Pregnant women with hiv
HIV Medicines During Pregnancy and Childbirth
HIV Medicines During Pregnancy and Childbirth
Last Reviewed: August 18, 2021
Key Points
- All pregnant women with HIV should take HIV medicines throughout pregnancy for their own health and to prevent perinatal transmission of HIV. (HIV medicines are called antiretrovirals). Perinatal transmission of HIV is also called mother-to-child transmission of HIV.
- Most HIV medicines are safe to use during pregnancy. In general, HIV medicines do not increase the risk of birth defects.
- Generally, pregnant women with HIV can use the same HIV treatment regimens recommended for non-pregnant adults—unless the risk of any known side effects to a pregnant woman or her baby outweighs the benefits of a treatment regimen.
- All pregnant women with HIV should start taking HIV medicines as soon as possible during pregnancy.
In most cases, women who are already on an effective HIV treatment regimen when they become pregnant should continue using the same regimen throughout their pregnancies.
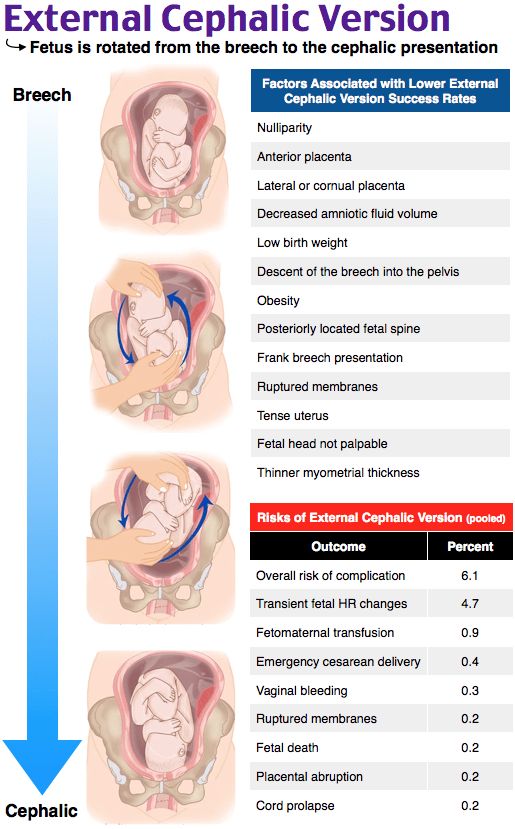
- A scheduled cesarean delivery (sometimes called a C-section) to prevent perinatal transmission of HIV is recommended for women who have high or unknown viral loads near the time of delivery.
Should women with HIV take HIV medicines during pregnancy?
Yes. All pregnant women with HIV should take HIV medicines throughout pregnancy for their own health and to prevent perinatal transmission of HIV. (HIV medicines are called antiretrovirals.) Perinatal transmission of HIV is also called mother-to-child transmission of HIV.
HIV medicines, when taken as prescribed, prevent HIV from multiplying and reduce the amount of HIV in the body (called the viral load). An undetectable viral load is when the level of HIV in the blood is too low to be detected by a viral load test. The risk of perinatal transmission of HIV during pregnancy and childbirth is lowest when a woman with HIV has an undetectable viral load. Maintaining an undetectable viral load also helps keep the mother-to-be healthy.
The risk of perinatal transmission of HIV during pregnancy and childbirth is lowest when a woman with HIV has an undetectable viral load. Maintaining an undetectable viral load also helps keep the mother-to-be healthy.
Are HIV medicines safe to use during pregnancy?
Most HIV medicines are safe to use during pregnancy. In general, HIV medicines do not increase the risk of birth defects.
When recommending HIV medicines to use during pregnancy, health care providers consider the benefits and risks of specific HIV medicines for women and their unborn babies.
When should pregnant women with HIV start taking HIV medicines?
All pregnant women with HIV should start taking HIV medicines as soon as possible during pregnancy. In most cases, women who are already on an effective HIV treatment regimen when they become pregnant should continue using the same regimen throughout their pregnancies.
What HIV medicines should a pregnant woman with HIV take?
The choice of an HIV treatment regimen to use during pregnancy depends on several factors, including a woman’s current or past use of HIV medicines, other medical conditions she may have, and the results of drug-resistance testing. In general, pregnant women with HIV can use the same HIV treatment regimens recommended for non-pregnant adults—unless the risk of any known side effects to a pregnant woman or her baby outweighs the benefits of a treatment regimen.
Sometimes, a woman’s HIV treatment regimen may change during pregnancy. Women and their health care providers should discuss whether any changes need to be made to an HIV treatment regimen during pregnancy.
Do women with HIV continue to take HIV medicines during childbirth?
Yes. A baby is exposed to any HIV in the mother's blood and other fluids while passing through the birth canal. During childbirth, HIV medicines that pass from mother to baby across the placenta prevent perinatal transmission of HIV, especially near delivery.
During childbirth, HIV medicines that pass from mother to baby across the placenta prevent perinatal transmission of HIV, especially near delivery.
Women who are already taking HIV medicines when they go into labor should continue taking their HIV medicines on schedule as much as possible during childbirth.
Can a cesarean delivery reduce the risk of perinatal transmission of HIV?
Yes. A scheduled cesarean delivery (sometimes called a C-section) can reduce the risk of perinatal transmission of HIV in women who have a high viral load (more than 1,000 copies/mL) or an unknown viral load near the time of delivery. A cesarean delivery to reduce the risk of perinatal transmission of HIV is scheduled for the 38th week of pregnancy, 2 weeks before a woman’s expected due date.
A scheduled C-section to reduce the risk of perinatal transmission of HIV is not routinely recommended for women who are taking HIV medicines and have a viral load of 1,000 copies/mL or less. Of course, regardless of her viral load, a woman with HIV may have a C-section for other medical reasons.
Of course, regardless of her viral load, a woman with HIV may have a C-section for other medical reasons.
With the help of their health care providers, women can decide which HIV medicines to use during childbirth and whether they should have a scheduled C-section to prevent perinatal transmission of HIV.
Do women with HIV continue to take HIV medicines after childbirth?
Prenatal care for women with HIV includes counseling on the benefits of continuing HIV medicines after childbirth. HIV medicines help people with HIV live longer, healthier lives and reduce the risk of HIV transmission. Together with their health care providers, women with HIV make decisions about continuing or changing their HIV medicines after childbirth.
After birth, babies born to women with HIV receive HIV medicine to reduce the risk of perinatal transmission of HIV. Several factors determine what HIV medicine they receive and how long they receive the medicine.
To learn more, read the HIVinfo fact sheet on Preventing Perinatal Transmission of HIV After Birth.
This fact sheet is based on information from the following sources:
From the Department of Health and Human Services:
- Recommendations for the Use of Antiretroviral Drugs in Pregnant Women with HIV Infection and Interventions to Reduce Perinatal HIV Transmission in the United States:
- What's New in the Guidelines
- General Principles Regarding Use of Antiretroviral Drugs During Pregnancy: Teratogenicity
- Recommendations for Use of Antiretroviral Drugs During Pregnancy: Overview
- Intrapartum Care for Women with HIV
- Management of Infants Born to Women with HIV Infection: Antiretroviral Management of Newborns with Perinatal HIV Exposure or HIV Infection
Also see the HIV Source collection of HIV links and resources.
Pregnancy and HIV | Office on Women's Health
A diagnosis of HIV does not mean you can't have children. But you can pass HIV to your baby during the pregnancy, while in labor, while giving birth, or by breastfeeding. The good news is that there are many ways to lower the risk of passing HIV to your unborn baby to almost zero.
But you can pass HIV to your baby during the pregnancy, while in labor, while giving birth, or by breastfeeding. The good news is that there are many ways to lower the risk of passing HIV to your unborn baby to almost zero.
What can I do before getting pregnant to lower my risk of passing HIV to my baby?
If you plan to become pregnant, talk to your doctor right away. Your doctor can talk with you about how HIV can affect your health during pregnancy and your unborn baby's health. Your doctor can work with you to prepare for a healthy pregnancy before you start trying to become pregnant.
Everyone living with HIV should take HIV medicines to stay healthy. If you are thinking about becoming pregnant and are not taking HIV treatment, it is important that you begin, because this will lower your chances of passing the virus to your baby when you become pregnant.
There are ways for you to get pregnant that will limit your partner's risk of HIV infection. You can ask your doctor about ways to get pregnant and still protect your partner.
I do not have HIV, but my partner does. Can I get pregnant without getting HIV?
Women have a higher risk of HIV infection during vaginal sex than men. If you do not have HIV but your male partner does, the risk of getting HIV while trying to get pregnant can be reduced but not totally eliminated.
Talk to your doctor about HIV medicine you can take (called pre-exposure prophylaxis or PrEP) to help protect you and your baby from HIV.
You may also want to consider donor sperm or assisted reproductive technology, such as semen washing or in vitro fertilization, to get pregnant. These options can be expensive and may not be covered by your health insurance.
I'm pregnant. Will my baby have HIV?
If you just found out you are pregnant, see your doctor right away. Find out what you can do to take care of yourself and to give your baby a healthy start to life.
With your doctor's help, you can decide on the best treatment for you and your baby before, during, and after the pregnancy. You should also take these steps before and during your pregnancy to help you and your baby stay healthy.
You should also take these steps before and during your pregnancy to help you and your baby stay healthy.
Just because you have HIV doesn't mean your child will get HIV. In the United States, before effective treatment was available, about 25% of pregnant mothers with HIV passed the virus to their babies. Today, if you take HIV treatment and have an undetectable viral load, your risk of passing HIV to your baby is less than 1%.1
What can I do to lower my risk of passing HIV to my baby?
Thanks to more HIV testing and new medicines, the number of children infected with HIV during pregnancy, labor and childbirth, and breastfeeding has decreased by 90% since the mid-1990s.1
The steps below can lower the risk of giving HIV to your baby:
Tell your doctor you want to get pregnant. Your doctor can help you decide if you need to change your treatments to lower your viral load, to help you get pregnant without passing HIV to your partner, and to prevent you from passing the virus to your baby. He or she will also help you get as healthy as possible before you get pregnant to improve your chances of a healthy pregnancy and baby. Don't stop using condoms for STI prevention and another method of birth control for pregnancy prevention until your doctor says you are healthy enough to start trying.
He or she will also help you get as healthy as possible before you get pregnant to improve your chances of a healthy pregnancy and baby. Don't stop using condoms for STI prevention and another method of birth control for pregnancy prevention until your doctor says you are healthy enough to start trying.
Get prenatal care. Prenatal care is the care you receive from your doctor while you are pregnant. You need to work closely with your doctor throughout your pregnancy to monitor your treatment, your health, and your baby's health.
Start HIV treatment. You can start treatment before pregnancy to lower the risk of passing HIV to your baby. If you are already on treatment, do not stop, but do see your doctor right away. Some HIV drugs should not be used while you're pregnant. For other drugs, you may need a different dosage.
Manage side effects. Side effects from HIV medicines can be especially challenging during pregnancy, but it is still important that you take your medicine as directed by your doctor. Talk to your doctor about any side effects you have and about ways to manage them.
Talk to your doctor about any side effects you have and about ways to manage them.
Do not breastfeed. You can pass the virus to your baby through your breastmilk even if you are taking medicine. The best way to avoid passing HIV to your baby is to feed your infant formula instead of breastfeeding.
Make sure your baby is tested for HIV right after birth. You should choose a doctor or clinic experienced in caring for babies exposed to HIV. They will tell you what follow-up tests your baby will need and when. Talk to your doctor about whether your baby may benefit from starting treatment right away.
Ask your pediatric HIV specialist if your baby might benefit from anti-HIV medicines before you know if your baby is HIV-positive or HIV-negative. Research has shown that giving combination HIV drugs to newborns is better at preventing HIV than taking AZT (azidothymidine, an antiretroviral medicine) alone.
Can I take HIV medicine during pregnancy?
HIV-infected pregnant women should take HIV medicines. These medicines can lower the risk of passing HIV to a baby and improve the mother's health.
These medicines can lower the risk of passing HIV to a baby and improve the mother's health.
If you haven't used any HIV drugs before pregnancy and are in your first trimester, your doctor will help you decide if you should start treatment. Here are some things to consider:
- Nausea and vomiting may make it hard to take the HIV medicine early during pregnancy.
- It is possible the medicine may affect your baby. Your doctor will prescribe medicine that is safe to use during pregnancy.
- HIV is more commonly passed to a baby late in pregnancy or during delivery. HIV can be passed early in pregnancy if your viral load is detectable.
- Studies show treatment works best at preventing HIV in a baby if it is started before pregnancy or as early as possible during pregnancy.
If you are taking HIV drugs and find out you're pregnant in the first trimester, talk to your doctor about sticking with your current treatment plan. Some things you can talk about with your doctor include:
Some things you can talk about with your doctor include:
- Whether to continue or stop HIV treatment in the first trimester. Stopping HIV medicine could cause your viral load to go up. If your viral load goes up, the risk of infection also goes up. Your disease also could get worse and cause problems for your baby. So this is a serious decision to make with your doctor.
- What effects your HIV medicines may have on the baby
- Whether you are at risk for drug resistance. This means the HIV medicine you take no longer works against HIV. Never stop taking your HIV medicine without first talking to your doctor.
Can I get help paying for care during pregnancy?
If you are pregnant, Medicaid may pay for your prenatal care. If you are pregnant and living with HIV, Medicaid might pay for counseling, medicine to lower the risk of passing HIV to your baby, and treatment for HIV. Each state makes its own rules regarding Medicaid. Contact your local or county medical assistance, welfare, or social services office to learn more.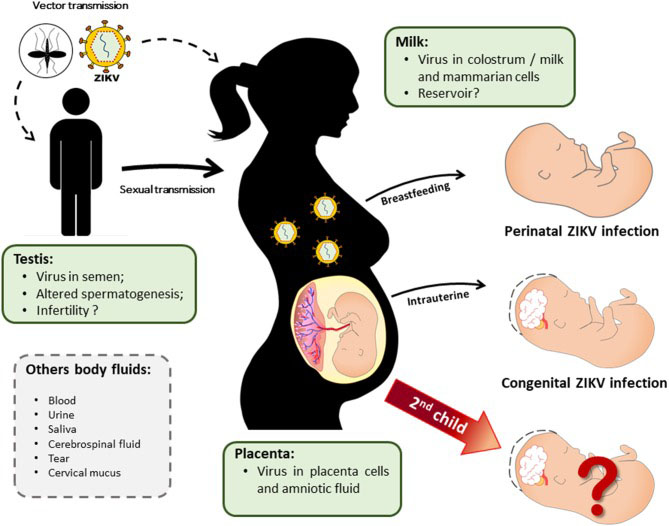 If you are unable to find that number, search your state's department of health.
If you are unable to find that number, search your state's department of health.
If you don't think you qualify for assistance, check again. Sometimes states change their Medicaid rules. Under the Affordable Care Act, Medicaid eligibility expanded to cover many more people. Also, you may be newly eligible for Medicaid because of increased income limits for prenatal care and HIV treatment for pregnant women.
You may also access care through the Ryan White HIV/AIDS Program. Find a Ryan White HIV/AIDS Program medical care provider near you.
Did we answer your question about HIV and pregnancy?
For more information about HIV and pregnancy, call the OWH Helpline at 1-800-994-9662 or check out the following resources from other organizations:
- HIV Among Pregnant Women, Infants, and Children — Fact sheet from the Centers for Disease Control and Prevention (CDC).
- HIV and Pregnancy — Information from AIDSinfo.
- Infant feeding and HIV — Publication from UNICEF.
- Elimination of Mother-to-Child HIV Transmission (EMCT) in the United States — Fact sheet from CDC.
- One Test. Two Lives. — Campaign information from the CDC.
Sources
- Centers for Disease Control and Prevention. (2016). HIV Among Pregnant Women, Infants, and Children.
All material contained on these pages are free of copyright restrictions and maybe copied, reproduced, or duplicated without permission of the Office on Women’s Health in the U.S. Department of Health and Human Services. Citation of the source is appreciated.
Page last updated: February 18, 2021
Pregnancy and childbirth in HIV-positive women
A little more than thirty years have passed since the discovery and description of the human immunodeficiency virus, and in this relatively short period, HIV infection has not only reached the level of an epidemic, but has also significantly changed its prevalence. In recent years, there has been a transition of HIV infection from drug users and persons practicing homosexual contacts to the general population, which leads to an increase in the proportion of women among HIV-infected people.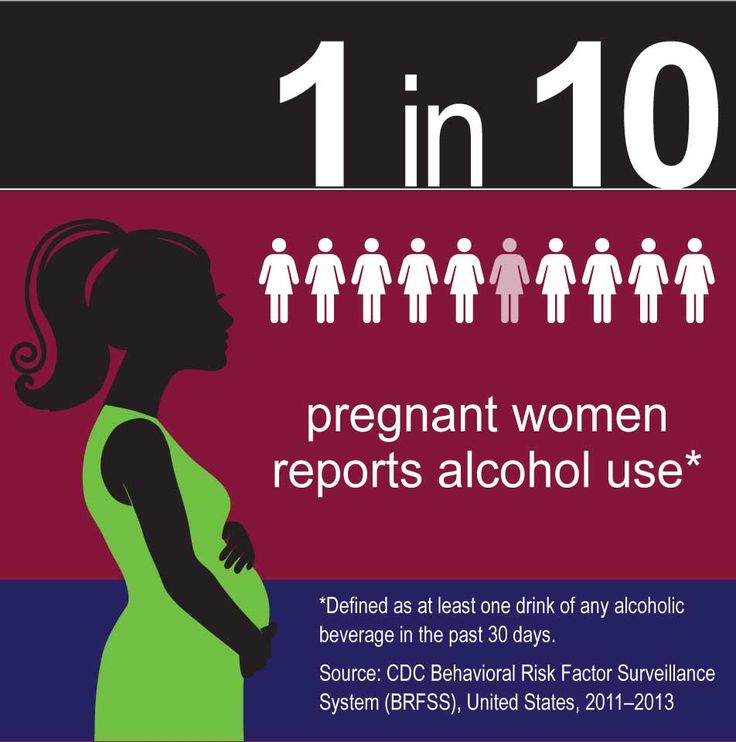 According to the latest data, women of reproductive age make up more than half of all HIV-positive women. The tragedy of recent years has been the increase in the number of HIV-infected pregnant women. In some Russian regions, the frequency of their detection has increased 600 times over the past 10 years. nine0003
According to the latest data, women of reproductive age make up more than half of all HIV-positive women. The tragedy of recent years has been the increase in the number of HIV-infected pregnant women. In some Russian regions, the frequency of their detection has increased 600 times over the past 10 years. nine0003
According to current concepts, the detection of HIV infection in a pregnant woman is an indication for the prevention of mother-to-child transmission of HIV, and not for termination of pregnancy. The desired pregnancy must be maintained, and the doctor must take all necessary steps to successfully carry out drug prophylaxis and other preventive measures.
Without preventive measures, mother-to-child transmission of HIV is 20–40%; the use of special preventive measures reduces the transmission of infection to 1–2%. nine0003
Ideally, every HIV-infected woman should receive pregnancy preparation, including reproductive and physical health assessments, STI testing, folic acid administration to both spouses. It is mandatory to consult an infectious disease specialist in order to correct antiretroviral (ARV) therapy. All pregnancy planning activities are carried out three months before the abolition of contraception.
It is mandatory to consult an infectious disease specialist in order to correct antiretroviral (ARV) therapy. All pregnancy planning activities are carried out three months before the abolition of contraception.
When pregnancy occurs against the background of HIV infection, as well as when HIV infection is first detected during pregnancy, a woman is referred for a consultation by an infectious disease specialist at the Center for the Prevention and Control of AIDS in order to prescribe ARV drugs, taking into account the stage of HIV infection , the state of the patient's immune system and the effect of drugs on the fetus. Such centers operate in all regions of the Russian Federation. nine0003
The objective of prescribing ARV drugs during pregnancy is to suppress the reproduction of HIV in the woman's body as much as possible, and, as a result, reduce the risk of HIV transmission to the fetus.
A pregnant woman must clearly understand that the effectiveness of ARV prophylaxis is determined by the conscientiousness of fulfilling all medical prescriptions. It is important not only to strictly adhere to the prescribed regimen for taking medications, but also to regularly visit an infectious disease specialist to study the effectiveness of the prescribed therapy, the state of the immune system and the activity of the infectious process. nine0003
It is important not only to strictly adhere to the prescribed regimen for taking medications, but also to regularly visit an infectious disease specialist to study the effectiveness of the prescribed therapy, the state of the immune system and the activity of the infectious process. nine0003
Screening is done every four weeks and includes CD4 count, viral load, clinical and biochemical blood tests.
Viral load testing 2 weeks before the expected date of delivery (36-38 weeks) is essential to select the method of delivery. According to WHO recommendations, if the viral load is above 1000 copies of HIV RNA per ml of blood plasma, a planned caesarean section is recommended at the 38th week of pregnancy. nine0003
When conducting vaginal delivery, preventive measures are mandatory to reduce the risk of infection of the newborn, including, among other things, continuing to take ARV drugs.
In the postpartum period, all HIV-positive women are advised to stop breastfeeding, as the risk of infection in the newborn reaches 20%.
Operative delivery, refusal of breastfeeding are forced measures, but necessary, since the characteristics of the course of labor and breastfeeding itself are the most dangerous in terms of transmission of infection from mother to child. After all, health is the main thing that a woman can give to her baby! nine0003
Obstetrician-gynecologist
antenatal clinic No. 14
Khivrich E.B.
Tags: pregnancy
HIV and pregnancy
Every pregnant woman registered in the antenatal clinic must be tested for HIV twice - at the first visit and in the third trimester. If a positive or doubtful test for antibodies to HIV is detected, the woman is immediately sent for a consultation to the AIDS Center to clarify the diagnosis. nine0003
Mother-to-child transmission of HIV is possible during pregnancy, more often during late pregnancy, during childbirth and while breastfeeding.
Without preventive measures, the risk of HIV transmission is up to 30%. The risk of infection of the child increases if the mother was infected within six months before the onset of pregnancy or during pregnancy, and also if the pregnancy occurred in the late stages of HIV infection. The risk increases with a high viral load (the amount of virus in the blood) and low immunity. An increase in the risk of infection of the child occurs with repeated pregnancies. nine0003
The risk of infection of the child increases if the mother was infected within six months before the onset of pregnancy or during pregnancy, and also if the pregnancy occurred in the late stages of HIV infection. The risk increases with a high viral load (the amount of virus in the blood) and low immunity. An increase in the risk of infection of the child occurs with repeated pregnancies. nine0003
With proper preventive measures, the risk of mother-to-child transmission of HIV infection is reduced to 2%.
In this brochure you will find information on how to reduce the risk of infection of a child and on the terms of dispensary observation of a child at the AIDS Center.
Reducing the risk of mother-to-child transmission of HIV infection
When contacting the AIDS Center, a pregnant woman receives advice from an infectious disease specialist, an obstetrician-gynecologist, a pediatrician; passes all the necessary tests (viral load, immune status, etc.), after which the issue of prescribing antiretroviral (ARV) drugs to the woman is decided. When ARV drugs are taken correctly, the amount of virus in the blood decreases and the risk of passing HIV to an unborn child is reduced. The choice of the regimen and the term of prescription of ARV drugs is decided individually. The safety of their use for the fetus and the pregnant woman herself has been proven. The medicines are given out free of charge according to the prescriptions of the doctors of the AIDS Center. nine0003
When ARV drugs are taken correctly, the amount of virus in the blood decreases and the risk of passing HIV to an unborn child is reduced. The choice of the regimen and the term of prescription of ARV drugs is decided individually. The safety of their use for the fetus and the pregnant woman herself has been proven. The medicines are given out free of charge according to the prescriptions of the doctors of the AIDS Center. nine0003
The effectiveness of drugs should be checked by the end of pregnancy (viral load laboratory test).
A pregnant woman must continue to be observed at the antenatal clinic at the place of residence.
Prevention of mother-to-child transmission of HIV includes 3 stages:
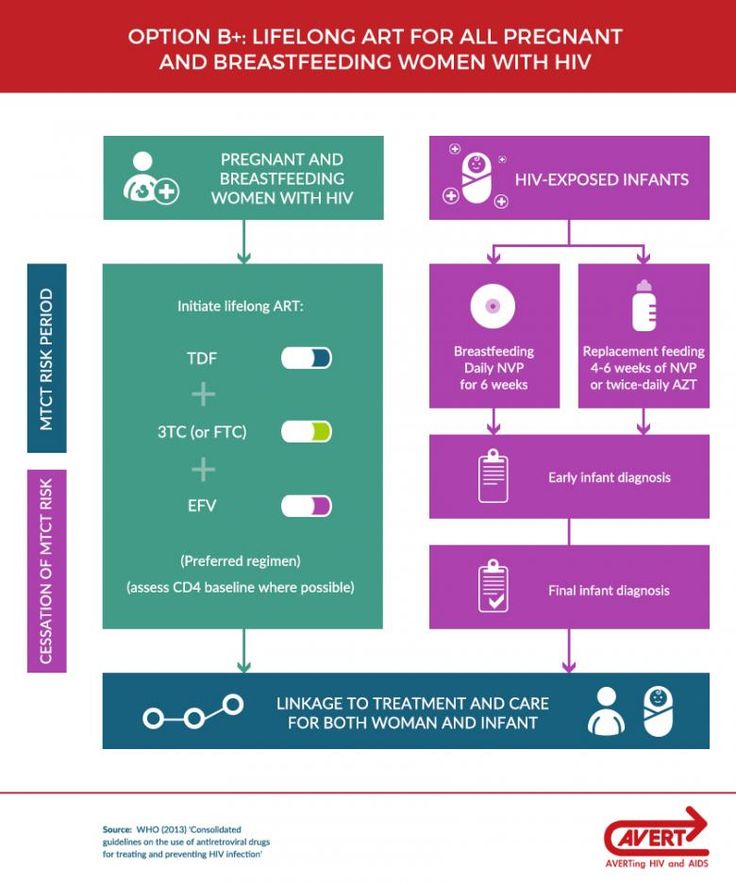
1 stage. Taking medication by a pregnant woman. Prevention should be started as early as possible, preferably from 13 weeks of gestation, with three drugs and continued until delivery. nine0003
Stage 2. Intravenous administration of an ARV drug to a woman during childbirth (“dropper”).
Stage 3. Taking medications for a newborn baby. Taking drugs by a child begins in the first 6 hours after birth (no later than 3 days). Most children receive zidovudine syrup at a dose of 0.4 ml per 1 kg of body weight twice a day (every 12 hours) for 28 days. In special cases, the doctor can add 2 more drugs to the child for prevention: viramune suspension - 3 days, epivir solution - within one week. nine0003
Births take place in maternity hospitals where the woman lives. Maternity hospitals in the Kostroma region are provided with all the necessary ARV drugs for prevention. The method of delivery (natural childbirth or caesarean section) is chosen by the general decision of the infectious disease specialist and obstetrician-gynecologist.
Breastfeeding is one of the ways of transmission of HIV infection (not only breastfeeding, but also feeding with expressed milk).
Without exception, women with HIV should not breastfeed! nine0003
Timing of examination of children born to HIV-infected mothers in the first year of life.

Up to 1 year of age, the child is examined three times:
- In the first 2 days after birth, blood is taken in the maternity hospital for HIV testing by PCR (detects virus particles) and ELISA (detects antibodies - protective proteins produced by the human body for the presence of infection ) for delivery to the AIDS Center.
- At 1 month of life - blood is taken for HIV by PCR in a children's clinic or hospital, in the HIV prevention office at the place of residence (if you have not donated blood at the place of residence, this will need to be done at the AIDS Center at 2 months). nine0076
- At the age of 4 months - it is necessary to come to the AIDS Center to examine the child by a pediatrician and to test the blood for HIV by PCR. Also, the doctor may prescribe additional tests for your child (immune status, hematology, biochemistry, hepatitis C, etc.).
If you miss one of the examination dates, do not postpone it until a later time.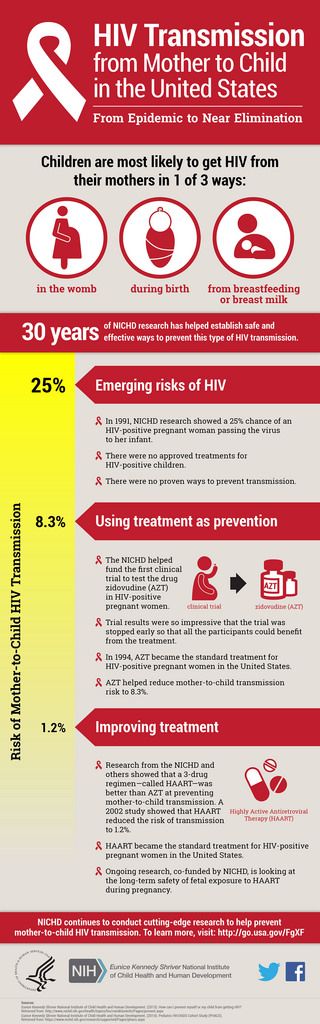 At the age of 1 month and up to 1 year of life, the child must be tested for HIV by PCR at least 2 times! nine0003
At the age of 1 month and up to 1 year of life, the child must be tested for HIV by PCR at least 2 times! nine0003
What do the test results mean?
Positive blood test for HIV antibodies
All children of HIV-positive mothers are also positive from birth, and this is normal! The mother passes on her proteins (antibodies) in an attempt to protect the baby. Maternal antibodies should leave the blood of a healthy child by 1.5 years (on average).
Positive PCR result
This study directly detects the virus itself, which means that a positive PCR may indicate a possible infection of the child. An urgent appearance of the child in the AIDS Center for rechecking is required. nine0003
Negative PCR
A negative result is the best! Virus not detected.
- A negative PCR on the second day of a child's life indicates that the child most likely did not become infected during pregnancy.
- Negative PCR at 1 month of life says that the child was not infected during childbirth.
 The reliability of this analysis at the age of one month is about 93%.
The reliability of this analysis at the age of one month is about 93%. - Negative PCR over 4 months of age - the child is not infected with a probability of almost 100%. nine0076
Examinations of children from 1 year.
If a child already has a negative blood test for HIV by PCR, the main method of research from the age of 1 year is the determination of antibodies to HIV in the child's blood. The average age when the child's blood is completely "cleared" of maternal proteins is 1.5 years.
- At the age of 1, the child donates blood for antibodies to HIV at the AIDS Center or at the place of residence. If a negative test result is obtained, repeat after 1 month and the child can be deregistered ahead of schedule. A positive or questionable result for HIV antibodies requires a retake after 1.5 years. nine0076
- Over the age of 1.5 years, one negative HIV antibody result is enough to deregister the child if there are previous tests.
Deregistration of children
- Age of child - over 1 year old;
- The presence of two or more negative PCR at the age of over 1 month;
- Having two or more negative HIV antibody tests over 1 year of age; nine0076
- Not breastfeeding in the last 12 months.
Confirmation of the diagnosis of HIV infection in a child
Confirmation is possible at any age from 1 to 12 months with two positive HIV PCR results.
In children older than 1.5 years, the diagnostic criteria are the same as for adults (presence of a positive blood test for antibodies to HIV).
The diagnosis is confirmed only by specialists from the AIDS Center. nine0003
Children with HIV infection are constantly under the supervision of a pediatrician of the AIDS Center, as well as in the children's polyclinic at the place of residence. HIV infection may be asymptomatic, but there comes a time when the doctor will prescribe treatment for the child. Modern drugs can suppress the immunodeficiency virus, thereby eliminating its effect on the body of a growing child. Children with HIV can lead a full life, visit any children's institutions on a general basis.
Vaccination
Children of positive mothers are vaccinated like all other children according to the national calendar, but with two exceptions:
- The polio vaccine must be inactivated (not live).