How long does a cold last in infants
Colds (0-12 Months)
Is this your child's symptom?
- Runny nose and sore throat caused by a virus
- You think your child has a cold. Reason: family members, friends or other children in child care have same symptoms.
- Also called an Upper Respiratory Infection (URI).
Symptoms of a Cold
- Runny or stuffy nose
- The nasal discharge starts clear but changes to gray. It can also be yellow or green.
- Most children have a fever at the start.
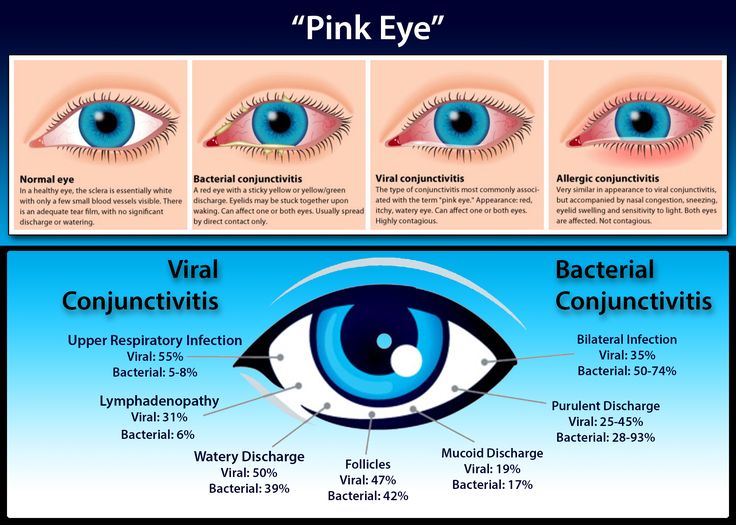
- At times, the child may also have a cough and hoarse voice. Sometimes, watery eyes and swollen lymph nodes in the neck also occur.
Cause of Colds
- Colds are caused by many respiratory viruses. Healthy children get about 6 colds in the first year.
- Influenza virus causes a bad cold with more fever and muscle aches.
- Colds are not serious. With a cold, about 5 to 10% of children develop a complication. Most often, this is an ear or sinus infection.
These are caused by a bacteria.
Trouble Breathing: How to Tell
Trouble breathing is a reason to see a doctor right away. Respiratory distress is the medical name for trouble breathing. Here are symptoms to worry about:
- Struggling for each breath or shortness of breath
- Tight breathing so that your child can barely cry
- Ribs are pulling in with each breath (called retractions)
- Breathing has become noisy (such as wheezes)
- Breathing is much faster than normal
- Lips or face turn a blue color
When to Call for Colds (0-12 Months)
Call 911 Now
- Severe trouble breathing (struggling for each breath, can barely cry)
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Trouble breathing, but not severe. Exception: gone after cleaning out the nose.
- Wheezing (purring or whistling sound) occurs
- Breathing is much faster than normal
- Trouble swallowing and new onset drooling
- High-risk child (such as with chronic lung disease)
- Weak immune system.
 Examples are sickle cell disease, HIV, cancer, organ transplant, taking oral steroids.
Examples are sickle cell disease, HIV, cancer, organ transplant, taking oral steroids. - Fever over 104° F (40° C)
- Fever in baby less than 12 weeks old. Caution: Do NOT give your baby any fever medicine before being seen.
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Contact Doctor Within 24 Hours
- Age less than 6 months old
- Earache or ear drainage
- Yellow or green pus from eyes
- Fever lasts more than 3 days
- Fever returns after gone for more than 24 hours
- You think your child needs to be seen, but the problem is not urgent
Contact Doctor During Office Hours
- Blocked nose wakes up from sleep
- Yellow scabs around the nasal openings. Use an antibiotic ointment.
- Nasal discharge lasts more than 2 weeks
- You have other questions or concerns
Self Care at Home
- Mild cold with no other problems
Seattle Children's Urgent Care Locations
If your child’s illness or injury is life-threatening, call 911.
- Bellevue
- Everett
- Federal Way
- Seattle
Care Advice for a Cold
- What You Should Know About Colds:
- It's normal for healthy children to get at least 6 colds a year. This is because there are so many viruses that cause colds. With each new cold, your child's body builds up immunity to that virus.
- Most parents know when their child has a cold. Sometimes, they have it too or other children in child care have it.
 Most often, you don't need to call or see your child's doctor. You do need to call your child's doctor if your child develops a complication. Examples are an earache or if the symptoms last too long.
Most often, you don't need to call or see your child's doctor. You do need to call your child's doctor if your child develops a complication. Examples are an earache or if the symptoms last too long. - The normal cold lasts about 2 weeks. There are no drugs to make it go away sooner.
- But, there are good ways to help many of the symptoms. With most colds, the starting symptom is a runny nose. This is followed in 3 or 4 days by a stuffy nose. The treatment for each symptom is different.
- Here is some care advice that should help.
- For a Runny Nose with Lots of Discharge: Suction the Nose
- The nasal mucus and discharge are washing germs out of the nose and sinuses.
- For younger children, gently suction the nose with a suction bulb.
- Put petroleum jelly on the skin under the nose. Wash the skin first with warm water. This will help to protect the nostrils from any redness.
- Nasal Saline to Open a Blocked Nose:
- Use saline (salt water) nose spray to loosen up the dried mucus.
 If you don't have saline, you can use a few drops of water. Use distilled water, bottled water or boiled tap water.
If you don't have saline, you can use a few drops of water. Use distilled water, bottled water or boiled tap water. - Step 1. Put 1 drop in each nostril.
- Step 2. Suction each nostril out while closing off the other nostril. Then, do the other side.
- Step 3. Repeat nose drops and suctioning until the discharge is clear.
- How Often. Do nasal saline rinses when your child can't breathe through the nose.
- Limit to no more than 4 times per day. Before breast or bottle feedings are a good time.
- Saline nose drops or spray can be bought in any drugstore. No prescription is needed.
- Reason for nose drops: Suction alone can't remove dried or sticky mucus. Also, babies can't nurse or drink from a bottle unless the nose is open.
- Other option: use a warm shower to loosen mucus. Breathe in the moist air, then suction each nostril.
- For young children, can also use a wet cotton swab to remove sticky mucus.
- Use saline (salt water) nose spray to loosen up the dried mucus.
- Fluids - Offer More:
- Try to get your child to drink extra formula or breastmilk.
- Goal: Keep your child well hydrated.
- It also will thin out the mucus discharge from the nose.
- It also loosens up any phlegm in the lungs. Then it's easier to cough up.
- Try to get your child to drink extra formula or breastmilk.
- Humidifier:
- If the air in your home is dry, use a humidifier.
- Reason: Dry air makes nasal mucus thicker.
- Drugstore Medicines for Colds:
- Cold Medicines. Don't give any drugstore cold or cough medicines to young children. They are not approved by the FDA under 6 years. Reasons: not safe and can cause serious side effects. Also, they are not helpful. They can't remove dried mucus from the nose. Nasal saline works best.
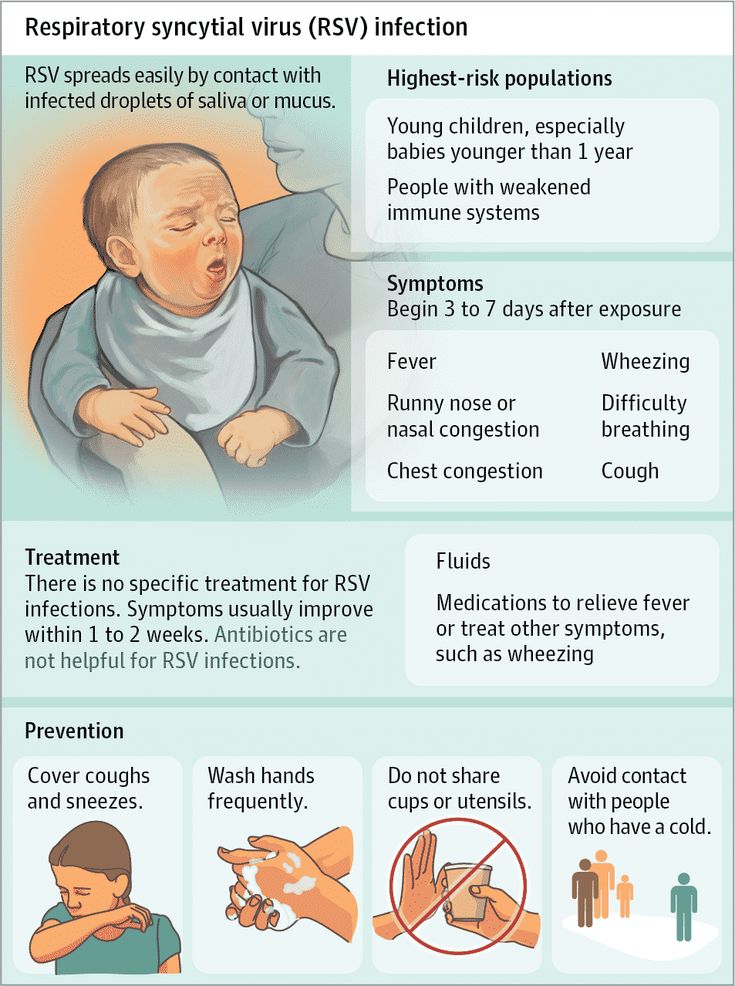
- No Antibiotics. Antibiotics are not helpful for colds. Antibiotics may be used if your child gets an ear or sinus infection.
- Other Symptoms of Colds - Treatment:
- Pain or Fever. Use acetaminophen (such as Tylenol) to treat muscle aches, sore throat or headaches.
 Another choice is an ibuprofen product (such as Advil). Caution: avoid ibuprofen until 6 months or older. You can also use these medicines for fever above 102° F (39° C).
Another choice is an ibuprofen product (such as Advil). Caution: avoid ibuprofen until 6 months or older. You can also use these medicines for fever above 102° F (39° C). - Red Eyes. Rinse eyelids often with wet cotton balls.
- Pain or Fever. Use acetaminophen (such as Tylenol) to treat muscle aches, sore throat or headaches.
- Return to Child Care:
- Your child can go back to child care after the fever is gone.
- For practical purposes, the spread of colds can't be prevented.
- What to Expect:
- Fever can last 2-3 days
- Nasal drainage can last 7-14 days
- Cough can last 2-3 weeks
- Call Your Doctor If:
- Trouble breathing occurs
- Earache occurs
- Fever lasts more than 3 days or goes above 104° F (40° C)
- Any fever if under 12 weeks old
- Nasal discharge lasts more than 14 days
- Cough lasts more than 3 weeks
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.

Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Last Reviewed: 11/30/2022
Last Revised: 09/18/2022
Copyright 2000-2022 Schmitt Pediatric Guidelines LLC.
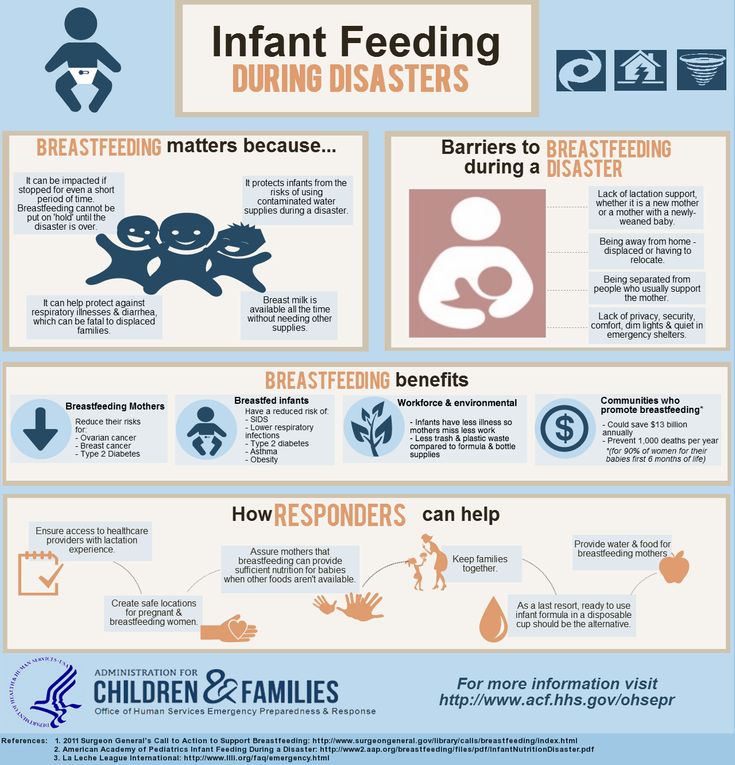
Infant colds: What's normal and what's not
Dr. Todd Twogood, a pediatrician at the Sanford Medical Center in Bismarck, North Dakota, talks about infant colds and what parents can do to help.
What causes the common cold?
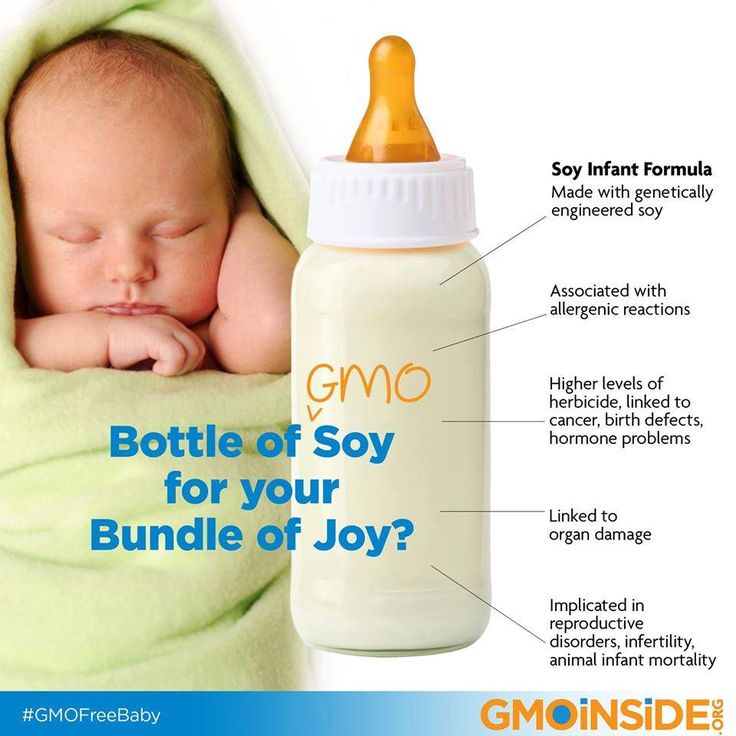
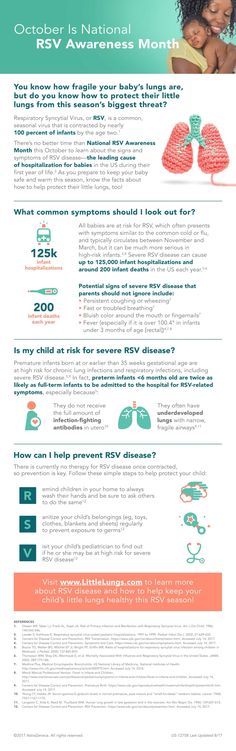
The general cause of a common cold is a virus. A few common viruses are rhinovirus, enterovirus, respiratory syncytial virus (RSV). A lot of parents have misconceptions of RSV and believe that if their child gets it they’re going to end up in the hospital, quite sick or even develop asthma. But, that’s not quite true. Since 96 percent of all children develop RSV at least once before they’re 2, it can be considered a common cold as well.
Related: Winter’s worst bugs — Protect your child from RSV
What are the symptoms of a cold in an infant?
Symptoms of a cold in an infant generally start with a low grade fever and nasal congestion. Infants get all plugged up inside and then two to three days later generally start having a lot of post-nasal drip, increasing a cough and causing a runny nose. If your child has a green or yellow runny nose in the first three to four days of a cold, that’s normal and not considered a sinus infection — it’s just that the mucus has been setting in the nose for so long. That generally fades away within seven to 10 days and the fever is usually gone in two to three days.
Infants get all plugged up inside and then two to three days later generally start having a lot of post-nasal drip, increasing a cough and causing a runny nose. If your child has a green or yellow runny nose in the first three to four days of a cold, that’s normal and not considered a sinus infection — it’s just that the mucus has been setting in the nose for so long. That generally fades away within seven to 10 days and the fever is usually gone in two to three days.
Is there anything parents can do to prevent a cold?
Avoid close contact with your child. More specifically, no sharing cups, spoons or straws. Your child should also have their own towel when they have a cold. You should avoid close kissing as well. You can maybe kiss them on the forehead, but not too close.
What do you know about the common cold? Take our quiz.
What can a parent do at home to help a child with a cold?
Humidified air is one of the best things you can do. It will help lubricate the nasal sinuses and prevent cough.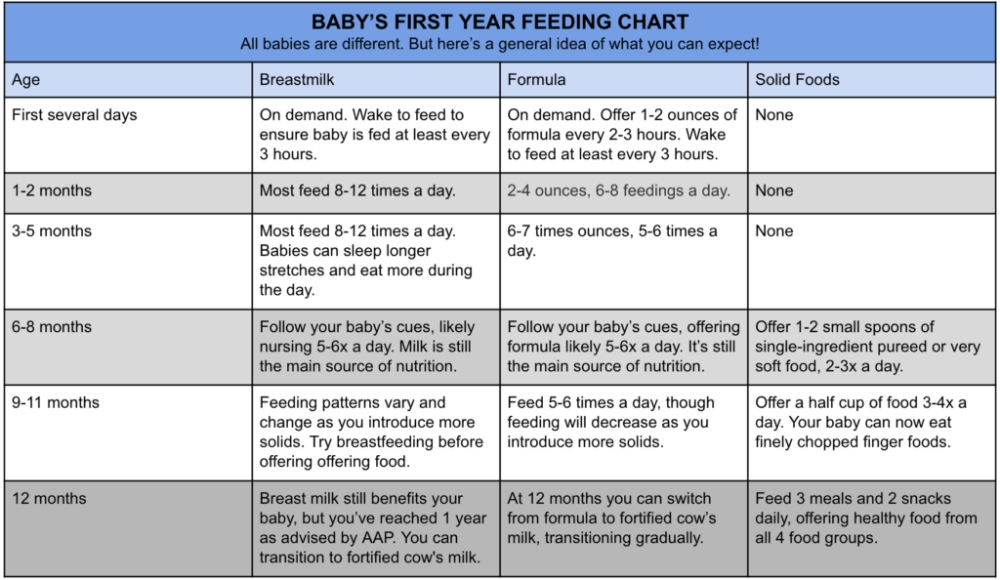 If your child’s uncomfortable, use of Tylenol and Ibuprofen would be appropriate. Use upright positioning for small infants and children, but only while they’re awake, and flat positioning while they sleep. Nasal saline can also help congestion.
If your child’s uncomfortable, use of Tylenol and Ibuprofen would be appropriate. Use upright positioning for small infants and children, but only while they’re awake, and flat positioning while they sleep. Nasal saline can also help congestion.
Is there anything that a parent should NOT do?
The first thing a parent shouldn’t do is worry. Most colds last seven to 10 days. As long as your child is comfortable and does not have prolonged fever or respiratory difficulties, hang in there and things will get better. Just provide supportive care to your child. Visit a health care professional if you have further concerns.
When does a child need to see a physician?
During a cold, your baby or infant may need to see a physician or health care professional if their symptoms are prolonged. If they extend past seven to 10 days, you may want to call or bring your child in. If there are symptoms such as irritability, prolonged fever or respiratory difficulty, make sure to see a physician or health care professional.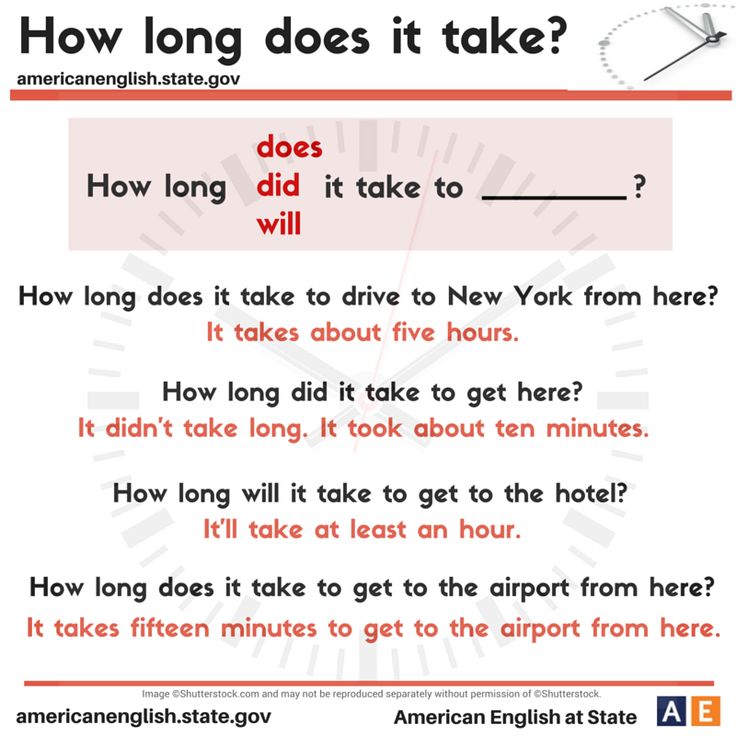
How long will it take for the child to get better?
With a cold, your child should get better within seven to 10 days. If you have more serious concerns be sure to call or visit your provider. Children with special needs or chronic health care conditions may need to be seen earlier or with special consideration. But, all of our children deserve that special love and attention.
More stories
- Choosing a doctor for your child
- Ear infections in children: What to do and what to know
- How to manage your child’s food allergies
- Children’s specialty care: A team approach
Recommendations from Academy of Pediatrics
The American Academy of Pediatrics strongly advises not using over-the-counter (OTC) cold and cough medicines for children younger than age 4. From age 4 to 6, these medicines should only be used if your child’s health care provider tells you to. Several studies show that cold and cough products don’t work in young children and they can have possibly serious side effects.
Many products also have a mix of ingredients meant to treat more than a single symptom, possibly including symptoms your child does not have. This also increases the risk that your child may overdose on an ingredient if you are giving your child more than one medicine.
Ask your child’s health care provider what he or she advises for different symptoms. Do this before your child gets a cold.
Here are some common cold symptoms and ingredients to look for on labels if your child’s provider advises medicine.
Fever and pain
Typical colds don’t cause more than a slight fever in kids. It’s OK to let a slight fever run its course if your child is taking liquids and acting well. In fact, fever may help your child’s natural immune system fight off the infection sooner. Only two OTC fever or pain medicines are available for children: acetaminophen and ibuprofen. Others are available by prescription. Both help aches and ease fevers. Some multi-ingredient cold medicines contain one or the other of these ingredients.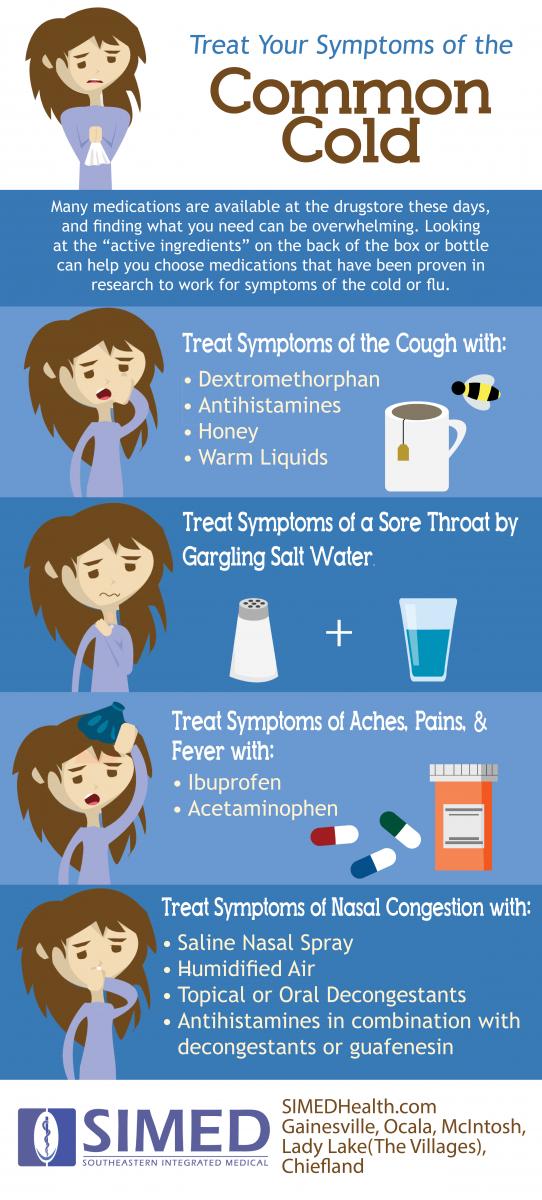 So read labels carefully so you won’t give extra medicine that may not be needed.
So read labels carefully so you won’t give extra medicine that may not be needed.
Never give aspirin to infants, children, or teens because of the risk for Reye syndrome. This is a rare but possibly fatal disease that can cause liver and brain damage.
Call your child’s health care provider right away if your child is younger than 3 months old and has a fever over 100.4°F (38°C).
Stuffy nose and sneezing
If your child has a runny nose, use a bulb syringe to gently suction out the mucus. Or have your child blow his or her nose. Antihistamines only work if the runny nose is caused by allergies. Antihistamines don’t work well for the common cold.
For a blocked nose, saltwater (saline) spray or drops may help. They dilute the mucus. This makes it easier for the child to blow it out or for you to suction it out. There are no medicines that can remove mucus from the nose. You can buy saline drops and spray at the pharmacy. Or you can make your own by mixing ½ teaspoon of salt in eight ounces of warm tap water. For babies, use the drops before feeding. Older babies and children may use the drops or spray whenever their nose is blocked. Don’t give your child OTC medicated nasal sprays without first talking with your health care provider.
For babies, use the drops before feeding. Older babies and children may use the drops or spray whenever their nose is blocked. Don’t give your child OTC medicated nasal sprays without first talking with your health care provider.
Coughing
For babies younger than one year, it is enough to keep them well hydrated and comfortable. Ask your child’s health care provider if your child should have extra water or warm fluids. For children older than a year, honey may be more helpful than any OTC cough medicine and is much safer. Give your child ½ to one teaspoon of honey as needed. Don’t give honey to babies younger than a year. They are at risk of getting a disease called infantile botulism.
Children in daycare or school often spread colds to each other. Keep your child at home if they have a cold or if many children in the class have colds.
Your child can help prevent colds by washing their hands often, by not touching their nose or eyes, and by staying away from people with colds or upper respiratory infections. Alcohol-based hand gels can help prevent spreading a cold or other viral infection.
Alcohol-based hand gels can help prevent spreading a cold or other viral infection.
Feeling better without medicine
There isn’t enough scientific proof to back claims about vitamin C, echinacea and zinc for cold relief. But the following suggestions may help your child feel more comfortable:
- Liquids. Give your child plenty of water or other liquids to drink.
- Cough drops. Lemon and peppermint drops can help a scratchy throat. Cough drops should only be given to older children who can handle hard candies without a risk of choking.
- Bed rest. If your child seems tired, let them relax.
- Steam. Steam treatment can be helpful. Use cool mist humidifiers at night. Warm humidifiers are not advised because they can burn a child. Mold can grow in any humidifier. So clean the equipment well between uses. Running a warm shower in the same room as your child may also ease symptoms if you don’t have a humidifier.

…
Posted In Children's, Health Information, Specialty Care
Physiological runny nose in a newborn — Medical Center "Healer"
When it comes to a runny nose in a baby, one must understand that this is primarily a physiological process. A newborn baby, as soon as it is born, begins to breathe on its own. In the womb, babies breathe in a completely different way, they have a nose, lungs did not develop, but they received oxygen in a completely different way, through the umbilical cord. And now, having been born into the world, the baby begins to get used to the environment on its own.
Features
Normally, a baby's runny nose lasts 10-12 weeks. During this period of adaptation, the child naturally develops more mucus in the nose. There is nothing pathological in this. Such transparent mucus in the nose absolutely does not prevent the baby from living an independent life, does not prevent him from eating on his own.
We are very fond of young mothers because of their inexperience to resort to various aspiratory devices for pumping mucus out of their child's nose. They think they help him in some way. The child already has narrow, swollen nasal passages, and we still climb there with an aspirator and try to get the mucus out of there. Thus, we only injure the mucous surface.
If your baby has a runny nose because he is too cold, you can simply warm him up. And this runny nose will soon pass. Physiological rhinitis does not go away so quickly. And so the child must be helped. Usually we like to have the child lie down all the time. We walk with him in a stroller, he lies at home. And how is this mucus in this case supposed to move up and down? Turn the baby over more often, do not forget about airing the room, about walking in the fresh air.
Do not confuse with pathology
Do not confuse physiological rhinitis with allergic or inflammatory rhinitis. Experienced pediatric ENT doctors in Makhachkala know that a newborn does not usually suffer from allergic rhinitis.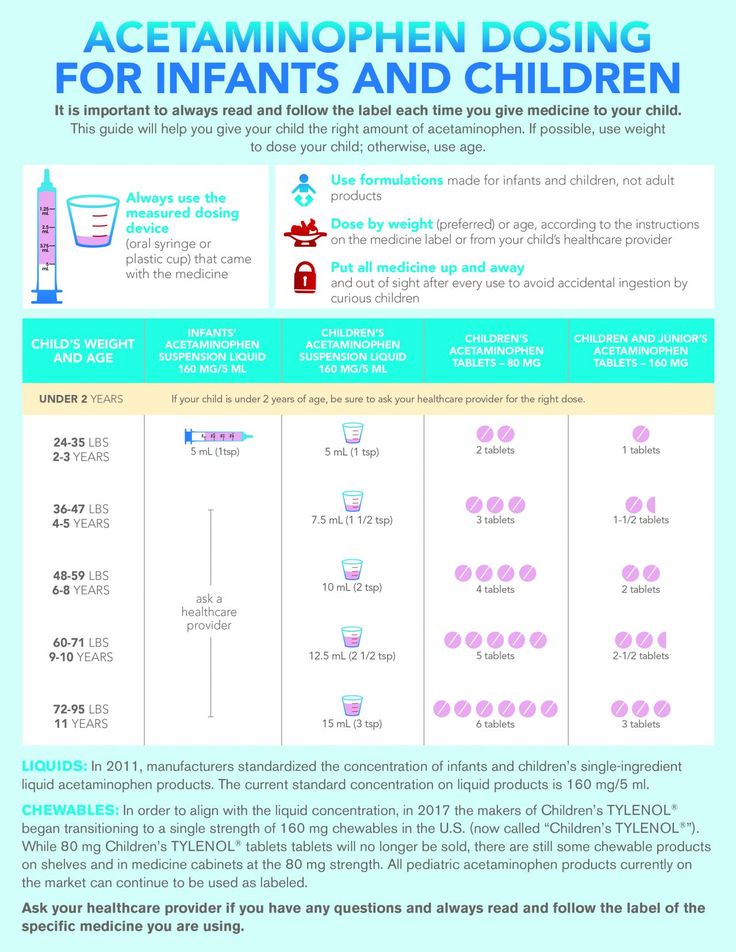 Only if an allergen somehow got into the body, or it happens that the mixture did not fit. But in this case, as soon as we remove the allergic process, the runny nose stops.
Only if an allergen somehow got into the body, or it happens that the mixture did not fit. But in this case, as soon as we remove the allergic process, the runny nose stops.
In the inflammatory nature of the discharge from the nose is not transparent, but yellowish, greenish with an admixture of blood. Of course, then you already need to run to a medical clinic to a specialist. Because the process can become chronic. Do not get used to vasoconstrictor drops. After all, they do not cure a runny nose, but only relieve a symptom, and besides, it is very easy to get used to them. Thus, you will not even notice how your child's normal physiological runny nose has become chronic.
Preventive measures
The heating season is ahead of us. We will definitely face the fact that the heaters will turn on in the rooms, and this will lead to overdrying of the air in the living quarters. Specialists in ENT diseases in children are advised to hang in the room where the baby sleeps, next to the crib, hang a hygrometer to determine humidity and a thermometer that will show the temperature in the room.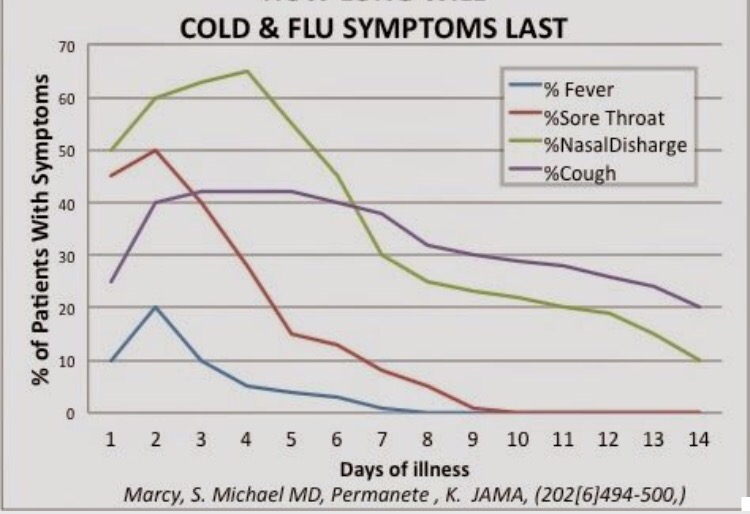 The temperature for newborns in the room should be within 18-20 degrees, and humidity 60-70%.
The temperature for newborns in the room should be within 18-20 degrees, and humidity 60-70%.
"If parents see that the child has accumulated mucus in the nasal passages, it is recommended to put 1 drop into each nostril of a solution with sea salt. It can be Aqualor or Aquamaris. It is also very useful to put small children on their tummy. put on his tummy. Let him buck and move. Yes, it is uncomfortable for him, it is not comfortable. It is also desirable to put your hand, let him push off. Thus, he physiologically begins to breathe actively, and with this air, the accumulated mucus will independently and easily come out of nasal passages".
Other items
Gadzhikuliev Nuri Babayevich
circumcision, urologist, surgeon
Dropsy of the testicles in children: what is it, how is it manifested and how is it treated?
Dropsy of the testicular membranes (hydrocele) is a benign process in which serous fluid accumulates in the scrotum cavity…
How to recognize eye diseases in a child?
You have a joyful event in your family – a child is born! But you must remember that there are certain rules for inspecting this new…
November 17, 2022
Rules for preparing for analyzes
For the most accurate diagnosis of diseases, the most modern laboratory equipment is not enough.
November 1, 2022
Inkova Aishat Inkavovna
neuro-ophthalmologist, ophthalmologist
Prevention of visual impairment in children
Thanks to vision, a person receives up to 90% of information about the world around him. That is why the importance of good health should not be underestimated…
October 31, 2022
Runny nose in a baby causes and treatment
Snot in a baby appears very often, but not all parents understand how dangerous or harmless it is and what to do if their baby has a runny nose .
A runny nose in infants is not always due to the addition and development of the disease, it can also have completely physiological causes associated with the age and development of the child's body during this tender period.
As with any other pathological condition, there may be causes of a runny nose in infants.
- physiological;
- pathological.
Physiological causes
The mucous membrane of the nasal cavities immediately after birth, although it is formed correctly, but cannot fully perform its functions, participate in the regulatory mechanisms of the body. In some children, this leads to excessive dryness of the nasal cavity with insufficient secretion production, while in others to its abundant secretion - a newborn runny nose.
Mucosal function returns to normal only after reaching 10 months of age. It's not worth worrying. This is not dangerous and should go away on its own over time, but the ENT doctors of Dr. Korenchenko's clinic advise you to go to the pediatrician. so as not to miss the beginning of the development of the pathological process behind imaginary well-being.
Pathological causes
The most common cause is colds, which are especially common in newborns. Own immunity has not yet been formed, and maternal immunity is not always effective enough and, moreover, is weakening every day. Any infection that for an adult or older child will go completely unnoticed in a newborn can cause acute respiratory infections and a runny nose.
Own immunity has not yet been formed, and maternal immunity is not always effective enough and, moreover, is weakening every day. Any infection that for an adult or older child will go completely unnoticed in a newborn can cause acute respiratory infections and a runny nose.
The first symptoms of an acute infectious disease are fever and a runny nose. Later, cough, shortness of breath, shortness of breath join. Sleep and appetite disorders. The child becomes restless, cries, refuses to eat. Abundant snot in infants causes irritation of the skin around the nose, on the upper lip, in the nasolabial folds. At the first appearance of such symptoms, we strongly advise you to contact your pediatrician immediately.
Another common cause of a runny nose in a newborn is an allergic reaction to an external irritant. With age and with the formation of one's own full-fledged immune defense, this disease can go away on its own, but in infancy, intolerance to any substances is more common than in adults. Irritants can be ordinary household dust, pet or bird hair, extraneous odors, creams and preparations that treat the baby's skin, even the smell of the mother and breast milk can provoke snot in the baby.
Irritants can be ordinary household dust, pet or bird hair, extraneous odors, creams and preparations that treat the baby's skin, even the smell of the mother and breast milk can provoke snot in the baby.
Relatively infrequently, the cause of snot in infants is vasomotor rhinitis, a disease associated with impaired blood supply to the nasal mucosa. The correct diagnosis can only be established by a doctor.
Treatment
To free the nasal passages, use special micro-suckers or a small enema, but only for suctioning the secretions, not for washing. The pear cannula or enema should be inserted with caution and very shallowly, only 0.5-0.8 cm deep into the nasal passage.
Any folk or sorcerer's remedies, potions or manipulations can be performed only after agreement with the doctor. Uncontrolled self-medication can harm the baby. Too tender age for a child to take such risks!
Medicines should only be used as prescribed by a doctor, strictly following his instructions and recommendations. Only a doctor can accurately determine the condition of the child and correctly prescribe the treatment of a runny nose in infants with medications.
Only a doctor can accurately determine the condition of the child and correctly prescribe the treatment of a runny nose in infants with medications.
Most commonly prescribed drugs
- Aqua Maris;
- Aqualor Baby;
- Nazol Baby;
- Otrivin Baby;
- Doctor Mom;
- Saline;
- Nazivin for children.
Please note that all listed preparations have the prefix "baby" or "children's". It is impossible to use adult medicines to treat a runny nose in infants.
Physiological runny nose in infants does not need treatment, but only a doctor can determine the absence of pathology.
DO NOT!
- use an enema to wash the sinuses with fluid injection.
 A pear and an enema can only be used to suck snot from a baby, and then with caution;
A pear and an enema can only be used to suck snot from a baby, and then with caution; - independently prescribe antibacterial and antiviral drugs;
- use vasoconstrictor nasal drops and sprays without medical advice.
Remember! At this age, the baby's health is very fragile. Having taken up the treatment of a runny nose in a baby on your own or according to the recipes of familiar grandmothers, instead of improving your health, you can do much harm to him.
A runny nose in a baby should not be left untreated. With the pathological nature of the process, the disease will progress and can cause the development of serious and life-threatening complications for the infant.
Prevention of the common cold in infants
See also
Treatment of ENT diseases
Snot in a child
Chronic rhinitis
Treatment of rhinitis
Maintain an optimal microclimate in the room where the child is.