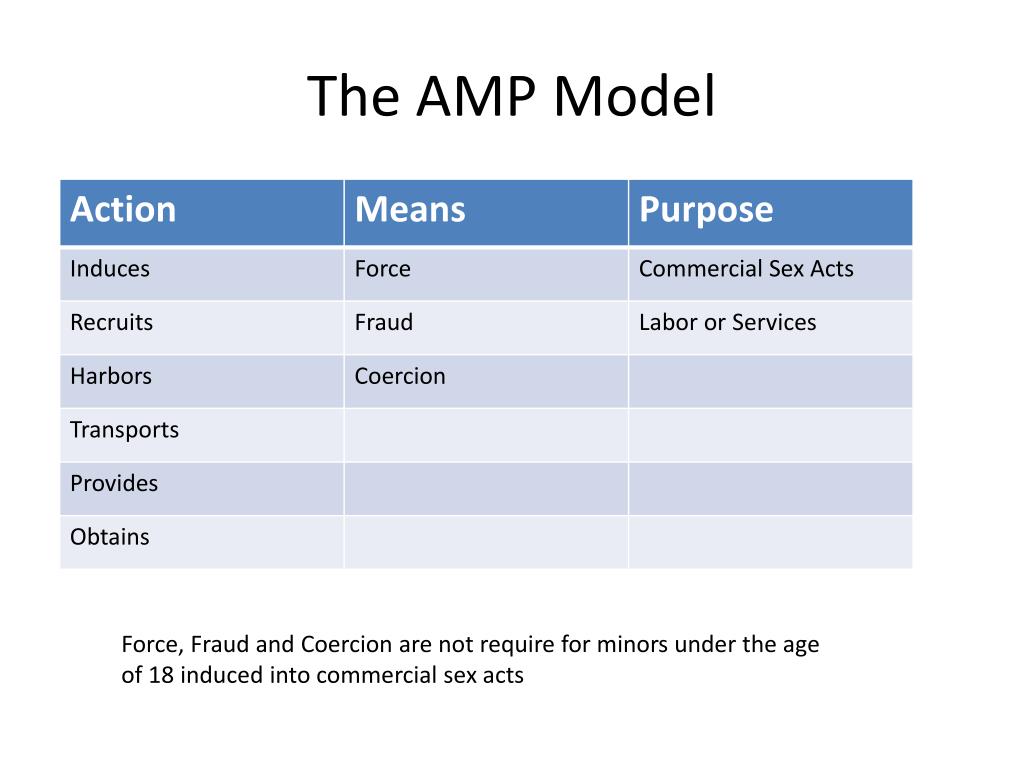
How do you get induced into labor
Inducing Labor (for Parents) - Nemours KidsHealth
It's common for many pregnant women, especially first-time mothers, to watch their baby's due date come and go without so much as a contraction. The farther away from the expected delivery date (called the EDD) you get, the more anxious you might become. You may start to wonder — is this baby ever going to come?
Late pregnancy can be challenging — you may feel large all over, your feet and back might hurt, you might not have the energy to do much of anything, and you're beyond ready to meet the little one you've nurtured all this time. Which is why waiting a little longer than you'd expected can be particularly hard.
Still, being past your due date doesn't guarantee that your doctor (or other health care provider) will do anything to induce (or artificially start) labor — at least not right away.
What Is It?
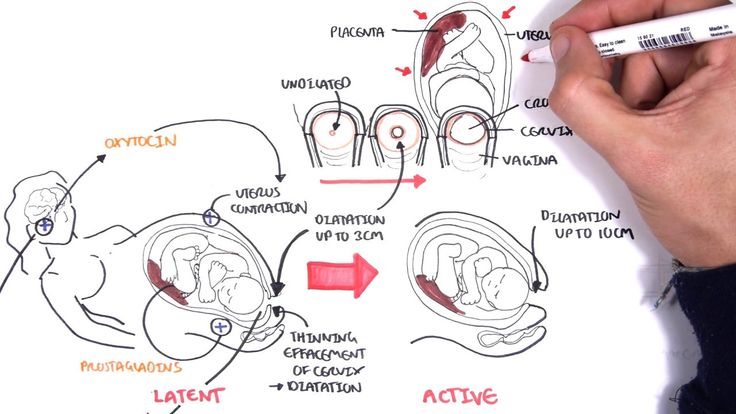
Labor induction is what doctors use to try to help labor along using medications or other medical techniques. Years ago, some doctors routinely induced labor. But now it's not usually done unless there's a true medical need for it. Labor is usually allowed to take its natural course. However, in some situations, a health care provider may recommend induction.
Why It's Done
Your doctor might suggest an induction if:
- your water broke but you are not having contractions
- your baby still hasn't arrived by 2 weeks after the due date (when you're considered post-term — more than 42 weeks into your pregnancy)
- you have an infection in the uterus (called chorioamnionitis)
- you have certain risk factors (e.g., gestational diabetes or high blood pressure)
- there is not enough amniotic fluid
- there is a problem with the placenta
- the baby is not growing appropriately
Induction also can be appropriate under certain circumstances, as with a mother who is full term and has a history of rapid deliveries or lives far from a hospital.
Some mothers request elective inductions for convenience, but these do come with risks. Doctors try to avoid inducing labor early because the due date may be wrong and/or the woman's cervix might not be ready yet.
Page 2
How It's Done
Some methods of induction are less invasive and carry fewer risks than others. Ways that doctors may try to induce labor by getting contractions started include:
- Stripping the membranes. The doctor puts on a glove and inserts a finger into the vagina and through the cervix (the opening that connects the vagina to the uterus). He or she moves the finger back and forth to separate the thin membrane connecting the amniotic sac (which houses the baby and amniotic fluid) to the wall of the uterus. When the membranes are stripped, the body releases hormones called prostaglandins, which help prepare the cervix for delivery and may bring on contractions. This method works for some women, but not all.
- Breaking your water (also called an amniotomy).
 The doctor ruptures the amniotic sac during a vaginal exam using a little plastic hook to break the membranes. If the cervix is ready for labor, amniotomy usually brings on labor in a matter of hours.
The doctor ruptures the amniotic sac during a vaginal exam using a little plastic hook to break the membranes. If the cervix is ready for labor, amniotomy usually brings on labor in a matter of hours. - Giving the hormone prostaglandin to help ripen the cervix. A gel or vaginal insert of prostaglandin is inserted into the vagina or a tablet is given by mouth. This is typically done overnight in the hospital to make the cervix "ripe" (soft, thinned out) for delivery. Administered alone, prostaglandin may induce labor or may be used before giving oxytocin.
- Giving the hormone oxytocin to stimulate contractions. Given continuously through an IV, the drug (Pitocin) is started in a small dose and then increased until labor is progressing well. After it's administered, the fetus and uterus need to be closely monitored. Oxytocin is also frequently used to spur labor that's going slowly or has stalled.
What Will It Feel Like?
Stripping the membranes can be a little painful or uncomfortable, although it usually only takes a minute or so. You may also have some intense cramps and spotting for the next day or two.
You may also have some intense cramps and spotting for the next day or two.
It can also be a little uncomfortable to have your water broken. You may feel a tug followed by a warm trickle or gush of fluid.
With prostaglandin, you might have some strong cramping as well. With oxytocin, contractions are usually more frequent and regular than in a labor that starts naturally.
Page 3
Risks and Precautions
Inducing labor is not like turning on a faucet. If the body isn't ready, an induction might fail and, after hours or days of trying, a woman may end up having a cesarean delivery (C-section). This appears to be more likely if the cervix is not yet ripe.
If the doctor ruptures the amniotic sac and labor doesn't begin, another method of inducing labor also might be necessary because there's a risk of infection to both mother and baby if the membranes are ruptured for a long time before the baby is born.
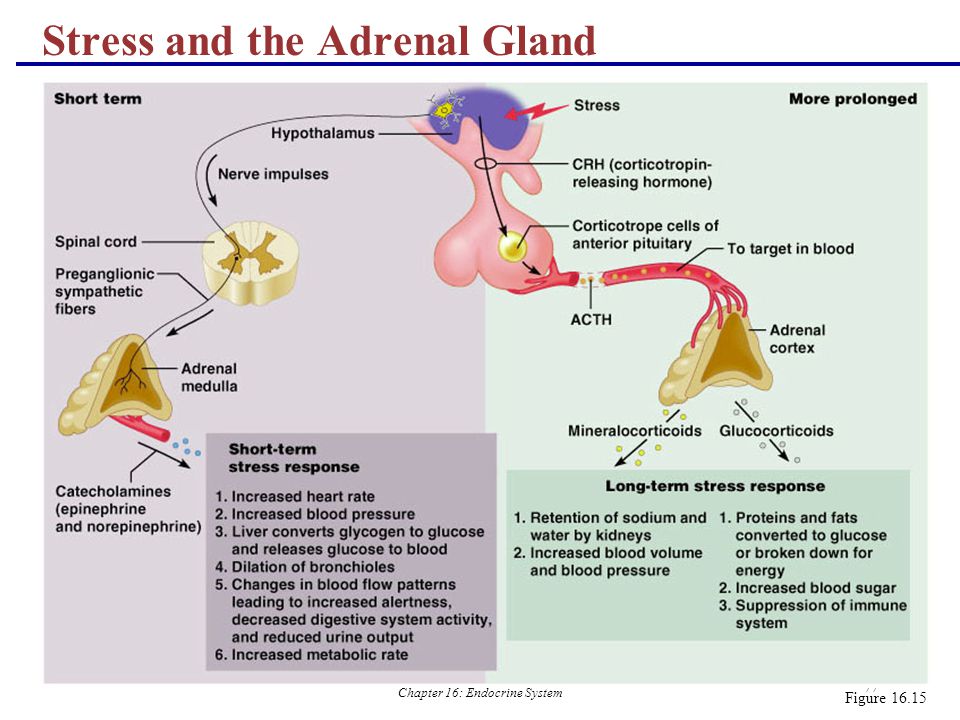
When prostaglandin or oxytocin is used, there is a risk of abnormal contractions developing.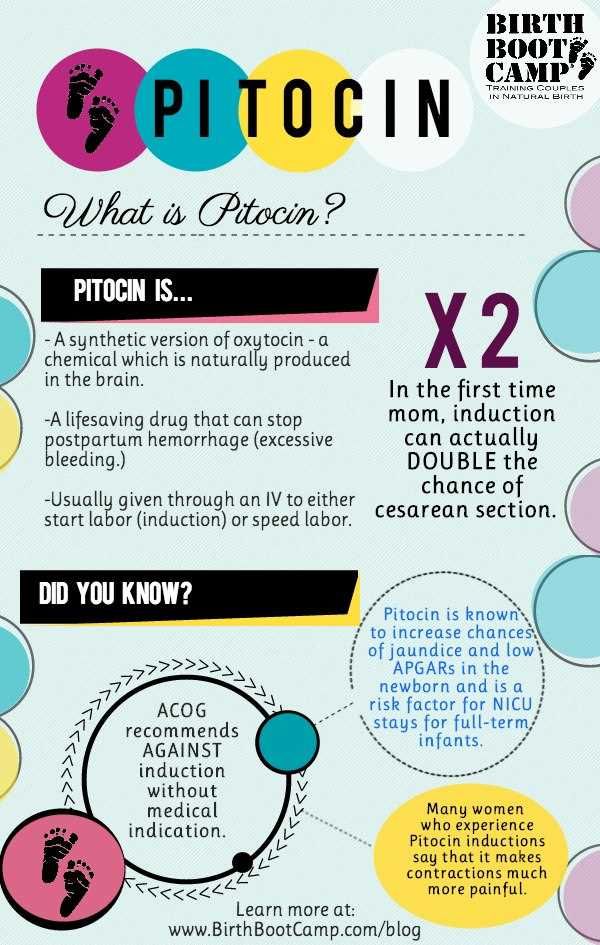 In that case, the doctor may remove the vaginal insert or turn the oxytocin dose down. While it is rare, there is an increase in the risk of developing a tear in the uterus (uterine rupture) when these medications are used. Other complications associated with oxytocin use are low blood pressure and low blood sodium (which can cause problems such as seizures).
In that case, the doctor may remove the vaginal insert or turn the oxytocin dose down. While it is rare, there is an increase in the risk of developing a tear in the uterus (uterine rupture) when these medications are used. Other complications associated with oxytocin use are low blood pressure and low blood sodium (which can cause problems such as seizures).
Another potential risk of inducing labor is giving birth to a late pre-term baby (born after 34 and before 37 weeks). Why? Because the due date (EDD) may be wrong. Your due date is 40 weeks from the first day of your last menstrual period (LMP).
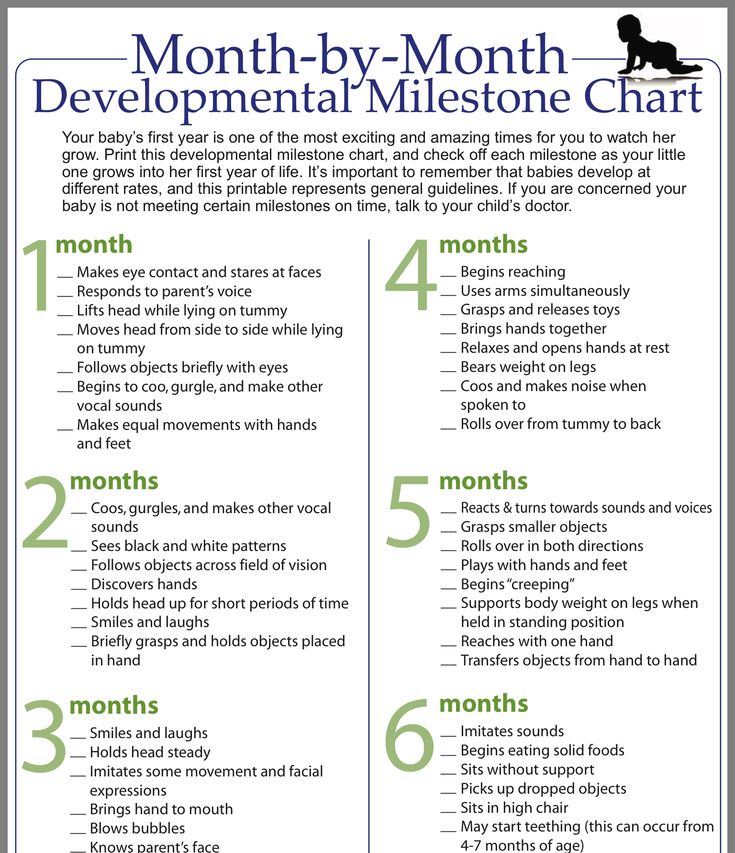
Babies born late pre-term are generally healthy but may have temporary problems such as jaundice, trouble feeding, problems with breathing, or difficulty maintaining body temperature. They may also be more likely than full term babies to have developmental or school problems later on.
Even though inductions do come with risks, going beyond 42 weeks of pregnancy can be risky, too. Many babies are born "post-term" without any complications, but concerns include:
Many babies are born "post-term" without any complications, but concerns include:
- A vaginal delivery may become harder as the baby gets bigger. As babies get bigger, the chance of an injury during delivery, such as a broken bone, increases.
- The placenta that helps to provide the baby with nourishment is deteriorating.
- The amniotic fluid can become low or contain meconium — the baby's first feces. If the baby breathes in meconium, it can cause breathing problems.
Old wives' tales abound about ways to induce labor, such as the use of castor oil. It is not safe to try to artificially start labor yourself by taking castor oil, which can lead to nausea, diarrhea, and dehydration. And herbs and herbal supplements meant to induce labor can be harmful. Breast stimulation can cause uterine contractions by causing the release of oxytocin. However, some studies have suggested that the baby might have abnormal heartbeats after breast stimulation. Some women feel that having sex in late pregnancy can induce labor, but there is no conclusion on this yet.
Talk to your doctor before doing anything to try to encourage your little one's arrival. Inducing labor is best left to medical professionals — you may cause more harm than good.
As frustrating as it can be waiting for your baby to finally decide to arrive, letting nature take its course is often best, unless your doctor tells you otherwise. Before you know it, you'll be too busy to remember your baby was ever late at all!
Labor induction - Mayo Clinic
Overview
Labor induction — also known as inducing labor — is prompting the uterus to contract during pregnancy before labor begins on its own for a vaginal birth.
A health care provider might recommend inducing labor for various reasons, primarily when there's concern for the mother's or baby's health. An important factor in predicting whether an induction will succeed is how soft and expanded the cervix is (cervical ripening). The gestational age of the baby as confirmed by early, regular ultrasounds also is important.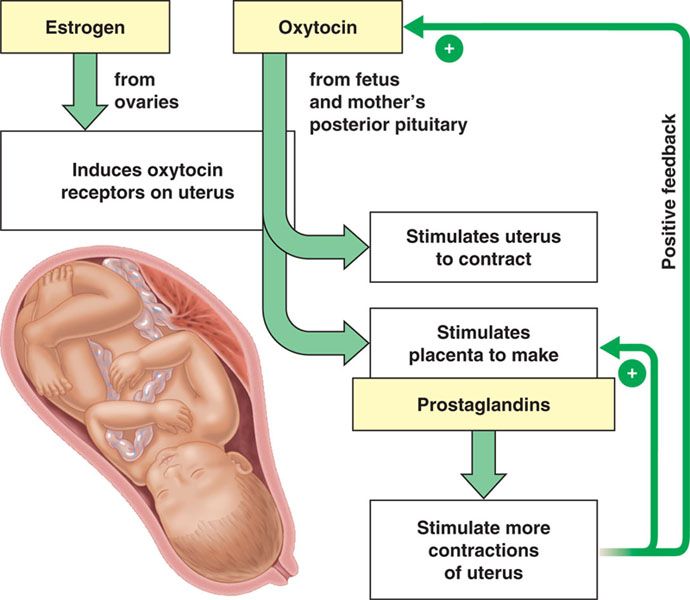
If a health care provider recommends labor induction, it's typically because the benefits outweigh the risks. If you're pregnant, understanding why and how labor induction is done can help you prepare.
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Book: Mayo Clinic Guide to a Healthy Pregnancy
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
To determine if labor induction is necessary, a health care provider will likely evaluate several factors. These include the mother's health and the status of the cervix. They also include the baby's health, gestational age, weight, size and position in the uterus. Reasons to induce labor include:
- Nearing 1 to 2 weeks beyond the due date without labor starting (postterm pregnancy).
- When labor doesn't begin after the water breaks (prelabor rupture of membranes).
- An infection in the uterus (chorioamnionitis).

- When the baby's estimated weight is less than the 10th percentile for gestational age (fetal growth restriction).
- When there's not enough amniotic fluid surrounding the baby (oligohydramnios).
- Possibly when diabetes develops during pregnancy (gestational diabetes), or diabetes exists before pregnancy.
- Developing high blood pressure in combination with signs of damage to another organ system (preeclampsia) during pregnancy. Or having high blood pressure before pregnancy, developing it before 20 weeks of pregnancy (chronic high blood pressure) or developing the condition after 20 weeks of pregnancy (gestational hypertension).
- When the placenta peels away from the inner wall of the uterus before delivery — either partially or completely (placental abruption).
- Having certain medical conditions. These include heart, lung or kidney disease and obesity.
Elective labor induction is the starting of labor for convenience when there's no medical need. It can be useful for women who live far from the hospital or birthing center or who have a history of fast deliveries.
It can be useful for women who live far from the hospital or birthing center or who have a history of fast deliveries.
A scheduled induction might help avoid delivery without help. In such cases, a health care provider will confirm that the baby's gestational age is at least 39 weeks or older before induction to reduce the risk of health problems for the baby.
As a result of recent studies, women with low-risk pregnancies are being offered labor induction at 39 to 40 weeks. Research shows that inducing labor at this time reduces several risks, including having a stillbirth, having a large baby and developing high blood pressure as the pregnancy goes on. It's important that women and their providers share in decisions to induce labor at 39 to 40 weeks.
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Risks
Uterine incisions used during C-sections
Uterine incisions used during C-sections
A C-section includes an abdominal incision and a uterine incision. After the abdominal incision, the health care provider will make an incision in the uterus. Low transverse incisions are the most common (top left).
After the abdominal incision, the health care provider will make an incision in the uterus. Low transverse incisions are the most common (top left).
Labor induction carries various risks, including:
- Failed induction. An induction might be considered failed if the methods used don't result in a vaginal delivery after 24 or more hours. In such cases, a C-section might be necessary.
- Low fetal heart rate. The medications used to induce labor — oxytocin or a prostaglandin — might cause the uterus to contract too much, which can lessen the baby's oxygen supply and lower the baby's heart rate.
- Infection. Some methods of labor induction, such as rupturing the membranes, might increase the risk of infection for both mother and baby. The longer the time between membrane rupture and labor, the higher the risk of an infection.
-
Uterine rupture. This is a rare but serious complication in which the uterus tears along the scar line from a prior C-section or major uterine surgery.
 Rarely, uterine rupture can also occur in women who have not had previous uterine surgery.
Rarely, uterine rupture can also occur in women who have not had previous uterine surgery.An emergency C-section is needed to prevent life-threatening complications. The uterus might need to be removed.
- Bleeding after delivery. Labor induction increases the risk that the uterine muscles won't properly contract after giving birth, which can lead to serious bleeding after delivery.
Labor induction isn't for everyone. It might not be an option if:
- You've had a C-section with a classical incision or major uterine surgery
- The placenta is blocking the cervix (placenta previa)
- Your baby is lying buttocks first (breech) or sideways (transverse lie)
- You have an active genital herpes infection
- The umbilical cord slips into the vagina before delivery (umbilical cord prolapse)
If you have had a C-section and have labor induced, your health care provider is likely to avoid certain medications to reduce the risk of uterine rupture.
How you prepare
Labor induction is typically done in a hospital or birthing center. That's because mother and baby can be monitored there, and labor and delivery services are readily available.
What you can expect
During the procedure
There are various ways of inducing labor. Depending on the circumstances, the health care provider might use one of the following ways or a combination of them. The provider might:
-
Ripen the cervix. Sometimes prostaglandins, versions of chemicals the body naturally produces, are placed inside the vagina or taken by mouth to thin or soften (ripen) the cervix. After prostaglandin use, the contractions and the baby's heart rate are monitored.
In other cases, a small tube (catheter) with an inflatable balloon on the end is inserted into the cervix. Filling the balloon with saline and resting it against the inside of the cervix helps ripen the cervix.
- Sweep the membranes of the amniotic sac.
 With this technique, also known as stripping the membranes, the health care provider sweeps a gloved finger over the covering of the amniotic sac near the fetus. This separates the sac from the cervix and the lower uterine wall, which might help start labor.
With this technique, also known as stripping the membranes, the health care provider sweeps a gloved finger over the covering of the amniotic sac near the fetus. This separates the sac from the cervix and the lower uterine wall, which might help start labor. -
Rupture the amniotic sac. With this technique, also known as an amniotomy, the health care provider makes a small opening in the amniotic sac. The hole causes the water to break, which might help labor go forward.
An amniotomy is done only if the cervix is partially dilated and thinned, and the baby's head is deep in the pelvis. The baby's heart rate is monitored before and after the procedure.
- Inject a medication into a vein. In the hospital, a health care provider might inject a version of oxytocin (Pitocin) — a hormone that causes the uterus to contract — into a vein. Oxytocin is more effective at speeding up labor that has already begun than it is as at cervical ripening.
 The provider monitors contractions and the baby's heart rate.
The provider monitors contractions and the baby's heart rate.
How long it takes for labor to start depends on how ripe the cervix is when the induction starts, the induction techniques used and how the body responds to them. It can take minutes to hours.
After the procedure
In most cases, labor induction leads to a vaginal birth. A failed induction, one in which the procedure doesn't lead to a vaginal birth, might require another induction or a C-section.
By Mayo Clinic Staff
Related
Products & Services
Induction of labor or induction of labor
The purpose of this informational material is to familiarize the patient with the induction of labor procedure and to provide information on how and why it is performed.
In most cases, labor begins between the 37th and 42nd weeks of pregnancy. Such births are called spontaneous. If drugs or medical devices are used before the onset of spontaneous labor, then the terms "stimulated" or "induced" labor are used in this case.
Labor should be induced when further pregnancy is for some reason unsafe for the mother or baby and it is not possible to wait for spontaneous labor to begin.
The purpose of stimulation is to start labor by stimulating uterine contractions.
When inducing labor, the patient must be in the hospital so that both mother and baby can be closely monitored.
Labor induction methods
The choice of labor induction method depends on the maturity of the cervix of the patient, which is assessed using the Bishop scale (when viewed through the vagina, the position of the cervix, the degree of its dilatation, consistency, length, and the position of the presenting part of the fetus in the pelvic area are assessed). Also important is the medical history (medical history) of the patient, for example, a past caesarean section or operations on the uterus.
The following methods are used to induce (stimulate) labor:
- Oral misoprostol is a drug that is a synthetic analogue of prostaglandins found in the body.
 It prepares the body for childbirth, under its action the cervix becomes softer and begins to open.
It prepares the body for childbirth, under its action the cervix becomes softer and begins to open. - Balloon Catheter - A small tube is placed in the cervix and the balloon attached to the end is filled with fluid to apply mechanical pressure to the cervix. When using this method, the cervix becomes softer and begins to open. The balloon catheter is kept inside until it spontaneously exits or until the next gynecological examination.
- Amniotomy or opening of the fetal bladder - in this case, during a gynecological examination, when the cervix has already dilated sufficiently, the fetal bladder is artificially opened. When the amniotic fluid breaks, spontaneous uterine contractions will begin, or intravenous medication may be used to stimulate them.
- Intravenously injected synthetic oxytocin - acts similarly to the hormone of the same name produced in the body. The drug is given by intravenous infusion when the cervix has already dilated (to support uterine contractions).
 The dose of the drug can be increased as needed to achieve regular uterine contractions.
The dose of the drug can be increased as needed to achieve regular uterine contractions.
When is it necessary to induce labor?
Labor induction is recommended when the benefits outweigh the risks.
Induction of labor may be indicated in the following cases:
- The patient has a comorbid condition complicating pregnancy (eg, high blood pressure, diabetes mellitus, preeclampsia, or some other condition).
- The duration of pregnancy is already exceeding the norm - the probability of intrauterine death of the fetus increases after the 42nd week of pregnancy.
- Fetal problems, eg, problems with fetal development, abnormal amount of amniotic fluid, changes in fetal condition, various fetal disorders.
- If the amniotic fluid has broken and uterine contractions have not started within the next 24 hours, there is an increased risk of inflammation in both the mother and the fetus. This indication does not apply in case of preterm labor, when preparation of the baby's lungs with a special medicine is necessary before delivery.
- Intrauterine fetal death.
What are the risks associated with labor induction?
Labor induction is not usually associated with significant complications.
Occasionally, after receiving misoprostol, a patient may develop fever, chills, vomiting, diarrhea, and too frequent uterine contractions (tachysystole). In case of too frequent contractions to relax the uterus, the patient is injected intravenously relaxing muscles uterus medicine. It is not safe to use misoprostol if you have had a previous caesarean section as there is a risk of rupture of the uterine scar.
The use of a balloon catheter increases the risk of inflammation inside the uterus.
When using oxytocin, the patient may rarely experience a decrease in blood pressure, tachycardia (rapid heartbeat), hyponatremia (lack of sodium in the blood), which may result in headache, loss of appetite, nausea, vomiting, abdominal pain, depression strength and sleepiness.
Induction of labor, compared with spontaneous labor, increases the risk of prolonged labor, the need for instrumentation
(use of vacuum or forceps), postpartum hemorrhage, uterine rupture, the onset of too frequent uterine contractions and the associated deterioration of the fetus, prolapse umbilical cord, as well as premature detachment of the placenta.
If induction of labor is not successful
The time frame for induction of labor varies from patient to patient, on average labor begins within 24-72 hours. Sometimes more than one method is required.
The methods used do not always work equally quickly and in the same way on different patients. If the cervix does not dilate as a result of induction of labor, your doctor will tell you about your next options (which may include inducing labor later, using a different method, or delivering by caesarean section).
ITK833
This informational material was approved by the Women's Clinic on 01/01/2022.
Tutta Larsen - about sex two days before giving birth - Moscow 24, 14.09.2016
September 14, 2016, 18:18
Society
Hello everyone from Tutta Larsen! We always discuss issues of pregnancy and childbirth: Where and with whom is it better to give birth? What vitamins and nutrition do we need during pregnancy? But what to do if the due date has come up, and the baby still does not want to be born? This topic is very exciting for many mothers. What to do if you are overstepping? Are there any secrets to speed up the process?
I had such a situation with my youngest son Vanya, the date of birth approached, but he was in no hurry to appear. This is such a moment when the question "Well, when will you give birth already?" just haunts you. Of course, I know that there are many ways that are advised to bring the date of birth closer - walk the stairs, mop the floors, some even advise drinking champagne, and, of course, having sex with your spouse.
There are doctors who really recommend this method of accelerating labor and, in principle, there is a scientific justification for this - semen contains chemical elements that help the maturation of the cervix and thus prepare the body for the birth of a child, being a natural stimulant. In addition, lovemaking gives a woman the opportunity to relax, let go of thoughts and fears of childbirth, which also helps speed up the process.
I must say right away that for me sex a few days before giving birth is not an option. Personally, I did not consider this method for myself in order to bring the birth of the baby closer. It seems to me that my body is already fully tuned "to the exit", and not to the "input", I personally was set up completely differently and did not want anything from my spouse at all.
Tutta Larsen. Photo: Lara Bardina
However, we still had our own life hack in this situation. My doctor advised me to watch comedies and have a good laugh. On the same evening, my husband and I watched two cool French films, including the well-known Beaver to complain tears laughed, and at night they went to give birth. Probably, laughter promotes relaxation, the release of endorphins and the mother's body gives the child a signal that it is ready for childbirth.
On the same evening, my husband and I watched two cool French films, including the well-known Beaver to complain tears laughed, and at night they went to give birth. Probably, laughter promotes relaxation, the release of endorphins and the mother's body gives the child a signal that it is ready for childbirth.
If a couple nevertheless decides to use such a pleasant way as making love to speed up the birth, then you need to be aware of the possible risks. Closer to the date of the appearance of the baby, the mucous plug that protects the fetus from infections may move away and not prevent the infection from entering the uterine cavity. Those bacteria that are not normally pathogenic during this period can be dangerous to the fetus and this is not my personal horror story - some doctors are of this opinion.
Of course, if you're overwearing for a long time, then it's better to turn to professionals. If the period is short, then it is worth remembering that childbirth is a joint attitude and readiness of both mother and child.