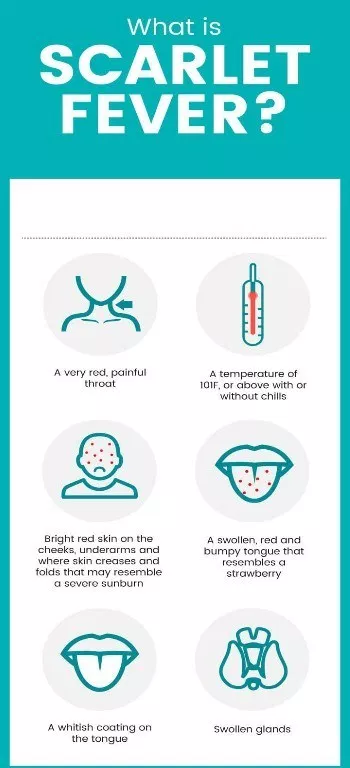 They’re also caused by different things. Psoriasis is an autoimmune disease, while eczema could be the result of genetic or environmental factors.
They’re also caused by different things. Psoriasis is an autoimmune disease, while eczema could be the result of genetic or environmental factors.
With eczema, “the barrier of your skin is damaged and you’re losing moisture,” says Katie Rodan, MD, a board-certified dermatologist and cofounder of Rodan + Fields based in Oakland, California. She compares the condition to a leaky roof: When you have eczema, “anything irritating and allergenic can enter [the skin] more easily, making you more prone to rashes and infections.”
About 20 percent of infants have eczema, according to Johns Hopkins Medicine. Many kids outgrow eczema, though it sometimes sticks around into adolescence or adulthood.
Commonly affected areas include the eyelids, elbows, hands, feet, knees, and ankles, according to the Mayo Clinic. Triggers for eczema include environmental factors, such as hot weather, according to Penn Medicine, or contact with certain products, such as chemicals or drying detergents, says Joyce Davis, MD, a board-certified dermatologist based in New York City. “It is vital to wear gloves when working with chemicals and be sure to use a laundry detergent that is hypoallergenic and gentle on skin, like the Arm & Hammer Sensitive Skin, Free & Clear laundry detergent,” she says.
“It is vital to wear gloves when working with chemicals and be sure to use a laundry detergent that is hypoallergenic and gentle on skin, like the Arm & Hammer Sensitive Skin, Free & Clear laundry detergent,” she says.
First, stop scratching!
“Eczema creates a vicious itch-scratch cycle,” Dr. Hirsch says. “The skin’s dryness [causes] itchiness, which makes you scratch. Scratching makes your skin thicker, which itches more.”
The Mayo Clinic and Hirsch recommend a combination of treatments and lifestyle changes:
- Use an anti-itch lotion, such as a topical steroid with 1 percent hydrocortisone, which is available over the counter. If over-the-counter products don’t work, a dermatologist can prescribe creams that control the itching and help repair the skin. But long-term use of steroid treatments isn’t recommended, because they can thin the skin.
- Choose mild soap that doesn’t include dyes or fragrances, and be sure to thoroughly rinse it off the body.

- Buy skin-care products that are unscented, not fragrance free. “Fragrance free means they’ve used a chemical to mask a scent, and those chemicals can be irritating,” Hirsch says.
- Avoid long, hot showers and instead take a bath with baking soda, uncooked oatmeal, or colloidal oatmeal. Pat the skin dry afterward, and apply moisturizer while the skin is still damp. “If you put a thin layer on damp, not dry, skin, it will penetrate quickly,” Hirsch says.
RELATED: 6 Useful Apps and Devices for Managing Eczema or Atopic Dermatitis
203
Contact Dermatitis
ShutterstockContact dermatitis is a different type of eczema, triggered by physically touching something that irritates or causes an allergic reaction, according to the American Academy of Dermatology Association (AAD). Intense itching, accompanied by a rash with fluid-filled blisters, is the hallmark of the disorder, according to AAD.
There are two types of contact dermatitis: irritant, which is more common and occurs when your skin reacts to something chemical (like a perfume or detergent), and allergic contact dermatitis, which is caused by a reaction to a substance, according to the Mayo Clinic. Common contact dermatitis triggers include nickel jewelry, hair dye, cosmetics, skin-care products, nail polish, formaldehyde, rubbing alcohol, and poison ivy.
Common contact dermatitis triggers include nickel jewelry, hair dye, cosmetics, skin-care products, nail polish, formaldehyde, rubbing alcohol, and poison ivy.
“It is usually not immediate; it takes a few days for contact dermatitis to appear on your skin the first time around,” Dr. Davis says. “The second time, it may appear sooner.”
Rash RxFor both irritant and allergic contact dermatitis, use over-the-counter or prescription topical cortisone, Davis says.
“Unfortunately, there is no ‘cure’ for an irritant or allergic sensitivity, although some can improve with time,” says Lisa Anthony, MD, a board-certified dermatologist at Westmed Medical Group in Westchester, New York. Preventing contact dermatitis, however, can be simple: Avoid what’s making you break out — if you’re able to identify the culprit yourself, says the Mayo Clinic. Dr. Anthony says that’s not always easy.
Identifying an allergic reaction may require a test, in which a doctor applies a small patch with allergens on it to see if your skin reacts, per a study published in the July–August 2015 issue of Missouri Medicine.
If costume jewelry is the problem, here’s a quick fix: Paint clear nail polish or apply clear tape on the underside to create a barrier between it and your skin, the Mayo Clinic advises.
RELATED: A Comprehensive Eczema Glossary
204
Seborrheic Dermatitis
Warut Chinsai/ShutterstockLike dandruff gone haywire, seborrheic dermatitis (sometimes called “scalp eczema”) is a fungus that typically crops up in oily areas such as the scalp, face, upper chest, and back, according to research published in Pharmacy and Therapeutics.
The study noted that it’s extremely common and affects about 12 percent of the population and up to 70 percent of infants in their first three months of life. It seems to be caused by yeasts belonging to the genus Malassezia, the authors wrote.
Rash RxSeborrheic dermatitis on the scalp is often treated with over-the-counter dandruff shampoos with ingredients that reduce the skin’s fungal population, Anthony says. Look for shampoos with zinc, selenium, or ketoconazole, and leave the shampoo on the scalp for five minutes before rinsing, recommends Harvard Health Publishing. “Depending on your individual hair type, try to shampoo daily until the condition improves,” Anthony says. “For thicker scale, one can add mineral oil to soften and comb out stubborn flakes.”
Look for shampoos with zinc, selenium, or ketoconazole, and leave the shampoo on the scalp for five minutes before rinsing, recommends Harvard Health Publishing. “Depending on your individual hair type, try to shampoo daily until the condition improves,” Anthony says. “For thicker scale, one can add mineral oil to soften and comb out stubborn flakes.”
If that doesn’t work, your doctor can prescribe stronger shampoos and medications.
Outbreaks on the face and body can be treated with topical corticosteroids or antifungal medications, notes the Cleveland Clinic.
Try lifestyle changes too, including de-stressing tactics. Stress is one factor that can trigger seborrheic dermatitis, according to the AAD.
RELATED: How Stress Can Trigger Eczema and How to Avoid a Flare-Up
205
Fungal Infection
Jock itch, athlete’s foot, ringworm: These all belong to a family of infections known as tinea, involving fungus that thrives in warm, moist areas, such as in the groin, toes, and underarms, according to Johns Hopkins Medicine.
“These warm, dark, moist areas create the perfect environment for fungus to breed,” says Crystal Murray Holmes, DPM, a podiatrist in Canton, Michigan, and an associate professor at the University of Michigan.
The symptoms depend on where on the body the infection appears, according to MedlinePlus. A red ring-shaped rash may be — you guessed it — ringworm, while athlete’s foot and jock itch appear as itchy, burning rashes on the skin.
How do you contract it? By coming into contact with an infected person or pet or infected surface, such as a communal shower floor, per MedlinePlus.
They can also be passed through things like shoes and towels, Anthony says. Fungus that causes jock itch, for example, thrives on damp towels and sweaty workout gear and is easily picked up in a locker room, MedlinePlus says.
Rash RxYour best bet for treating fungal infections are antifungal creams and oral medications, according to Cedars Sinai. Be sure to wash your hands before and after applying the creams to keep the fungus from spreading further.
Cedars Sinai recommends preventing infection by drying skin folds, feet, and the groin area well, and wearing clean, loose-fitting underwear. “Wear socks made of microfiber, which is designed to wick moisture away from the skin,” Holmes says.
Also, use flip-flops in public showers and around pools or other wet spots, and try to rotate through different pairs of shoes to minimize moisture and fungus buildup, advises Johns Hopkins Medicine.
RELATED: How Ringworm Spreads and How to Deal With It
206
Bacterial Infections
Bacterial infections can start small but grow into a big problem if left untreated. An untended wound, insect bite, or other break in the skin can allow bacteria to creep into your skin and fester, according to Merck and Co. The resulting infection can be the size of a tiny spot or can spread across the entire body, and the severity of the infection can also range from no big deal to life-threatening.
If it’s a small infection, an antibiotic ointment can be applied to the area to clear it up. But if it affects a larger area of the skin, oral or intravenous antibiotics may be needed, according to Merck and Co.
But if it affects a larger area of the skin, oral or intravenous antibiotics may be needed, according to Merck and Co.
Unfortunately, the World Health Organization notes, overuse of antibiotics has created super-strains of bacteria that don’t respond to those drugs anymore.
“Because of antibiotic resistance, bacterial infections are becoming more virulent,” Dr. Rodan says.
In a worst-case scenario, the infection can get into the blood and be fatal. “People really do die of cuts,” Hirsch says.
Rash RxYour doctor will likely start with oral antibiotics, according to the nonprofit health system Fairview. Expedite your visit and see a doctor immediately if you spot yellow pus or foul-smelling drainage from a wound, increased redness and pain at the site of the wound, changes in color or size, red streaks in the skin surrounding the wound, or if you come down with a fever. Hirsch says those symptoms are cause for concern.
You can also prevent skin infections from developing by cleaning every cut or wound immediately with soap and water, and covering with a bandage, according to Merck and Co.
RELATED: How to Wash Your Hands Correctly
207
Hives
Areeya Yodplob/AlamyA mysterious, sometimes random skin condition that may come and go, hives (also known as urticaria) have many triggers, including certain foods (such as peanuts, eggs, nuts, and shellfish), extreme cold or heat, some medications and illnesses, and insect bites, according to the American College of Allergy, Asthma, and Immunology. Genetics can also be to blame. “There can be a genetic component to hives where individuals are more prone to allergy, asthma, and eczema,” Anthony says.
In response to the trigger, the cells in your body release histamine, a chemical that makes the body go into inflammatory overdrive to get rid of the allergen, according to the Cleveland Clinic. Hives and swelling result as your body responds to the flood of histamines.
If hives are accompanied by swelling of the eyes, mouth, hands, feet, or throat, or difficulty breathing, you may have angioedema. “It is similar to hives, but it can be more severe and often affects the eyes and lips,” Anthony says. “In the most severe cases, internal organs such as the respiratory tract and gut can be involved.”
Sometimes hives disappear on their own without any treatment, though applying a cold washcloth to the area can help soothe the skin, the Mayo Clinic says.
If not, try an over-the-counter oral antihistamine to reduce itching and swelling. Still not getting relief? See your doctor for an anti-inflammatory medication such as prednisone, advises the Mayo Clinic.
“Like all allergic skin reactions, each subsequent exposure can get worse” and may even be life-threatening, Rodan says.
Of course, the best remedy is prevention. Try to identify your trigger for hives and avoid it.
RELATED: What Are the Symptoms of Hives?
208
Herpes
BSIP SA/AlamyThough herpes simplex virus (HSV) infections can be transmitted through sex, that’s not the only way the virus is passed between people, according to the CDC.
“At least 80 percent of us are exposed to the herpesvirus by the time we enter kindergarten,” Rodan says, thanks to shared toys, kisses from relatives, and slobbering, germy friends.
Our immune systems usually fight off the disease, but about 20 percent of people break out in sores, Rodan says.
Oral herpes, usually HSV type 1, is usually the culprit behind cold sores and originates during childhood through nonsexual contact, according to the CDC.
“Any close contact like kissing, sharing utensils, or using a department store lipstick tester can cause it to spread,” Hirsch says. But HSV type 1 can also be transferred to the genitals during oral sex, according to the CDC.
A herpes outbreak can be triggered by stress, illness, fatigue, and sun exposure, according to Harvard Health Publishing. Though it’s rare, laser and injectable procedures (such as lip filler) at a doctor’s office can also trigger outbreaks, Davis says.
Herpes infections tend to recur in the same spot on your body because the virus lives in the nerve beneath the skin, Davis says. “When it gets triggered back to skin, it’s within the same vicinity,” she says.
HSV can be tricky to diagnose since it oftentimes looks like an allergic reaction, according to Cedars Sinai. Your doctor may take a virus culture, blood sample, or biopsy to confirm the presence of HSV.
There is no cure, but prescription antiviral medication like Valtrex can reduce the number of herpes outbreaks, according to the Mayo Clinic. Taken in pill form, it can reduce the severity and duration of outbreaks.
A doctor can prescribe topical treatments, such acyclovir and hydrocortisone, to help lessen the symptoms, says the University of Michigan.
RELATED: Is It Herpes or Something Else?
209
Shingles
Geoff Oliver/AlamyShingles, another viral rash, is a reactivation of the chicken pox virus, according to the CDC. These painful, itchy, and tingly rashes tend to appear on the torso and will follow the path of a nerve on just one side of the body. “It picks one nerve on either the left or the right side of the body,” Davis says. “It goes around the rib, one part of the face, and it’s very easy to diagnose.”
People with shingles won’t spread shingles to other people, but they can infect others with chicken pox if the person on the receiving end hasn’t had it, according to the Mayo Clinic.
Shingles can occur among people who’ve had chicken pox before, and since most adults in the United States did have chicken pox as kids, they’re at risk, especially if they’re over 50 and have compromised immune systems, according to the Mayo Clinic.
A shingles rash usually goes away within five weeks, and most people will only get shingles once, according to the National Institute on Aging. Sometimes, however, the pain will linger, especially among older people. Known as postherpetic neuralgia (PHN), it can lead to depression, trouble sleeping, and weight loss.
Rash RxThere are two shingles vaccinations, which should prevent an infection in the first place, according to the CDC. And, as with herpes, an antiviral medication can reduce the severity and duration of a shingles outbreak, especially when taken within three days of the rash appearing, according to MedlinePlus. If you have mild pain, an over-the-counter pain reliever, cool washcloth, calamine lotion, and oatmeal baths may help.
RELATED: How to Prevent and Treat Shingles
Allergic rash - urticaria | Symptoms
Drugs, contrast agents (used in imaging studies such as computed tomography)
Signs: Allergic rash that begins within 48 hours after using the drug.
Emotional and physical stimuli (stress and anxiety, cold, exercise, skin pressure, heat, sunlight, sweating)
Signs: Allergic rash, which usually begins within seconds or minutes after contact with an irritant; an allergic rash that starts within 4 to 6 hours and affects only the area of skin where pressure has been applied, or an allergic rash that only affects the area of skin exposed to sunlight.
Food (food allergens)
Signs: Allergic rash that starts within minutes or hours of consumption.
Infections (bacterial, parasitic, viral)
Signs: Fever, chills, and fatigue. Specific infection symptoms, particularly for parasitic infections, recent travel to a developing country.
Insect bites or burns
Signs: Allergic rash that starts within seconds or minutes of an insect bite or burn.
Serum sickness
Signs: Allergic rash that begins within 7 to 10 days after an injection of a blood product (as in a transfusion), a drug derived from the blood of animals (used to treat venomous snake and spider bites). May be accompanied by fever, joint pain, swollen lymph nodes, and abdominal pain.
Contact allergens (latex, animal saliva or dander, dust, pollen or mold)
Signs: Allergic rash that begins within minutes or hours of contact.
Transfusion reactions
Signs: Allergic rash that usually starts within minutes of a blood product transfusion.
Systemic lupus erythematosus
Signs: Various symptoms depending on the autoimmune disease. In systemic lupus erythematosus, symptoms may include fever, fatigue, headache, joint pain and swelling, pain when breathing, and mouth ulcers.
Sjögren's syndrome
Signs: Dry eyes and dry mouth.
Urticarial vasculitis
Signs: An allergic rash that may be painful but not itchy. Usually lasts more than 24 hours. Does not whiten (brighten) when pressure is applied. May be accompanied by the formation of small blisters and red-violet spots (purpura).
Cancer (digestive or lung or lymphoma)
Signs: Weight loss, night sweats, abdominal pain, cough (sometimes with blood), jaundice, swollen lymph nodes, or a combination of these symptoms.
Chronic idiopathic allergic rash
Signs: Allergic rash that occurs almost daily and itching that lasts for 6 weeks with no apparent cause.
Endocrine disorders (thyroid disease or elevated progesterone)
Signs: For thyroid disorders: difficulty in tolerating heat or cold, slow or fast heart rate, and shaking (tremor) or slowness. Occurs in women who take birth control pills, undergo hormone therapy, or who have an allergic rash that appears before the onset of the menstrual period and disappears after it ends.
Mastocytosis
Signs: Small red bumps that turn into an allergic rash when touched. Sometimes abdominal pain, mild flushing, and recurring headaches.
symptoms and signs, treatment of urticaria in children and adults
Urticaria ranks second after bronchial asthma among dangerous allergic diseases. Urticaria most often manifests itself in the form of an allergy to some irritant or may be a consequence of a certain disease. It manifests itself in acute or chronic form. Acute urticaria occurs suddenly and lasts for several days or for 1-2 weeks. Chronic urticaria is observed for a long time for several years, rashes occur every day or at intervals.
There are several types of urticaria depending on the factors of the disease:
- Allergic urticaria - the reaction occurs due to various pathogens, insect bites, food products.
- Idiopathic urticaria - this type of disease is diagnosed if it is impossible to determine the causes of allergies.
- Cholinergic urticaria - occurs due to severe emotional stress or physical exertion, in the presence of disorders of the nervous system. May present in a chronic form.
- Cold urticaria - manifested as a result of the body's reaction to a cold climate, wind or water. Most common in countries with cold and temperate climates.
Causes of urticaria
The basis of the disease is the body's reaction to irritating factors. Urticaria is caused by high sensitivity to a specific pathogen. It could be an insect bite or some foods. The antigen causes a reaction in the body, and the antibody is produced by the immune system to destroy the extracellular antigen.
Urticaria may occur against the background of anaphylactoid reactions. In this case, the ability of mast cells (cells that are located under the skin and mucous membranes and contain a large amount of biologically active substances) to release accumulated enzymes and active proteins increases. This phenomenon occurs without the participation of cells of the immune system in it.
Among the causes of urticaria are chronic liver diseases, which lead to a decrease in the destruction of histamine, which is actively involved in the allergic reaction. In many cases, urticaria appears after an autoimmune inflammation. In this state, the body's immune system perceives its own tissues as foreign, resulting in an allergy.
Other causes of urticaria are not fully understood, doctors find new factors every year. The disease is exacerbated after taking certain drugs, products, insect bites. The chronic form of urticaria develops against the background of changes in the body and long-term diseases: chronic cholecystitis, adnexitis, tonsillitis, sinusitis, stomach diseases, viral and bacterial diseases, alcoholism and others.
Symptoms of urticaria
Urticaria is much more severe in children than in adults. It can manifest itself in mild, moderate and severe forms. A mild form of urticaria is accompanied by mild symptoms: slight itching, no nausea, no swelling. Rashes on the skin are formed in one place and disappear after a day.
In moderate form of urticaria, the patient's condition worsens. Nausea, headaches, fever may occur, Quincke's edema forms in some areas of the body. This is a rapidly occurring swelling of the skin with allergies, which spreads throughout the body in a short period. First, swelling occurs on the eyelids and lips, then the face and hands swell. The most dangerous is swelling of the larynx and tongue, in which the patient can suffocate if he is not helped in time. The skin swells, rashes are accompanied by painful sensations.
The most characteristic symptom of urticaria is the formation of blisters on the face and hands. Formations of a red or pink hue, resemble a trace from an insect bite or a burn after a nettle. At the site of the rash, the skin itches and becomes red. Skin formations can merge, covering some parts of the body. As a rule, they are symmetrical.
Moderate urticaria may affect the gastrointestinal tract, causing severe nausea and vomiting. The patient may experience a slight burning sensation and itching of the skin. Edema disappears after a few hours, or after 1-2 days, relapses of the disease are not excluded. In a severe form of the disease, the temperature rises, Quincke's edema occurs, which must be eliminated with allergy medications. Eruptions appear on the mucous membranes of various organs.
Urticaria proceeds mostly without complications, the skin returns to its previous appearance. After the rash, there is no pigmentation, scarring and other traces. Blisters can occur anywhere on the body and spread to the skin. In the chronic form of the disease, nervous disorders and insomnia can occur due to severe itching and discomfort on the skin.
Treatment of urticaria
How to treat urticaria:
- elimination of the pathogen;
- correct diet, excluding allergen foods;
- taking allergy medications;
- body cleansing.
Treatment of urticaria involves, first of all, the elimination of the negative factor that causes allergies. If the disease has arisen due to products, it is necessary to remove allergen substances from the body. You can take a laxative and drink plenty of fluids. Allergy to foods is quickly removed with the help of a cleansing enema, diuretics. It is most effective in the first hours of manifestation of urticaria.
Symptoms of urticaria are eliminated with the help of effective antihistamines, sulfates. Due to their influence on the body, the patient's condition is facilitated, the rash on the skin and itching are reduced. The medicine is used in the form of injections or tablets. It is best to take the drugs at bedtime, as they cause apathy and drowsiness.
You can book medicines on our website.
Cold compresses help relieve discomfort and itching. To do this, mix one tablespoon of vinegar in a glass of cool water, moisten a bandage and apply to the affected area of the skin.
Proper nutrition is equally important in the treatment of urticaria. It is aimed at eliminating painful symptoms and protecting the body from external factors. It is necessary to exclude the food allergen from the diet, and strictly adhere to the prescribed diet for 2 weeks or a month.
With this diagnosis, you can consume dairy products in the form of kefir and cottage cheese, boiled or steamed vegetables, some fruits, excluding citrus fruits, strawberries and other allergens. Confectionery, pastries, strong tea and coffee, canned food, salty foods should be excluded from the diet. During the treatment of urticaria, it is necessary to refrain from milk, eggs, carrots, beets, tomatoes, red peppers, mushrooms, apples, cocoa, nuts, honey, seasonings and spices, as well as fried and smoked dishes and foods.
New products should be introduced into the patient's diet gradually, giving in small quantities. If, after the inclusion of a new product in the diet, the urticaria has not returned, you can give boiled meat or fish. In this case, the diet should be followed for a month. During treatment, you can not treat the urticaria rash with a regular cream or ointment. This will only exacerbate the rash.
During the treatment period, it is forbidden to take a hot bath, visit a sauna or bath, spend time on the beach, as the sun's rays irritate and dry the skin. If a person gets sick with hives in the summer, before going out, it is necessary to lubricate the skin with a high protection sun cream. In the cold season, you need to dress warmer, be sure to use gloves and a hat.
To restore the metabolic process in the body, it is necessary to take iron complexes, B vitamins, sodium and others. During an attack of urticaria, glucocorticoids, as well as histaglobin, can be used. For external treatment, baths with a decoction of chamomile, string, starch and bran are used, the skin is lubricated with water-zinc paste, ointments with hormones. However, external therapy for urticaria has little effect.
Prevention of urticaria
Prevention of urticaria primarily involves the exclusion of the negative factor that causes allergies. It is necessary to treat diseases of the gastrointestinal tract, liver, kidneys, to avoid viral diseases, helminthic pathogens. It is important to observe proper nutrition, lead an active lifestyle, protect yourself from the effects of stress and other loads.
Patients with chronic urticaria are advised by allergists to adhere to certain rules:
- wash hands and take a shower in warm water, as hot water negatively affects the skin and causes irritation;
- it is better to buy clothes from natural fabrics made from cotton, linen, as they do not cause irritation, it is better to refuse synthetics;
- for hygiene, you should choose liquid soap with natural oils so that it does not dry the skin;
- after bathing or taking a shower, you need to wipe yourself with a soft-bristled towel so as not to injure the skin;
- it is worth excluding exposure to direct sunlight and sunbathing in a solarium, especially for women;
- avoid emotional stress and stress, take sedatives in the form of herbal preparations and tinctures to calm down;
- exclude aspirin in the diagnosis of allergic urticaria;
- observe proper nutrition, do not eat foods, fruits and vegetables that cause an allergic reaction.