Procedure for turning a breech baby
External cephalic version (ECV) | Pregnancy Birth and Baby
External cephalic version (ECV) | Pregnancy Birth and Baby beginning of content4-minute read
Listen
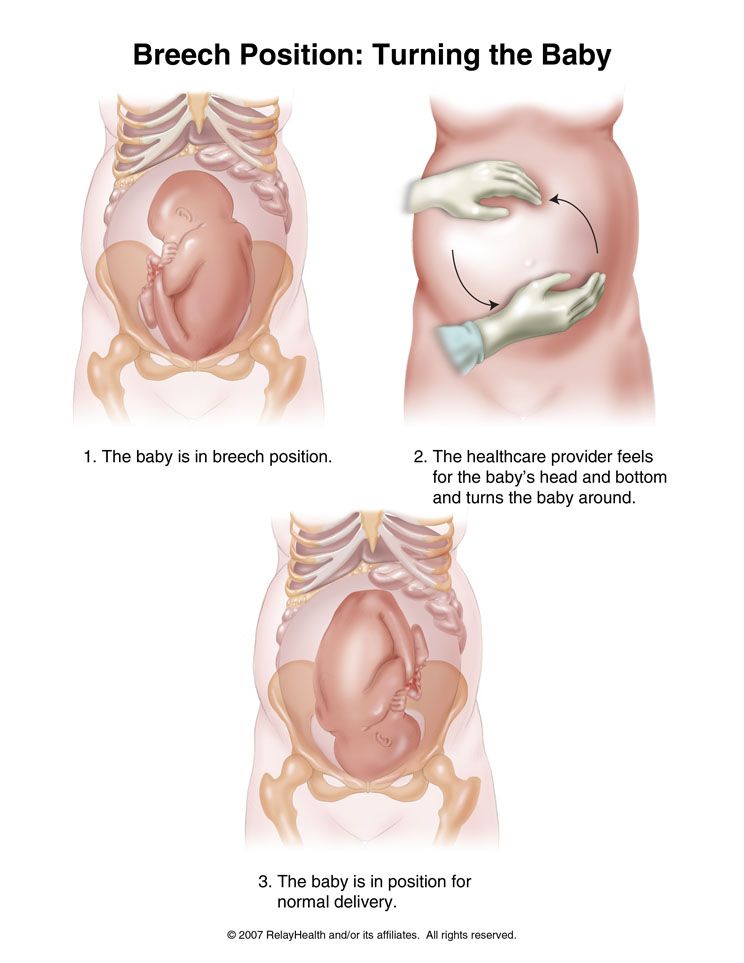
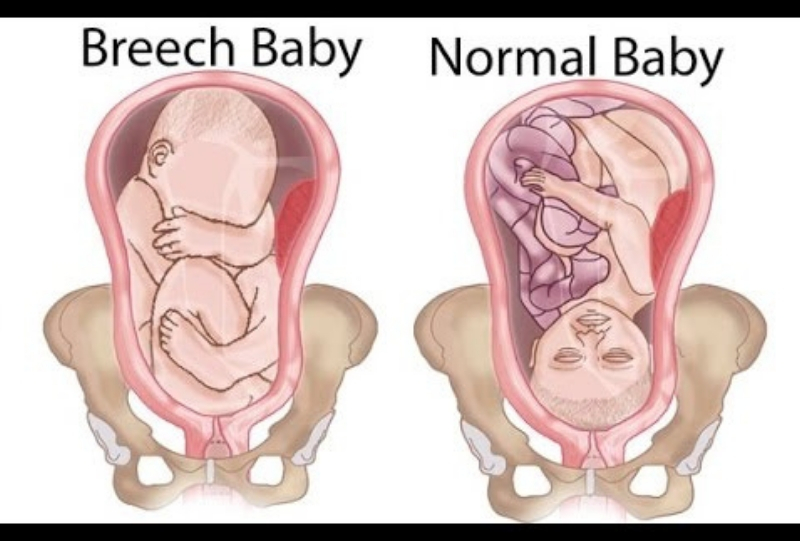
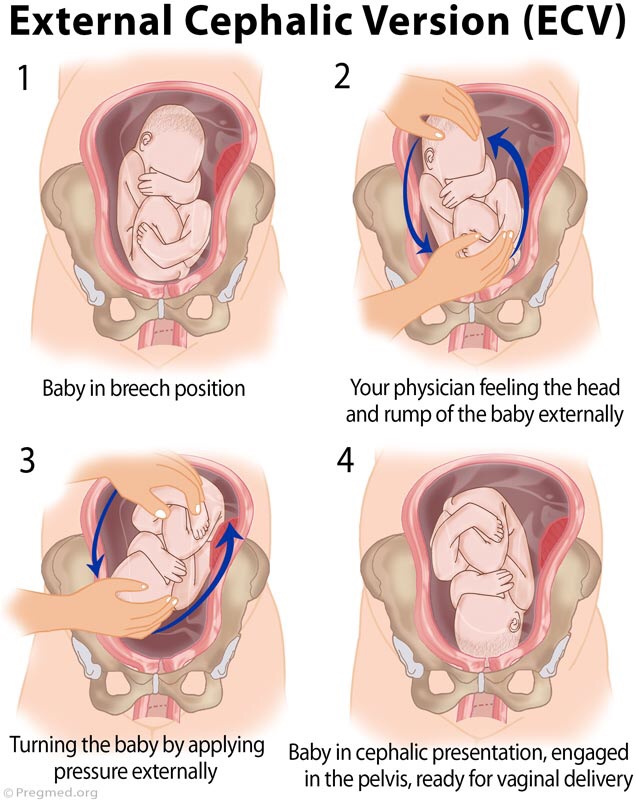
Giving birth is more challenging for babies who are bottom-down, or breech, when labour starts. This page explains external cephalic version (ECV), which tries to turn breech babies to the head-down position ready for a normal vaginal birth.
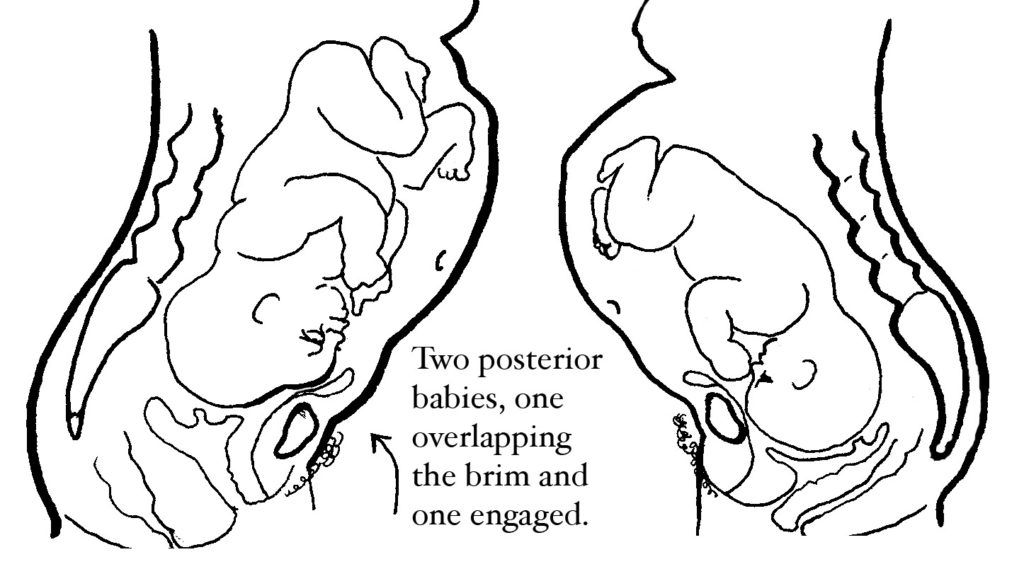
The breech position
Throughout your pregnancy, your baby repeatedly turns around and changes position. Most babies will settle into a head-down, or 'cephalic', position by 36 weeks of pregnancy. But about 3 in 100 babies are in a breech position at 36 weeks. For these babies, birth would be more difficult than if they were in the cephalic position.
Some breech babies turn naturally in the last month of pregnancy. If this is your first baby, the chance of the baby turning itself after 36 weeks is about 1 in 8. If this is your second or subsequent baby, the chance is about 1 in 3.
If your baby is still in a breech position at 36 weeks, your doctor or midwife might suggest you consider an external cephalic version, or ECV. The aim is to turn your baby so that it is head-down when labour starts.
An ECV is performed after 37 weeks of pregnancy.
Can anyone have an ECV?
Most women can have an ECV if they have a healthy pregnancy with a normal amount of amniotic fluid. However, an ECV is not recommended if:
- you need a caesarean for other reasons
- you have had vaginal bleeding in the previous 7 days
- the baby's heart rate is not normal
- a complicated pregnancy
- you are having twins or triplets
- you have an unusually shaped uterus
- you recently had vaginal bleeding
- you have placenta praevia (your placenta is growing close to, or on, your cervix)
- other health conditions, like high blood pressure or diabetes
ECV might also not be recommended if your unborn baby is unwell or not growing well.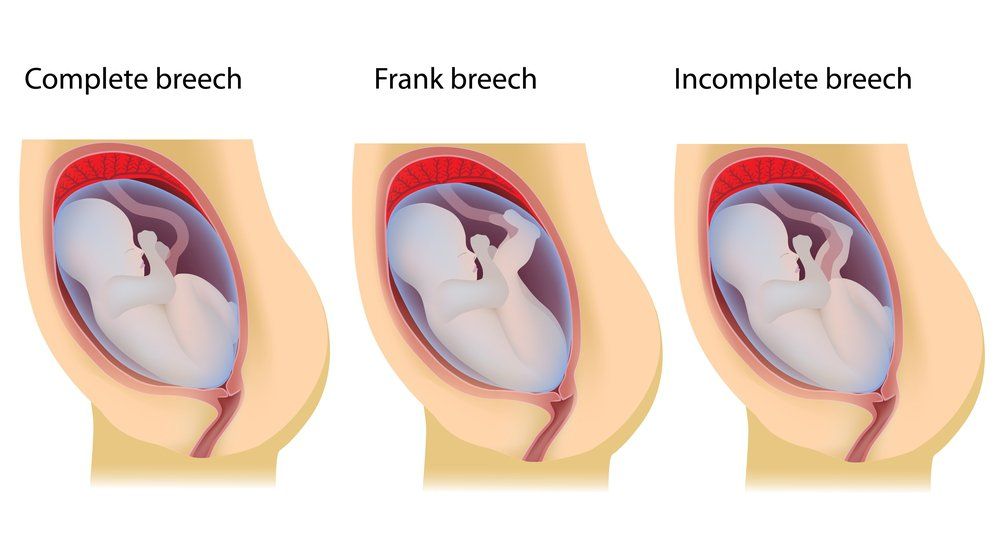
If you have had a caesarean section before, an ECV can still be performed but there are special considerations that need to be discussed with your doctor.
How is an ECV performed?
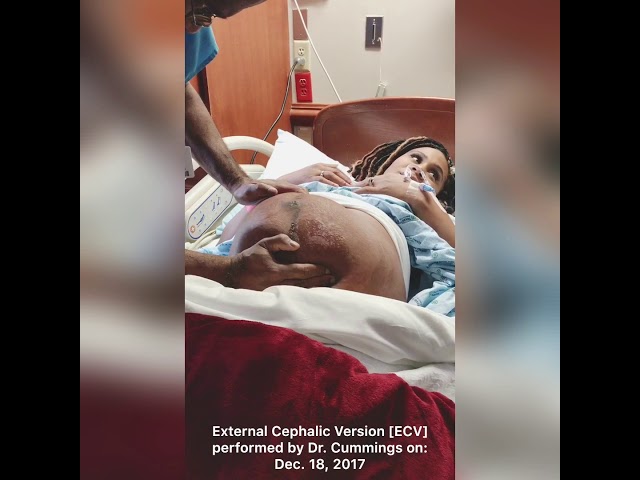
A health professional with appropriate expertise, usually an obstetrician, puts their hands on your abdomen to try to turn your baby into a head-down position.
A cardiotocograph, or CTG, will monitor your baby’s wellbeing for 20 to 30 minutes before the procedure.
A small needle will be inserted into your hand so that medication to relax your uterus can be administered directly into your vein.
An obstetrician will then perform an ultrasound to confirm the position of the baby, and then attempt to turn the baby by pressing their hands firmly on your abdomen. Some women find this uncomfortable, while others don’t. The pressure on your abdomen lasts a few minutes. If the first attempt is unsuccessful, the obstetrician might try again.
The CTG might be applied again after the procedure to assess your baby’s wellbeing before you leave.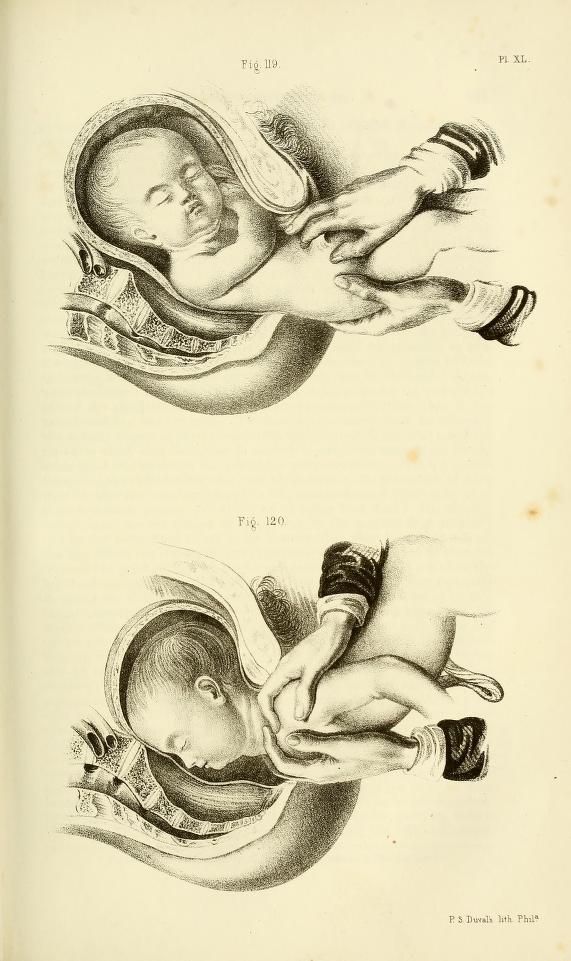
It usually takes about 3 hours from start to finish.
Where would I have an ECV?
Although complications from an ECV are rare, it is recommended that the procedure is done by an experienced health professional, in a hospital where there are facilities for emergency caesarean section. About 1 in 1,000 women go into labour after an ECV. About 1 in 200 women need an immediate caesarean section.
Will ECV work?
ECV can work, although there is no guarantee of success. If it does work, there is a small chance the baby will turn again to the breech position. But overall, ECV improves a woman’s chances of having a vaginal birth.
What happens if ECV doesn’t work?
A vaginal birth may still be possible, depending on your individual clinical circumstances and the type of breech position your baby is in. Talk to your doctor or midwife about your options.
What other methods are there to potentially turn my baby from a breech position?
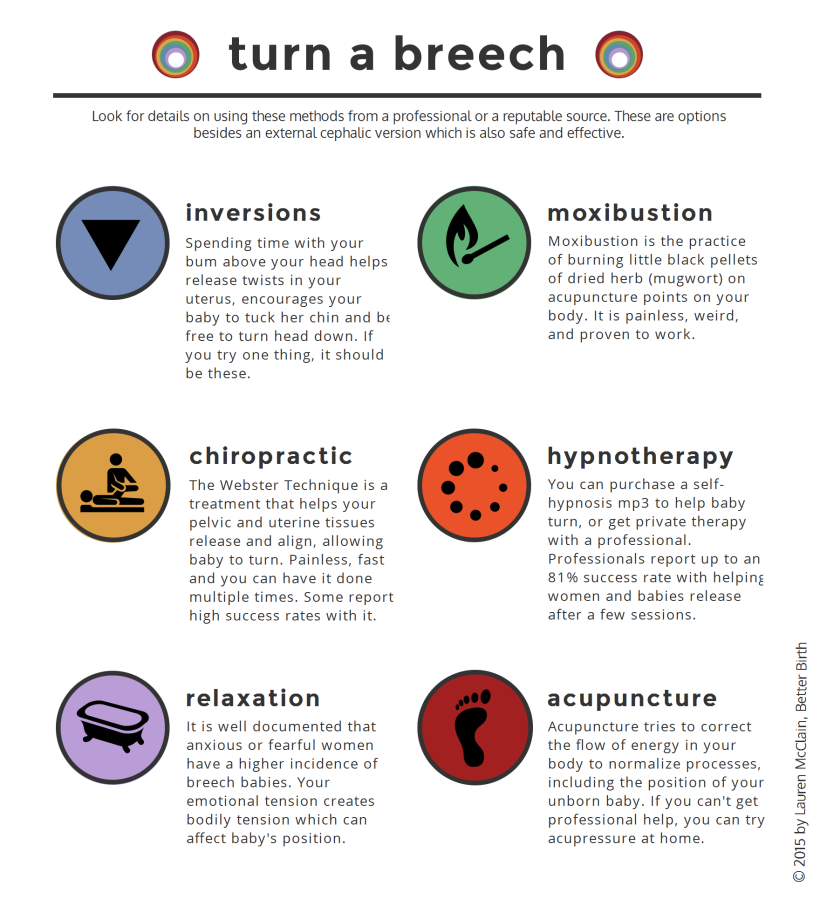
Some people think that you might be able to encourage your baby to turn by holding yourself in certain positions, such as kneeling with your bottom in the air and your head and shoulders flat to the ground.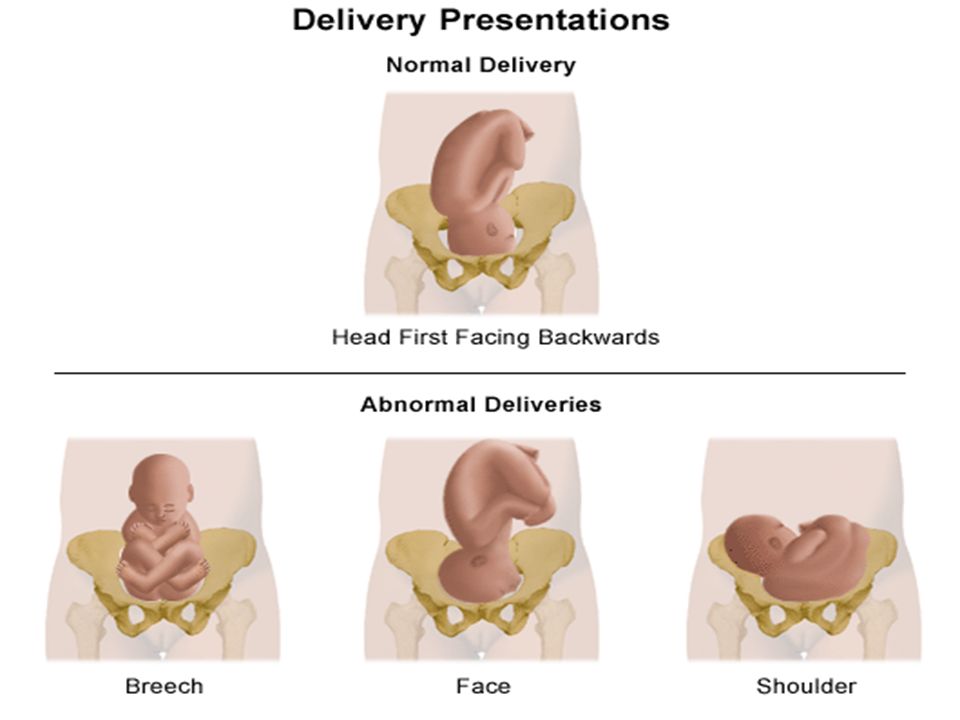 Other options you might hear include acupuncture, a Chinese herb called moxibustion and chiropractic treatment. There is no good evidence that these work. Discuss with your doctor or midwife before having any treatment during pregnancy.
Other options you might hear include acupuncture, a Chinese herb called moxibustion and chiropractic treatment. There is no good evidence that these work. Discuss with your doctor or midwife before having any treatment during pregnancy.
Sources:
Mater Hospital Brisbane (Pregnancy: External Cephalic Version), Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Breech Presentation at the End of your Pregnancy), BioMed Central (Does moxibustion work? An overview of systematic reviews (BMC Research Notes 20103:284)), Department of Health (Clinical practice guidelines: Pregnancy care), SA Department for Health and Ageing (Perinatal practice guideline: Breech presentation), NSW Health (External Cephalic Version (ECV) for Breech Presentation)Learn more here about the development and quality assurance of healthdirect content.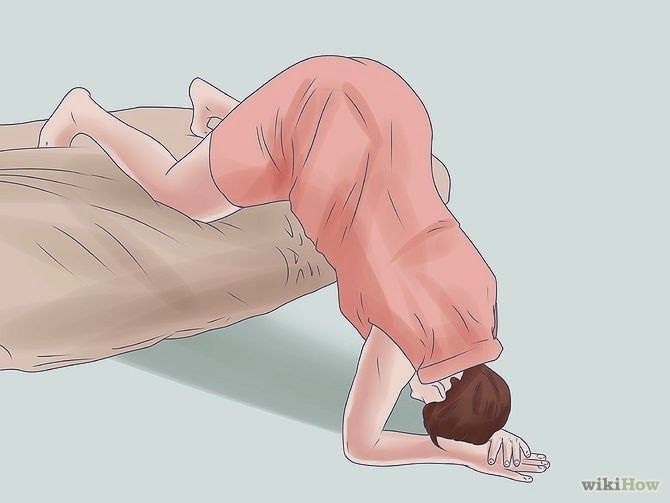
Last reviewed: April 2020
Back To Top
Related pages
- Breech birth
- Breech pregnancy
Need more information?
External Cephalic Version for Breech Presentation - Maternal, child and family health
This information brochure provides information about an External Cephalic Version (ECV) for breech presentation
Read more on NSW Health website
Breech presentation and turning the baby
In preparation for a safe birth, your health team will need to turn your baby if it is in a bottom first ‘breech’ position.
Read more on WA Health website
Breech pregnancy
When a baby is positioned bottom-down late in pregnancy, this is called the breech position.
Read more on Pregnancy, Birth & Baby website
Labour complications
Even if you’re healthy and well prepared for childbirth, there’s always a chance of unexpected problems. Learn more about labour complications.
Read more on Pregnancy, Birth & Baby website
Malpresentation
Malpresentation is when your baby is in an unusual position as the birth approaches. Sometimes it’s possible to move the baby, but a caesarean maybe safer.
Read more on Pregnancy, Birth & Baby website
Pregnancy at week 35
You'll probably be having lots of Braxton Hicks contractions by now. It's your body's way of preparing for the birth. They should stop if you move position.
They should stop if you move position.
Read more on Pregnancy, Birth & Baby website
Anatomy of pregnancy and birth - pelvis
The pelvis helps carry your growing baby and is especially tailored for vaginal births. Learn more about the structure and function of the female pelvis.
Read more on Pregnancy, Birth & Baby website
Rhesus D negative in pregnancy
Find out what being Rhesus D negative could mean for your baby and how it is treated.
Read more on Pregnancy, Birth & Baby website
Placental abruption - Better Health Channel
betterhealth.vic.gov.au
Read more on Better Health Channel website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.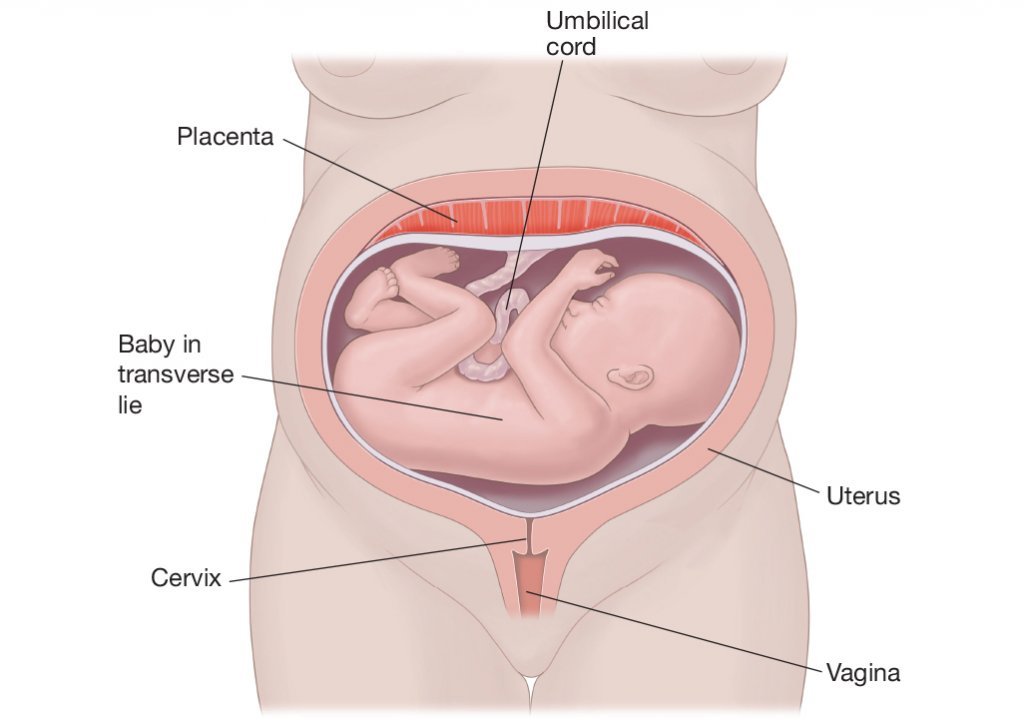
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari.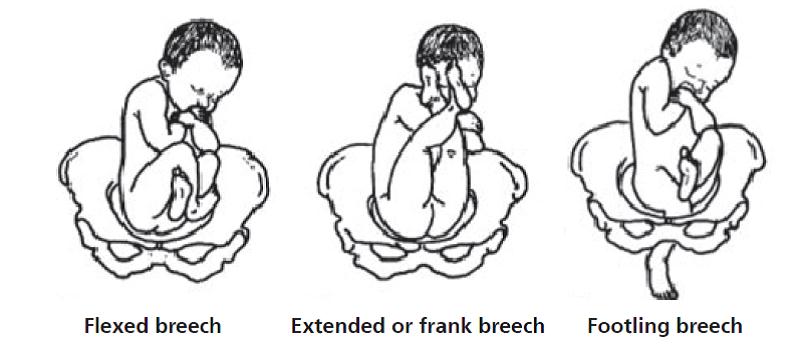 For more information, please visit the links below:
For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
What Is It, Procedure, Risks, Labor, & More
External Cephalic Version: What Is It, Procedure, Risks, Labor, & MoreMedically reviewed by Holly Ernst, PA-C — By Becky Young on April 12, 2018
What is external cephalic version?
An external cephalic version is a procedure used to help turn a baby in the womb before delivery. During the procedure, your healthcare provider places their hands on the outside of your belly and attempts to manually turn the baby.
This procedure may be recommended if your baby is in a breech position. This means that their bottom or feet are pointing down toward the vagina, and their head is at the top of your uterus, near your rib cage. A vaginal breech birth is more complicated than a birth where the baby is head down, so it’s preferable that baby is head down before labor starts.
A vaginal breech birth is more complicated than a birth where the baby is head down, so it’s preferable that baby is head down before labor starts.
Some women opt to birth their babies via cesarean delivery (C-section) rather than attempt a vaginal breech birth if they’re near or past their estimated due date and the baby still hasn’t turned.
Is it safe?
Most women who are 37 weeks pregnant with a baby in the breech position are candidates for an external cephalic version. The procedure has been found to be successful in turning these babies into a head-down position in around 50 percent of cases. Since breech babies often result in C-sections, a successful external cephalic version may reduce your need for this type of delivery, which is considered an abdominal surgery.
There are some situations in which your healthcare providers may suggest an external cephalic version isn’t right for you. This procedure may not be right for you if:
- you’re already in labor or experiencing any vaginal bleeding
- you’ve had any issues with your placenta during the pregnancy
- there are signs of or concerns for fetal distress
- you are pregnant with more than one baby, such as twins or triplets
- you have any structural abnormalities in your uterus, like large fibroids
Your healthcare provider may also advise against the procedure if you’ve had a previous C-section, your baby is suspected to be larger than average, or you have low or high levels of amniotic fluid. These risk factors are based upon clinical opinion, so you should talk with your healthcare provider to see what they recommend based on your individual pregnancy.
These risk factors are based upon clinical opinion, so you should talk with your healthcare provider to see what they recommend based on your individual pregnancy.
You discuss external cephalic version between 34 and 37 weeks of pregnancy with your doctor if your baby is noted to be breech. Babies often turn on their own before 34 weeks, so there is no need to attempt the procedure earlier in the pregnancy.
The procedure does increase your risk for premature labor and fetal distress. For that reason, most healthcare providers recommend waiting until you’re at term, or 37 weeks pregnant, to attempt this procedure. That reduces risk for complications in your baby if you do need to deliver shortly following the procedure.
You can also talk with your doctor about waiting past 37 weeks, as the baby may spontaneously turn to a head-down position.
The most common risk with an external cephalic version is a temporary change in your baby’s heart rate, which occurs in about 5 percent of cases. Serious complications are extremely rare but can include the need for emergency C-section, vaginal bleeding, loss of amniotic fluid, and umbilical cord prolapse.
Serious complications are extremely rare but can include the need for emergency C-section, vaginal bleeding, loss of amniotic fluid, and umbilical cord prolapse.
What to expect during the procedure
The procedure will normally be performed by an obstetrician. During an external cephalic version, your doctor will place their hand on your belly to physically push the baby into the optimal position. The procedure usually takes around 5 minutes and your baby’s heart rate will be monitored before, during, and after the procedure. If your doctor suspects your baby isn’t responding well to the procedure, it will be stopped.
Many women report that the procedure is uncomfortable, but medications can be used to reduce the amount of pain felt. Using certain medications during the procedure may also increase the chances of successfully turning the baby. This may be because the medication helps your muscles and uterus relax, allowing the healthcare provider to successfully turn the baby more easily.
How will this procedure affect labor and delivery?
If an external cephalic version is successful, then most of the time labor progresses in a regular way following the procedure. The procedure doesn’t generally affect the length of your labor.
There is a small risk that the procedure will rupture membranes e. This can mean that you will begin labor earlier than you might otherwise have done, and your contractions may be more intense from the beginning of labor instead of building in intensity as the labor progresses.
If the procedure is unsuccessful and your baby remains in the breech position, you could opt for a C-section or choose to attempt a vaginal breech delivery.
One of the main risks involved with a vaginal breech delivery is that your baby’s head could become trapped in the birth canal. The other serious concern is umbilical cord prolapse. With umbilical cord prolapse, the umbilical cord leaves your body before your baby. That increases the risk of the cord becoming compressed during delivery, which cuts off the baby’s supply of oxygen and nutrients.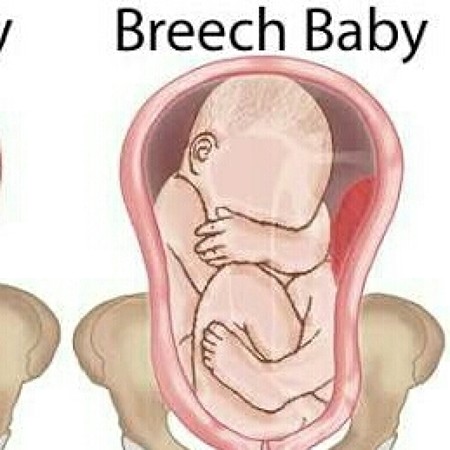
Both of these complications are a medical emergency. Evidence does show an increased risk of perinatal mortality in planned vaginal breech birth as opposed to a C-section with breech presentation.
Are there other ways to turn the baby?
There are a number of different exercises you can try to attempt to turn your baby from the breech position, though these haven’t been proven in studies to be effective in spontaneously turning the breech baby. Always talk to your healthcare provider before trying these exercises to make sure that they are safe for your pregnancy.
Hip tilt
- Lie on the floor in front of a sofa or chair, with your feet on the sofa or chair. Place cushions under your hips to offer additional support. Your hips should be elevated about 1.5 feet above your head, and your body should be at a 45-degree angle.
- Hold this position for 10 to 15 minutes, three times a day. It’s best to do this when your baby is active.
Pelvic rotations
- Stand or sit on an exercise or birthing ball.
- Once you are in position, gently rotate your hips clockwise in a circular movement. Repeat 10 rotations.
- Switch directions, rotating your hips counterclockwise for 10 rotations.
- Repeated three times a day
Rocking back and forth
- Place your hands and knees on the floor.
- Keeping your hands and knees in place, gently rock your body back and forth.
- Do this for 15 minutes. Repeat up to three times a day.
Walk or swim
- Walk, swim, or engage in another low-impact exercise.
- Do this for 30 minutes a day. Staying active may help your baby move out of the breech position.
The takeaway
It’s recommended that an external cephalic version be offered to all women who have a baby in breech position at or close to term, where there are no other complications. The procedure has been shown to be successful in around half of all cases and may lower the likelihood that a C-section will be needed. There are some possible risks, so be sure to discuss the risks and benefits with your healthcare provider before moving forward with this procedure.
There are some possible risks, so be sure to discuss the risks and benefits with your healthcare provider before moving forward with this procedure.
Last medically reviewed on April 12, 2018
- Parenthood
- Pregnancy
- 3rd Trimester
How we vetted this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Berhan Y, et al. (2015). The risks of planned vaginal breech delivery versus planned caesarean section for term breech birth: A meta-analysis including observational studies. DOI:
10.1111/1471-0528.13524 - Grootscholten K, et al. (2008). External cephalic version-related risks: A meta-analysis [Abstract]. DOI:
10. 1097/AOG.0b013e31818b4ade
1097/AOG.0b013e31818b4ade - Kathpalia BSK, et al. (2012). Outcome of external cephalic version in breech presentation. DOI:
10.1016/S0377-1237(12)60036-7 - Kuppens SM, et al. (2017). Fetal heart rate abnormalities during and after external cephalic version: Which fetuses are at risk and how are they delivered? DOI:
10.1186/s12884-017-1547-6 - Lim PS, et al. (2014). Successful external cephalic version: Factors predicting vaginal birth. DOI:
10.1155/2014/860107 - Wang Z-H, et al. (2017). Remifentanil analgesia during external cephalic version for breech presentation in nulliparous women at term: A randomized controlled trial. DOI:
10.1097/MD.0000000000006256 - What happens if your baby is breech? (2017).
nhs.uk/conditions/pregnancy-and-baby/breech-birth/
Share this article
Medically reviewed by Holly Ernst, PA-C — By Becky Young on April 12, 2018
related stories
What Is Back Labor and What Causes It?
Can You Turn a Transverse Baby?
What You Need to Know If Your Baby Is in an Oblique Lie
Is It Safe to Use Exercise to Induce Labor?
How Early Can You Safely Give Birth?
Read this next
What Is Back Labor and What Causes It?
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
Back labor can happen when your baby's head is against your cervix.
 We'll tell you what it's like and how to manage it.
We'll tell you what it's like and how to manage it.READ MORE
Can You Turn a Transverse Baby?
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
As you near the end of your pregnancy, you may worry that your baby's transverse position will cause issues during delivery. Learn more about possible…
READ MORE
What You Need to Know If Your Baby Is in an Oblique Lie
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
An oblique lie is a fetal position in which baby's head is just to the side of the pelvic inlet. It presents some challenges, but there are ways to…
READ MORE
Is It Safe to Use Exercise to Induce Labor?
Medically reviewed by Michael Weber, MD
If you’re pregnant and past your due date, you might wonder if exercising will help induce labor.
 Here’s the truth.
Here’s the truth. READ MORE
How Early Can You Safely Give Birth?
Medically reviewed by Meredith Wallis, MS, APRN, CNM, IBCLC
Not all babies arrive on their due dates — in fact, most don't. So how many weeks early is safe to give birth? Learn more about why certain weeks are…
READ MORE
These Guided Pregnancy Journals Will Help You Document All the Feels
Medically reviewed by Meredith Wallis, MS, APRN, CNM, IBCLC
The pregnancy and postpartum periods are full of emotions (rightfully so!), and these pregnancy journals are a great place to document it all.
READ MORE
What You Need to Know If You’re Having a High Risk Pregnancy
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
A high risk pregnancy is any pregnancy that comes with increased health risks for either the pregnant parent, the fetus, or both.
READ MORE
What Are Conjoined Twins?
Conjoined twins are identical twins who are born connected and likely share one or more organs. We explain how they develop and when separation is…
READ MORE
The Acupressure Points for Inducing Labor
Medically reviewed by Debra Sullivan, Ph.D., MSN, R.N., CNE, COI
Are you pregnant and past your due date? Help induce labor naturally by pressing on these acupressure points along the body.
READ MORE
Support for the Non-Birthing Partner after Stillbirth
Medically reviewed by Matthew Boland, PhD
The grief that accompanies stillbirth or infant loss isn’t reserved for the birthing parent — partners also feel this loss deeply.
READ MORE
The problem of breech presentation of the fetus.
 External obstetric rotation of the fetus on the head.
External obstetric rotation of the fetus on the head. Breech presentation of the fetus occurs in 3% -5% of cases at full-term pregnancy. Vaginal delivery with breech presentation is associated with high risks both on the mother's side and on the fetus's side. Thus, breech presentation is currently considered pathological, even if the conditions necessary for childbirth through the birth canal are ideally met, and the fetus is relatively small relative to the size of the mother's pelvis. During vaginal delivery, the arms and head of the fetus may tilt back, which can lead to injury.
Currently the most common method of delivery in breech presentation is a caesarean section (90%). Among the indications for the use of caesarean section, breech presentation ranks third among others in the world. However, this the operation does not make it possible to completely eliminate the risk of trauma to the fetus, since when it is removed, it is also possible to tilt the arms and head of the fetus, and their release requires the use of complex manipulations.
To correct breech presentation today, the world is using EXTERNAL OBTETAL TURNING OF THE FETUS ON THE HEAD proposed at the end the century before last by the Russian obstetrician Arkhangelsky B.A.
External obstetric cephalic rotation (EFRT) is a procedure during which the doctor turns the fetus from the outside through the wall of the uterus breech presentation in the head. A successful attempt at NAPP allows women to give birth on their own, avoiding a caesarean section.
What is required for external cephalic fetal rotation?
External obstetric rotation of the fetus on the head is performed before the onset of labor, usually starting from 36 weeks of pregnancy.
It is necessary to consult a doctor and conduct an ultrasound examination to confirm the fact breech presentation of the fetus and determine the conditions for NAPP, starting from 34-35 weeks of pregnancy.
| The operation of external rotation of the fetus on the head in breech presentation |
When NAPP is possible:
- From 36 to 37 weeks, since with earlier use, it is likely that it will return to the breech presentation.

- In the presence of a singleton pregnancy.
- Subject to the mobility of the buttocks of the fetus (if they are tightly pressed against the entrance to the mother's pelvis, it will be extremely difficult to change the position of the fetus).
- Sufficient amount of amniotic fluid. With oligohydramnios, this manipulation can be traumatic for the fetus, while with polyhydramnios there is a high probability of a reverse rotation of the fetus in a breech presentation.
- Sufficient amount of amniotic fluid. With oligohydramnios, this manipulation can be traumatic for the fetus, while with polyhydramnios there is a high probability of a reverse rotation of the fetus in a breech presentation.
- Fetal head flexed
When NAPP is not possible:
- With the outflow of amniotic fluid.
- If the patient has contraindications to the use of drugs used to relax the uterus (tocolysis).

- In the presence of obstetric indications or indications from the health of the mother for delivery by caesarean section.
- With the extensor position of the fetal head.
- If the fetus has congenital developmental features.
- With multiple pregnancy.
- In the presence of structural features of the uterus in a pregnant woman
However, in addition to this, there are a number of factors that may favor or, on the contrary, serve as a contraindication to external obstetric turning the fetus on the head, and which can only be determined by a doctor during a direct examination of a pregnant woman.
How NAPP is conducted
For manipulation, hospitalization in the maternity hospital is necessary. Preliminarily, an additional examination of the pregnant woman is carried out in the required volume, including ultrasound.
During the NAPP:
Immediately before the start of the manipulation, a CTG is recorded to assess the condition of the fetus.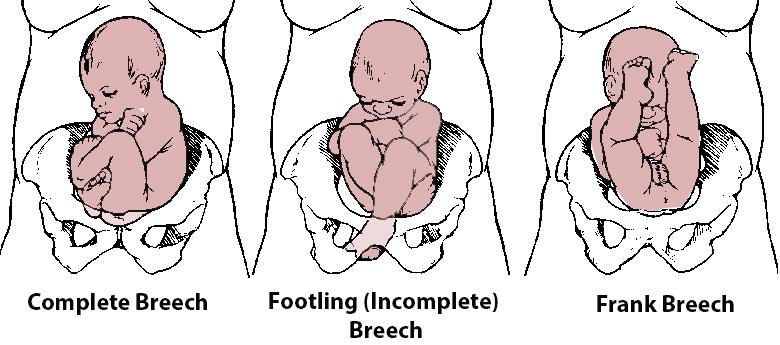
Drugs that prevent uterine contractions (tocolytics) are administered.
Further, under constant ultrasound and KGT control, as well as the continued administration of drugs that relax the uterus, the doctor performs a turn.
Holding both hands on the surface of the pregnant woman's abdomen, one on the head of the fetus, and the other on the buttocks of the fetus, the doctor pushes and rotates the fetus to the upside down position. A pregnant woman may feel some discomfort during the procedure. The degree of discomfort depends on the individual sensitivity of each patient.
After the procedure is successfully completed, the CTG is recorded again, to make sure that the fetus feels well and has successfully undergone the procedure. Usually, during the day, the condition of the mother and fetus is monitored, after which the patient is discharged and continues the pregnancy until spontaneous delivery occurs.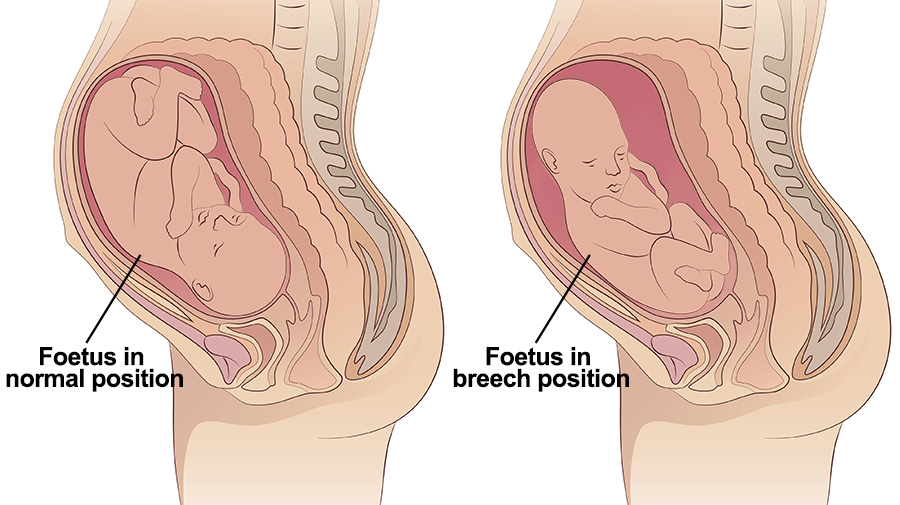
If the doctor notices a deterioration in the condition of the fetus according to the monitoring data, then the procedure is immediately stopped.
If the first attempt was not successful, your doctor may suggest another attempt if the fetus is in good health.
APP is performed ONLY in a maternity ward where there is an opportunity for an emergency delivery, if necessary.
Risks associated with NAPP
Subject to constant monitoring of the condition of the fetus, constant tocolysis (administration of drugs that relax the uterus) The risks associated with this procedure are minimal. Complications from its use occur in less than 1-2% of cases.
Complications of NAPP include:
- compression or "twisting" of the umbilical cord. In this case, constant monitoring of the fetal condition allows you to immediately fix its deterioration and stop the procedure.
- discharge of amniotic fluid or the development of labor.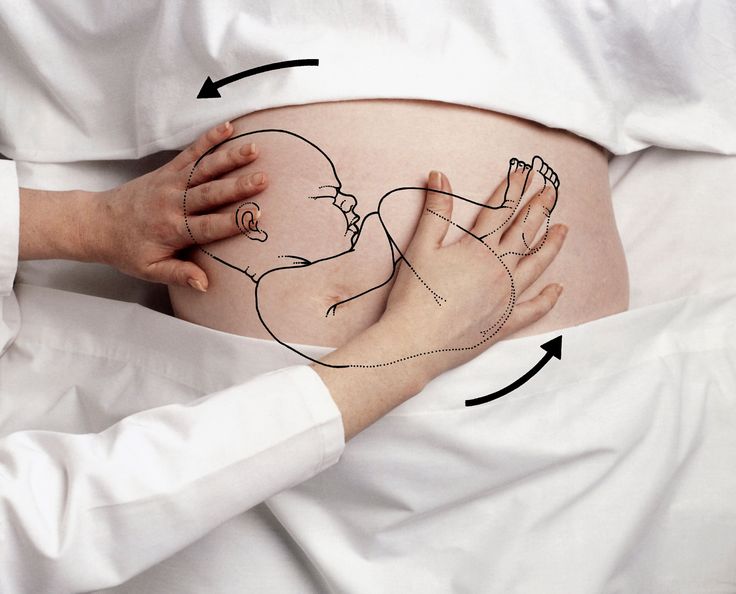 This complication can be considered relative, since the rotation in most cases is carried out at full-term pregnancy.
This complication can be considered relative, since the rotation in most cases is carried out at full-term pregnancy.
Any deviation from the normal course of the procedure serves as a reason to stop the manipulation and decide on the choice of further management tactics.
Carrying out NAPP with Rh-negative mother's blood.
The presence of Rh isoimmunization (that is, the presence of anti-Rh antibodies in the mother's blood) is a contraindication to this procedure, as it increases the risk of anemia in the fetus.
In the absence of isoimmunization (absence of anti-Rhesus antibodies) it is possible to carry out NAPP with prophylaxis by introducing anti-Rhesus immunoglobulin.
If you have a breech presentation of the fetus and you want to know about further options for pregnancy management, delivery, external obstetric rotation of the fetus on the head, the presence of indications and contraindications for its implementation, please consult our specialists.
consequences for the child in case of incorrect position
January 18, 2022
January 18
5 minutes
5 minutes
45705
36
6
Breech presentation for most expectant mothers is a very disturbing moment - how the child will be born, is a caesarean section always indicated in such cases, what complications are possible. Let's answer these and many other questions in this article.
Breech presentation of the fetus is one of the options for the location of the child in the uterus of the mother. If we could look into a woman's belly, we would see a child who seems to be "sitting" in the uterus, and his head is pointing up. Normally, breech presentation lasts up to 32 weeks, and then the baby, as a rule, turns over and directs the head to the birth canal.
Article content
- Can a woman determine the presentation of the fetus?
- What is breech presentation
- Common causes of presentation
- How to determine breech presentation
- What to do to make the child roll over
- What can a woman do
- What can an obstetrician do
- What can a doctor do
- FAQ
Can a woman identify fetal presentation?
Only an experienced doctor who leads the pregnancy can determine the breech presentation, and the assumption is confirmed with the help of ultrasound.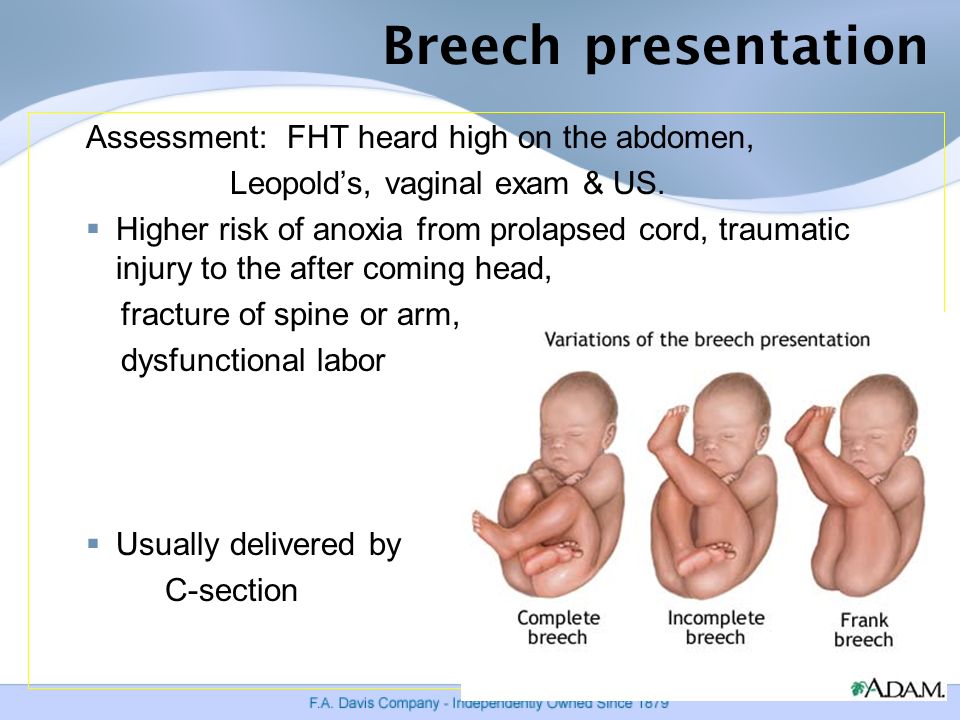
In the event that the baby is positioned “incorrectly”, the doctor may recommend special exercises to turn the baby over into the optimal position for childbirth. This is important, because it is at 32-34 weeks that you need to undergo an examination and make sure that the baby has taken the right direction.
What is breech presentation
Doctors distinguish two types of breech presentation:
| Gluteal | In such a situation, during childbirth at the birth of a baby, the buttocks are the first to be born. The legs are located along the body. This option is the most favorable, rarely gives complications, so childbirth is most often carried out naturally. |
| foot | At birth, the legs appear first, such a presentation. |
Common causes of presentation
Of course, any expectant mother has a question - why does breech presentation occur. There are many reasons for this, the main ones are:
There are many reasons for this, the main ones are:
- multiple pregnancy - when there are two or three babies in the uterus, it is difficult for them to move and turn over head down
- polyhydramnios - in such a situation, the baby can move a lot and simply not take the correct position before childbirth
- oligohydramnios - in a situation where there is little amniotic fluid, the child simply cannot take the correct position
- cord entanglement
- fibroids or other diseases of the uterus
How to determine breech presentation
It is impossible to independently determine the position of the child.
To understand what kind of presentation a child has, you can use:
| Visual examination and palpation of the abdomen by an experienced specialist | So he determines where the head is and where the legs of the fetus are |
| Feeling the baby through the vagina | This method is used if a woman has entered an emergency delivery and is already in them. |
| ultrasound | The most reliable way to determine the position of the baby. The procedure is carried out at 32-34 weeks, when the baby takes its final position |
Example
A pregnant woman at 38 weeks was diagnosed with breech presentation. The woman was advised certain exercises in order to delicately turn the fetus over. The task was unsuccessful, so the specialist tried to make an obstetric coup, however, this did not lead to the desired result. As a result, the doctor decided to carry out the delivery by surgery and perform a caesarean section. The operation was successful, mother and child are doing well.
How to make a child roll over
In this matter, three directions need to be considered: what the woman herself can do, what her obstetrician-gynecologist can do, and what the doctor in charge of childbirth can do.
What a woman can do
Let's figure out what may depend on the future mother herself, and what she can do.
- First, tune in a positive way. The state of the child largely depends on the psychological state of the mother, so it is not recommended to be nervous and anxious.
- Second, talk to your child and ask him to roll over. Skeptics may scoff at such advice, but experienced psychologists and obstetricians say that this method works.
- And finally, do special exercises, for example, turns. Starting position - lying on your back, legs slightly bent at the knees. Gently and smoothly, without jerking, you need to turn on your right side and lie down in this position for 2 minutes. After that, roll over to your left side and also lie down. Repeat 5 times for each side. All movements should be as delicate as possible.
What an obstetrician can do
If mom did not succeed in stimulating the coup, this is absolutely normal. At a period of more than 35 weeks, an obstetrician takes over, who tries to make the so-called obstetric coup.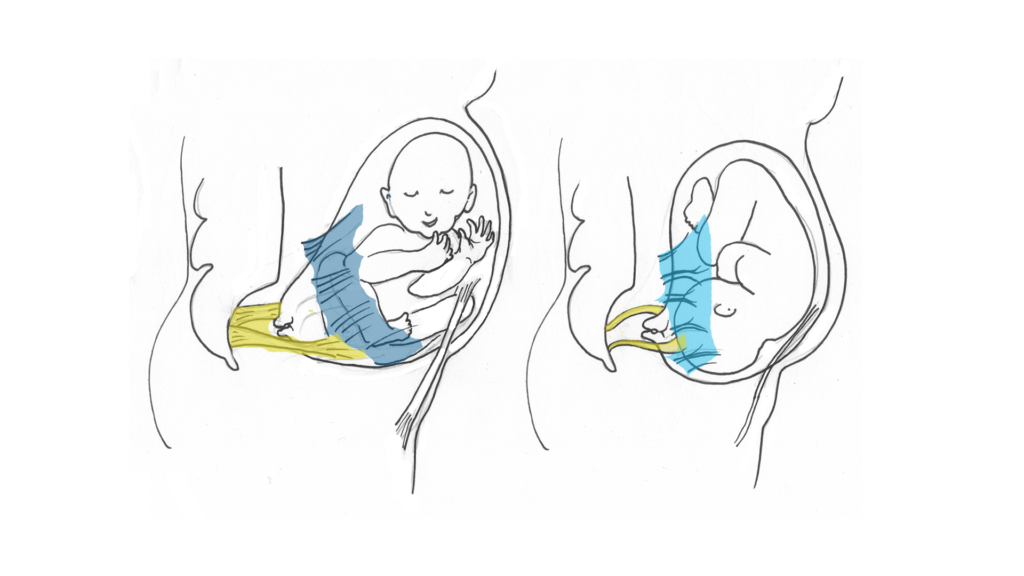 During the procedure, with the help of special manipulations, he acts on the woman's stomach, trying to give the fetus the optimal position for childbirth. However, it is impossible not to notice that most of the babies "inverted by the midwife" will soon return to the breech presentation.
During the procedure, with the help of special manipulations, he acts on the woman's stomach, trying to give the fetus the optimal position for childbirth. However, it is impossible not to notice that most of the babies "inverted by the midwife" will soon return to the breech presentation.
What a doctor can do
Quite often, in order to reduce the risks for both the mother and her baby, the doctor decides to perform a caesarean section. However, many women give birth naturally.
The choice of birth management is always personalized, taking into account the individual characteristics of the mother and her child. It is important to choose a good specialist at the initial stage of pregnancy.
FAQ
Breech presentation of the fetus at the 20th week of pregnancy - is it dangerous?
+
Absolutely not. We begin to talk about the fact that breech presentation is a conditional pathology no earlier than 32 weeks. Until this time, the child may roll over, and sometimes more than once. I will say even more - at this time the child is most often located with his legs down and this is absolutely normal.
Until this time, the child may roll over, and sometimes more than once. I will say even more - at this time the child is most often located with his legs down and this is absolutely normal.
Foot presentation - is it the wrong position of the fetus?
+
What gestational age are we talking about? Initially, the child “tumbles” in his mother’s stomach, then most often he is just the same in a foot or breech presentation, when his legs are down and his head is up. And only closer to childbirth, a coup usually occurs and the child is located head down - at the entrance to the birth canal. If this does not happen, we can talk about the breech / foot / breech presentation.
What are the consequences of breech presentation for a child?
+
In general, with the correct management of childbirth, there will be no negative consequences for the child. He can suffer only if the doctor chooses the wrong method of obstetric care.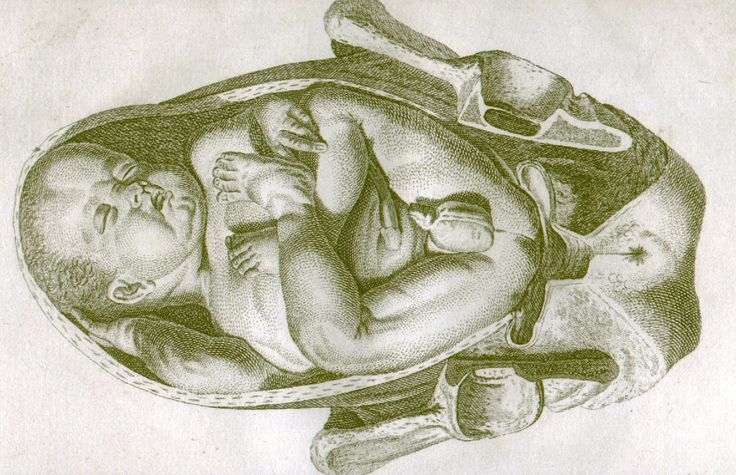 In all other respects, there are no problems, the fetus develops absolutely normally.
In all other respects, there are no problems, the fetus develops absolutely normally.
How to understand that the child turned upside down?
+
The position of the child in the womb can only be determined by a competent specialist. The most effective and reliable method is ultrasound.
And is there an unstable position of the fetus?
+
The fetus rotates many times during the entire pregnancy, at the end of the third trimester it usually turns head down and takes this position until delivery. However, it also happens that the child rolls over several times. In this case, we can talk about the unstable position of the fetus.
What is an obstetric revolution?
+
During the procedure, with the help of special manipulations, he acts on the woman's stomach, trying to give the fetus the optimal position for childbirth.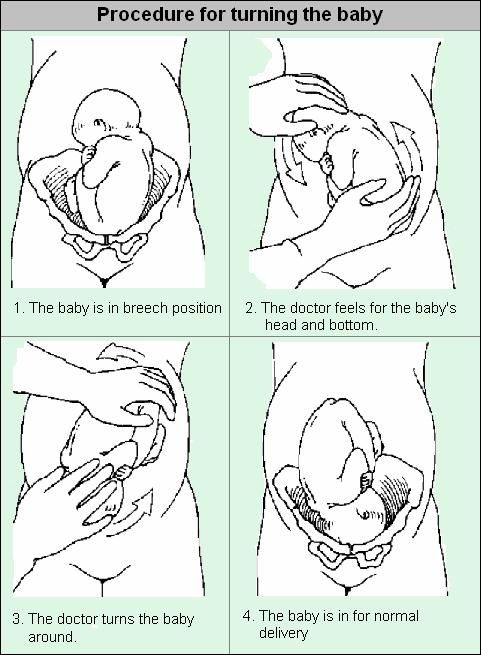 However, it is impossible not to notice that most of the babies "inverted by the midwife" will soon return to the breech presentation.
However, it is impossible not to notice that most of the babies "inverted by the midwife" will soon return to the breech presentation.
Breech presentation of the fetus at 34 weeks of gestation - normal or pathological?
+
Breech presentation at this time is not a "final verdict." the baby can still roll over. If this does not happen, the doctor will assess the size and position of the child closer to the MDD and decide on the tactics of childbirth.
How to understand if the child turned upside down?
+
You yourself will not be able to understand this, or at least be sure that the coup has happened. I would recommend that you do an ultrasound - with the help of this study it will become known in which presentation your baby is.
We publish only verified information
Article author
Menshikova Maria Viktorovna obstetrician-gynecologist
Experience 38 years
Consultations 1816
Art. 46
46
Specialist with extensive practical experience. He has a certificate of a mammologist, a certificate of professional certification. Participates in foreign business trips and individual training programs (Los Angeles).
- 1982 - 1986 NPO MONIIAG - obstetrician-gynecologist
- 1987 - 1989 VNITs OZMIR - obstetrician-gynecologist
- 1989 - 1992 departmental polyclinic st. Moscow - Kurskaya - obstetrician-gynecologist
- 1992 - 2001 NPO MONIIAG - obstetrician-gynecologist
- 2007 - 2008 NP KMIKM - doctor administrator
- 2009 - 2013 Pereslavl Central District Hospital, women's consultation - obstetrician-gynecologist
- 2020 to present LLC Teledoctor24 - doctor - consultant (gynecologist)
Sources
- ... Savelyeva G.M., Shalina R.I., Panina O.B.
 "Obstetrics" - M .: "GEOTAR - Media", 2010
"Obstetrics" - M .: "GEOTAR - Media", 2010 - ... Chernukha E.A., Puchko T.K. "Pelvic presentation of the fetus", a guide for doctors - M .: "GEOTAR - Media", 2007
- ... Clinical protocol "Management of pregnancy and childbirth in breech presentation of the fetus" // Institute of Health and Family. Project "Mother and Child" - 2011
Share:
Category: Pregnancy and childbirth
About health Pregnancy and childbirth About children healthy lifestyle Psychology Neurology Gastroenterology Personal care Medicines and dietary supplementsPrevious article
Salt room
Next article
Diastasis after childbirth
Other related articles
Monakhova Albina Petrovna
14.