Are utis common during pregnancy
Urinary tract infections (UTIs) in pregnancy - symptoms, causes
Urinary tract infections (UTIs) in pregnancy - symptoms, causes | Pregnancy Birth and Baby beginning of content5-minute read
Listen
What is a urinary tract infection?
A urinary tract infection (UTI) is an infection of the urinary system. UTIs are the most common bacterial infection that women develop during pregnancy. They can occur in different parts of the urinary tract, including the bladder (cystitis), urethra (urethritis) or kidneys (pyelonephritis). Sometimes when a UTI develops and bacteria are detected in the urinary tract, you may not have any symptoms of an infection. This is known as asymptomatic bacteriuria.
While anyone can get a UTI, they are much more common in women than men and they are also more likely to occur in the very young and the elderly.
What are the symptoms of UTIs during pregnancy?
Common symptoms of a UTI during pregnancy are similar to those that you might experience at any other time, and include:
- a burning sensation when you pass urine
- feeling the urge to urinate more often than usual
- urinating before you reach the toilet (‘leaking’ or incontinence)
- feeling like your bladder is full, even after you have urinated
- urine that looks cloudy, bloody or is very smelly
- pain above the pubic bone
- fever
Sometimes the first sign of an infection is a faint prickly sensation when you pass urine. If the infection is more advanced and has moved up to the kidneys, you may also experience fever with a particularly high temperature, back pain and vomiting.
What are the common causes of UTIs?
Your urinary tract is normally free of bacteria. If bacteria enter the tract and multiply, they can cause a UTI. There are several factors that increase the risk of developing an infection:
- Infection with common bacteria in your gut, usually from faeces (poo) can contaminate your urinary tract
- Being sexually active increases the risk of bacteria moving around the genital area and entering the urinary tract
- If you have weak pelvic floor muscles your bladder might not empty completely, which can lead to an infection
- Women with diabetes are at increased risk of developing a UTI since the sugar in their urine may cause bacteria to multiply
Are UTIs a risk during pregnancy?
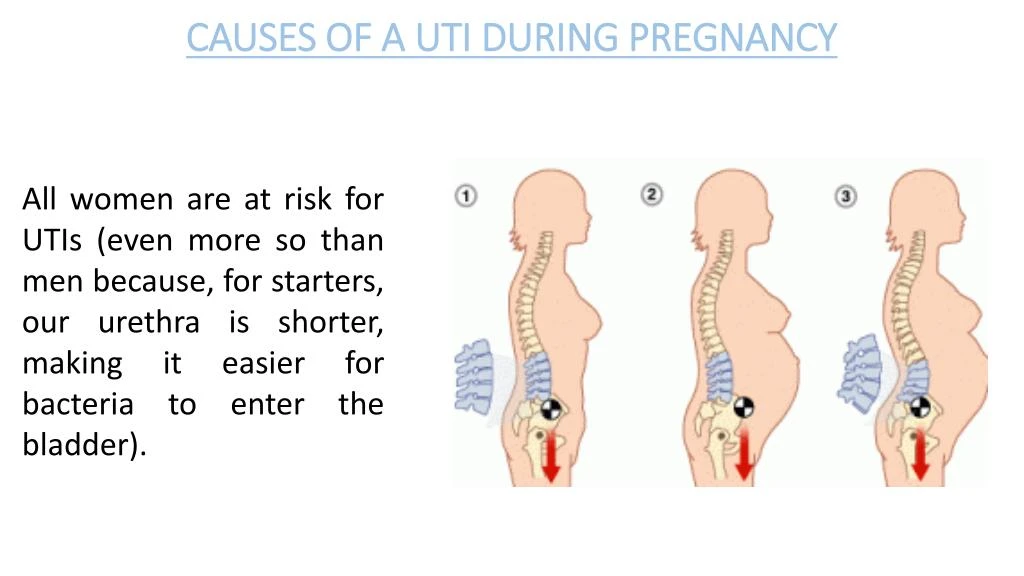
During pregnancy, many changes occur in your body that increase your risk of developing a UTI, including changes to the make-up of your urine and immune system.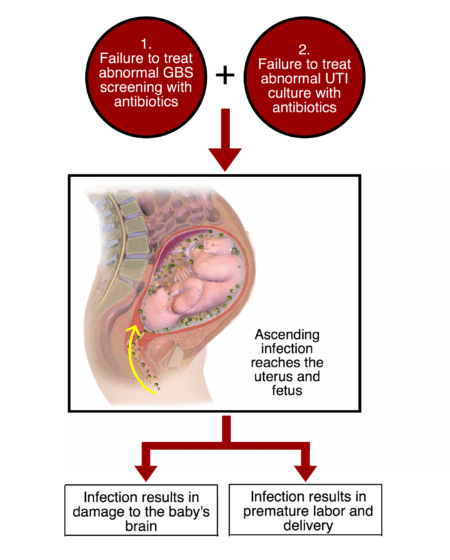 As your baby grows, there is also an increase in the pressure on your bladder, which can reduce the flow of your urine and lead to an infection.
As your baby grows, there is also an increase in the pressure on your bladder, which can reduce the flow of your urine and lead to an infection.
UTIs can affect women whether they are pregnant or not. However, pregnant women are more likely to develop repeated or more severe infections. Up to 1 in 10 pregnant women will have a UTI but not have any symptoms at all.
Is there a risk to my baby?
Having a UTI during pregnancy can increase your risk of developing high blood pressure, and your baby may be born early and smaller than usual. For this reason, even if you don’t have any symptoms, it is important to treat a UTI as soon as possible.
How are UTIs diagnosed?
UTIs are diagnosed by taking a urine sample which is checked in a laboratory for bacteria. Your doctor may also perform a physical examination if they think you have an infection.
All pregnant women are offered a urine test, usually at their first antenatal visit or soon after. You may need to repeat the urine test if you have a history of UTIs; have symptoms of a UTI; have a contaminated sample or if your doctor thinks you are at high risk of developing a UTI. If you have frequent UTIs, you may also need additional tests such as an ultrasound of your kidneys.
If you have frequent UTIs, you may also need additional tests such as an ultrasound of your kidneys.
How are UTIs treated during pregnancy?
When you have a UTI, it is important to drink plenty of water to flush out the urinary tract. UTIs are treated with antibiotics that are safe in pregnancy. Your doctor will select the right antibiotic, based on your infection and the type of bacteria found in your urine sample.
Can I prevent UTIs?
You can lower your risk of developing a UTI during pregnancy by:
- drinking plenty of fluids, especially water
- quickly treating any vaginal infection that may occur, including thrush or a sexually transmitted infection
- avoiding becoming constipated
Some women have also found the following tips helpful:
- urinate immediately after sex
- don’t delay going to the toilet — go as soon as you feel the need
- wipe from the front to the back after going to the toilet
- wear cotton underwear
When should I see my doctor?
See your midwife or doctor if you have any symptoms of a UTI. It’s important not to delay treatment since infections develop quickly, and can affect both you and your baby.
It’s important not to delay treatment since infections develop quickly, and can affect both you and your baby.
More information
UTIs are very common during pregnancy, and are best treated early. If you notice the symptoms of an infection, seek medical advice from your doctor, midwife or pharmacist.
For more information on UTIs, visit the Kidney Health Australia page on UTIs.
Sources:
Government of South Australia (Urinary Tract Infection in Pregnancy), Jean Hailes (Urinary Tract Infections), Kidney Health Australia (Factsheet: Urinary Tract Infections), Government of Western Australia North Metropolitan Health Service (Urinary Tract Infection in Pregnant Women)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: August 2021
Back To Top
Related pages
- Frequent urination during pregnancy
- Incontinence during pregnancy
Need more information?
Urinary tract infection (UTI) - MyDr.
 com.au
com.au Urinary tract infection occurs when part of the urinary tract becomes infected. UTIs are usually caused by bacteria and generally clear up with a course of antibiotics.
Read more on myDr website
Urinary tract infections (UTIs) explained - NPS MedicineWise
Learn about the causes & treatments for urinary tract infections (UTIs).
Read more on NPS MedicineWise website
Urinary tract infection (UTI) | SA Health
Urinary tract infection (UTI) is an infection of the urinary system. Infection may occur in the kidneys, bladder or urethra.
Read more on SA Health website
Urinary Tract Infections (UTIs) | Jean Hailes
A comprehensive guide to urinary tract infections. Everything you should know about UTIs including causes, symptoms, management and treatment.
Everything you should know about UTIs including causes, symptoms, management and treatment.
Read more on Jean Hailes for Women's Health website
Urinary Tract Infections (UTIs) | Kidney Health Australia
Do you have a urinary tract infection (UTI)? Learn about causes, symptoms and treatment, and find out if you’re at risk.
Read more on Kidney Health Australia website
Incontinence & Bladder Weakness | Jean Hailes
What makes a normal bladder. Types of incontinence. Causes and symptoms. Diagnosis and treatment. Prevention and management.
Read more on Jean Hailes for Women's Health website
Pyelonephritis
Infection of the kidneys.
Read more on Queensland Health website
Check-ups, tests and scans available during your pregnancy
Antenatal care includes several check-ups, tests and scans, some of which are offered to women as a normal part of antenatal care in Australia. Learn more here.
Read more on Pregnancy, Birth & Baby website
Thrush | SA Health
Thrush or Candidiasis is a common vaginal infection, caused by an overgrowth of yeasts and is not considered to be a sexually transmitted infection
Read more on SA Health website
Pregnancy at week 9
Your baby is now the size of a peanut. You won't be showing just yet, but you may have put on a little weight.
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.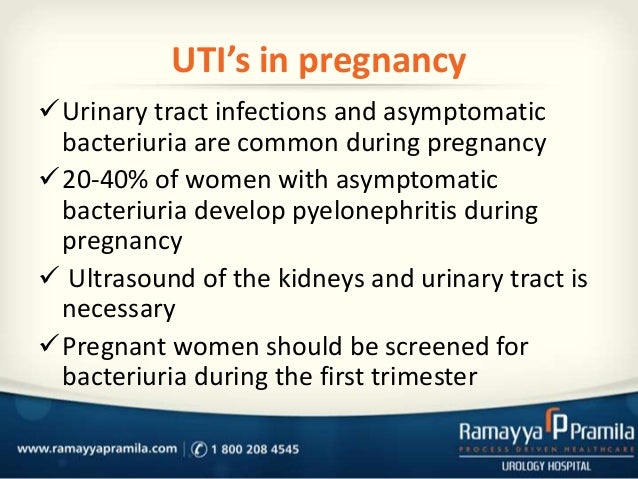
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Urinary Tract Infections (UTI) During Pregnancy
Written by WebMD Editorial Contributors
Medically Reviewed by Nivin Todd, MD on September 04, 2022
In this Article
- UTI Symptoms
- Why Are UTIs More Common During Pregnancy?
- UTI Diagnosis
- UTI Treatment During Pregnancy
- UTI Complications During Pregnancy
- UTI Prevention
A urinary tract infection (UTI) is an infection of some part of your body's urinary system, which includes your:
- Kidneys
- Ureters (tubes that carries urine from your kidneys to your bladder)
- Bladder
- Urethra (a short tube that carries urine from your bladder to outside your body)
Bacteria cause most UTIs. Anyone can get one, but they're most common in women, and they can be extra concerning if you're pregnant.
Anyone can get one, but they're most common in women, and they can be extra concerning if you're pregnant.
If you think you might have a UTI, tell your doctor. With proper care, you and your baby should be fine.
Usually, these infections are in the bladder and urethra. But sometimes they can lead to kidney infections. If they do, UTIs may lead to preterm labor (giving birth too early) and low birth weight.
UTI Symptoms
If you have a UTI, you may have:
- An urgent need to pee, or peeing more often
- Trouble with peeing
- A burning sensation or cramps in your lower back or lower belly
- A burning feeling when you pee
- Urine that looks cloudy or has an odor
- Blood in your pee, which can turn it red, bright pink, or cola-colored
If you have a kidney infection, you may have:
- Fever
- Nausea
- Vomiting
- Upper back pain, often on just one side
If you have symptoms of a kidney infection, see your doctor right away. Without treatment, the infection can spread into your bloodstream and cause life-threatening conditions.
Without treatment, the infection can spread into your bloodstream and cause life-threatening conditions.
Why Are UTIs More Common During Pregnancy?
Hormones are one reason. In pregnancy, they cause changes in the urinary tract, and that makes women more likely to get infections. Changes in hormones can also lead to vesicoureteral reflux, a condition in which your pee flows back up from your bladder to your kidneys. This can cause UTIs.
When you’re pregnant, your pee has more sugar, protein, and hormones in it. These changes also put you at higher risk for a UTI.
Because you’re pregnant, your growing uterus presses on your bladder. That makes it hard for you to let out all the urine in your bladder. Leftover urine can be a source of infection.
Other causes of UTIs include:
Escherichia coli and other bacteria from your poop. E. Coli is the most common cause of UTIs and can move from your rectum to your urethra if you don’t wipe from front to back.
Sexual activity. Fingers, your partner’s penis, or devices can move bacteria near your vagina into your urethra.
Group B streptococcus. Many women have this bacteria in their colon and vagina. It can cause UTIs and women can pass it to their newborns. Your doctor will test you for this bacteria around weeks 36 to 37 of pregnancy. If you’re positive for group B strep, your doctor will give you IV antibiotics during labor.
UTI Diagnosis
You’ll take a urine test. Your doctor will test it for bacteria and red and white blood cells. A urine culture may also be checked. It shows what kind of bacteria are in the urine.
UTI Treatment During Pregnancy
You’ll take antibiotics for 3 to 7 days or as your doctor recommends. If your infection makes you feel uncomfortable, your doctor will probably start your treatment before you get your urine test results.
Your symptoms should go away in 3 days. Take all of your medication on schedule anyway. Don’t stop it early, even if your symptoms fade.
Don’t stop it early, even if your symptoms fade.
Many common antibiotics -- amoxicillin, erythromycin, and penicillin, for example -- are considered safe for pregnant women. Your doctor wouldn’t prescribe others, such as ciprofloxacin (Cipro), sulfamethoxazole, tetracycline, or trimethoprim (Primsol, Proloprim, Trimpex), that can affect your baby’s development.
UTI Complications During Pregnancy
Pyelonephritis is a UTI that affects the kidneys. If you’re pregnant it can cause:
- Preterm labor
- Severe infection
- Adult respiratory distress syndrome
- Anemia
- Long-term infection
UTI Prevention
To try to avoid getting a UTI:
- Drink at least eight glasses of water a day.
- Wipe yourself from front to back when you go to the bathroom.
- Empty your bladder shortly before and after sex.
- If you need a lubricant when you have sex, choose a water-based one.
- Don't douche.
- Avoid strong feminine deodorants or soaps that cause irritation.

- Wash your genital area with warm water before sex.
- Wear cotton underwear.
- Take showers instead of baths.
- Don’t wear pants that are too tight.
- Pee often.
- Avoid alcohol, citrus juices, spicy food, and caffeinated drinks, which can irritate your bladder.
Women's Health Guide
- Screening & Tests
- Diet & Exercise
- Rest & Relaxation
- Reproductive Health
- Head to Toe
450106, Ufa, st. Art. Kuvykina, 96. e-mail: [email protected]
Good afternoon, dear friends! Today we will talk about cardiovascular diseases in women during pregnancy. Despite the fact that pregnancy is a completely natural state of a woman, at this time her health is especially vulnerable, as the body works to create and form a new life. For nine months of waiting, the expectant mother may face various problems, one of which is arrhythmia.
The risk of developing arrhythmias can be quite high. Indeed, with serious violations of the heart rhythm, problems with the health of the mother and fetus can occur. Not all arrhythmias observed in pregnant women are associated with heart disease. They can also be observed in conditions whose causes are the influence of external factors on the nervous system.
These include:
• severe physical and emotional stress,
• unhealthy diet,
• bad habits,
• diseases of the respiratory tract,
• diseases of the central nervous system;
• problems with the gastrointestinal tract;
• disturbances in electrolyte metabolism;
• diseases associated with heredity;
• problems with the endocrine system.
Some types of arrhythmias also occur in apparently healthy women. Not all arrhythmias, especially in pregnant women, should be treated medically, especially surgically. In some cases, it is necessary to treat the underlying disease, such as anemia, which causes heart rhythm disturbances.
Arrhythmia can occur in absolutely any pregnant woman, but there are such risk factors that significantly increase the possibility of developing the disease. First of all, it is a hereditary predisposition.
In women with a history of congenital and acquired heart defects, especially with decompensation of the disease during pregnancy, the risk of rhythm disturbances, including life-threatening ones, is quite high.
Very often, rhythm disturbances appear at long gestational ages. After all, along with the growth of the child, the load on the heart gradually increases due to an increase in blood volume in the body. The heart is forced to work with a greater load, which leads to various functional disorders, including arrhythmias.
Heart rhythm disorders can be associated with various hormonal changes and changes in the activity of the autonomic nervous system.
During pregnancy, cardiac arrhythmias are possible by the type of slowing of the heart rate (bradycardia), which in most cases are congenital and asymptomatic. The first manifestation of such a condition can lead to loss of consciousness and is an indication for the implantation of an artificial pacemaker. Each case is individual, therefore, the issue of treatment and methods of its implementation is decided by the observing doctor - gynecologist, taking into account the recommendations of the cardiologist (arrhythmologist) and the therapist.
The first manifestation of such a condition can lead to loss of consciousness and is an indication for the implantation of an artificial pacemaker. Each case is individual, therefore, the issue of treatment and methods of its implementation is decided by the observing doctor - gynecologist, taking into account the recommendations of the cardiologist (arrhythmologist) and the therapist.
Sinus tachycardia is very common in pregnant women, when the heart rate reaches one hundred or more beats per minute. In most cases, it is non-cardiac in nature and does not require active antiarrhythmic therapy. One of the most common forms of arrhythmia is extrasystole. This form of rhythm disturbance during pregnancy most often does not cause much discomfort and only sometimes manifests itself in the form of a feeling of heart rhythm failure or discomfort in the chest. Although such symptoms frighten the pregnant woman, they do not require special medical treatment and do not lead to the need to refuse natural childbirth.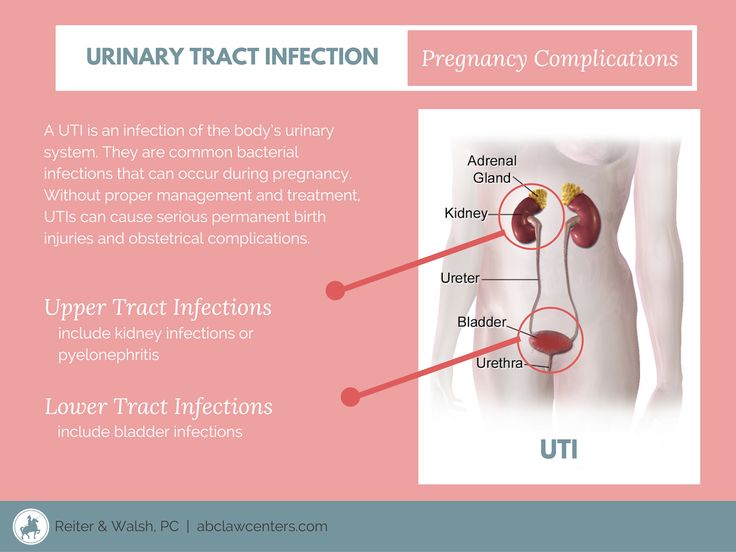 Specific drugs are prescribed by a specialist only after a comprehensive examination and if there is a risk of ventricular tachycardia.
Specific drugs are prescribed by a specialist only after a comprehensive examination and if there is a risk of ventricular tachycardia.
We must remember that self-treatment harms health, first of all, the health of the unborn child. Therefore, specialist advice is required.
The reason for special therapy is the presence of atrial fibrillation or palpitations, which can cause hypoxia in the child and even lead to miscarriage. traumatic factor that caused its appearance (alcohol, nicotine, caffeine, emotional and physical overwork). When this is not enough, medications are prescribed, but when prescribing drugs, the gynecologist, first of all, evaluates the appropriateness of prescribing them in terms of future benefits and possible harm to the child.
If you do not want to be a hostage to arrhythmia during pregnancy, the best way to prevent the disease is to have a timely examination and thorough preparation of the family for planning a child. It is before conception that a woman can take a course of treatment without fear for the life and health of the unborn baby.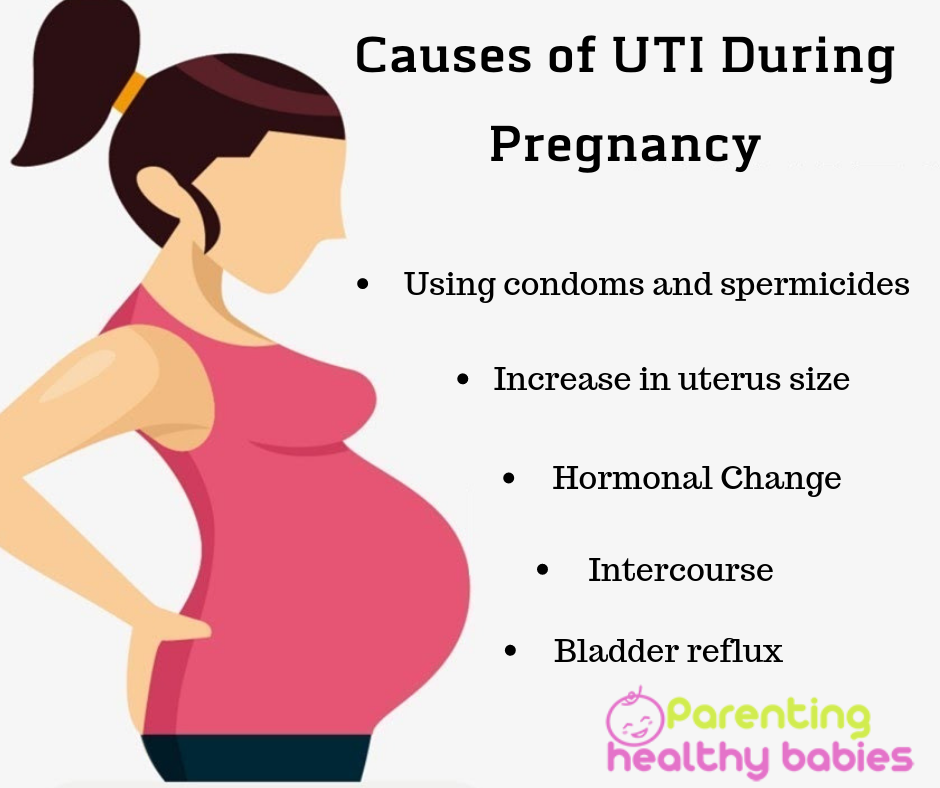
To protect a woman from possible complications during childbearing, the doctor must diagnose possible diseases of the cardiovascular system, lungs, bronchi, thyroid gland and other abnormalities of the body that can provoke heart rhythm disturbances even before pregnancy. Every pregnant woman who is suspected of having a heart rhythm disorder can get qualified advice at the Republican Cardiology Center. Do not forget that a healthy lifestyle and movement are the key to a cheerful mood and excellent health. Practice exercises in the morning and take more walks in the fresh air, then you will certainly notice that arrhythmia worries you less!
Article "Pregnancy and heartburn"
Hormonal changes that the body undergoes during pregnancy is the root cause of heartburn. In early pregnancy, the ovaries, and then the placenta, produce the hormone progesterone, one of the main functions of which is to relax the smooth muscles of the body, including the muscles of the uterus. Similarly, progesterone acts on other smooth muscles in our body, for example, the muscles of the esophagus, stomach, and intestines. Progesterone also has a relaxing effect on the sphincters (circular muscles), the main task of which is to separate the various organs of the gastrointestinal system from each other. Relaxation of the esophageal-gastric sphincter leads to the fact that in pregnant women its lumen is open, and hydrochloric acid, which is produced by the stomach, can be thrown into the esophagus, which causes an unpleasant sensation of pain and burning - heartburn.
Similarly, progesterone acts on other smooth muscles in our body, for example, the muscles of the esophagus, stomach, and intestines. Progesterone also has a relaxing effect on the sphincters (circular muscles), the main task of which is to separate the various organs of the gastrointestinal system from each other. Relaxation of the esophageal-gastric sphincter leads to the fact that in pregnant women its lumen is open, and hydrochloric acid, which is produced by the stomach, can be thrown into the esophagus, which causes an unpleasant sensation of pain and burning - heartburn.
Another cause of heartburn in pregnant women is the weakening of motility - the wave-like movement of the gastrointestinal tract, slowing down the processes of digestion. Food passes through the digestive tract more slowly, lingering in the stomach. Heartburn in pregnant women is also provoked by the large size of the uterus, which increases intra-abdominal pressure and increases pressure on all the internal organs of the pregnant woman - the stomach and intestines as well. The stomach changes its location during pregnancy, pushed up and to the side by the uterus - all these factors also contribute to the violation of the motility of the esophagus, stomach and intestines and create conditions for the occurrence of heartburn.
The stomach changes its location during pregnancy, pushed up and to the side by the uterus - all these factors also contribute to the violation of the motility of the esophagus, stomach and intestines and create conditions for the occurrence of heartburn.
Heartburn can start at any stage of pregnancy, but is most common in the second and third trimesters. As a rule, discomfort occurs after 24 weeks, when the uterus rises above the navel, and becomes especially severe after 30 weeks. Especially intense heartburn can be in a woman if she had an increased acidity of gastric juice before pregnancy.
To avoid heartburn during pregnancy, first of all, you need to review your menu and exclude fatty, fried, spicy, salty foods from it, you must give up coffee and carbonated drinks. Include cereals, dairy products, lean meats and mashed vegetables in the diet. It is advisable to eat often and in small portions every 1.5-2 hours. Spend more time eating, remember to chew food thoroughly so that it is digested properly. Drink water between meals, not with meals. After a meal, it is not recommended to sit or lie down, but take a walk for some time (about 30-40 minutes). Try to avoid sharp torso bending after eating. Do not eat at night, the last meal is desirable 2-3 hours before going to bed. Remember to put an extra pillow under your head, sometimes this helps to cope with heartburn. And if heartburn still appears, you need to try to reduce it.
Drink water between meals, not with meals. After a meal, it is not recommended to sit or lie down, but take a walk for some time (about 30-40 minutes). Try to avoid sharp torso bending after eating. Do not eat at night, the last meal is desirable 2-3 hours before going to bed. Remember to put an extra pillow under your head, sometimes this helps to cope with heartburn. And if heartburn still appears, you need to try to reduce it.
At the first signs of heartburn, you can drink a small amount of alkaline mineral water without gas or take a few sips of low-fat milk. Drink should be in small sips. Kissels work well. They envelop the esophagus and thus reduce burning sensation. The safest in the treatment of heartburn in pregnant women are antacids containing sodium bicarbonate, calcium carbonate, preparations containing magnesium and other substances. Antacids neutralize gastric acid, are not absorbed into the bloodstream and cannot affect the developing fetus. Caution should be taken only to antacids that contain aluminum - because of the theoretical risk of absorption of aluminum ions into the body of a pregnant woman and their penetration into the tissues of the fetus.