Post natal physiotherapy
Physiotherapy advice after pregnancy | Pregnancy Birth and Baby
Physiotherapy advice after pregnancy | Pregnancy Birth and Baby beginning of content6-minute read
Listen
Key facts
- Pregnancy and birth can affect your body in many ways, causing muscles stretch, and ligaments soften, especially those in your abdomen and your pelvic floor.
- Being pregnant and having a baby increase your chance of bladder and bowel problems (incontinence).
- It's important to do exercises to strengthen your pelvic floor and abdominal muscles while you are pregnant, but if you've already had your baby, it's not too late to start.
- These exercises can help reduce your chance of injury and other problems in the future.
- Continence and women's health or pelvic floor physiotherapists can assess your pelvic floor function, and design an exercise program that meets your needs.
How does pregnancy and childbirth affect my body?
When you are pregnant, your body changes in many ways. Your muscles stretch, and ligaments soften, especially those in your abdomen and your pelvic floor. Pelvic floor weakness can start during pregnancy and may continue after birth. If you've had multiple births, assisted births (with forceps), tearing, or babies over 4kg you are at greater risk of injury.
Will having a baby cause incontinence?
If you’ve had a baby, then you have around 1 in 3 chance of bladder and bowel problems (incontinence).
If you had bladder or bowel symptoms, such as irritable bowel syndrome or an overactive bladder before you were pregnant, you are more likely to have this problem worsen after pregnancy.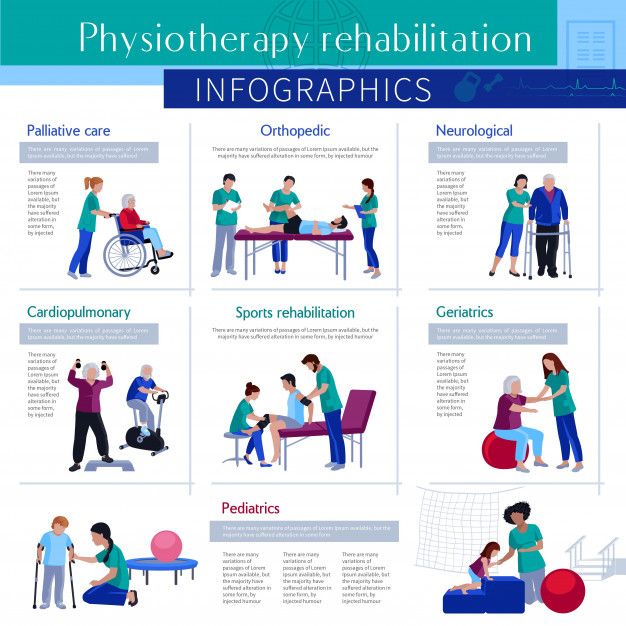
You are also more likely to have incontinence after pregnancy if:
- your baby is large
- your labour was long (especially the second (pushing) stage)
- you had a difficult vaginal delivery or needed stitches
You may also experience incontinence if you’ve had an easy birth.
Incontinence after pregnancy will often improve in the first 6 months, as the pelvic floor muscles and nerves recover. Regular pelvic floor muscle exercises before, during and after pregnancy will help.
How can I strengthen my pelvic floor to avoid incontinence?
It is important to do exercises to strengthen your pelvic floor and abdominal muscles while you are pregnant, but if you’ve already had your baby, it’s not too late to start.
If you've had a vaginal birth, you only need to wait 2 days to begin pelvic floor exercises. If you had a caesarean birth, it's best to wait 5 days. If you feel any pain, stop doing the exercises and see a physiotherapist or your midwife for advice.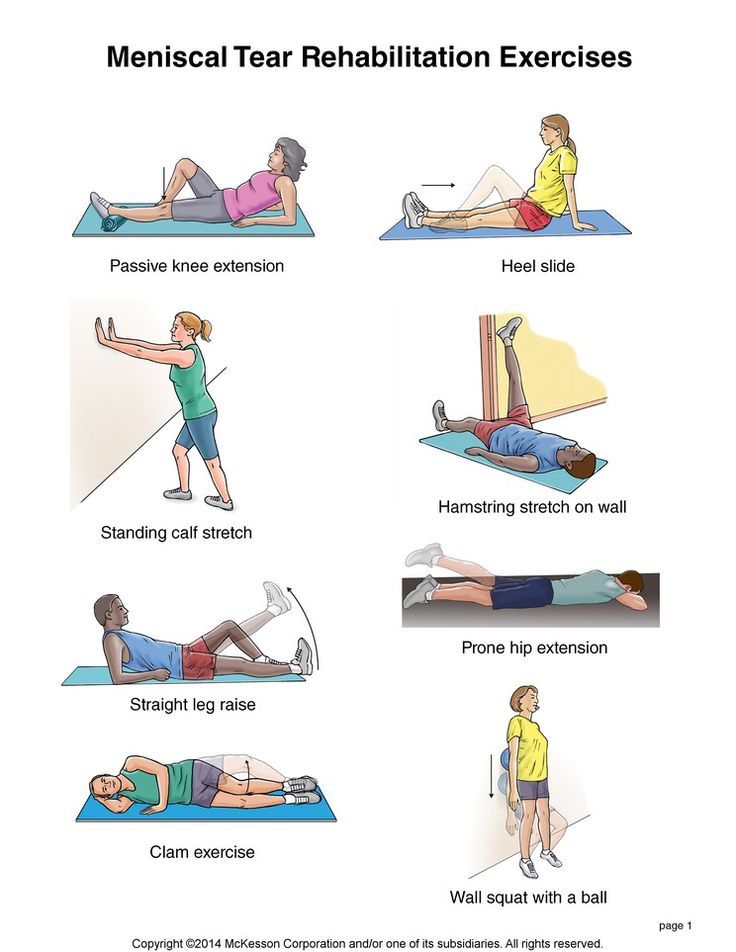
To exercise your pelvic floor muscles:
- squeeze the muscles all around your front and back passages
- lift them up and inwards, as if you are trying to stop urine (wee) from escaping
- relax for about 5 seconds
- repeat up to 10 times
You can do these exercises several times each day, wherever you are. Practicing this routine daily will improve the strength and endurance of your pelvic floor muscles.
Pelvic floor exercises are most effective when individually tailored and monitored. Continence and women's health or pelvic floor physiotherapists can assess your pelvic floor function, and design an exercise program to meet your needs.
Pregnancy, Birth and Baby's service directory can help you find women's health or pelvic floor physiotherapists, or call the National Continence Helpline on 1800 33 00 66. Your GP may also be able to refer you to a pelvic floor physiotherapist.
How can I strengthen my abdominal muscles?
Doing abdominal exercises every day after you give birth can help you regain your strength and help with back and stomach support. Don't do sit-ups for at least 12 weeks after giving birth. Instead, it's best to do pelvic tilts and abdominal bracing exercises.
Don't do sit-ups for at least 12 weeks after giving birth. Instead, it's best to do pelvic tilts and abdominal bracing exercises.
To perform pelvic tilts:
- lie, stand or sit with your knees bent and your feet flat
- gently flatten the curve of your lower back by tilting your pelvis backwards
- hold for 3 to 5 seconds
- repeat 5 to 10 times
To perform abdominal bracing:
- lie, sit or stand
- gently draw your belly button in towards your spine
- hold for 5 to 10 seconds
- repeat 5 to 10 times
How can I care for my back?
It's important to look after your back to help prevent backache and injury. New parents are at risk of back injury because they are lifting and bending more than usual.
You can help look after your back by:
- keeping good posture and bend your knees
- working at benches or tables at waist height
- using chairs with good back support
- not lifting anything heavier than your baby for the first 6 weeks
How do I establish healthy habits?
Regular exercises can help you strengthen your muscles, to help you look after your body during pregnancy, and to recover after childbirth.
Many hospitals offer postnatal physiotherapy classes, where you can learn the best exercises to do under professional guidance.
Some important habits include:
- exercise — walk every day, and do daily pelvic floor and abdominal exercises
- good bladder habits — drink plenty of fluids and only urinate when your bladder feels full (don't go 'just in case')
- good bowel habits — avoid constipation and straining by eating plenty of high fibre foods, such as wholegrains, fruit and vegetables
Sources:
Queensland Health (How to find and exercise your pelvic floor muscles (men and women)), Continence Foundation of Australia (Pregnancy and childbirth), Continence Foundation of Australia (Pelvic Floor Health for Expectant and New Mums 2022), Western Australia North Metropolitan Health Service (Physio after childbirth - Booklet), NSW Health (Having a baby), The Royal Women's Hospital (Exercise)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: June 2022
Back To Top
Related pages
- Pelvic pain in pregnancy
- Abdominal separation (diastasis recti)
- Backache in pregnancy
- Pelvic floor exercises
- Birth injury (to the mother)
- Safe return to exercise after pregnancy
- Bladder weakness after birth
Need more information?
Looking after your body after having a baby
Over the last 9 months, your body has had to change to accommodate your growing baby and preparing to give birth.
Read more on Pregnancy, Birth & Baby website
Pelvic floor exercises & care: in pictures | Raising Children Network
Your pelvic floor holds your bladder, bowel and uterus in place, but pregnancy and birth can weaken it. Do pelvic floor exercises: squeeze, lift and hold.
Do pelvic floor exercises: squeeze, lift and hold.
Read more on raisingchildren.net.au website
Pelvic floor exercises
Pelvic floor exercises help to strengthen the muscles of the pelvic floor which come under great strain in pregnancy and childbirth.
Read more on Pregnancy, Birth & Baby website
Bladder weakness after birth
Leaking urine after childbirth is very common. It can be embarrassing and inconvenient, but there are ways to improve bladder weakness.
Read more on Pregnancy, Birth & Baby website
Losing weight after birth safely
Tips for losing weight after birth, including how to enjoy a healthy lifestyle, setting realistic goals, breastfeeding and weight loss and when to seek help.
Read more on Pregnancy, Birth & Baby website
Safe return to exercise after pregnancy
Exercise can help you recover after childbirth, make you stronger and improve mood. Here are some tips on how to exercise safely after a pregnancy.
Read more on Pregnancy, Birth & Baby website
Anatomy of pregnancy and birth - perineum and pelvic floor
The perineum – the skin between the vagina and anus - stretches during childbirth and can sometimes tear. Learn here how to prepare the perineum for the birth.
Read more on Pregnancy, Birth & Baby website
Exercising during pregnancy
Doing regular moderate physical activity has health benefits during pregnancy and also helps to prepare the body for childbirth. Read about getting fit during pregnancy.
Read about getting fit during pregnancy.
Read more on Pregnancy, Birth & Baby website
Postnatal exercise - sample workout - Better Health Channel
Make sure your abdominal muscles have healed before you do any vigorous tummy exercises, such as crunches.
Read more on Better Health Channel website
Frequent urination during pregnancy
Having to urinate more often during pregnancy is very common. Find out why it happens and how you can reduce it.
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Five reasons to see a physiotherapist after giving birth
By Taryn Watson, FitRight Physio
The early weeks and months after giving birth are a blur. Sleep deprivation, adjusting to new challenges, learning new skills – as beautiful and awesome as this time is, it’s an accomplishment just to make it through each day.Which is why it’s a big ask to advise a new mother at 6 weeks postpartum to not only get to appointments with the paediatrician, the obstetrician or midwife, the GP for immunisations and the Child Health Nurse, but to also see a specialist Women’s Health Physiotherapist as well. Surely attending all of these other appointments are adequate to get the all clear to return to exercise?
Surely attending all of these other appointments are adequate to get the all clear to return to exercise?
In reality, the vast majority of what goes on in these appointments is actually centred around the health and well being of your newborn baby. In general (and I’m sure there are exceptions to this), the only check ups that are involved in this for the mother are:
- A screening test for Postnatal Depression
- A conversation about birth control and family planning
- A check of the healing stitches (either perineal/vaginal or from a Caesarean section) if there are concerns
- A pap smear if it’s due
Again, there may be exceptions to the rule, but I haven’t come across anyone who has had their pelvic floor muscles assessed at this check up, or had a plan put in place for gradual, individualised return to exercise.
And that’s to be expected – these musculoskeletal assessments and exercise prescriptions are not the domain of obstetricians, midwives and GP’s. Their specialities are delivering babies and ensuring that mother and baby are medically well. These are instead the domain of physiotherapists who have done post-graduate training to specialise in Women’s Health and Continence.
Their specialities are delivering babies and ensuring that mother and baby are medically well. These are instead the domain of physiotherapists who have done post-graduate training to specialise in Women’s Health and Continence.
So, why should you prioritise this extra check up at this already-hectic time? Here are five things that a specialist physiotherapist can help you with at a postnatal check:
1. Pelvic floor muscle assessment
The pelvic floor muscles are the muscles that form a sling at the bottom of the pelvis, and they are responsible for keeping our bladder and bowel from leaking, holding in our pelvic organs, supporting our lower back and pelvis, and maintaining optimal sexual function. Pretty important roles, it’s not a muscle group you want to neglect!
If you’ve had a vaginal birth, the pelvic floor muscles have had to stretch up to four times their normal length to allow the baby to be born. The muscles may have torn or been cut, but even if they are intact, they have still undergone the equivalent of a significant sporting injury and need adequate rest and rehabilitation.
If you’ve had a caesarean birth – I’m sorry to say you’re not completely in the clear! Research has shown that long term, it’s the pregnancy that is the main risk factor for pelvic floor muscle dysfunction, due to the weight of the growing uterus directly down on the muscles and the hormonal changes that occur.
At a postnatal assessment, the physiotherapist will assess your pelvic floor muscles. This may be off-putting to some people – but it doesn’t necessarily have to be done via a vaginal examination. A screening test can be done with an ultrasound through your lower tummy, which shows the physiotherapist how well you can elevate and relax those muscles – and you, the patient, can see this on the screen too, which is great for feedback and learning.
A vaginal examination, however, is the gold standard and a lot more information can be gained such as pelvic floor muscle strength, tone and the presence of pain or a vaginal prolapse. This more thorough examination is even more highly recommended if you wish to return to impact exercise or weight training, or have any symptoms of pelvic floor dysfunction, such as:
- Bladder or bowel incontinence
- A feeling of vaginal heaviness
- Any pain in the vaginal area.

2. Abdominal muscle assessment
The presence of a Rectus Abdominis Diastasis (RAD) will be determined, which means whether or not your ‘six-pack muscles’ and the connective tissue in the midline, has returned to normal after being stretched in pregnancy.
This stretching of the two muscle bellies apart from each other is completely normal if you carry a baby to full term, so if this was assessed immediately after delivery, we would expect the muscles to still be sitting apart from each other and be quite weak in the midline.
For most women, it should be enough in these early weeks to encourage optimal healing with relative rest and avoiding activities that cause repetitive increases in abdominal pressure, such as:
- Sit ups
- Heavy lifting
- Chronic coughing and sneezing
- Straining to open your bowels.
But did you know that research has shown that natural healing only occurs in the first 8 weeks? If the tissue in the midline isn’t back to being thick and strong by that stage, you will need to do specific exercises to rectify it.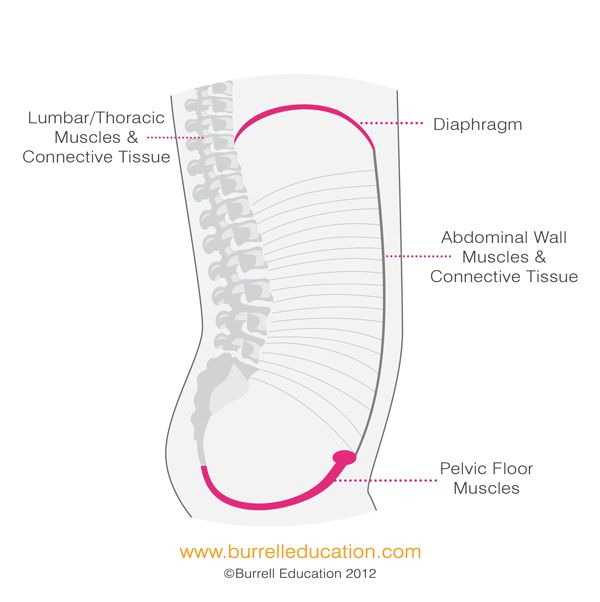 The physiotherapist can put a program in place for you at this appointment if you need it.
The physiotherapist can put a program in place for you at this appointment if you need it.
3. Musculoskeletal assessment
The physiotherapist will ask you about any current or past pain or injury to any joints or muscles. The most common complaints in these early weeks are:
- Pelvic girdle pain (pain in the pubic bone or buttock region)
- Back pain
- Wrist pain
Early diagnosis and management of these issues is essential to stop them becoming chronic problems.
4. Bladder and bowel function screening
Many women experience bladder or bowel dysfunction during and in the early weeks after pregnancy. The physiotherapist will ask you questions about:
- How much you’re drinking
- How often you’re opening your bladder and bowels
- Whether you feel an urgent need to get to the toilet
- Whether you have a history of pain with intercourse
- Whether you experience any urinary or faecal leakage
And a whole lot more questions that will make you question why any of us specialised in this area! Honestly – we are so immune to the fact that we talk about wee and poo and sex all day!
These may be embarrassing issues to discuss, but it’s so important that someone asks these questions and probes into whether there are any early signs of dysfunction. Prevention is better than cure, and if we can pick up anything at this stage that isn’t quite right, we can help you to put in place a plan to optimise it again before it becomes a bigger issue.
Prevention is better than cure, and if we can pick up anything at this stage that isn’t quite right, we can help you to put in place a plan to optimise it again before it becomes a bigger issue.
5. Return to exercise plan and goal setting
Everyone has different postpartum goals regarding return to exercise and activity. One woman might want to run a half marathon in four months time, another woman may wish to be pain free when caring for her newborn baby and two toddlers.
Whatever your goals are, it is important to discuss them with a specialist physiotherapist and work out how achievable they are, and what needs to happen to safely achieve those goals.
We want nothing more than to help all women live active lives. But postnatal rehabilitation needs to be viewed like building a house – the foundations need to be strong before you start building the walls and roof on top otherwise you will always have issues down the track. This assessment will test where you’re at with your core strength and your ability to transfer load effectively when you do abdominal muscle exercises, high impact exercises, loaded weights exercises etc – whatever it is that you individually want to achieve.
In this way, it is a very individual approach to postnatal exercise – there is no ‘recipe’ that you should be able to achieve a certain level of activity at a certain number of months postnatal. We can never assume that one woman’s muscle activation, hormonal changes, and birth trauma are the same as the next woman.
So, the take home message is that although there are many common issues that affect women in the short and long term after childbirth – incontinence, vaginal prolapse, back pain etc – there are things that can be put in place to help to prevent and treat these issues. You don’t need wait for problems to occur or to worsen, you can be proactive by seeing a specialist Women’s Health & Continence Physiotherapist in the early months after delivery.
Find out more about FitRight Physio at www.fitright.physio
Postpartum rehabilitation
Recovery after childbirth is a certain period in a woman's life, it has its own characteristics and remains in memory, as a rule, not the best memory. However, recovery after childbirth can be easier and faster if you know what to expect during this period and how to properly overcome the problems that may arise. Of course, during the 9 months of pregnancy, the body undergoes significant changes, and you should not expect them to disappear immediately after childbirth. nine0003
However, recovery after childbirth can be easier and faster if you know what to expect during this period and how to properly overcome the problems that may arise. Of course, during the 9 months of pregnancy, the body undergoes significant changes, and you should not expect them to disappear immediately after childbirth. nine0003
It is important to remember that recovery is a gradual process, a countdown to how the body was before pregnancy. The entire recovery process can be conditionally divided into the following stages:
1. The first 2 hours after childbirth
bleeding, increased pressure or body temperature. At this stage, a mandatory examination of the uterus with massage, if necessary, is carried out. After some procedures, which are carried out under the supervision of a doctor, bed rest occurs - about 6-8 hours after childbirth. nine0003
During this period, symptoms such as fever due to dehydration, chills, thirst, severe fatigue from prolonged labor, and pain at the suture site and numbness in this area are possible during this period.
2. The first days after childbirth
Doctors' attention gradually weakens, and the young mother remains left to herself. However, if her well-being improves, then the view in the mirror gives little pleasure. Due to childbirth, significant changes in appearance can occur: red eyes due to burst blood vessels and brown dots on the face that look like moles are far from the most unpleasant of them. nine0003
After childbirth, there may be muscle pain in the body, cramping pain in the abdomen, which will increase during breastfeeding. The latter occurs due to postpartum contraction of the uterus. Of course, there are pains in the perineum, which can be both associated with tears, and regardless of them. A bursting pain occurs in the chest area, but milk appears only for 2-3 days, and in the first days colostrum is released - a thick yellowish liquid. All these are normal phenomena that occur in every woman and can be both serious and completely imperceptible, depending on the individual characteristics of the organism. nine0003
nine0003
During this period, active healing takes place, so many restrictions are possible - for example, it is forbidden to sit because of the risk of rupture of the stitches, as well as regular examinations for 7-10 days by nurses to monitor the recovery process after childbirth at each stage.
Cesarean section complicates this period by the fact that the first day after the operation it is allowed to drink only water with lemon juice. However, on the second day after cesarean, they are already transferred to the postpartum department, where the young mother can immediately begin to lead a relatively active lifestyle, including feeding the baby. nine0003
3. The first weeks after childbirth
The first weeks after childbirth, the woman still feels pain: for example, chest pain, especially during feeding. Discharges also continue - they can last from two to six weeks. Episiotomy sutures should be closely monitored, especially when showering.
After a caesarean section, a nurse cleans the stitches daily with antiseptics. The skin scar is formed only a week after the operation, it is then that it becomes possible to calmly take a shower without disturbing the seam. In the absence of complications, discharge occurs on the 7-10th day after childbirth, but for some time after this, the woman is advised to refrain from tilting due to the scar. nine0003
The skin scar is formed only a week after the operation, it is then that it becomes possible to calmly take a shower without disturbing the seam. In the absence of complications, discharge occurs on the 7-10th day after childbirth, but for some time after this, the woman is advised to refrain from tilting due to the scar. nine0003
Compared to physical discomfort, psychological discomfort can become much stronger. This is a purely individual process, it does not manifest itself in everyone and depends on many factors. However, during recovery after childbirth, postpartum depression becomes quite common.
The main thing to remember from the beginning is that this is normal. A woman has an even greater responsibility after childbirth than during pregnancy. Childbirth depletes her body, and after them, increased production of hormones begins, which in total leads to a period of mental instability. After high spirits in the first week of pregnancy, apathy, fatigue and disappointment often come about the absence of the same strong emotions in relation to the child. This is the result of the stabilization of the hormonal background, which is why young mothers are advised to walk more, relax, concentrate only on positive emotions and support the body recovering after childbirth with natural products. nine0003
This is the result of the stabilization of the hormonal background, which is why young mothers are advised to walk more, relax, concentrate only on positive emotions and support the body recovering after childbirth with natural products. nine0003
Physiotherapy in gynecology
Physiotherapy is an important method in the fight against diseases of the female reproductive system. Most often, this branch of medicine is used to treat acute and chronic pathologies. However, physiotherapy is effective in preparation for surgical procedures or in the postoperative period, during pregnancy, and also after childbirth.
Indications
- cracked nipples;
- lactational mastitis;
- vulvitis; nine0046
- vaginitis;
- vulvovaginitis;
- bartholinitis;
- colpitis;
- cervical erosion;
- inflammatory diseases of the uterus, appendages, as well as the pelvic peritoneum and cellular tissue in the acute and chronic stages;
- functional ovarian cysts in remission;
- dysfunctional uterine bleeding;
- weakness of labor activity; nine0045 menstrual disorders not accompanied by bleeding;
- endocrine syndromes in gynecology;
- painful menstruation;
- recovery after gynecological operations;
- recovery from abortion, treatment of miscarriage;
- preparation for IVF.

Physiotherapy can reduce the duration of treatment of diseases, helps in cases where other methods of treatment are ineffective (for example, during the onset of chronic pelvic pain in adhesive disease), reduces the rehabilitation period after surgical interventions, and is also used in the prevention of complications and relapses. nine0003
Aims of physiotherapy
Treatment with natural factors has the following effects:
- pain relief;
- improvement of blood circulation and lymph circulation;
- restoration of hormonal levels;
- restoration of organ function;
- resorption and prevention of adhesion formation;
- improvement of trophism and metabolic processes in tissues;
- stimulation of cellular immunity, processes of repair and tissue regeneration. nine0046
Contraindications to physiotherapy
Contraindications to physiotherapy procedures are:
- cysts;
- endometriosis;
- malignant, benign formations;
- bleeding;
- fever;
- serious condition of the patient;
- cachexia;
- mental illness in the acute stage; nine0045 period of menstruation;
- acute renal and hepatic insufficiency;
- purulent pathologies;
- genital tuberculosis;
- urolithiasis.

Physiotherapy during pregnancy
The use of physical factors during childbearing is justified and safe.
Physiotherapy is prescribed for toxicosis, uterine hypertonicity, weakness of labor activity. Exposure to physical factors makes it possible to refuse the appointment of pharmacological drugs or significantly reduce their dosage, as well as avoid the development of side effects of drugs. nine0003
In the postpartum period, physiotherapy is also important, since very often the development of lactation is accompanied by the appearance of mastitis. In addition, physiotherapy is indicated in the recovery period after caesarean section, to stimulate the healing of sutures after episiotomy and ruptures.
Applied factors
The appointment of physiotherapeutic procedures should correspond to the existing deviations and be carried out according to the therapeutic effects of physical factors and their mechanisms of action. nine0003
In the postoperative period, magnetotherapy is actively and successfully used.
For pain relief, removal of vascular spasm, electro-ultrasound therapy is prescribed.
Ultrasound therapy is used to stimulate the hormonal function of the ovaries. For resorption and softening of adhesions, ultrasound and electrophoresis with enzyme preparations are used.
In inflammatory pathologies with bacteriostatic and bactericidal function, ultraviolet irradiation is prescribed. nine0003
Infrared irradiation has a deep warming effect and is used for low-grade inflammatory diseases.
Electric, magnetic and ultrasound therapy is used to improve blood circulation.
Laser therapy has a pronounced reparative and regenerative effect, stimulates cellular immunity, but is not used during pregnancy.
Electric or magnetic fields are prescribed for anti-inflammatory and decongestant purposes. nine0003
Natural factors in the form of mineral waters and mud are used in the treatment of many gynecological pathologies, since the mineral composition and biologically active substances have a powerful beneficial effect on the entire body.
Thermal procedures in the form of paraffin and ozokerite therapy allow you to cope with pain, as well as stimulate the hormonal function of the ovaries.
Treatment sessions are carried out both transcutaneously, that is, through the skin, and in the abdominal way. nine0003
Through the skin, the procedure is carried out by influencing the abdomen, lower back, inner thighs, perineum. The cavity technique is performed transvaginally or transrectally. Sessions are scheduled from 5-7 days of the menstrual cycle, which is associated with ovulation.
Massage is used to improve blood circulation, normalize muscle tone. During pregnancy, due to the increasing load on the spine, women are often worried about pain in the cervical region and back. In this situation, it is possible to assign a massage to these departments. nine0003
In the postpartum period, massage improves the tone of the uterus, helping it to restore its previous size in a short time, restore the tone of the muscles of the anterior abdominal wall.