Pregnant anxiety and depression
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders. This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid.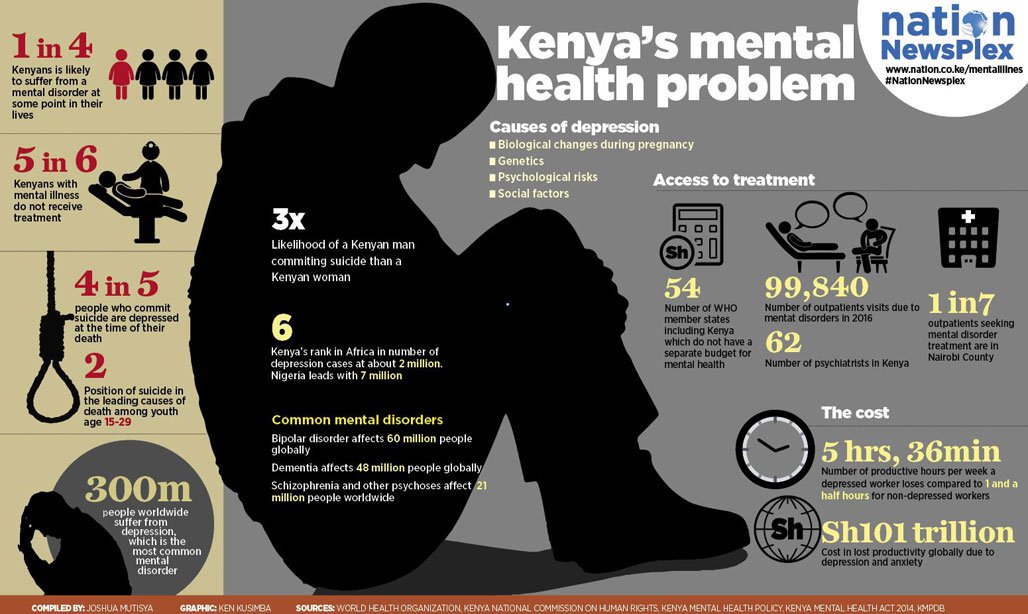 If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
Alcohol, Tobacco, and Other Drugs
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Misusing alcohol, tobacco, and other drugs can have both immediate and long-term health effects.The misuse and abuse of alcohol, tobacco, illicit drugs, and prescription medications affect the health and well-being of millions of Americans. SAMHSA’s 2020 National Survey on Drug Use and Health reports that approximately 19.3 million people aged 18 or older had a substance use disorder in the past year.
Alcohol
Data:
- In 2020, 50.0% of people aged 12 or older (or 138.5 million people) used alcohol in the past month (i.e., current alcohol users) (2020 NSDUH)
- Among the 138.5 million people who were current alcohol users, 61.
 6 million people (or 44.4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH)
6 million people (or 44.4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH) - The percentage of people who were past month binge alcohol users was highest among young adults aged 18 to 25 (31.4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH)
- The 2019 National Survey on Drug Use and Health reports that 139.7 million Americans age 12 or older were past month alcohol users, 65.8 million people were binge drinkers in the past month, and 16 million were heavy drinkers in the past month
- About 2.3 million adolescents aged 12 to 17 in 2019 drank alcohol in the past month, and 1.2 million of these adolescents binge drank in that period (2019 NSDUH)
- Approximately 14.5 million people age 12 or older had an alcohol use disorder (2019 NSDUH)
- Excessive alcohol use can increase a person’s risk of stroke, liver cirrhosis, alcoholic hepatitis, cancer, and other serious health conditions
- Excessive alcohol use can also lead to risk-taking behavior, including driving while impaired.
 The Centers for Disease Control and Prevention reports that 29 people in the United States die in motor vehicle crashes that involve an alcohol-impaired driver daily
The Centers for Disease Control and Prevention reports that 29 people in the United States die in motor vehicle crashes that involve an alcohol-impaired driver daily
Programs/Initiatives:
- STOP Underage Drinking interagency portal - Interagency Coordinating Committee on the Prevention of Underage Drinking
- Interagency Coordinating Committee on the Prevention of Underage Drinking
- Talk. They Hear You.
- Underage Drinking: Myths vs. Facts
- Talking with your College-Bound Young Adult About Alcohol
Relevant links:
- National Association of State Alcohol and Drug Abuse Directors
- Department of Transportation Office of Drug & Alcohol Policy & Compliance
- Alcohol Policy Information Systems Database (APIS)
- National Institute on Alcohol Abuse and Alcoholism
Tobacco
Data:
- In 2020, 20.7% of people aged 12 or older (or 57.
 3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH)
3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH) - Among past month users of nicotine products, nearly two thirds of adolescents aged 12 to 17 (63.1%) vaped nicotine but did not use tobacco products. In contrast, 88.9% of past month nicotine product users aged 26 or older used only tobacco products (2020 NSDUH)
- Data from the 2019 NSDUH reports that 58.1 million people were current (i.e., past month) tobacco users. Specifically, 45.9 million people aged 12 or older in 2019 were past month cigarette smokers (2019 NSDUH)
- Tobacco use is the leading cause of preventable death, often leading to lung cancer, respiratory disorders, heart disease, stroke, and other serious illnesses. The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States
- The CDC’s Office on Smoking and Health reports that more than 16 million Americans are living with a disease caused by smoking cigarettes
Electronic cigarette (e-cigarette) use data:
- Data from the Centers for Disease Control and Prevention’s 2020 National Youth Tobacco Survey.
 Among both middle and high school students, current use of e-cigarettes declined from 2019 to 2020, reversing previous trends and returning current e-cigarette use to levels similar to those observed in 2018
Among both middle and high school students, current use of e-cigarettes declined from 2019 to 2020, reversing previous trends and returning current e-cigarette use to levels similar to those observed in 2018 - E-cigarettes are not safe for youth, young adults, or pregnant women, especially because they contain nicotine and other chemicals
Resources:
- Tips for Teens: Tobacco
- Tips for Teens: E-cigarettes
- Implementing Tobacco Cessation Programs in Substance Use Disorder Treatment Settings
- Synar Amendment Program
Links:
- Truth Initiative
- FDA Center for Tobacco Products
- CDC Office on Smoking and Health
- National Institute on Drug Abuse: Tobacco, Nicotine, and E-Cigarettes
- National Institute on Drug Abuse: E-Cigarettes
Opioids
Data:
- Among people aged 12 or older in 2020, 3.4% (or 9.5 million people) misused opioids in the past year.
 Among the 9.5 million people who misused opioids in the past year, 9.3 million people misused prescription pain relievers and 902,000 people used heroin (2020 NSDUH)
Among the 9.5 million people who misused opioids in the past year, 9.3 million people misused prescription pain relievers and 902,000 people used heroin (2020 NSDUH) - An estimated 745,000 people had used heroin in the past year, based on 2019 NSDUH data
- In 2019, there were 10.1 million people age 12 or older who misused opioids in the past year. The vast majority of people misused prescription pain relievers (2019 NSDUH)
- An estimated 1.6 million people aged 12 or older had an opioid use disorder based on 2019 NSDUH data
- Opioid use, specifically injection drug use, is a risk factor for contracting HIV, Hepatitis B, and Hepatitis C. The CDC reports that people who inject drugs accounted for 9 percent of HIV diagnoses in the United States in 2016
- According to the Centers for Disease Control and Prevention’s Understanding the Epidemic, an average of 128 Americans die every day from an opioid overdose
Resources:
- Medication-Assisted Treatment
- Opioid Overdose Prevention Toolkit
- TIP 63: Medications for Opioid Use Disorder
- Use of Medication-Assisted Treatment for Opioid Use Disorder in Criminal Justice Settings
- Opioid Use Disorder and Pregnancy
- Clinical Guidance for Treating Pregnant and Parenting Women With Opioid Use Disorder and Their Infants
- The Facts about Buprenorphine for Treatment of Opioid Addiction
- Pregnancy Planning for Women Being Treated for Opioid Use Disorder
- Tips for Teens: Opioids
- Rural Opioid Technical Assistance Grants
- Tribal Opioid Response Grants
- Provider’s Clinical Support System - Medication Assisted Treatment Grant Program
Links:
- National Institute on Drug Abuse: Opioids
- National Institute on Drug Abuse: Heroin
- HHS Prevent Opioid Abuse
- Community Anti-Drug Coalitions of America
- Addiction Technology Transfer Center (ATTC) Network
- Prevention Technology Transfer Center (PTTC) Network
Marijuana
Data:
- The percentage of people who used marijuana in the past year was highest among young adults aged 18 to 25 (34.
 5%) compared with 16.3% of adults aged 26 or older and 10.1% of adolescents aged 12 to 17 (2020 NSDUH)
5%) compared with 16.3% of adults aged 26 or older and 10.1% of adolescents aged 12 to 17 (2020 NSDUH) - 2019 NSDUH data indicates that 48.2 million Americans aged 12 or older, 17.5 percent of the population, used marijuana in the past year
- Approximately 4.8 million people aged 12 or older in 2019 had a marijuana use disorder in the past year (2019 NSDUH)
- Marijuana can impair judgment and distort perception in the short term and can lead to memory impairment in the long term
- Marijuana can have significant health effects on youth and pregnant women.
Resources:
- Know the Risks of Marijuana
- Marijuana and Pregnancy
- Tips for Teens: Marijuana
Relevant links:
- National Institute on Drug Abuse: Marijuana
- Addiction Technology Transfer Centers on Marijuana
- CDC Marijuana and Public Health
Emerging Trends in Substance Misuse:
- Methamphetamine—In 2019, NSDUH data show that approximately 2 million people used methamphetamine in the past year.
 Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia.
Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia. - Cocaine—In 2019, NSDUH data show an estimated 5.5 million people aged 12 or older were past users of cocaine, including about 778,000 users of crack. The CDC reports that overdose deaths involving have increased by one-third from 2016 to 2017. In the short term, cocaine use can result in increased blood pressure, restlessness, and irritability. In the long term, severe medical complications of cocaine use include heart attacks, seizures, and abdominal pain.
- Kratom—In 2019, NSDUH data show that about 825,000 people had used Kratom in the past month. Kratom is a tropical plant that grows naturally in Southeast Asia with leaves that can have psychotropic effects by affecting opioid brain receptors.
 It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
Resources:
- Tips for Teens: Methamphetamine
- Tips for Teens: Cocaine
- National Institute on Drug Abuse
More SAMHSA publications on substance use prevention and treatment.
Last Updated: 04/27/2022
Pregnancy against the background of anxiety-depressive states Obstetrics and Gynecology
1 First Moscow State Medical University. I. M. Sechenov, Moscow; 2 FGBU Scientific Center for Obstetrics, Gynecology and Perinatology named after Academician V. I. Kulakov, Ministry of Health of Russia, Moscow
In recent years, the number of studies on the psychophysiological state of pregnant women has increased. Anxiety and depression are common but often unrecognized conditions that lead to negative consequences for the health of the woman and the fetus. The number of women experiencing anxiety throughout pregnancy and taking psychotropic drugs in connection with this is increasing. However, the use of drugs is considered unsafe for the mother and fetus, which requires the search for alternative methods for correcting the psychological conditions of pregnant women. The review presents data for the last 10 years on the impact and relationship of anxiety, depression, fear of childbirth on the course of childbirth, as well as possible methods of prenatal non-drug psychocorrection. nine0004
The number of women experiencing anxiety throughout pregnancy and taking psychotropic drugs in connection with this is increasing. However, the use of drugs is considered unsafe for the mother and fetus, which requires the search for alternative methods for correcting the psychological conditions of pregnant women. The review presents data for the last 10 years on the impact and relationship of anxiety, depression, fear of childbirth on the course of childbirth, as well as possible methods of prenatal non-drug psychocorrection. nine0004
anxiety
depression
pregnancy
psychotherapy
According to the World Health Organization, mental illness is one of the main components of illness in women aged 15–44 years [1]. The prevalence of mental disorders during pregnancy is similar to that in the postpartum period and ranges from 10 to 50% depending on the sample. At the same time, it is higher in groups with low socioeconomic status, in adolescents, and also in women with a history of mental illness [2–6]. According to A. Faisal-Cury, P. Rossi Menezes, “for generalized anxiety disorder, the prevalence rate during pregnancy is about 5%, while anxiety disorders associated with pregnancy occur in 54% of women” [7]. nine0004
According to A. Faisal-Cury, P. Rossi Menezes, “for generalized anxiety disorder, the prevalence rate during pregnancy is about 5%, while anxiety disorders associated with pregnancy occur in 54% of women” [7]. nine0004
According to some authors, subclinical anxiety is widespread and more common than depressive disorders in all periods of pregnancy [8]. Research results A.M. Lee, S.K. Lam, S.M. Sze Mun Lau et al. showed that about 54% of women experience anxiety throughout pregnancy (as opposed to depression, which is found in 34% of women). The first manifestations of anxiety can be observed in different periods of pregnancy, however, anxiety and depression are most common and more pronounced in the first and third trimesters of pregnancy, which makes it difficult to diagnose them during single examinations [9].]. As noted by J. Alder, N. Fink, J. Bitzer et al., anxiety during pregnancy often remains unrecognized and little studied [10]. C. Teixeira et al. conducted a study that showed that a higher prevalence of anxiety disorders was noted in the first (15%) and third trimesters (18%) of pregnancy, while in the second trimester of pregnancy, prevalence rates were lower [11].
A large longitudinal study of 8323 pregnant women by J. Heron et al. found that anxiety was diagnosed in approximately 16% of women at examination at 32 weeks and in 8.5% at examination 8 weeks after delivery [12] . Women with increased levels of anxiety in the 1st trimester of pregnancy are more likely to experience nausea and vomiting, as a result of which they visit the doctor more often [13]. In addition, anxiety during pregnancy has an impact on changing the pattern of behavior, increasing the frequency of alcohol and tobacco use [14]. nine0004
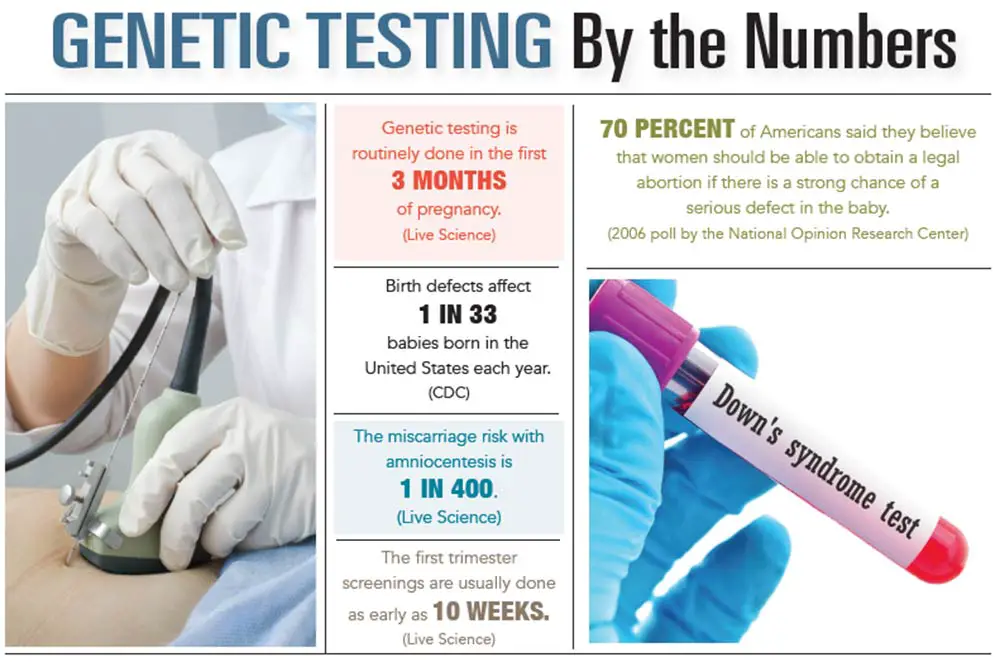
Anxiety during pregnancy is a predictor of complications in the neonatal period [15]. Invasive procedures such as in vitro fertilization (IVF), amniocentesis, comorbidities (arterial hypertension, diabetes mellitus) and fetal abnormalities are additional causes that increase anxiety levels [16, 17]. K. Stahl et al. consider that doctors labeling pregnancy as “difficult” or “risk-related” increases the level of anxiety in pregnant women due to a sense of loss of control and feelings of helplessness [18]. However, researchers' conclusions often have a limited range of interpretation due to small sample sizes and methodological limitations [10]. nine0004
However, researchers' conclusions often have a limited range of interpretation due to small sample sizes and methodological limitations [10]. nine0004
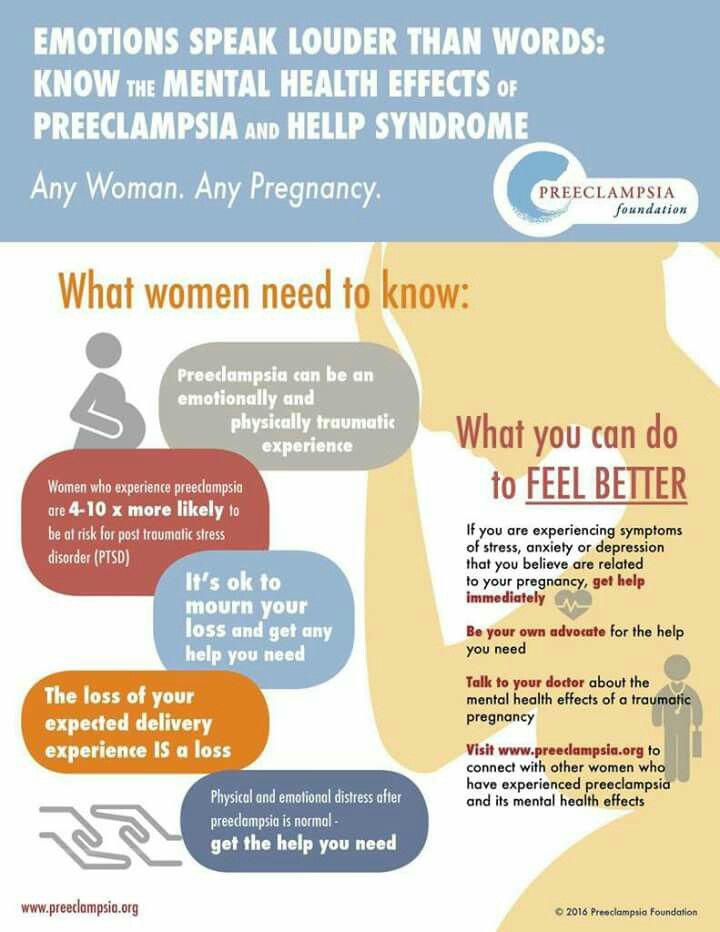
The results of studies on the role of increased levels of anxiety in the development of preeclampsia are contradictory [14, 19]. During the T Kurki. et al. In a prospective population-based study of 623 women with a first singleton pregnancy, 28 women (4.5%) developed preeclampsia. Multivariate analysis, after adjusting for potential confounding factors, showed an increased risk of preeclampsia in the presence of depression (odds ratio 2.5, 95% confidence interval 1.1–5.4) and anxiety (odds ratio 3.2, 95% confidence interval 1.4–7.4). J. Sikkema in his study assessed the level of cortisol in saliva in women with anxiety and the development of preeclampsia. Of the 250 pregnant women examined, preeclampsia occurred in 9 cases. When compared with the control group, there was a similar level of change in the level of cortisol in saliva. The analysis performed did not reveal significant differences in cortisol levels or levels of anxiety between groups, indicating that there is no role for anxiety or increased levels of stress hormones in the pathogenesis of preeclampsia [19].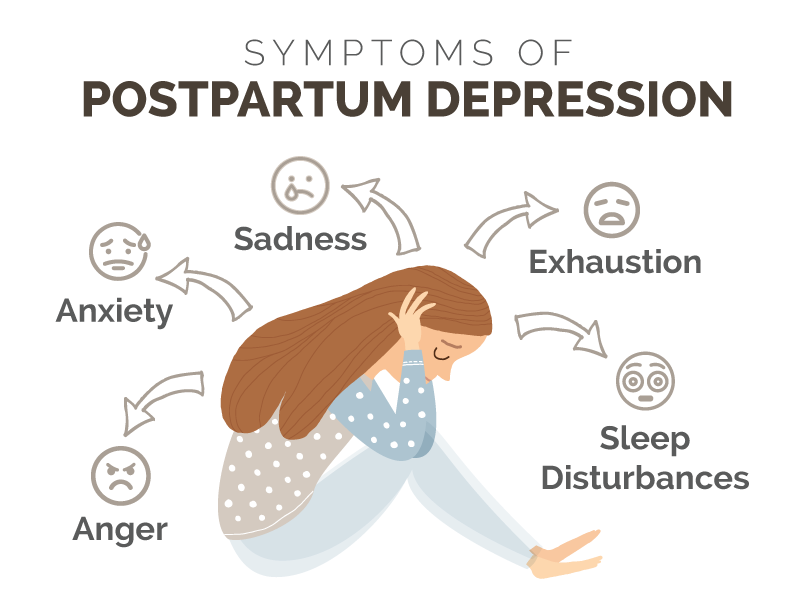 Numerous studies have examined the relationship between anxiety and depression during pregnancy. So, T.S. Rutledge et al. suggest an extremely adverse effect of comorbid depression and anxiety on cardiovascular morbidity in the mother [20]. T. Field et al. confirms the impact of this kind of comorbidity on the prevalence of preterm birth compared with other groups of pregnant women [21]. ON. Korotkova found that anxiety disorders during pregnancy are one of the main risk factors for emotional stress after childbirth, leading to maladjustment, regardless of the existence of depression and other disorders. This study notes that an increase in the level of anxiety, depression of moderate or severe severity, as a rule, is accompanied by dyssomnic disorders [22]. Interesting studies of the relationship between anxiety and depressive disorders and biochemical processes occurring in a woman's body. As noted by J. Dayan, C. Creveuil, M.N. Marks et al., the synthesis and release of placental corticotropin-releasing hormone (CRH) occurs as a result of stimulation by stress hormones, leading to the activation of labor [23].
Numerous studies have examined the relationship between anxiety and depression during pregnancy. So, T.S. Rutledge et al. suggest an extremely adverse effect of comorbid depression and anxiety on cardiovascular morbidity in the mother [20]. T. Field et al. confirms the impact of this kind of comorbidity on the prevalence of preterm birth compared with other groups of pregnant women [21]. ON. Korotkova found that anxiety disorders during pregnancy are one of the main risk factors for emotional stress after childbirth, leading to maladjustment, regardless of the existence of depression and other disorders. This study notes that an increase in the level of anxiety, depression of moderate or severe severity, as a rule, is accompanied by dyssomnic disorders [22]. Interesting studies of the relationship between anxiety and depressive disorders and biochemical processes occurring in a woman's body. As noted by J. Dayan, C. Creveuil, M.N. Marks et al., the synthesis and release of placental corticotropin-releasing hormone (CRH) occurs as a result of stimulation by stress hormones, leading to the activation of labor [23]. Another possible mechanism that worsens the outcome of pregnancy in anxiety and depression is the complex biochemical interaction of various neurotransmitters. So, according to the results of research T Field. found a significant decrease in dopamine levels in early and late gestation in women with comorbid depression and anxiety. The highest level of adrenaline was noted in the same group in the postnatal period. According to L.M. Evans, M.M. Myers, C. Monk, comorbid depression and anxiety during pregnancy is a condition in which excessive stimulation of the hypothalamic-pituitary-adrenal-cortical axis (HPA) with excessive secretion of stress hormones is most likely [24]. P. Rondó, J. Martini et al. concluded that the presence of anxiety disorders and subjectively perceived distress in a pregnant woman leads to a significant increase in the risk of intrauterine growth retardation [25], affects the formation of brain structures responsible for mental health, which increases the overall susceptibility to psychopathological disorders in a child [26] and also increases the risk of maternal depressive disorders in the postpartum period [27].
Another possible mechanism that worsens the outcome of pregnancy in anxiety and depression is the complex biochemical interaction of various neurotransmitters. So, according to the results of research T Field. found a significant decrease in dopamine levels in early and late gestation in women with comorbid depression and anxiety. The highest level of adrenaline was noted in the same group in the postnatal period. According to L.M. Evans, M.M. Myers, C. Monk, comorbid depression and anxiety during pregnancy is a condition in which excessive stimulation of the hypothalamic-pituitary-adrenal-cortical axis (HPA) with excessive secretion of stress hormones is most likely [24]. P. Rondó, J. Martini et al. concluded that the presence of anxiety disorders and subjectively perceived distress in a pregnant woman leads to a significant increase in the risk of intrauterine growth retardation [25], affects the formation of brain structures responsible for mental health, which increases the overall susceptibility to psychopathological disorders in a child [26] and also increases the risk of maternal depressive disorders in the postpartum period [27].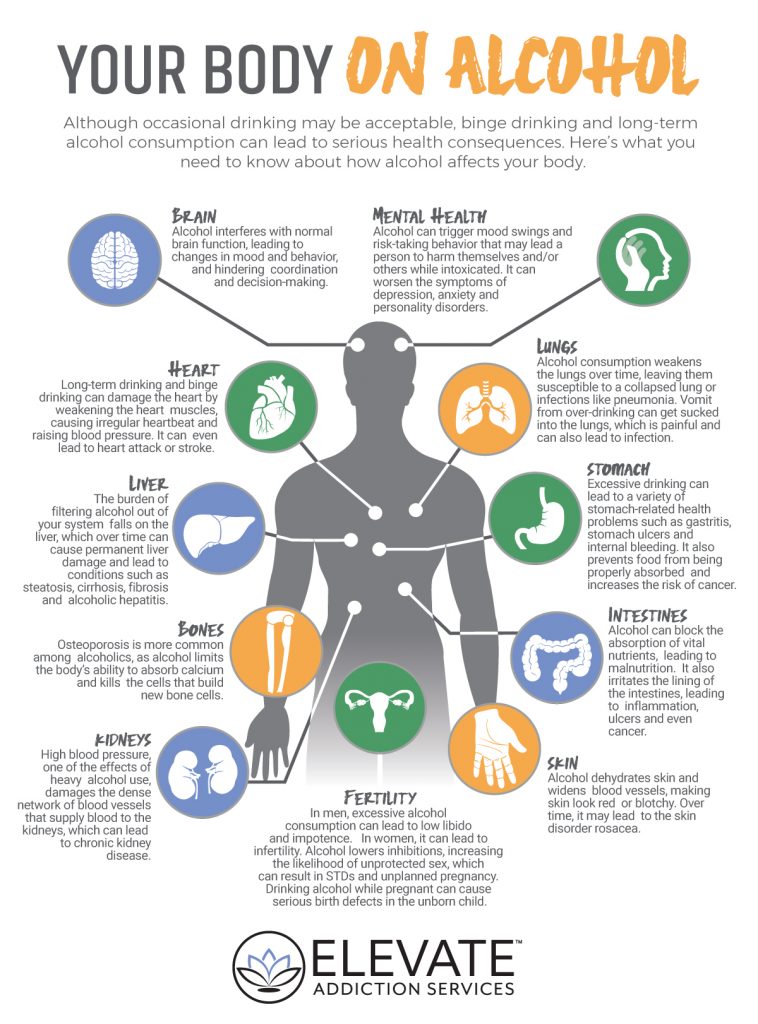 Newborns whose mothers had depression, comorbid depression, and anxiety during pregnancy had the highest levels of cortisol and norepinephrine and significantly lower levels of dopamine and serotonin [21]. The hypothesis that women with anxiety and depressive disorders are more likely to experience the fear of childbirth (tocophobia), compared with women without mental disorders, has been confirmed by studies [28, 29].
Newborns whose mothers had depression, comorbid depression, and anxiety during pregnancy had the highest levels of cortisol and norepinephrine and significantly lower levels of dopamine and serotonin [21]. The hypothesis that women with anxiety and depressive disorders are more likely to experience the fear of childbirth (tocophobia), compared with women without mental disorders, has been confirmed by studies [28, 29].
Tokophobia, according to K. Hofberg and I. Brockington, is defined as an intense fear in which a woman experiences a state of horror at the mere thought of childbirth and, for this reason, tries to avoid pregnancy [30].
Fear of childbirth can occur in both primiparous and multiparous women, however, according to K. Spice, S.L. Jones et al., in primiparas, the prevalence of fear of childbirth is the highest [29]. C. Nilsson et al. revealed a pattern that women who already have the experience of childbirth are more self-confident and calm. However, the same authors note that in the case of a previous negative experience of childbirth, the likelihood of fear of childbirth during repeated pregnancy increases sharply [31]. nine0004
nine0004
In a large prospective cohort study of 25,297 healthy women conducted in Denmark between 1997 and 2003, an association was established between fear of childbirth and incoordination of labor [5]. Fear and anxiety during pregnancy lead to a violation of the physiological course of labor, causing a violation of the contractile activity of the myometrium, increase the duration of the second stage of labor (as well as fetal asphyxia, weakness of labor) and are the most common indication for caesarean section [32, 33]. Fear of childbirth, smoking, repeated childbirth, as well as concomitant mental disorders increase the frequency of taking psychotropic drugs during pregnancy [34]. nine0004
However, along with pharmacological preparations, non-drug psychotherapeutic methods can also be used. Research results A.M. Costei, E. Kozer, T. Ho et al. show that anxiety disorders respond well to treatment with cognitive behavioral therapy [35]. I. Elkin et al. found that the effectiveness of interpersonal psychotherapy is comparable in effectiveness to imipramine and cognitive-behavioral psychotherapy in the treatment of mild to moderate depression [36]. As noted by R. Reay, Y. Fisher, M. Robertson et al., women in the active intervention group had a significantly more pronounced decrease in the score on the Hamilton depression scale and on the Beck questionnaire [37]. nine0004
As noted by R. Reay, Y. Fisher, M. Robertson et al., women in the active intervention group had a significantly more pronounced decrease in the score on the Hamilton depression scale and on the Beck questionnaire [37]. nine0004
Another effective therapeutic tool within the framework of integrative medical approaches is the use of music, which, by neutralizing negative emotions, increases the threshold for stress resistance, promotes harmonization of internal processes, and helps the patient achieve deeper relaxation [38]. Women who had a caesarean delivery with music therapy experienced a significant reduction in anxiety and increased satisfaction with the operation [39]. The use of resonant music therapy in the management of high-risk pregnant women has shown a decrease in the level of anxiety according to the Spielberger scale [40]. Psychoeducational approaches are also used in work with pregnant women, which include various psychological strategies with group education to change a woman's attitude towards pregnancy and childbirth.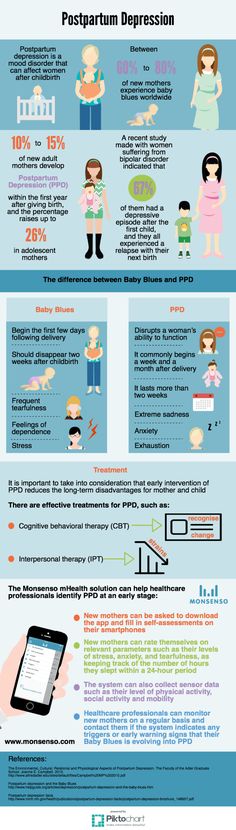 In one randomized clinical trial, which included 176 pregnant women with fear of childbirth, against the background of psychoeducational techniques, there was a decrease in the fear of vaginal delivery [41]. nine0004
In one randomized clinical trial, which included 176 pregnant women with fear of childbirth, against the background of psychoeducational techniques, there was a decrease in the fear of vaginal delivery [41]. nine0004
The format of the work consisted of ten group sessions (main group - 85 women), 91 women received standard therapy. Although there was no reduction in overall anxiety in the active intervention group compared to controls, there was a reduction in fear of labor pain (p=0.04). An analysis of a randomized controlled trial of 58 pregnant women who used active and passive relaxation showed a significant reduction in anxiety, maternal heart rate (HR), and serum cortisol concentrations in both groups compared with baseline. At the same time, in the active intervention group, there was a decrease in the level of anxiety and heart rate compared with the passive relaxation group [42]. nine0004
Conclusion
Mental disorders are a serious social and medical problem. Worldwide, there is an increasing number of women experiencing anxiety throughout pregnancy and taking psychotropic drugs in connection with this.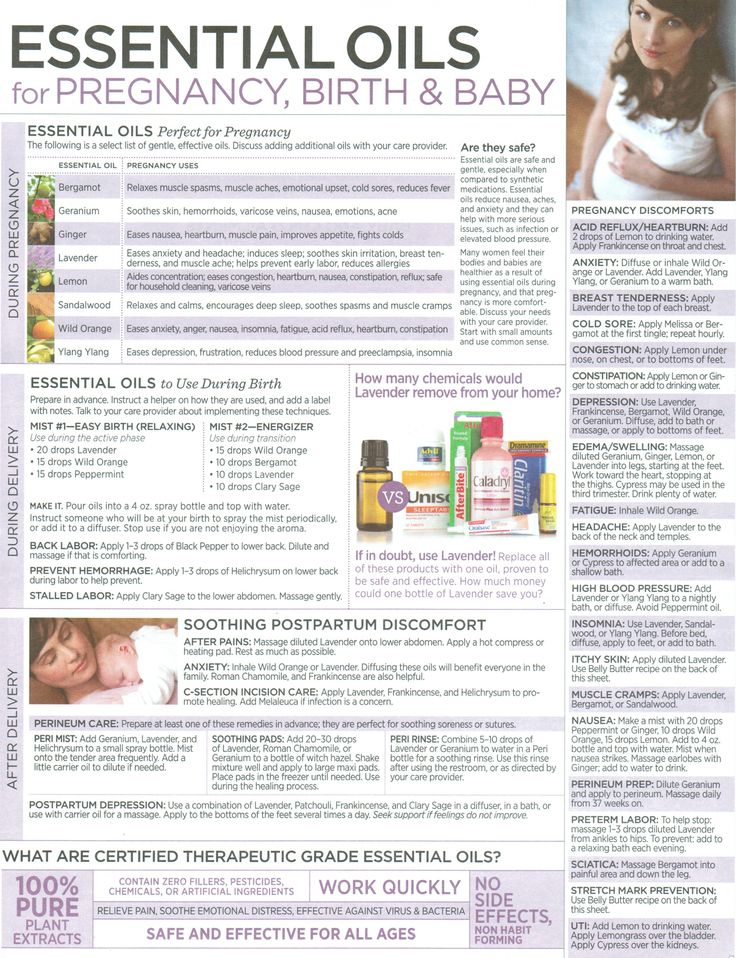 Obstetricians and general practitioners are interested in finding alternative methods for correcting the psychological conditions of pregnant women due to the fact that the use of drugs is considered unsafe for the mother and fetus. Methods of prenatal preparation enable a woman to optimize her psychophysiological status, reduce the negative expectations of labor pain, and reduce anxiety. In addition, comprehensive psychotherapeutic prenatal preparation contributes to the prevention of postpartum depression, improving perinatal outcomes, improving the quality of life of mother and child. The need to conduct clinical studies of the effectiveness of various methods and directions in the field of perinatal medicine and psychology is dictated by the lack of criteria for assessing the quality of prenatal preparation and a unified psychotherapeutic approach to accompanying pregnant women, taking into account individual characteristics. nine0004
Obstetricians and general practitioners are interested in finding alternative methods for correcting the psychological conditions of pregnant women due to the fact that the use of drugs is considered unsafe for the mother and fetus. Methods of prenatal preparation enable a woman to optimize her psychophysiological status, reduce the negative expectations of labor pain, and reduce anxiety. In addition, comprehensive psychotherapeutic prenatal preparation contributes to the prevention of postpartum depression, improving perinatal outcomes, improving the quality of life of mother and child. The need to conduct clinical studies of the effectiveness of various methods and directions in the field of perinatal medicine and psychology is dictated by the lack of criteria for assessing the quality of prenatal preparation and a unified psychotherapeutic approach to accompanying pregnant women, taking into account individual characteristics. nine0004
1. World Health Organization. The global burden of disease—2004 update. Geneva: World Health Organization; 2008. http://www.who.int/healthinfo/global_burden_disease/2004_report_update/en/
Geneva: World Health Organization; 2008. http://www.who.int/healthinfo/global_burden_disease/2004_report_update/en/
2. De Tychey C., Spitz E., Briancon S., Lighezzolo J., Girvan F., Rosati A. et al. Pre- and postnatal depression and coping: a comparative approach. J. Affect. Discord. 2005; 85:323–26.
3. Giardinelli L., Innocenti A., Benni L., Stefanini M.C., Lino G., Lunardi C. et al. Depression and anxiety in perinatal period: prevalence and risk factors in an Italian sample. Arch. Women's Ment. health. 2012; 15(1): 21–30.
4. Hobfoll S., Ritter C., Lavin J., Hulsizer M., Cameron R. Depression prevalence and incidence among inner-city pregnant and postpartum women. J. Consult. Clin. Psychol. 1995; 63(3): 445–53.
5. Lancaster C., Gold K., Flynn H., Yoo H., Marcus S., Davis M. Risk factors for depressive symptoms during pregnancy: a systematic review. Am J. Obstet. Gynecol. 2010; 202(1): 5–14. nine0004
6. Vesga-López O., Blanco C., Keyes K., Olfson M., Grant B., Hasin D. Psychiatric disorders in pregnant and postpartum women in the United States. Arch. Gen. Psychiatry. 2008; 65(7): 805–15.
Vesga-López O., Blanco C., Keyes K., Olfson M., Grant B., Hasin D. Psychiatric disorders in pregnant and postpartum women in the United States. Arch. Gen. Psychiatry. 2008; 65(7): 805–15.
7. Faisal-Cury A., Rossi Menezes P. Prevalence of anxiety and depression during pregnancy in a private setting sample. Arch.Women's Ment. health. 2007; 10(1): 25–32.
8. Lee A.M., Lam S.K., Sze Mun Lau S.M., Chong C.S., Chui H.W., Fong D.Y. nine0046 Prevalence, course, and risk factors for antenatal anxiety and depression. obstet. Gynecol. 2007; 110(5): 1102–12.
9. Lederman R.P., Lederman E., Work B.A. Jr., McCann D.S. The relationship of maternal anxiety, plasma catecholamines, and plasma cortisol to progress in labor. Am. J. Obstet. Gynecol. 1978; 132(5): 495–500.
10. Alder J., Fink N., Bitzer J., Hösli I., Holzgreve W. Depression and anxiety during pregnancy: a risk factor for obstetric, fetal and neonatal outcome? A critical review of the literature.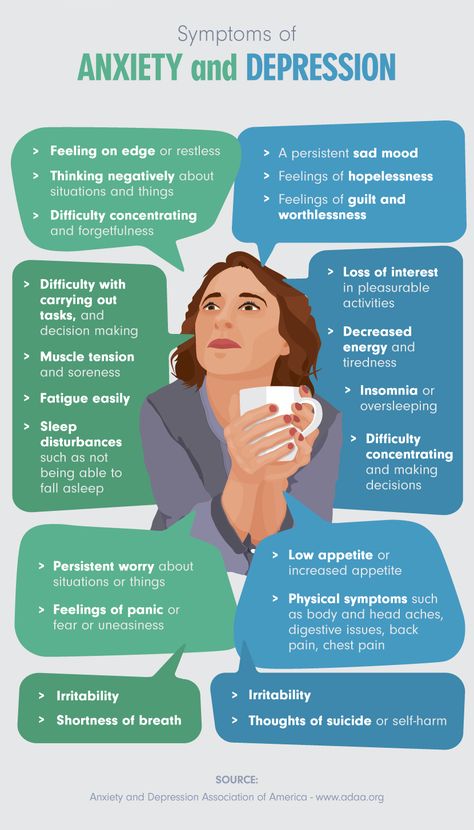 J. Matern. Fetal Neonatal Med. 2007; 20(3):189-209.
J. Matern. Fetal Neonatal Med. 2007; 20(3):189-209.
11. Teixeira C., Figueiredo B., Conde A., Pacheco A., Costa R. Anxiety and depression during pregnancy in women and men. J. Affect. Discord. 2009; 119(1-3):142-8.
12. Heron J., O’Connor T.G., Evans J., Golding J., Glover V. The course of anxiety and depression through pregnancy and the postpartum in a community sample. J. Affect. Discord. 2004; 80(1): 65–73.
13. Stowe Z.N., Hostetter A.L., Newport D.J. The onset of postpartum depression: Implications for clinical screening obstetrical and primary case. Am. J. Obstet. Gynecol. 2005; nineteen2:522–6.
14. Kurki T., Hiilesmaa V., Raitasalo R., Mattila H., Ylikorkala O. Depression and anxiety in early pregnancy and risk for preeclampsia. obstet. Gynecol. 2000; 95(4): 487–90.
15. Zelkowitz P., Papageorgiou A. Maternal anxiety: an emerging prognostic factor in neonatology. Acta Paediatr. 2005; 94(12): 1704–5.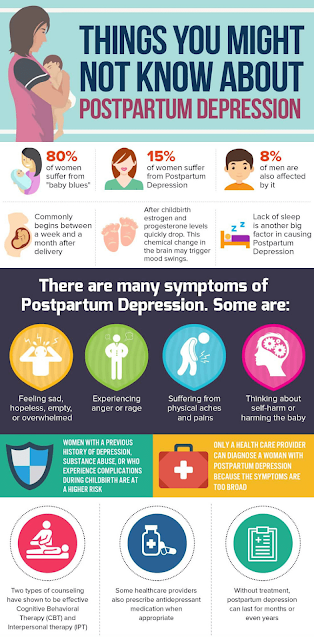
16. Sosa C., Althabe F., Belizan J., Bergel E. Bed rest in singleton pregnancies for preventing preterm birth. Cochrane Database Syst. Rev. 2004; (1): CD003581.pub2
17. Vendittelli F., Lachcar P. Threat of premature labor, stress, psychosocial support and psychotherapy: a review of the literature. Gynecol. obstet. fertil. 2002; 30(6): 503–13.
18. Stahl K., Hundley V. Risk and risk assessment in pregnancy – do we scare because we care? midwifery. 2003; 19(4): 298–309.
19. Sikkema J.M., Robles de Medina P.G., Schaad R.R., Mulder E.J., Bruinse H.W., Buitelaar J.K. et al. Salivary cortisol levels and anxiety are not increased in women destined to develop preeclampsia. J. Psychosom. Res. 2001; 50(1): 45–9.
20. Rutledge T., Linke S.E., Krantz D.S., Johnson B.D., Bittner V., Eastwood J.A. et al. Comorbid depression and anxiety symptoms as predictors of cardiovascular events: results from the NHLBI-sponsored Women's Ischemia Syndrome Evaluation (WISE) study. Psychosom. Med. 2009; 71:958–64.
Psychosom. Med. 2009; 71:958–64.
21. Field T., Diego M., Hernandez-Reif M., Figueiredo B., Deeds O., Ascencio A. et al. Comorbid depression and anxiety effects on pregnancy and neonatal outcome. Infant Behav. dev. 2010; 33(1): 23–9.
22. Korotkova N.A. The influence of pregnancy and childbirth on the occurrence of postpartum stress and psychovegetative disorders in puerperas: Abstract of the thesis. dis. … Dr. med. Sciences. M.; 2011
23 Dayan J., Creveuil C., Marks M.N., Conroy S., Herlicoviez M., Dreyfus M. et al. Prenatal depression, prenatal anxiety, and spontaneous preterm birth: a prospective cohort study among women with early and regular care. Psychosom. Med. 2006; 68(6): 938–46.
24. Evans L.M., Myers M.M., Monk C. Pregnant women's cortisol is elevated with anxiety and depression – but only when comorbid. Arch. Women's Ment. health. 2008; 11(3): 239–48.
25. Rondó P., Ferreira R., Nogueira F. , Ribeiro M., Lobert H., Artes R. Maternal psychological stress and distress as predictors of low birth weight, prematurity and intrauterine growth retardation. Eur. J.Clin. Nutr. 2003; 57(2): 266–72.
, Ribeiro M., Lobert H., Artes R. Maternal psychological stress and distress as predictors of low birth weight, prematurity and intrauterine growth retardation. Eur. J.Clin. Nutr. 2003; 57(2): 266–72.
26. Lupien S.J., McEwen B.S., Gunnar M.R., Heim C. Effects of stress throughout the lifespan on the brain, behavior and cognition. Nat. Rev. neurosci. 2009; 10(6): 434–45.
27. Martini J., Knappe S., Beesdo-Baum K., Lieb R., Wittchen H.U. Anxiety disorders before birth and self-perceived distress during pregnancy: associations with maternal depression and obstetric, neonatal and early childhood outcomes. early hum. dev. 2010; 86(5): 305–10.
28. Storksen H.T., Eberhard-Gran M., Garthus-Niegel S., Eskild A. Fear of childbirth; the relation to anxiety and depression. Acta Obstet. Gynecol. Scand. 2012; 91:237–42.
29. Spice K., Jones S.L., Hadjistavropoulos H.D., Kowalyk K., Stewart S.H. Prenatal fear of childbirth and anxiety sensitivity.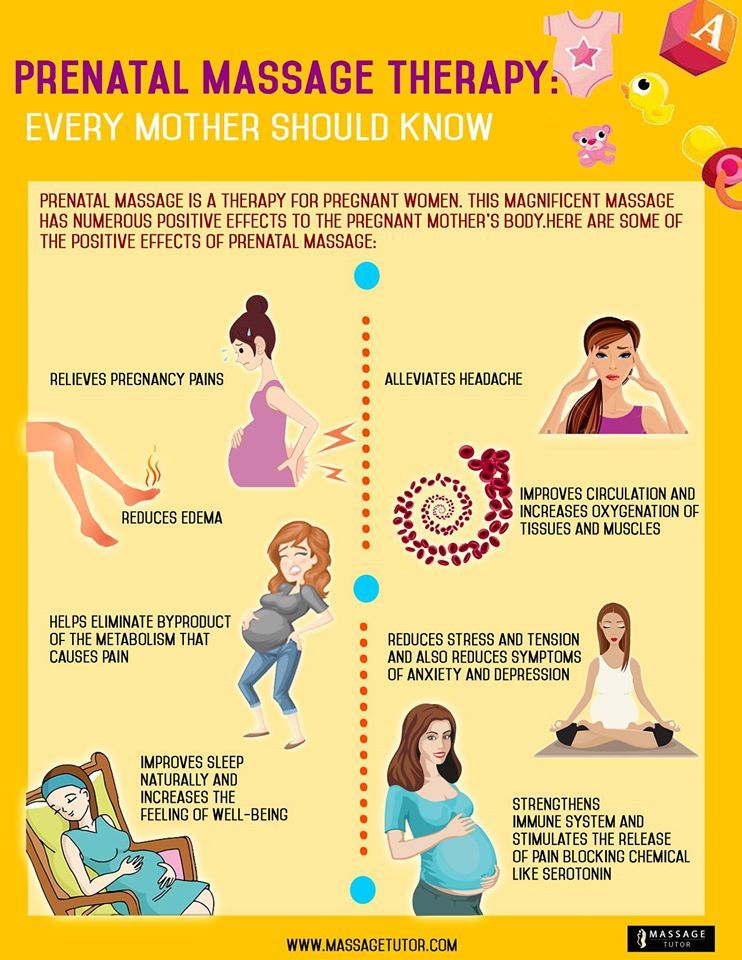 J. Psychosom. obstet. Gynaecol. 2009; 30:168–74.
J. Psychosom. obstet. Gynaecol. 2009; 30:168–74.
30. Hofberg K., Brockington I. Tokophobia: an unreasoning dread of childbirth. Br. J. Psychiatry. 2000; 176:83–5.
31. Nilsson C., Lundgren I. Women's lived experience of fear of childbirth. midwifery. 2009; 25:1–9.
32. Laursen M., Johansen C., Hedegaard M. Fear of childbirth and risk for birth complications in nulliparous women in the Danish National Birth Cohort. Br. J. Obstet. Gynaecol. 2009; 116(10): 1350–5.
33. Sjögren B., Thomassen P. Obstetric outcome in 100 women with severe anxiety over childbirth. Acta Obstet. Gynecol. Scand. 1997; 76(10): 948–52.
34. Nordeng H., Hansen C., Garthus-Niegel S., Eberhard-Gran M. Fear of childbirth, mental health, and medication use during pregnancy Arch. Women's Ment. health. 2012; 15(3): 203-9.
35. Costei A.M., Kozer E., Ho T., Ito S., Koren G. Perinatal outcome following third trimester exposure to paroxetine. Arch. Pediatr. Adolesc. Med. 2002; 156(11): 1129–32.
Arch. Pediatr. Adolesc. Med. 2002; 156(11): 1129–32.
36. Elkin I., Shea T., Watkins J. T., Imber S. D., Sotsky S. M., Collins J. F. et al. National Institute of Mental Health Treatment of Depression Collaborative Research Program. General effectiveness of treatments. Arch. Gen. Psychiatry. nineteen89; 46(11): 971–82; discussion: 983.
37. Reay R., Fisher Y., Robertson M., Owen C., Kumar R. The effectiveness of group iterpersonal psychotherapy for postnatal depression: a pilot study. Arch. Women's Ment. health. 2006; 9(1): 31–9.
38. Olson S.L. Bedside musical care: applications in pregnancy, childbirth and neonatal care. J. Obstet. Gynecol. Neonatal Nurs. 1998; 27:569–75.
39. Chang S.C., Chen C.H. Effects of music therapy on women’s physiologic measures, anxiety and satisfaction during cesarean delivery. Res. Nurs. health. 2005; 28:453–61. nine0004
40. Sidorenko V.N. Clinical application of Medical Resonance Therapy Music in high-risk pregnancies.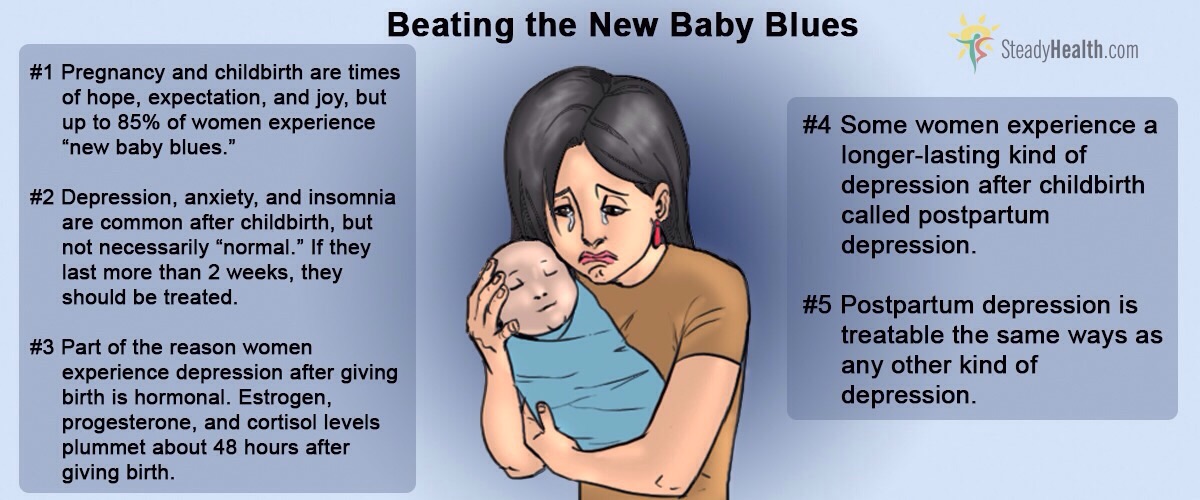 integration physiol. behavior. sci. 2000; 35(3): 199–207.
integration physiol. behavior. sci. 2000; 35(3): 199–207.
41. Saisto T., Salmela-Aro K., Nurmi J.E., Kononen T., Halmesmaki E. A randomized controlled trial of intervention in fear of childbirth. obstet. Gynecol. 2001; 98:820–6.
42. Teixeira J., Martin D., Prendiville O., Glover V. The effects of acute relaxation on indices of anxiety during pregnancy. J. Psychosom. obstet. Gynaecol. 2005; 26(4): 271–6. nine0004
Perova Ekaterina Igorevna, post-graduate student, First Moscow State Medical University. THEM. Sechenov of the Ministry of Health of Russia
Address: 119991, Moscow, st. Trubetskaya, d. 8, building 2. Phone: 8 (915) 359-07-28. E-mail: [email protected]
Stenyaeva Natalia Nikolaevna Academician V.I. Kulakov of the Ministry of Health of Russia
Address: 117997, Moscow, st. academician Oparin, 4. Phone: 8 (495) 735-10-55. E-mail: [email protected]
Apolikhina Inna Anatolyevna, Doctor of Medical Sciences, Professor, Head of the Gynecological Department of Restorative Treatment of the Federal State Budgetary Institution Scientific Center for Anti-Age and Pedagogical Medicine named after A. I. Academician V.I. Kulakov of the Ministry of Health of Russia
I. Academician V.I. Kulakov of the Ministry of Health of Russia
Address: 117997, Moscow, st. academician Oparin, 4. Phone: 8 (495) 735-10-55. E-mail: [email protected]
Treatment of anxiety during pregnancy without antidepressants – Allianz Central Medical Health Center
Pregnancy is a time of happy chores in anticipation of a miracle. But fear for the future baby sometimes overshadows this bright period. “Will I take it? Will he be born healthy? Will the birth go smoothly? Can I bear the pain? Did so-and-so hurt my baby (a glass of champagne at a party before the news of motherhood, a quarrel at work, a smoking neighbor ...).” nine0004
Important
If a woman is suspicious, prone to worries, if she has a first child, or, especially, there were miscarriages before this pregnancy, an anxiety condition may develop during pregnancy.
Inexplicable anxieties that a woman cannot cope with worsen the course of pregnancy, because these are not only subjective experiences and thoughts, but also quite real symptoms of fear: heartbeat and rapid breathing, sweating, dizziness, nervous trembling, aggravation of symptoms of toxicosis of pregnant women. All this, of course, harms the child. Therefore, a pregnant woman with an anxiety disorder needs the help of a doctor. nine0004
All this, of course, harms the child. Therefore, a pregnant woman with an anxiety disorder needs the help of a doctor. nine0004
Anxiety and pregnancy are frequent neighbors
The entire nervous system of a woman is inflated and aimed at the maximum preservation of the child. But sometimes the hyperactivity of this natural mechanism has the opposite effect. And therefore it is important to monitor the condition of the expectant mother. If she worries more often than she rejoices, her worries do not have a specific reason (the pregnancy is going smoothly), and she cannot distract herself from them - perhaps this is already a disease.
Often a pregnant woman, even realizing that something is wrong with her, is afraid to seek help because she may be advised to terminate the pregnancy or prescribe medications that will harm the baby. There is a way out of this situation! nine0004
Treatment of a pregnant woman is different from therapy for ordinary patients, because it is important not only to help the mother, but also to protect the baby.
The path to happy motherhood
Anxiety disorder after childbirth, especially against the background of postpartum depression, is a frequent visitor to a young family, especially where the child is the first and long-awaited.
For both pregnant and breastfeeding mothers, treating anxiety without antidepressants and sedatives is a priority. And this is not at all a reason to stop breastfeeding - the best thing created for the health of the baby. nine0004
Psychotherapy, auto-training and self-relaxation training, work with significance, in special cases - hypnosis - this is the psychotherapist's arsenal in the case when there are two patients.
The doctors of the Mental Health Center have extensive experience in working with pregnant women and women after childbirth. A full-fledged arsenal of modern psychotherapy tools allows for treatment without drugs, avoiding harmful effects on the child and giving the mother the opportunity to fully enjoy the joy of motherhood.