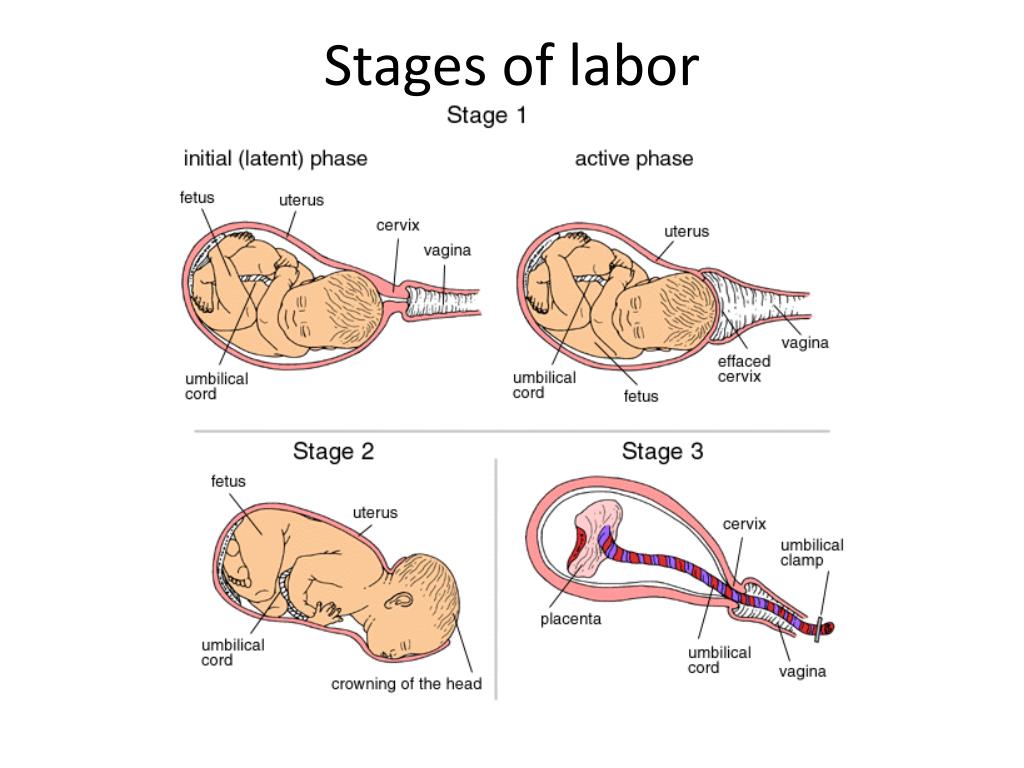
Process of labor and delivery
Signs, Progression & What To Expect
What to expect during labor and delivery.How does labor work?
As your pregnancy begins to wrap up, your body will prepare for labor and delivery. This is the process through which your baby will be born. Labor is often different for each person. Some have quick labors and some long, difficult labors. Other people may even experience labor that stalls or stops, leading to medical intervention.
Early labor
The average labor lasts 12 to 24 hours for a first birth and is typically shorter (eight to 10 hours) for other births. Throughout this time, you’ll experience three stages of labor. The first stage of labor is usually the longest and it ranges from when you first go into labor until your cervix is open. The beginning of this stage is called early labor. Early labor is described as dilating from 0 to 6 centimeters.
Active labor
As you progress and your contractions become stronger, you’ll move into the second part of the first stage of labor called active labor. Active labor is dilating from 6 to 8 centimeters and then transitioning into the second stage as you dilate 8 to 10 centimeters. Your contractions will become even stronger during active labor and your cervix will open up quickly. The second stage of labor is when you push. This is the phase of your labor when you will actually give birth to your baby.
Afterbirth
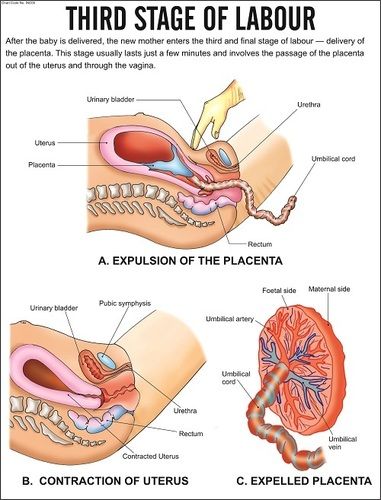
The third stage is the point when you deliver the placenta. This is also called afterbirth.
During these stages, your body prepares for childbirth by going through dilation and effacement.
- Dilation: This is a process where your cervix stretches and opens to make way for your baby’s birth. Dilation is measured from 1 to 10 centimeters. Your provider will do a vaginal exam to check how dilated you are throughout your labor.
 You’ll be 10 centimeters dilated in the second stage of labor for the delivery of your baby.
You’ll be 10 centimeters dilated in the second stage of labor for the delivery of your baby. - Effacement: The cervix not only stretches during labor but it also becomes thinner. The shortening and thinning of your cervix are measured in percentages. You’ll progress from 0% to 100% effacement during your labor.
Think of your cervix as a round doorway that needs to stretch outward and get thinner before your baby can pass through it. This stretching and thinning are caused by contractions. Contractions can be described in a variety of ways ranging from uncomfortable, period-like cramps to a painful tightening of your abdomen. You might also feel a dull ache in your back and lower abdomen, as well as pressure in your pelvis.
When you have a contraction, it’s actually the muscles of your uterus tightening at regular intervals to dilate and efface (open and thin) your cervix. During contractions, your abdomen becomes hard. Between contractions, your uterus relaxes and your abdomen becomes soft. Even though they can be painful, each contraction helps move you forward through your labor.
Even though they can be painful, each contraction helps move you forward through your labor.
How will I know I’m in labor?
It can be difficult to know when you’re in true labor. First-time parents, in particular, might mistake other symptoms or irregular practice contractions (called Braxton Hicks contractions) for true labor. True labor has a pattern and progresses steadily over time.
When you’re in true labor, you’ll notice a pattern in your contractions. Instead of the irregular Braxton Hicks contractions you might have felt during your pregnancy that showed up and then went away randomly, these contractions will keep coming for an extended period of time. There are three things you’ll want to look for when you are in true labor.
- Frequency: How often are your contractions happening? Keep track of them with a journal or labor app on your phone to make sure they're coming at regular intervals.
- Duration: How long are each of your contractions? As your labor continues, your contractions will last longer and longer.
 Use a stopwatch, watch a clock or keep the timer on your phone handy so you can record the length of each contraction.
Use a stopwatch, watch a clock or keep the timer on your phone handy so you can record the length of each contraction. - Intensity: Are your contractions getting stronger? Contractions can get stronger and you might feel them more intensely as you move through the stages of labor. Keep track of how your contractions feel over time.
Are there any signs that I will go into labor soon?
Many women have several pre-labor signs that might hint that labor will start soon. These signs of labor include:
- Backaches.
- Diarrhea.
- Weight loss.
- Nesting (cleaning and organizing your home).
No one knows for sure what causes labor to start, but several hormonal and physical changes may point to the beginning of labor.
What are Braxton Hicks contractions?
Often called practice contractions, Braxton Hicks are irregular contractions that don’t cause cervical change. Think of them as a test run for the real thing.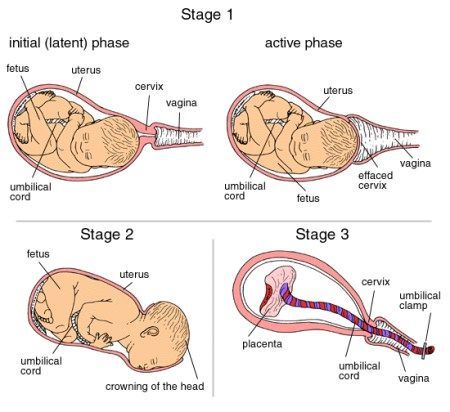 They can start happening at the end of your pregnancy and can startle people into thinking they’re in labor. This is called false labor.
They can start happening at the end of your pregnancy and can startle people into thinking they’re in labor. This is called false labor.
A Braxton Hicks contraction will feel like a sudden, sharp tightening of your abdominal muscles. Even though this is very similar to how a contraction feels, Braxton Hicks contractions don’t follow a pattern or progress over time. They may also stop when you lay down or relax. When you start to experience these practice contractions, keep track of them. Writing them down is the best way to tell the difference between true and false labor.
What is lightening?
Lightening is the process where your baby settles or lowers into your pelvis. This can happen a few weeks or a few hours before labor. When this happens, you may experience some increased lower pelvic pressure. Because your uterus rests on your bladder more after lightening, you might also feel the need to urinate more frequently. You might notice that you’re not as short of breath once your baby drops.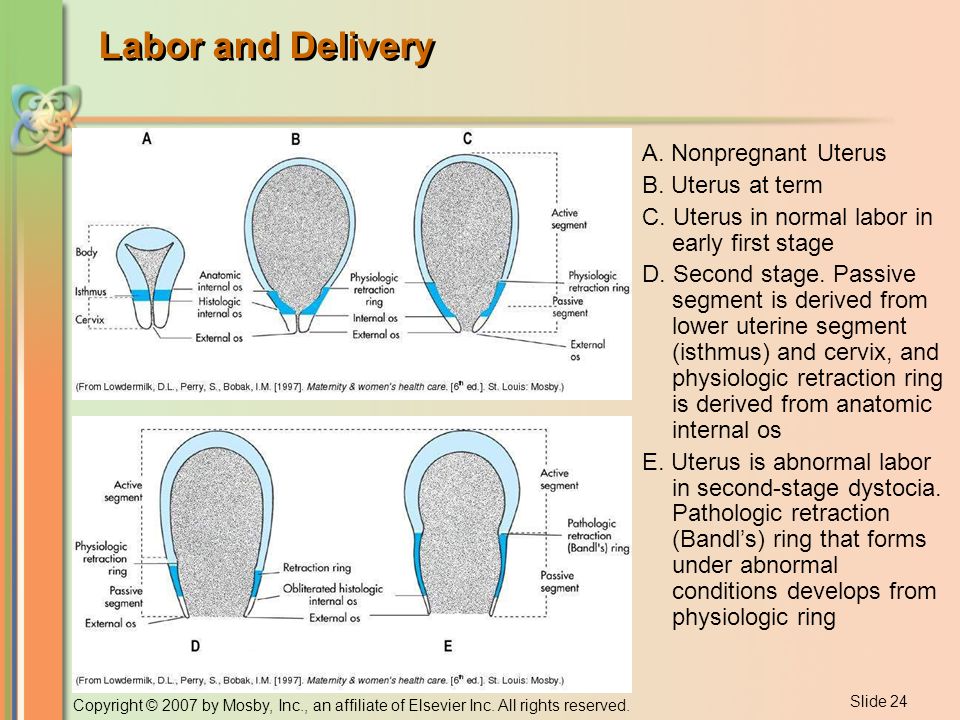
What’s the mucus plug and what does it mean when it falls out?
During pregnancy, a thick piece of mucus called a plug blocks the cervical opening. This plug keeps your uterus closed off from the birth canal and the outside of your body and prevents bacteria from traveling into your uterus. When your cervix begins to soften, thin, and open, the mucus is expelled into your vagina. Not every mucus plug will look the same. Possible colors of the mucus plug can include:
- Clear.
- Pink.
- Slightly bloody.
Labor could start shortly after you lose your mucus plug or it could begin several weeks later.
How do I time my contractions?
Once you’re in labor, it’s important to keep track of your contractions. Your healthcare provider will need to know how long your contractions are lasting (duration), how often they’re happening (frequency) and how intense they are. When you’re timing your contractions, you will want to have a way to record each one – pen and paper or through an app on your phone – and a timer or clock. Make sure you keep track of each contraction from start to end, as well as the time between each contraction. This second measurement will help your provider know the frequency of your contractions.
Make sure you keep track of each contraction from start to end, as well as the time between each contraction. This second measurement will help your provider know the frequency of your contractions.
It can be difficult to record the intensity of your contractions. This can really vary from person to person. Often, an easy way to keep track of the intensity of your contractions is to record when you cannot walk, talk or laugh during contractions.
Is there anything I can do to cope with contractions?
As you approach the end of your pregnancy, it’s a good idea to talk to your healthcare provider about different ways to deal with pain and discomfort during labor. There are several options your provider will discuss with you to relieve pain.
There are also ways to deal with the discomforts of labor at home or without medication, including:
- Distract yourself by taking a walk, going shopping or watching a movie.
- Soak in a warm tub or take a warm shower.
 Make sure to ask your healthcare provider if you should take a tub bath if your bag of water has broken.
Make sure to ask your healthcare provider if you should take a tub bath if your bag of water has broken. - Sit on a birth ball.
- Listen to music.
- Dim the lights.
- Use aromatherapy.
- Get a massage.
- Stay in an upright position. This can help with the descent and rotation of your baby.
- Try to sleep if it’s evening. You’ll want to store up your energy before active labor and delivery.
How will I know when my water breaks?
You may be familiar with the common phrase “my water broke.” This is actually the rupturing of your amniotic membrane. During pregnancy, your baby is inside a fluid-filled sac, also called your bag of water. When this membrane breaks, you might feel a sudden gush or trickle of fluid. Like many parts of labor and childbirth, this experience can be different for each person. The fluid is usually odorless and may look clear or straw-colored.
Unlike urine leakage that some pregnant women experience, this won’t stop.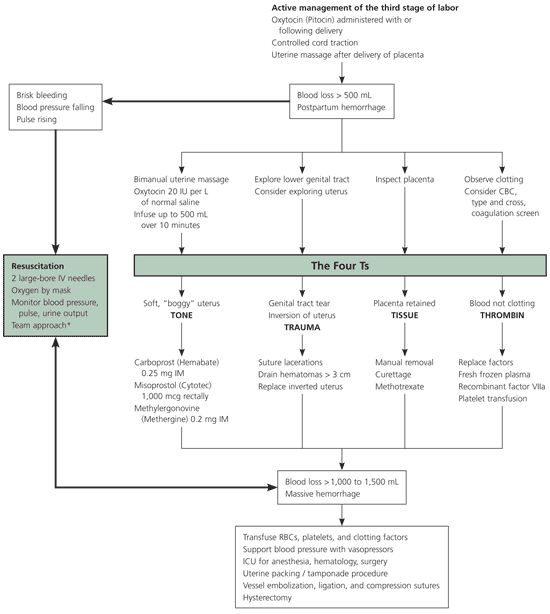 The amniotic fluid will often continue to leak.
The amniotic fluid will often continue to leak.
If your water breaks, call your healthcare provider. Let your provider know what time your water broke, the amount (trickle or gush), the color of the fluid and the odor. Don't use tampons if your water has broken. Your labor might start right after your water breaks. Some women are already in labor when their water breaks while others don’t experience the first stage of labor for a while after their water breaks.
When should I call my healthcare provider or go to the hospital?
If you ever have any questions, it’s always a good idea to call your healthcare provider. Your provider can answer any questions you have about true labor versus false labor and discuss how you’re feeling. When you start to notice that you’re having regular contractions, call your provider to talk about when you should go to the hospital. Some women are able to stay home throughout early labor, while others may need to come in sooner.
You should also call your healthcare provider if you:
- Think your water has broken.
 This could be a sudden gush of fluid or a trickle of fluid that leaks steadily.
This could be a sudden gush of fluid or a trickle of fluid that leaks steadily. - Are bleeding (more than spotting).
- Experience contractions that are very uncomfortable and have been coming every five minutes, lasting for one minute and have been like this for one hour.
What happens when I get to the hospital?
When you get to the hospital, you will check in at the labor and delivery desk. Most people will be seen in a triage room first. This is part of the admission process. It’s usually recommended that you only bring one person with you to the triage room.
From the triage room, you will be taken to the labor, delivery and recovery (LDR) room. You’ll be asked to wear a hospital gown. Your pulse, blood pressure and temperature will be checked. An external fetal monitor will be placed on your abdomen for a short time to check for uterine contractions and measure your baby’s heart rate. Your healthcare provider will also examine your cervix to see how far labor has progressed. An intravenous (IV) line might be placed into a vein in your arm to deliver fluids and medications.
An intravenous (IV) line might be placed into a vein in your arm to deliver fluids and medications.
What does it mean to have labor induced?
Labor doesn’t always start naturally or progress as it should. In these cases, your provider might talk to you about inducing labor. This is a medical procedure where labor is started by your healthcare provider. This could happen if you:
- Are past your due date.
- Have health complications like high blood pressure, preeclampsia, infection or diabetes.
- Had your water break but labor didn’t start.
- Have low levels of amniotic fluid.
Your labor can be advanced or induced in several ways. Your provider will advise you about the best and safest option depending on your health. Inducing labor can be done by using:
- Medications (oxytocin) given through an IV (directly into your vein).
- Breaking your amniotic sac (water).
- Separating the amniotic membrane (the sac of fluid the baby is inside within your uterus) from your uterine wall.
 This is also called sweeping the membrane.
This is also called sweeping the membrane. - Softening your cervix and encouraging it to open with a medication that can be placed directly in your vagina.
Labor induction can take longer than spontaneous labor because the cervical ripening process takes time.
What are the different types of delivery?
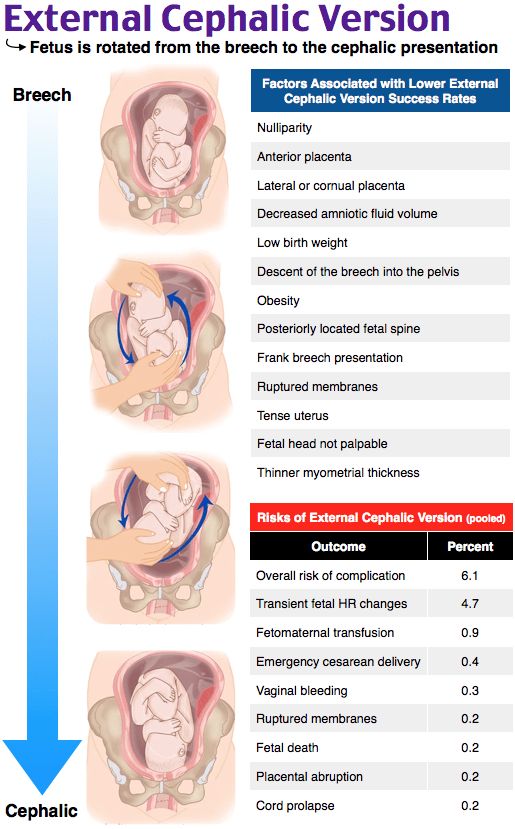
There are two main types of delivery: vaginal and cesarean section (C-section). During vaginal birth, your baby will pass naturally through the birth canal. A C-section is a surgical procedure where your provider makes an incision (cut) in your abdomen and delivers the baby in an operating room. Vaginal delivery is the most common type of birth. However, sometimes you might need a C-section for a variety of reasons, including:
- If your baby is not in the head-down position.
- If your baby is too large to naturally pass through your pelvis.
- If your baby is in distress.
- If the placenta blocks your cervix (a condition called placenta previa).
- If you have health issues or complications that make a C-section the safest option.
- If there’s an emergency situation that requires your baby to be delivered quickly.
In many cases, a cesarean delivery is not determined until after labor begins.
How long will I be in the hospital?
The length of your hospital stay can depend on the hospital where you deliver your baby and the type of delivery you have. Typically, you will stay in the hospital longer if you have a C-section delivery because it's a surgical procedure. You may also need to stay in the hospital for a longer period of time if you experience any complications or health issues during your delivery.
A note from Cleveland Clinic:
You're bound to a lot of feelings as you prepare to deliver your baby. It's normal to feel both excited and nervous. Discussing the signs and symptoms with your healthcare provider can help you know what to expect. Your partner and healthcare team are here to support you and will help you remain as comfortable as possible through the delivery process.
Stages of labor and delivery, explained
Toward the end of pregnancy, it might be tempting to grab your hospital bag whenever you feel something new, thinking it’s an early sign of labor. There may even be a few false alarms – after all, your due date is only an estimate.
Whether labor begins on its own or you need an induction, it can be helpful to know what you may experience as your labor progresses toward delivering your baby, and when to head to the hospital or birth center.
Below, we explain the three stages of labor and delivery for vaginal births. This includes what marks the start and end of each stage, how long each may last, how your body is likely to feel and more.
Click the links below to jump to each of the three stages of labor:
- The first stage of labor is usually the longest as your body gets ready for delivery.
- The second stage of labor is the process of delivering your baby after your cervix has fully dilated.
- The third stage of labor occurs after the baby is born and lasts until the placenta is delivered.

1. The first stage of labor
The first stage of labor is the preparation phase. For months, your body has been working to keep baby in. And now it’s time for your baby to come out.
Your body does this through contractions. Contractions help dilate (open) and efface (thin) the cervix, which is what connects your uterus to your vagina (birth canal).
What happens during the first stage of labor?
The first stage of labor is mainly distinguished by how dilated the cervix is and the characteristics of the contractions. Within this first stage, there are three phases: early, active and transition. If it’s your first time giving birth, the first stage of labor may take several days to complete. Here’s about how long each phase typically lasts:
- Early phase: Up to 24-48 hours
- Active phase: Up to about eight hours
- Transition phase: Up to about three hours
Early (latent) phase of labor
In the latent phase, contractions start out mild and irregular, typically lasting for less than a minute. They’ll gradually become stronger and more frequent as your cervix dilates. During this phase, you may notice thick pink or red vaginal discharge – this is the mucus plug that helped keep bacteria from passing through the cervix during pregnancy.
They’ll gradually become stronger and more frequent as your cervix dilates. During this phase, you may notice thick pink or red vaginal discharge – this is the mucus plug that helped keep bacteria from passing through the cervix during pregnancy.
Active phase of labor
You may have reached active labor once your contractions last for around a minute and have been occurring at least every 5 minutes for an hour (or ever 7 minutes if it’s not your first baby). This is when it’s time to call your provider or hospital, as you have been instructed. Other signs that it’s time to go to the hospital include:
- Your water breaks. This can feel like a sudden gush or a slow trickle from your vagina. It’s possible for your water to break before you reach active labor – call your care provider if it does.
- Intense contractions that you can’t walk or talk through.
- Bloody discharge that’s more watery than the mucus plug.
During active labor, you may also experience:
- Nausea or vomiting
- Leg cramps
- Pain and pressure in your lower back
Transition phase of labor
The end of active labor is sometimes referred to as the transition to the second stage of labor. It’s when the cervix completely dilates to a full 10 centimeters, and is the shortest – but generally considered the hardest – part of labor. If this is your first time giving birth, transition may take up to a few hours, or it may progress quickly. Contractions will be the longest, strongest and most frequent so far.
It’s when the cervix completely dilates to a full 10 centimeters, and is the shortest – but generally considered the hardest – part of labor. If this is your first time giving birth, transition may take up to a few hours, or it may progress quickly. Contractions will be the longest, strongest and most frequent so far.
During the transition phase, you may also feel:
- Pressure in the lower back and rectum
- An urge to push (tell your care provider if you do, as they’ll want to make sure you’re fully dilated first)
Inducing labor
There are some cases where labor has to be started manually (induced). Labor induction may be recommended for reasons such as:
- Labor hasn’t started naturally around two weeks after the due date.
- Your water has broken but contractions haven’t started for several hours.
- There’s not enough amniotic fluid.
- You have an infection or other pregnancy complication.
Pain relief
If you choose to labor at a hospital or hospital-based birth center, you’ll likely have some flexibility around pain management once you reach active labor. If you’ve been unsure whether to try for an unmedicated birth or use an epidural, this may be when you make your final decision – only you will know how much pain relief you need.
If you’ve been unsure whether to try for an unmedicated birth or use an epidural, this may be when you make your final decision – only you will know how much pain relief you need.
Unmedicated methods like hydrotherapy and massage may work great for you, or you may choose medication like an epidural to provide a strong numbing sensation. Generally, you can expect to have a few different options for managing labor and delivery pains, but it can be helpful to research them ahead of time as you write your birth plan.
The second stage of labor
The second stage of labor begins once your cervix is fully dilated, and ends when your baby is born. It may take anywhere from a few minutes to a few hours. It’s possible that this stage could take longer if you find it harder to push from the numbness of an epidural, or if it’s your first time giving birth.
What happens during the second stage of labor?
The second stage of labor is all about pushing. Your doctor or midwife will guide you through how and when to push – you may be instructed to push when you feel the urge, or when you’re having a contraction. Contractions could remain as intense as they were at the end of stage one, but they may be a little less frequent.
Contractions could remain as intense as they were at the end of stage one, but they may be a little less frequent.
The third stage of labor
Once your baby has been born, you’re in the third stage of labor. This stage is considered complete once the placenta has been delivered, which generally happens within 30 minutes of childbirth.
What happens during the third stage of labor?
You’ll continue to have contractions, but they’ll be milder. These contractions will move the placenta out of your uterus, and over the next few days, help your uterus return to its normal size. If necessary, your care provider will remove any remaining tissue from your uterus.
The first hours of recovery after labor
It’s finally time to meet, hold and celebrate your baby! Most babies are ready to breastfeed shortly after birth. Breastfeeding releases the hormone oxytocin, which encourages helpful, mild “post-birth” contractions and reduces bleeding. If your baby’s ready and you’re having trouble getting started, you can ask for help from a nurse or breastfeeding consultant. And if you or your baby don’t want to breastfeed, you’ll still get to hold them skin-to-skin to begin bonding unless your baby needs medical attention.
And if you or your baby don’t want to breastfeed, you’ll still get to hold them skin-to-skin to begin bonding unless your baby needs medical attention.
These first hours after birth mark the start of your recovery, and are sometimes referred to as the fourth stage of labor. During the rest of your hospital stay, your care team will monitor your blood pressure and other vital signs, and make sure you aren’t bleeding too much. They may also give you a shot of oxytocin and abdominal massages to promote contractions and control bleeding. You may find that you get chills or shakes during this stage, so ask for a blanket if you need one. If you had an epidural, the tube will be removed from your back, and if you had any small tears during delivery, you’ll be given local anesthetic and stitches.
And before you go home, you’ll receive plenty of tips for continuing your postpartum recovery and information about what to expect now that you’ve given birth.
What to know about the possibility of a C-section
Not every parent goes through all the stages of labor and delivery as they’re described above. A cesarean delivery (C-section), which involves surgically delivering a baby through the abdomen, isn’t something many people think about as they approach their due date, unless it’s planned. However, C-sections account for up to 20-35% of births in the United States.
A cesarean delivery (C-section), which involves surgically delivering a baby through the abdomen, isn’t something many people think about as they approach their due date, unless it’s planned. However, C-sections account for up to 20-35% of births in the United States.
The most important thing to know is that a C-section is only recommended when it’s the best choice for you and your baby. One may be scheduled in advance if there’s a clear medical reason for doing so, but often the need for a C-section doesn’t arise until closer to, or during, labor. For example, one of the most common reasons for an unplanned C-section is stalled labor, in which the cervix stops opening despite continued contractions.
Start preparing for labor and delivery
Everybody’s big day is different. But if you’re reading this, you’re already doing two of the best things you can to get ready: learning and planning. In addition to becoming familiar with the process of giving birth, here are a few other tips:
- Take a class: Childbirth classes can teach you everything from tools for staying relaxed during labor to what to expect from different forms of pain relief, and more.

- Prepare a birth plan: Writing a birth plan to give to your care team will help them support your labor, delivery and postpartum care according to your preferences.
- Strengthen your pelvic floor: Your pelvic floor muscles are going to go through a lot during labor. Practicing Kegels (flexing the muscles that stop urination) and other exercises can help reduce your risk of pelvic floor dysfunction after birth.
Finally, talk with your care provider. Whether you’re working with a doctor or a midwife, they’ll be able to answer questions and walk you through anything you might be unsure about. Take advantage of their expertise – they want to help.
Talk to your care provider
The process of childbirth
This event must be approached with self-confidence, one's strengths, capabilities and reliability of information received about childbirth during pregnancy. Tuning in the right way and doing everything right, knowledge helps. It is incomparably easier for pregnant women who have a good idea of all the stages of the birth process and are psychologically prepared for the upcoming event than for those expectant mothers who are poorly aware of what will happen to them.
Childbirth is divided into three periods:
- Disclosure period . As a result of regular contractions (involuntary contraction of the muscles of the uterus), the cervix opens.
- The period of expulsion of the fetus from the uterine cavity. Attempts are added to the contractions - arbitrary (that is, controlled by the woman in labor) contractions of the abdominal muscles. The baby moves through the birth canal and is born.
- Follow-up period . The placenta and membranes are born. nine0010
First stage of labor
The fact that labor has already begun or is about to begin is indicated by the appearance of regular contractions and / or the outflow of amniotic fluid. Contractions are involuntary periodic contractions of the muscles of the uterus, aimed at shortening and opening the cervix. Normally, the length of the cervix is 3-5 cm, and the diameter is only a few millimeters. And for the birth of a child, it is necessary that the cervix completely shorten and open up to 9-10 cm.
And for the birth of a child, it is necessary that the cervix completely shorten and open up to 9-10 cm.
The period of dilation is the longest in the process of childbirth. In the natural course of childbirth, this period lasts 10-11 hours for primiparas, 6-7 hours for multiparous ones. nine0003
At the beginning of this period there are regular contractions that last 15-20 seconds with an interval of about 15 minutes. As the cervix dilates, the contractions intensify, become longer, and the intervals between them shorten. When the break between contractions is 10 minutes, you need to go to the maternity hospital.
During the opening period, it is recommended to walk, move, breathe properly, take a warm shower or bath. These measures contribute to a faster opening of the cervix, while reducing pain. You can ask your husband or midwife to massage the lumbar region - this will reduce the discomfort from contractions. nine0003
Second stage of labor
Most women agree that the end of the dilation phase, before the onset of the second stage of labor, is the most difficult. Contractions become frequent and painful, anesthesia by this moment usually ceases to act, fatigue accumulates, it is still impossible to push. The state of many women at this moment is described by one single phrase: “That's it! I can not anymore!". The only consolation is that it doesn't last long.
Contractions become frequent and painful, anesthesia by this moment usually ceases to act, fatigue accumulates, it is still impossible to push. The state of many women at this moment is described by one single phrase: “That's it! I can not anymore!". The only consolation is that it doesn't last long.
After the cervix is fully dilated, the doctor allows the mother to push. A woman usually herself feels strong urges to "push" the child out of the birth canal. These urges are called pushes. nine0003
In order for pushing to be effective, you need to push properly and breathe properly. Before pushing, you need to get more air into the lungs, hold your breath and try to push effectively. It is important not to strain your face and legs during attempts, but on the contrary - to relax as much as possible. Between attempts, you also need to relax and rest.
The second stage of labor lasts from 15 minutes to two hours, and in multiparous this stage is shorter than in primiparas. During this period, doctors especially carefully monitor the condition of the mother and fetus (they regularly listen to heartbeats, etc.). nine0003
During this period, doctors especially carefully monitor the condition of the mother and fetus (they regularly listen to heartbeats, etc.). nine0003
Meanwhile, the baby is moving along the genital tract. At the height of one of the attempts from the genital slit, the lower pole of the head (or buttocks - in breech presentation) is shown, after the end of the attempt, the head is hidden in the genital slit. This process - cutting the head - continues for some time. At a certain moment, the pole of the head remains in the genital gap and in between attempts. Under the influence of continuing attempts, the eruption of the head begins, which continues until its full birth. There is very little left. A few more attempts - and the whole child is born. nine0003
The newborn is placed on the mother's belly (ideally) and they get to know each other for a while, resting after the birth. The midwife or doctor then cuts the umbilical cord and takes the baby away for proper treatment, bathing, weighing and examination by a pediatrician.
10-15 minutes after the birth of the baby can be applied to the breast. This promotes uterine contraction and milk production.
Third stage of labor
The last stage of labor - the birth of the placenta - is the shortest. Usually, the afterbirth is born 10-20 minutes after the birth of the baby. Mom might need to push a little for this. nine0003
If the placenta does not separate for more than 30 minutes, doctors diagnose the retention of the placenta in the uterus and begin to take emergency measures.
The delivered placenta is carefully examined for its integrity. If everything is fine, that is, the placenta has separated completely, the woman is sewn up with tears or incisions (if any). After that, a heating pad with ice is placed on her stomach and observed for some time in the delivery room (1.5-2 hours).
This is where the birth process ends and a new life begins for mother and baby. nine0003
References
- Florian S., Ichou M.
 , Panico L. Parental migrant status and health inequalities at birth: The role of immigrant educational selectivity. // Soc Sci Med - 2021 - Vol278 - NNULL - p.113915; PMID:33905985
, Panico L. Parental migrant status and health inequalities at birth: The role of immigrant educational selectivity. // Soc Sci Med - 2021 - Vol278 - NNULL - p.113915; PMID:33905985 - Naja S., Al Kubaisi N., Singh R., Abdalla H., Bougmiza I. Screening for antenatal depression and its determinants among pregnant women in Qatar: revisiting the biopsychosocial model. // BMC Pregnancy Childbirth - 2021 - Vol21 - N1 - p.330; PMID:33902481
- Shchepin VO., Khabriev RU. [The characteristics of population mortality of the Russian Federation, the Central Federal Okrug and City of Moscow in 2020]. // Probl Sotsialnoi Gig Zdravookhranenniiai Istor Med - 2021 - Vol29 - N2 - p.189-193; PMID:332
- Saavedra LPJ., Prates KV., Gonçalves GD., Piovan S., Matafome P., Mathias PCF. COVID-19 During Development: A Matter of Concern. // Front Cell Dev Biol - 2021 - Vol9 - NNULL - p.659032; PMID:33898461
- Caparros-Gonzalez RA., Romero-Gonzalez B., Puertas-Gonzalez JA.
 , Quirós-Fernandez S., Coca-Guzman B., Peralta-Ramirez MI. [Midwives and psychologists as professionals to screen and prevent pregnancy-specific stress.] // Rev Esp Salud Publica - 2021 - Vol95 - NNULL - p.; PMID:33896933
, Quirós-Fernandez S., Coca-Guzman B., Peralta-Ramirez MI. [Midwives and psychologists as professionals to screen and prevent pregnancy-specific stress.] // Rev Esp Salud Publica - 2021 - Vol95 - NNULL - p.; PMID:33896933 - Burakowska K., Gorka P., Penner GB. Effects of canola meal inclusion rate in starter mixtures for Holstein heifer calves on dry matter intake, average daily gain, ruminal fermentation, plasma metabolites, and total-tract digestibility. // J Dairy Sci - 2021 - Vol - NNULL - p.; PMID:33896627
- Toker E., Aktaş S. The childbirth experiences of Syrian refugee mothers living in Turkey: a qualitative study. // J Reprod Infant Psychol - 2021 - Vol - NNULL - p.1-17; PMID:33896296
- Mérillet L., Pavoine S., Kopp D., Robert M., Mouchet M. Biomass of slow life history species increases as local bottom trawl effort decreases in the Celtic sea. // J Environ Manage - 2021 - Vol290 - NNULL - p.112634; PMID:33895454
- Patskun E., Yevtushok L., Zymak-Zakutnia N.
 , Lapchenko S., Akhmedzhanova D., Wertelecki W. A teratology information system in vernacular: Closing an information gap. // Birth Defects Res - 2021 - Vol - NNULL - p.; PMID:33893758 nine0007 Fu A., Liu C. Is Pregnancy Following a TRAM or DIEP Flap Safe? A Critical Systematic Review and Meta-analysis. // Aesthetic Plast Surg - 2021 - Vol - NNULL - p.; PMID:33893518
, Lapchenko S., Akhmedzhanova D., Wertelecki W. A teratology information system in vernacular: Closing an information gap. // Birth Defects Res - 2021 - Vol - NNULL - p.; PMID:33893758 nine0007 Fu A., Liu C. Is Pregnancy Following a TRAM or DIEP Flap Safe? A Critical Systematic Review and Meta-analysis. // Aesthetic Plast Surg - 2021 - Vol - NNULL - p.; PMID:33893518
Important to know - St. Petersburg citizen's health
The total duration of childbirth and its course
The total duration of childbirth depends on many factors: age, physique and physical condition of the woman, her psychological mood, the speed of cervical dilatation, first pregnancy or repeated , the size of the child, the type of presentation and a number of other points. nine0003
Labor activity proceeds differently for all women, but the main periods of childbirth are clearly distinguished: 1st period - the period of contractions, the longest and most intense, 2nd period - the direct birth of a baby, 3rd period - the birth of the afterbirth (placenta).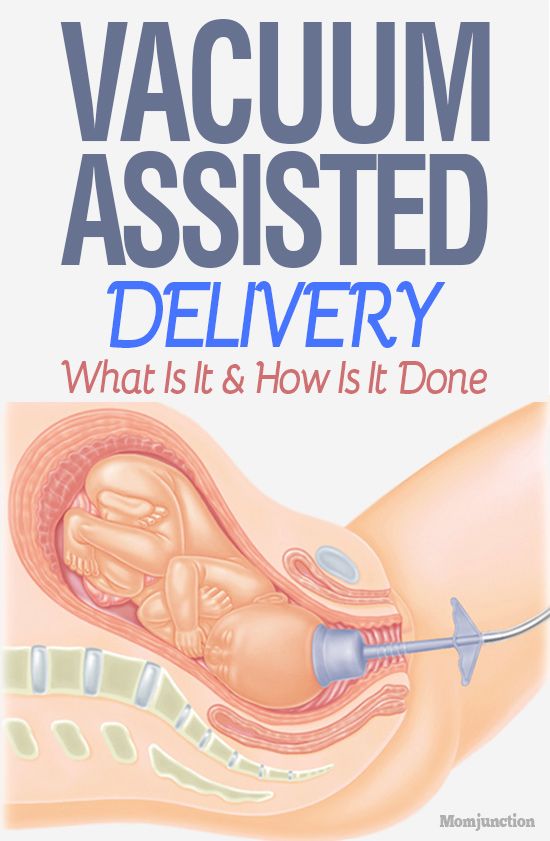
First stage of labor (opening period)
As the name implies, during this period there is a gradual opening of the cervix as a result of regular contractions of the uterine muscles. Contractions occur with a decreasing interval, while they themselves become longer and more frequent. nine0087 The dilation period is the time elapsed from the onset of regular contractions to the full dilation of the cervix. During this period, the birth canal is prepared for the passage of the fetus through them with all the fetal formations.
Cervical dilatation occurs gradually: at first the cervix is smoothed out, then the pharynx opens up to 3-4 cm and at the end of the first stage of labor up to 10 cm. This is already a complete dilatation of the cervix. With it, during contractions, the fetal bladder becomes tense and bursts at the height of one of them, the anterior portion of amniotic fluid is poured out. nine0003
The first stage of labor is the longest and consists of three phases:
1. Latent phase (lasts 5-6 hours). It is characterized by the establishment of regular contractions, with an interval between them of 10-15 minutes. Latent, or hidden, this phase is called because the contractions of the uterus during it are painless or slightly painful. By the end of the phase, the cervix is completely flattened and opens about 4 cm.
Latent phase (lasts 5-6 hours). It is characterized by the establishment of regular contractions, with an interval between them of 10-15 minutes. Latent, or hidden, this phase is called because the contractions of the uterus during it are painless or slightly painful. By the end of the phase, the cervix is completely flattened and opens about 4 cm.
2. Active phase (lasts 3-4 hours). Contractions become more intense, last at least 20 seconds, and the interval between them is reduced to 5-6 minutes. Normally, during the active phase, amniotic fluid is poured out, which contributes to a faster full disclosure of the uterine pharynx. By the end of the phase, the uterus opens by 8 cm.
3. Transitional (transient) phase, or deceleration phase (lasts from 40 minutes to 2 hours, may be absent in multiparas). This phase is not always clearly manifested, but it is nevertheless distinguished due to the usual weakening of contractions during disclosure from 8 to 10 cm. The child's head descends and stands in the narrow part of the small pelvis, which necessitates a slower and smoother process.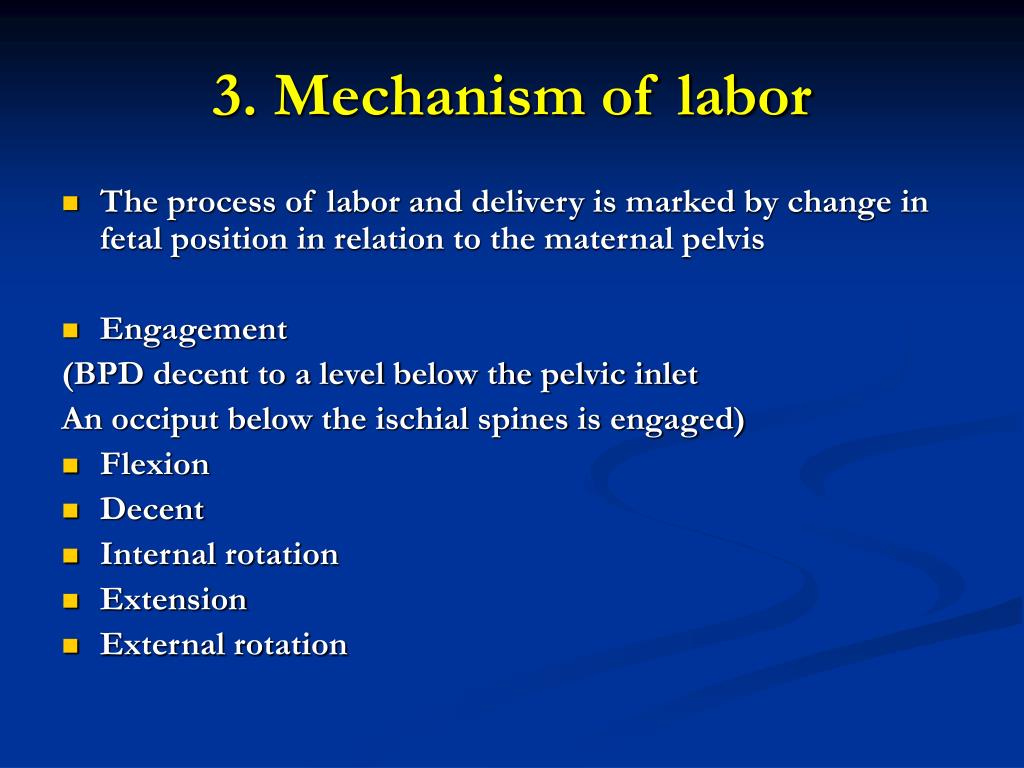 Already in the transitional phase, the woman in labor feels the desire to push, to push the baby out. But in order for the head to pass through the birth canal without the risk of injury, it is necessary to achieve cervical dilatation up to 10 cm.
Already in the transitional phase, the woman in labor feels the desire to push, to push the baby out. But in order for the head to pass through the birth canal without the risk of injury, it is necessary to achieve cervical dilatation up to 10 cm.
Second stage of labor (exile period)
The period of exile is the time from the moment of full opening of the pharynx until the birth of the fetus.
It is the second stage of childbirth that is their culmination, because in a short time (compared to contractions) the long-awaited birth of the baby takes place.
After the discharge of the amniotic fluid, contractions temporarily stop. The volume of the uterine cavity decreases, the uterine cavity and vagina appear as a single birth canal. Contractions reappear and become more intense. They are joined by attempts - contractions of the muscle press (abdominal wall, diaphragm and pelvic floor). The frequency and intensity of contractions and attempts are constantly increasing. The head descends and compresses the nerves of the sacral plexus. A woman has a strong desire to squeeze the head out of the birth canal, she is looking for supports for her arms and legs to strengthen her efforts. nine0003
The head descends and compresses the nerves of the sacral plexus. A woman has a strong desire to squeeze the head out of the birth canal, she is looking for supports for her arms and legs to strengthen her efforts. nine0003
Pushing is a lot of physical work. During attempts, a woman experiences maximum physical stress (blood pressure rises, pulse and respiration become more frequent). During the attempts, the woman holds her breath, and in the intervals between them she rests and "gathers her strength for a new attempt."
During one of the attempts, the head is born. Next, the shoulders are born (first the front, then the back) and the torso. Following the fetus, the posterior amniotic fluid is poured out with an admixture of cheese-like lubricant. nine0003
A woman in labor, having experienced severe fatigue, rests after hard work (pulse and respiration rate decrease).
Third stage of labor (postpartum period).
The afterbirth period is the time from the birth of the fetus to the birth of the placenta.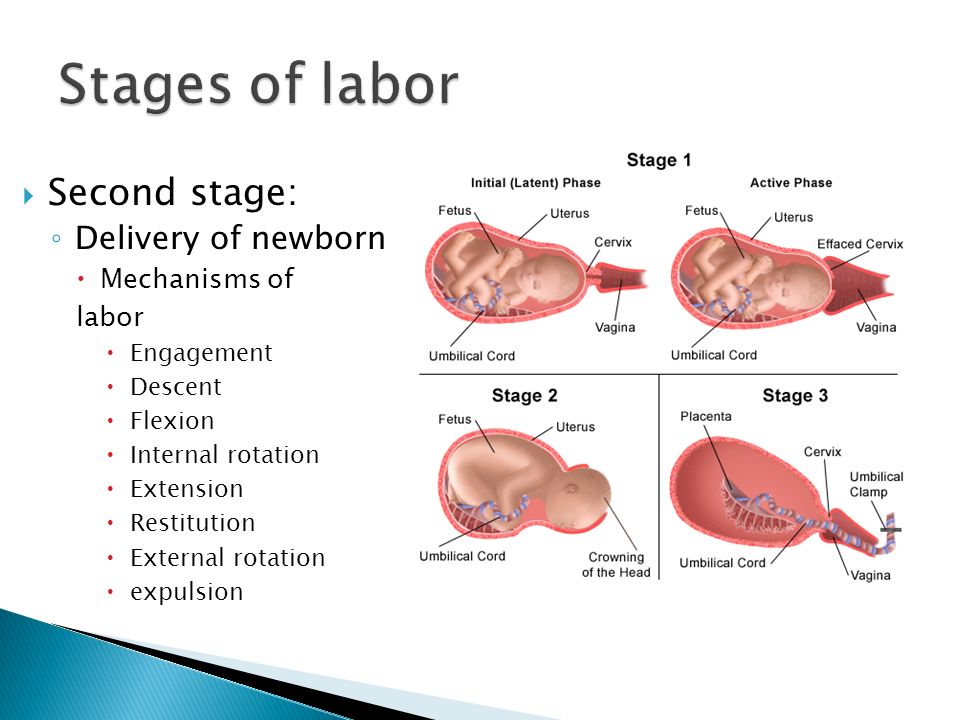 During this period, the placenta separates from the walls of the uterus and the birth of the placenta (placenta with membranes and umbilical cord).
During this period, the placenta separates from the walls of the uterus and the birth of the placenta (placenta with membranes and umbilical cord).
In the process of separation of the placenta from the walls of the uterus, uteroplacental vessels are damaged, which is normally accompanied by blood loss in the amount of 100-200 ml, without adversely affecting the woman's condition. After the birth of the placenta, the uterus contracts sharply, becomes dense, which is necessary to stop bleeding in the area of the placental site; its bottom is in the middle between the womb and the navel. nine0003
During this period, the woman's pulse and respiration normalize. Her demeanor is calm. Chills can sometimes be observed (as a reaction to the transferred strong physical stress).
The third period is no longer as exciting and tense as the previous two. The child was born and the matter remains for the small - the separation of the placenta, or placenta. Nature provides for the resumption of contractions a few minutes after the birth of the baby, necessary for effective exfoliation from the uterus of tissues that nourished the fetus during pregnancy (placenta, membranes, umbilical cord).