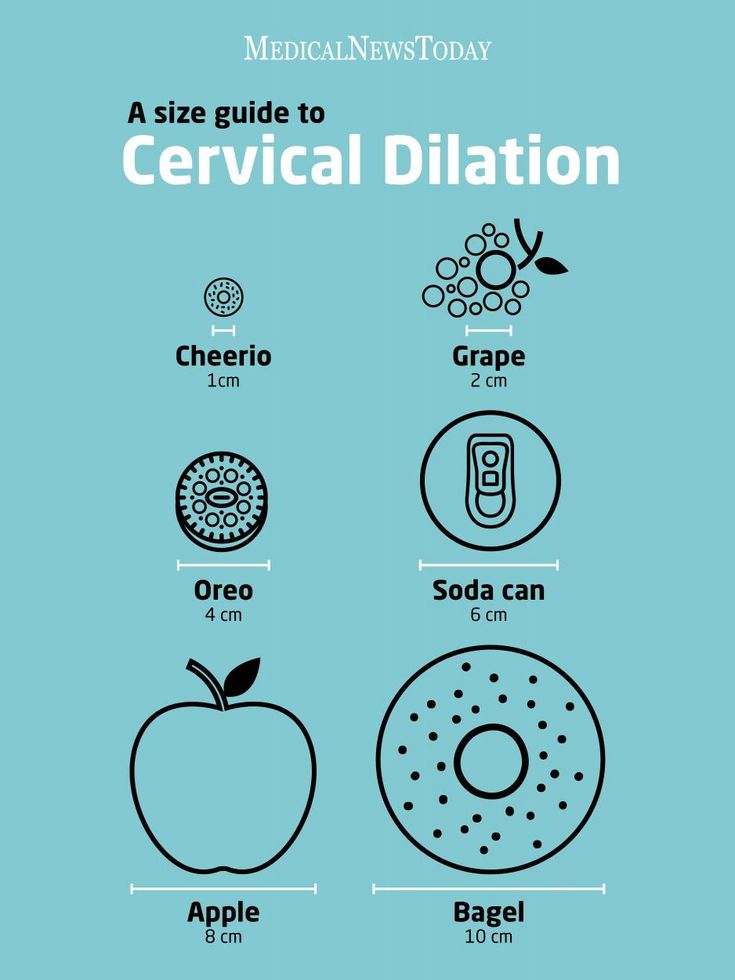
Dilation cervix diagram
Cervix Dilation Chart: Stages of Labor
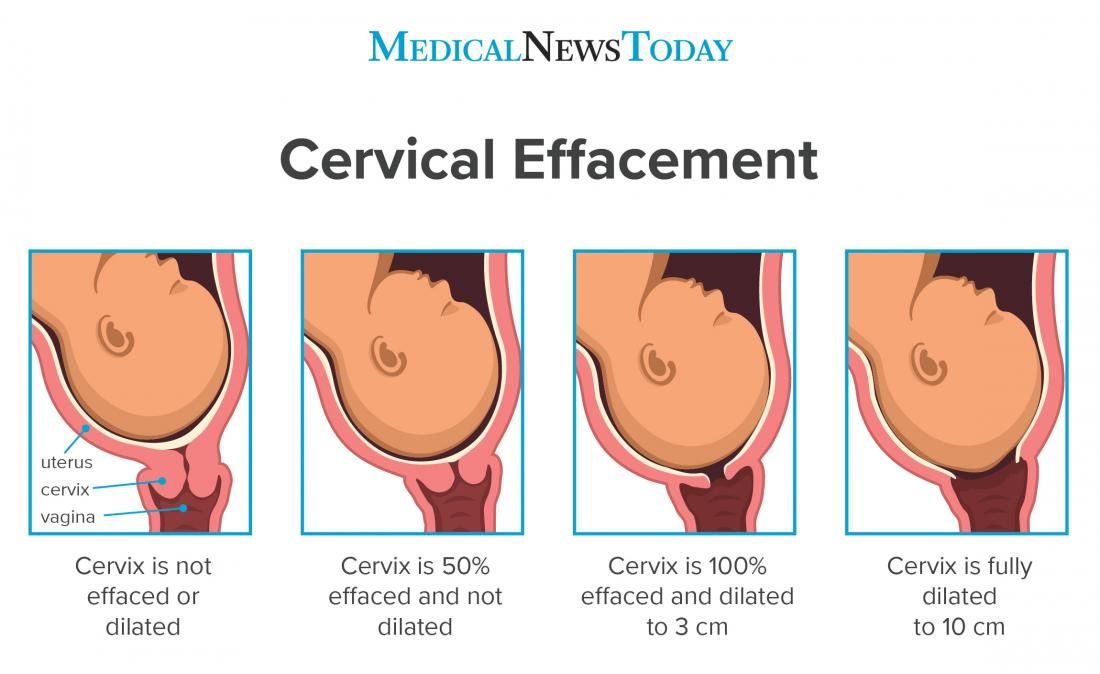
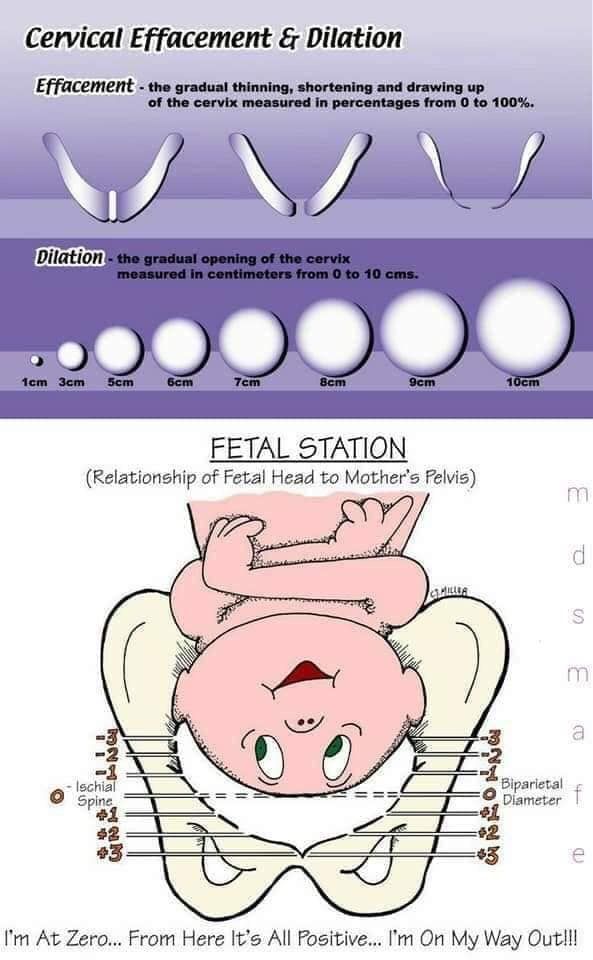
The cervix, which is the lowest portion of the uterus, opens when a woman has a baby, through a process called cervical dilation. The process of the cervix opening (dilating) is one way that healthcare staff track how a woman’s labor is progressing.
During labor, the cervix opens to accommodate the passage of baby’s head into the vagina, which is around 10 centimeters (cm) dilated for most term babies.
If your cervix is dilated with regular, painful contractions, you’re in active labor and getting closer to delivering your baby.
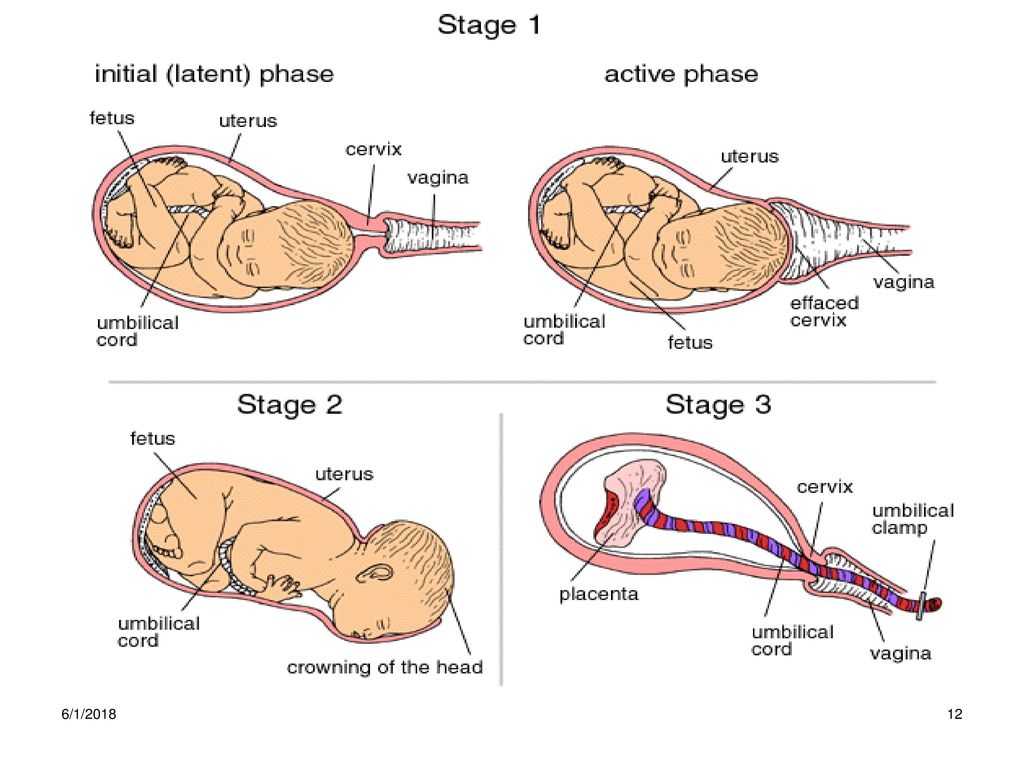
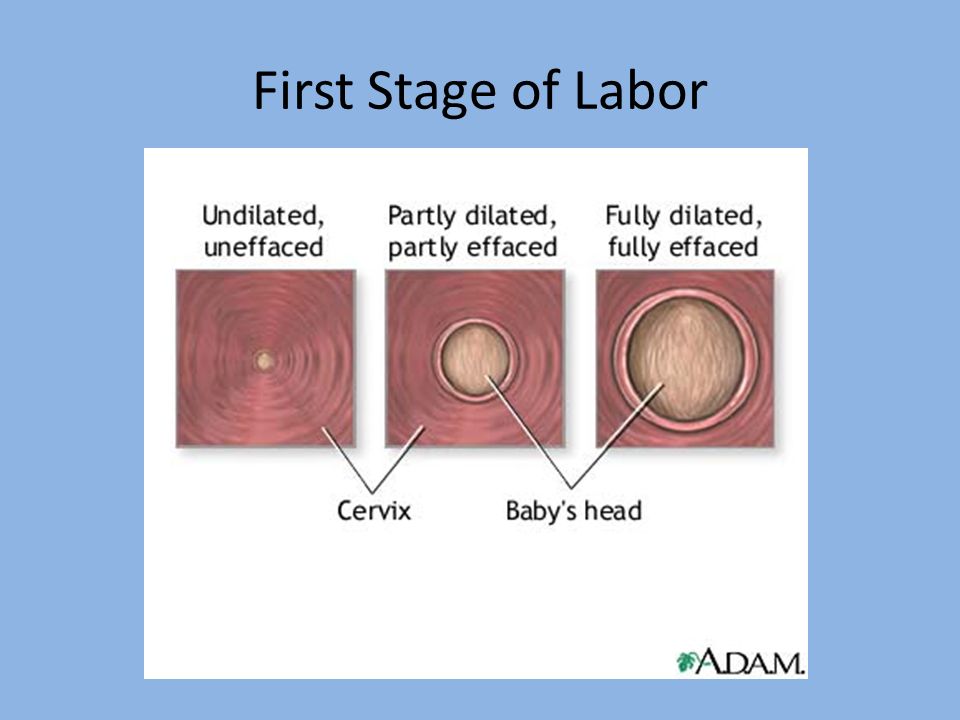
The first stage of labor is divided into two parts: the latent and active phases.
Latent phase of laborThe latent phase of labor is the first stage of labor. It can be thought of more as the “waiting game” stage of labor. For first-time moms, it can take a while to move through the latent phase of labor.
In this stage, contractions aren’t yet strong or regular. The cervix is essentially “warming up,” softening, and shortening as it prepares for the main event.
You might consider picturing the uterus as a balloon. Think of the cervix as the neck and opening of the balloon. As you fill that balloon up, the neck of the balloon draws up with the pressure of the air behind it, similar to the cervix.
The cervix is simply the bottom opening of the uterus drawing up and opening wider to make room for the baby.
Active stage of laborA woman is considered to be in the active stage of labor once the cervix dilates to around 5 to 6 cm and contractions begin to get longer, stronger, and closer together.
The active stage of labor is characterized more by the rate of regular cervical dilation per hour. Your doctor will expect to see your cervix opening at a more regular rate during this stage.
How long does stage 1 of labor last?There’s no scientific hard and fast rule for how long the latent and active phases last in women.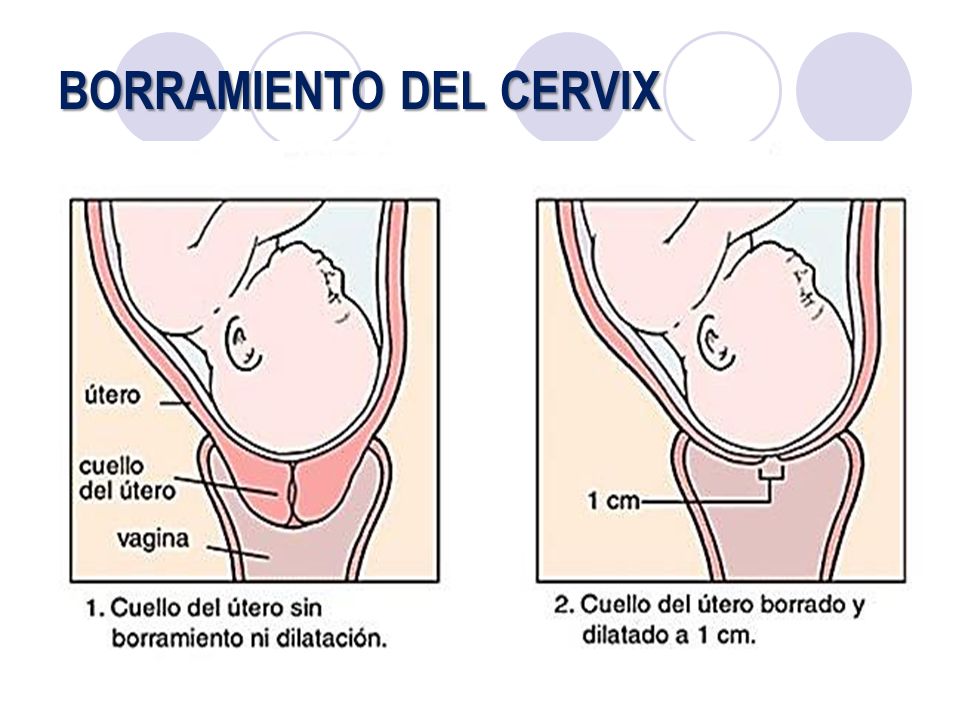 The active stage of labor can range from a woman dilating anywhere from 0.5 cm per hour up to 0.7 cm per hour.
The active stage of labor can range from a woman dilating anywhere from 0.5 cm per hour up to 0.7 cm per hour.
How fast your cervix dilates will also depend on if it’s your first baby or not. Mothers who have delivered a baby before tend to move more quickly through labor.
Some women will simply progress more quickly than others. Some women may “stall” at a certain stage, and then dilate very quickly.
In general, once the active stage of labor kicks in, it’s a safe bet to expect a steady cervical dilation every hour. Many women don’t start really dilating more regularly until closer to around 6 cm.
The first stage of labor ends when a woman’s cervix is fully dilated to 10 cm and fully effaced (thinned out).
The second stage of labor begins when a woman’s cervix is fully dilated to 10 centimeters. Even though a woman is fully dilated, it doesn’t mean that the baby is necessarily going to be delivered immediately.
A woman may reach full cervical dilation, but the baby may still need time to move down the birth canal fully to be ready for birth. Once the baby is in prime position, it’s time to push. The second stage ends after the baby is delivered.
Once the baby is in prime position, it’s time to push. The second stage ends after the baby is delivered.
In this stage, there’s again a wide range for how long it can take for the baby to come out. It can last anywhere from minutes to hours. Women may deliver with only a few hard pushes, or push for an hour or more.
Pushing occurs only with contractions, and the mother is encouraged to rest between them. At this point, the ideal frequency of contractions will be about 2 to 3 minutes apart, lasting 60 to 90 seconds.
In general, pushing takes longer for first-time pregnant people and for women who have had epidurals. Epidurals can reduce the woman’s urge to push and interfere with her ability to push. How long a woman is allowed to push depends on:
- the hospital’s policy
- the doctor’s discretion
- the health of the mom
- the health of the baby
The mother should be encouraged to change positions, squat with support, and rest between contractions.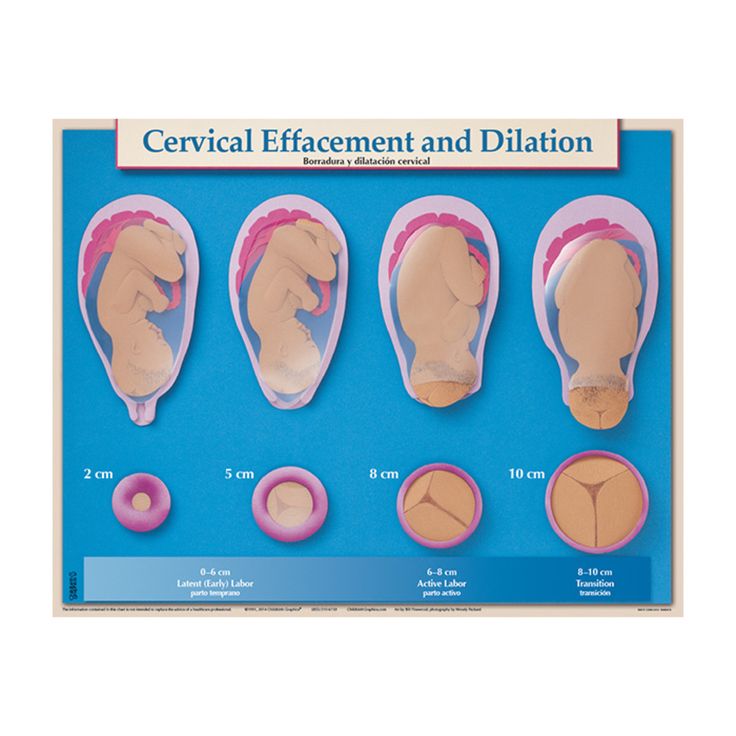 Forceps, vacuum, or cesarean delivery is considered if the baby isn’t progressing or the mother is becoming exhausted.
Forceps, vacuum, or cesarean delivery is considered if the baby isn’t progressing or the mother is becoming exhausted.
Again, every woman and baby is different. There’s no universally accepted “cut-off time” for pushing.
The second stage ends with the birth of the baby.
The third stage of labor is perhaps the most forgotten phase. Even though the “main event” of birth has occurred with the birth of the baby, a woman’s body still has important work to do. In this stage, she’s delivering the placenta.
A woman’s body actually grows an entirely new and separate organ with the placenta. Once the baby is born, the placenta no longer has a function, so her body must expel it.
The placenta is delivered the same way as the baby, through contractions. They may not feel as strong as the contractions that are needed to expel the baby. The doctor directs the mother to push and the delivery of the placenta is typically over with one push.
How long does stage 3 of labor last?The third stage of labor can last anywhere from 5 to 30 minutes. Putting the baby on the breast for breastfeeding will hasten this process.
Putting the baby on the breast for breastfeeding will hasten this process.
Postpartum recovery
Once the baby is born and the placenta has been delivered, the uterus contracts and the body recovers. This is often referred to as the fourth stage of labor.
After the hard work of moving through the stages of labor is finished, a woman’s body will need time to return to its nonpregnant state. On average, it takes about 6 weeks for the uterus to return to its nonpregnant size and for the cervix to return to its prepregnancy state.
Physiology, Cervical Dilation - StatPearls
Osarieme Evbuomwan; Yuvraj S. Chowdhury.
Author Information
Last Update: May 20, 2022.
Introduction
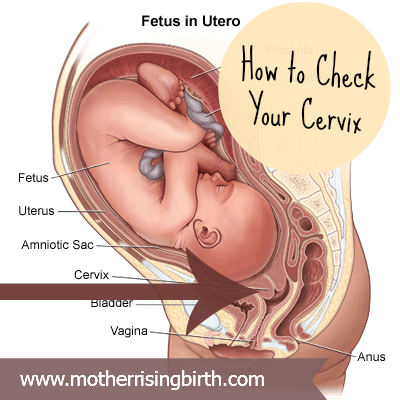
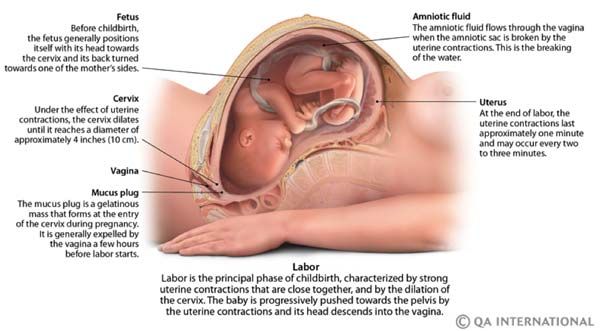
The cervix is a fibromuscular organ linking the uterus to the vagina. The upper two-thirds of the uterus is termed the corpus, or body of the uterus. The lower one-third of the uterus comprises the cervix, with the upper boundary of the cervix being the internal os.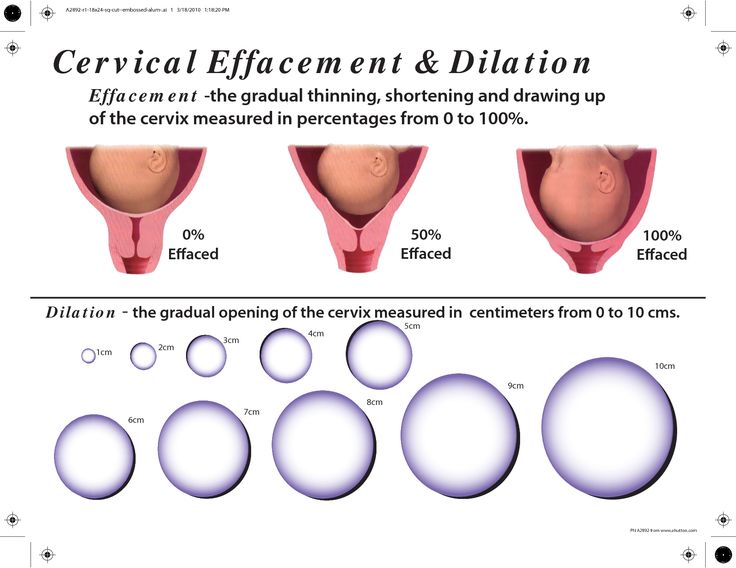 The cervix lies anterior to the bowel and posterior to the bladder. Anatomically, internal to external: uterine cavity, internal os, endocervix (endocervical canal), external os, ectocervix, vagina. In pre-menopausal women, the cervix faces downward and protrudes into the vagina. The cervix serves as a passageway between the endometrial cavity and the vagina and is physiologically important in reproduction and childbirth.[1] Towards the end of pregnancy, as the time of labor approaches, the cervix must undergo cervical effacement (thinning) and dilation (widening) to facilitate and accommodate the delivery of the fetus.[2]
The cervix lies anterior to the bowel and posterior to the bladder. Anatomically, internal to external: uterine cavity, internal os, endocervix (endocervical canal), external os, ectocervix, vagina. In pre-menopausal women, the cervix faces downward and protrudes into the vagina. The cervix serves as a passageway between the endometrial cavity and the vagina and is physiologically important in reproduction and childbirth.[1] Towards the end of pregnancy, as the time of labor approaches, the cervix must undergo cervical effacement (thinning) and dilation (widening) to facilitate and accommodate the delivery of the fetus.[2]
Issues of Concern
Complete dilation of the cervix is achieved when the cervix dilates to 10 cm. How rapidly a female will progress to full dilation is dependent on several factors, including her parity, medical history, pelvic anatomy, the size of the fetus, and the position of the fetus at the time of labor.[3] Multigravida women progress to full dilation more quickly than primigravida.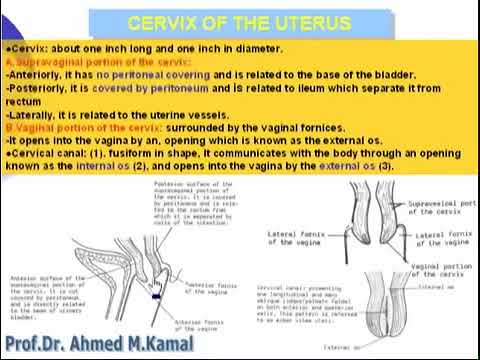 If the pelvic anatomy of the mother is too narrow or has any other anatomic anomaly, cephalopelvic disproportion between the fetus and the mother may lead to prolonged or arrest of labor.[4] If the fetus is in the breech position, this may also lead to labor difficulties and hinder the ability of the cervix to dilate fully.[5]
If the pelvic anatomy of the mother is too narrow or has any other anatomic anomaly, cephalopelvic disproportion between the fetus and the mother may lead to prolonged or arrest of labor.[4] If the fetus is in the breech position, this may also lead to labor difficulties and hinder the ability of the cervix to dilate fully.[5]
The stages of labor and their associated cervical dilations are as follows:
Stage 1: Effacement and dilation of the cervix from 0 to 10 cm
Latent phase: 0-6 cm
Active phase: 6-10 cm
Stage 2: Delivery of the fetus
Stage 3: Expulsion of the placenta[6]
The latent phase should not exceed 20 hours in a primigravida female or 14 hours in a multigravida female. If the mother does not fully dilate by these average time estimates, she is said to be having an arrest of the active phase of Stage 1 labor.
Cellular
The cervix is composed of multiple cell types. The endocervix is lined by simple columnar epithelium interspersed with mucus-producing goblet cells, while the ectocervix and vagina are composed of squamous epithelium.[7] The transition point between these two epithelia occurs at the external os and is termed the squamocolumnar junction (SCJ), or the "transformation zone."
The endocervix is lined by simple columnar epithelium interspersed with mucus-producing goblet cells, while the ectocervix and vagina are composed of squamous epithelium.[7] The transition point between these two epithelia occurs at the external os and is termed the squamocolumnar junction (SCJ), or the "transformation zone."
Unlike the uterus, a purely smooth muscle organ, the cervix is a collagenous structure composed of proteoglycans, fibrin, and glycosaminoglycans (GAGs) with smooth muscle present throughout the organ.[8] These components of the cervix give it elastic properties that allow it to dilate and efface during pregnancy and recoil after delivery, making it more similar to connective tissue.[9] While the mechanism is not entirely understood, studies suggest that the cervix undergoes temporary hyperplasia with a multitude of collagenous cells to support the birthing process.[10] Once delivery is complete, these cells undergo apoptosis and return the cervix to its pre-pregnancy state. [11]
[11]
Development
The cervix and upper one-third of the vagina form from two paramesonephric (Mullerian) ducts that fuse and recanalize, also giving rise to the body of the uterus and the fallopian tubes. The paramesonephric ducts are present in all embryos from day 0. Without the Mullerian inhibiting factor (MIF), a hormone produced by male embryos, the paramesonephric ducts will develop into the fallopian tubes, uterus, upper one-third of the vagina, and cervix by default.[7]
A recent study found that obvious discernment of a developing cervix is present around 18 weeks of gestation. However, before this time, at roughly 8-10 weeks, the cervical domain can be inferred based upon craniocaudal position within the uterovaginal canal and subtle histological differentiation of the epithelium.[12]
Function
To protect the developing fetus from the outside world, the cervix maintains its anatomy as a tightly-closed tubular structure throughout the majority of the pregnancy.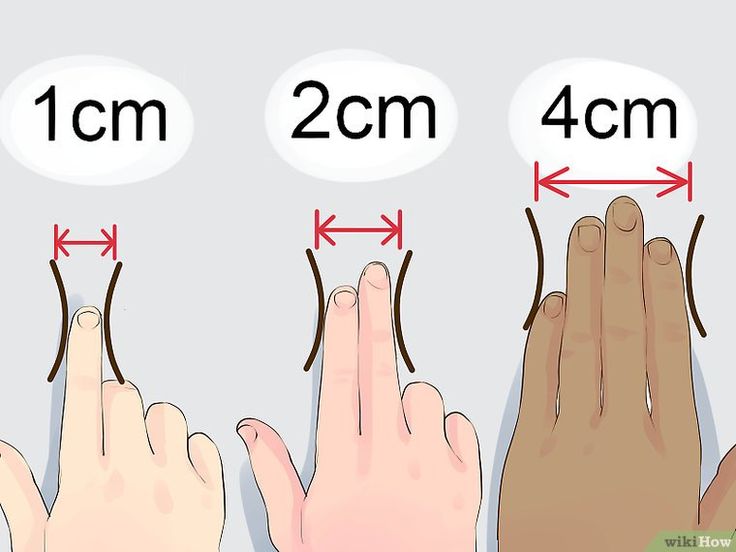 As a mother approaches the term segment of her pregnancy, which is recognized anywhere between 37 and 42 weeks, the cervix undergoes dilation and effacement to enable the passage of the fetus from the uterus down through the vaginal canal.[13] Effacement refers to the thinning and stretching of the entire cervix, while dilation refers to the softening and widening of the external os of the cervix.[9]
As a mother approaches the term segment of her pregnancy, which is recognized anywhere between 37 and 42 weeks, the cervix undergoes dilation and effacement to enable the passage of the fetus from the uterus down through the vaginal canal.[13] Effacement refers to the thinning and stretching of the entire cervix, while dilation refers to the softening and widening of the external os of the cervix.[9]
Mechanism
As previously mentioned, the first stage of labor contains a latent phase and an active phase. During the latent phase, the cervix will dilate to 6 centimeters. The latent phase tends to last longer and shows less predictability of cervical change than is observed in the active phase of labor. The cervix changes at a more rapid and predictable pace in the active phase until it reaches complete dilation (10 cm). The cervix dilates at approximately 1.2 to 1.5 centimeters per hour during the active phase, with multiparous women demonstrating more rapid cervical dilation than nulliparous.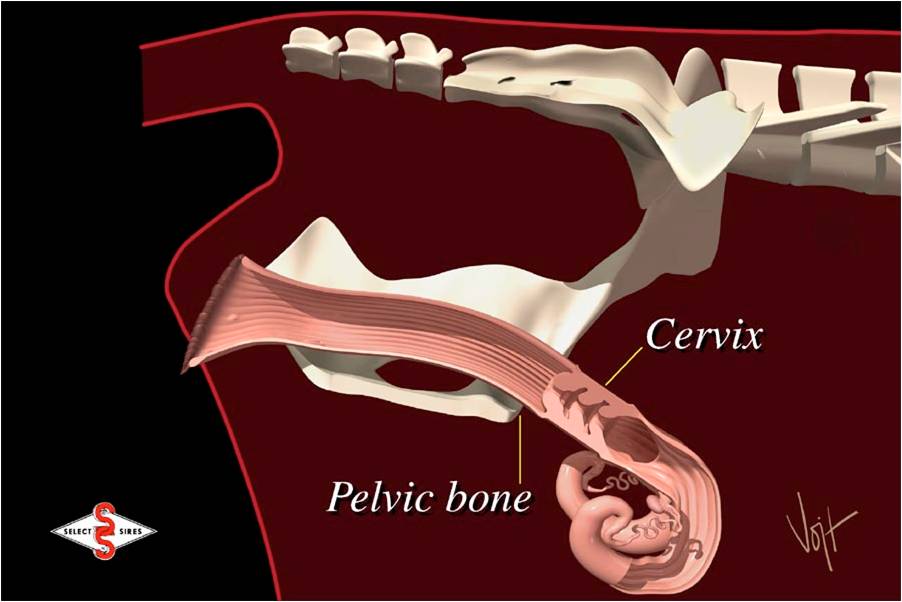 [1]
[1]
A positive feedback loop requiring oxytocin plays a pivotal role in the progression of the first stage of labor. Oxytocin is made in the hypothalamus and released into the bloodstream by the posterior pituitary gland, where it is transported to the uterus and stimulates uterine contractions. These contractions result in the descent of the fetus, with the descending fetal head activating stretch receptors on the cervix. These cervical stretch receptors send signals to the hypothalamus via afferent nerves, stimulating the additional release of oxytocin, thereby closing the loop. This loop results in progressively intensifying contractions and dilation over time.
Related Testing
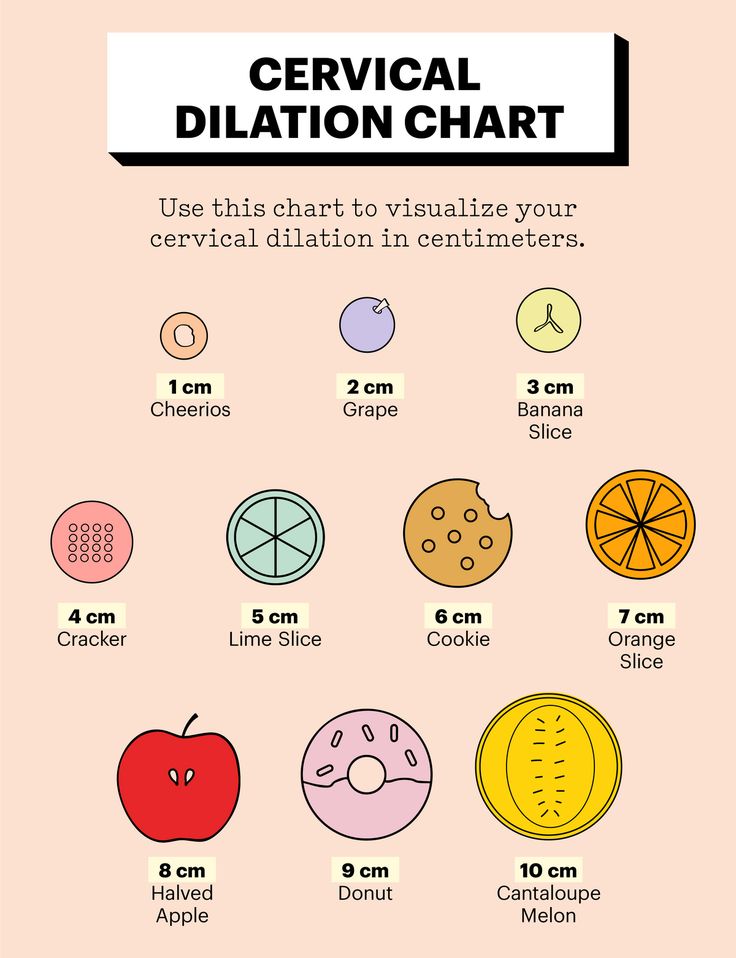
The most commonly used method of measuring cervical dilation during labor is a digital cervical exam. The obstetrician places two fingers inside the vagina and measures the width of the opening of the external os of the cervix using fingers to approximate the distance. In simple terms, 1 cm is about one finger's width, and 3 cm is the width of two fingers.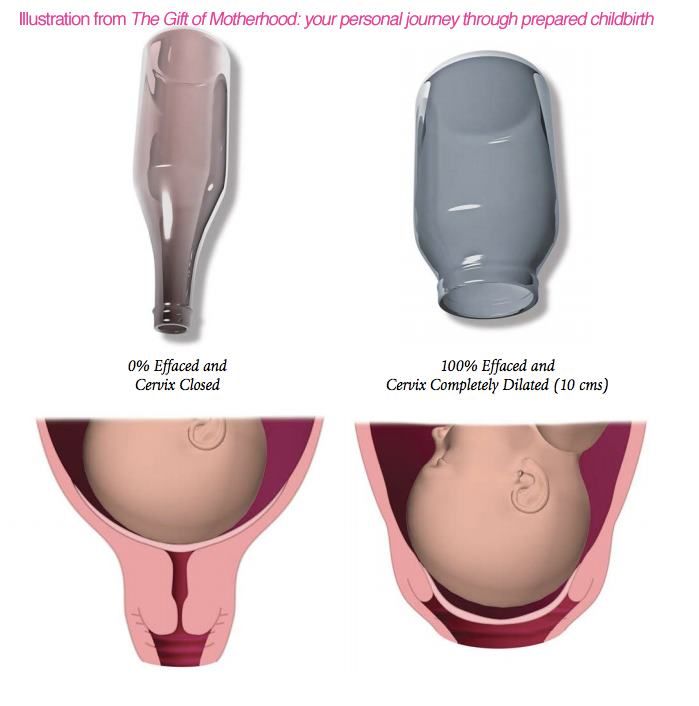 4 cm dilated is when the two fingers are approximately 1 cm apart. The widest stretch of the two fingers is about 7 to 8 cm. At 10 cm (full dilation), the cervix should not be present in front of the presenting fetal part (typically the head).
4 cm dilated is when the two fingers are approximately 1 cm apart. The widest stretch of the two fingers is about 7 to 8 cm. At 10 cm (full dilation), the cervix should not be present in front of the presenting fetal part (typically the head).
One meta-analysis suggested that ultrasound may play a new role in measuring cervical dilation to assess labor progression accurately. Still, at the moment, the digital cervical exam remains the gold standard.[14]
A pelvic scoring system, known as the Bishop score, is an important criterion utilized to determine the probability of successful labor induction. It is a clinical tool used to assess the cervix in pregnant women that can be obtained at the time of induction by a digital cervical exam. This scoring system considers the dilation and effacement of the cervix, its position and consistency, and the fetal station. There is a maximum score of 13, with a higher score (defined as 6+) indicating a more "favorable" cervix for vaginal delivery.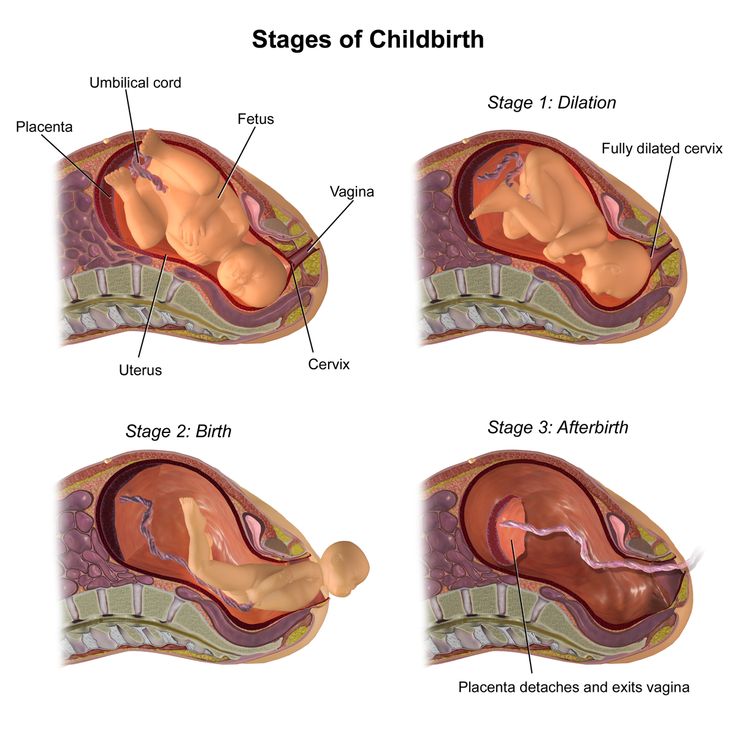 A lower score indicates a more "unfavorable" cervix for vaginal delivery and a higher chance of the woman undergoing cesarean delivery.[15]
A lower score indicates a more "unfavorable" cervix for vaginal delivery and a higher chance of the woman undergoing cesarean delivery.[15]
Pathophysiology
Failure of the cervix to dilate an appropriate amount in a certain amount of time can lead to protracted or arrested labor. The definitions of what is termed protracted vs. arrested labor are listed below.
Abnormal labor patterns
First stage
Protracted latent phase (dilation < 6 cm)
> 20 hours (primigravida)
> 14 hours (multigravida)
Protracted active phase (dilation 6+ cm)
Arrested active phase
No cervical change for 4+ hours with adequate contractions
No cervical change for 6+ hours with inadequate contractions
The absence of cervical change for greater than 4 hours in the presence of adequate contractions or six hours with inadequate contractions is considered an arrest of labor and may warrant clinical intervention.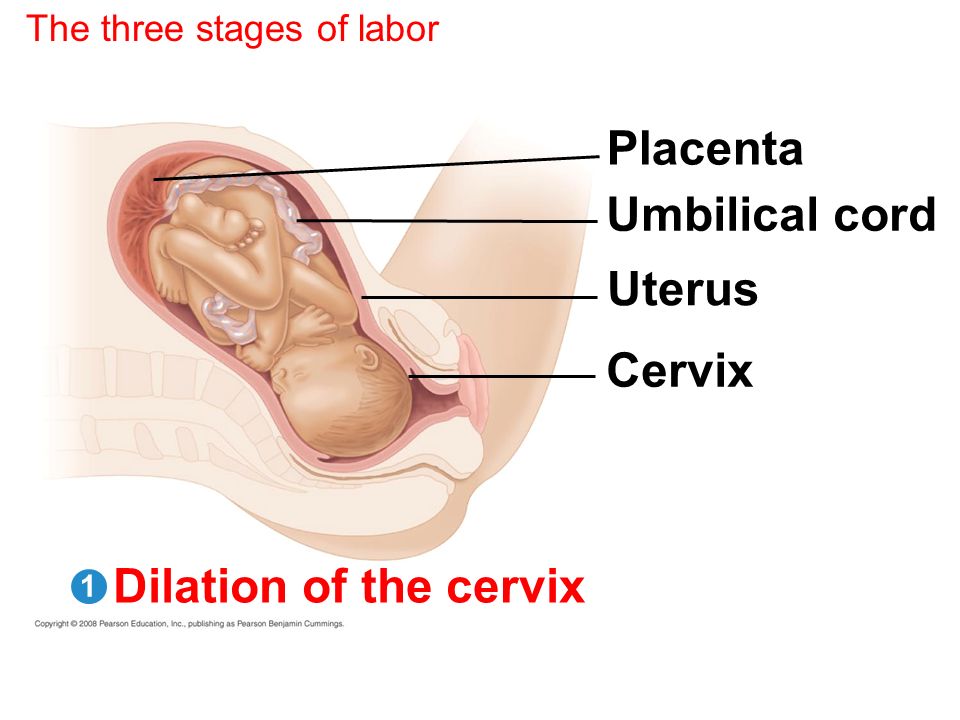 [7]
[7]
Clinical Significance
In those with a Bishop score < 6 or arrest of labor, multiple methods of cervical ripening can be performed by the obstetrician.
Pharmacologic Methods of Cervical Ripening [16]
Misoprostol: synthetic prostaglandin E1 analog administered orally or vaginally
Dinoprostone: prostaglandin E2 agent may be given as a vaginal insert or cervical gel
Mifepristone: progesterone antagonist administered orally
Oxytocin: does not directly induce cervical dilation but instead causes the uterus to contract more fully. This pushes the fetal head against the cervix, further stimulating the thinning and widening.
Many patients will inquire about natural methods of augmenting labor and cervical dilation. The clinician should verbalize to the patient that these non-pharmacologic methods continue to maintain an uncertain efficacy role in labor induction and cervical ripening.
Non-pharmacologic Methods of Cervical Ripening
Herbal: evening primrose oil and red raspberry leaves[17]
Breast stimulation: facilitates the release of oxytocin
Sexual intercourse: promotes the release of oxytocin via breast and nipple stimulation. Stimulation of the lower uterine segment via penetration may result in the local release of prostaglandins.[18]
Acupuncture: may trigger the release of oxytocin and prostaglandins[19]
Mechanical Methods of Cervical Ripening
Hygroscopic dilators: absorb endocervical fluids, allowing the device to expand within the endocervix, leading to dilation.
Balloon catheter: a specialized balloon catheter or foley catheter may be used. The catheter is introduced into the endocervix and inflated with saline. The balloon is retracted to rest on the internal os, applying direct pressure to the cervix, mimicking the fetal head pressure against the cervix.
 This, in turn, increases the cervical tissue response to oxytocin and prostaglandin.[20]
This, in turn, increases the cervical tissue response to oxytocin and prostaglandin.[20]
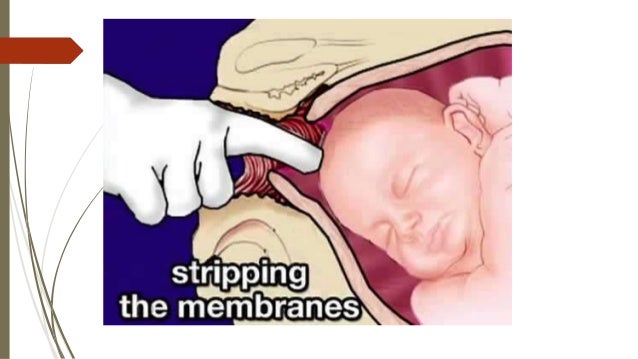
Surgical Methods of Cervical Ripening
Membrane stripping: inserting a finger through the internal cervical os and moving it in a circle, detaching the inferior pole of the membranes from the lower uterine segment.
Amniotomy: also known as artificial rupture of the membranes (AROM)
The majority of the above methods of cervical ripening may also be utilized to ripen and dilate the cervix in dilation and curettage.
Also of clinical importance is the length of the cervix. It is well known that the cervical length is a strong indicator of whether or not a birth will be preterm. The shorter the cervical length, the higher the risk of spontaneous preterm birth. For clinical ease, the cutoff above which a cervix can be considered normal is 25 mm (2.5 cm). Those below this cutoff are at an increased risk of spontaneous preterm birth. [21] For reference, a meta-analysis of 158,000 women who underwent a transvaginal ultrasound between 16 and 24 weeks showed a mean cervical length of 3.8 cm.[22]
[21] For reference, a meta-analysis of 158,000 women who underwent a transvaginal ultrasound between 16 and 24 weeks showed a mean cervical length of 3.8 cm.[22]
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Jung H. [Ripening processes of the uterine cervix and their significance for parturition]. Z Geburtshilfe Perinatol. 1984 Jan-Feb;188(1):1-6. [PubMed: 6538726]
- 2.
Danforth DN. The morphology of the human cervix. Clin Obstet Gynecol. 1983 Mar;26(1):7-13. [PubMed: 6839572]
- 3.
Ness A, Goldberg J, Berghella V. Abnormalities of the first and second stages of labor. Obstet Gynecol Clin North Am. 2005 Jun;32(2):201-20, viii. [PubMed: 15899355]
- 4.
Handa VL, Laros RK. Active-phase arrest in labor: predictors of cesarean delivery in a nulliparous population. Obstet Gynecol. 1993 May;81(5 ( Pt 1)):758-63.
 [PubMed: 8469468]
[PubMed: 8469468]- 5.
Krause M, Fischer T, Feige A. [What effect does leg position in breech presentation have on mode of delivery and early neonatal morbidity?]. Z Geburtshilfe Neonatol. 1997 Jul-Aug;201(4):128-35. [PubMed: 9410517]
- 6.
Gill P, Henning JM, Van Hook JW. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): May 11, 2022. Abnormal Labor. [PubMed: 29083834]
- 7.
Reich O, Fritsch H. The developmental origin of cervical and vaginal epithelium and their clinical consequences: a systematic review. J Low Genit Tract Dis. 2014 Oct;18(4):358-60. [PubMed: 24977630]
- 8.
Ferland DJ, Darios ES, Watts SW. The persistence of active smooth muscle in the female rat cervix through pregnancy. Am J Obstet Gynecol. 2015 Feb;212(2):244.e1-8. [PubMed: 25108144]
- 9.
Aubard Y, Chinchilla AM, Dubayle G, Cantaloube M, Gana J, Baudet J. [The cervix uteri in pregnancy]. J Gynecol Obstet Biol Reprod (Paris).
 1998 Dec;27(8):755-64. [PubMed: 10021988]
1998 Dec;27(8):755-64. [PubMed: 10021988]- 10.
Ludmir J, Sehdev HM. Anatomy and physiology of the uterine cervix. Clin Obstet Gynecol. 2000 Sep;43(3):433-9. [PubMed: 10949747]
- 11.
Ichijo M, Shimizu T, Sasai Y. Histological aspects of cervical ripening. Tohoku J Exp Med. 1976 Feb;118(2):153-61. [PubMed: 136067]
- 12.
Cunha GR, Robboy SJ, Kurita T, Isaacson D, Shen J, Cao M, Baskin LS. Development of the human female reproductive tract. Differentiation. 2018 Sep - Oct;103:46-65. [PMC free article: PMC6234064] [PubMed: 30236463]
- 13.
Liao JB, Buhimschi CS, Norwitz ER. Normal labor: mechanism and duration. Obstet Gynecol Clin North Am. 2005 Jun;32(2):145-64, vii. [PubMed: 15899352]
- 14.
Brancadoro M, Tognarelli S, Fambrini F, Ragusa A, Menciassi A. Devices for Measuring Cervical Dilation During Labor: Systematic Review and Meta-analysis. Obstet Gynecol Surv. 2018 Apr;73(4):231-241.
 [PubMed: 29701868]
[PubMed: 29701868]- 15.
Wormer KC, Bauer A, Williford AE. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Sep 9, 2021. Bishop Score. [PubMed: 29261961]
- 16.
Kelsey JJ, Prevost RR. Drug therapy during labor and delivery. Am J Hosp Pharm. 1994 Oct 01;51(19):2394-402; quiz 2504-5. [PubMed: 7847404]
- 17.
McFarlin BL, Gibson MH, O'Rear J, Harman P. A national survey of herbal preparation use by nurse-midwives for labor stimulation. Review of the literature and recommendations for practice. J Nurse Midwifery. 1999 May-Jun;44(3):205-16. [PubMed: 10380441]
- 18.
Schaffir J. Sexual intercourse at term and onset of labor. Obstet Gynecol. 2006 Jun;107(6):1310-4. [PubMed: 16738157]
- 19.
Smith CA, Crowther CA, Grant SJ. Acupuncture for induction of labour. Cochrane Database Syst Rev. 2013 Aug 15;(8):CD002962. [PubMed: 23945980]
- 20.
Košec V, Djaković I, Sabolović Rudman S.
 CERVICAL RIPENING BALLOON AS A METHOD OF PREINDUCTION - ONE CENTER STUDY. Acta Clin Croat. 2018 Dec;57(4):762-767. [PMC free article: PMC6544105] [PubMed: 31168214]
CERVICAL RIPENING BALLOON AS A METHOD OF PREINDUCTION - ONE CENTER STUDY. Acta Clin Croat. 2018 Dec;57(4):762-767. [PMC free article: PMC6544105] [PubMed: 31168214]- 21.
O'Hara S, Zelesco M, Sun Z. Cervical length for predicting preterm birth and a comparison of ultrasonic measurement techniques. Australas J Ultrasound Med. 2013 Aug;16(3):124-134. [PMC free article: PMC5029998] [PubMed: 28191186]
- 22.
Bortoletto TG, Silva TV, Borovac-Pinheiro A, Pereira CM, Silva AD, França MS, Hatanaka AR, Argenton JP, Passini R, Mol BW, Cecatti JG, Pacagnella RC. Cervical length varies considering different populations and gestational outcomes: Results from a systematic review and meta-analysis. PLoS One. 2021;16(2):e0245746. [PMC free article: PMC7886126] [PubMed: 33592005]
Important to know - Health of a Petersburger
The total duration of childbirth and their course
The total duration of childbirth depends on many factors: age, physique and physical condition of the woman, her psychological mood, the speed of cervical dilatation, first pregnancy or repeated, the size of the child, the type of presentation and a number of other points.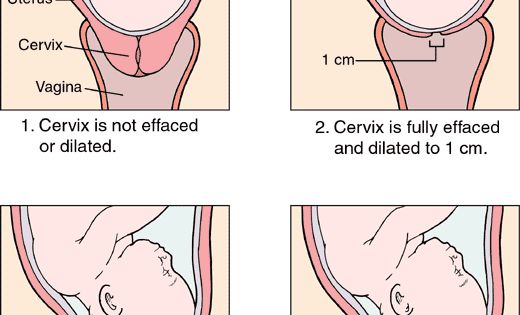
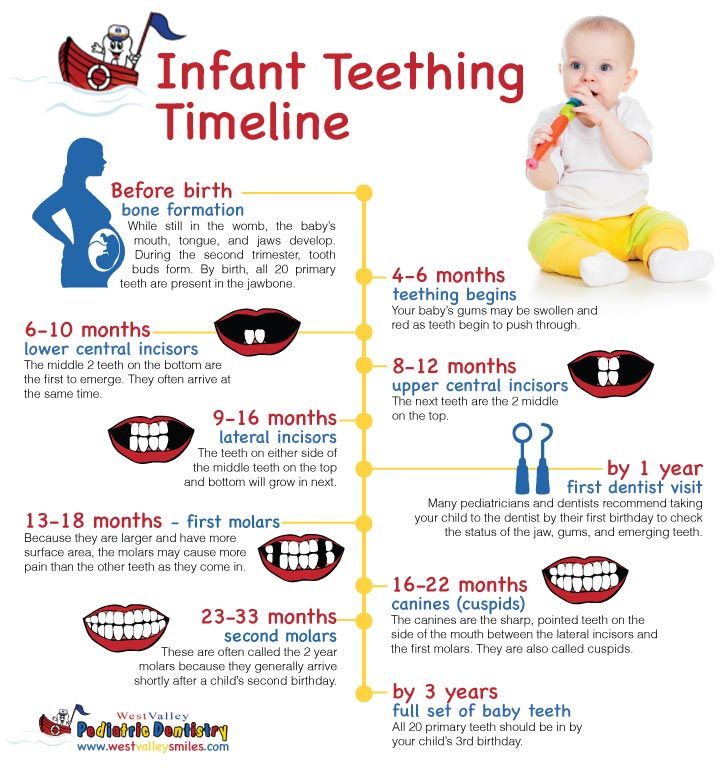
Labor activity proceeds differently for all women, but the main periods of childbirth are clearly distinguished: 1st period - the period of contractions, the longest and most intense, 2nd period - the direct birth of a baby, 3rd period - the birth of the afterbirth (placenta).
First stage of labor (opening period)
As the name implies, during this period there is a gradual opening of the cervix as a result of regular contractions of the uterine muscles. Contractions occur with a decreasing interval, while they themselves become longer and more frequent.
The dilation period is the time elapsed from the onset of regular contractions until the cervix is fully dilated. During this period, the birth canal is prepared for the passage of the fetus through them with all the fetal formations.
Cervical dilatation occurs gradually: at first the cervix is smoothed out, then the pharynx opens up to 3-4 cm and at the end of the first stage of labor up to 10 cm.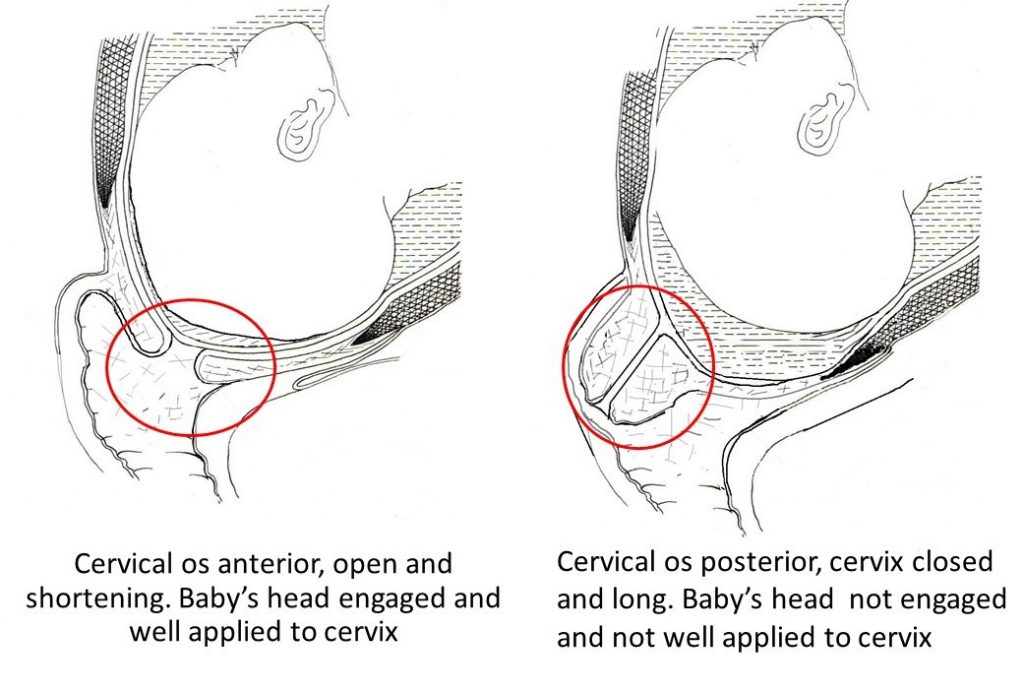 This is already a complete dilatation of the cervix. With it, during contractions, the fetal bladder becomes tense and bursts at the height of one of them, the anterior portion of amniotic fluid is poured out.
This is already a complete dilatation of the cervix. With it, during contractions, the fetal bladder becomes tense and bursts at the height of one of them, the anterior portion of amniotic fluid is poured out.
The first stage of labor is the longest and consists of three phases:
1. Latent phase (lasts 5-6 hours). It is characterized by the establishment of regular contractions, with an interval between them of 10-15 minutes. Latent, or hidden, this phase is called because the contractions of the uterus during it are painless or slightly painful. By the end of the phase, the cervix is definitively flattened and opens about 4 cm.
2. Active phase (lasts 3-4 hours). Contractions become more intense, last at least 20 seconds, and the interval between them is reduced to 5-6 minutes. Normally, during the active phase, amniotic fluid is poured out, which contributes to a faster full disclosure of the uterine pharynx. By the end of the phase, the uterus opens by 8 cm.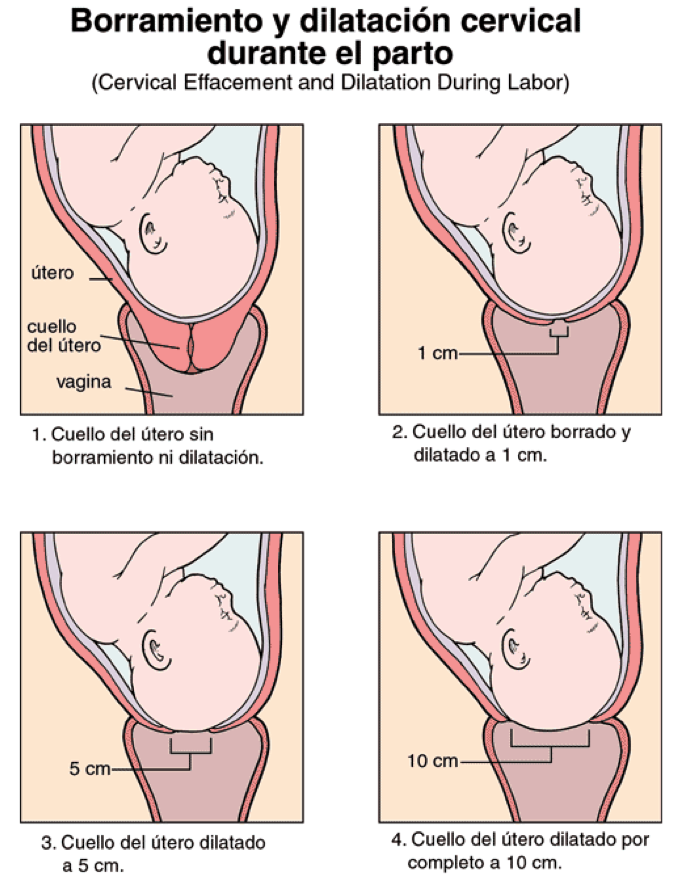 This phase is not always clearly manifested, but it is nevertheless distinguished due to the usual weakening of contractions during disclosure from 8 to 10 cm. The child's head descends and stands in the narrow part of the small pelvis, which necessitates a slower and smoother process. Already in the transitional phase, the woman in labor feels the desire to push, to push the baby out. But in order for the head to pass through the birth canal without the risk of injury, it is necessary to achieve cervical dilatation up to 10 cm.
This phase is not always clearly manifested, but it is nevertheless distinguished due to the usual weakening of contractions during disclosure from 8 to 10 cm. The child's head descends and stands in the narrow part of the small pelvis, which necessitates a slower and smoother process. Already in the transitional phase, the woman in labor feels the desire to push, to push the baby out. But in order for the head to pass through the birth canal without the risk of injury, it is necessary to achieve cervical dilatation up to 10 cm.
Second stage of labor (exile period)
The period of exile is the time from the moment of full opening of the pharynx until the birth of the fetus.
It is the second stage of childbirth that is their culmination, because for a short time (compared to contractions) the long-awaited birth of the baby takes place.
After the discharge of amniotic fluid, contractions temporarily stop. The volume of the uterine cavity decreases, the uterine cavity and vagina appear as a single birth canal.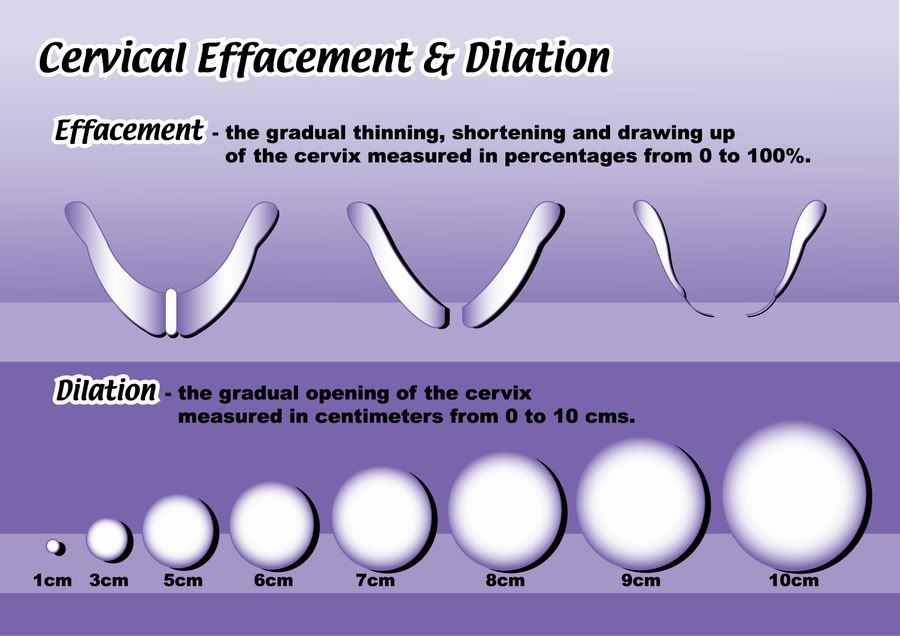 Contractions reappear and become more intense. They are joined by attempts - contractions of the muscle press (abdominal wall, diaphragm and pelvic floor). The frequency and intensity of contractions and attempts are constantly increasing. The head descends and compresses the nerves of the sacral plexus. A woman has a strong desire to squeeze the head out of the birth canal, she is looking for supports for her arms and legs to strengthen her efforts.
Contractions reappear and become more intense. They are joined by attempts - contractions of the muscle press (abdominal wall, diaphragm and pelvic floor). The frequency and intensity of contractions and attempts are constantly increasing. The head descends and compresses the nerves of the sacral plexus. A woman has a strong desire to squeeze the head out of the birth canal, she is looking for supports for her arms and legs to strengthen her efforts.
Pushing is a lot of physical work. During attempts, a woman experiences maximum physical stress (blood pressure rises, pulse and respiration become more frequent). During the attempts, the woman holds her breath, and in the intervals between them she rests and "gathers her strength for a new attempt."
In the process of one of the attempts, the head is born. Next, the shoulders are born (first the front, then the back) and the torso. Following the fetus, the posterior amniotic fluid is poured out with an admixture of cheese-like lubricant.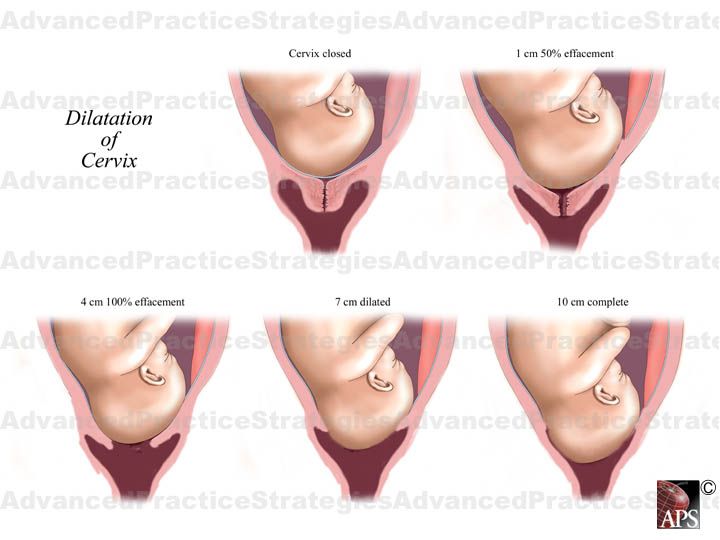
A woman in labor, having experienced severe fatigue, rests after hard work (pulse and respiration rate decrease).
Third stage of labor (postpartum period).
The afterbirth period is the time from the birth of the fetus to the birth of the placenta. During this period, the placenta separates from the walls of the uterus and the birth of the placenta (placenta with membranes and umbilical cord).
In the process of separation of the placenta from the walls of the uterus, the uteroplacental vessels are damaged, which is normally accompanied by blood loss in the amount of 100-200 ml, without adversely affecting the woman's condition. After the birth of the placenta, the uterus contracts sharply, becomes dense, which is necessary to stop bleeding in the area of the placental site; its bottom is in the middle between the womb and the navel.
During this period, the woman's pulse and respiration normalize. Her demeanor is calm. Chills can sometimes be observed (as a reaction to the transferred strong physical stress).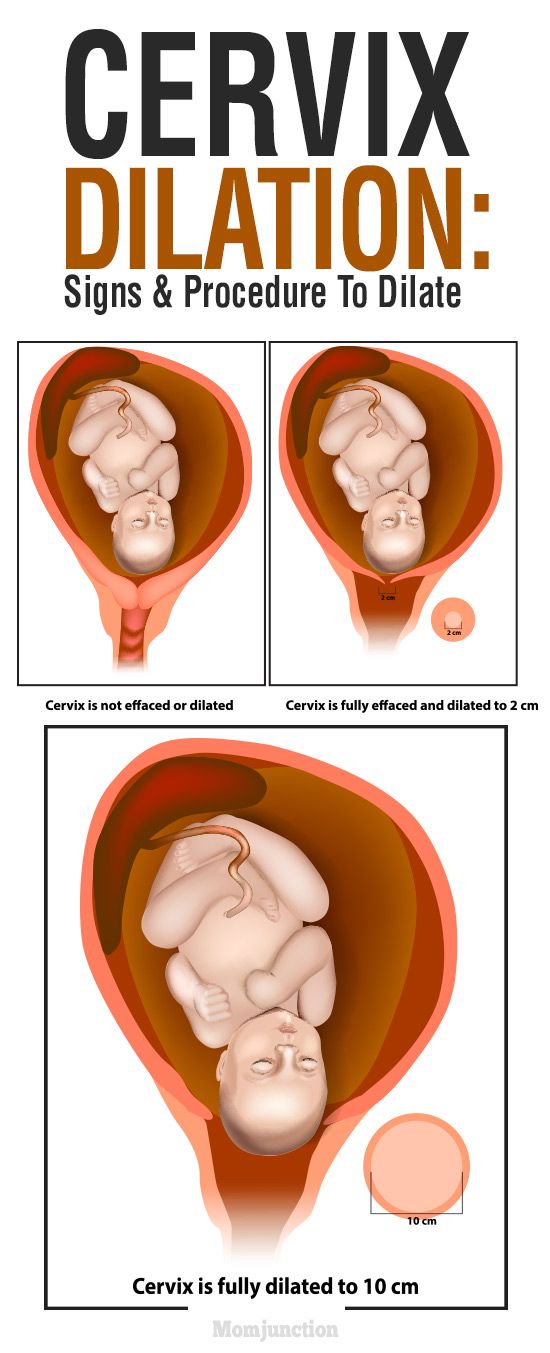
The third period is no longer as exciting and tense as the previous two. The child was born and the matter remains for the small - the separation of the placenta, or placenta. Nature provides for the resumption of contractions a few minutes after the birth of the baby, necessary for effective exfoliation from the uterus of tissues that nourished the fetus during pregnancy (placenta, membranes, umbilical cord).
Three periods of physiological labor - the natural end of a nine-month wait. Most likely, during the birth process itself, the woman in labor will not care what the period or phase of childbirth is now, but it is still desirable to know about them, at least for greater certainty before going to the hospital.
Cervix: general information, structure
Consultation with a specialist:
The structure of the cervix and its functions
The organ has a cylindrical shape, and its inner part is a hollow “tube” lined with epithelial tissue.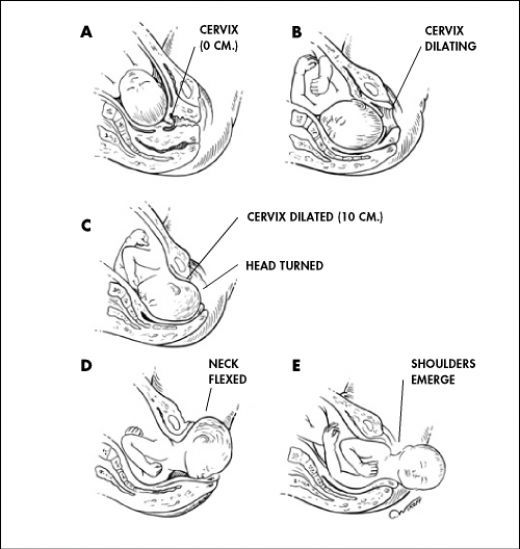
The cervix is divided into two regions:
- Vaginal. Enters the vaginal cavity. It has a convex shape. Lined with stratified squamous epithelium.
- Supravaginal. Lies above the vagina. Lined with columnar epithelium.
The area where the squamous epithelium of the vaginal part changes to the cylindrical epithelium of the cervical canal is called the transformation zone.
The cervical canal is the central part of the cervix. It has an internal pharynx that goes to the body of the uterus, as well as an external one facing the vagina - it is seen by the gynecologist when examining the patient. In nulliparous women, the external os has a round or oval shape, in those who have given birth, it is slit-like. The channel always contains a certain amount of mucus.
Cervical mucus is a biological fluid, the importance of which in a woman's reproductive health can hardly be overestimated.
It has antibacterial properties and prevents penetration into the uterine cavity infection.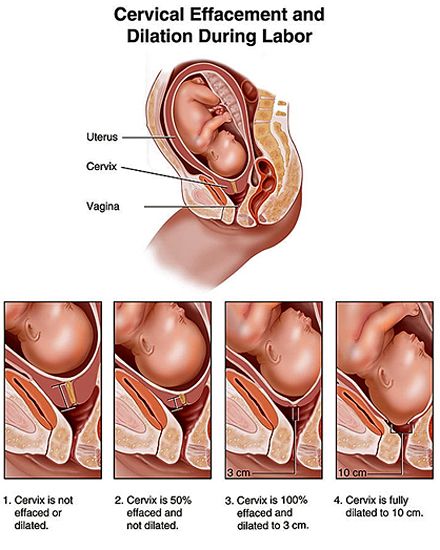 When a woman becomes pregnant, the cervical canal is closed with a dense mucous plug, which reliably protects the fetus from pathogenic microorganisms.
When a woman becomes pregnant, the cervical canal is closed with a dense mucous plug, which reliably protects the fetus from pathogenic microorganisms.
The rheological characteristics of cervical mucus change depending on the woman's monthly cycle. During ovulation and menstruation, it becomes more fluid. In the first case, it helps the sperm to move through the canal, which means it promotes conception. In the second, it facilitates the outflow of menstrual blood.
Call now
+7 (495) 215-56-90
Sign up
Cervix during pregnancy
The task of the cervix during this period is to protect the fetus from infection and prevent abortion or premature birth.
Shortly after conception, the following changes occur in it:
- The pink surface of the channel takes on a bluish tint due to the increased pattern of blood vessels. This is facilitated by intensive blood circulation in the uterus.
- The mucous membrane becomes softer. This is also due to increased blood circulation and mucus secretion.
- The cervix descends lower, and the lumen of the canal narrows and is tightly “sealed” with a cork.
According to these changes, the gynecologist can visually determine pregnancy a few weeks after conception.
As the fetus develops in the womb, the length of the cervix gradually decreases. It is very important that it matches the gestational age, since a too short neck can threaten miscarriage or premature birth.
In the third trimester, the cervix becomes shorter, softer, and closer to childbirth, it begins to open slightly. The mucus plug may come off within a few weeks of labor.
Cervix and childbirth
Before the onset of active labor activity, the organ shortens to 1 cm and its anatomical position changes. The neck, previously directed slightly backward, moves to the center and is located under the head of the child.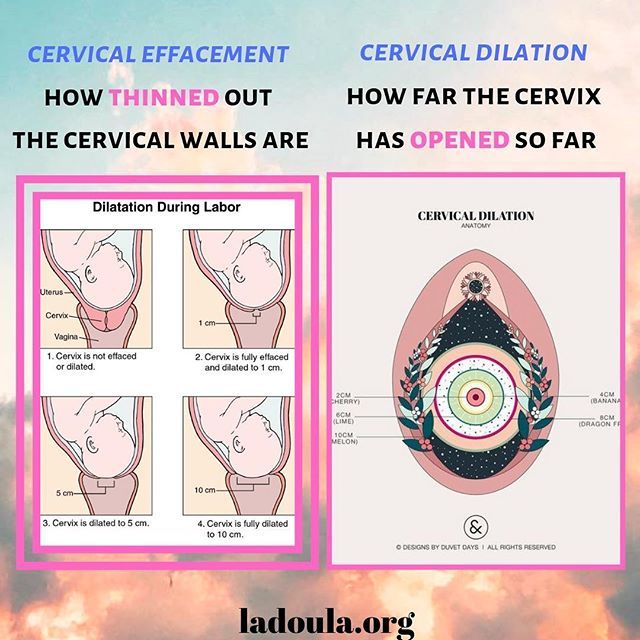
As labor proceeds, the cervix shortens and smoothes, and its lumen gradually opens so that the baby's head can pass through it. Full dilatation of the cervix - about 10 cm.
At the first birth, the internal os opens first, and then the external one. With subsequent disclosure occurs at the same time, so childbirth is faster.
Diseases of the cervix
Diseases of this organ are divided into the following types:
- Background - not associated with malignant processes.
- Precancerous (dysplasia) - there are areas with damaged cell structure (atypical cells), but without malignant changes.
- Cancer - malignant changes in the cellular structure.
Most of the diseases of the cervix occur without symptoms. In some cases, they may be accompanied by increased discharge, discomfort during sexual contact, bloody discharge. But even cervical cancer can give severe symptoms only at a late stage, when the disease is difficult to cure.
Cervical pathology can only be detected by specialized methods during a gynecological examination.
These methods include:
- Pap smear. Allows you to suspect the presence of atypical cells and the degree of their damage, to identify the inflammatory process in the cervix. Based on the results of the Pap test, further examination of the patient is performed.
- Colposcopy. Visual examination of the mucous membrane of an organ using an optical device - a colposcope. During colposcopy, various tests can be performed to identify damaged areas, as well as a tissue fragment (biopsy) is taken to perform a histological examination.
- Histological analysis. The study of the cellular structure of the selected biomaterial under a microscope. The diagnosis of "dysplasia" and "cervical cancer" can only be made based on the results of histology.
- Flora smear. It is performed to identify pathogenic flora and determine its sensitivity to antibiotics and antimycotics (antifungal drugs).
 The analysis is necessary for organizing the treatment of inflammatory processes.
The analysis is necessary for organizing the treatment of inflammatory processes.
Your doctor may also order blood tests for sexually transmitted diseases (STDs) and human papillomavirus (HPV). Some strains of HPV are oncogenic and provoke dysplasia and cervical cancer.
Oncological processes of the cervix are formed rather slowly, passing through three stages of dysplasia - mild, moderate and severe. And even the third degree of dysplasia can be treated with full preservation of the reproductive function of a woman.
Early stage cervical cancer also has a favorable prognosis for the patient if treatment was started on time. Whether the organ will be preserved at the same time, the doctor decides according to indications.
At later stages, a radical hysterectomy is practiced - removal of the uterus with appendages, pelvic lymph nodes and the upper region of the vagina.
We repeat that dysplasia and subsequently cervical cancer develop slowly, almost asymptomatically, but are easily diagnosed during a medical examination. Whether a woman gets this type of cancer or not is largely a matter of her personal responsibility. An annual visit to a gynecologist for preventive examinations will protect you from this serious illness and preserve your reproductive health.
Whether a woman gets this type of cancer or not is largely a matter of her personal responsibility. An annual visit to a gynecologist for preventive examinations will protect you from this serious illness and preserve your reproductive health.
Call now
+7 (495) 215-56-90
Sign up
About clinic
Otradnoye Polyclinic is the largest multidisciplinary medical center in Moscow.
About 3,500 types of medical services for adults and children are provided on 4 floors in one building. More than 80 doctors serve thousands of patients per month.
The services of the center are available to all segments of the population, and treatment and diagnostic procedures are carried out according to modern protocols.
Our clinic has a diagnostic base for a complete examination, and surgeons perform operations both on an outpatient basis and in a well-equipped hospital.
We also have a wide range of physiotherapy and dental services available.