How large is the uterus
Does a Uterus Really Double in Size During Menstruation?
By Whitney Akers — Updated on September 24, 2018
A viral post that claims the ballooning size of a uterus during a period is to blame for a “heavy” feeling many women experience isn’t backed by science.
A viral photo making its way around Facebook claims to explain the reason many women feel “heavy” during their periods.
The photo compares two uterus models side-by-side. One represents a smaller, nonmenstruating uterus. The other model is a dark-colored menstruating uterus almost double in size.
The claim comes from Apples and Ovaries, an account run by a holistic nutritional therapist and natural fertility health consultant.
“This is why we feel so heavy at the beginning of our bleed. Why it can feel like our uterus is about to drop out and hit the pavement… And why we need to take things slooooooow,” Apples and Ovaries wrote as a caption for the photo.
Nearly 25,000 people have shared the Facebook post and 19,000 have liked it. The resounding response in more than 6,000 comments is, “Well that explains it.”
One woman wrote, “Ahhh, that is a wonderful confirmation of the discomfort. All makes more sense now.”
Another woman wrote, “WOW good to know cause I do feel so bloated and heavy on the 2nd day.”
But two gynecologists say the models aren’t grounded in science.
Healthline asked Dr. Safrir Neuwirth, an OB-GYN at CentraState Healthcare System, if a woman’s uterus nearly doubles in size monthly during her period.
“The simple answer is no,” Neuwirth responded. “In my 20 years of practice, I’ve never noticed much of a change in the size of the uterus during the period.”
Another OB-GYN, Dr. Kimberly Gecsi, who practices at University Hospitals Cleveland Medical Center, had a similar reaction. “I’ve never heard anything about a uterus increasing in size during a woman’s period,” she said.
“There are certain things that happen physiologically during a woman’s period that do increase the volume of the uterus and make it slightly more swollen,” Neuwirth noted.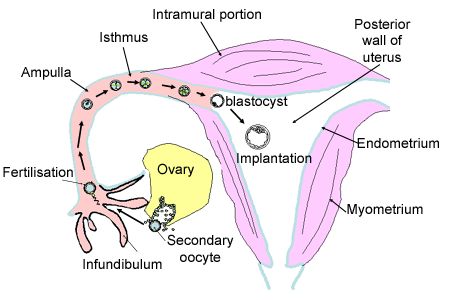 “But does the uterus double in size like this picture? No way.”
“But does the uterus double in size like this picture? No way.”
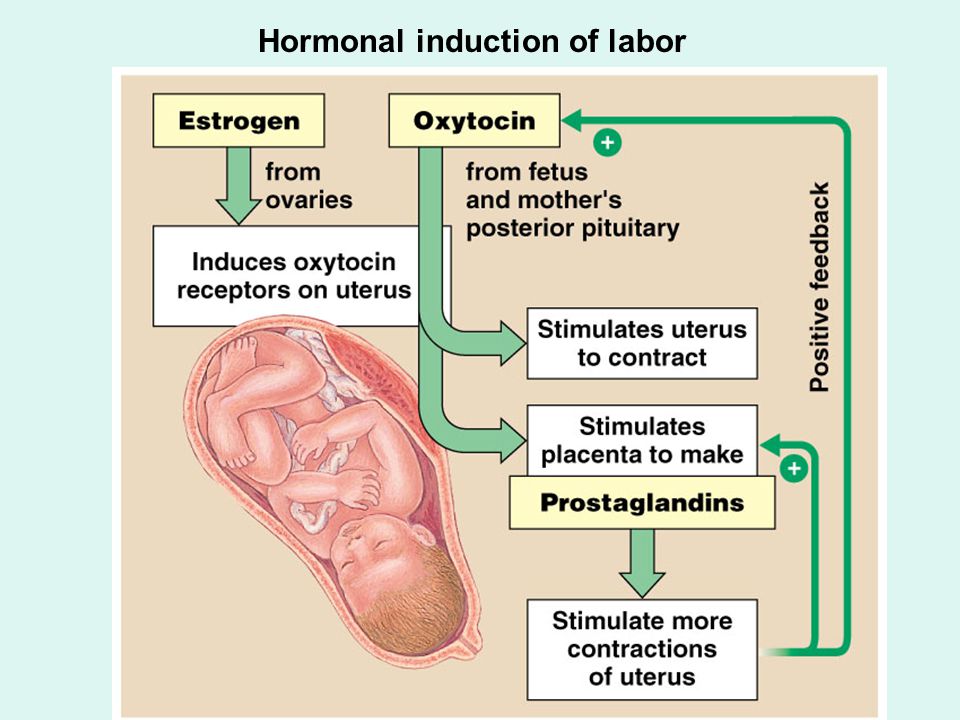
Neuwirth explained that there’s increased blood flow to the uterus during that time of the month, driven by a surge in hormones.
The lining of the uterus, which is what sheds during a period, also thickens by about half a centimeter leading up to the first day of menstruation.
“The combination of the two factors might slightly increase the volume of the uterus by as much as 10 to 15 percent,” Neuwirth told Healthline.
Megan Assaf, a licensed massage therapist and the founder of Wombs for Wisdom, created these uterus models. She said the two sizes are “based on a unique combination of medical science data, medical illustrations, cadaver observation, over a decade of manual palpation of living wombs, and concepts from traditional folk healing.”
Assaf told Healthline that the medical basis she cited comes from a Maya Abdominal Therapy book written by Rosita Arvigo, DN.
According to Assaf, the book states that in a woman who isn’t pregnant, the uterus weighs 4 ounces.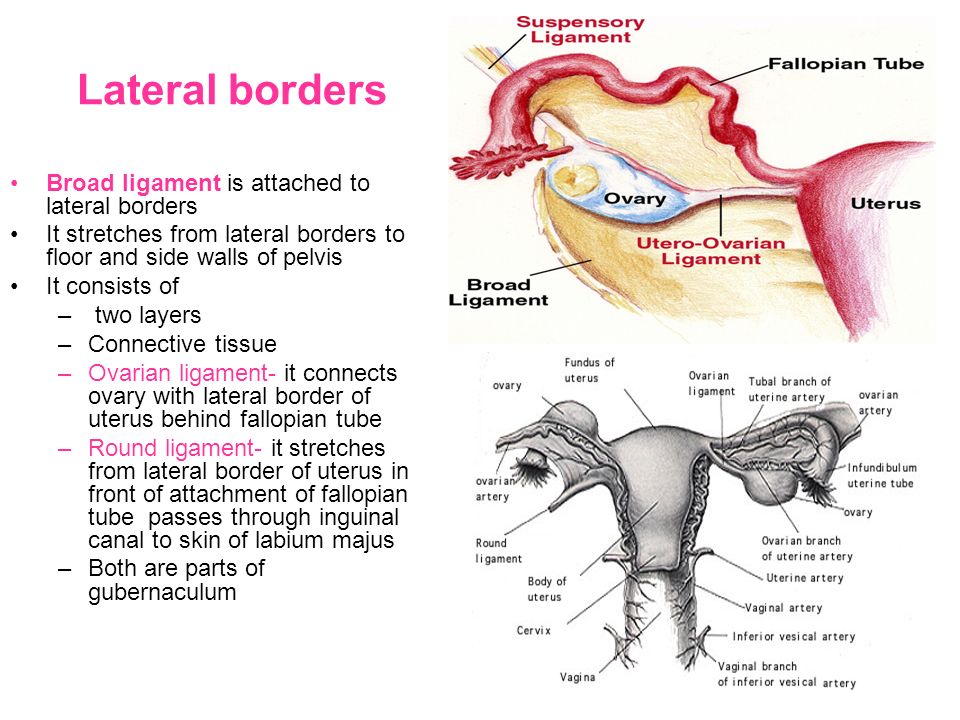 During menstruation, the uterus can weigh as much as 8 ounces.
During menstruation, the uterus can weigh as much as 8 ounces.
However, changes in weight and size aren’t the same thing.
The typical size of a uterus is approximately 7 centimeters long, 5 centimeters wide, and 4 centimeters thick.
But the size varies considerably, emphasized Neuwirth.
“The uterus models in the picture are both totally normal uterine sizes,” Gecsi clarified. “The smaller one looks like a uterus you could see in someone who’s never had children or is postmenopausal, and the other is pretty representative of a uterus in a woman who’s had a few children.”
Neuwirth further explained that having babies increases the size of the uterus, or womb. Most of the time after childbirth, the uterus will remain larger, he said.
There are a few other reasons for the variety in uterus size. About 20 to 80 percent of women will develop uterine fibroids by the time they’re 50. Fibroids are noncancerous growths on the side of the uterus wall. They vary in size and can enlarge the uterus overall.
Genetics are also at play in uterus size.
“It’s important know that if a woman’s uterus is enlarged, it could be a sign of a different problem” and to consult a doctor, Gecsi warned.
She pointed out that since the uterus is set deep into the pelvis, a woman wouldn’t be able to notice the change in size herself.
It’s easy for things to go viral without being fact checked, and these models certainly look compelling.
But the lack of scientific evidence to back up the change in uterine size during menstruation highlights the need to research medical information you read on social media if it’s not from a trusted source.
Since feeling “heavy” during a period is common, the picture of the uterus models resonated with thousands of women.
While women might experience a heavier feeling because of the increased volume of blood in the uterus, Neuwirth said, the main factor behind that full, uncomfortable feeling comes from a combination of bloating, extra water retention, and excess gas.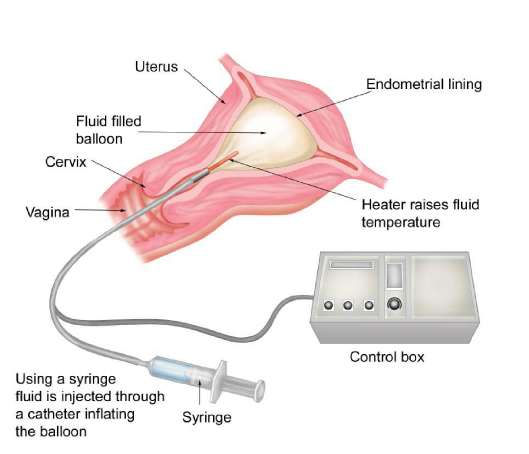
You can blame those symptoms on the plummeting levels of the hormone progesterone during a period — not a ballooning uterus.
Average Uterus Size & How Fibroids Change It
Thursday, May 19th, 2022
Average Uterus SizeIf your doctor has talked to you about having an average uterus size or discussed the concern of an enlarged uterus, you may wonder about the definition of “average.” It may help you better understand your uterus and any health concerns if you realize how this organ is measured and what makes it average.
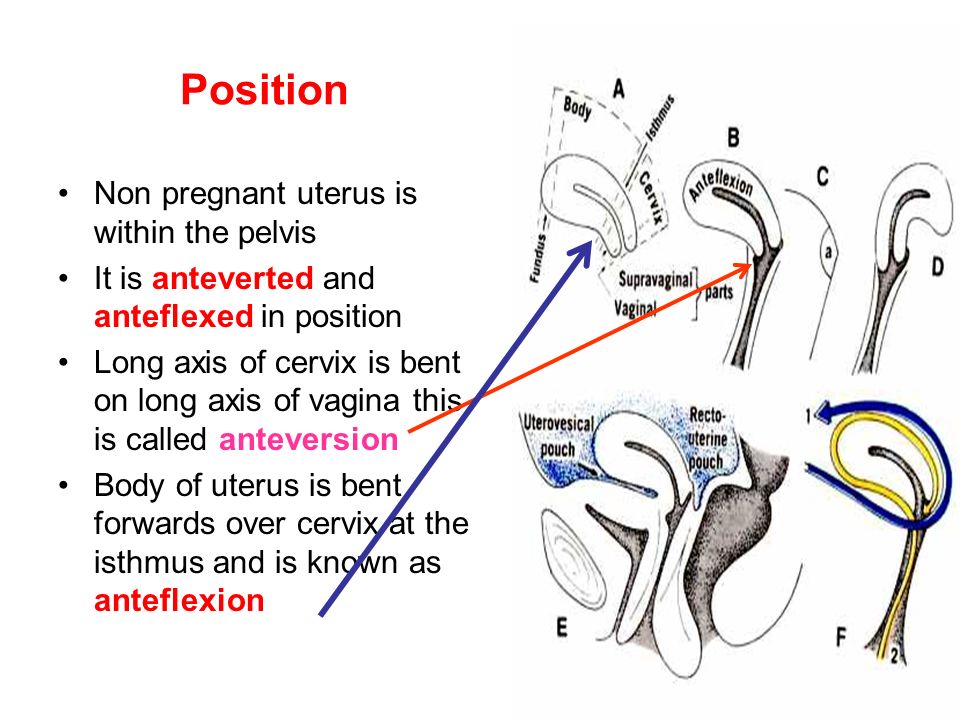
The uterus measurements are found in three ways. First, it is measured by the length, from the fundus of the uterus to the outside opening. The fundus is the part of the uterus farthest from the opening. It may also be measured by the width of the uterus, which is measured across the fundus. The third measurement is the thickness of the uterus.
The uterus grows at puberty when it becomes pear-shaped. At this point, it has reached its full size, but the volume will continue to change during a woman’s reproductive years. It changes throughout the menstrual cycle, ranging from 75 ccs to 200 ccs.
It changes throughout the menstrual cycle, ranging from 75 ccs to 200 ccs.
The normal size of the uterus is about three inches in length and two inches at the widest part. The uterus can expand up to five times its normal size during pregnancy. Compare this change in the uterus as if it were going from a lemon to the size of a watermelon.
If your uterus has changed size and you experience other symptoms of uterine fibroids, you can seek treatment with a fibroid specialist through Uterine Fibroid Embolization (UFE). UFE is a minimally invasive procedure which can help your uterus go back to its original size and shape.
Schedule a consultation
Uterus Size with FibroidsUterine fibroids are benign tumors that can grow inside or on the uterus. The fibroids in your uterus can continue to grow and change the shape and size of the average uterus size. How much the fibroids increase the size of the uterus will depend on how many fibroids are present, where they are located, and how big they grow.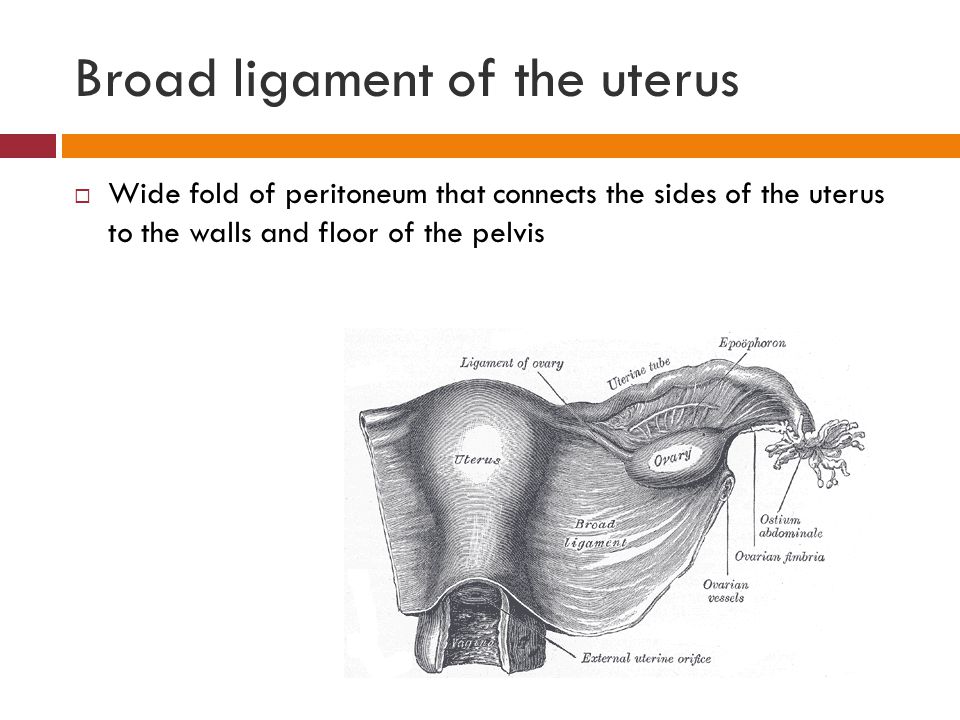
Fibroids can have a wide range of sizes, with the ability to change the average uterus size by causing it to expand. They can start small, about the size of a small seed, and grow to be quite large, tor the size of a grapefruit. Large fibroids are classified as those that range from a grapefruit to a watermelon or more than 10 cm in diameter. Even medium fibroids can be large enough to increase the size of the uterus. These fibroids may range from the size of a plum to an orange.
If you have multiple fibroids, they can cause the average size uterus to expand and make you look like you’re pregnant. They can cause the uterus to expand to the point that it reaches the rib cage. As the fibroids grow, they can cause discomfort. You may be concerned about how they will impact your uterus.
What Do Fibroids Do to Your Uterus?Fibroids can cause the average size of the uterus to change shape and expand as they grow. They can also cause the uterus to press on other organs, such as the bladder, making it difficult to empty the bladder or cause you to feel the need to urinate more often.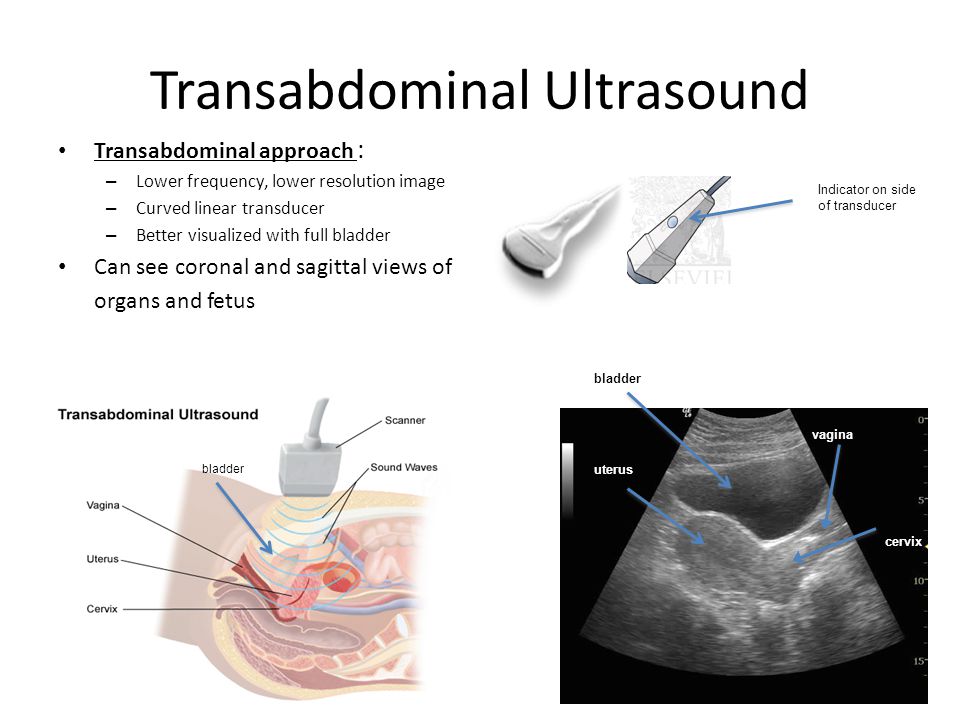
Fibroids often cause heavy bleeding because the pressure makes the endometrial tissue bleed more than normal. They may prevent the uterus from contracting properly to stop menstrual bleeding as expected with a normal period.
Submucosal Fibroids
Submucosal fibroids are one type of uterine fibroid located in the uterus’s inner lining, also known as the endometrium. Submucosal fibroids can grow alone or in a cluster. They often cause heavy menstrual bleeding, which can lead to anemia. They may cause pain in the lower back and fatigue and dizziness, which is often attributed to anemia.
Subserosal Fibroids
Subserosal fibroids are another type of growth which may not change the average uterus size because they are found on the outside of the organ. They can impact nearby organs, such as the bladder. These fibroids can vary in size and location in different areas around the uterus. They may cause abdominal pain, cramping, feeling full or heavy, and frequent urination.
Fibroid symptoms can vary based on size and location in a normal size uterus. They can also be similar to other conditions that affect the reproductive system, so it is important to discuss symptoms with your doctor.
Typical symptoms of fibroids include:
- Heavy menstrual bleeding and longer periods
- Bleeding between periods
- Severe menstrual cramping
- Pain in the pelvis or lower back
- Frequent urination
- Stomach swelling
- Pain during sex
- Anemia
- Bloating and/or constipation
If you experience these symptoms, you should see your doctor. They may diagnose fibroids during a regular pelvic exam or use other tests to reach a diagnosis. They may recommend:
- Ultrasound
- MRI
- Hysterosonography
- Hysteroscopy
These tests can confirm a diagnosis of uterine fibroids.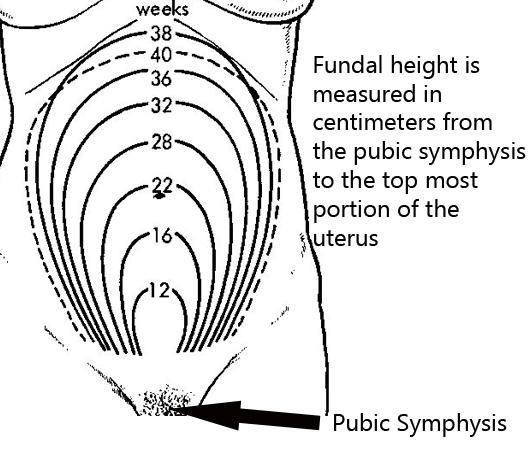
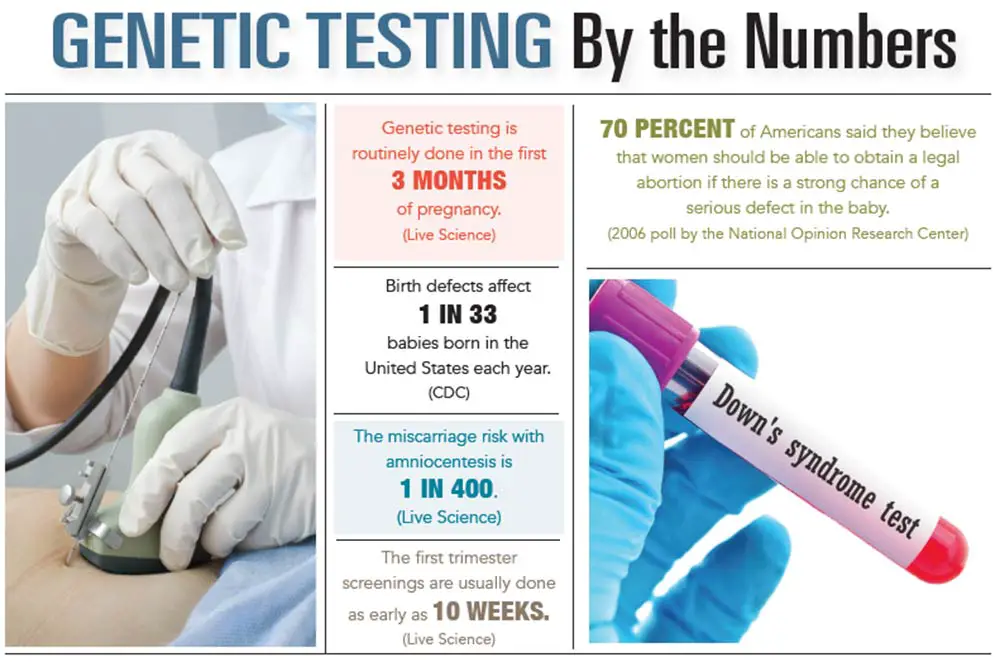
Fibroids can cause complications with pregnancy. They may grow in size during pregnancy because of the increase in progesterone. They can outgrow their blood supply, which may lead to severe pain and hospitalization to monitor the mother and baby’s conditions.
Fibroids can affect the baby’s position in the uterus, increasing the risk of miscarriage. They may also increase the risk for preterm delivery and the need for a cesarean section delivery.
Uterine Fibroid TreatmentUSA Fibroid Centers offers a minimally invasive treatment for uterine fibroids to help reduce their size and accompanying symptoms. UFE treats conditions to reduce or eliminate symptoms while keeping the uterus intact, unlike a hysterectomy.
When UFE is performed, a fibroid specialist will use ultrasound technology to locate the fibroid. They will insert a tiny catheter into the thigh or wrist and inject embolic materials into the artery feeding the fibroid. When the fibroid can no longer receive nutrients, it shrinks and dies.
When the fibroid can no longer receive nutrients, it shrinks and dies.
If you are concerned about fibroids, how they can affect an average size uterus, or the symptoms that negatively impact your life, you can get help with USA Fibroid Centers. Our specialists will work with you to determine the right treatment plan. Schedule a free consultation online or call us at 855.615.2555 to visit one of our facilities.
Our Locations
Related Posts
Uterine fibroids sizes for surgery, small and large fibroids
Many women ask gynecologists about the size of fibroids for surgery in millimeters, centimeters. When can I limit myself to regular visits to the gynecologist and ultrasound, and in what cases should fibroids be removed? Let's figure it out.
Size doesn't matter
Fibroids are one of the most common conditions in gynecology.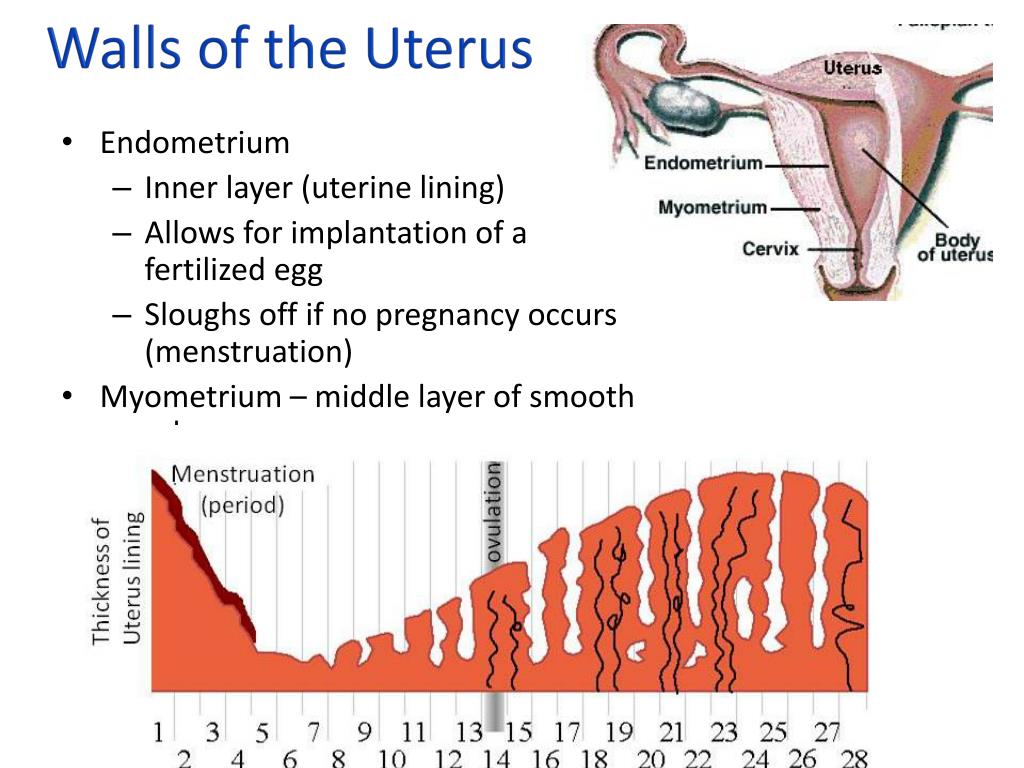 It occurs very often, but it is difficult to calculate exact statistics. In many women, fibroids remain undiagnosed because they do not cause symptoms, the woman does not go to the doctor and does not undergo examination. nine0003
It occurs very often, but it is difficult to calculate exact statistics. In many women, fibroids remain undiagnosed because they do not cause symptoms, the woman does not go to the doctor and does not undergo examination. nine0003
Fibroids vary in size, from barely noticeable on ultrasound to huge. They also behave differently: some grow literally before our eyes, the size of others almost does not change over time.
There is no clear relationship between the size of the fibroids and the symptoms a woman experiences. Sometimes fibroids, which are only 2-3 cm in diameter, lead to severe uterine bleeding and deterioration of health, in other cases, the node has time to grow significantly without causing any problems. nine0003
Previously, gynecologists followed the standard management of patients with fibroids. If a small node was detected, the woman was under observation for some time: she periodically appeared for examinations, underwent an ultrasound scan. When the size of the fibroids increased significantly, the doctor issued a referral for surgical treatment. If the node could not be removed separately, the entire uterus was removed.
If the node could not be removed separately, the entire uterus was removed.
Now approaches have changed. The size of myomatous nodes is no longer such a significant criterion as before. nine0003
What matters?
Current indications for treatment of fibroids are as follows:
- If fibroids cause symptoms. First of all, uterine bleeding. If a large knot compresses neighboring organs, this manifests itself in the form of frequent urination, impaired urine outflow, and constipation. With heavy bleeding, anemia develops.
- If the nodes are growing rapidly. What does "fast" mean? Ultrasound helps to understand this: according to the results of 2–3 ultrasound examinations performed with an interval of 4–6 months, the fibroids should increase by more than 1–2 cm.
- If a woman plans to have a baby, and fibroids can prevent the onset, course of pregnancy.
Fibroids in myomas - discord
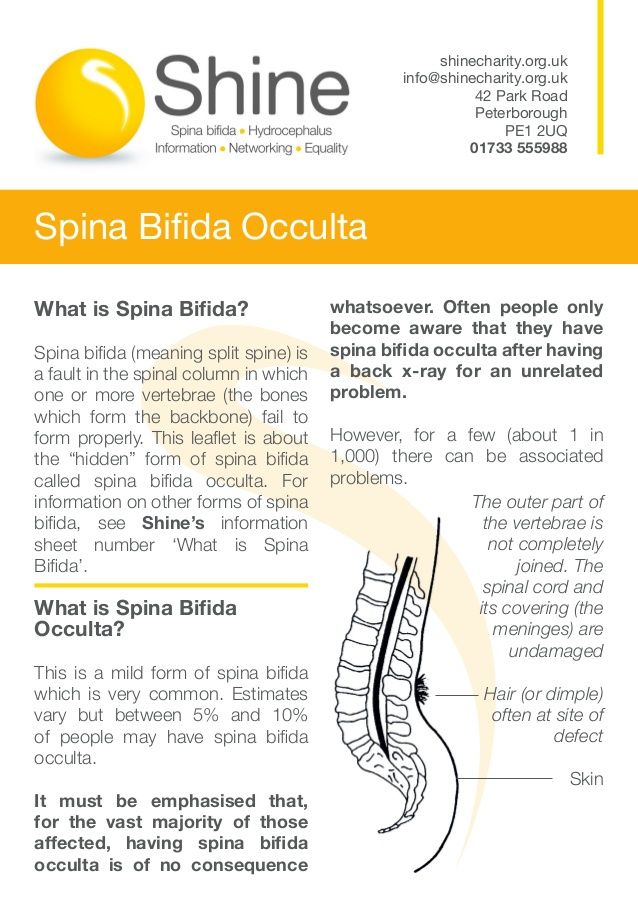
Fibroids in the uterus can occupy a different position, and the symptoms and the need for treatment depend on this. The wall of the uterus consists of three layers: the mucous membrane, the muscular layer and the outer serous membrane. Myoma grows from muscle tissue, it can be located in the thickness of the muscles (intramural), inside the uterus under the mucosa (submucosa), outside under the serous membrane (subserous). nine0003
The wall of the uterus consists of three layers: the mucous membrane, the muscular layer and the outer serous membrane. Myoma grows from muscle tissue, it can be located in the thickness of the muscles (intramural), inside the uterus under the mucosa (submucosa), outside under the serous membrane (subserous). nine0003
In terms of symptoms, submucosal and subserous nodes are the most harmless. They often grow very large and are diagnosed by chance during an ultrasound scan.
Things are different with submucosal fibroids. After all, during menstruation, the mucous membrane of the uterus is rejected, and bleeding develops. The submucosal fibroid stretches it, does not allow it to contract, so the bleeding will be longer and stronger. A submucosal fibroid with a size of more than 4–5 cm protrudes into the uterine cavity, prevents the fertilized egg from attaching, developing the fetus, “robbing” it, pulling the blood flow onto itself. Learn more about the types of fibroids. nine0003
Surgery as a last resort
Myomectomy and hysterectomy were often used by gynecologists in the past. Some still adhere to this approach in the old fashioned way. According to modern concepts, surgical treatment, even with fairly large fibroids, should be considered as a last resort. Among surgeons, there has long been such a popular expression: "the best operation is the one that was avoided." In the case of fibroids, this is especially true, because there has long been an effective minimally invasive treatment method - uterine artery embolization (UAE). nine0003
Some still adhere to this approach in the old fashioned way. According to modern concepts, surgical treatment, even with fairly large fibroids, should be considered as a last resort. Among surgeons, there has long been such a popular expression: "the best operation is the one that was avoided." In the case of fibroids, this is especially true, because there has long been an effective minimally invasive treatment method - uterine artery embolization (UAE). nine0003
Myomectomy should only be performed if a number of conditions are met:
- If there is no chance that the entire uterus will have to be removed when removing the fibroids.
- If the woman is planning a child in the near future. When planning a pregnancy in the long term, myomectomy is not the preferred method of treatment, since the risk of recurrence is high in the next 2-5 years.
- If the operation does not cause much harm to the uterus, if after it the organ does not leave many scars. nine0024
- If the node is more than 4–5 cm, located subserously and has a thin base (leg) - there is a risk of torsion during pregnancy.
In other cases, modern gynecologists try to resort to embolization of the uterine arteries.
Thus, the size of the fibroid undoubtedly plays a role. But, as can be seen from the above, other factors are much more important. Unfortunately, at present, not all gynecologists in Russia are well informed. Some adhere to old approaches, try to treat a woman with outdated ineffective drugs or persuade her to remove the uterus, dissuade her from UAE, scaring her with various serious complications. nine0003
Get a second opinion from a gynecologist experienced in UAE to see if this procedure is right for you.
+7 (495) 734-91-09 (around the clock) Expert advice
Cervical cancer staging
Staging is a way of describing cancer, i.e. determination of its localization, distribution and influence on the functions of other organs of the body. Doctors use diagnostic tests to determine the stage of cancer, so staging cannot be completed until all tests are completed. Knowing the stage helps the doctor determine the most appropriate type of treatment and make a prognosis for recovery. There are different descriptions of stages in different types of cancer. nine0003
Knowing the stage helps the doctor determine the most appropriate type of treatment and make a prognosis for recovery. There are different descriptions of stages in different types of cancer. nine0003
One of the staging tools is the TNM system. This system uses three criteria to evaluate the stage of a cancer: the tumor itself, nearby lymph nodes, and whether the tumor has spread to other parts of the body. The results are combined to determine the stage of the cancer. There are five stages: stage 0 (stage zero) and stages I-IV. Staging provides a common way to describe cancer and doctors to work together to better plan treatment.
TNM is an abbreviation for T(tumor), N(node), and M(metastasis). Doctors consider these three factors to determine the stage of cancer:
- How big is the primary tumor and where is it located? (Tumor, T)
- Has the tumor spread to the lymph nodes? (Knot, N)
- Is there cancer metastasis in other parts of the body? (Metastases, M)
Tumor.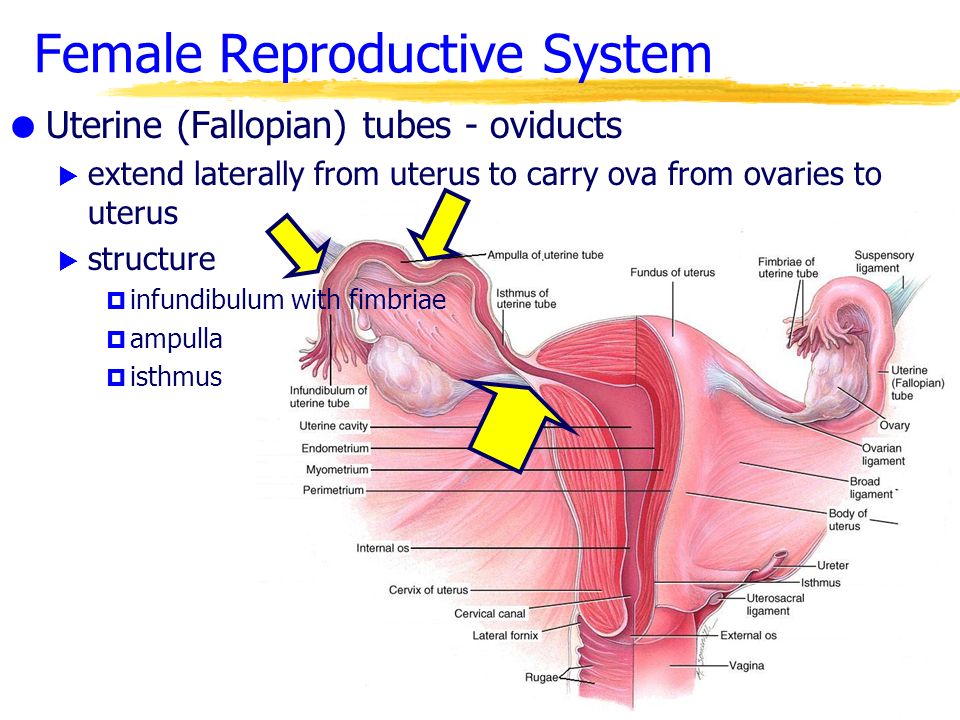 In the TNM system, “T” plus a letter or number (from 1 to 4) is used to describe the size and location of the tumor. Some stages are divided into smaller groups for a more detailed description of the tumor
In the TNM system, “T” plus a letter or number (from 1 to 4) is used to describe the size and location of the tumor. Some stages are divided into smaller groups for a more detailed description of the tumor
TX: Primary tumor cannot be assessed due to lack of information. Additional tests may be required. nine0003
Tis: This stage is called cancer in situ and means that the cancer is found only in the layer of cells lining the cervix and has not spread deeper into the cervix.
T1/FIGO I: Carcinoma found only in the cervix.
T1a/FIGO IA: Invasive cancer was only detected under a microscope. Note: Any tumor found macroscopically (i.e. large enough to be detected visually or by hand examination) is classified as T1b or FIGO IB. nine0003
T1a1/FIGO IA1: Cancer area 3.0 mm or less deep and 7.0 mm or less horizontal.
T1a2/FIGO IA2: Cancer area greater than 3.0 mm but not greater than 5.0 mm and its horizontal extension 7.0 mm or less.
T1b/FIGO IB: At this stage, the doctor may see a pathological change, and the cancer is found only in the cervix, or there is a microscopic pathological change (which can be seen under a microscope) that is larger than the T1a2/FIGO IA2 tumor.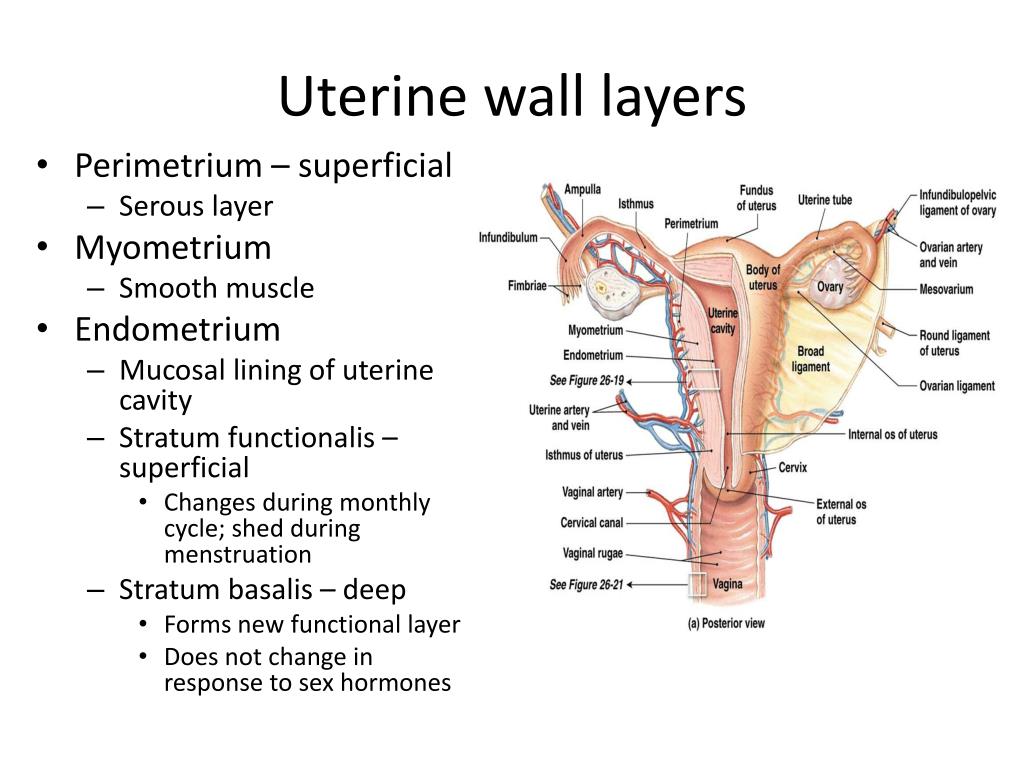 Cancer may have been detected by physical examination, laparoscopy, or other means. nine0003
Cancer may have been detected by physical examination, laparoscopy, or other means. nine0003
T1b1/FIGO IB1: Tumor - 4 cm or less.
T1b2/FIGO IB2: tumor larger than 4 cm.
T2/FIGO II: Cervical cancer has spread beyond the uterus but not to the pelvic wall or the lower third of the vagina.
T2a/FIGO IIA: The tumor has not spread to adjacent tissues of the cervix.
T2b/FIGO IIB: Tumor has spread to tissue adjacent to the cervix.
T3/FIGO III: The tumor reaches the pelvic wall and/or the lower third of the vagina and/or causes hydronephrosis, kidney failure, or ureteral obstruction. nine0003
T3a/FIGO IIIA: The tumor has spread to the lower third of the vagina but has not grown into the pelvic wall.
T3b/FIGO IIIB: The tumor has grown into the pelvic wall and/or is causing hydronephrosis or kidney damage.
T4/FIGO IVA: The tumor has spread to the lining of the bladder or rectum and has spread beyond the pelvis.
Assembly. The “N” in the TNM system stands for lymph nodes, small bean-shaped organs that help fight infection. Lymph nodes near the cancerous area are called regional. Lymph nodes in other parts of the body are called distant. nine0003
The “N” in the TNM system stands for lymph nodes, small bean-shaped organs that help fight infection. Lymph nodes near the cancerous area are called regional. Lymph nodes in other parts of the body are called distant. nine0003
NX: Regional lymph nodes could not be identified.
N0 (N plus zero): No metastases in regional lymph nodes.
N1: The tumor has invaded one or more regional lymph nodes.
Distant metastases. The "M" in the TNM system indicates whether the cancer has spread to other parts of the body.
MX: Distant metastases cannot be identified.
M0(M plus zero): No distant metastases.
M1: Distant metastases exist. nine0003
Cancer staging grouping
Doctors determine the stage of cancer by combining T, N, and M values.
Stage 0: Cancer is defined as in situ, i. cancer is found only in the first layer of cells inside the cervix, not in deeper tissues (Tis, N0, M0). Cancer in situ is not considered invasive cancer.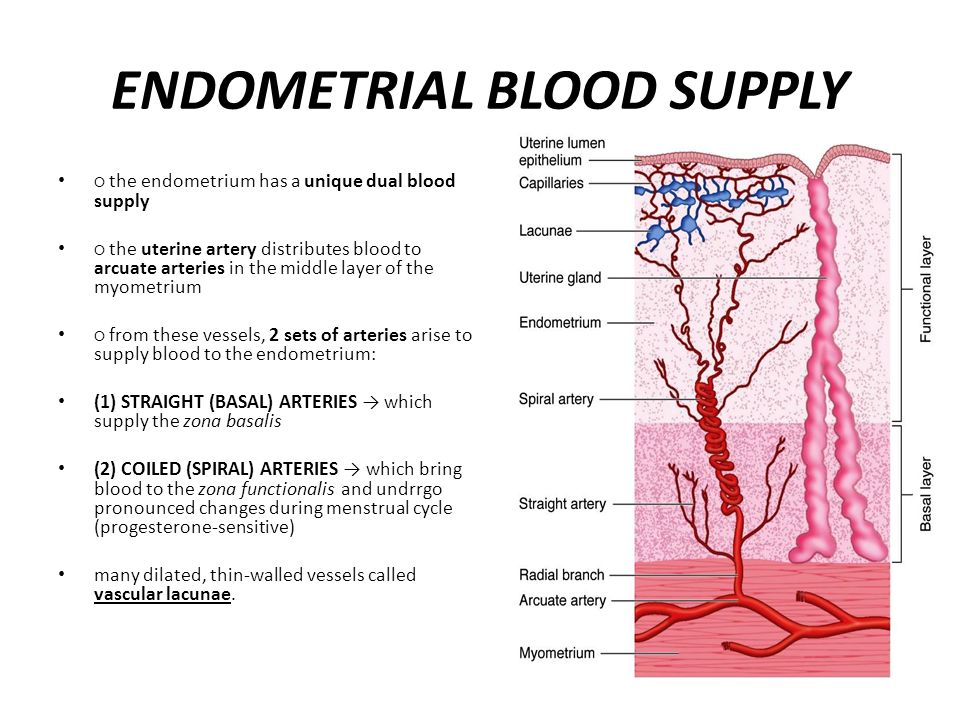
Stage I: Cancer has spread from the lining of the cervix to deeper tissues but is only found in the uterus. It has not penetrated the lymph nodes or other parts of the body (T1, N0, M0). This stage can be described in more detail. nine0003
Stage Ia: T1a, N0, M0
Stage Ia1: T1a1, N0, M0
Stage Ia2: T1a2, N0, M0
Stage Ib: T1b, N0, M0
Stage Ib2: T1b2, N0, M0
Stage II: The cancer has spread beyond the cervix to nearby areas such as the vagina or tissues near the cervix, but is still in the pelvis. It has not penetrated the lymph nodes or other parts of the body (T2, N0, M0). This stage can be described in more detail.
Stage IIa: T2a, N0, M0
Stage IIb: T2b, N0, M0
Stage III: The cancer has spread beyond the cervix and vagina, but has not spread to the lymph nodes or other parts of the body (T3, N0, M0).
Stage IIIa: Cancer has spread to the lower vagina but is absent elsewhere in the body (T3a, N0, M0) T3a; N1, M0).