White nipple breastfeeding pain
Extremely Sore Nipples? Nipples Changing Colour After Breastfeeding? Could it Be Vasospasm?
Most people will not have heard of the term vasospasm. It is a rather cool sounding name, but, unfortunately, it often brings a lot of pain with it...
Share this content
Vasospasm is not exceedingly common but this definitely happens to a few women. In this blog, we will discuss nipple blanching and vasospasm as they are separate issues, which can often be mistaken for the same thing.
What is Nipple Blanching?
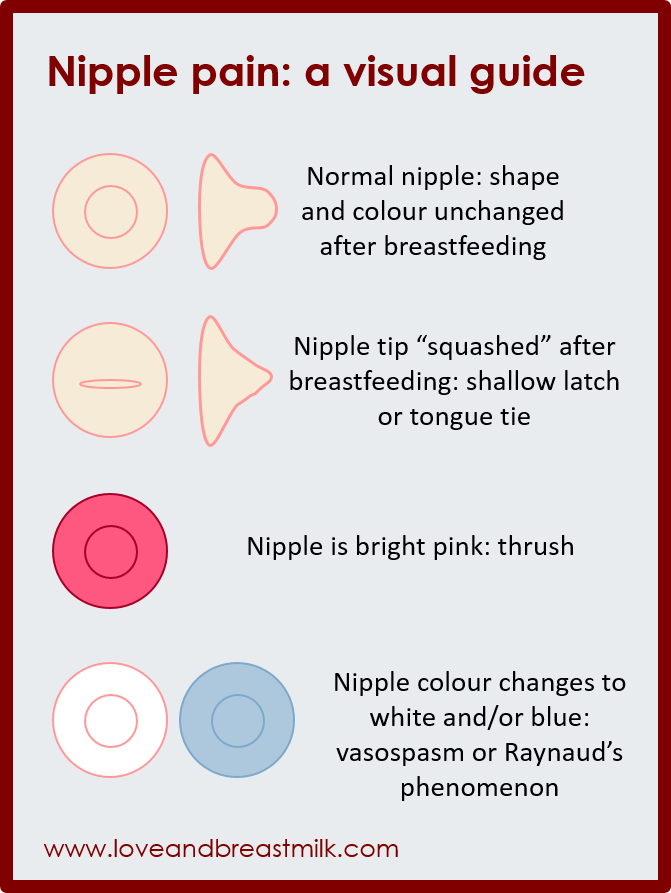
Nipple Blanching happens when the nipple comes out from your baby’s mouth whitened and misshapen. The most frequent reason for this is due to your baby compressing your nipple during a breastfeed.
When you notice your nipple is white after breastfeeding, you may see that the end of the nipple is also flattened, creased or pointed; imagine the shape of a new lipstick – that’s a misshapen nipple!
Your nipple should always come out of baby’s mouth the same shape it went in, but, maybe a little elongated.
You may find that pain in your nipple increases several seconds to a few minutes after the feed.
Nipple blanching can be due to:
- Incorrect attachment at your breast
- Your baby clamping down on your nipple in order to slow down your fast flow of milk
- Your baby may have a tongue-tie (your lactation consultant will be able to assess for this)
- There may be certain oral palate variations (your lactation consultant will be able to assess for this)
It is really important to seek help with breastfeeding from a lactation consultant or your maternal child health nurse to enable you and bub to find a way to solve this for you. This way you will be able to go on enjoying your feeding time together.
What is Vasospasm?
A condition known as Raynaud’s phenomenon, where your fingers turn white when they are cold can also affect the nipples.
Pain can occur during, immediately after, or even between breastfeeds. You may notice that your nipple turns white. Then, you will often see the nipple change colour again; from white to blue to red as the blood flow returns to the nipple.
You may notice that your nipple turns white. Then, you will often see the nipple change colour again; from white to blue to red as the blood flow returns to the nipple.
Vasospasm due to Raynaud’s is more likely to occur on both nipples.
Vasospasm tends to last for longer periods of time than nipple blanching and does not go away even with good attachment at the breast during feeds.
Cold is usually the trigger for vasospasm. This happens when your baby stops breastfeeding and pulls off the breast exposing your nipple to the cooler air.
The pain from vasospasm can be mild or severe, and may be in the form of sharp or burning pains and throbbing.
Vasospasm is often mistaken for thrush of the nipple because of the similarities in how women describe the pain. But the colour change in the nipple tends to make it clearer when it is vasospasm rather than thrush.
What Can You Do if You Think You May Be Suffering from Vasospasm?
First, seek help from a lactation consultant to check your breastfeeding attachment and suggest nipple vasospasm treatment. Your lactation consultant can also check for any nipple damage, infections or thrush of the nipple.
Your lactation consultant can also check for any nipple damage, infections or thrush of the nipple.
Try and keep your nipples warm. Here are a few options that may help:
- Using a warm heat pack on your nipples straight after feeding
- Placing a pair of clean warm socks in your bra
- Purchasing some Breast Warmers which reflect your own body heat through the reflective material in the Breast Warmers
- Wearing an extra layer of clothes
- Avoiding exposing your nipples to “air” them
Massaging your nipple with olive oil when you are feeling pain is helpful for some women.
Avoid caffeine, nicotine, diet pills and cold medications containing pseudoephedrine or phenylephrine, beta blockers, and other vasoconstrictive drugs. These can all make your symptoms worse.
Oral contraceptives containing estrogen have also been associated with vasospasm, so, it is important to discuss this further with your GP or Gynaecologist.
There are some supplements which have been shown to help vasospasm and may be appropriate to look further into if the above recommendations are not working:
- Magnesium tablets help to relax the blood vessels.
 It is advisable to speak to a naturopath to discuss the best dose. This can be done in the health store.
It is advisable to speak to a naturopath to discuss the best dose. This can be done in the health store. - Fish oil capsules or evening primrose oil may also improve blood vessel relaxation.
- Dietary supplementation with a vitamin B complex that includes B6 and niacin may help.
- Ibuprofen for may be helpful for pain management.
Some women may need to discuss this further with their GP or lactation consultant. If none of the above is helping they may need to take a prescription medicine of low dose oral nifedipine to relieve the vasospasm.
The good news is that vasospasm can be treated and you will be able to go on breastfeeding, pain free.
Please reach out to health professionals qualified in breastfeeding support to gain the best information and support for vasospasm and nipple blanching.
If you have suffered with vasospasm or nipple blanching share your thoughts and comments with us on our Medela Australia Facebook page.
Why do my nipples turn white when I breastfeed?
Have you been finding breastfeeding painful and noticing that your nipples are turning white? You could be experiencing nipple blanching.
Do your nipples turn white—and maybe even hurt—during breastfeeding? This is called nipple blanching and can be caused by a few different things. It’s usually a result of blood flow to your nipple being restricted, often because your baby is compressing your nipples because the latch is too shallow, your baby is tongue-tied, or your milk lets down so quickly that she clamps down in an attempt to slow the flow. With this type of blanching, your nipple might also look flattened, creased or pointed when your baby comes off the breast. And for some moms, it can be quite painful.
Nipple blanching can also be caused by vasospasms, a tightening of the blood vessels due to lack of blood flow and oxygen that usually occurs during and right after breastfeeding, when the baby comes off the breast. This is typically caused by latch issues, and it can be extremely painful, often searing at first, then throbbing. “Vasospasms could be your body’s reaction to the fact that your nipples were damaged early on by latch issues or, in some cases, even thrush,” says Pam Davey, a certified doula and registered lactation consultant. They will eventually go away, but you’ll need to seek professional help to correct the problem causing it, and it can take a long time for the nipple damage to heal.
This is typically caused by latch issues, and it can be extremely painful, often searing at first, then throbbing. “Vasospasms could be your body’s reaction to the fact that your nipples were damaged early on by latch issues or, in some cases, even thrush,” says Pam Davey, a certified doula and registered lactation consultant. They will eventually go away, but you’ll need to seek professional help to correct the problem causing it, and it can take a long time for the nipple damage to heal.
Often, the key to both preventing and stopping nipple blanching from compression or vasospasm is as simple as improving the latch, says Nathalie Pambrun, vice-president of the Canadian Association of Midwives, who recommends getting help from a lactation consultant. “In the case of vasospasm, you can relieve the symptoms by keeping your body warm to avoid blood vessel constriction during nursing, and applying a hot washcloth or dry heat with a blow dryer set on low to your breasts afterwards.”
“In the case of vasospasm, you can relieve the symptoms by keeping your body warm to avoid blood vessel constriction during nursing, and applying a hot washcloth or dry heat with a blow dryer set on low to your breasts afterwards.”
10 ways to prevent and treat sore nipples
Another, although less common, cause of nipple blanching is Raynaud’s disease. This condition affects both men and women and isn’t related to being pregnant or breastfeeding. In addition to white nipples after nursing, you might have cold fingers, toes, lips or ears, changes in skin colour in response to cold or stress, and a tingling or throbbing feeling when circulation returns after a few minutes or a few hours. Blanching in this case comes with severe and searing pain, which are also symptoms of thrush and so it is often misdiagnosed. A doctor can do a blood test for the disease and, in more severe cases, may prescribe a medication to widen your blood vessels and increase circulation. To relieve symptoms of Raynaud’s, breastfeed in warm environments and wearing warm clothing, prevent a temperature change by covering your breasts with your shirt or your hand as soon as your baby has finished nursing, apply dry heat with a blow dryer set on low, or massage your nipples with olive oil to help return blood flow and soothe any lingering pain or discomfort.
To relieve symptoms of Raynaud’s, breastfeed in warm environments and wearing warm clothing, prevent a temperature change by covering your breasts with your shirt or your hand as soon as your baby has finished nursing, apply dry heat with a blow dryer set on low, or massage your nipples with olive oil to help return blood flow and soothe any lingering pain or discomfort.
Don’t hesitate to contact a lactation consultant or your doctor if you’re experiencing blanching or pain while nursing.
Read more:
How to handle oversupply and overactive letdown
How do I know my baby’s getting enough breast milk?
Stay in touch
Subscribe to Today's Parent's daily newsletter for our best parenting news, tips, essays and recipes.- Email*
- CAPTCHA
- Consent*
Yes, I would like to receive Today's Parent's newsletter. I understand I can unsubscribe at any time.
 **
**
FILED UNDER: Breastfeeding breastfeeding problems Maternal health sore nipples
Nursing nipple care | Breast Care
Breastfeeding is good for you and your baby, but it can be a real challenge for the nipples. Check out our tips and tricks to help reduce the pain.
Share this information
Sioned Hilton, health visitor, neonatal nurse and lactation consultant:
A mother of three, Sioned Hilton has been supporting families with newborns and young children for over 30 years. She provides advice on breastfeeding and pumping, both in clinics and at home. In addition, Schoned writes articles for parenting magazines, attends conferences, and conducts seminars for attending physicians.
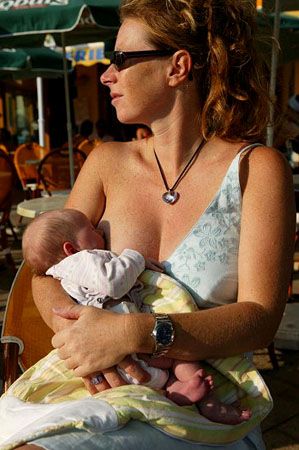
New mothers often hear: "Breastfeeding doesn't have to be painful." However, in the early days, many are faced with the opposite.
In most women during pregnancy, the nipples enlarge and become more sensitive. When a newborn baby begins to suckle, it creates a certain pressure, and this is a completely new and unfamiliar sensation for a woman (at least for a first-time mother).
When a newborn baby begins to suckle, it creates a certain pressure, and this is a completely new and unfamiliar sensation for a woman (at least for a first-time mother).
Feedings can be prolonged for a long time, sometimes up to an hour, and the child may ask to be breastfed up to 13 times a day. 1 This sucking, pressure and saliva of the baby can cause sore nipples.
Remember how your lips crack in the wind and sun. The more often you lick them, the more they will dry and become inflamed. Therefore, lips require good hydration to soften, protect and speed up the healing of cracks. The same thing happens with nipples.
However, sore nipples usually don't last more than a couple of weeks and go away as your baby and your breasts get used to breastfeeding. It is important to start nipple care as early as possible to prevent the situation from worsening. Therefore, if your nipples become very inflamed, crack or bleed, contact your doctor as soon as possible. 2
2
Prevention is better than cure, so check out our tips.
Check your baby's latch-on
Correct latch is the key to pain-free breastfeeding. When putting the baby to the breast, point the nipple towards his palate. This will allow him to grab the nipple and the part of the areola (the darker skin around the nipple) underneath. When the nipple and part of the breast is in the baby's mouth, feeding is taking place correctly. 3
For the first few days, see a lactation consultant or specialist to check for proper latch. He will be able to give you advice on how to solve problems and recommend other feeding positions that will make it less painful for you to feed your baby.
Check tongue tie
Tongue tie (ankyloglossia) occurs in 4-11% of
newborns. 4 At the same time, the strip of skin that attaches the tongue to the bottom of the mouth - the so-called frenulum - is too short. A child with a shortened frenulum will not be able to open his mouth wide enough to latch onto the breast well, and his tongue will not cover the lower gum when sucking. As a result, the baby will be nervous, and your nipples may become inflamed.
As a result, the baby will be nervous, and your nipples may become inflamed.
The doctor or lactation consultant must examine the baby to make this diagnosis. The problem of a shortened bridle is solved by a simple undercutting procedure. It is performed by a doctor, and is usually done without blood and does not require anesthesia. Cutting the bridle allows you to restore the normal feeding mechanism almost instantly. 5
Less common in children is a short frenulum of the upper lip. In this case, it is necessary to dissect the skin that connects the upper lip to the gum. A shortened frenum of the tongue or upper lip in a newborn is not always detected during the examination conducted immediately after birth, so if you think that this is what is causing your nipples pain, seek medical advice as soon as possible. 4
Breastfeeding Tips
- Wash your breasts with water only when you shower or bathe. Small bumps on the areola (Montgomery's glands) secrete oil that moisturizes and protects your nipples.
 Soaps and shower gels can strip away this natural defense, causing dryness and irritation. 6
Soaps and shower gels can strip away this natural defense, causing dryness and irritation. 6 - Pat the nipples gently with a soft towel or simply let them air dry. In the past, women were often advised to rub their nipples to make them stiffer, but thankfully, such advice is a thing of the past!
- Do not wash breasts or nipples before feeding. The bacteria found on the surface of the breast actually help the baby's intestinal microflora to develop. 7
- Fresh breast milk helps to heal cracked nipples, 8 so rub a few drops of milk into them before and after feeding.
- Change your bra pads often if they get wet. This will reduce the risk of bacterial and fungal infections, including thrush. 6
- It is not necessary to increase the intervals between feedings to give the nipples a "rest". For a baby to be healthy and grow well, it needs to be fed on demand. Remember, frequent feeding stimulates and maintains milk production, so keep feeding despite the pain.
 9
9
Healthy teat care products
- Pure lanolin teat cleaner, a natural product derived from sheep's wool. It moisturizes and promotes healing of the nipples. This cream is safe for the baby, so it does not need to be washed off before feeding.
- Hydrogel Pads* can be applied to sore nipples to relieve pain while feeding and help promote healing. They can even be stored in the refrigerator to enhance the soothing cooling effect.
- Breast pads* fit into the bra. They help prevent nipple irritation from clothing and have air holes to help nipples heal.
- Nursing Bras** are made from breathable material such as cotton or a special fabric that dries quickly and wicks moisture away from sore nipples.
- Nursing pads* are special silicone pads that fit over the nipples. They have small holes through which milk flows when you are breastfeeding. The pads help to protect the skin underneath and help the baby to better latch on to the nipple by making the nipple stiffer.
 Do not use nursing pads for a long time. If you have problems or pain, contact your healthcare professional or lactation consultant.
Do not use nursing pads for a long time. If you have problems or pain, contact your healthcare professional or lactation consultant.
When to Seek Medical Care
The soreness should go away as your nipples and baby get used to breastfeeding. It is worth repeating that the main cause of sore nipples is improper grip. If your lactation consultant has not been able to resolve your pain while feeding, see another specialist and a third if necessary.
If nipple pain persists or if you notice unusual symptoms, talk to your doctor. The appearance of white spots or flakes on the nipples may be a sign of thrush, whitish or bluish nipples may indicate a circulation disorder such as Raynaud's disease (vasospasm), and pus and redness indicate an infection. 2
Literature
1 Kent JC et al. Volume and frequency of breastfeedings and fat content of breast milk throughout the day. Pediatrics. 2006;117(3): e 387-395. - Kent J.S. et al., "Amount and frequency of breastfeeding and fat content of breast milk during the day." Pediatrix (Pediatrics). 2006;117(3):e387-95.
- Kent J.S. et al., "Amount and frequency of breastfeeding and fat content of breast milk during the day." Pediatrix (Pediatrics). 2006;117(3):e387-95.
2 Berens P et al. Academy of Breastfeeding Medicine. ABM Clinical Protocol#26: Persistent pain with breastfeeding. Breastfeeding Medicine. 2016;11(2):46-53. - Behrens, P. et al., Academy of Breastfeeding Medicine, AVM Clinical Protocol #26: Persistence of Breastfeeding Pain. Brestfeed Med (Breastfeeding Medicine). 2016;11(2):46-53.
3 Cadwell K. Latching - On and Suckling of the Healthy Term Neonate: Breastfeeding Assessment. J Midwifery & Women's Health. 2007;52(6):638-42. — Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." F Midwifery Women Health. 2007;52(6):638-642.
4 Segal LM et al. Prevalence, diagnosis, and treatment of ankyloglossia: methodological review. Canadian Family Physician. 2007;53(6):1027-1033. - Segal L.M. et al., Incidence, Diagnosis, and Treatment of Ankyloglossia: A Methodological Review. Canadian Family Physic. 2007;53(6):1027-1033.
Canadian Family Physician. 2007;53(6):1027-1033. - Segal L.M. et al., Incidence, Diagnosis, and Treatment of Ankyloglossia: A Methodological Review. Canadian Family Physic. 2007;53(6):1027-1033.
5 O'Shea JE et al. Frenotomy for tongue - tie in newborn infants. The Cochrane Library. 2017. - O'Shea J.I. et al., "Dissection of the frenulum in the newborn", The Cochrane Labrery (Cochrane Library), 2017.
6 Jacobs A et al. S3-guidelines for the treatment of inflammatory breast disease during the lactation period. Geburtshilfe und Frauenheilkunde. 2013;73(12):1202-1208. - Jacobs A. et al., "Recommendations S -3 for the treatment of inflammatory diseases of the breast during breastfeeding. Geburtskhilfe und Frauenheilkünde. milk bacterial communities and establishment and development of the infant gut microbiome JAMA pediatrics 2017;171(7):647-654 - P. S. Pannaraj et al. development of the neonatal gut microbiome." JAMA pediatric. 2017;171(7):647-654.
S. Pannaraj et al. development of the neonatal gut microbiome." JAMA pediatric. 2017;171(7):647-654.
8 Mohammadzadeh A et al. The effect of breast milk and lanolin on sore nipples. Saudi medical journal. 2005;26(8):1231-1234. — Mohammedzade A. et al., "Effects of breast milk and lanolin on sore nipples." Saudi Medical Journal. 2005;26(8):1231-1234.
9 Kent JC et al. Principles for maintaining or increasing breast milk production. J Obstet , Gynecol , & Neonatal Nurs . 2012;41(1):114-121. - Kent J.S. et al., "Principles for Maintaining and Increasing Milk Production". J Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121.
Read instructions before use. Consult a specialist about possible contraindications.
* RC № № ФСЗ 2010/07352 dated 19.07.2010
** RU No. ФСЗ 2009/05592 dated November 25, 2009
ФСЗ 2009/05592 dated November 25, 2009
Solving nine breastfeeding problems in the first month
Expert advice on solving the main problems of breastfeeding in the first month.
Share this information
Cathy Garbin, child health nurse, midwife and lactation consultant:
Cathy, a mother of two, was a research fellow at the renowned Human Lactation Research Institute, founded by Peter Hartmann, for seven years, providing support to breastfeeding mothers in clinics and at home. Today, she still works as a family counselor, and also conducts seminars for attending physicians and speaks at international conferences.
Breastfeeding is as much a skill as driving a car, and in the first month mother and baby may encounter some obstacles along the way. It takes time and experience to make it familiar to both of you. Solving breastfeeding problems in the first month helps establish good milk production and increase the duration of breastfeeding in the future. Below you will find tips on how to overcome the main breastfeeding problems that mothers often face from the end of the first week to the end of the first month after giving birth.
Below you will find tips on how to overcome the main breastfeeding problems that mothers often face from the end of the first week to the end of the first month after giving birth.
Problem #1. A painful lump appeared in the breast
Lumps and bumps in the breast of a breastfeeding woman can appear for various reasons. One of the most common is blockage of the milk ducts, which results in a hard and painful lump that can become inflamed.
Solutions 1–3
- Massage the inflamed area, especially while breastfeeding or expressing, to clear the blockage.
- Gently apply warm flannel to your breasts or take a warm shower before feeding to relieve discomfort.
- Continue breastfeeding as usual to avoid milk accumulation that can cause mastitis.
- Try expressing milk from the inflamed breast after feeding to ensure that it is completely emptied.
 This will help to remove the blockage and restore the patency of the duct. See what breast pumps* Medela has to offer and choose the right one for you.
This will help to remove the blockage and restore the patency of the duct. See what breast pumps* Medela has to offer and choose the right one for you. - Try ultrasound therapy. If you have repeated blocked ducts, your lactation consultant or healthcare professional may suggest this procedure to help restore milk flow. The procedure is performed by a physiotherapist.
- Call your healthcare provider, if you notice signs of infection (breast redness and tenderness or flu-like symptoms such as fever, aches, malaise and headache), or if you think the lump is not related to breastfeeding .
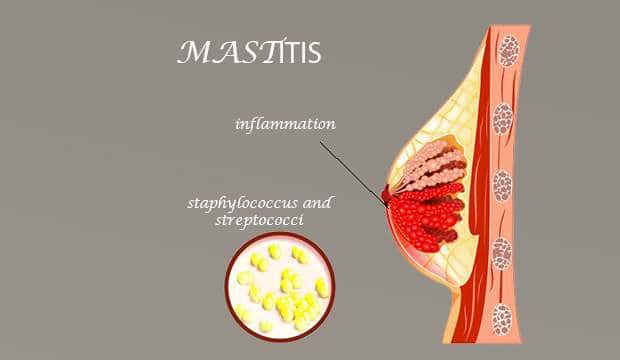
Problem #2. The breast is red and sore
If one or both mammary glands are red and sore, and this is not due to blockage of the ducts, the possibility of mastitis, that is, inflammation of the breast tissue, is not excluded. Mastitis is characterized by redness, burning, and soreness of the breasts, combined with flu-like symptoms: You feel hot and cold, your joints ache, and your temperature rises above 38. 5 °C (101.3 °F). Seek medical attention immediately if you experience these symptoms. Mastitis needs to be treated as soon as possible, as your condition can worsen in just a few hours. 3
5 °C (101.3 °F). Seek medical attention immediately if you experience these symptoms. Mastitis needs to be treated as soon as possible, as your condition can worsen in just a few hours. 3
Mastitis can be caused by the following causes:
- untreated blocked ducts,
- Bacteria entering the breast through cracked and damaged nipples,
- improper breastfeeding,
- long periods between feedings,
- breasts too full,
- wearing a bra that is too tight or that cuts into the skin,
- Abrupt weaning,
- excess milk.
Solutions 3
In addition to seeking medical attention:
- Continue to breastfeed or express milk frequently. Your milk is still safe for your baby. Its release will help eliminate blockage of the ducts and prevent painful accumulation of milk. Sudden cessation of feeding or pumping may exacerbate symptoms. After feeding, it is advisable to express any remaining milk.

- Give the child the inflamed breast first. This way the child can empty it completely. If it hurts too much, start feeding on the healthy breast, and when milk begins to flow, go back to the first one.
- Have a good rest, drink and eat. You need to get enough fluids and good nutrition.
- Massage the sore area under a warm shower or apply a warm flannel or warm pack to clear the blockage and relieve symptoms before feeding or pumping.
- Apply a cooling pack after feeding, , to reduce inflammation.
Problem #3. My strength is running out
Breastfeeding in the first weeks can be very tiring and seem endless. The baby will ask for a breast every few hours, day and night, and you have not yet grown stronger after giving birth.
Solutions
- Take care of yourself. This may be easier said than done when you have a newborn in your arms, but still try to get as much rest as possible, eat healthy and regular meals, and drink plenty of water.
 Do not refuse the help of your partner, relatives and friends, or even hire an assistant if you can afford it.
Do not refuse the help of your partner, relatives and friends, or even hire an assistant if you can afford it. - Feed lying down. This will allow you to relax and reduce stress on sore spots, stitches or c-section scars.
- Do not skip feedings. Your partner may offer to bottle feed your baby while you are resting. However, despite this temptation, it should be remembered that milk production is best established in the first four weeks through breastfeeding. When breastfeeding is well established, you can give your baby expressed milk, but before that, ask family or friends to help you with other things so you can fully focus on breastfeeding.
Problem #4. How can I increase breast milk production?
It's easy to question whether you're making enough breastmilk, especially when your baby has developmental spikes between the third and fourth weeks. It may seem to you that the child asks for breasts more often because he does not have enough milk. However, if the number of wet and soiled diapers doesn't change—see Breastfeeding: What to Expect in the First Month—the baby is likely to breastfeed more often to calm down. The baby is surrounded by many new sounds and images that are easy to get tired of, and at the breast he feels safe. 4
However, if the number of wet and soiled diapers doesn't change—see Breastfeeding: What to Expect in the First Month—the baby is likely to breastfeed more often to calm down. The baby is surrounded by many new sounds and images that are easy to get tired of, and at the breast he feels safe. 4
Solutions 4.5
- Do not try to supplement your baby with formula, unless doctors are concerned about weight gain or fluid loss. Continue breastfeeding your baby. This will help naturally increase breast milk production.
- Do not feed on a schedule. Feed your baby on demand. Thus, the production of breast milk will adapt to his needs.
- Use the breast pump, , to help increase breast milk production while continuing to breastfeed.
Problem #5. I have too much milk
Hyperlactation, or too much milk, can also be difficult for you and your baby. You may experience discomfort from swollen and leaking breasts, and your baby may have difficulty latch-on, choke on the milk flowing too fast, and be unable to empty the breast properly. 6
You may experience discomfort from swollen and leaking breasts, and your baby may have difficulty latch-on, choke on the milk flowing too fast, and be unable to empty the breast properly. 6
Solutions
- Express some breast milk at the start of a feed to reduce the force of the flush. Don't pump too much as this can aggravate the situation - pump only as much as needed to ease the discomfort. Try hand pumping or use a breast pump (check out the Medela* breast pump range and choose the right one for you).
- Use the towel or pad to soak up excess milk, or place the milk collection pad** on the other breast while you breastfeed first.
- The child must feel supported. Hold him firmly (this gives a sense of security) and in a comfortable position so that he can turn his head. Talk to the baby during the first rapid flush, then he will not be frightened by surprise and will not push the breast.
- Contact a lactation consultant or health care professional who will monitor you and suggest single-sided feedings or hourly breast changes (“breast duty”) to normalize your milk supply.
- Be patient . Problems with milk production usually go away after a few weeks.
Problem #6. I have different breasts!
You have noticed that the baby prefers one breast, or that one breast produces more milk than the other, and as a result, the mammary glands have acquired different sizes and shapes. This happens quite often and does not pose any problems for breastfeeding. If this does not bother you or your baby, you can leave everything as it is. If this makes you uncomfortable, try the following tricks.
Solutions
- Offer less demanded breasts first during feeding as babies usually breastfeed more vigorously at the start of a feed.
- Use the breast pump to increase breast milk production in the smaller breast.
- Don't give up on bigger breasts. Breastfeeding should continue with fuller breasts to avoid blocked ducts and mastitis.
- See a doctor. Sometimes an ear infection is the reason for a baby to latch on only one side. However, some positions may cause him discomfort, so try to keep the child more upright. In addition, a breast infection can change the taste of milk and cause milk to be rejected as well.
Problem #7. A blister has appeared on the nipple
With frequent feeding, sometimes painful friction occurs, and a blood bubble may appear on the breast,
nipple or areola. 7
Solutions
- Ask a lactation consultant or specialist to check the baby's latch on. A shallow grip can cause blistering of the nipples and areolas.
- Talk to your doctor about what medication you can take to relieve pain if needed.
- Try other feeding positions to avoid pressure on the painful area.

- Lubricate inflammation with pure lanolin.
- Use Breast Pads** to avoid rubbing your blister with clothing and help it heal faster with air circulation, or try cooling hydrogel pads** to help relieve pain as well as promote healing.
- Try expressing milk. Using a breast pump can be an alternative way to get breast milk without bladder irritation. Choose the correct funnel size so that the nipple can move freely and the bubble does not rub against the walls of the tunnel.
- Do not pierce the vial as this may lead to infection.
- Seek medical attention, if the problem persists and causes you pain.
Problem #8. Painful white spot on nipple
When the opening of the milk duct is blocked by milk or a thin layer of skin grows over it, a small white or yellowish spot may appear on the tip of the nipple. For some, these blocked ducts, sometimes called milk vesicles or blisters, cause pinpoint pain, especially during feeding or pumping. Others do not experience any discomfort. White blisters may persist for several days or weeks until the skin breaks and hardened milk comes out. 8
Others do not experience any discomfort. White blisters may persist for several days or weeks until the skin breaks and hardened milk comes out. 8
Solutions
- Follow the tips above to solve friction bubble problems.
- Remove the blockage, if you see that the milk cork is starting to bulge. Try to squeeze it out very gently with clean nails.
- Continue breastfeeding or pumping, to clear the milk duct. If the milk duct clears during feeding, it will not harm the baby in any way.
- Apply hot wet flannel pad to the vial just before feeding or pumping. This will help open the blocked duct. You can also try rubbing the area quickly with a clean, damp cloth.
- Hand express some milk before feeding, trying to push out hardened milk clots. If this does not help, feed the baby or express milk as usual. Repeat several times a day.

- Soak a cotton swab with olive oil and place it in the bra, pressing it against the bubble nipple. This will help soften the skin.
- Seek medical attention, if problem persists. Your doctor may remove the plug with a sterile needle. This should be done immediately after feeding, when the bubble is as inflated as possible.
Issue #9. My nipples hurt while breastfeeding
At the start of breastfeeding, my nipples may become more tender, sore, and even inflamed, but this usually goes away after a few days. If your baby's latch is checked by a specialist and the inflammation persists or the nipples hurt with every feeding, you may need medical attention to resolve this problem. 2.7
The following symptoms and signs that appear on one or both breasts during or after feeding may indicate a bacterial infection or thrush:
- burning, itching or moderate to severe pain in the nipples,
- pain in nipples aggravated by contact with clothing,
- nipple pain persists despite attempts to attach baby differently,
- nipples hurt to touch,
- stitching, shooting, burning or deep aching pain,
- chest pain during feeding and almost an hour after,
- hot pink nipples,
- discoloration and texture of the areola (hot pink, darkening, dryness or peeling),
- white rash on chest or areola.

Also check if your child has the following symptoms and signs:
- hard white patches or coating on the tongue,
- white indelible spots on the cheeks,
- bright red spotted rash on buttocks not helped by diaper rash creams.
Solutions 7
- Seek medical attention. He will most likely suggest testing for infections to make a diagnosis. Bacterial and fungal (yeast) infections are treated differently, so appropriate treatment should be started as soon as possible. There are other reasons that can cause similar nipple pain, such as eczema, psoriasis or vasospasm (narrowing of the blood vessels) in the mother and problems with latch or tongue frenulum in the child. Therefore, it is very important to make an accurate diagnosis.
- Strict hygiene. Wash hands before and after feeding and applying any medication, and after changing diapers. Change bra pads regularly, wash bras, tank tops and towels in high temperature water, thoroughly wash breast cups and anything your baby puts in her mouth, such as nipples.

- Let the nipples dry after feeding, as all infections love a warm and humid environment.
- See your doctor again if there is no improvement after a few days. Do not let the problem run its course, otherwise the situation may worsen.
Materials on the topic. Breastfeeding: what to expect in the first month
Breastfeeding: what to expect after the first month
Breastfeeding problems after the first month
Literature
Academy of Breastfeeding Medicine Protocol Committee. ABM clinical protocol # 20: Engorgement. Breastfeed Med. 2009;4(2):111-113.- Breastfeeding Academy Protocol Committee, "AVM Clinical Protocol #20: Breast engorgement." Brestfeed Med (Breastfeeding Medicine). 2009;4(2):111-113.
2 Jacobs A et al. S3-guidelines for the treatment of inflammatory breast disease during the lactation period. Geburtshilfe and Frauenheilkunde . 2013;73(12):1202-1208. - Jacobs A. et al., "Recommendations 2014;9(5):239-243.
2013;73(12):1202-1208. - Jacobs A. et al., "Recommendations 2014;9(5):239-243.
4 Kent JC et al. Principles for maintaining or increasing breast milk production. 2012;41(1):114-121. - Kent J.S. et al., "Principles for Maintaining and Increasing Milk Production". F Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121.
5 Amir L. Breastfeeding managing ‘supply’ difficulties. Aust fam physician . 2006;35(9):686. - - Amir L., "Breastfeeding: problems of 'supply'. Aust fam physis. 2006;35(9):686.
6 Trimeloni L, Spencer J. Diagnosis and management of breast milk oversupply Journal Am Board Fam Med . 2016;29(1):139-142. - Trimeloni L., Spencer J., "Diagnosis and correction of excess breast milk production.