What is in an epidural injection for labor
What is an Epidural | American Pregnancy Association
Epidural anesthesia is the most popular method of pain relief during labor. Women request an epidural by name more than any other method of pain relief. More than 50% of women giving birth at hospitals use epidural anesthesia.
As you prepare yourself for “labor day,” try to learn as much as possible about pain relief options so that you will be better prepared to make decisions during the labor and birth process. Understanding the different types of epidurals, how they are administered, and their benefits and risks will help you in your decision-making during the course of labor and delivery.
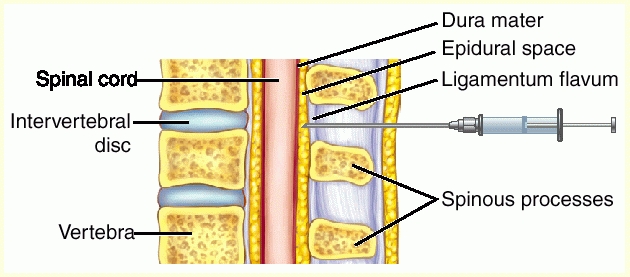
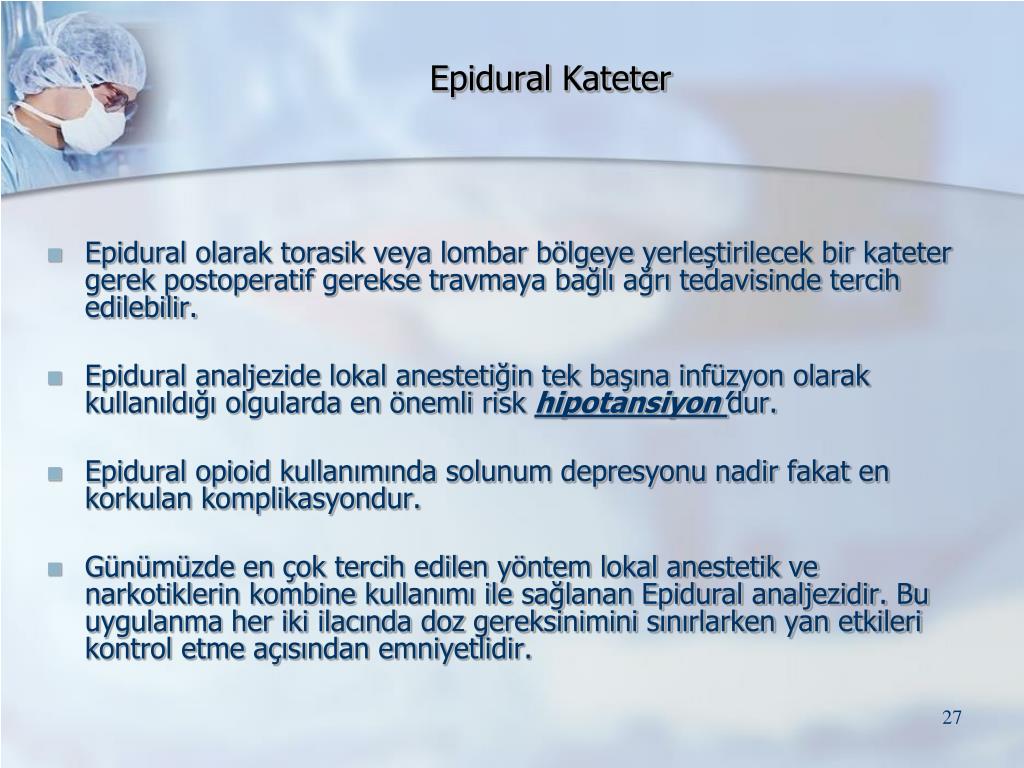
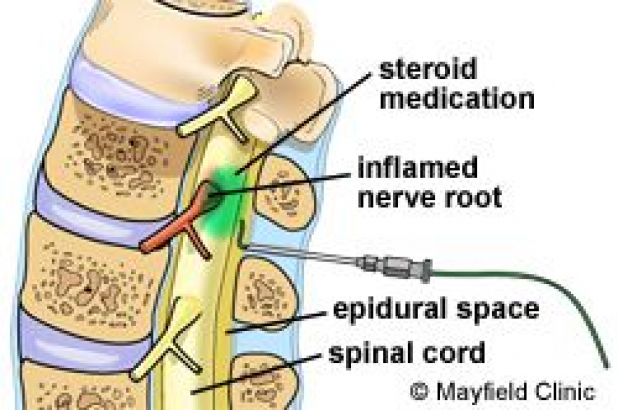
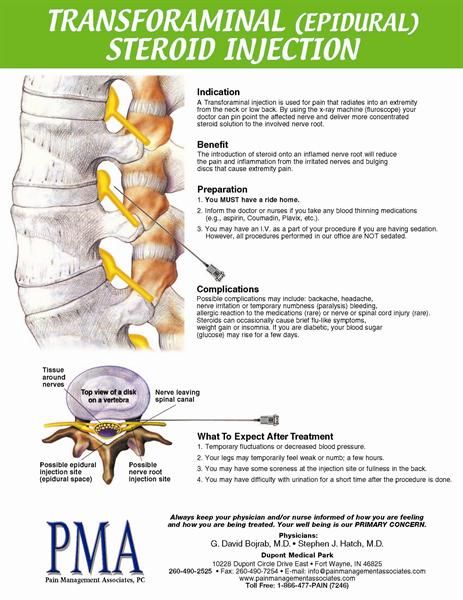
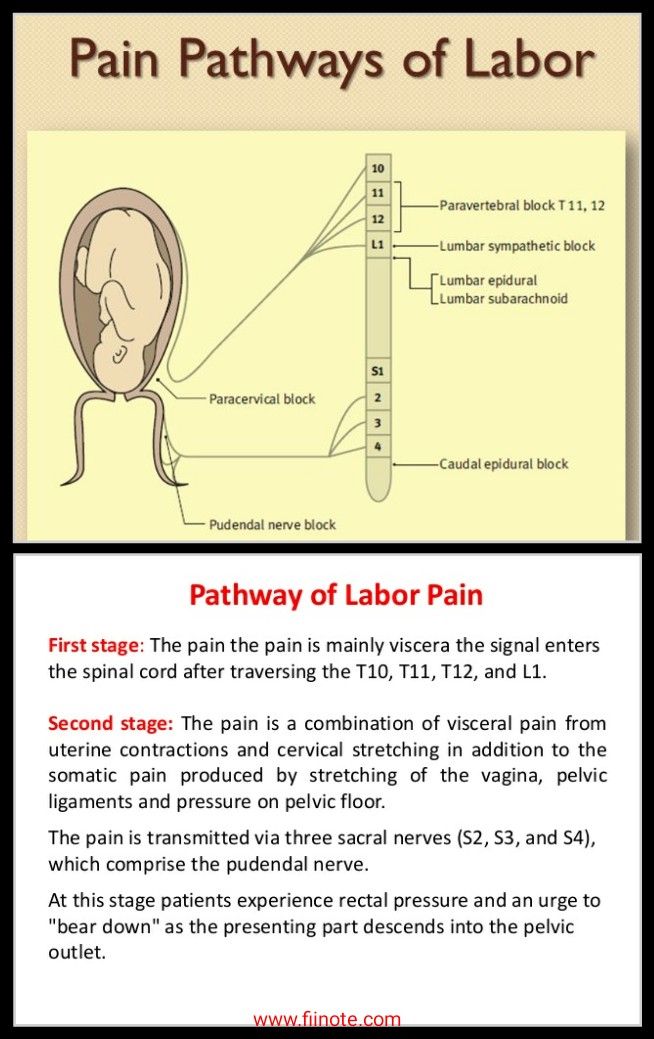
Epidural anesthesia is regional anesthesia that blocks pain in a particular region of the body. The goal of an epidural is to provide analgesia, or pain relief, rather than anesthesia, which leads to a total lack of feeling. Epidurals block the nerve impulses from the lower spinal segments. This results in decreased sensation in the lower half of the body.
Epidural medications fall into a class of drugs called local anesthetics, such as bupivacaine, chloroprocaine, or lidocaine. They are often delivered in combination with opioids or narcotics such as fentanyl and sufentanil in order to decrease the required dose of local anesthetic.
This produces pain relief with minimal effects. These medications may be used in combination with epinephrine, fentanyl, morphine, or clonidine to prolong the epidural’s effect or to stabilize the mother’s blood pressure.
How is an epidural given?
Intravenous (IV) fluids will be started before active labor begins and prior to the procedure of placing the epidural. You can expect to receive 1-2 liters of IV fluids throughout labor and delivery. An anesthesiologist (specialize in administering anesthesia), an obstetrician or nurse anesthetist will administer your epidural.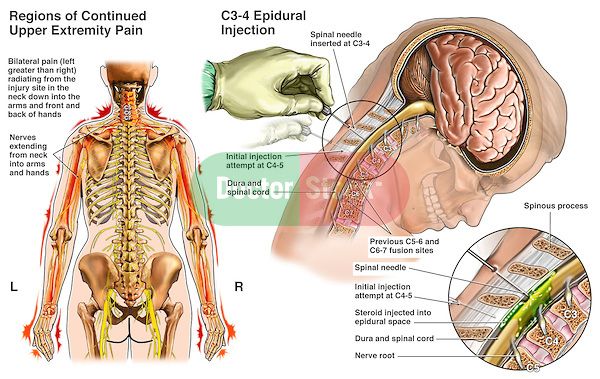
You will be asked to arch your back and remain still while lying on your left side or sitting up. This position is vital for preventing problems and increasing epidural effectiveness.
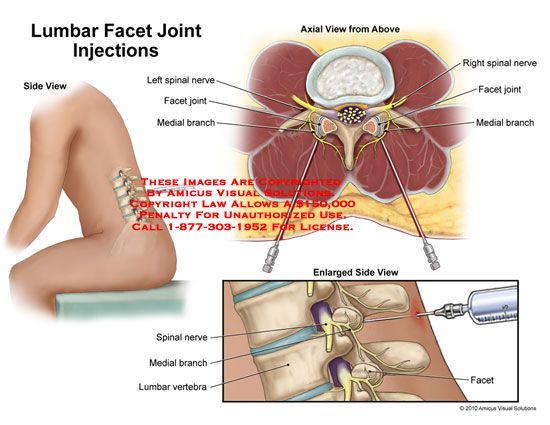
- An antiseptic solution will be used to wipe the waistline area of your mid-back to minimize the chance of infection. A small area on your back will be injected with a local anesthetic to numb it. A needle is then inserted into the numbed area surrounding the spinal cord in the lower back.
- After that, a small tube or catheter is threaded through the needle into the epidural space. The needle is then carefully removed, leaving the catheter in place to provide medication either through periodic injections or by continuous infusion. The catheter is taped to the back to prevent it from slipping out.
- You’ll start to notice the numbing effect about 10 to 20 minutes after the first dose of medication, though the nerves in your uterus will begin to go numb within a few minutes. You’ll receive continuous doses of medication through the catheter for the rest of your labor.
What are the different types?
There are two basic epidurals in use today. Hospitals and anesthesiologists will differ on the dosages and combinations of medication. You should ask your care providers at the hospital about their practices in this regard.
Regular Epidural
After the catheter is in place, a combination of narcotic and anesthesia is administered either by a pump or by periodic injections into the epidural space. A narcotic such as fentanyl or morphine is given to replace some of the higher doses of anesthetic, like bupivacaine, chloroprocaine, or lidocaine.
This helps reduce some of the adverse effects of the anesthesia. You will want to ask about your hospital’s policies about staying in bed and eating.
Combined Spinal-Epidural (CSE) or “Walking Epidural”
A spinal block is sometimes used in combination with an epidural during labor to provide immediate pain relief. A spinal block, like an epidural, involves an injection in the lower back. While you sit or lie on your side in bed, a small amount of medication is injected into the spinal fluid to numb the lower half of the body. It brings good relief from pain and starts working quickly, but it lasts only an hour or two and is usually given only once during labor. The epidural provides continued pain relief after the spinal block wears off.
While you sit or lie on your side in bed, a small amount of medication is injected into the spinal fluid to numb the lower half of the body. It brings good relief from pain and starts working quickly, but it lasts only an hour or two and is usually given only once during labor. The epidural provides continued pain relief after the spinal block wears off.
What are the benefits of epidural anesthesia?
- An epidural provides a route for very effective pain relief that can be used throughout your labor.
- The anesthesiologist can control the effects by adjusting the type, amount, and strength of the medication. This is important because as your labor progresses and your baby moves down into your birth canal, the dose you’ve been getting might no longer be adequate, or you might suddenly have pain in a different area.
- The medication only affects a specific area, so you’ll be awake and alert during labor and birth. And because you’re pain-free, you can rest (or even sleep!) as your cervix dilates and conserve your energy for when it comes time to push.
- Unlike with systemic narcotics, only a tiny amount of medication reaches your baby.
- Once the epidural is in place, it can be used to provide anesthesia if you need a c-section or if you’re having your tubes tied after delivery.
What are the risks of epidural anesthesia?
- You have to stay still for 10 to 15 minutes while the epidural is put in, and then wait up to 20 minutes before the medication takes full effect.
- Epidurals may cause your blood pressure to suddenly drop. For this reason, your blood pressure will be routinely checked to help ensure adequate blood flow to your baby. If there is a sudden drop in blood pressure, you may need to be treated with IV fluids, medications, and oxygen.
- You may experience a severe headache caused by leakage of spinal fluid. Less than 1% of women experience this side effect. If symptoms persist, a procedure called a “blood patch”, which is an injection of your blood into the epidural space can be performed to relieve a headache.
- After your epidural is placed, you will need to alternate sides while lying in bed and have continuous monitoring for changes in fetal heart rate. Lying in one position can sometimes cause labor to slow down or stop.
- You might experience the following side effects: shivering, a ringing of the ears, backache, soreness where the needle is inserted, nausea, or difficulty urinating.
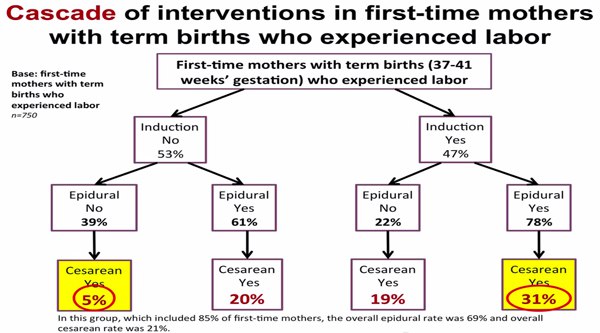
- You might find that your epidural makes pushing more difficult and additional medications or interventions may be needed, such as forceps or cesarean. Talk to your doctor when creating your birth plan about what interventions he or she generally uses in such cases.
- For a few hours after the birth, the lower half of your body may feel numb. Numbness will require you to walk with assistance.
In rare instances, permanent nerve damage may result in the area where the catheter was inserted. - Though research is somewhat ambiguous, most studies suggest that some babies will have trouble “latching on” causing breastfeeding difficulties.
 Other studies suggest that a baby might experience respiratory depression, fetal malpositioning, and an increase in fetal heart rate variability, thus increasing the need for forceps, vacuum, cesarean deliveries, and episiotomies.
Other studies suggest that a baby might experience respiratory depression, fetal malpositioning, and an increase in fetal heart rate variability, thus increasing the need for forceps, vacuum, cesarean deliveries, and episiotomies.
How Long Does an Epidural Last?
Once the catheter is in place, the anaesthetist can set up an epidural pump. The pump feeds the epidural solution into the catheter continuously, providing pain relief for as long as needed.
The type, amount and strength of the anaesthetic can be adjusted, as necessary. You might also be given the option of having control of the medication pump. This is called patient controlled analgesia. The amount of painkiller is still regulated, so you can’t accidentally overdose.
You can have the dose lowered for second stage pushing, but it takes some time for the pain relief and numbness to wear off, so if this is important to you, discuss it with your care provider early on.
Common Questions About Epidurals
Does the placement of epidural anesthesia hurt?The answer depends on who you ask.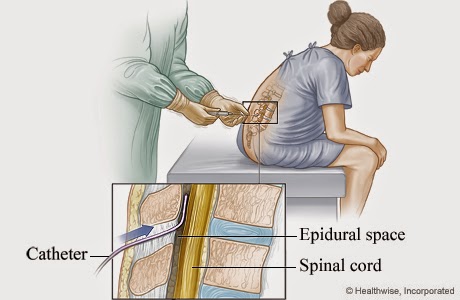 Some women describe an epidural placement as creating a bit of discomfort in the area where the back was numbed, and a feeling of pressure as the small tube or catheter was placed.
Some women describe an epidural placement as creating a bit of discomfort in the area where the back was numbed, and a feeling of pressure as the small tube or catheter was placed.
Typically epidurals are placed when the cervix is dilated to 4-5 centimeters and you are in true active labor.
Can an epidural slow labor or lead to a cesarean delivery (C-section)?There is no credible evidence that it does either. When a woman needs a C-section, other factors usually are at play, including the size or position of the baby or slow progression of labor due to other issues. With an epidural, you might be able to feel contractions — they just won’t hurt — and you’ll be able to push effectively. There is some evidence that epidurals can speed the first stage of labor by allowing the mother to relax.
How can an epidural affect my baby?As previously stated, research on the effects of epidurals on newborns is somewhat ambiguous, and many factors can affect the health of a newborn.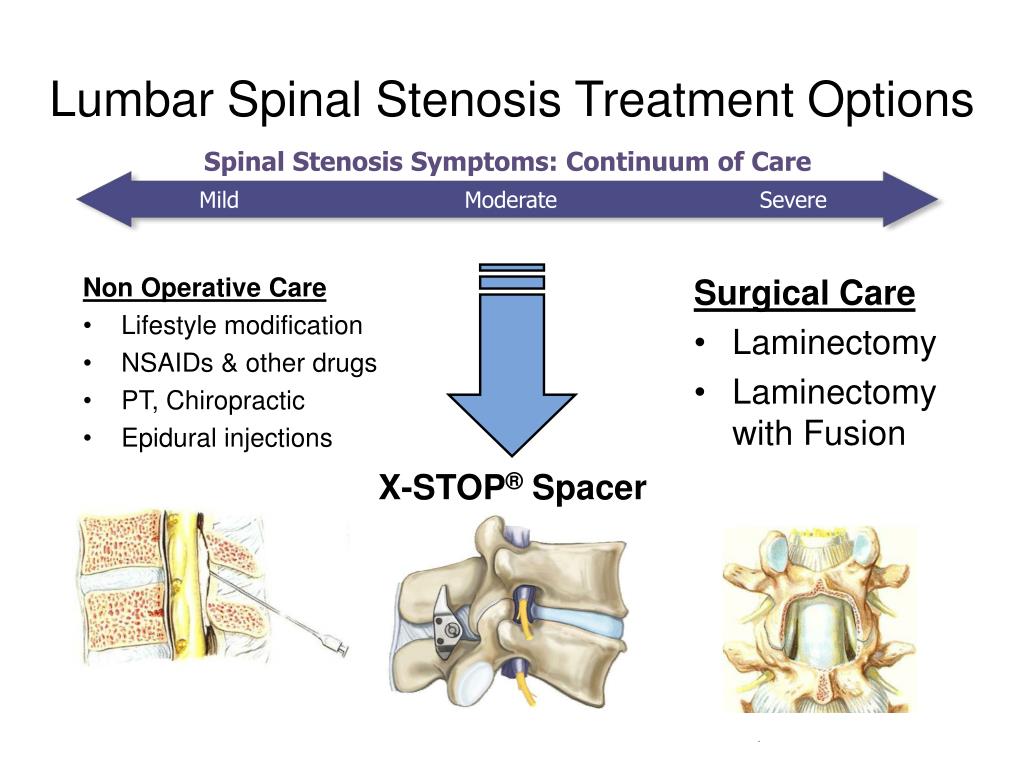 How much of an effect these medications will have is difficult to predetermine and can vary based on dosage, the length of labor, and the characteristics of each individual baby.
How much of an effect these medications will have is difficult to predetermine and can vary based on dosage, the length of labor, and the characteristics of each individual baby.
Since dosages and medications can vary, concrete information from research is currently unavailable. One possible side effect of an epidural with some babies is a struggle with “latching on” in breastfeeding. Another is that while in-utero, a baby might also become lethargic and have trouble getting into position for delivery.
These medications have also been known to cause respiratory depression and decreased fetal heart rate in newborns. Though the medication might not harm these babies, they may have subtle effects on the newborn.
How will I feel after the placement of an epidural?The nerves of the uterus should begin to numb within a few minutes after the initial dose. You will probably feel the entire numbing effect after 10-20 minutes. As the anesthetic dose begins to wear off, more doses will be given–usually every one to two hours.
Depending on the type of epidural and dosage administered, you can be confined to your bed and not allowed to get up and move around.
If labor continues for more than a few hours you will probably need urinary catheterization, because your abdomen will be numb, making urinating difficult. After your baby is born, the catheter is removed and the effects of the anesthesia will usually disappear within one or two hours.
Some women report experiencing an uncomfortable burning sensation around the birth canal as the medication wears off.
Will I be able to push?You might not be able to tell that you are having a contraction because of your epidural anesthesia. If you can not feel your contractions, then pushing may be difficult to control. For this reason, your baby might need additional help coming down the birth canal. This is usually done by the use of forceps.
Does an epidural always work?For the most part, epidurals are effective in relieving pain during labor. Some women complain of being able to feel pain, or they feel that the drug worked better on one side of the body.
Some women complain of being able to feel pain, or they feel that the drug worked better on one side of the body.
An epidural may not be an option to relieve pain during labor if any of the following apply:
- You use blood thinners
- Have low platelet counts
- Are hemorrhaging or in shock
- Have an infection on or in your back
- Have a blood infection
- If you are not at least 4 cm dilated
- Epidural space cannot be located by the physician
- If labor is moving too fast and there is not enough time to administer the d
Questions to ask your healthcare providers now and at the time of delivery in the hospital:
- What combination and dosage of drugs will be used?
- How could the medications affect my baby?
- Will I be able to get up and walk around?
- What liquids and solid foods will I be able to consume?
Want to Know More?
- Nitrous Oxide During Labor
- Stages of Labor: Stage 1
- Inducing Labor
- Cord Blood Banking: Your Three Choices Explained
Compiled using information from the following sources:
1. American Academy of Family Physicians
American Academy of Family Physicians
https://www.aafp.org
2. William’s Obstetrics Twenty-Second Ed. Cunningham, F. Gary, et al, Ch. 19.
3. Mayo Clinic Guide To A Healthy Pregnancy Harms Roger W., M.D., et al, Part 2.
Epidurals: Meaning and Side Effects of Anesthesia During Labor
An epidural is the most common type of anesthetic used for pain relief during labor. Here’s what you should know before having an epidural, including information that dispels some common myths.
How and when is an epidural for labor pain administered?If you choose to have an epidural, an anesthesiologist will insert a needle and a tiny tube, called a catheter, in the lower part of your back. The needle is removed and the catheter left in place for delivery of the medication through the tube as needed. You can begin an epidural at any time during your labor — in the beginning, in the middle, or even toward the end — in consultation with your physician.
The anesthesiologist will numb the area where the epidural is administered, which may cause a momentary stinging or burning sensation. But because of this numbing, there is very little pain associated with an epidural injection. Instead, most patients will feel some pressure as the needle is inserted.
What does an epidural do?An epidural provides anesthesia that creates a band of numbness from your bellybutton to your upper legs. It allows you to be awake and alert throughout labor, as well as to feel pressure. The ability to feel second-stage labor pressure enables you to push when it’s time to give birth to your baby. It can take about 15 minutes for the pain medication to work.
How long does the pain relief last?You can continue to receive pain relief through an epidural for as long as you need it. The amount of medication you receive through the epidural can be increased or decreased as necessary.
There is no credible evidence that it does either. When a woman needs a C-section, other factors usually are at play, including the size or position of the baby or slow progression of labor due to other issues. With an epidural, you might be able to feel contractions — they just won’t hurt — and you’ll be able to push effectively. There is some evidence that epidurals can speed the first stage of labor by allowing the mother to relax.
Can epidurals harm the baby?The amount of medication that reaches the baby from the epidural is very small, and there is no evidence that it causes any harm.
Are there risks and side effects?Epidurals are very safe; serious complications are extremely rare. However, as with all medications and medical procedures, there are potential side effects:
- Decrease in blood pressure – The medication may lower your blood pressure, which may slow your baby’s heart rate.
 To make this less likely, you will be given extra fluids through a tube in your arm (IV), and you may need to lie on your side. Sometimes, your anesthesiologist will give you a medication to maintain your blood pressure.
To make this less likely, you will be given extra fluids through a tube in your arm (IV), and you may need to lie on your side. Sometimes, your anesthesiologist will give you a medication to maintain your blood pressure. - Sore back – Your lower back may be sore where the needle was inserted to deliver the medication. This soreness should last no more than a few days. There is no evidence that an epidural can cause permanent back pain.
- Headache – On rare occasions, the needle pierces the covering of the spinal cord, which can cause a headache that may last for a few days if left untreated. If this situation arises, discuss the treatment options with your anesthesiologist.
A spinal block is sometimes used in combination with an epidural during labor to provide immediate pain relief. A spinal block, like an epidural, involves an injection in the lower back.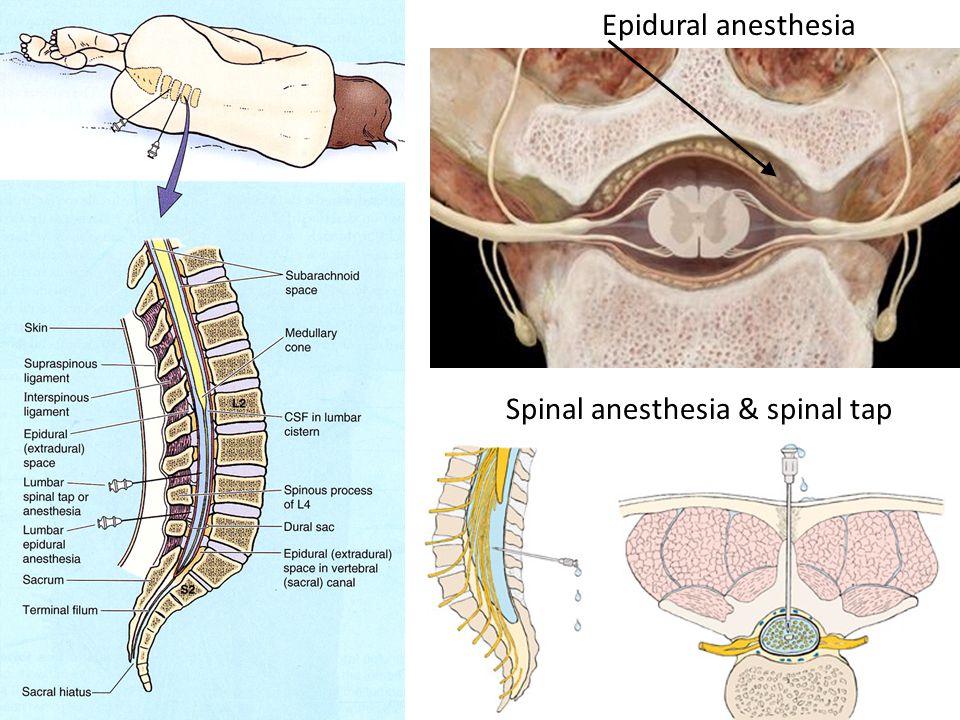 While you sit or lie on your side in bed, a small amount of medication is injected into the spinal fluid to numb the lower half of the body. It brings good relief from pain and starts working quickly, but it lasts only an hour or two and is usually given only once during labor. The epidural provides continued pain relief after the spinal block wears off.
While you sit or lie on your side in bed, a small amount of medication is injected into the spinal fluid to numb the lower half of the body. It brings good relief from pain and starts working quickly, but it lasts only an hour or two and is usually given only once during labor. The epidural provides continued pain relief after the spinal block wears off.
Anesthesiologists are committed to patient safety and high-quality care, and have the necessary knowledge to understand and treat the entire human body.
Error 404 | Regional Perinatal Center
⚡⚡⚡
Total Test "Accessible Environment"
From December 2 to 10, 2022 at 10:00 am Moscow time, the annual All-Russian campaign "Total Test" "Accessible Environment" will be held. The event is dedicated to the
International Day of Persons with Disabilities and is aimed at drawing the attention of Russian residents to the topic of inclusion, rehabilitation, an accessible environment and respect for the rights of people with disabilities.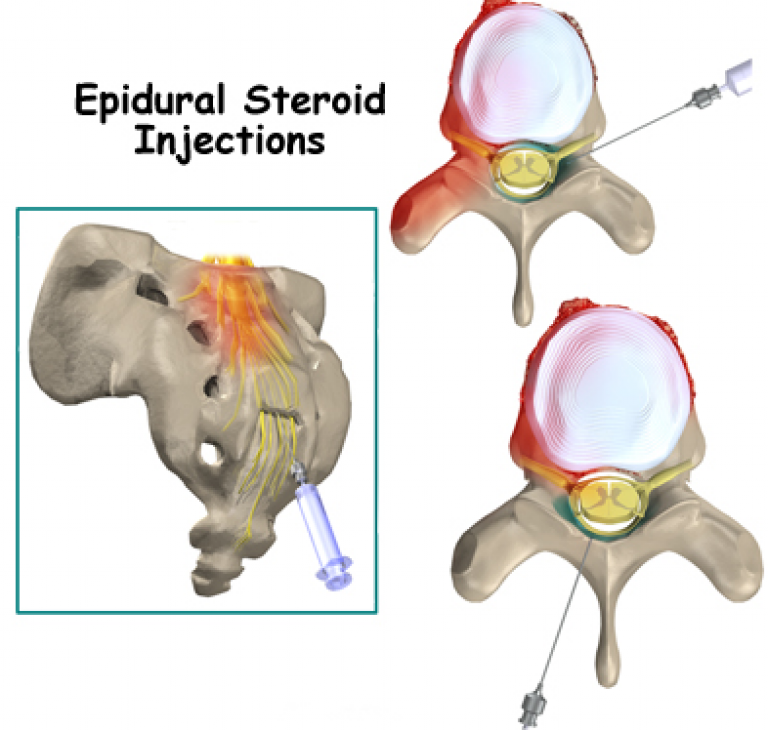
Participants pass the "Accessible Environment" Total Test remotely from any personal device with Internet access. Testing is traditionally conducted online. It includes questions on several thematic blocks: creating an accessible environment, ethics of communication with people with disabilities, rules for providing situational assistance. Also, at the end of the event, a public discussion of issues and training with the participation of leading experts will be held.
Registration on the event website using the link www.total-test.ru.
----------------------------------------------- -------------------------------------------------- -------------------------------------------------- -----------
⚡⚡⚡
Taking into account the epidemiological situation, there is currently a restriction on visits to inpatient departments of the Perinatal Center.
⚡⚡⚡ Partner births resumed.
GBUZ YaO "Regional Perinatal Center", based on letters from the Head of the Rospotrebnadzor Administration for the Yaroslavl Region dated March 21, 2022 No.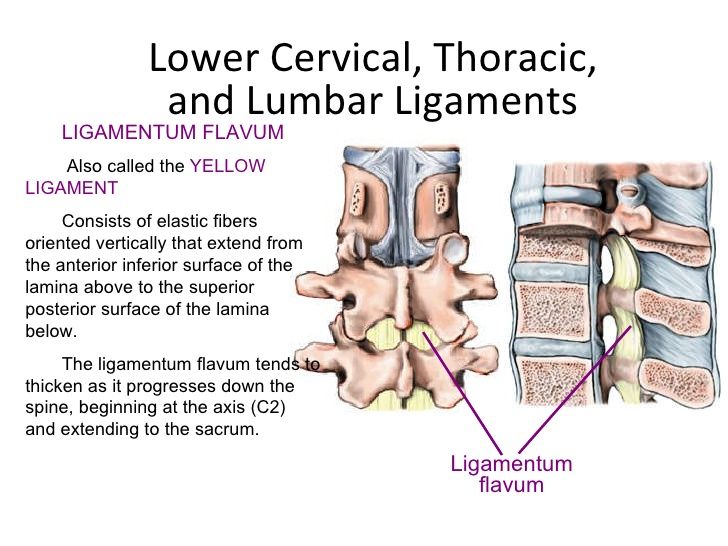 76-00-04 / 41-1099-2022, dated 04.20.2022 No. 76-00-04 / 48-1632-2022 and dated 07.01.2022 No. 76-00-04 / 41-2515-2022, informs about the possibility of partner childbirth from 03.23.2022, subject to the following conditions: the partner has a QR code about vaccination, as well as a PCR test made no later than 48 hours before delivery (!!!express test is not accepted).
76-00-04 / 41-1099-2022, dated 04.20.2022 No. 76-00-04 / 48-1632-2022 and dated 07.01.2022 No. 76-00-04 / 41-2515-2022, informs about the possibility of partner childbirth from 03.23.2022, subject to the following conditions: the partner has a QR code about vaccination, as well as a PCR test made no later than 48 hours before delivery (!!!express test is not accepted).
On the basis of clause 811. Decree of the Chief State Sanitary Doctor of the Russian Federation dated January 28, 2021 No. 4 “On approval of sanitary rules and norms SanPiN 3.3686-21 “Sanitary and epidemiological requirements for the prevention of infectious diseases”, who is present at partner childbirth, is obliged to provide the result of an examination for tuberculosis (fluorography of the chest organs) not older than 1 year.
In addition, the future father needs to have a passport, a change of shoes (clean rubber slippers), a change of clean clothes (t-shirt and pants), a pair of clean handkerchiefs, a pack of wet antibacterial wipes and a small bottle of drinking water.
⚡⚡⚡Information for accompanying persons
Due to the increased risk of the spread of COVID-19, persons accompanying patients in outpatient departments are not allowed in the building of the Perinatal Center. Entrance to the building of the Perinatal Center is allowed only for accompanying disabled patients and patients with disabilities.
⚡⚡⚡ Information for patients with infertility who need ART
In accordance with the order of the Ministry of Health of the Russian Federation of July 31, 2020 No. 803n "On the procedure for the use of assisted reproductive technologies, contraindications and restrictions to their use", which entered in force 01.01.2021, the presence of indications for ART programs is carried out by the attending physician. He also draws up a referral for infertility treatment by IVF.
To receive a referral, you need to consult a reproductive health specialist at the Department of Reproductive Health of the Regional Perinatal Center, who decides on referral to the IVF program.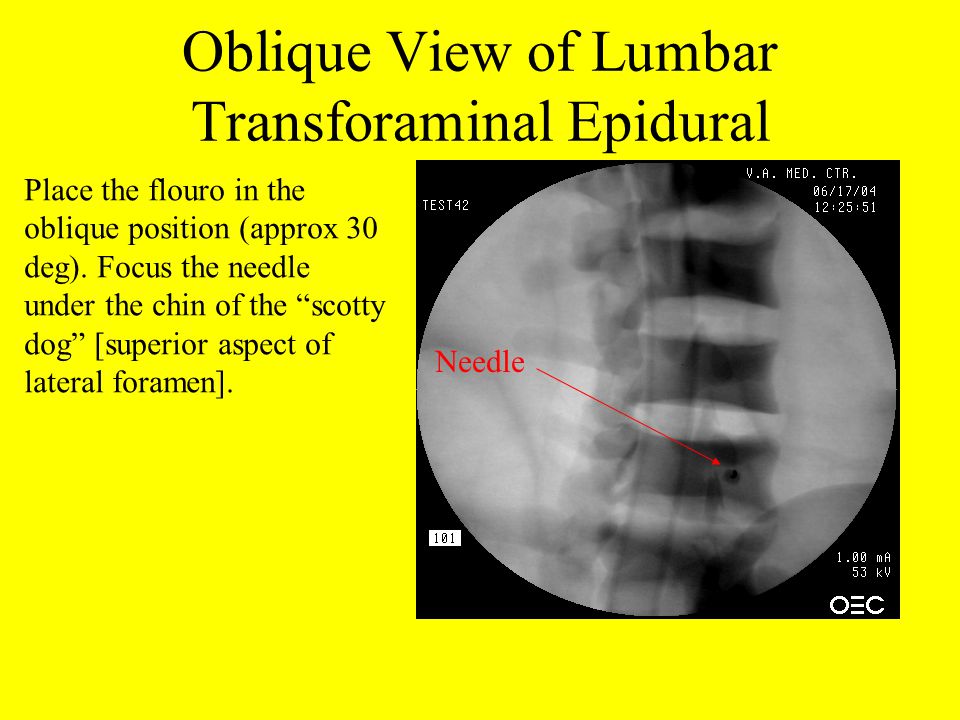 Recording by phone reception (4852) 78-81-96.
Recording by phone reception (4852) 78-81-96.
⚡⚡⚡ Memo for citizens on actions in case of asymptomatic or mild course of a new coronavirus infection and acute respiratory viral infection (Download full memo, download short memo)
⚡⚡⚡
Department of Health and Pharmacy of the Yaroslavl Region informs that within the framework of the implementation of the standard pilot project "Reproductive Health", approved by the Deputy Prime Minister of the Russian Federation Golikova T.A. dated November 25, 2021 No. 12752p-P12, regular meetings of citizens with experts on problematic issues of reproductive health continue.
Meetings are held every Saturday on the Reproductive Health channel, which is available at the links:
https://rutube.ru/channel/25385590/ . https://www.youtube.com/channel/UCpEP5EFRcqul2Ae6Y6RbGuA . .com/popsovet.
Questions to experts are accepted by e-mail: [email protected].
Schedule of the educational project "Reproductive Health" for August - December 2022
| Item No. | Date
| Time | Expert | Subject name |
| 1. | 13.08 | 10-00 | O.M. Drapkina A.B. Hecht | Obesity as an interdisciplinary problem. Prevention and correction of eating disorders. Proper nutrition and psychological aspects of women's health disorders. |
| 2. | 20.08 | 10-00 | O.I. Apolichin | Modern possibilities of drug and surgical treatment of disorders of male reproductive health. |
| 3. | 27.08 | 10-00 | M.F. Ippolitova | Pregnancy, childbirth and abortion in adolescents. Features of preventive examination of minors. Modern methods of contraception for adolescents and youth. |
| 4. | 3.09
| 9-00 | L.V. Adamyan
| Uterine fibroids: asymptomatic, symptomatic. family forms. Possible options for examination and treatment. |
| 5. | 10.09
| 10-00 | A. (R.G. Akzhigitov) | Consequences of COVID-19 in women (post-COVID syndrome). |
| 6. | 17.09 | 10-00 | A.D. Kaprin | Prostate cancer and stereotypes of male reproductive health. The possibilities of modern medicine and the right attitude to one's health. |
| 7. | 24.09 | 10-00 | E.E. Voronin L.Yu. Afonina | HIV, hepatitis and pregnancy. Prevention of HIV and hepatitis among young people. |
| 8. | 1.10 | 10-00 | I. | Benign dysplasia of the mammary glands. Precancerous diseases and risk factors for the development of malignant neoplasms of the breast. What you need to know: simple answers to women's questions. |
| 9. | 8.10 | 10-00 | N.V. Mokrysheva | "Letters to my son": what endocrine aspects of reproductive health do we need to tell adolescents |
| 10. | 15.10
| 10-00 | A.D. Kaprin M.V. Kiseleva | Reproductive health of cancer patients: opportunities to become parents are real. |
| 11. | 10/22 | 10-00 | A.
| Prevention of postpartum depression, including during periods of limited social interaction. Postcovid syndrome. |
| 12. | 29.10 | 10-00 | N.V. Mokrysheva
| Family planning for diabetes and thyroid disease: what to look for. |
| 13. | 5.11 | 10-00 | A.A. Steam horse | Oncology and pregnancy: preservation of reproductive function, preparation and management of pregnancy in oncological diseases. |
| 14. | 12.11 | 10-00 | A. E.V. Uvarova | Teenage pregnancy: abortion cannot be delivered. Where to put a punctuation mark or what to do in a difficult situation? |
| 15. | 11/19 | 10-00 | L.V. Adamyan | Modern aesthetic and plastic gynecology. The unity of beauty, sexuality and psychological comfort. |
| 16. | 11/26 | 10-00 | O.I. Apolichin | We are what we eat. Nutrition and male fertility. What and how to eat, drink to maintain fertility? |
| 17.
| 03.12 | 10-00 | N. O.I. Apolichin A.A. Olina | Medical genetic counseling for pregnancy planning. Assisted reproductive technologies, family assistance programs. Inefficiency of ART and ways to overcome it. |
| 18. | 10.12 | 10-00 | N.G. Mokrysheva
| Beyond genes: the role of parents in childhood obesity. The impact of obesity on the somatic, psychological and social well-being of children and adolescents. |
| 19. | 17.12 | 10-00 | Final event | New opportunities in medicine and reproduction ( genetics, immunology, cell technology, endocrinology, reproductive surgery, gynecology, urology, oncology ). |
Epidural analgesia in childbirth - GBUZ VO "REGIONAL PERINATAL CENTER"
The use of epidural analgesia during childbirth is becoming popular because of the convenience it provides. An epidural block reduces sensation in the lower parts of the body, but does not affect consciousness. The stage of labor at which an epidural is used may differ from patient to patient. If you need an epidural, your obstetrician and anesthesiologist will need to evaluate you and your baby, history of past anesthesias, and the progress of your labor. The most frequently asked questions when performing epidural analgesia in labor are:
When is epidural analgesia performed?
The time to start epidural analgesia is determined by the obstetrician and anesthesiologist, depending on the needs of the mother and baby during labor.
How is an epidural block performed?
Epidural lumbar anesthesia is performed in the lower back with the patient sitting or lying on her side.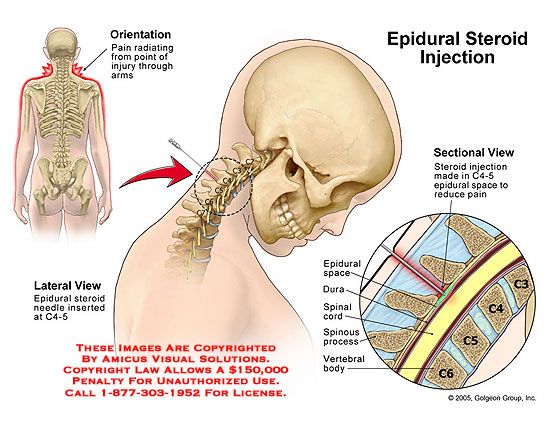 Anesthesia is performed below the level where the spinal cord ends.
Anesthesia is performed below the level where the spinal cord ends.
Before performing the block, the skin is treated with an antiseptic solution. The anesthesiologist then performs local anesthesia of the skin at the puncture site. After that, a special needle is inserted into the epidural space of the spine, slightly short of the spinal space. An epidural catheter, which is a thin, flexible tube, is inserted through the needle. Sometimes the catheter can touch a nerve, causing a shooting sensation in the leg.
Next, the needle is removed and the catheter is attached to the back. Subsequent injections will no longer require a second puncture, but are made through a catheter. An epidurally administered local anesthetic is thought to provide an epidural block by bathing the spinal nerves.
How soon does an epidural block occur and how long does it last?
The start of the block is gradual and slow. Pain relief usually develops 10-20 minutes after epidural administration and may be continued until the end of labor as additional doses of drugs can be administered through the epidural catheter.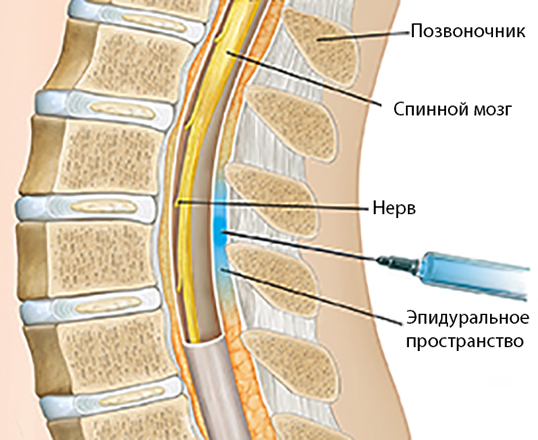 After delivery, the catheter is removed and after a few hours your sensations return to normal.
After delivery, the catheter is removed and after a few hours your sensations return to normal.
How does an epidural block feel?
With a significant reduction in pain, there may be a feeling of pressure during contractions and vaginal examination by an obstetrician. There may be transient numbness, weakness, and heaviness in the legs.
Do I need to stay in bed after an epidural?
Usually, during analgesia, you are warned not to get out of bed and lie on your back for more than 10 minutes during labor. However, it is believed that maintaining the vertical position of the body contributes to the favorable course of childbirth. There is a type of epidural analgesia that allows you to sit and walk. This type of analgesia is called "walking epidural" or ambulatory, mobile epidural.
Does epidural analgesia affect the child?
Studies show that epidural analgesia is safe for mother and child.
Will an epidural block slow down labor?
In some patients, the effects of epidural analgesia may reduce contractions for a short time.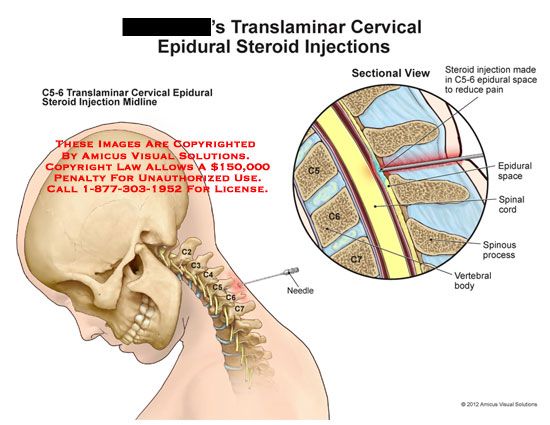 Most patients note that epidural analgesia helps them relax, while at the same time, uterine contractility improves.
Most patients note that epidural analgesia helps them relax, while at the same time, uterine contractility improves.
Will the ability to push remain?
Epidural analgesia will allow you to relax and maintain strength during the longest part of labor - when the cervix opens. In the pushing period of childbirth, if properly applied, it will not affect the attempts and even make them more pleasant.
What are the possible side effects of epidural analgesia?
Rarely, even with careful monitoring and precautions by the anesthetist, complications or side effects may occur. The most common complications are arterial hypotension and headache. More severe complications are a toxic reaction to local anesthetics, respiratory arrest, and neurological disorders. They are extremely rare.
Lowering blood pressure. You will receive intravenous fluids to prevent this complication. In addition, during delivery, you usually need to lie on your side, and after delivery, you need to stay in bed until the block wears off.
Headache occurs infrequently, in about 0.7-1.4% of cases. Maintaining the required position during the puncture helps to prevent its occurrence. When a headache occurs, simple measures are usually effective: bed rest, fluids, and pain medications. If pain persists, additional treatment may be required.
Chills is a common reaction during childbirth, but may also occur during anesthesia. Warming helps a lot.
Itching in most cases is mild, but if it becomes intolerable, it can be cured by the administration of drugs.
Difficulty breathing , very rarely anesthesia can affect the intercostal muscles and make breathing difficult. In this case, the condition of the woman in labor will facilitate the administration of oxygen.
Reaction to local anesthetics is rare but can be serious. During pregnancy, the veins passing through the epidural space dilate, and therefore there is a risk of intravascular injection. In order to avoid unwanted reactions, the anesthesiologist initially administers a test dose of the drug and asks the woman in labor to pay attention to the possibility of dizziness, metallic taste, palpitations or numbness.
In order to avoid unwanted reactions, the anesthesiologist initially administers a test dose of the drug and asks the woman in labor to pay attention to the possibility of dizziness, metallic taste, palpitations or numbness.
Insufficient anesthesia. Sometimes the effect of the anesthetic is "mosaic" or one-sided. The anesthetist may change your position in bed or pull up your epidural catheter. Rarely, repeat epidural anesthesia may be required.
The anesthesia anesthetist evaluates your condition and takes precautions during the procedure. You can discuss with him the possibilities of pain relief and your concerns about it.
When should epidurals not be used?
Contraindications to the use of epidural anesthesia are:
- bleeding disorders or the use of anticoagulants,
- generalized infection or infection at the puncture site,
- bleeding,
- patient refusal,
- severe neurological disease,
- heart diseases with fixed cardiac output.
 Assisted reproductive technologies for male infertility.
Assisted reproductive technologies for male infertility.  B. Hecht
B. Hecht  V. Soldiers
V. Soldiers 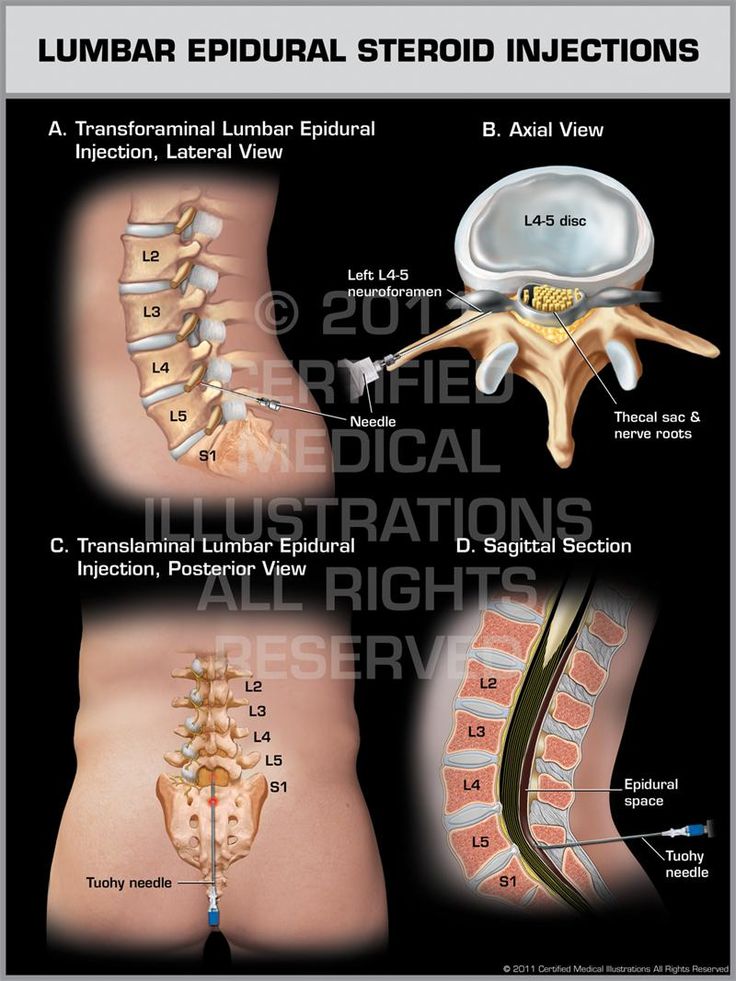 B. Hecht
B. Hecht 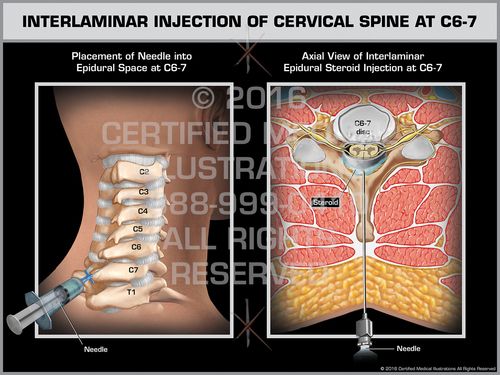 A. Olina
A. Olina 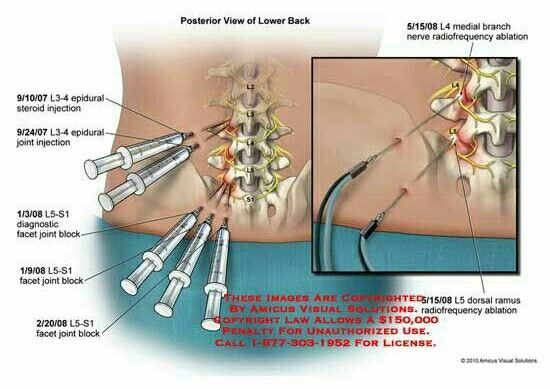 V. Dolgushin
V. Dolgushin