Problems with thyroid during pregnancy
Thyroid conditions during pregnancy
In This Topic
What is the thyroid?
The thyroid is a tiny, butterfly-shaped gland in your neck. A gland is an organ that makes substances that help your body work. The thyroid makes hormones (chemicals) that play a big role in your health. For example, thyroid hormones can affect your heart rate (how fast your heart beats) and your metabolism (how well and fast your body processes what you eat and drink).
Sometimes the thyroid gland makes too much or too little of certain hormones. When this happens, you have a thyroid disorder. Some women have a thyroid disorder that begins before pregnancy (also called a pre-existing condition). Others may develop thyroid problems for the first time during pregnancy or soon after giving birth.
With treatment, a thyroid condition may not cause any problems during pregnancy. But untreated thyroid conditions can cause problems for you and your baby during pregnancy and after birth.
What are the main kinds of thyroid conditions?
There are two main kinds of thyroid conditions:
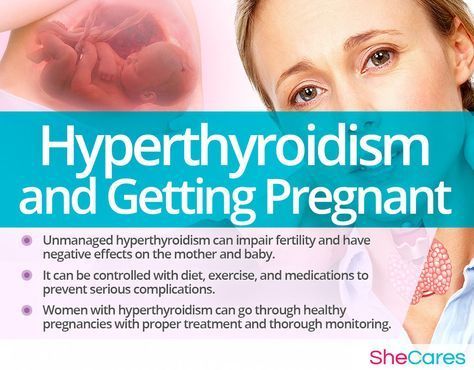
- Hyperthyroidism (“hyper” means too much).
This is when the thyroid is overactive and makes too much thyroid hormone. This condition can cause many of your body’s functions to speed up. Hyperthyroidism during pregnancy usually is caused by an autoimmune disorder called Graves’ disease. Autoimmune disorders are health conditions that happen when antibodies (cells in the body that fight off infections) attack healthy tissue by mistake. If you have Graves’ disease, your immune system makes antibodies that cause your thyroid to make too much thyroid hormone. In rare cases, hyperthyroidism is linked to a severe form of morning sickness called hyperemesis gravidarum (excessive nausea and vomiting during pregnancy). Also in rare cases, hyperthyroidism can be caused by thyroid nodules. These are lumps in your thyroid that make too much thyroid hormone.
- Hypothyroidism (“hypo” means too little or not enough). This is when the thyroid is underactive and doesn’t make enough thyroid hormones, so many of your body’s functions slow down.
 Hypothyroidism during pregnancy usually is caused by an autoimmune disorder called Hashimoto’s disease. When you have Hashimoto’s disease, your immune system makes antibodies that attack your thyroid and damage it so it can’t produce thyroid hormones.
Hypothyroidism during pregnancy usually is caused by an autoimmune disorder called Hashimoto’s disease. When you have Hashimoto’s disease, your immune system makes antibodies that attack your thyroid and damage it so it can’t produce thyroid hormones.
If you have a thyroid condition during pregnancy, treatment can help you have a healthy pregnancy and a healthy baby.
How are thyroid conditions during pregnancy diagnosed?
Health care providers don’t usually test your thyroid before or during pregnancy unless you’re at high risk of having a thyroid condition or you have signs or symptoms of one. If you have signs or symptoms of a thyroid condition, especially during pregnancy, tell your provider. Signs of a condition are things someone else can see or know about you, like that you have a rash or you’re coughing. Symptoms are things you feel yourself that others can’t see, like having a sore throat or feeling dizzy. Signs and symptoms of thyroid conditions may appear slowly over time. Many are signs and symptoms of other health conditions, so having one doesn’t always mean you have a thyroid problem.
Many are signs and symptoms of other health conditions, so having one doesn’t always mean you have a thyroid problem.
Your provider gives you a physical exam and a blood test to check for thyroid conditions. The blood test measures the levels of thyroid hormones and thyroid stimulating hormone (also called TSH) in your body. TSH is a hormone that tells your thyroid gland to make thyroid hormones. If you think you may have a thyroid condition, ask your provider about testing.
Are you at risk for having a thyroid condition during pregnancy?
You’re at higher risk for a thyroid condition during pregnancy than other women if you:
- Are currently being treated for a thyroid condition or you have thyroid nodules or a goiter. A goiter is a swollen thyroid gland that can make your neck look swollen.
- Have had a thyroid condition in the past (including after giving birth), or you’ve had a baby who had a thyroid condition
- Have an autoimmune disorder or you have a family history of autoimmune thyroid disease, like Graves’ disease or Hashimoto’s disease.
 Family history means that the condition runs in your family (people in your family have or have had the condition). Use the March of Dimes family health history form and share it with your provider. The form helps you keep a record of any health conditions and treatments that you, your partner and everyone in both of your families has had. It can help your provider check for health conditions that may affect your pregnancy. If you have a family history of thyroid or autoimmune conditions, ask your provider about testing.
Family history means that the condition runs in your family (people in your family have or have had the condition). Use the March of Dimes family health history form and share it with your provider. The form helps you keep a record of any health conditions and treatments that you, your partner and everyone in both of your families has had. It can help your provider check for health conditions that may affect your pregnancy. If you have a family history of thyroid or autoimmune conditions, ask your provider about testing. - Have type 1 diabetes. Diabetes is a condition in which your body has too much sugar (called glucose) in the blood. Type 1 diabetes is a kind of preexisting diabetes, which means you have it before you get pregnant. If you have type 1 diabetes, your pancreas stops making insulin. Insulin is a hormone that helps keep the right amount of glucose in your body.
- Have had high-dose neck radiation or treatment for hyperthyroidism. Radiation is a kind of energy.
 It travels as rays or particles in the air.
It travels as rays or particles in the air.
If you’ve had a thyroid condition or think you’re at risk for having a thyroid condition, ask your provider about testing.
What are signs and symptoms of hyperthyroidism?
Hyperthyroidism that’s untreated or not treated correctly is linked to problems for women and babies during pregnancy and after birth.
Problems for women can include:
- Preeclampsia. This is a serious blood pressure condition that can happen after the 20th week of pregnancy or after giving birth (also called postpartum preeclampsia). It’s when a woman has high blood pressure and signs that some of her organs, like her kidneys and liver, may not be working normally. Blood pressure is the force of blood that pushes against the walls of your arteries. Arteries are blood vessels that carry blood away from your heart to other parts of the body. High blood pressure (also called hypertension) is when the force of blood against the walls of the blood vessels is too high.
 It can stress your heart and cause problems during pregnancy.
It can stress your heart and cause problems during pregnancy. - Pulmonary hypertension. This is a kind of high blood pressure that happens in the arteries in your lungs and on the right side of your heart.
- Placental abruption. This is a serious condition in which the placenta separates from the wall of the uterus before birth. The placenta grows in your uterus (womb) and supplies the baby with food and oxygen through the umbilical cord.
- Heart failure. This is when your heart can’t pump enough blood to the rest of your body.
- Thyroid storm. This is when your symptoms suddenly get much worse. It’s a rare, but life-threatening condition during pregnancy. Pregnant women who have thyroid storm are at high risk of heart failure.
Problems for babies can include:
- Premature birth. This is birth that happen too early, before 37 weeks of pregnancy.
- Goiter
- Low birthweight.
 This is when a baby is born weighing less than 5 pounds, 8 ounces.
This is when a baby is born weighing less than 5 pounds, 8 ounces. - Thyroid problems. Antibodies that cause Graves’ disease cross the placenta during pregnancy. If you have Graves’ disease during pregnancy, your baby is at risk for thyroid conditions during and after birth. If you had treatment for Graves’ disease with radioactive iodine before pregnancy, your baby is at risk for Graves’ disease.
- Miscarriage or stillbirth. Miscarriage is when a baby dies in the womb before 20 weeks of pregnancy. Stillbirth is when a baby dies in the womb after 20 weeks of pregnancy.
How can hypothyroidism affect pregnancy?
Untreated hypothyroidism during pregnancy is linked to problems for women and babies during pregnancy and after birth.
Problems for women can include:
- Anemia. This is when you don’t have enough healthy red blood cells to carry oxygen to the rest of your body.
- Gestational hypertension. This is high blood pressure that starts after 20 weeks of pregnancy and goes away after you give birth.
- Preeclampsia
- Placental abruption
- Postpartum hemorrhage (also called PPH). This when a woman has heavy bleeding after giving birth. It’s a serious but rare condition. It usually happens within 1 day of giving birth, but it can happen up to 12 weeks after having a baby.
- Myxedema, a rare condition caused by severe, untreated hypothyroidism that can cause you to go into a coma and can cause death
- Heart failure. This is when your heart doesn’t pump blood as well as it should. Heart failure cause by hypothyroidism is rare.
Problems for babies can include:
- Infantile myxedema, a condition that’s linked to severe hypothyroidism. It can cause dwarfism, intellectual disabilities and other problems.
 Dwarfism (also called little people) is a condition in which a person is very short (less than 4 feet 10 inches as an adult). Intellectual disability causes a lower-than-average intelligence and a lack of skills needed to function in daily life.
Dwarfism (also called little people) is a condition in which a person is very short (less than 4 feet 10 inches as an adult). Intellectual disability causes a lower-than-average intelligence and a lack of skills needed to function in daily life. - Low birthweight.
- Problems with growth and brain and nervous system development. The nervous system is made up of your brain, spinal cord and nerves. Your nervous system helps you move, think and feel. Untreated hypothyroidism, especially when it happens during the first trimester, can cause low IQ in a baby.
- Thyroid problems. This is rare, but it can happen in babies of women with Hashimoto’s disease because the antibodies can cross the placenta during pregnancy.
- Miscarriage or stillbirth
What is postpartum thyroiditis?
In about 1 to 21 in 100 women (1 to 21 percent), the thyroid becomes swollen in the first year after giving birth. This is an autoimmune condition called postpartum thyroiditis. It can cause your thyroid to be overactive, underactive and even a combination of both.
This is an autoimmune condition called postpartum thyroiditis. It can cause your thyroid to be overactive, underactive and even a combination of both.
How are thyroid conditions treated during pregnancy and while breastfeeding?
Many medicines used to treat thyroid conditions during pregnancy are safe for your baby. Thyroid medicines can help keep the right level of thyroid hormones in your body. Your provider gives you blood tests during pregnancy to check your TSH and T4 levels to make sure your medicine is at the right amount (also called dose). T4 is a hormone made by your thyroid.
If you’re taking medicine for a thyroid condition before pregnancy, talk to your provider before you get pregnant. Your provider may want to adjust or change your medicine to make sure it’s safe for your baby. If you’re already taking thyroid medicine when you get pregnant, keep taking it and talk to your provider about it as soon as possible.
Treating hyperthyroidism. If you have mild hyperthyroidism, you may not need treatment. If it’s more severe, you may need to take an antithyroid medicine. This medicine causes your thyroid to make less thyroid hormone.
If you have mild hyperthyroidism, you may not need treatment. If it’s more severe, you may need to take an antithyroid medicine. This medicine causes your thyroid to make less thyroid hormone.
Most providers treat pregnant women with an overactive thyroid with antithyroid medicines called propylthiouracil in the first trimester and methimazole in the second and third trimesters. The timing of these medicines is important. Propylthiouracil after the first trimester can lead to liver problems. And methimazole in the first trimester may increase the risk of birth defects. Birth defects are health conditions that are present at birth. They change the shape or function of one or more parts of the body. Birth defects can cause problems in overall health, how the body develops, or how the body works.
Providers sometimes use radioactive iodine to treat hyperthyroidism. Pregnant women shouldn’t take this medicine because it can cause thyroid problems in the baby.
Antithyroid medicines are safe to take at low doses while you’re breastfeeding.
Treating hypothyroidism. Levothyroxine is the most common medicine used to treat an underactive thyroid during pregnancy. Levothyroxine replaces the thyroid hormone T4, which your own thyroid isn’t making or isn’t making enough of. It’s safe to take this medicine during pregnancy. Thyroid medicines that contain the T3 hormone aren’t safe to use during pregnancy.
If you had hypothyroidism before getting pregnant, you most likely need to increase the amount of medicine you take during pregnancy. Talk to your health care provider about your medicine as soon as you find out you’re pregnant. Your provider can check to make sure you’re taking the right dose by checking your TSH levels during pregnancy.
Talk to your provider about taking levothyroxine or other medicine to treat hypothyroidism while breastfeeding.
More information- American Thyroid Association
- MotherToBaby
Last reviewed: February, 2019
See also: Prescription medicine during pregnancy
Thyroid Disease & Pregnancy | NIDDK
On this page:
- What role do thyroid hormones play in pregnancy?
- Hyperthyroidism in Pregnancy
- Hypothyroidism in Pregnancy
- Postpartum Thyroiditis
- Is it safe to breastfeed while I’m taking beta-blockers, thyroid hormone, or antithyroid medicines?
- Thyroid Disease and Eating During Pregnancy
- Clinical Trials
Thyroid disease is a group of disorders that affects the thyroid gland. The thyroid is a small, butterfly-shaped gland in the front of your neck that makes thyroid hormones. Thyroid hormones control how your body uses energy, so they affect the way nearly every organ in your body works—even the way your heart beats.
The thyroid is a small, butterfly-shaped gland in the front of your neck that makes thyroid hormones. Thyroid hormones control how your body uses energy, so they affect the way nearly every organ in your body works—even the way your heart beats.
Sometimes the thyroid makes too much or too little of these hormones. Too much thyroid hormone is called hyperthyroidism and can cause many of your body’s functions to speed up. “Hyper” means the thyroid is overactive. Learn more about hyperthyroidism in pregnancy. Too little thyroid hormone is called hypothyroidism and can cause many of your body’s functions to slow down. “Hypo” means the thyroid is underactive. Learn more about hypothyroidism in pregnancy.
If you have thyroid problems, you can still have a healthy pregnancy and protect your baby’s health by having regular thyroid function tests and taking any medicines that your doctor prescribes.
What role do thyroid hormones play in pregnancy?
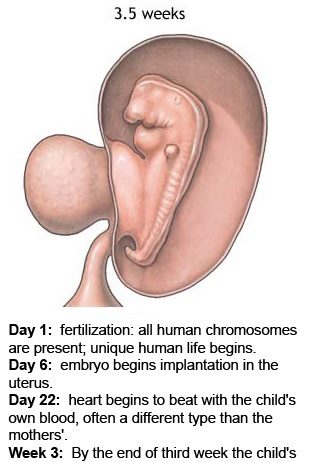
Thyroid hormones are crucial for normal development of your baby’s brain and nervous system.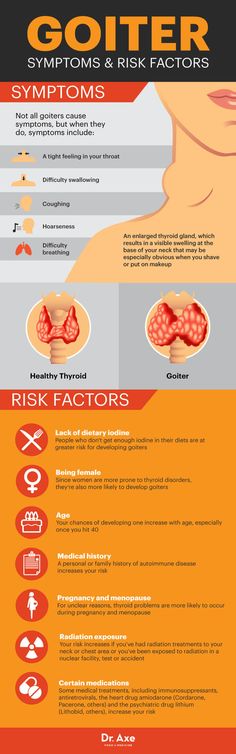 During the first trimester—the first 3 months of pregnancy—your baby depends on your supply of thyroid hormone, which comes through the placenta. At around 12 weeks, your baby’s thyroid starts to work on its own, but it doesn’t make enough thyroid hormone until 18 to 20 weeks of pregnancy.
During the first trimester—the first 3 months of pregnancy—your baby depends on your supply of thyroid hormone, which comes through the placenta. At around 12 weeks, your baby’s thyroid starts to work on its own, but it doesn’t make enough thyroid hormone until 18 to 20 weeks of pregnancy.
Two pregnancy-related hormones—human chorionic gonadotropin (hCG) and estrogen—cause higher measured thyroid hormone levels in your blood. The thyroid enlarges slightly in healthy women during pregnancy, but usually not enough for a health care professional to feel during a physical exam.
Thyroid problems can be hard to diagnose in pregnancy due to higher levels of thyroid hormones and other symptoms that occur in both pregnancy and thyroid disorders. Some symptoms of hyperthyroidism or hypothyroidism are easier to spot and may prompt your doctor to test you for these thyroid diseases.
Another type of thyroid disease, postpartum thyroiditis, can occur after your baby is born.
Hyperthyroidism in Pregnancy
What are the symptoms of hyperthyroidism in pregnancy?
Some signs and symptoms of hyperthyroidism often occur in normal pregnancies, including faster heart rate, trouble dealing with heat, and tiredness.
Other signs and symptoms can suggest hyperthyroidism:
- fast and irregular heartbeat
- shaky hands
- unexplained weight loss or failure to have normal pregnancy weight gain
What causes hyperthyroidism in pregnancy?
Hyperthyroidism in pregnancy is usually caused by Graves’ disease and occurs in 1 to 4 of every 1,000 pregnancies in the United States.1 Graves’ disease is an autoimmune disorder. With this disease, your immune system makes antibodies that cause the thyroid to make too much thyroid hormone. This antibody is called thyroid stimulating immunoglobulin, or TSI.
Graves’ disease may first appear during pregnancy. However, if you already have Graves’ disease, your symptoms could improve in your second and third trimesters. Some parts of your immune system are less active later in pregnancy so your immune system makes less TSI. This may be why symptoms improve. Graves’ disease often gets worse again in the first few months after your baby is born, when TSI levels go up again. If you have Graves’ disease, your doctor will most likely test your thyroid function monthly throughout your pregnancy and may need to treat your hyperthyroidism.1 Thyroid hormone levels that are too high can harm your health and your baby’s.
If you have Graves’ disease, your doctor will most likely test your thyroid function monthly throughout your pregnancy and may need to treat your hyperthyroidism.1 Thyroid hormone levels that are too high can harm your health and your baby’s.
Rarely, hyperthyroidism in pregnancy is linked to hyperemesis gravidarum—severe nausea and vomiting that can lead to weight loss and dehydration. Experts believe this severe nausea and vomiting is caused by high levels of hCG early in pregnancy. High hCG levels can cause the thyroid to make too much thyroid hormone. This type of hyperthyroidism usually goes away during the second half of pregnancy.
Less often, one or more nodules, or lumps in your thyroid, make too much thyroid hormone.
How can hyperthyroidism affect me and my baby?
Untreated hyperthyroidism during pregnancy can lead to
- miscarriage
- premature birth
- low birthweight
- preeclampsia—a dangerous rise in blood pressure in late pregnancy
- thyroid storm—a sudden, severe worsening of symptoms
- congestive heart failure
Rarely, Graves’ disease may also affect a baby’s thyroid, causing it to make too much thyroid hormone. Even if your hyperthyroidism was cured by radioactive iodine treatment to destroy thyroid cells or surgery to remove your thyroid, your body still makes the TSI antibody. When levels of this antibody are high, TSI may travel to your baby’s bloodstream. Just as TSI caused your own thyroid to make too much thyroid hormone, it can also cause your baby’s thyroid to make too much.
Even if your hyperthyroidism was cured by radioactive iodine treatment to destroy thyroid cells or surgery to remove your thyroid, your body still makes the TSI antibody. When levels of this antibody are high, TSI may travel to your baby’s bloodstream. Just as TSI caused your own thyroid to make too much thyroid hormone, it can also cause your baby’s thyroid to make too much.
Tell your doctor if you’ve had surgery or radioactive iodine treatment for Graves’ disease so he or she can check your TSI levels. If they are very high, your doctor will monitor your baby for thyroid-related problems later in your pregnancy.
Tell your doctor if you’ve had surgery or radioactive iodine treatment for Graves’ disease.An overactive thyroid in a newborn can lead to
- a fast heart rate, which can lead to heart failure
- early closing of the soft spot in the baby’s skull
- poor weight gain
- irritability
Sometimes an enlarged thyroid can press against your baby’s windpipe and make it hard for your baby to breathe. If you have Graves’ disease, your health care team should closely monitor you and your newborn.
If you have Graves’ disease, your health care team should closely monitor you and your newborn.
How do doctors diagnose hyperthyroidism in pregnancy?
Your doctor will review your symptoms and do some blood tests to measure your thyroid hormone levels. Your doctor may also look for antibodies in your blood to see if Graves’ disease is causing your hyperthyroidism. Learn more about thyroid tests and what the results mean.
How do doctors treat hyperthyroidism during pregnancy?
If you have mild hyperthyroidism during pregnancy, you probably won’t need treatment. If your hyperthyroidism is linked to hyperemesis gravidarum, you only need treatment for vomiting and dehydration.
If your hyperthyroidism is more severe, your doctor may prescribe antithyroid medicines, which cause your thyroid to make less thyroid hormone. This treatment prevents too much of your thyroid hormone from getting into your baby’s bloodstream. You may want to see a specialist, such as an endocrinologist or expert in maternal-fetal medicine, who can carefully monitor your baby to make sure you’re getting the right dose.
Doctors most often treat pregnant women with the antithyroid medicine propylthiouracil (PTU) during the first 3 months of pregnancy. Another type of antithyroid medicine, methimazole, is easier to take and has fewer side effects, but is slightly more likely to cause serious birth defects than PTU. Birth defects with either type of medicine are rare. Sometimes doctors switch to methimazole after the first trimester of pregnancy. Some women no longer need antithyroid medicine in the third trimester.
Small amounts of antithyroid medicine move into the baby’s bloodstream and lower the amount of thyroid hormone the baby makes. If you take antithyroid medicine, your doctor will prescribe the lowest possible dose to avoid hypothyroidism in your baby but enough to treat the high thyroid hormone levels that can also affect your baby.
Antithyroid medicines can cause side effects in some people, including
- allergic reactions such as rashes and itching
- rarely, a decrease in the number of white blood cells in the body, which can make it harder for your body to fight infection
- liver failure, in rare cases
Stop your antithyroid medicine and call your doctor right away if you develop any of these symptoms while taking antithyroid medicines:
- yellowing of your skin or the whites of your eyes, called jaundice
- dull pain in your abdomen
- constant sore throat
- fever
If you don’t hear back from your doctor the same day, you should go to the nearest emergency room.
You should also contact your doctor if any of these symptoms develop for the first time while you’re taking antithyroid medicines:
- increased tiredness or weakness
- loss of appetite
- skin rash or itching
- easy bruising
If you are allergic to or have severe side effects from antithyroid medicines, your doctor may consider surgery to remove part or most of your thyroid gland. The best time for thyroid surgery during pregnancy is in the second trimester.
Radioactive iodine treatment is not an option for pregnant women because it can damage the baby’s thyroid gland.
Hypothyroidism in Pregnancy
What are the symptoms of hypothyroidism in pregnancy?
Symptoms of an underactive thyroid are often the same for pregnant women as for other people with hypothyroidism. Symptoms include
- extreme tiredness
- trouble dealing with cold
- muscle cramps
- severe constipation
- problems with memory or concentration
Most cases of hypothyroidism in pregnancy are mild and may not have symptoms.
What causes hypothyroidism in pregnancy?
Hypothyroidism in pregnancy is usually caused by Hashimoto’s disease and occurs in 2 to 3 out of every 100 pregnancies.1 Hashimoto’s disease is an autoimmune disorder. In Hashimoto’s disease, the immune system makes antibodies that attack the thyroid, causing inflammation and damage that make it less able to make thyroid hormones.
How can hypothyroidism affect me and my baby?
Untreated hypothyroidism during pregnancy can lead to
- preeclampsia—a dangerous rise in blood pressure in late pregnancy
- anemia
- miscarriage
- low birthweight
- stillbirth
- congestive heart failure, rarely
These problems occur most often with severe hypothyroidism.
Because thyroid hormones are so important to your baby’s brain and nervous system development, untreated hypothyroidism—especially during the first trimester—can cause low IQ and problems with normal development.
How do doctors diagnose hypothyroidism in pregnancy?
Your doctor will review your symptoms and do some blood tests to measure your thyroid hormone levels. Your doctor may also look for certain antibodies in your blood to see if Hashimoto’s disease is causing your hypothyroidism. Learn more about thyroid tests and what the results mean.
How do doctors treat hypothyroidism during pregnancy?
Treatment for hypothyroidism involves replacing the hormone that your own thyroid can no longer make. Your doctor will most likely prescribe levothyroxine, a thyroid hormone medicine that is the same as T4, one of the hormones the thyroid normally makes. Levothyroxine is safe for your baby and especially important until your baby can make his or her own thyroid hormone.
Your thyroid makes a second type of hormone, T3. Early in pregnancy, T3 can’t enter your baby’s brain like T4 can. Instead, any T3 that your baby’s brain needs is made from T4. T3 is included in a lot of thyroid medicines made with animal thyroid, such as Armour Thyroid, but is not useful for your baby’s brain development. These medicines contain too much T3 and not enough T4, and should not be used during pregnancy. Experts recommend only using levothyroxine (T4) while you’re pregnant.
Some women with subclinical hypothyroidism—a mild form of the disease with no clear symptoms—may not need treatment.
Your doctor may prescribe levothyroxine to treat your hypothyroidism.If you had hypothyroidism before you became pregnant and are taking levothyroxine, you will probably need to increase your dose. Most thyroid specialists recommend taking two extra doses of thyroid medicine per week, starting right away. Contact your doctor as soon as you know you’re pregnant.
Your doctor will most likely test your thyroid hormone levels every 4 to 6 weeks for the first half of your pregnancy, and at least once after 30 weeks.1 You may need to adjust your dose a few times.
Postpartum Thyroiditis
What is postpartum thyroiditis?
Postpartum thyroiditis is an inflammation of the thyroid that affects about 1 in 20 women during the first year after giving birth1 and is more common in women with type 1 diabetes. The inflammation causes stored thyroid hormone to leak out of your thyroid gland. At first, the leakage raises the hormone levels in your blood, leading to hyperthyroidism. The hyperthyroidism may last up to 3 months. After that, some damage to your thyroid may cause it to become underactive. Your hypothyroidism may last up to a year after your baby is born. However, in some women, hypothyroidism doesn’t go away.
Not all women who have postpartum thyroiditis go through both phases. Some only go through the hyperthyroid phase, and some only the hypothyroid phase.
What are the symptoms of postpartum thyroiditis?
The hyperthyroid phase often has no symptoms—or only mild ones. Symptoms may include irritability, trouble dealing with heat, tiredness, trouble sleeping, and fast heartbeat.
Symptoms of the hypothyroid phase may be mistaken for the “baby blues”—the tiredness and moodiness that sometimes occur after the baby is born. Symptoms of hypothyroidism may also include trouble dealing with cold; dry skin; trouble concentrating; and tingling in your hands, arms, feet, or legs. If these symptoms occur in the first few months after your baby is born or you develop postpartum depression, talk with your doctor as soon as possible.
If these symptoms occur in the first few months after your baby is born or you develop postpartum depression, talk with your doctor as soon as possible.
What causes postpartum thyroiditis?
Postpartum thyroiditis is an autoimmune condition similar to Hashimoto’s disease. If you have postpartum thyroiditis, you may have already had a mild form of autoimmune thyroiditis that flares up after you give birth.
Postpartum thyroiditis may last up to a year after your baby is born.How do doctors diagnose postpartum thyroiditis?
If you have symptoms of postpartum thyroiditis, your doctor will order blood tests to check your thyroid hormone levels.
How do doctors treat postpartum thyroiditis?
The hyperthyroid stage of postpartum thyroiditis rarely needs treatment. If your symptoms are bothering you, your doctor may prescribe a beta-blocker, a medicine that slows your heart rate. Antithyroid medicines are not useful in postpartum thyroiditis, but if you have Grave’s disease, it may worsen after your baby is born and you may need antithyroid medicines.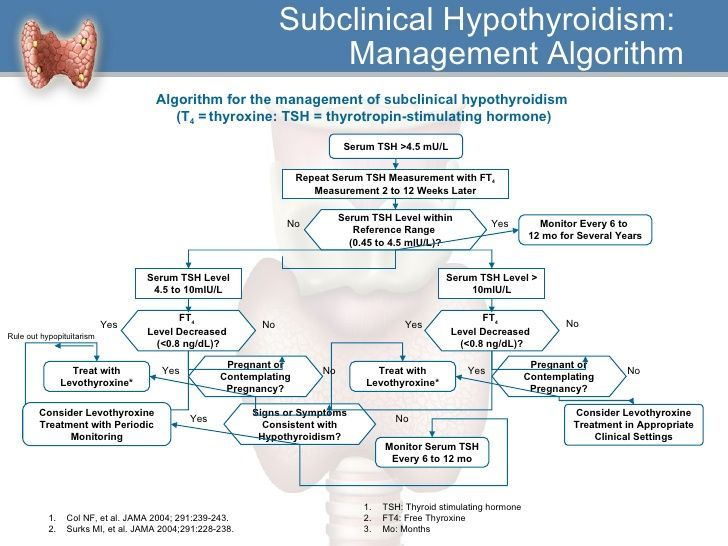
You’re more likely to have symptoms during the hypothyroid stage. Your doctor may prescribe thyroid hormone medicine to help with your symptoms. If your hypothyroidism doesn’t go away, you will need to take thyroid hormone medicine for the rest of your life.
Is it safe to breastfeed while I’m taking beta-blockers, thyroid hormone, or antithyroid medicines?
Certain beta-blockers are safe to use while you’re breastfeeding because only a small amount shows up in breast milk. The lowest possible dose to relieve your symptoms is best. Only a small amount of thyroid hormone medicine reaches your baby through breast milk, so it’s safe to take while you’re breastfeeding. However, in the case of antithyroid drugs, your doctor will most likely limit your dose to no more than 20 milligrams (mg) of methimazole or, less commonly, 400 mg of PTU.
Thyroid Disease and Eating During Pregnancy
What should I eat during pregnancy to help keep my thyroid and my baby’s thyroid working well?
Because the thyroid uses iodine to make thyroid hormone, iodine is an important mineral for you while you’re pregnant. During pregnancy, your baby gets iodine from your diet. You’ll need more iodine when you’re pregnant—about 250 micrograms a day.1 Good sources of iodine are dairy foods, seafood, eggs, meat, poultry, and iodized salt—salt with added iodine. Experts recommend taking a prenatal vitamin with 150 micrograms of iodine to make sure you’re getting enough, especially if you don’t use iodized salt.1 You also need more iodine while you’re breastfeeding since your baby gets iodine from breast milk. However, too much iodine from supplements such as seaweed can cause thyroid problems. Talk with your doctor about an eating plan that’s right for you and what supplements you should take. Learn more about a healthy diet and nutrition during pregnancy.
During pregnancy, your baby gets iodine from your diet. You’ll need more iodine when you’re pregnant—about 250 micrograms a day.1 Good sources of iodine are dairy foods, seafood, eggs, meat, poultry, and iodized salt—salt with added iodine. Experts recommend taking a prenatal vitamin with 150 micrograms of iodine to make sure you’re getting enough, especially if you don’t use iodized salt.1 You also need more iodine while you’re breastfeeding since your baby gets iodine from breast milk. However, too much iodine from supplements such as seaweed can cause thyroid problems. Talk with your doctor about an eating plan that’s right for you and what supplements you should take. Learn more about a healthy diet and nutrition during pregnancy.
Clinical Trials
The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) and other components of the National Institutes of Health (NIH) conduct and support research into many diseases and conditions.
What are clinical trials, and are they right for you?
Clinical trials are part of clinical research and at the heart of all medical advances. Clinical trials look at new ways to prevent, detect, or treat disease. Researchers also use clinical trials to look at other aspects of care, such as improving the quality of life for people with chronic illnesses. Find out if clinical trials are right for you.
What clinical trials are open?
Clinical trials that are currently open and are recruiting can be viewed at www.ClinicalTrials.gov.
References
Thyroid gland and pregnancy - GAUZ City Clinical Hospital No. 9
The thyroid gland is a small, butterfly-shaped organ located on the front of the neck. Its weight is on average 18-30 and depends on the region of residence. The thyroid gland produces the most important hormones for the body: thyroxine (or T4) and triiodothyronine (TK), the material for them is amino acid and iodine. The functions of the thyroid gland are monitored by the "superior" glands - the pituitary gland (which produces the thyroid-stimulating hormone TSH) and the hypothalamus.
Thyroid hormones perform a number of important functions in the body. First of all, they regulate the basic metabolism, i.e. the production of energy necessary for the life of the whole organism. Also, thyroid hormones affect the laying and intrauterine development of such organs and systems of the child as the nervous, cardiovascular, reproductive systems, musculoskeletal system, etc. In the first three years of life, they are especially important for the normal functioning of the brain, in the future, for the development and maintenance of intelligence.
In order for the thyroid gland to be able to produce the hormones T3 and T4 in the amount necessary for the body, 150-200 micrograms of iodine with food should enter the human body per day. During pregnancy and lactation, this need increases to 250-300 mcg. A large territory of Russia, including the Ural region, is a zone of iodine deficiency, therefore, meat, fish, dairy and vegetable products eaten do not satisfy the body's daily need for iodine. Together with the deteriorating environmental situation, harmful, but common habits of young people (smoking, alcohol), this leads to the development of iodine deficiency conditions.
Together with the deteriorating environmental situation, harmful, but common habits of young people (smoking, alcohol), this leads to the development of iodine deficiency conditions.
An underactive thyroid (hypothyroidism) and an overactive thyroid (hyperthyroidism) cause certain problems. How do they threaten a pregnant woman and her offspring?
Iodine deficiency can lead to low levels of thyroid hormones even before pregnancy. Therefore, when planning a pregnancy, it is very important to consult an endocrinologist, especially if you notice any signs of hypothyroidism (weakness, weight gain, drowsiness, decreased memory and speed of thinking, dry skin, brittle nails, hair loss, menstrual irregularities). , decreased blood pressure, hoarseness).
The thyroid gland and pregnancy.
If you find that you have a decrease in thyroid function and find out the cause, most likely, the doctor will prescribe you replacement therapy, i.e. “Add” a certain amount of thyroxine to the body. Thyroxine will also need to be taken during pregnancy and breastfeeding.
Thyroxine will also need to be taken during pregnancy and breastfeeding.
Hypothyroidism during pregnancy can lead to spontaneous abortion, fetal death, the birth of a child with malformations, mental retardation, psychomotor disorders. To avoid these complications, in addition to taking thyroxin, it is necessary to carry out iodine prophylaxis: daily take a drug containing potassium iodide at a dose of 250 mcg. Hormone doses are set only by an endocrinologist, so his consultations are necessary during pregnancy. In addition to adding tableted iodine, it is necessary to include seafood (shrimp, seaweed, squid), dairy products, and meat in the diet of a pregnant woman. It must be remembered that from the first weeks of pregnancy, the unborn child receives hormones and trace elements from the mother. The laying of the thyroid gland in the fetus occurs by 4-5 weeks of intrauterine development, from the 12th week this thyroid gland is able to synthesize hormones by itself, and by the 16th week it is fully formed and functioning.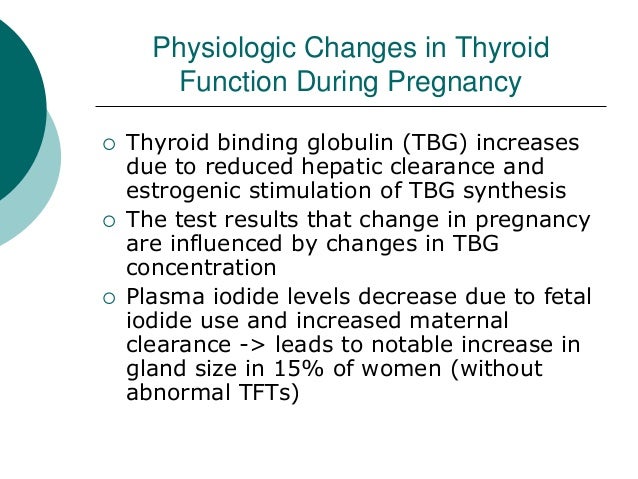 But the only source of iodine for her is the iodine circulating in the mother's blood.
But the only source of iodine for her is the iodine circulating in the mother's blood.
In the first trimester, the mother's thyroid gland works hard, "covering" the unformed thyroid gland of the fetus. This is manifested by temporary (transient) hyperthyroidism. Most often it does not require any treatment and goes away on its own. But diffuse toxic goiter (DTG) may develop, requiring timely treatment. Possible complaints in hyperthyroidism: weakness, weight loss, feeling hot, hot skin, irritability, nervousness, tearfulness, palpitations, rapid pulse, increased blood pressure, muscle weakness, trembling of the hands, body, loose stools, sweating, menstrual irregularities, shine eyes, widened palpebral fissures.
Having such complaints, a pregnant woman should report them to her gynecologist and be sure to consult an endocrinologist. After all, mood changes, sensations of heat, vomiting, some weight loss can be manifestations of early toxicosis or symptoms of diffuse toxic goiter. In addition, with diffuse toxic goiter, an increase in the thyroid gland, tachycardia (more than 100 beats per minute), the difference between systolic and diastolic pressure will attract attention. The main diagnostic role is played by the determination of the content of the level of thyroid hormones and thyroid-stimulating hormone of the pituitary gland.
In addition, with diffuse toxic goiter, an increase in the thyroid gland, tachycardia (more than 100 beats per minute), the difference between systolic and diastolic pressure will attract attention. The main diagnostic role is played by the determination of the content of the level of thyroid hormones and thyroid-stimulating hormone of the pituitary gland.
The prognosis for the mother and fetus depends on how much hyperthyroidism is compensated.
With hyperthyroidism, premature birth, malformations of the newborn, low fetal weight, severe gestosis, severe fetal hypothyroidism are possible.
In all cases, the treatment of thyrotoxicosis is carried out by a doctor !!!
Very low doses are used to suppress maternal thyroid function, and sometimes surgery is required.
After childbirth, the woman's immune system, which was suppressed during pregnancy, is restored. There is a surge in the activity of the immune system, antibodies are produced that destroy thyroid cells. In 3-5% of young mothers, postpartum thyroiditis develops 1-3 months after birth. Its peculiarity is the change of the phase of a moderate increase in the function of the thyroid gland by the phase of a moderate decrease in its function. As a rule, after 6-8 months, the immune system returns to normal and postpartum thyroiditis disappears. It must be remembered that postpartum thyroiditis increases the likelihood of developing persistent hypothyroidism in the future with all its clinical manifestations that interfere with normal life.
In 3-5% of young mothers, postpartum thyroiditis develops 1-3 months after birth. Its peculiarity is the change of the phase of a moderate increase in the function of the thyroid gland by the phase of a moderate decrease in its function. As a rule, after 6-8 months, the immune system returns to normal and postpartum thyroiditis disappears. It must be remembered that postpartum thyroiditis increases the likelihood of developing persistent hypothyroidism in the future with all its clinical manifestations that interfere with normal life.
In summary, it is recommended that all women planning pregnancy have their thyroid function tested before it occurs. Timely iodine prophylaxis will prevent the birth of children with low intellectual abilities. If a woman went to the doctor after pregnancy, the thyroid gland should be examined as early as possible and start taking iodine-containing drugs. It must be remembered that a high need for iodine persists in children immediately after birth and those who are both natural and artificially fed. A nursing mother should continue taking iodine supplements for the entire period of feeding. If the child is on artificial feeding, it is necessary to use milk mixtures with a high content of iodine.
A nursing mother should continue taking iodine supplements for the entire period of feeding. If the child is on artificial feeding, it is necessary to use milk mixtures with a high content of iodine.
Thus, you will provide your offspring with a good level of thyroid hormones, which means you will improve the formation of his cognitive abilities, improve intellectual development, in the future this will manifest itself in a high IQ of the child and reduce his morbidity.
Obstetrician-gynecologist, endocrinologist MBUZ City Clinical Hospital No. 9,
Chernysheva E.V.
Thyroid gland - we keep it under control
Important hormones
The main task of the thyroid gland - is the production of hormones: thyroxine - T4 (tetraiodothyronine) and T3 (triiodothyronine). It is these hormones that throughout life support the work of the brain, heart, muscles, regulate the metabolism in the body. So our mental abilities, body weight, physical activity, sexual development, skeletal bone strength, skin and hair condition, sleep and appetite depend on the thyroid gland.:strip_icc():format(jpeg)/kly-media-production/medias/2785562/original/028627600_1556001360-shutterstock_1019963743.jpg) The thyroid gland works correctly - a person is alert, active, calm, feels good and looks good. There are violations in its activity - the symptoms can be very different: for example, let's take body weight. With increased production of thyroid hormones, a person can eat as much as he wants, but will lose weight. And with a reduced function, you can eat nothing at all, but gain weight, because the so-called mucous edema develops in the body. And the matter will not be at all in nutrition, but in the thyroid gland.
The thyroid gland works correctly - a person is alert, active, calm, feels good and looks good. There are violations in its activity - the symptoms can be very different: for example, let's take body weight. With increased production of thyroid hormones, a person can eat as much as he wants, but will lose weight. And with a reduced function, you can eat nothing at all, but gain weight, because the so-called mucous edema develops in the body. And the matter will not be at all in nutrition, but in the thyroid gland.
Essential iodine
Various factors affect how the thyroid gland functions: even stress and insomnia can disrupt the production of its hormones. But still, most of all, for normal functioning of the thyroid gland, iodine is needed, it is from it that thyroid hormones consist of 65%. Our body cannot produce this microelement on its own, we get it only from the outside - from food, water or medicines. And if there is little iodine in the diet, then, therefore, the thyroid gland will not be able to produce the required amount of hormones. In ordinary life, of course, this is also bad, but not yet so critical, but during pregnancy, iodine deficiency can cause real problems. After all, now this trace element is needed not only by a woman, but also by her child. Both the very bearing of the baby and his health will be under threat: after all, as mentioned above, the thyroid gland affects all organs and systems.
In ordinary life, of course, this is also bad, but not yet so critical, but during pregnancy, iodine deficiency can cause real problems. After all, now this trace element is needed not only by a woman, but also by her child. Both the very bearing of the baby and his health will be under threat: after all, as mentioned above, the thyroid gland affects all organs and systems.
Development of the baby
Let's start with the fact that the baby is completely dependent on the mother's thyroid gland. In the unborn child, the thyroid gland, although it begins to form already at the 4–5th week of pregnancy, but it begins to function, that is, it begins to produce hormones only at 12 weeks, and it is capable of finally working at full strength by the 16–17th week. pregnancy. Until that time, the development of the child and the laying of all his organs and systems are "under the protection" of the mother's thyroid gland. And if a woman has little iodine, then this means that some system or organ of the baby may suffer. And even when the child’s own thyroid gland is formed and starts working, she can still take iodine only from the mother’s body.
And even when the child’s own thyroid gland is formed and starts working, she can still take iodine only from the mother’s body.
Iodine deficiency most strongly affects intellectual development, even if a child is born physically healthy, his mental abilities may be lower than those of his peers.
In slow motion
Lack of iodine leads to the development of hypothyroidism – decrease in the production of thyroid hormones , which means that energy is produced less intensively and all processes in the body slow down. At first, the woman feels weak, she constantly wants to sleep. Hair fades, splits and falls out, nails exfoliate and break. There is excess weight, constipation, a feeling of chilliness. With developed hypothyroidism, the face becomes puffy, the eyelids swell, dry skin flakes and sometimes even turns slightly yellow. Due to swelling of the vocal cords, the voice may become lower. Many of these symptoms of hypothyroidism are similar to the usual “troubles” of pregnancy (especially weakness, drowsiness, excess weight, constipation), but if they are significantly pronounced, there is a reason for examining the thyroid gland. So if the expectant mother is tired, looks bad, she does not care what is happening around, do not blame everything on pregnancy or beriberi. Perhaps there are problems with the thyroid gland.
So if the expectant mother is tired, looks bad, she does not care what is happening around, do not blame everything on pregnancy or beriberi. Perhaps there are problems with the thyroid gland.
Change of mood
When pregnancy begins, when the thyroid gland starts working for two, it enlarges a little and produces a little more hormones. This is a common occurrence, and after pregnancy everything will return to normal. But there are women in whom, for some reason, the thyroid gland begins to produce too many hormones and without the influence of pregnancy, hyperthyroidism (or thyrotoxicosis) occurs. Then other symptoms appear - imbalance, tearfulness, agitation, increased appetite, slight trembling in the hands, sleep disturbances. The body temperature can rise to small values for no reason, the head often hurts, the heart beats faster, and blood pressure rises. If such symptoms appear, especially if there is still vomiting that seems to be normal for pregnant women with significant weight loss, an examination of the thyroid gland is necessary.
Going to the doctor
If the future mother has not been to an endocrinologist before, now is the time to visit this specialist and, possibly, do a blood test to determine the level of thyroid hormones.
Even if everything is in order with the thyroid gland, the doctor will still recommend taking either a separate medicine with iodine or a vitamin complex. The fact is that in Russia, in most regions, both water and food contain little iodine, so that it does not come with enough food. Moreover, if before pregnancy the daily dose of iodine was 150 mcg, now the expectant mother should take 200 mcg already. But still, before taking even harmless vitamins with iodine, it is better to check the level of thyroid hormones.
Also, in order to prevent iodine deficiency, you can salt your food with iodized salt (although salt itself is not healthy). A lot of iodine is found in sea fish, seaweed, squid, persimmon, feijoa, dates, dried figs, dairy products and meat.
Pay attention to the thyroid gland, and it will definitely help you look and feel good!
Attention! Prices for services in different clinics may vary. To clarify the current cost, select a clinic
Clinical Hospital MD GROUPClinical Hospital Lapino-1 "Mother and Child"Clinic KG "Lapino" in Odintsovo (branch)Clinic "Mother and Child" Khodynskoye PoleClinic "Mother and Child" KuntsevoClinic "Mother and Child" SavelovskayaClinic "Mother and Child" Yugo-ZapadMother and Child Clinic NovogireevoMother and Child Clinic Lefortovo
All directionsSpecialist consultations (adults)Specialist consultations (children)Laboratory of molecular geneticsGeneral clinical studiesTreatment roomTelemedicine for adultsTherapeutic studiesUltrasound examinations for adults
01.