Braxton hicks starts at what week
Braxton Hicks contractions | Pregnancy Birth and Baby
Braxton Hicks contractions | Pregnancy Birth and Baby beginning of content4-minute read
Listen
If you feel tightening or cramping in your abdomen during your pregnancy, you may be having Braxton Hicks contractions. This is normal and not a sign that you’re ready to give birth.
Braxton Hicks contractions are sometimes called ‘false’ or ‘practice’ contractions.
What are Braxton Hicks contractions?
Braxton Hicks contractions are a tightening in your abdomen that comes and goes. They are contractions of your uterus in preparation for giving birth. They tone the muscles in your uterus and may also help prepare the cervix for birth.
Braxton Hicks contractions don’t cause labour and aren’t a sign that labour is beginning.
If you’re not sure whether what you’re experiencing is Braxton Hicks contractions or actual labour, contact your doctor or midwife. They will be able to tell by doing a vaginal examination — if there are no signs that your cervix is changing, it is not labour.
What do they feel like?
Braxton Hicks contractions feel like muscles tightening across your belly, and if you put your hands on your belly when the contractions happen, you can probably feel your uterus becoming hard.
The contractions come irregularly and usually last for about 30 seconds. While they can be uncomfortable, they usually aren’t painful.
If the pain or discomfort of your contractions eases off, they’re probably Braxton Hicks contractions.
When do you get them?
Braxton Hicks contractions occur from early in your pregnancy but you may not feel them until the second trimester. If this is your first pregnancy, you might start to feel them from about 16 weeks. In later pregnancies, you may feel Braxton Hicks contractions more often, or earlier. Some women won’t feel them at all.
Some women won’t feel them at all.
In late pregnancy, you may experience Braxton Hicks contractions more often — perhaps as much as every 10 to 20 minutes. This is a sign that you are preparing for labour — known as prelabour.
How are Braxton Hicks contractions different from labour pain?
There are some differences between Braxton Hicks contractions and true labour contractions that will help your doctor or midwife decide whether you are in labour:
Braxton Hicks contractions:
- don’t result in your cervix thinning and opening
- usually last for about 30 seconds
- can be uncomfortable, but usually aren’t painful
- come and go at irregular times
- usually occur no more than once or twice an hour (until late in the pregnancy), a few times a day
- usually stop if you change position or activity or go for a walk
- usually go if you have a warm bath or shower
Real labour contractions:
- result in your cervix thinning and opening
- last 30 to 70 seconds
- become very regular
- get closer together
- last longer as time goes by
- get stronger or come more often when you walk
- get stronger over time
Should I call my doctor or midwife?
If you are less than 37 weeks pregnant, contractions can be a sign of premature labour. Contact your doctor or midwife immediately if:
Contact your doctor or midwife immediately if:
- you feel pain, pressure or discomfort in your pelvis, abdomen or lower back
- the contractions become stronger, closer together and more regular
- there is fluid leaking or gushing from your vagina
If you are full-term, you may choose to wait until a bit later in your labour, depending on what you have arranged with your doctor or midwife. If your waters break, or your contractions are strong and 5 minutes apart, it’s time to go to the hospital.
As any stage of pregnancy, you should contact your doctor or midwife immediately if you:
- you have persistent pain in your abdomen
- you have vaginal bleeding
- you notice your baby’s movements have slowed or stopped
- you feel very unwell
If you are in doubt, don’t hesitate to call your doctor or midwife for advice.
How can I ease the discomfort?
Braxton Hicks contractions are normal and don’t need treatment. But if you feel uncomfortable, you can try:
But if you feel uncomfortable, you can try:
- lying down
- taking a walk
- relaxing in a warm bath
- having a massage
It may help to practise your breathing exercises during your Braxton Hicks contractions.
Sources:
Raising Children Network (23 weeks pregnant), RANZCOG (Labour and birth), Elsevier Patient Education (Braxton Hicks Contractions)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: October 2020
Back To Top
Related pages
- Giving birth - stages of labour
- Health professionals involved in your pregnancy
- Signs of premature labour
Need more information?
Pregnancy at week 22
By week 22, some parts of your baby’s body are fully formed, while some women experience Braxton Hicks contractions about now.
Read more on Pregnancy, Birth & Baby website
Pregnancy at week 35
You'll probably be having lots of Braxton Hicks contractions by now. It's your body's way of preparing for the birth. They should stop if you move position.
Read more on Pregnancy, Birth & Baby website
Giving birth - contractions
Contractions are when the muscles in your uterus tighten and then relax. They occur throughout the later stages of your pregnancy.
Read more on Pregnancy, Birth & Baby website
What happens to your body in childbirth
During childbirth, your body's hormones, ligaments and muscles, as well as the shape of your pelvis, all work together to bring your baby safely into the world.
Read more on Pregnancy, Birth & Baby website
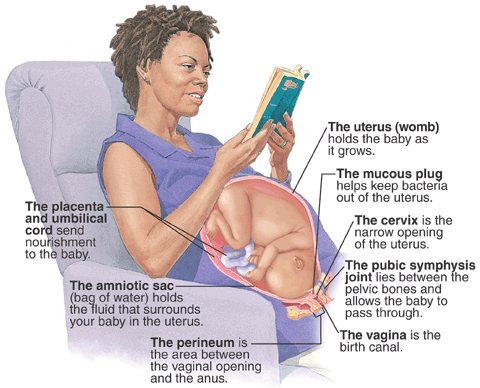
Anatomy of pregnancy and birth - uterus
The uterus is your growing baby’s home during pregnancy. Learn how the uterus works, nurtures your baby and how it changes while you are pregnant.
Read more on Pregnancy, Birth & Baby website
Preterm labour - MyDr.com.au
Going into labour before your 37th week of pregnancy is called preterm labour, or premature labour. Find out what it means for you and your baby.
Read more on myDr website
38 weeks pregnant | Raising Children Network
38 weeks pregnant? In this pregnancy week by week guide, find out how your baby is growing, how your body is changing and how to look after yourself.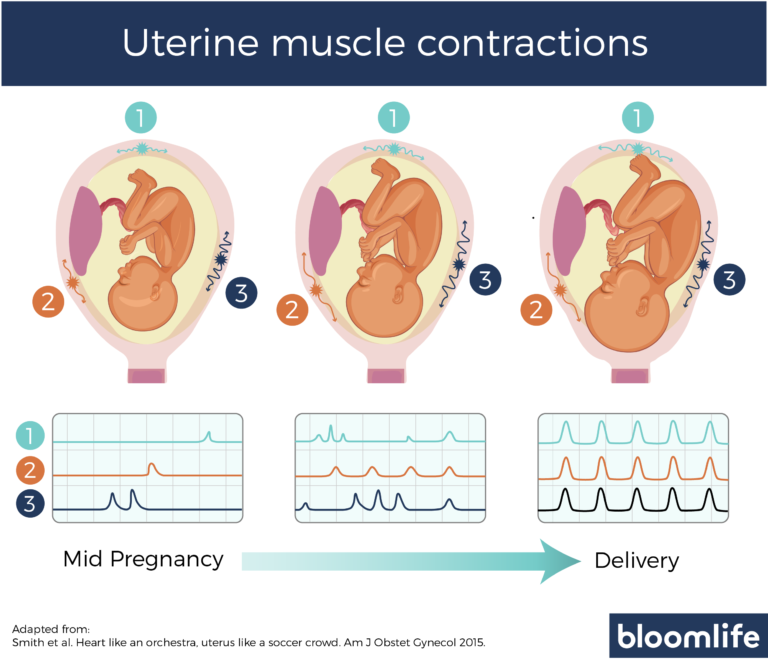
Read more on raisingchildren.net.au website
26 weeks pregnant | Raising Children Network
26 weeks pregnant? In this pregnancy week by week guide, find out how your baby is growing, how your body is changing and how to look after yourself.
Read more on raisingchildren.net.au website
Giving birth - early signs of labour
You can know the early signs of labour, even if you cannot predict when your labour will begin. Find out also what to do if something appears to be wrong.
Read more on Pregnancy, Birth & Baby website
Anatomy of pregnancy and birth
From conception to giving birth, a woman's body goes through many physical changes. Learn what happens to your body during pregnancy and labour.
Learn what happens to your body during pregnancy and labour.
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Braxton Hicks Contractions - StatPearls
Deborah A. Raines; Danielle B. Cooper.
Author Information
Last Update: August 8, 2022.
Continuing Education Activity
Braxton-Hicks contractions, also known as prodromal or false labor pains, are contractions of the uterus that typically are not felt until the second or third trimester of the pregnancy. Braxton-Hicks contractions are the body's way of preparing for true labor, but they do not indicate that labor has begun. Because many pregnant patients have not been educated about Braxton-Hicks contractions, they often seek care and undergo unnecessary evaluation for these contractions. This activity reviews the evaluation and management of patients with Braxton-Hicks contractions and highlights the role of the interprofessional team in educating the patient about the condition.
Braxton-Hicks contractions are the body's way of preparing for true labor, but they do not indicate that labor has begun. Because many pregnant patients have not been educated about Braxton-Hicks contractions, they often seek care and undergo unnecessary evaluation for these contractions. This activity reviews the evaluation and management of patients with Braxton-Hicks contractions and highlights the role of the interprofessional team in educating the patient about the condition.
Objectives:
Describe the etiology of Braxton-Hicks contractions.
Review the presentation of a patient with Braxton-Hicks contractions.
Explain how to evaluate a patient with Braxton-Hicks contractions.
Employ strategies to improve interprofessional communication, which will improve outcomes in patients with Braxton-Hicks contractions.
Access free multiple choice questions on this topic.
Introduction
Braxton Hicks contractions are sporadic contractions and relaxation of the uterine muscle. Sometimes, they are referred to as prodromal or “false labor" pains. It is believed they start around 6 weeks gestation but usually are not felt until the second or third trimester of the pregnancy. Braxton Hicks contractions are the body's way of preparing for true labor, but they do not indicate that labor has begun or is going to start.
Sometimes, they are referred to as prodromal or “false labor" pains. It is believed they start around 6 weeks gestation but usually are not felt until the second or third trimester of the pregnancy. Braxton Hicks contractions are the body's way of preparing for true labor, but they do not indicate that labor has begun or is going to start.
Braxton Hicks contractions are a normal part of pregnancy. They may be uncomfortable, but they are not painful. Women describe Braxton Hicks contractions as feeling like mild menstrual cramps or a tightening in a specific area of the abdomen that comes and goes.[1][2][3]
Braxton Hicks contractions can be differentiated from the contractions of true labor. Braxton Hicks contractions are irregular in duration and intensity, occur infrequently, are unpredictable and non-rhythmic, and are more uncomfortable than painful. Unlike true labor contractions, Braxton Hicks contractions do not increase in frequency, duration, or intensity. Also, they lessen and then disappear, only to reappear at some time in the future. Braxton Hicks contractions tend to increase in frequency and intensity near the end of the pregnancy. Women often mistake Braxton Hicks contractions for true labor. However, unlike true labor contractions, Braxton Hicks contractions do not cause dilatation of the cervix and do not culminate in birth.
Braxton Hicks contractions tend to increase in frequency and intensity near the end of the pregnancy. Women often mistake Braxton Hicks contractions for true labor. However, unlike true labor contractions, Braxton Hicks contractions do not cause dilatation of the cervix and do not culminate in birth.
Etiology
Braxton Hicks contractions are caused when the muscle fibers in the uterus tighten and relax. The exact etiology of Braxton Hicks contractions is unknown. However, there are known circumstances that trigger Braxton Hicks contractions including when the woman is very active, when the bladder is full, following sexual activity, and when the woman is dehydrated. A commonality among all these triggers is the potential for stress to the fetus, and the need for increased blood flow to the placenta to provide fetal oxygenation.[4][5][6]
Epidemiology
Braxton Hicks contractions are present in all pregnancies. However, each woman's experience is different. Most women become aware of Braxton Hicks contractions in the third trimester, and some women are aware of them as early as the second trimester.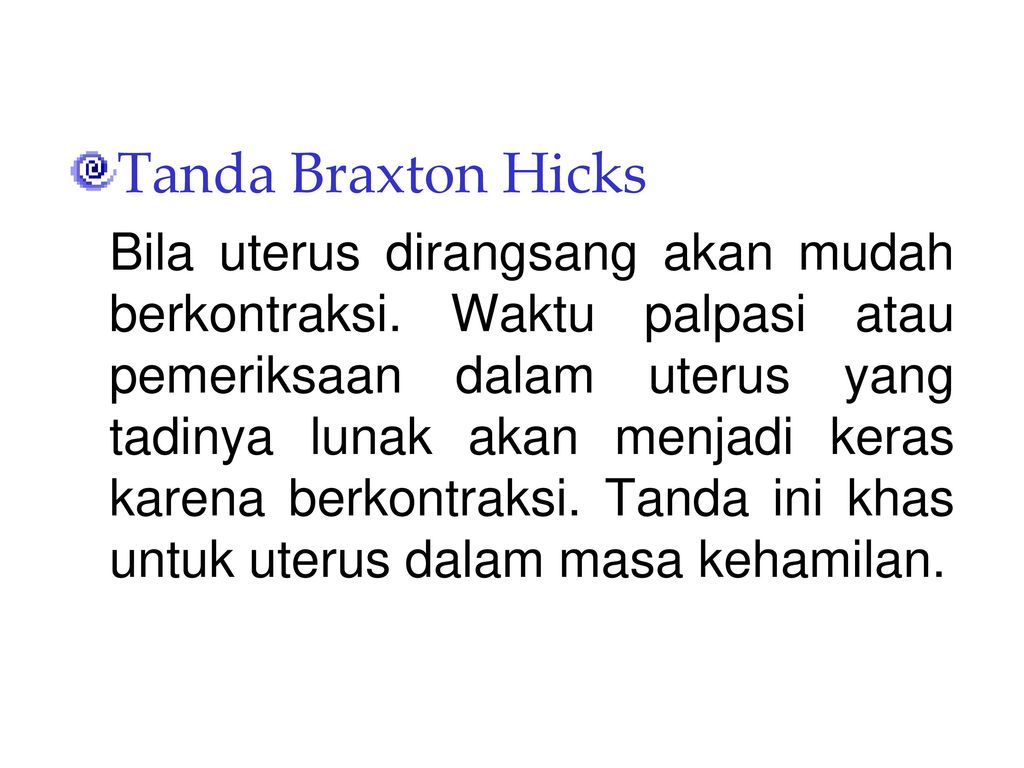 Sometimes Braxton Hick contractions occurring near the end of the third trimester of pregnancy are mistaken as the onset of true labor. It is not unusual, especially in a first pregnancy, for a woman to think she is in labor only to be told it is Braxton Hicks contractions and not true labor.
Sometimes Braxton Hick contractions occurring near the end of the third trimester of pregnancy are mistaken as the onset of true labor. It is not unusual, especially in a first pregnancy, for a woman to think she is in labor only to be told it is Braxton Hicks contractions and not true labor.
Pathophysiology
Braxton Hicks contractions are thought to play a role in toning the uterine muscle in preparation for the birth process. Sometimes Braxton Hicks contractions are referred to as "practice for labor." Braxton Hicks contractions do not result in dilation of the cervix but may have a role in cervical softening.
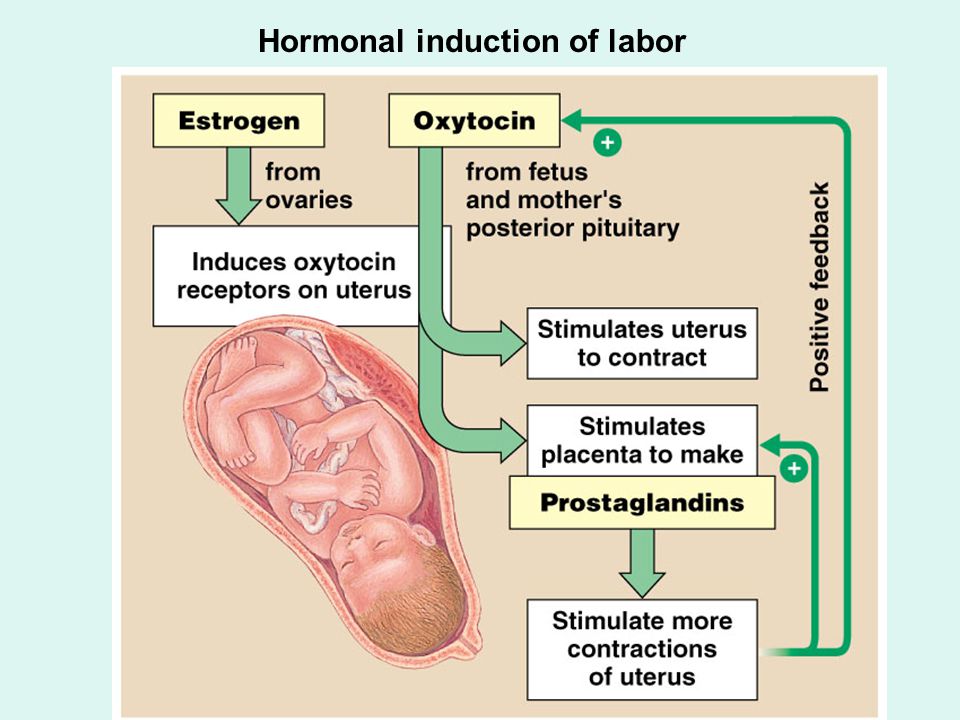
The intermittent contraction of the uterine muscle may also play a role in promoting blood flow to the placenta. Oxygen-rich blood fills the intervillous spaces of the uterus where the pressure is relatively low. The presence of Braxton Hicks contractions causes the blood to flow up to the chorionic plate on the fetal side of the placenta. From there the oxygen-rich blood enters the fetal circulation.
History and Physical
When assessing a woman for the presence of Braxton Hicks contractions, there are some key questions to ask. Her response to these questions will assist the healthcare provider to differentiate Braxton Hicks contractions and true labor contractions.[7][8][9]
How often are the contractions? Braxton Hicks contractions are irregular and do not get closer together over time. True labor contractions come at regular intervals, and as time goes on, they get closer together and stronger.
How long are the contractions? Braxton Hicks contractions are unpredictable. They may last less than 30 seconds or up to 2 minutes. True labor contractions last between 30 to less than 90 seconds and become longer over time.
How strong are the contractions? Braxton Hicks contractions are usually weak and either stay the same or become weaker and then disappear. True labor contractions get stronger over time.
Where are the contractions felt? Braxton Hicks contractions are often only felt in the front of the abdomen or one specific area.
 True labor contractions start in the midback and wrap around the abdomen towards the midline.
True labor contractions start in the midback and wrap around the abdomen towards the midline.Do the contractions change with movement? Braxton Hicks contractions may stop with a change in activity level or as the woman changes position. If she can sleep through the contraction, it is a Braxton Hicks contraction. True labor contractions continue and may even become stronger with movement or position change.
During the physical assessment, the provider may palpate an area of tightening or a "spasm" of the uterine muscle, but the presence of a uterine contraction in the uterine fundus is not palpable. The woman will be assessed for the presence of uterine bleeding or rupture of the amniotic membrane. An examination of the cervix reveals no change in effacement or dilatation as a result of the Braxton Hicks contractions.
Evaluation
There are no laboratory or radiographic tests to diagnose Braxton Hicks contractions. Evaluation of the presence of Braxton Hicks contractions is based on an assessment of the pregnant woman's abdomen, specifically palpating the contractions.
Treatment / Management
By the midpoint of pregnancy, the woman and provider should discuss what the woman may experience during the remainder of the pregnancy. Braxton Hicks contractions are one of the normal events a woman may experience. Teaching her about Braxton Hicks contractions will help her to be informed and to decrease her anxiety if they occur.[10][11][12]
There is no medical treatment for Braxton Hicks contractions. However, taking action to change the situation that triggered the Braxton Hicks contractions is warranted. Some actions to ease Braxton Hicks contractions include:
Changing position or activity level: if the woman has been very active, lie down; if the woman has been sitting for an extended time, go for a walk.
Relaxing: take a warm bath, get a massage, read a book, listen to music, or take a nap.
Drinking water to rehydrate.
If these actions do not lessen the Braxton Hicks contractions or if the contractions continue and are becoming more frequent or more intense, the patient's healthcare provider should be contacted.
Also, if any of the following are present the healthcare provider should be contacted immediately:
Vaginal bleeding
Leaking of fluid from the vagina
Strong contractions every 5-minutes for an hour
Contractions that the woman is unable to "walk through"
A noticeable change in fetal movement, or if there are less than ten movements every 2 hours.
Differential Diagnosis
Amenorrhea
Ascites
Full bladder
Hematometra
Nausea
Ovarian cysts
Pseudocyesis
Uterine fibroids
Vomiting
Pearls and Other Issues
In addition to Braxton Hicks contractions, there are other causes of abdominal pain during pregnancy. Some normal reasons for abdominal pain during pregnancy, in addition to Braxton Hicks contractions and true labor contractions, include:
Round ligament pain or a sharp, jabbing feeling felt in the lower abdomen or groin area on one or both sides.

Higher levels of progesterone can cause excess gas during pregnancy.
Constipation may be a source of abdominal pain.
Circumstances in which abdominal pain is a sign of a serious condition that requires immediate medical attention include:
Ectopic pregnancy.
Placental abruption. A key symptom of placental abruption is intense and constant pain that causes the uterus to become hard for an extended period without relief.
Urinary tract infection symptoms include pain and discomfort in the lower abdomen as well as burning with urination.
Preeclampsia is a condition of pregnancy occurring after 20-weeks gestation and characterized by high blood pressure and protein in the urine. Upper abdominal pain, usually under the ribs on the right side, can be present in preeclampsia.
If a woman is unsure if she is experiencing Braxton Hicks contractions or another condition, a discussion with a healthcare provider is needed. The healthcare provider may recommend a visit to the office setting or labor and delivery for an examination by a healthcare professional to determine the cause of the abdominal pain.
The healthcare provider may recommend a visit to the office setting or labor and delivery for an examination by a healthcare professional to determine the cause of the abdominal pain.
Enhancing Healthcare Team Outcomes
Braxton hicks contractions are fairly common and it is important for the emergency department physician labor & delivery nurse and nurse practitioner to be aware that this is not true labor. If there is any doubt, the obstetrician should be consulted. However, at the same time, the onus is on the healthcare workers to rule out true labor. Other organic disorders like appendicitis, urinary tract infection or cholecystitis must also be ruled out. With the right education, patients with braxton hicks contraction will not needlessly rush to the ED every time they sense a contraction.
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Hanghøj S.
 When it hurts I think: Now the baby dies. Risk perceptions of physical activity during pregnancy. Women Birth. 2013 Sep;26(3):190-4. [PubMed: 23711581]
When it hurts I think: Now the baby dies. Risk perceptions of physical activity during pregnancy. Women Birth. 2013 Sep;26(3):190-4. [PubMed: 23711581]- 2.
MacKinnon K, McIntyre M. From Braxton Hicks to preterm labour: the constitution of risk in pregnancy. Can J Nurs Res. 2006 Jun;38(2):56-72. [PubMed: 16871850]
- 3.
Dunn PM. John Braxton Hicks (1823-97) and painless uterine contractions. Arch Dis Child Fetal Neonatal Ed. 1999 Sep;81(2):F157-8. [PMC free article: PMC1720982] [PubMed: 10448189]
- 4.
Lockwood CJ. The diagnosis of preterm labor and the prediction of preterm delivery. Clin Obstet Gynecol. 1995 Dec;38(4):675-87. [PubMed: 8616965]
- 5.
Arduini D, Rizzo G, Rinaldo D, Capponi A, Fittipaldi G, Giannini F, Romanini C. Effects of Braxton-Hicks contractions on fetal heart rate variations in normal and growth-retarded fetuses. Gynecol Obstet Invest. 1994;38(3):177-82. [PubMed: 8001871]
- 6.

Kofinas AD, Simon NV, Clay D, King K. Functional asymmetry of the human myometrium documented by color and pulsed-wave Doppler ultrasonographic evaluation of uterine arcuate arteries during Braxton Hicks contractions. Am J Obstet Gynecol. 1993 Jan;168(1 Pt 1):184-8. [PubMed: 8420324]
- 7.
Lockwood CJ, Dudenhausen JW. New approaches to the prediction of preterm delivery. J Perinat Med. 1993;21(6):441-52. [PubMed: 8006770]
- 8.
Rhoads GG, McNellis DC, Kessel SS. Home monitoring of uterine contractility. Summary of a workshop sponsored by the National Institute of Child Health and Human Development and the Bureau of Maternal and Child Health and Resources Development, Bethesda, Maryland, March 29 and 30, 1989. Am J Obstet Gynecol. 1991 Jul;165(1):2-6. [PubMed: 1677235]
- 9.
Oosterhof H, Dijkstra K, Aarnoudse JG. Fetal Doppler velocimetry in the internal carotid and umbilical artery during Braxton Hicks' contractions.
 Early Hum Dev. 1992 Aug;30(1):33-40. [PubMed: 1396288]
Early Hum Dev. 1992 Aug;30(1):33-40. [PubMed: 1396288]- 10.
Oosterhof H, Dijkstra K, Aarnoudse JG. Uteroplacental Doppler velocimetry during Braxton Hicks' contractions. Gynecol Obstet Invest. 1992;34(3):155-8. [PubMed: 1427416]
- 11.
Bower S, Campbell S, Vyas S, McGirr C. Braxton-Hicks contractions can alter uteroplacental perfusion. Ultrasound Obstet Gynecol. 1991 Jan 01;1(1):46-9. [PubMed: 12797102]
- 12.
Hill WC, Lambertz EL. Let's get rid of the term "Braxton Hicks contractions". Obstet Gynecol. 1990 Apr;75(4):709-10. [PubMed: 2314790]
Braxton-Hicks contractions or false labor contractions are irregular contractions and relaxation of the muscles of the uterus as a way of preparing for true labor. They are thought to start around 6 weeks of gestation but are not usually felt until the 2nd or 3rd trimester.
False contractions are a normal part of pregnancy. They may be uncomfortable, but not painful. Women describe them as a feeling that feels like mild menstrual cramps or tightness in a specific area of the abdomen that quickly resolves. nine0003
They may be uncomfortable, but not painful. Women describe them as a feeling that feels like mild menstrual cramps or tightness in a specific area of the abdomen that quickly resolves. nine0003
They are also irregular in duration and intensity, occur infrequently, are unpredictable and not rhythmic, and are more uncomfortable than painful.
Braxton Hicks contractions tend to increase in frequency and intensity towards the end of pregnancy. Women often mistake Braxton Hicks contractions for real labor. However, unlike real contractions, they do not dilate the cervix and result in the birth of a baby.
Braxton Hicks contractions occur when the muscle fibers of the uterus contract and relax. The exact etiology of Braxton Hicks contractions is unknown. However, there are circumstances that can cause them:
- when the woman is very active,
- when the bladder is full,
- after sexual activity,
- when the woman is dehydrated.
Common among all these circumstances is the potential stress on the fetus and the need for increased blood flow to the placenta to provide oxygen to the fetus.
- Change position or activity level: if you have been very active, lie down; if you have been sitting for a long time, go for a walk. nine0014
- Relax: take a warm bath, massage, read a book, listen to music or take a nap.
If you have Braxton Hicks contractions or if they continue and become more frequent and intense, you should see your doctor.
When assessing for Braxton Hicks contractions, there are a few key questions to ask yourself. We have prepared a table for you with questions, the answers to which will help you understand what kind of contractions you have:
| Braxton Higgs contractions | Real labor pains | |
|---|---|---|
| How often do contractions occur? | Irregular and do not increase over time. | Occurs at regular intervals and gets stronger over time. |
| How long do contractions last? | Unpredictable. They can last less than 30 seconds or up to 2 minutes. nine0048 nine0048 | Lasts 30 to 90 seconds and gets longer over time. |
| How strong are the contractions? | Usually weak and either stay the same or get weaker and then disappear. | Increase over time. |
| Where do contractions feel? | Often only felt in the front of the abdomen or in one specific area. | Begin in the middle of the back and wrap around the belly towards the midline. nine0048 |
| Do abbreviations change with movement? | May stop if activity level changes or if woman's position changes. | Continue and may even get worse with movement or change of position. |
Back to the list of articles
what happens, the development of pregnancy and fetus
33 - 36 weeks of pregnancy
Elena Gevorkova
Obstetrician-gynecologist, Moscow
33rd week
BABY
At the 33rd week, the weight of the fetus is 1800-1900 g, and the body length is 43-44 cm. The amount of subcutaneous fat increases, due to which the folds and wrinkles on the baby's body are smoothed out, the skin turns pink. The fluffy hairs that cover the body of the fetus, which are called lanugo, become smaller, and the hair on the head darkens and thickens. The baby's skin is covered with a thin layer of cheese-like lubricant, its largest amount accumulates in the folds - axillary, cervical, inguinal - as well as on the back of the body and face. Grease is a viscous mass of white color, it is a secret of the sebaceous glands, mixed with skin scales. Its function is to protect the baby's skin from damage and facilitate its passage through the birth canal. nine0003
The amount of subcutaneous fat increases, due to which the folds and wrinkles on the baby's body are smoothed out, the skin turns pink. The fluffy hairs that cover the body of the fetus, which are called lanugo, become smaller, and the hair on the head darkens and thickens. The baby's skin is covered with a thin layer of cheese-like lubricant, its largest amount accumulates in the folds - axillary, cervical, inguinal - as well as on the back of the body and face. Grease is a viscous mass of white color, it is a secret of the sebaceous glands, mixed with skin scales. Its function is to protect the baby's skin from damage and facilitate its passage through the birth canal. nine0003
By this time, the movements of the fetus gradually change their habitual character - they become more and more limited and less pronounced in amplitude due to insufficient space. However, the strength of the movements increases, since by this time the muscular system of the fetus is already sufficiently strengthened. Sharp and strong tremors of the fetus can be sensitive to the internal organs of a pregnant woman. Depending on the position of the baby, the liver, stomach, bladder, ribs, etc. may “suffer”. By 33 weeks, the movements of the fetus are already quite coordinated. nine0003
Sharp and strong tremors of the fetus can be sensitive to the internal organs of a pregnant woman. Depending on the position of the baby, the liver, stomach, bladder, ribs, etc. may “suffer”. By 33 weeks, the movements of the fetus are already quite coordinated. nine0003
FUTURE MOTHER
The height of the fundus of the uterus from the level of the pubis at this time is 34 cm. The volume of the abdomen is increased due to the weight of the baby, placenta, amniotic fluid. The increase in uterine pressure and strong tremors of the fetus can cause some discomfort in the pregnant woman. Many movements previously available to the expectant mother, such as squats, become limited. Moderate physical activity - walking, fitness, etc. - Requires frequent respite.
A change in the center of gravity increases the load on the spine, which can manifest itself as pain in the lower back, sacrum, and pelvic region. The pressure of the uterus on the stomach can cause or increase nausea, heartburn, and a feeling of heaviness. An increase of almost 1 liter of the volume of circulating blood in the body of a pregnant woman increases the load on the kidneys, and the growing uterus puts pressure on the bladder. All this can be manifested by frequent urination. nine0003
An increase of almost 1 liter of the volume of circulating blood in the body of a pregnant woman increases the load on the kidneys, and the growing uterus puts pressure on the bladder. All this can be manifested by frequent urination. nine0003
These ailments are usually associated with the mechanical pressure of the uterus on the surrounding organs; they are not symptoms of the disease and are temporary. And to relieve nausea, heartburn and a feeling of heaviness in the stomach, frequent meals in small portions are recommended.
34th week
BABY
By this time, the weight of the fetus is approximately 2100 g, and the height is 45 cm. From this period, the cheeks are very pronounced, because, developing a sucking reflex, the fetus often sucks its thumb. This leads to the fact that the baby strengthens the facial muscles, in particular the buccal. The total muscle mass of the fetus increases, the bones become denser. nine0003
nine0003
There is an intensive functioning of the baby's internal organs. During the day, he repeatedly swallows portions of amniotic fluid. Passing through the gastrointestinal tract, the amniotic fluid stimulates the work of the muscular wall. The dense part of the amniotic fluid, which is a suspension of skin flakes, lubricant, vellus hair, is processed by the enzymes of the liver and pancreas, and the liquid part is intensively excreted by the kidneys of the fetus.
Approximately 500 ml of amniotic fluid is treated in this way per day. The production of bile continues, which accumulates in the gallbladder and, as the stomach fills with a suspension of amniotic water, enters the lumen of the small intestine. The functional development of the liver and pancreas during the prenatal period does not play a significant role, since the fetus does not have digestion; processes for the production of bile and enzymes: lipase, which breaks down fats; trypsin, which breaks down proteins; amylase, which breaks down carbohydrates, etc. - are preparatory in nature. nine0003
- are preparatory in nature. nine0003
FUTURE MOTHER
Most pregnant women begin to feel rather intense false contractions at this time. Strictly speaking, false or training contractions, which are also called Braxton-Hicks contractions, can occur after the 20th week of pregnancy: the longer the period, the more frequent and pronounced the contractions. They are episodic contractions of the muscles of the uterus, lasting from a few seconds to 3-5 minutes. Braxton Hicks contractions are not pathological - this is a completely normal process of preparing the muscles of the uterus for the difficult process of childbirth. This phenomenon with varying degrees of intensity is observed in almost all pregnant women. nine0003
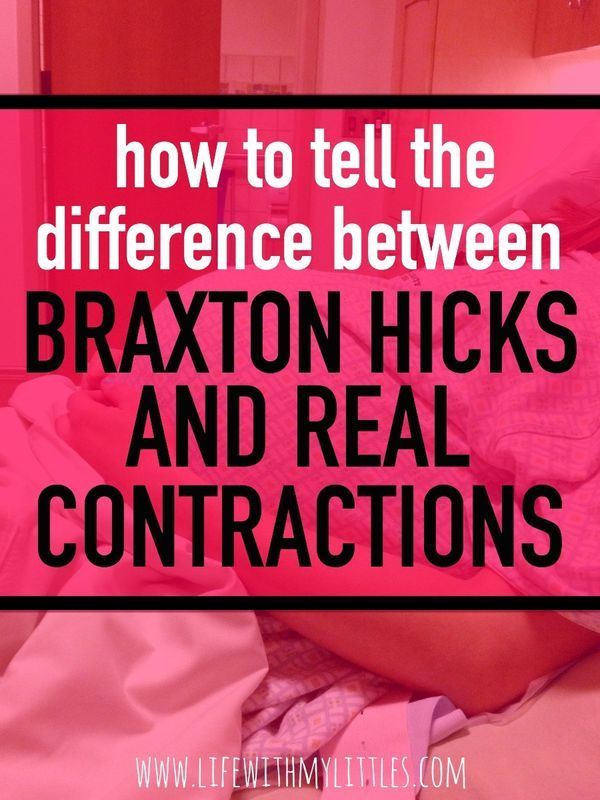
Many primiparas are concerned about the difference between preparatory contractions and labor.
Here are some differences:
- Frequency of contractions. Training bouts do not become more frequent, the intervals between them may be different.
 Labor pains are regular, the interval between them is reduced.
Labor pains are regular, the interval between them is reduced. - Duration of contractions. Training bouts have different durations, from a few seconds to minutes, their duration does not increase over time. Labor pains tend to lengthen. nine0014
- Soreness. Preparatory contractions may not be accompanied by pain at all, or they may be quite noticeable, up to a feeling of sharp pain. However, their intensity weakens over time and the pain disappears. Labor pains are painful and constantly intensifying.
- Localization. Braxton-Hicks contractions can be felt in various places - in the lower part of the uterus, in the area of \u200b\u200bits bottom, along the side walls, covering the entire abdomen. Labor pains begin with a contraction of the lower abdomen, spreading to the front. Often in childbirth, pain in the lower back is felt, while the nature of the pain resembles menstrual pain. nine0014
- Relationship with body position. Preparatory contractions may disappear after walking or, on the contrary, rest.
 A change in body position can relieve the tension in some muscles, which also causes a decrease in the appearance of training contractions. Labor pains may be somewhat relieved in a certain position - when leaning forward, in the knee-elbow position, etc. - but their frequency and duration will still increase.
A change in body position can relieve the tension in some muscles, which also causes a decrease in the appearance of training contractions. Labor pains may be somewhat relieved in a certain position - when leaning forward, in the knee-elbow position, etc. - but their frequency and duration will still increase. - Reaction to medication. The use of antispasmodic drugs - NO-ShPY, BUSCOPAN, PAPAVERIN, etc. - approved by the attending physician, can weaken or completely stop false contractions. The effect of antispasmodics on labor pains is minimal. nine0014
Any pain or discomfort should be reported to the gynecologist: this will help the expectant mother to resolve doubts and cope with anxiety. Feeling safe is the best companion of pregnancy.
35th week
BABY
The body length of the fetus is 46--47 cm, weight - 2200-2300 g. These figures in the last weeks of pregnancy can vary greatly. The growth and weight of the fetus largely depend on heredity, individual parameters. Starting from 35 weeks, the baby will gain 200-250 g weekly. The fetus occupies almost the entire uterine cavity, its back is rounded, arms and legs are bent, brought to the body. The layer of subcutaneous fat increases significantly, which significantly “rounds” the body of the fetus. The closing of the eyelids and the contraction of facial muscles change the baby's facial expression quite often. The skin of the body becomes pink, smooth, the amount of cheese-like lubricant begins to decrease. Vellus hair covers separate small areas of the body - shoulders, back. The nails protrude beyond the tips of the fingers. nine0003
Starting from 35 weeks, the baby will gain 200-250 g weekly. The fetus occupies almost the entire uterine cavity, its back is rounded, arms and legs are bent, brought to the body. The layer of subcutaneous fat increases significantly, which significantly “rounds” the body of the fetus. The closing of the eyelids and the contraction of facial muscles change the baby's facial expression quite often. The skin of the body becomes pink, smooth, the amount of cheese-like lubricant begins to decrease. Vellus hair covers separate small areas of the body - shoulders, back. The nails protrude beyond the tips of the fingers. nine0003
FUTURE MOTHER
The fundus of the uterus is 35 cm higher from the pubis and 15 cm higher from the navel. particularly light. The growing uterus does not allow the lungs to expand, respiratory movements are limited, which is manifested by shortness of breath. Almost all pregnant women to some extent experience a feeling of shortness of breath - a feeling of lack of air, frequent and shallow breathing, a desire to take a deep breath. As a rule, these sensations occur for a period of 28 weeks and reach their peak at the 35-36th week. After 37 weeks of pregnancy, the abdomen droops, which greatly facilitates breathing. nine0003
As a rule, these sensations occur for a period of 28 weeks and reach their peak at the 35-36th week. After 37 weeks of pregnancy, the abdomen droops, which greatly facilitates breathing. nine0003
Shortness of breath during pregnancy is associated not only with the mechanical pressure of the uterus on the diaphragm, but also with the relaxing effect of hormones on the muscles of the bronchi and lungs. Most often, it is provoked by physical activity - climbing stairs, a long walk, etc. However, it is not uncommon for shortness of breath to occur at rest, especially when lying down. Both prolonged lying in a horizontal position and excessive exercise can contribute to increased shortness of breath. To alleviate her condition, the expectant mother needs to be rational about the daily routine - it is reasonable to alternate rest and physical activity. It is important to monitor your posture, as slouching exacerbates shortness of breath, reducing the already insufficient lung capacity. If shortness of breath is accompanied by blue lips or nails, sensations of pain behind the sternum, darkening before the eyes, nausea or vomiting, fainting, then an urgent need to consult a doctor. nine0003
nine0003
36th week
BABY
The growth of the fetus by this term is approximately 47-48 cm, and the weight is about 2300-2500 g. The fetus enters a period of intensive preparation for childbirth. Each of the organs is already functionally mature enough to ensure the viability of the fetus. 36 weeks is the beginning of the preparatory journey, and the upcoming weeks of pregnancy are designed to finally form the baby's readiness for extrauterine life.
By 36 weeks, the fetus is in its final position in the uterus. As a rule, this is a longitudinal position, occipital presentation - in this case, the fetus is located head down, facing the mother's back. This is the most comfortable position that ensures the greatest safety of the baby during childbirth. More rarely, breech presentation is a condition in which the buttocks and legs of the fetus are located at the bottom of the uterus. This is a relative indication for operative delivery. The final decision on caesarean section or independent childbirth is made by doctors in each case individually. nine0003
The final decision on caesarean section or independent childbirth is made by doctors in each case individually. nine0003
A change in the position of the fetus in the uterus is possible, but this happens infrequently, since at this time the fetus occupies almost all the free space in the uterus, which significantly limits its motor activity. As a rule, if a change in the position of the fetus occurs, then only from the pelvic to the head. The reverse cases - the transition of the baby from the head position to the pelvic position - are practically impossible, since the head of the fetus is heavier than the buttocks and occupies the longitudinal position completely, by analogy with a float in water, the heavy part of which always outweighs. nine0003
FUTURE MOTHER
The height of the uterus is 36 cm, the volume of the abdomen is maximally increased, the bottom reaches the costal arches. At this time, the pregnant woman's body also begins its journey of preparing for the upcoming birth.