Pregnant low hcg levels
Low hCG Levels: Causes, Treatments, and Symptoms
Low hCG Levels: Causes, Treatments, and SymptomsMedically reviewed by Karen Gill, M.D. — By Becky Young on November 3, 2017
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission. Here’s our process.
What is an hCG test?
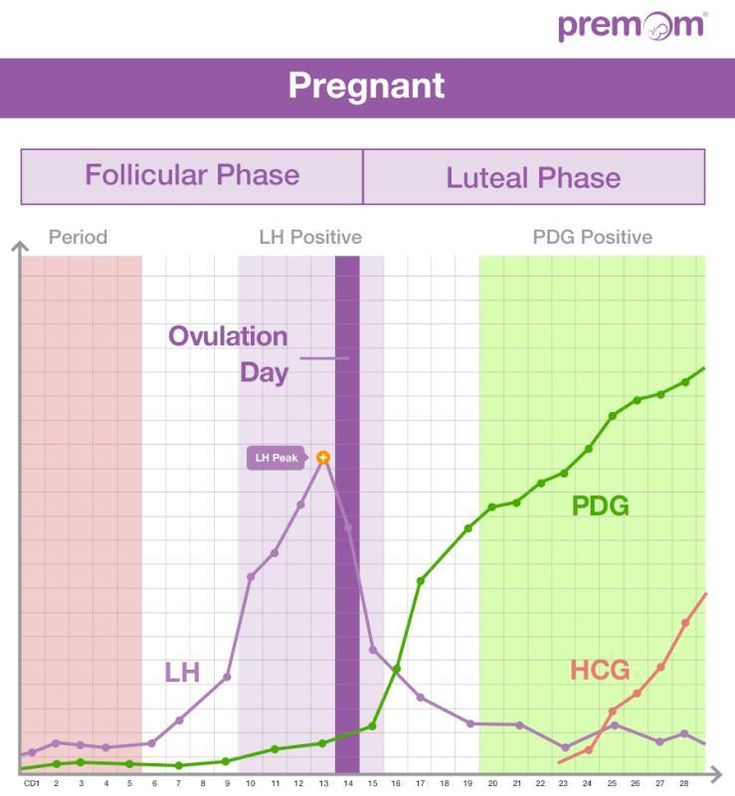
Human chorionic gonadotropin (hCG) is a hormone produced by your placenta once an embryo implants in the uterus.
The purpose of the hormone is to tell your body to continue to produce progesterone, which prevents menstruation from occurring. This protects the endometrial uterine lining and your pregnancy.
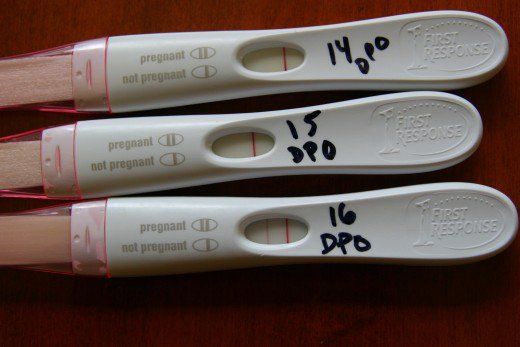
A pregnancy test can detect hCG in your urine if your levels are high enough. This is how the test identifies that you are pregnant. But only a blood test can give you a precise numerical hCG reading.
Purchase pregnancy tests here.
Standard hCG levels
Standard hCG levels vary quite massively from woman to woman. This is because hCG levels really depend on what is normal for you, how your body responds to pregnancy, as well as how many embryos you are carrying. The way a woman’s body reacts to pregnancy is entirely unique.
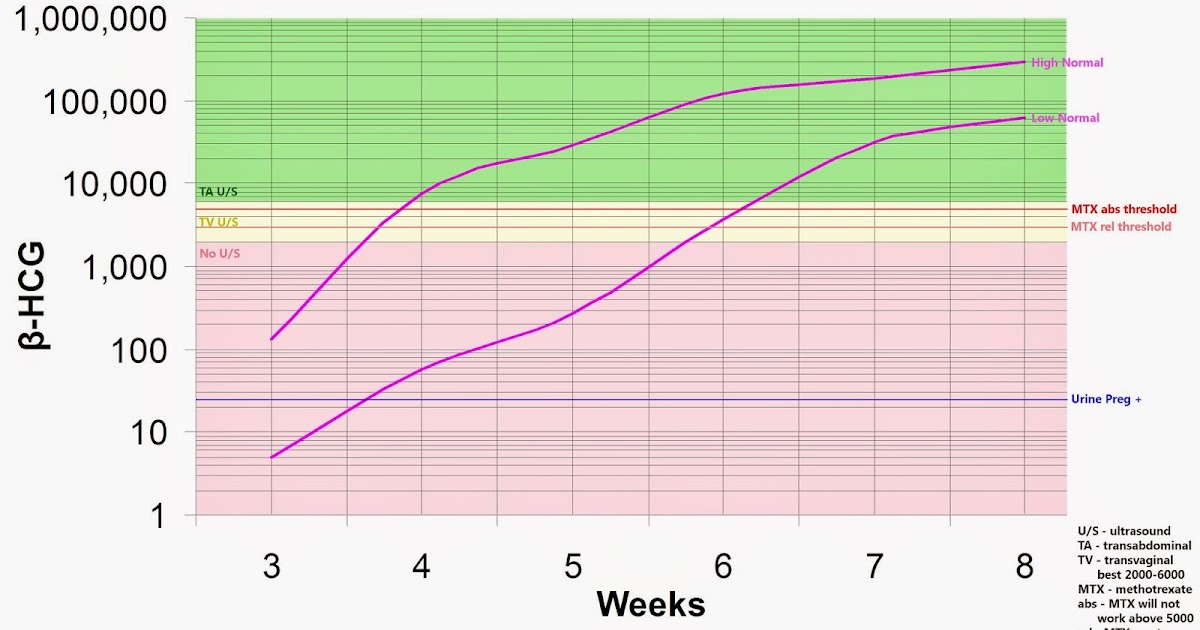
The table below gives you a guideline as to the normal wide range of hCG levels in each week of pregnancy. hCG levels are measured in milli-international units of hCG hormone per milliliter of blood (mIU/mL).
hCG levels usually consistently rise until around week 10–12 of your pregnancy, when the levels plateau or even decrease. This is the reason why pregnancy symptoms can be greater in the first trimester and ease off after this time for many women.
In early pregnancy, hCG levels usually double every two to three days. Interestingly, when the measurements start off high they don’t expand at the same rate. If they start off more slowly, the increase ends up happening much quicker.
If your hCG levels fall below the normal range, your doctor may want you to have a blood test every two to three days to ensure the levels are increasing. A single measurement of your hCG level is not useful. To give an accurate indication, a series of hCG blood tests needs to be taken a couple of days apart and the readings compared. There is often variation with a rapid increase in numbers, especially in the first few weeks of pregnancy.
A single measurement of your hCG level is not useful. To give an accurate indication, a series of hCG blood tests needs to be taken a couple of days apart and the readings compared. There is often variation with a rapid increase in numbers, especially in the first few weeks of pregnancy.
Causes of low hCG levels
If your hCG levels fall below the normal range, it’s not necessarily a cause for concern. Many women have gone on to have healthy pregnancies and babies with low hCG levels. Most women don’t ever have cause to find out what their hCG levels are specifically.
However, sometimes low hCG levels can be caused by an underlying problem.
Gestational age miscalculated
Typically, the gestational age of your baby is calculated by the date of your last menstruation. This can be easily miscalculated, particularly if you have a history of irregular periods or are unsure of your dates.
When low hCG levels are detected, it’s often because a pregnancy that was thought to be between 6 and 12 weeks is actually not that far along.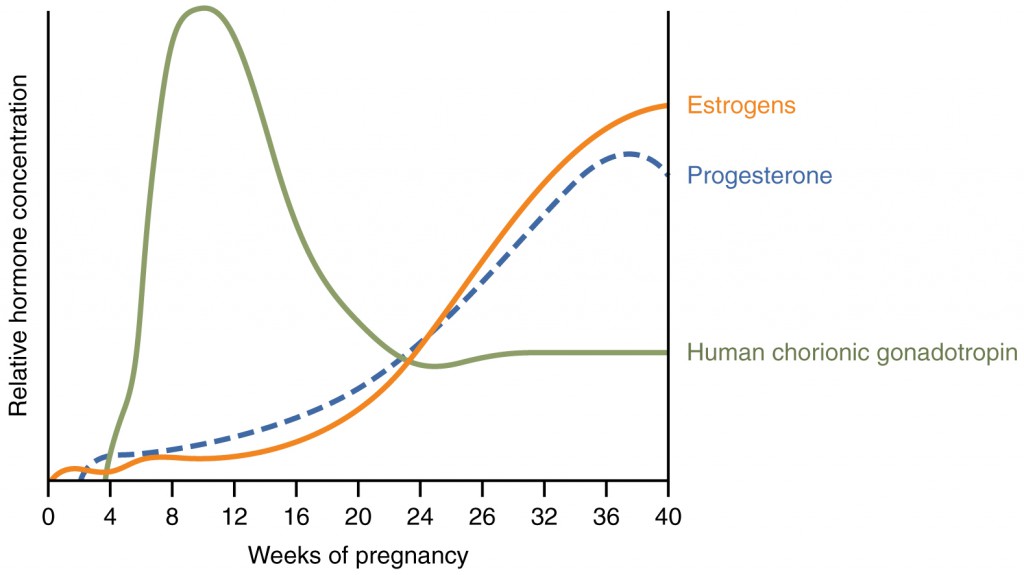 An ultrasound and further hCG tests can be used to calculate the gestational age correctly. This is usually the first step when low hCG levels are detected.
An ultrasound and further hCG tests can be used to calculate the gestational age correctly. This is usually the first step when low hCG levels are detected.
Miscarriage
A miscarriage is a pregnancy loss that occurs before 20 weeks of gestation. Sometimes low hCG levels can indicate that you have had or will have a miscarriage. If the pregnancy fails to develop a placenta, then the levels may be normal initially but fail to rise. Common signs that you are experiencing a miscarriage are:
- vaginal bleeding
- abdominal cramps
- passing tissue or clots
- cessation of pregnancy symptoms
- discharge of white/pink mucus
Blighted ovum
This is when an egg is fertilized and attaches to the wall of your womb, but does not continue to develop. When the gestational sac develops, hCG hormone can be released, but the level does not rise since the egg doesn’t develop.
This occurs very early in pregnancy. Most women won’t even know that it’s taken place.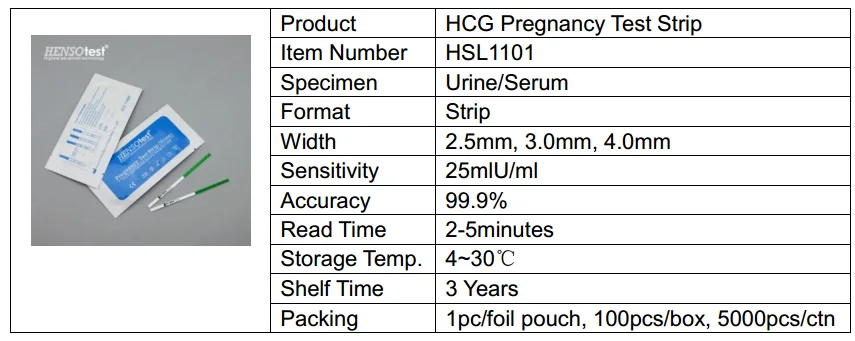 Usually you’ll experience your normal menstruation symptoms and assume it’s your usual period. However, if you’re trying to conceive, you may do an early pregnancy test that could pick up the presence of hCG.
Usually you’ll experience your normal menstruation symptoms and assume it’s your usual period. However, if you’re trying to conceive, you may do an early pregnancy test that could pick up the presence of hCG.
Ectopic pregnancy
An ectopic pregnancy is when the fertilized egg remains in the fallopian tube and continues to develop. It’s a dangerous and life-threatening condition, as it may cause the fallopian tube to rupture and bleed excessively. Low hCG levels can help to indicate an ectopic pregnancy. At first the symptoms of an ectopic pregnancy can be similar to those of a normal pregnancy, but as it progresses you can experience the following:
- abdominal or pelvic pain that worsens with straining or movement (this can happen strongly on one side initially and then spread)
- heavy vaginal bleeding
- shoulder pain caused by internal bleeding (the bleeding aggravates the diaphragm and presents as pain at the tip of the shoulder)
- pain during intercourse
- pain during a pelvic examination
- dizziness or fainting due to internal bleeding
- symptoms of shock
How is it treated?
Unfortunately, there is nothing that can be done to treat low hCG levels, though low levels alone are not always a cause for concern.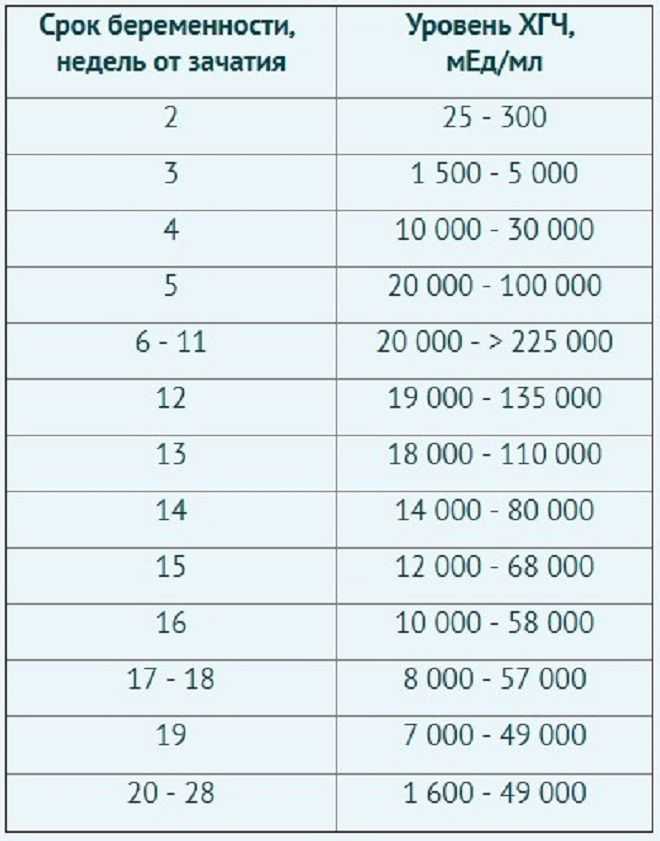
If your low hCG levels have been caused by a miscarriage, it’s possible that you may need treatment if any pregnancy tissue is left inside your womb. If there’s no tissue retained, then you won’t require any treatment at all. If there is, then there are three treatment options available:
- You can wait for the tissue to pass naturally.
- You can take medication to help you to pass the tissue.
- You can have it surgically removed.
Your doctor will discuss with you what the best course of action is.
The treatments for an ectopic pregnancy are similar. Medications are given to prevent the pregnancy from continuing to grow. If surgery is required, it’s standard for the doctors to remove the affected fallopian tube as well as the pregnancy.
What’s the outlook?
Low hCG levels alone are not necessarily a reason to be worried. There are many factors that affect the levels, and the normal range varies hugely between individual women.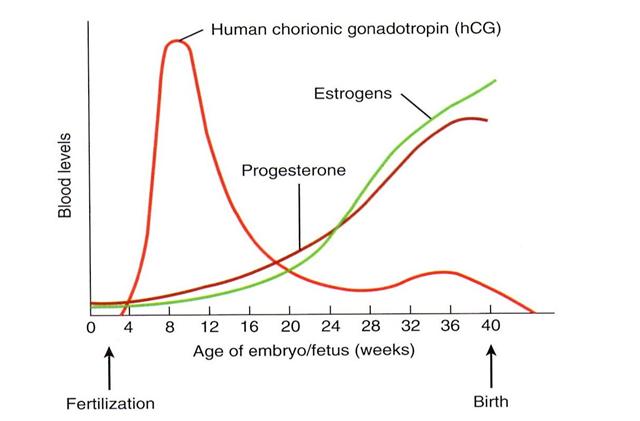 Your doctor will be able to monitor your hCG levels for you if you have concerns. Even if they remain low, there is nothing that you can do. It’s also important to remember that low hCG isn’t caused by anything you’ve done.
Your doctor will be able to monitor your hCG levels for you if you have concerns. Even if they remain low, there is nothing that you can do. It’s also important to remember that low hCG isn’t caused by anything you’ve done.
If your low hCG levels are due to a pregnancy loss, this doesn’t necessarily mean that you won’t be able to get pregnant and carry to term in the future. If you lose a fallopian tube due to an ectopic pregnancy, your fertility shouldn’t change significantly as long as your other tube is functioning. Even if it isn’t, reproductive technologies like in vitro fertilization can help lead to successful pregnancy.
Last medically reviewed on November 3, 2017
- Parenthood
- Pregnancy
How we vetted this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.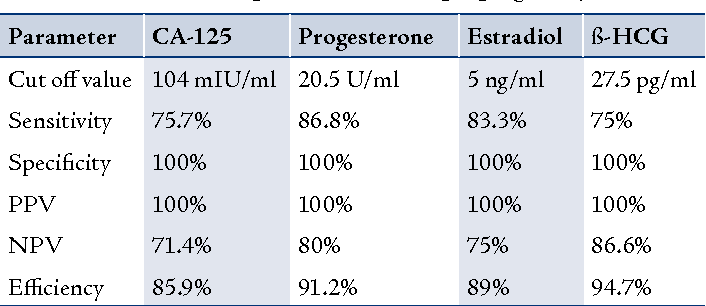
- Fan J, et al. (2017). Advances in human chorionic gonadotropin detection technologies: A review.
ncbi.nlm.nih.gov/pubmed/29056064 - Human chorionic gonadotropin (HCG): The pregnancy hormone. (2017).
americanpregnancy.org/while-pregnant/hcg-levels/ - Lawrenz B, et al. (2017). Luteal phase serum progesterone levels after GnRH-agonist trigger – how low is still high enough for an ongoing pregnancy?
ncbi.nlm.nih.gov/pubmed/29037085 - Matson PL, et al. (1990). Measurement of human chorionic gonadotropin during early pregnancy: A comparison of two immunoradiometric assays.
link.springer.com/article/10.1007/BF01135683 - Schumacher A. (2017). Human chorionic gonadotropin as a pivotal endocrine immune regulator initiating and preserving fetal tolerance.
ncbi.nlm.nih.gov/pubmed/29039764
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
Nov 3, 2017
By
Becky Young
Edited By
Phil Riches
Medically Reviewed By
Karen Richardson Gill, MD
Share this article
Medically reviewed by Karen Gill, M.D. — By Becky Young on November 3, 2017
Read this next
Human Chorionic Gonadotropin (hCG) Blood Test
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT
Get the facts on the human chorionic gonadotropin (hCG) blood test. Although it's often used to detect pregnancy, it has other uses such as detecting…
READ MORE
Can Taking Prometrium Vaginally Prevent Miscarriage?
Medically reviewed by Debra Sullivan, Ph.D., MSN, R.N., CNE, COI
Progesterone is known as the “pregnancy hormone.” Without enough progesterone, a woman’s body can’t continue to grow a fertilized egg. If you’ve…
READ MORE
How Does Clomid Work for Fertility?
Medically reviewed by Amanda Kallen, MD
Clomid is also known as clomiphene citrate.
 It’s an oral medication that is often used to treat certain types of female infertility.
It’s an oral medication that is often used to treat certain types of female infertility. READ MORE
How Many Eggs Are Women Born With? And Other Questions About Egg Supply
If you're looking to get pregnant, you may wonder how many eggs you have at various points in life. The short answer: It goes from millions to none.
READ MORE
Your Guide to the Egg Donation Process
Medically reviewed by Fernando Mariz, MD
There are many reasons you might consider donating your eggs. Learn more about the egg donation process, including possible risks, legal…
READ MORE
What’s the Connection Between Your Biological Clock and Fertility?
Medically reviewed by Amanda Kallen, MD
The biological clock describes the pressure people may feel to get pregnant while at the peak of their reproductive years, before fertility declines.
READ MORE
How Polycystic Ovary Syndrome (PCOS) Affects Fertility and What to Do
Medically reviewed by Amanda Kallen, MD
Polycystic ovary syndrome is a common cause of infertility. We'll discuss why and what you can do.
READ MORE
hCG Levels | The American Pregnancy Association
HCG (Human Chorionic Gonadotropin) is often called the pregnancy hormone because it is made by cells formed in the placenta, which nourishes the egg after it has been fertilized and becomes attached to the uterine wall. Levels can first be detected by a blood test about 11 days after conception and about 12-14 days after conception by a urine test.
Typically, the hCG levels will double every 72 hours. The level will reach its peak in the first 8-11 weeks of pregnancy and then will decline and level off for the remainder of the pregnancy.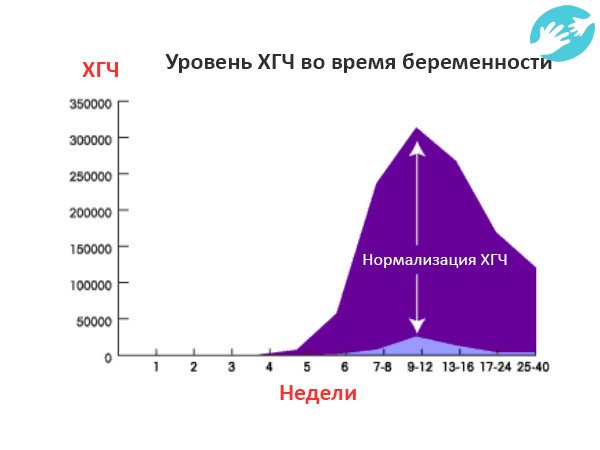
- As you get further along in pregnancy and the hCG level gets higher, the time it takes to double can increase to about every 96 hours.
- Caution must be used in making too much of hCG numbers. A normal pregnancy may have low hCG levels and result in a perfectly healthy baby. The results from an ultrasound after 5 -6 weeks gestation are much more accurate than using hCG numbers.
- An hCG level of less than 5 mIU/mL is considered negative for pregnancy, and anything above 25 mIU/mL is considered positive for pregnancy.
- An hCG level between 6 and 24 mIU/mL is considered a grey area, and you’ll likely need to be retested to see if your levels rise to confirm a pregnancy.
- The hCG hormone is measured in milli-international units per milliliter (mIU/mL).
- A transvaginal ultrasound should be able to show at least a gestational sac once the hCG levels have reached between 1,000 – 2,000 mIU/mL.
 Because levels can differentiate so much and conception dating can be wrong, a diagnosis should not be made by ultrasound findings until the hCG level has reached at least 2,000 mIU/mL.
Because levels can differentiate so much and conception dating can be wrong, a diagnosis should not be made by ultrasound findings until the hCG level has reached at least 2,000 mIU/mL. - A single reading is not enough information for most diagnoses. When there is a question regarding the health of the pregnancy, multiple testings of hCG done a couple of days apart give a more accurate assessment of the situation.
- The hCG levels should not be used to date a pregnancy since these numbers can vary so widely.
- There are two common types of hCG tests. A qualitative test detects if hCG is present in the blood. A quantitative test (or beta) measures the amount of hCG actually present in the blood.
Guideline to hCG levels in weeks during pregnancy
* These numbers are just a guideline – every woman’s level of hCG can rise differently.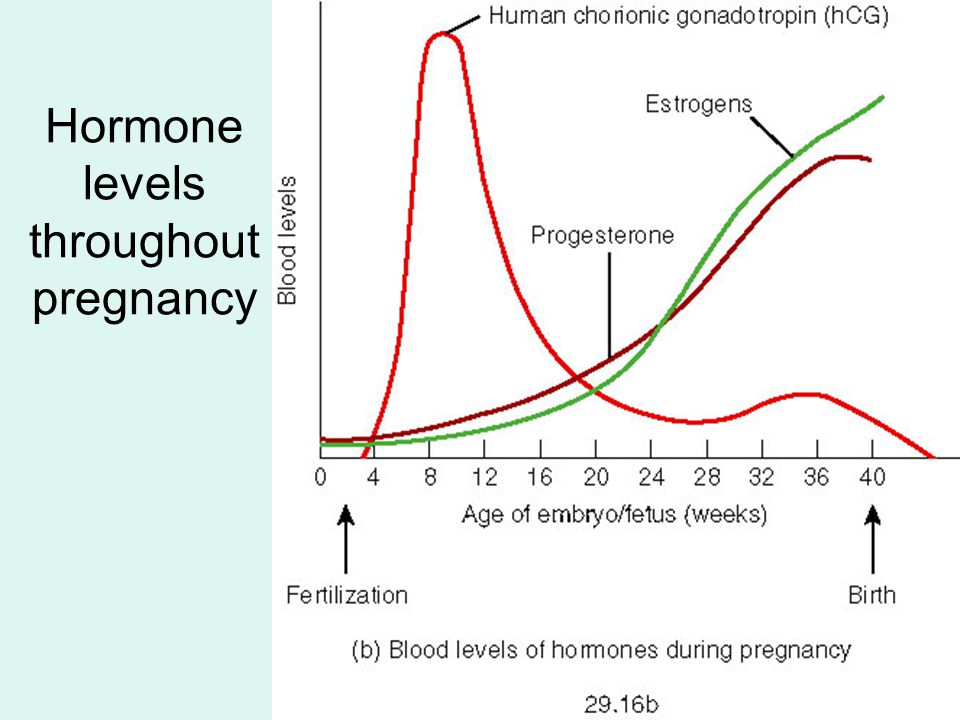 It is not necessarily the level that matters, but rather the change in the level.
It is not necessarily the level that matters, but rather the change in the level.
What Does a Low hCG Level Mean?
A low hCG level can mean any number of things and should be rechecked within 48-72 hours to see how the level is changing. A low level can indicate:
- Miscalculation of pregnancy dating
- Possible miscarriage or blighted ovum
- Ectopic pregnancy
Is a High hCG Level a Bad Thing?
A high level of hCG can also mean a number of things and should be rechecked within 48-72 hours to evaluate changes in the level. A high level can indicate:
- Miscalculation of pregnancy dating
- Molar pregnancy
- Multiple pregnancies
Should I Check My hCG level Regularly?
It’s not common for doctors to routinely check your hCG levels unless you are showing signs of a potential problem.
A health care provider may recheck your levels if you are bleeding, experiencing severe cramping, or have a history of miscarriage.
What Can I Expect After a Pregnancy Loss?
Most women can expect their levels to return to a non-pregnant range about 4 – 6 weeks after a pregnancy loss has occurred.
This can differentiate by how the loss occurred (spontaneous miscarriage, D & C procedure, abortion, natural delivery) and how high the levels were at the time of the loss.
Healthcare providers usually will continue to test hCG levels after a pregnancy loss to ensure they return back to <5.0.
What Can Interfere With My hCG Levels?
If you get a positive test result, you are most likely pregnant. False positives are extremely rare. However, there are some conditions that may cause a false positive, such as certain types of cancer and early miscarriage. Some antibodies may also interfere with test results.
Medications that contain hCG may interfere with hCG levels, as well.
These medications are often used infertility treatments, and your health care provider should advise you on how they may affect a test.
All other medications such as antibiotics, pain relievers, contraception or other hormone medications should not have any effect on a test that measures hCG.
Want to Know More?
- Pregnancy Calculator
- Calculating Gestation Age
- Concerns Regarding Early Fetal Development
Compiled using information from the following sources:
1. U.S. Food and Drug Administration
www.fda.gov
2. Bashir, I; Ihenetu, K; Miller, J.J.; Gim, M.; Lippmann, S. A Positive Pregnancy Test in the Post-Menopausal Psychiatric Patient — What to Think? Psychiatry (Edgemont). Feb. 2006.
Screening during pregnancy is carried out to assess the health of the baby
In medicine, the term "screening" means a mass examination to identify pathologies in both mother and child. That is, screening during pregnancy is an examination of expectant mothers to determine the health and full development of their future babies.
With the help of such a study, so-called congenital pathologies are detected in the early and middle stages of pregnancy.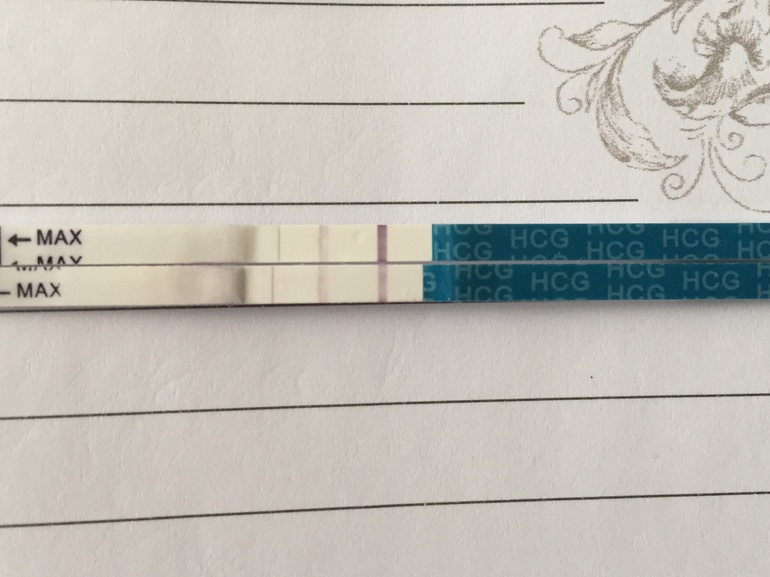 That is, you will know in advance whether your baby is healthy or he will need the help of doctors after birth.
That is, you will know in advance whether your baby is healthy or he will need the help of doctors after birth.
The main observations are aimed at identifying complex pathologies such as Down syndrome (trisomy 21), Edwards syndrome (trisomy 18) and neural tube defects (NTDs).
In addition, prenatal screening allows early detection of pathologies such as Corneli de Lange syndrome, Smith-Lemli-Opitz syndrome, non-molar triploidy, Patau syndrome.
Pregnancy screening consists of a series of tests and is carried out in parallel with the ultrasound examination of the baby with additional measurements. Let's consider everything in more detail and in turn.
First screening
The first comprehensive screening is carried out between 11 and 13 weeks of pregnancy and includes a biochemical analysis of venous blood to determine the content of the b-subunit of human chorionic gonadotropin and PAPP-A, a plasma protein associated with double pregnancy, this test is called.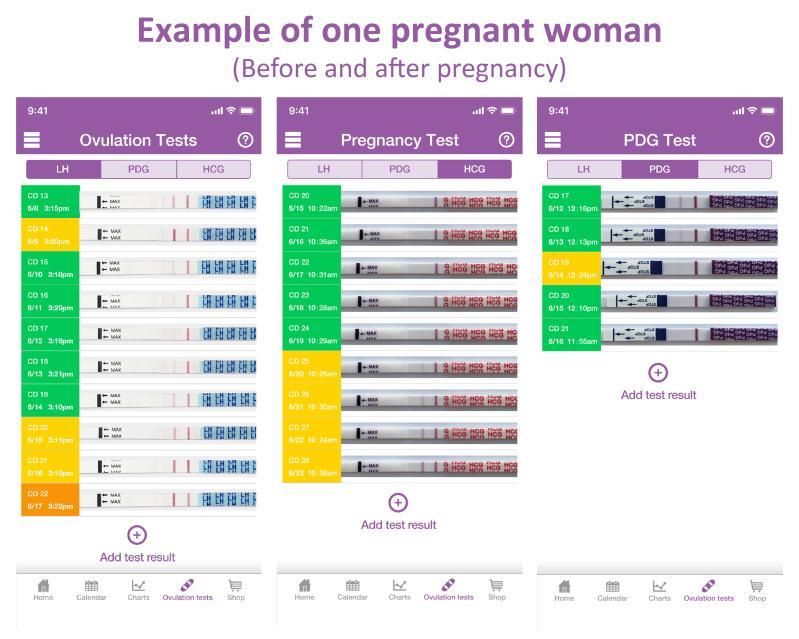
Low levels of b-hCG may indicate an ectopic pregnancy, delayed or halted development of the unborn child, and chronic placental insufficiency. A halved rate may mean a threatened miscarriage. An elevated level of b-hCG may indicate that a woman is pregnant with more than one child, especially if the cause of pregnancy was in vitro fertilization. The indicator also increases with gestosis (the presence of protein in the urine), with toxicosis, with diabetes in a pregnant woman, with fetal pathologies, malformations, and when taking medicinal hormonal preparations containing progestogen.
Reduced level of PAPP-A protein means:
1. The risk of abnormalities in the fetus at the chromosomal level;
2. Risk of having a child with Edwards syndrome;
3. Risk of having a child with Down syndrome;
4. Risk of having a child with Cornelia de Lange syndrome;
5. Pregnancy stopped developing;
6. There is a risk of threatened miscarriage. In this case, mom is sent for additional studies, such as amniocentesis (amniotic fluid is taken for analysis with a special needle) and chorionic villus biopsy.
In this case, mom is sent for additional studies, such as amniocentesis (amniotic fluid is taken for analysis with a special needle) and chorionic villus biopsy.
For the first screening, as a rule, women at risk are sent:
1. Over 35 years of age;
2. Those who have Down syndrome or other genetic pathologies in their families;
3. Those with a history of miscarriages, stillbirths, miscarriages, children with congenital abnormalities or genetic abnormalities;
4. Women who had viral diseases at the beginning of pregnancy, took drugs dangerous to the fetus or were exposed to radiation.
Ultrasound of the first screening:
1. Determine the number of embryos in the woman's uterus and their ability to survive;
2. Specifies the gestational age;
3. Gross malformations of organs in a child are revealed;
4. The thickness of the collar zone is determined, which involves measuring the subcutaneous fluid in the back of the neck and shoulders;
5. Examine the presence of the nasal bone.
Examine the presence of the nasal bone.
An abnormality at the first screening indicates the likelihood of a risk of various chromosomal and some non-chromosomal abnormalities. It is worth noting that the increased risk is not a cause for concern due to fetal malformations.
These studies involve more careful monitoring of pregnancy and the full development of the child. Often, if the result of the first screening showed an increased risk for some indicators, then conclusions can be drawn only after passing the second analysis. And in case of serious deviations from the norm, a woman is advised by a geneticist.
Second screening
The second comprehensive screening during pregnancy is performed from 18 to 21 weeks. This study implies a "triple" or "quadruple" test. It is performed in the same way as in the first trimester - a woman takes a biochemical analysis of venous blood.
But the second screening involves using the results of the analysis to determine three or less often four indicators:
- Free hCG beta subunit;
- Alpha-fetoprotein;
- Free estriol;
- Quadruple test - inhibin A.

An increased level of b-hCG indicates that the actual gestational age is determined incorrectly or the pregnancy is multiple, and also confirms the risks of developing a fetus with pathologies, genetic disorders.
Elevated ACE levels indicate the presence of liver necrosis in the fetus, the development of multiple pregnancy, possible disorders in the development of the neural tube, kidney pathology in the child, the presence of umbilical hernia and other developmental anomalies.
If the ACE test is low, this may mean that the fetus has a developmental delay, the fetus died, there is a hydatidiform mole instead of an embryo, the fetus is at risk of Down syndrome or Edwards syndrome, in the analyzes it looks like trisomy eighteen and trisomy twenty one. Or there is a great threat of miscarriage. A low ACE level can also mean that the gestational age is incorrect and the pregnancy is less than weeks old.
Estriol levels are very important for a successful pregnancy.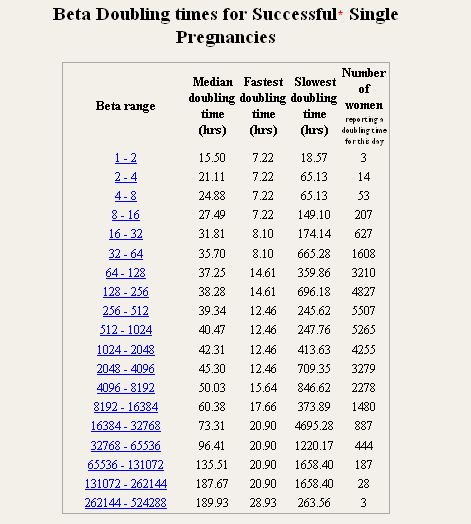 If the results of the analysis for the level of estriol show less than normal, then this means that there is a threat of miscarriage or premature birth, Down syndrome in a child, adrenal hypoplasia in a child, aencephaly, which means that there has been a violation of the formation of the neural tube in the fetus, in whole or in part missing brain tissue. And it can also mean that there is fetoplacental insufficiency, which manifests itself in violations in a woman, in a fetus or in a placenta, these violations have a negative effect on the relationship between the body of the mother and the child. Against the background of these disorders, fetal hypoxia, placental abruption, preeclampsia and other serious complications can occur.
If the results of the analysis for the level of estriol show less than normal, then this means that there is a threat of miscarriage or premature birth, Down syndrome in a child, adrenal hypoplasia in a child, aencephaly, which means that there has been a violation of the formation of the neural tube in the fetus, in whole or in part missing brain tissue. And it can also mean that there is fetoplacental insufficiency, which manifests itself in violations in a woman, in a fetus or in a placenta, these violations have a negative effect on the relationship between the body of the mother and the child. Against the background of these disorders, fetal hypoxia, placental abruption, preeclampsia and other serious complications can occur.
In addition, the level of estriol may be reduced due to liver and kidney disease in a woman, multiple pregnancies, a large child, or if the pregnant woman took hormonal drugs. It is best to take tests for all three hormones immediately on the same day as an ultrasound scan, such a set of blood tests is called a “triple test”, only the correct observance of the conditions for passing and processing tests gives the most correct result.
Calculations are carried out by a computer program, then analyzed by a doctor, who takes into account many individual parameters (the race of the pregnant woman and the father of the child; the presence of chronic, including inflammatory diseases; the number of embryos; the woman's body weight; the presence or absence of bad habits ). It is these secondary factors that can affect the change in the values of the studied indicators.
For maximum reliability, results must be compared with prenatal screening data in the first trimester. And in addition to biochemical analysis, ultrasound is also performed, which looks at the already formed organs of the baby.
If the results of the first and second screenings reveal abnormalities in the development of the baby, then the woman may be offered repeated tests or referred for a consultation with a genetics specialist.
Third screening
The third screening is carried out at 30-34 weeks of gestation.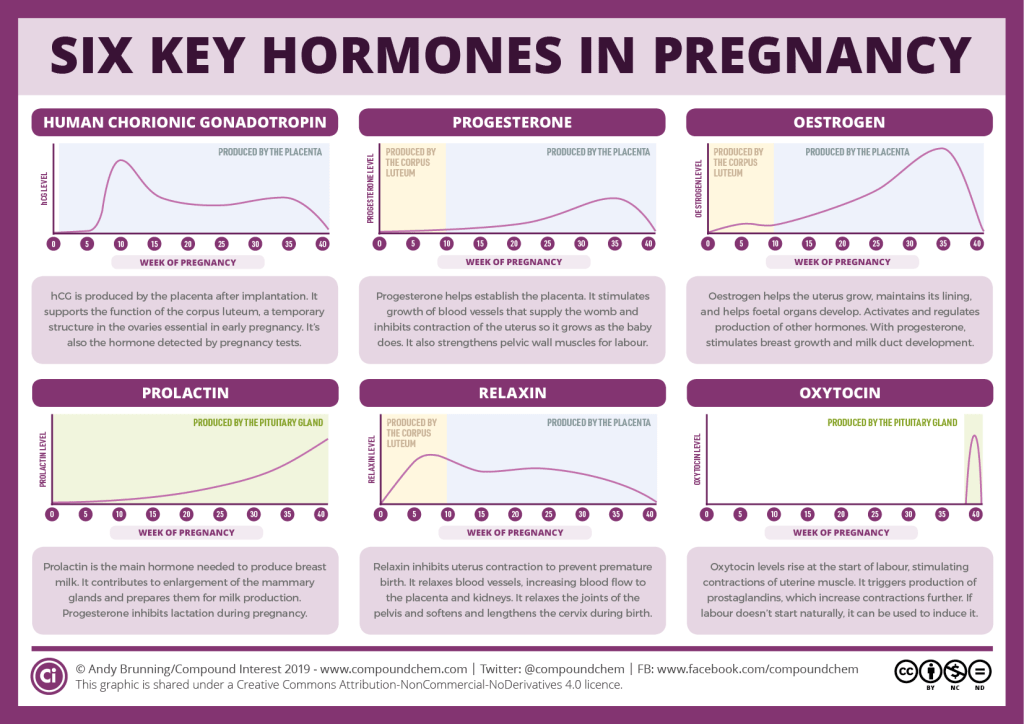 It is carried out in order to assess the functional state of the baby and make sure that the baby and the placenta interact effectively.
It is carried out in order to assess the functional state of the baby and make sure that the baby and the placenta interact effectively.
The position of the baby is also assessed. This will determine how he will behave in childbirth, and what tactics of childbirth the doctor should choose. In addition, the condition and location of the placenta is assessed, which is also important for future births.
During the third examination, the woman is again assigned to triple venous blood chemistry, and may also be sent for additional studies, such as dopplerography and cardiotocography.
Doppler ultrasound allows the doctor to assess the power of blood flow in the uterine and placental vessels, as well as in the great vessels of the child. This gives an understanding of how much oxygen and nutrition the baby receives and whether he has enough.
Cardiotocography (CTG) records the baby's heart rate even during labor. The child's pulse is determined by a special sensor. This test is carried out only after the 32nd week, because at periods earlier than 32 weeks the results will be unreliable.
This test is carried out only after the 32nd week, because at periods earlier than 32 weeks the results will be unreliable.
The first, second and third screenings are carried out in order to assess the health of your baby and his readiness for childbirth, because he must actively “work” in them. Research helps to anticipate some possible problems.
After all, it is easier to prevent any problem than to treat it long and hard later. In any case, it is necessary to perform certain examinations at a particular gestational age. Objectively, this is the only way to find out about the health of the baby in advance.
And do not believe the "popular" rumors that ultrasound is harmful to the baby or irritates him. This is absolutely not true, especially if you are conducting an examination in a clinic that has modern equipment and highly qualified specialists.
Even if the doctors said that you have a high risk of pathologies, do not despair. This does not always mean something serious that requires a global decision to keep the pregnancy or not.
Occasionally, a baby may have abnormalities that require surgery after birth. And if you and the doctor know about this in advance, then the chances of the most effective treatment and the excellent health of your baby are greatly increased.
As a mother, you are primarily responsible for the future of your child, so take all screenings seriously. Contact a specialist who will competently and clearly explain to you what is happening to you and your child, and thereby dispel all your fears and doubts. May all be well with you and your baby!
What low hCG indicates
During pregnancy, the female body undergoes significant changes that are necessary for the normal development of the unborn child. One of the most global changes is a change in the hormonal background, which affects not only the physical, but also the emotional state of a woman. Important for the development of the fetus is a hormone called human chorionic gonadotropin. It supports the functioning of the corpus luteum and provides many other functions..jpg)
What is hCG
HCG or human chorionic gonadotropin - is produced in large quantities in the female body during pregnancy. It is also synthesized in non-pregnant women and men, but in very small amounts. In this case, its increase requires an urgent consultation of a specialist, since an increase in this hormone without pregnancy indicates the development of an oncological disease. If you find an increased level of the hormone (in the absence of pregnancy or in men), you should contact your general practitioner, family doctor or oncologist to clarify the state of health.
HCG is produced by the chorion (upper germinal membrane) of the fetus almost immediately after it is implanted in the uterus. The presence of hCG and its rapid increase indicates the normal development of pregnancy.
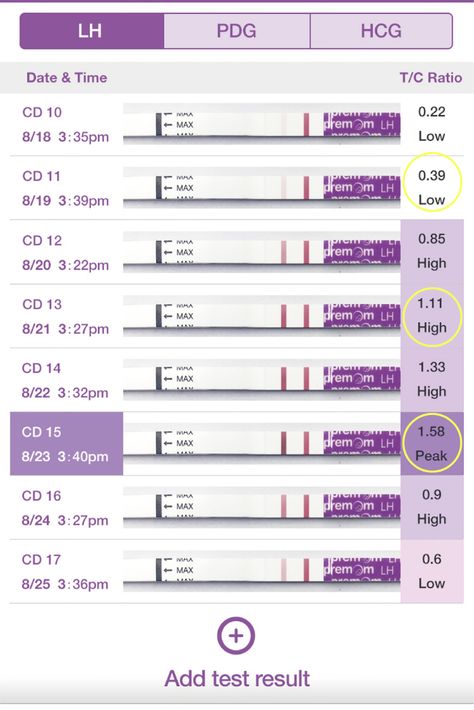
HCG is a gonadotropic hormone, similar to follicle-stimulating and luteinizing hormones, which are synthesized by the pituitary gland, but differ from them in amino acid sequence.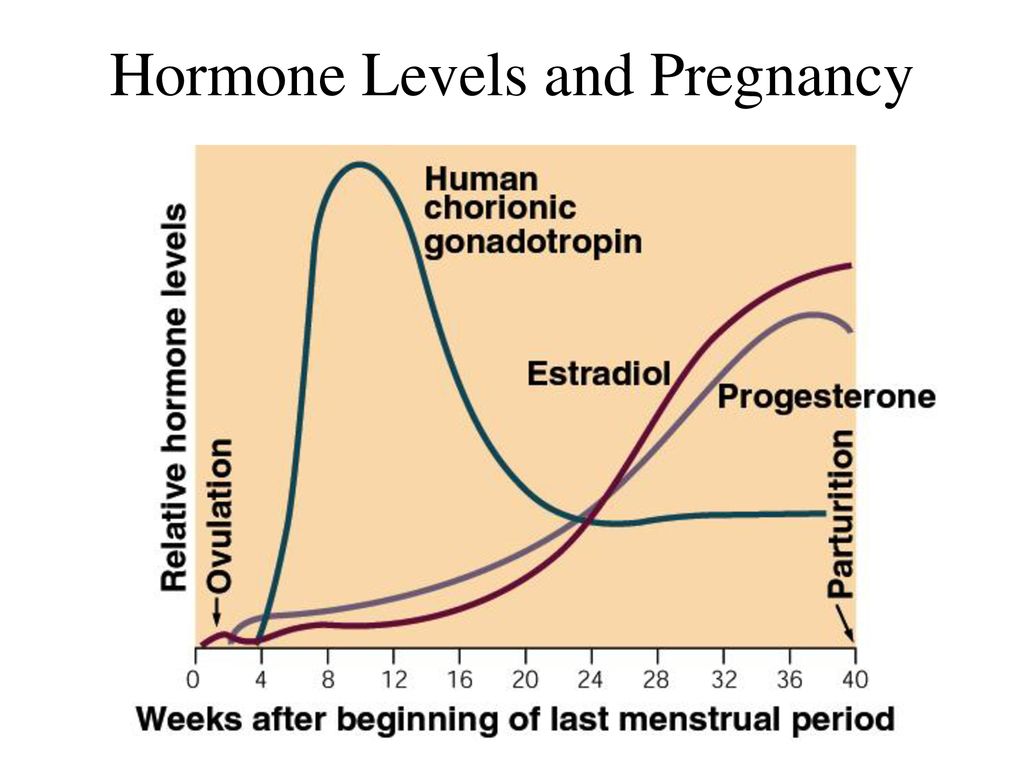 It consists of two subunits - α and β. The α-subunit is identical to the α-subunits of follicle-stimulating, luteinizing and thyroid-stimulating hormones, and the β-subunit has a biological and immunoreactive uniqueness specifically for human chorionic gonadotropin. Therefore, the β-subunit is used as a biochemical marker in prenatal screenings. In addition, the "home" test for pregnancy in the form of a strip is based on determining the presence of the β-subunit.
It consists of two subunits - α and β. The α-subunit is identical to the α-subunits of follicle-stimulating, luteinizing and thyroid-stimulating hormones, and the β-subunit has a biological and immunoreactive uniqueness specifically for human chorionic gonadotropin. Therefore, the β-subunit is used as a biochemical marker in prenatal screenings. In addition, the "home" test for pregnancy in the form of a strip is based on determining the presence of the β-subunit.
Functions of hCG
The main task of chorionic gonadotropin is to prolong the existence of the corpus luteum, which produces progesterone (a hormone necessary for the development of the fetus). At the same time, under the influence of hCG, the corpus luteum produces a very large amount of progesterone, which is impossible during the normal functioning of the body of a non-pregnant woman.
The corpus luteum forms at the site of a ruptured follicle after the release of an egg from it (ovulation). In a normal menstrual cycle, the corpus luteum exists for about 10-12 days, after which it dissolves.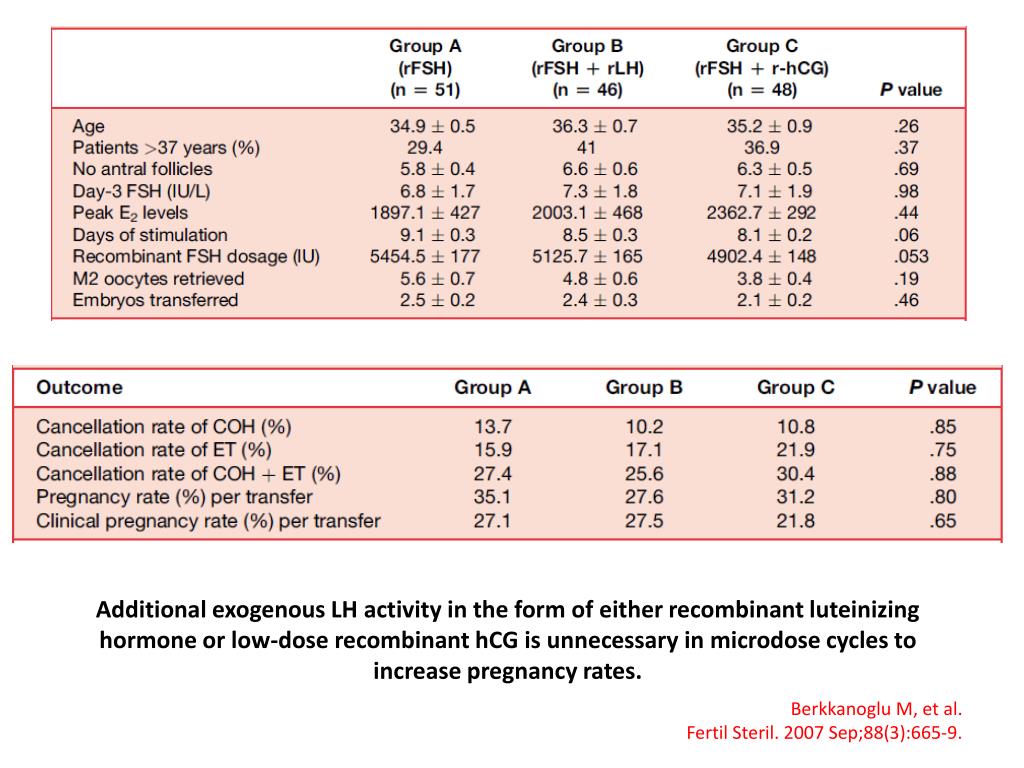 When pregnancy occurs, hCG does not allow it to disappear so that the production of progesterone does not stop. HCG will maintain the existence of the corpus luteum until the placenta of the fetus fully matures and begins to produce the required amount of progesterone on its own, i.e. by the end of the first trimester.
When pregnancy occurs, hCG does not allow it to disappear so that the production of progesterone does not stop. HCG will maintain the existence of the corpus luteum until the placenta of the fetus fully matures and begins to produce the required amount of progesterone on its own, i.e. by the end of the first trimester.
Thus, the level of the hormone begins to increase rapidly from the first days of pregnancy: starting from 0-25 mIU / ml and reaching approximately 200,000 mIU / ml by the twelfth week of pregnancy. Further, the level of hCG will gradually decrease, while still continuing to remain quite high.
In addition, human chorionic gonadotropin has an effect on the secretion of hormones in the adrenal cortex. An increase in the synthesis of glucocorticoids in pregnant women plays an important role in the mechanisms of adaptation of the female body to a stressful state, which, in essence, is pregnancy. Also, glucocorticoids provide physiological immunosuppression, which is necessary to support the development of a semi-foreign organism, i.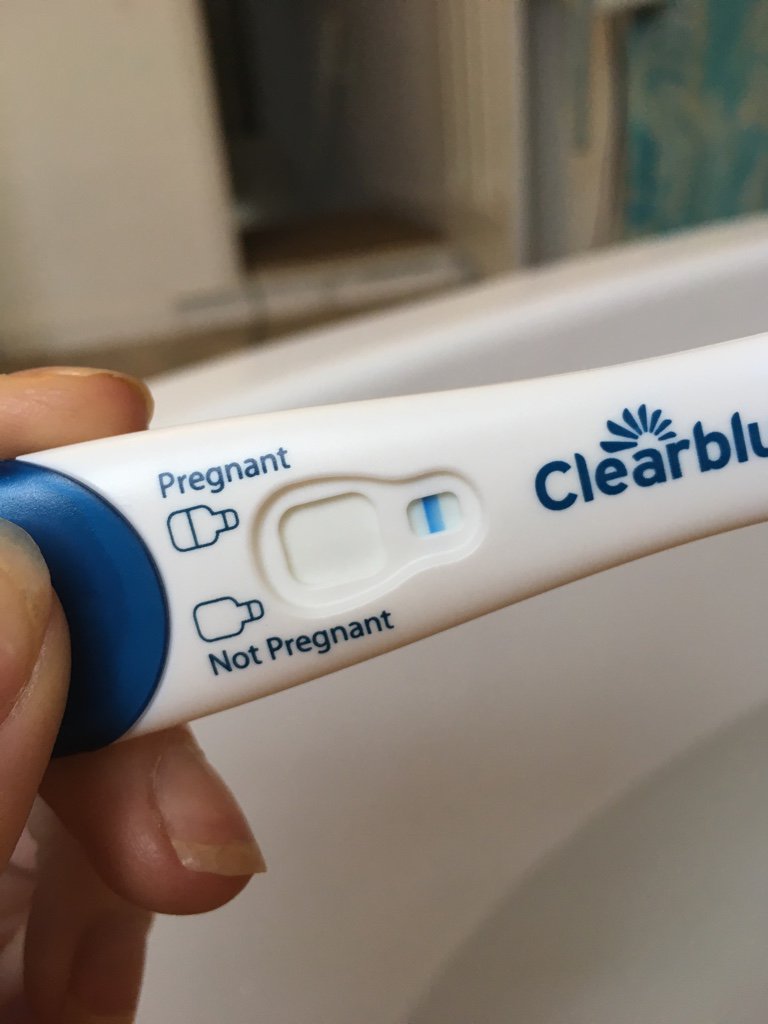 e. fetus.
e. fetus.
Chorionic gonadotropin has a beneficial effect on the development of the placenta, improving its trophism, and helps to increase the number of chorionic villi. HCG is also used to stimulate ovulation during assisted reproductive technologies. An hCG injection is a mandatory component during IVF. HCG contributes to the normal completion of the maturation of the follicles and provokes the release of eggs to the outside.
IVF procedure in Kaliningrad is possible in the IVF Center clinic. The clinic's specialists have extensive experience in various ART methods, including IVF.
When to check the level of hCG
In order to check the presence of pregnancy, women, in most cases, firstly carry out a pregnancy test using a special strip. Such a test strip can be bought at any pharmacy or supermarket. A blood test for hCG levels is one of the first tests that a woman will take after IVF to confirm pregnancy. Usually the test is carried out after a few days of delay in menstruation. With a planned pregnancy or after IVF, it is not rational to conduct a test earlier than 2 weeks after ovulation or embryo transfer: you can get a false result.
With a planned pregnancy or after IVF, it is not rational to conduct a test earlier than 2 weeks after ovulation or embryo transfer: you can get a false result.
Despite the fact that hCG begins to be synthesized in the body immediately after the implantation of the embryo in the uterus, its level in the urine will always be several times lower than in the blood. Therefore, the most informative is a blood test for the content of hCG in it. For examination, venous blood is used, which is taken on an empty stomach.
According to the level of chorionic hormone in the blood, you can determine the course of pregnancy if you monitor its performance in dynamics. The level should increase tens of thousands of times a week. With multiple pregnancies, the level will be even higher: hCG increases in proportion to the number of fetuses.
It should be noted that the same laboratory should be used to track the growth of hCG. This is due to the fact that laboratories may use different research methods: equipment and reagents may differ.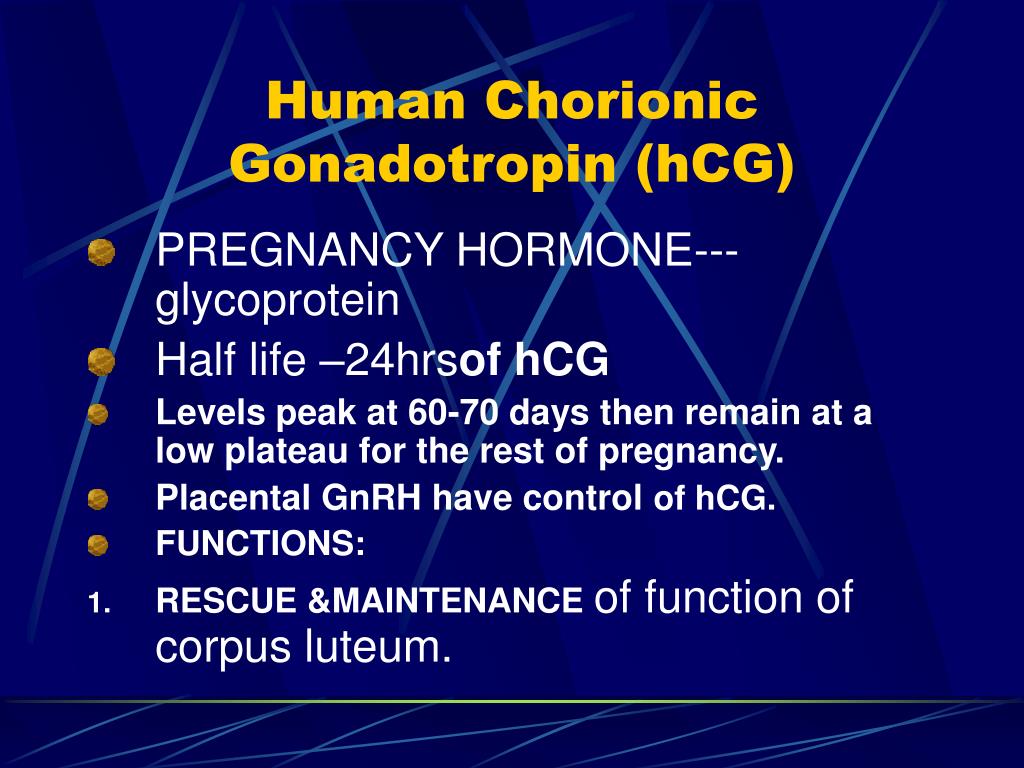 The units of measurement may also differ.
The units of measurement may also differ.
The study of hCG in dynamics also allows you to notice a decrease in its level in time, which may indicate the appearance of pregnancy developmental disorders.
In addition to the course of pregnancy, hCG analysis is part of prenatal screenings, which are carried out in the first and second trimester, to identify the risk of genetic abnormalities (Down syndrome, Edwards, etc.). During screenings, the hCG β-subunit is examined, as well as indicators of other hormones, the results of preliminary ultrasound and the incoming questionnaire data, which indicate the history of the pregnant woman. If the screening results show a high risk of pathologies, the woman is referred for invasive examinations, which will more accurately show the condition of the fetus.
Low hCG in ectopic pregnancy
An ectopic pregnancy is a condition in which a fertilized egg is implanted elsewhere in the female reproductive system than in the uterine wall.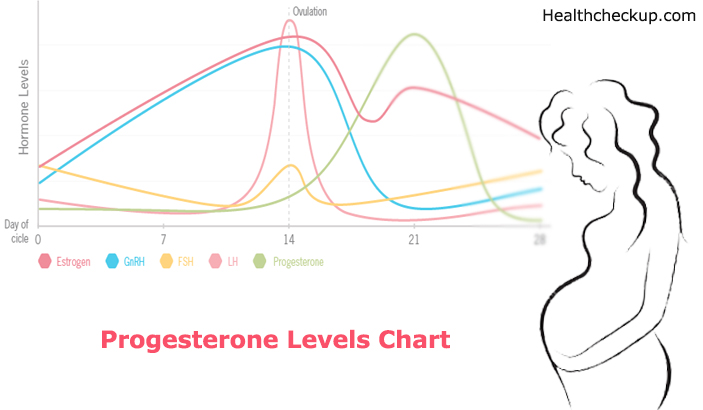 In most cases, this site is the fallopian tubes. This condition is very dangerous for a woman's health: it can cause deformation of the reproductive organs, severe bleeding, and even death. An ectopic pregnancy is difficult to diagnose right away because its onset is very similar to a normal pregnancy. During an ectopic pregnancy, menstruation is delayed, the level of the hormone in the blood begins to rise, respectively, and the test strip will give a positive result.
In most cases, this site is the fallopian tubes. This condition is very dangerous for a woman's health: it can cause deformation of the reproductive organs, severe bleeding, and even death. An ectopic pregnancy is difficult to diagnose right away because its onset is very similar to a normal pregnancy. During an ectopic pregnancy, menstruation is delayed, the level of the hormone in the blood begins to rise, respectively, and the test strip will give a positive result.
In the early stages, an ectopic pregnancy can only be detected by ultrasound. A signal to check the localization of implantation will be low hCG. With an ectopic pregnancy, the hCG level will first rise as usual, and then it will begin to drop sharply. That is why it is useful to conduct a study of hCG in dynamics.
An ectopic pregnancy can only be treated with surgery. If an ectopic pregnancy is localized in the fallopian tube, then it must be removed to preserve the rest of the reproductive system and the health of the woman.