Pregnancy and iron deficiency
Anemia in Pregnancy: Causes, Symptoms, and Treatment
Written by Jen Uscher
In this Article
- Types of Anemia During Pregnancy
- Risk Factors for Anemia in Pregnancy
- Symptoms of Anemia During Pregnancy
- Risks of Anemia in Pregnancy
- Tests for Anemia
- Treatment for Anemia
- Preventing Anemia
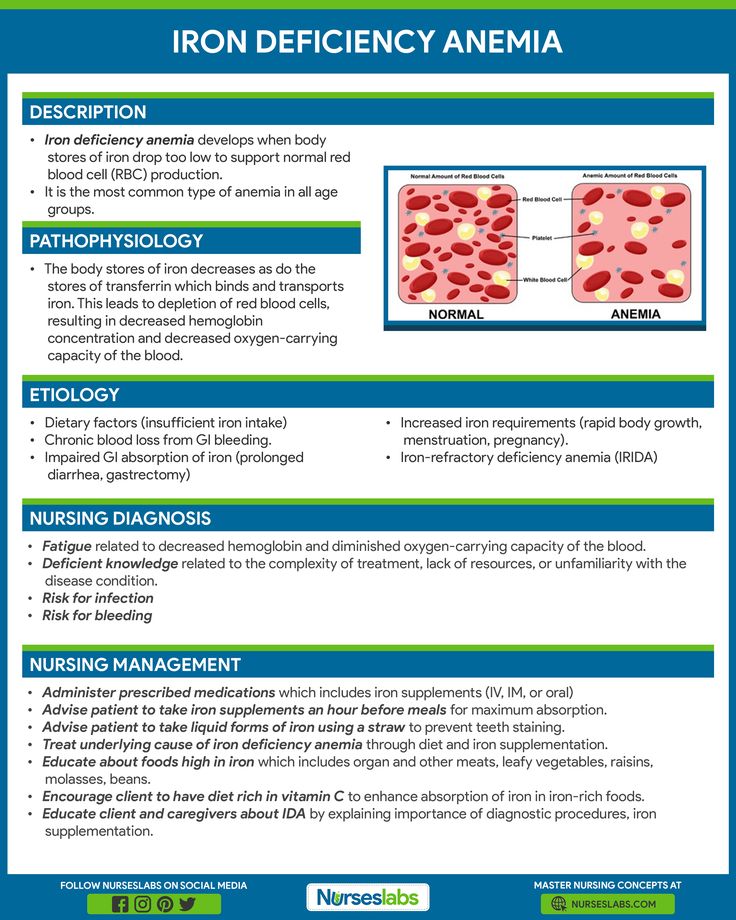
When you're pregnant, you may develop anemia. When you have anemia, your blood doesn't have enough healthy red blood cells to carry oxygen to your tissues and to your baby.
During pregnancy, your body produces more blood to support the growth of your baby. If you're not getting enough iron or certain other nutrients, your body might not be able to produce the amount of red blood cells it needs to make this additional blood.
It's normal to have mild anemia when you are pregnant. But you may have more severe anemia from low iron or vitamin levels or from other reasons.
Anemia can leave you feeling tired and weak. If it is severe but goes untreated, it can increase your risk of serious complications like preterm delivery.
Here's what you need to know about the causes, symptoms, and treatment of anemia during pregnancy.
Types of Anemia During Pregnancy
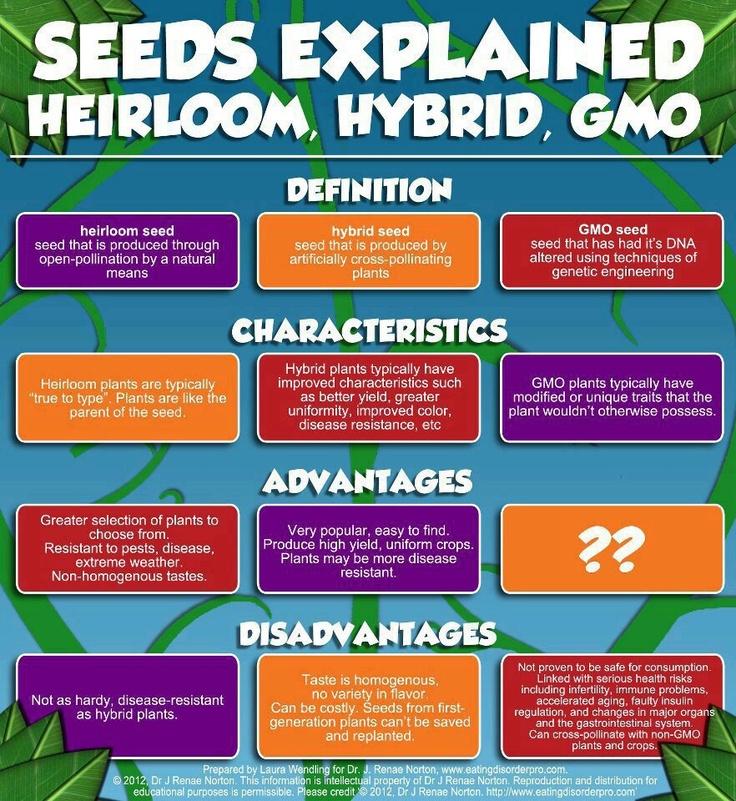
Several types of anemia can develop during pregnancy. These include:
- Iron-deficiency anemia
- Folate-deficiency anemia
- Vitamin B12 deficiency
Here's why these types of anemia may develop:
Iron-deficiency anemia. This type of anemia occurs when the body doesn't have enough iron to produce adequate amounts of hemoglobin. That's a protein in red blood cells. It carries oxygen from the lungs to the rest of the body.
In iron-deficiency anemia, the blood cannot carry enough oxygen to tissues throughout the body.
Iron deficiency is the most common cause of anemia in pregnancy.
Folate-deficiency anemia. Folate is the vitamin found naturally in certain foods like green leafy vegetables A type of B vitamin, the body needs folate to produce new cells, including healthy red blood cells.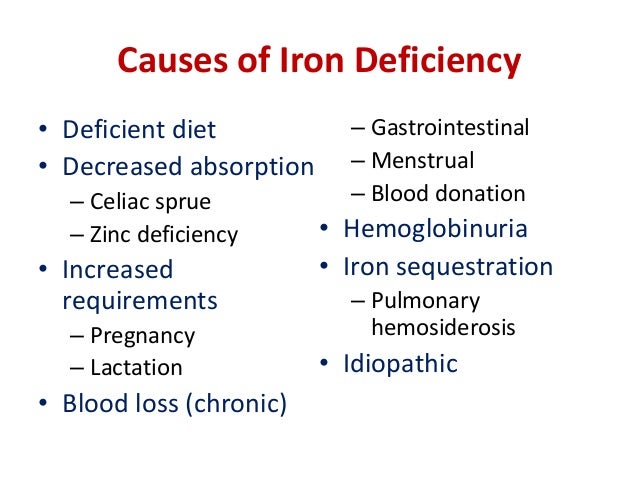
During pregnancy, women need extra folate. But sometimes they don't get enough from their diet. When that happens, the body can't make enough normal red blood cells to transport oxygen to tissues throughout the body. Man made supplements of folate are called folic acid.
Folate deficiency can directly contribute to certain types of birth defects, such as neural tube abnormalities (spina bifida) and low birth weight.
Vitamin B12 deficiency. The body needs vitamin B12 to form healthy red blood cells. When a pregnant woman doesn't get enough vitamin B12 from their diet, their body can't produce enough healthy red blood cells. Women who don't eat meat, poultry, dairy products, and eggs have a greater risk of developing vitamin B12 deficiency, which may contribute to birth defects, such as neural tube abnormalities, and could lead to preterm labor.
Blood loss during and after delivery can also cause anemia.
Risk Factors for Anemia in Pregnancy
All pregnant women are at risk for becoming anemic. That's because they need more iron and folic acid than usual. But the risk is higher if you:
That's because they need more iron and folic acid than usual. But the risk is higher if you:
- Are pregnant with multiples (more than one child)
- Have had two pregnancies close together
- Vomit a lot because of morning sickness
- Are a pregnant teenager
- Don't eat enough foods that are rich in iron
- Had anemia before you became pregnant
Symptoms of Anemia During Pregnancy
The most common symptoms of anemia during pregnancy are:
- Pale skin, lips, and nails
- Feeling tired or weak
- Dizziness
- Shortness of breath
- Rapid heartbeat
- Trouble concentrating
In the early stages of anemia, you may not have obvious symptoms. And many of the symptoms are ones that you might have while pregnant even if you're not anemic. So be sure to get routine blood tests to check for anemia at your prenatal appointments.
Risks of Anemia in Pregnancy
Severe or untreated iron-deficiency anemia during pregnancy can increase your risk of having:
- A preterm or low-birth-weight baby
- A blood transfusion (if you lose a significant amount of blood during delivery)
- Postpartum depression
- A baby with anemia
- A child with developmental delays
Untreated folate deficiency can increase your risk of having a:
- Preterm or low-birth-weight baby
- Baby with a serious birth defect of the spine or brain (neural tube defects)
Untreated vitamin B12 deficiency can also raise your risk of having a baby with neural tube defects.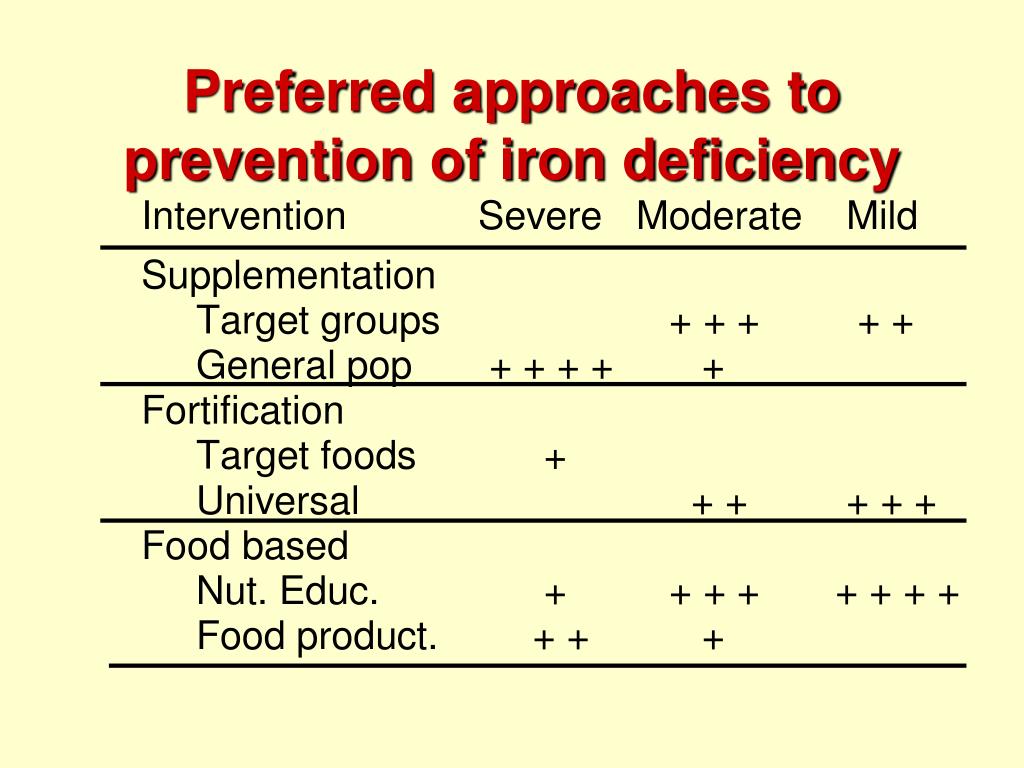
Tests for Anemia
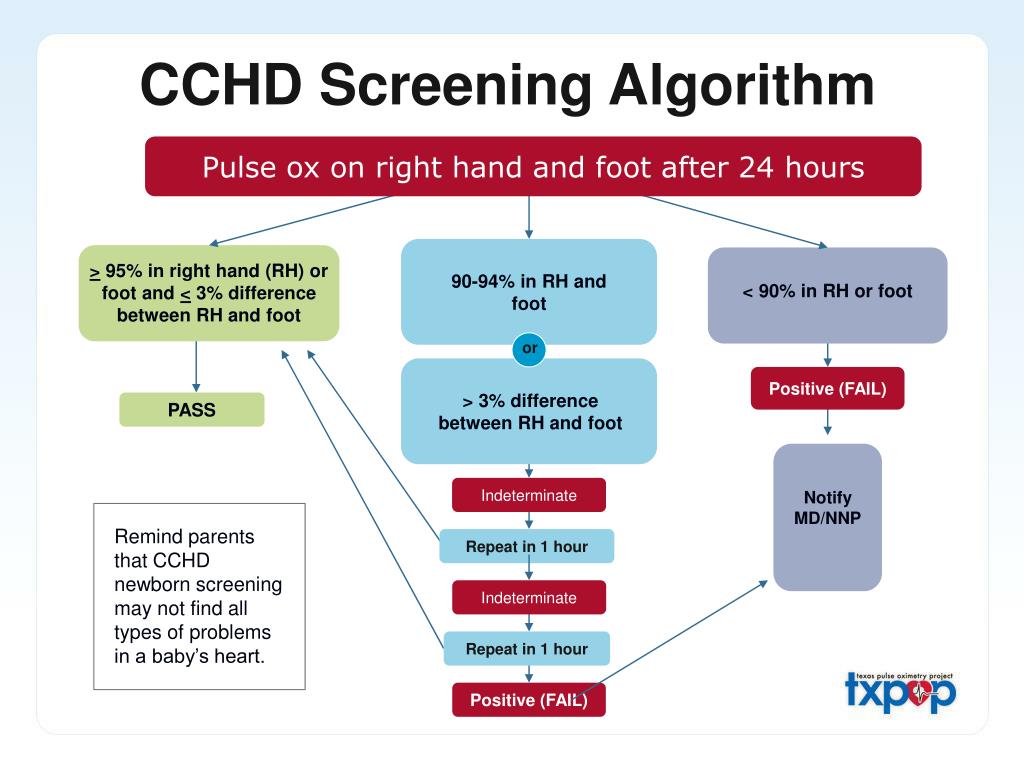
During your first prenatal appointment, you'll get a blood test so your doctor can check whether you have anemia. Blood tests typically include:
- Hemoglobin test. It measures the amount of hemoglobin -- an iron-rich protein in red blood cells that carries oxygen from the lungs to tissues in the body.
- Hematocrit test. It measures the percentage of red blood cells in a sample of blood.
If you have lower than normal levels of hemoglobin or hematocrit, you may have iron-deficiency anemia. Your doctor may check other blood tests to determine if you have iron deficiency or another cause for your anemia.
Even if you don't have anemia at the beginning of your pregnancy, your doctor will most likely recommend that you get another blood test to check for anemia in your second or third trimester.
Treatment for Anemia
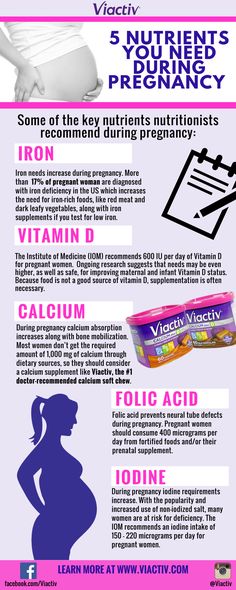
If you are anemic during your pregnancy, you may need to start taking an iron supplement and/or folic acid supplement in addition to your prenatal vitamins.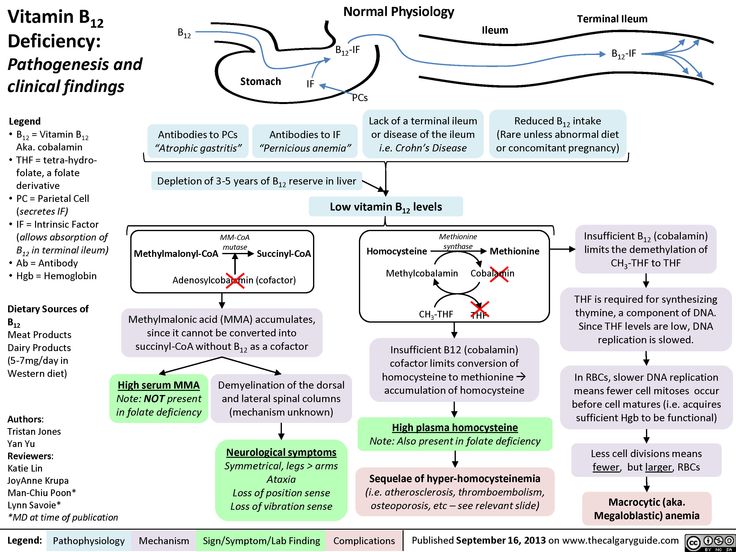 Your doctor may also suggest that you add more foods that are high in iron and folic acid to your diet.
Your doctor may also suggest that you add more foods that are high in iron and folic acid to your diet.
In addition, you'll be asked to return for another blood test after a specific period of time so your doctor can check that your hemoglobin and hematocrit levels are improving.
To treat vitamin B12 deficiency, your doctor may recommend that you take a vitamin B12 supplement.
The doctor may also recommend that you include more animal foods in your diet, such as:
- meat
- eggs
- dairy products
Your OB may refer you to a hematologist, a doctor who specializes in anemia/ blood issues. The specialist may see you throughout the pregnancy and help your OB manage the anemia.
Preventing Anemia
To prevent anemia during pregnancy, make sure you get enough iron. Eat well-balanced meals and add more foods that are high in iron to your diet.
Aim for at least three servings a day of iron-rich foods, such as:
- lean red meat, poultry, and fish
- leafy, dark green vegetables (such as spinach, broccoli, and kale)
- iron-enriched cereals and grains
- beans, lentils, and tofu
- nuts and seeds
- eggs
Foods that are high in vitamin C can help your body absorb more iron.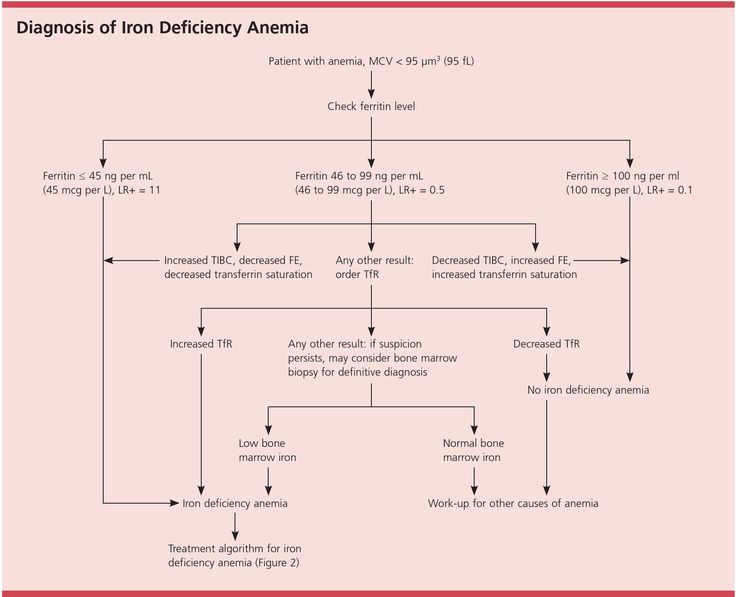 These include:
These include:
- citrus fruits and juices
- strawberries
- kiwis
- tomatoes
- bell peppers
Try eating those foods at the same time that you eat iron-rich foods. For example, you could drink a glass of orange juice and eat an iron-fortified cereal for breakfast.
Also, choose foods that are high in folate to help prevent folate deficiency. These include:
- leafy green vegetables
- citrus fruits and juices
- dried beans
- breads and cereals fortified with folic acid
Follow your doctor's instructions for taking a prenatal vitamin that contains a sufficient amount of iron and folic acid.
Vegetarians and vegans should talk with their doctor about whether they should take a vitamin B12 supplement when they're pregnant and breastfeeding.
Health & Pregnancy Guide
- Getting Pregnant
- First Trimester
- Second Trimester
- Third Trimester
- Labor and Delivery
- Pregnancy Complications
- All Guide Topics
Anemia in Pregnancy: Causes, Symptoms, and Treatment
Written by Jen Uscher
In this Article
- Types of Anemia During Pregnancy
- Risk Factors for Anemia in Pregnancy
- Symptoms of Anemia During Pregnancy
- Risks of Anemia in Pregnancy
- Tests for Anemia
- Treatment for Anemia
- Preventing Anemia
When you're pregnant, you may develop anemia.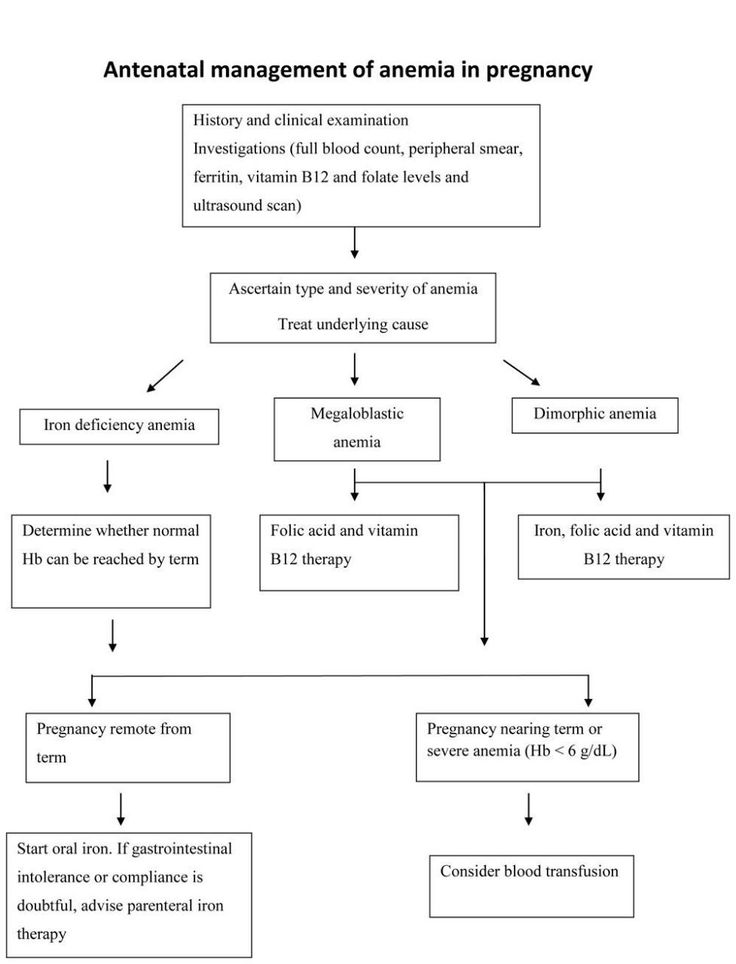 When you have anemia, your blood doesn't have enough healthy red blood cells to carry oxygen to your tissues and to your baby.
When you have anemia, your blood doesn't have enough healthy red blood cells to carry oxygen to your tissues and to your baby.
During pregnancy, your body produces more blood to support the growth of your baby. If you're not getting enough iron or certain other nutrients, your body might not be able to produce the amount of red blood cells it needs to make this additional blood.
It's normal to have mild anemia when you are pregnant. But you may have more severe anemia from low iron or vitamin levels or from other reasons.
Anemia can leave you feeling tired and weak. If it is severe but goes untreated, it can increase your risk of serious complications like preterm delivery.
Here's what you need to know about the causes, symptoms, and treatment of anemia during pregnancy.
Types of Anemia During Pregnancy
Several types of anemia can develop during pregnancy. These include:
- Iron-deficiency anemia
- Folate-deficiency anemia
- Vitamin B12 deficiency
Here's why these types of anemia may develop:
Iron-deficiency anemia.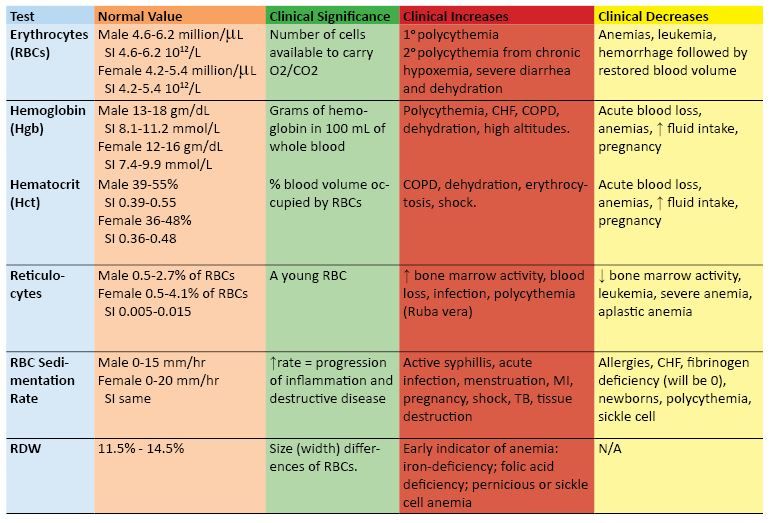 This type of anemia occurs when the body doesn't have enough iron to produce adequate amounts of hemoglobin. That's a protein in red blood cells. It carries oxygen from the lungs to the rest of the body.
This type of anemia occurs when the body doesn't have enough iron to produce adequate amounts of hemoglobin. That's a protein in red blood cells. It carries oxygen from the lungs to the rest of the body.
In iron-deficiency anemia, the blood cannot carry enough oxygen to tissues throughout the body.
Iron deficiency is the most common cause of anemia in pregnancy.
Folate-deficiency anemia. Folate is the vitamin found naturally in certain foods like green leafy vegetables A type of B vitamin, the body needs folate to produce new cells, including healthy red blood cells.
During pregnancy, women need extra folate. But sometimes they don't get enough from their diet. When that happens, the body can't make enough normal red blood cells to transport oxygen to tissues throughout the body. Man made supplements of folate are called folic acid.
Folate deficiency can directly contribute to certain types of birth defects, such as neural tube abnormalities (spina bifida) and low birth weight.
Vitamin B12 deficiency. The body needs vitamin B12 to form healthy red blood cells. When a pregnant woman doesn't get enough vitamin B12 from their diet, their body can't produce enough healthy red blood cells. Women who don't eat meat, poultry, dairy products, and eggs have a greater risk of developing vitamin B12 deficiency, which may contribute to birth defects, such as neural tube abnormalities, and could lead to preterm labor.
Blood loss during and after delivery can also cause anemia.
Risk Factors for Anemia in Pregnancy
All pregnant women are at risk for becoming anemic. That's because they need more iron and folic acid than usual. But the risk is higher if you:
- Are pregnant with multiples (more than one child)
- Have had two pregnancies close together
- Vomit a lot because of morning sickness
- Are a pregnant teenager
- Don't eat enough foods that are rich in iron
- Had anemia before you became pregnant
Symptoms of Anemia During Pregnancy
The most common symptoms of anemia during pregnancy are:
- Pale skin, lips, and nails
- Feeling tired or weak
- Dizziness
- Shortness of breath
- Rapid heartbeat
- Trouble concentrating
In the early stages of anemia, you may not have obvious symptoms.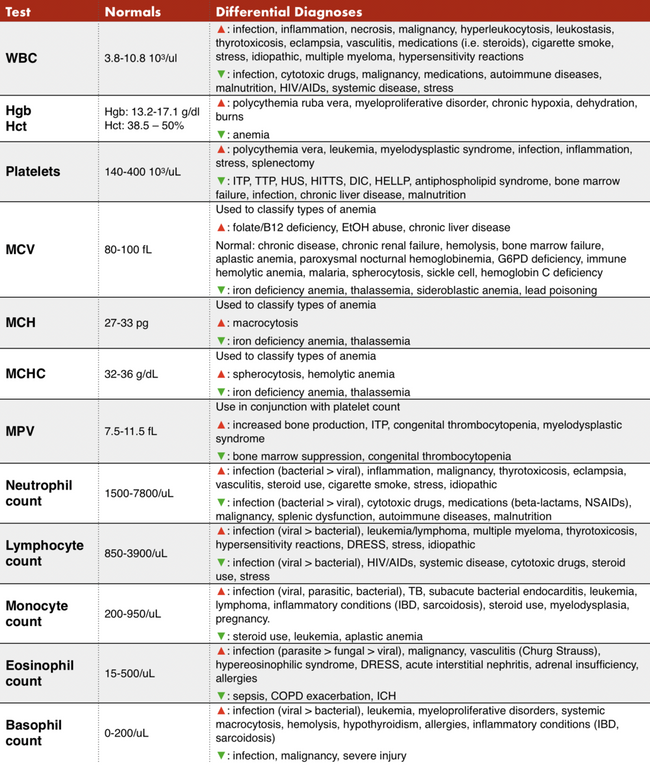 And many of the symptoms are ones that you might have while pregnant even if you're not anemic. So be sure to get routine blood tests to check for anemia at your prenatal appointments.
And many of the symptoms are ones that you might have while pregnant even if you're not anemic. So be sure to get routine blood tests to check for anemia at your prenatal appointments.
Risks of Anemia in Pregnancy
Severe or untreated iron-deficiency anemia during pregnancy can increase your risk of having:
- A preterm or low-birth-weight baby
- A blood transfusion (if you lose a significant amount of blood during delivery)
- Postpartum depression
- A baby with anemia
- A child with developmental delays
Untreated folate deficiency can increase your risk of having a:
- Preterm or low-birth-weight baby
- Baby with a serious birth defect of the spine or brain (neural tube defects)
Untreated vitamin B12 deficiency can also raise your risk of having a baby with neural tube defects.
Tests for Anemia
During your first prenatal appointment, you'll get a blood test so your doctor can check whether you have anemia.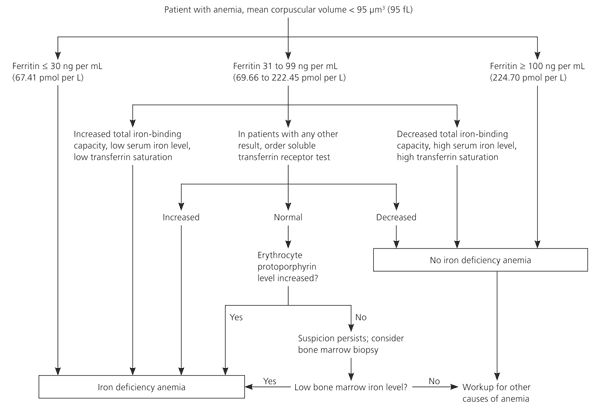 Blood tests typically include:
Blood tests typically include:
- Hemoglobin test. It measures the amount of hemoglobin -- an iron-rich protein in red blood cells that carries oxygen from the lungs to tissues in the body.
- Hematocrit test. It measures the percentage of red blood cells in a sample of blood.
If you have lower than normal levels of hemoglobin or hematocrit, you may have iron-deficiency anemia. Your doctor may check other blood tests to determine if you have iron deficiency or another cause for your anemia.
Even if you don't have anemia at the beginning of your pregnancy, your doctor will most likely recommend that you get another blood test to check for anemia in your second or third trimester.
Treatment for Anemia
If you are anemic during your pregnancy, you may need to start taking an iron supplement and/or folic acid supplement in addition to your prenatal vitamins. Your doctor may also suggest that you add more foods that are high in iron and folic acid to your diet.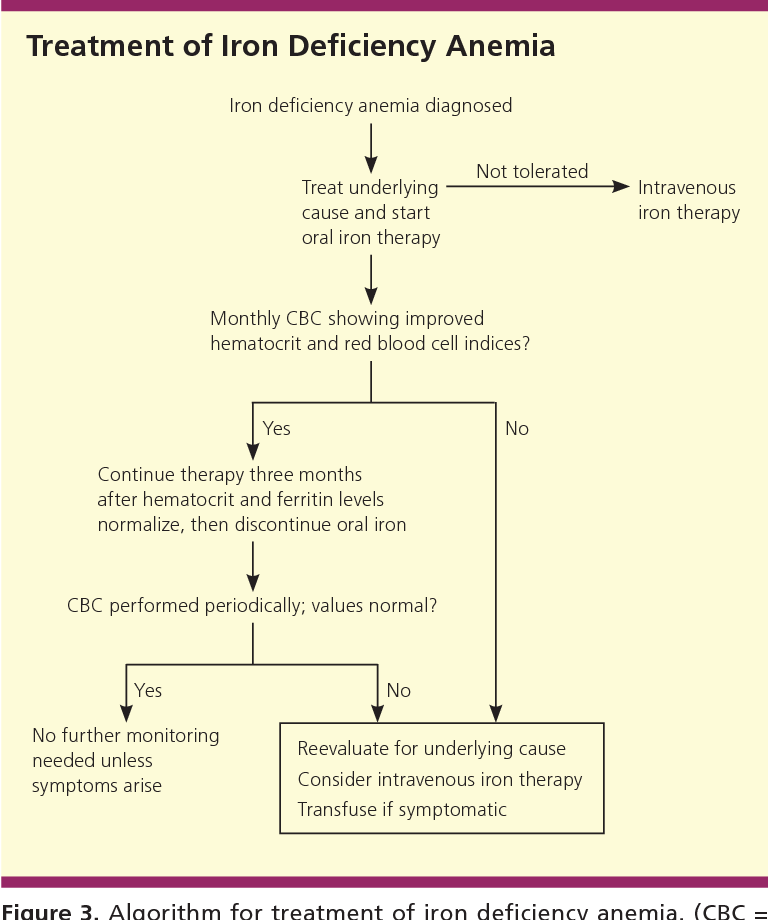
In addition, you'll be asked to return for another blood test after a specific period of time so your doctor can check that your hemoglobin and hematocrit levels are improving.
To treat vitamin B12 deficiency, your doctor may recommend that you take a vitamin B12 supplement.
The doctor may also recommend that you include more animal foods in your diet, such as:
- meat
- eggs
- dairy products
Your OB may refer you to a hematologist, a doctor who specializes in anemia/ blood issues. The specialist may see you throughout the pregnancy and help your OB manage the anemia.
Preventing Anemia
To prevent anemia during pregnancy, make sure you get enough iron. Eat well-balanced meals and add more foods that are high in iron to your diet.
Aim for at least three servings a day of iron-rich foods, such as:
- lean red meat, poultry, and fish
- leafy, dark green vegetables (such as spinach, broccoli, and kale)
- iron-enriched cereals and grains
- beans, lentils, and tofu
- nuts and seeds
- eggs
Foods that are high in vitamin C can help your body absorb more iron.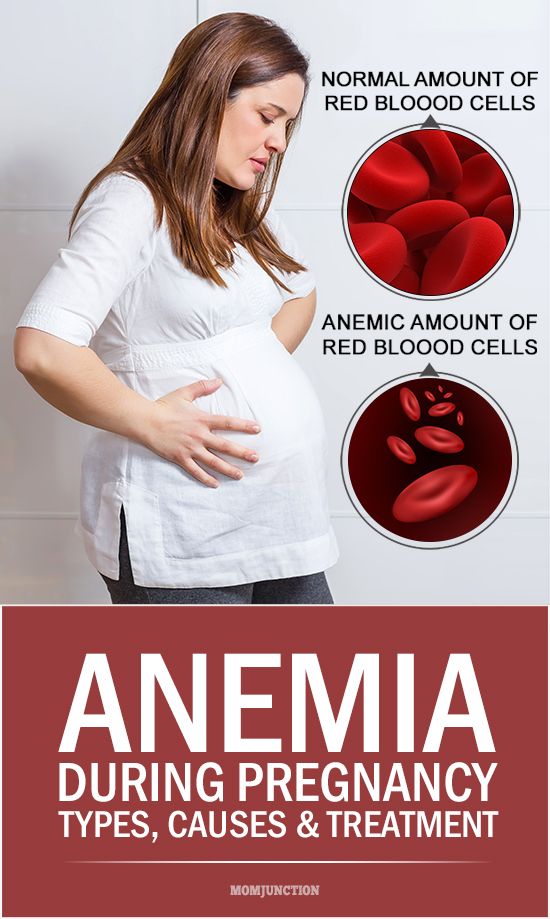 These include:
These include:
- citrus fruits and juices
- strawberries
- kiwis
- tomatoes
- bell peppers
Try eating those foods at the same time that you eat iron-rich foods. For example, you could drink a glass of orange juice and eat an iron-fortified cereal for breakfast.
Also, choose foods that are high in folate to help prevent folate deficiency. These include:
- leafy green vegetables
- citrus fruits and juices
- dried beans
- breads and cereals fortified with folic acid
Follow your doctor's instructions for taking a prenatal vitamin that contains a sufficient amount of iron and folic acid.
Vegetarians and vegans should talk with their doctor about whether they should take a vitamin B12 supplement when they're pregnant and breastfeeding.
Health & Pregnancy Guide
- Getting Pregnant
- First Trimester
- Second Trimester
- Third Trimester
- Labor and Delivery
- Pregnancy Complications
- All Guide Topics
Iron deficiency anemia during pregnancy KHEIDAR, assistant of the Department of Obstetrics and Gynecology, Moscow Faculty of the Russian State Medical University, doctor of the highest category, candidate of medical sciences; E.
 A. BOYAR, Assistant of the Department of Obstetrics and Gynecology, Moscow Faculty of the Russian State Medical University, doctor of the highest category, Candidate of Medical Sciences
A. BOYAR, Assistant of the Department of Obstetrics and Gynecology, Moscow Faculty of the Russian State Medical University, doctor of the highest category, Candidate of Medical Sciences Disease of every fourth inhabitant of the Earth
Iron deficiency anemia is one of the most common human diseases, affecting about 25% of the world's population. Iron deficiency anemia (IDA) is characterized by a lack of iron in the body, which is necessary for the construction of the hemoglobin molecule, in particular, its iron-containing part - heme.
The relevance of the problem of IDA in pregnant women is associated with its significant prevalence during pregnancy (from 21 to 80%) and adverse effects on the course of pregnancy, childbirth, the postpartum period, as well as on the development of fetal and newborn pathology.
According to world medical statistics, the prevalence of anemia during pregnancy in developing countries ranges from 35 to 56% in Africa, from 37 to 75% in Asia, and from 37 to 52% in Latin America.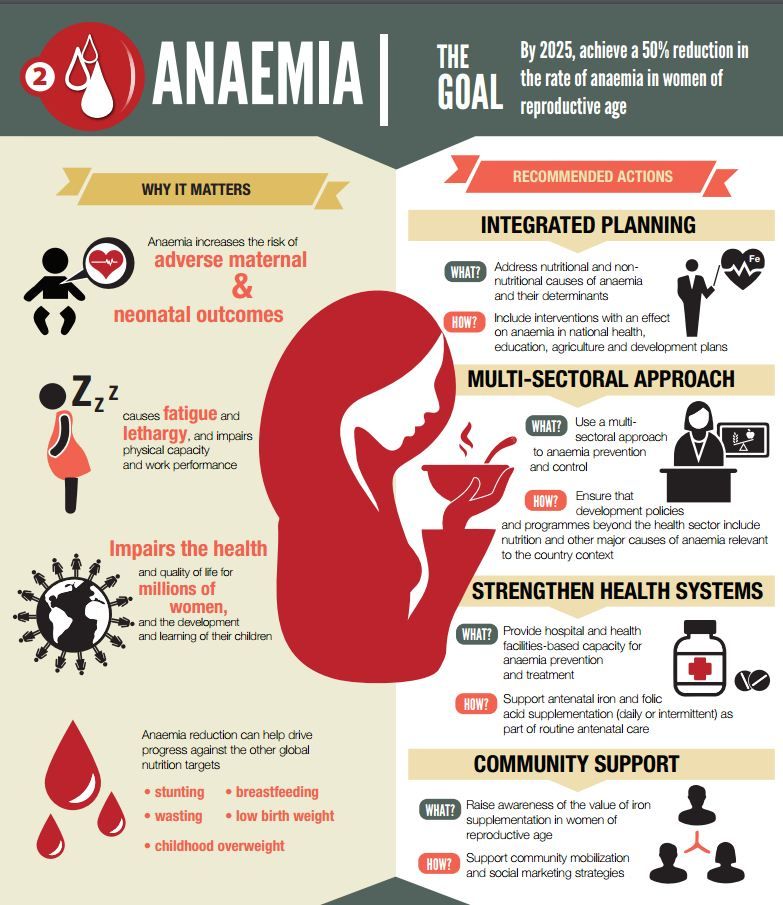 It is assumed that the most common etiological factor of this disease is iron and folic acid deficiency. It has been established that in 20% of pregnant women the hemoglobin level does not exceed 80 g/l, and in 2-7% of patients this indicator is not more than 70 g/l.
It is assumed that the most common etiological factor of this disease is iron and folic acid deficiency. It has been established that in 20% of pregnant women the hemoglobin level does not exceed 80 g/l, and in 2-7% of patients this indicator is not more than 70 g/l.
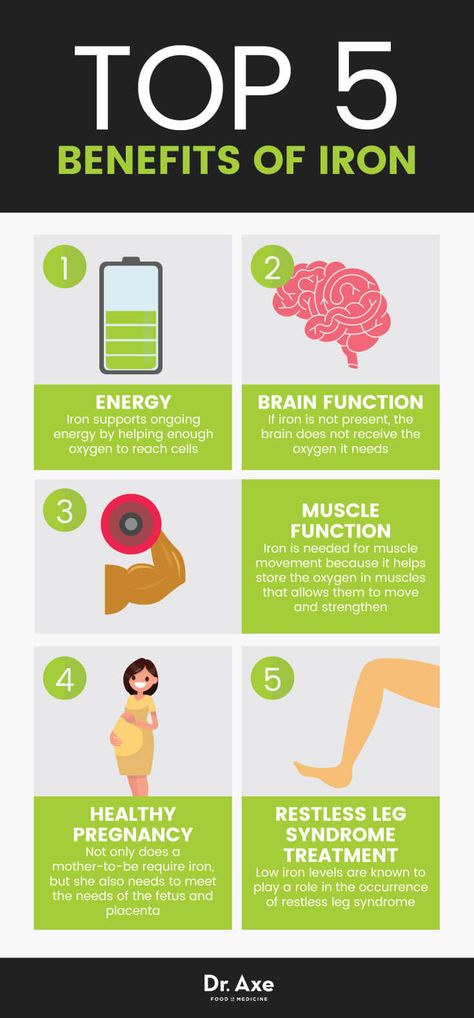
Iron deficiency during pregnancy is associated with an increase in the woman's need for iron. The daily requirement for iron during pregnancy increases and is: in the first trimester 0.6-0.8 mg / day, in the second trimester - 2.8-3 mg / day, in the third trimester - 3.5-4 mg / day This is due to the costs of the development of the placenta and fetus, the formation of an additional globular volume, accompanied by increased erythropoiesis, costs for the growing uterus and other needs.
Anemia is not only widespread in these countries in women during pregnancy, but also very common as a severe form of an independent disease. According to WHO, in industrialized countries, the average prevalence of this pathology is 18%.
How to diagnose anemia?
The main criteria for iron deficiency anemia are: a decrease in the level of hemoglobin (Hb), a color indicator that reflects the content of Hb in the erythrocyte. Morphologically, erythrocyte hypochromia, microcytosis, anisocytosis and poikilocytosis are determined. The content of reticulocytes in the blood is usually within the normal range.
There are several classifications of anemia based on etiological, pathogenetic and hematological features. In practice, the severity of the clinical course of anemia is usually determined by the level of hemoglobin in the peripheral blood, and the following classification of IDA is more often used:
- mild degree (Hb from 90 to 109 g/l)
- moderate (Hb 70 to 89 g/l)
- severe (Hb less than 70 g/l).
WHO experts consider Hb level to be anemia in pregnant women
The clinical picture of iron deficiency anemia depends on the severity of iron deficiency.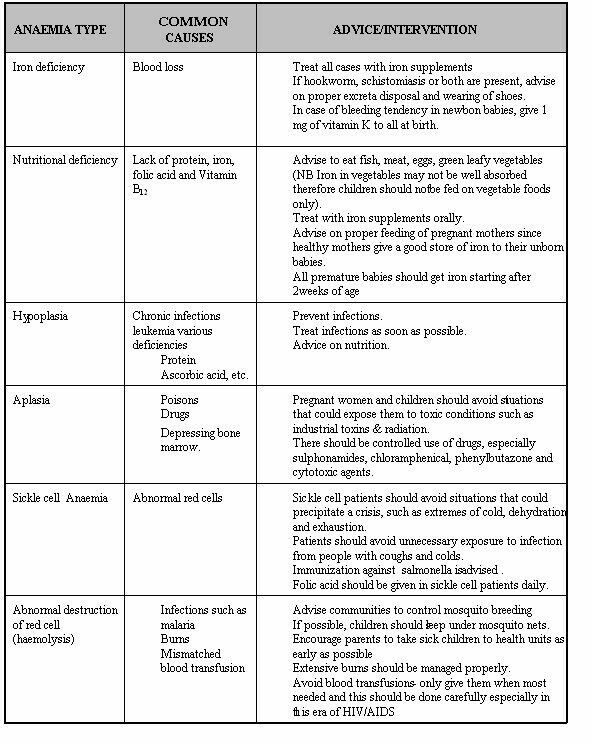 With a mild degree of IDA, clinical symptoms are usually absent and laboratory parameters are objective signs. Clinical symptoms appear, as a rule, with moderate anemia. As iron deficiency increases, weakness, dizziness, headache, palpitations, shortness of breath, fainting, decreased performance, and insomnia appear. These symptoms are not specific to iron deficiency anemia and may occur in anemia of other etiologies.
With a mild degree of IDA, clinical symptoms are usually absent and laboratory parameters are objective signs. Clinical symptoms appear, as a rule, with moderate anemia. As iron deficiency increases, weakness, dizziness, headache, palpitations, shortness of breath, fainting, decreased performance, and insomnia appear. These symptoms are not specific to iron deficiency anemia and may occur in anemia of other etiologies.
Dietary and drug therapy
Considering the important role of iron in the pathogenesis of iron deficiency anemia during pregnancy, it is necessary to follow the basic principles of dietary therapy. When choosing a diet, one should focus not on the amount of iron in the product, but on the form in which it is presented. It is the form that determines the percentage of absorption and assimilation of iron, therefore, the effectiveness of diet therapy. Iron is absorbed most effectively from foods where it is contained in the form of heme, when it is actively captured and absorbed by the cells of the intestinal mucosa in unchanged form (beef, beef tongue, rabbit meat, turkey, chicken).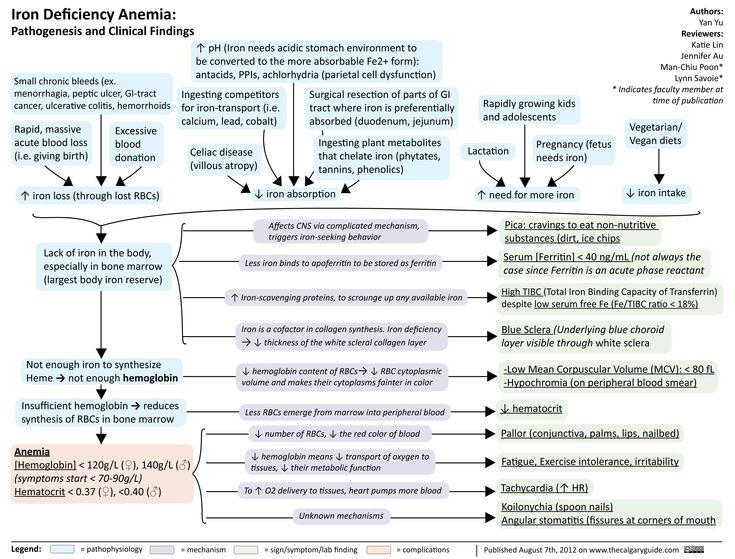
The incidence of anemia in pregnant women with epilepsy does not exceed the general population, but such cases require careful correction in order to reduce very serious obstetric complications. Epilepsy is a chronic brain disorder characterized by recurrent seizures that result from excessive neural activity. Epilepsy is one of the most common diseases of the nervous system and a significant medical and social problem.
The processes of heme absorption in the intestine do not depend on the acidity of the environment and inhibitory nutrients. In cereals, fruits and vegetables, iron is in non-heme form and absorption from them is much worse. The presence of oxalates, phosphates, tannin and other inhibitors of ferroabsorption also contributes to a decrease in absorption. It should be noted that meat, liver, fish, ascorbic acid, as well as substances that lower the pH of food (for example, lactic acid) increase the absorption of iron from vegetables and fruits while consuming them.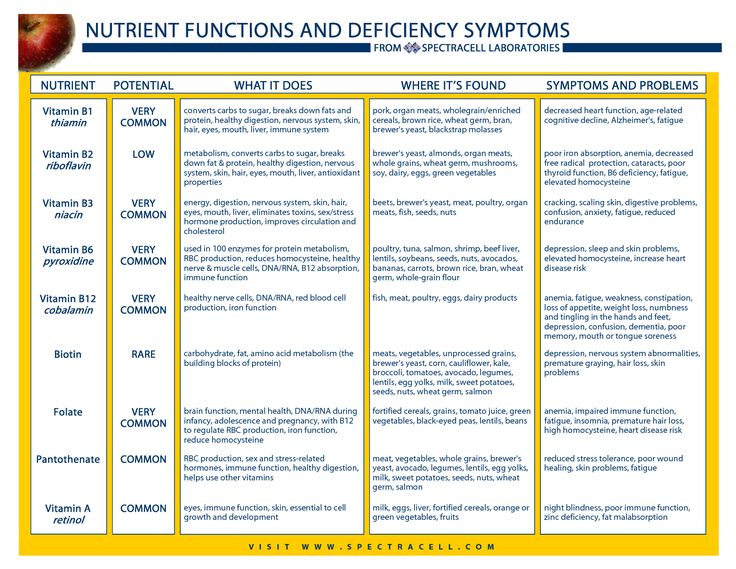 A complete and balanced diet in terms of the main ingredients only allows you to "cover" the body's physiological need for iron, but not eliminate its deficiency, and should be considered as one of the auxiliary components of therapy.
A complete and balanced diet in terms of the main ingredients only allows you to "cover" the body's physiological need for iron, but not eliminate its deficiency, and should be considered as one of the auxiliary components of therapy.
The traditional treatment for iron deficiency anemia in pregnancy is the use of oral iron supplements. Currently, oral ferropreparations are divided into two main groups: ionic - these are salts of ferrous iron (ferro-foilgamma, ferretab, sorbifer durules, actiferrin, tardiferron, totem, ferroplex, fenules, etc.) and non-ionic - represented by a protein and hydroxide-polymaltose complex ferric iron (maltofer, ferrum lek, ferlatum).
Benefits of generic drugs
In our practice, we prefer to prescribe ferro-foilgamma to pregnant patients with IDA, which is universal in terms of its pharmacological effects and spectrum of clinical effects. It contains: ferrous sulfate 100 mg, incl. iron (Fe2+) 37 mg, cyanocobalamin 10 mcg, folic acid 5 mg, ascorbic acid 100 mg.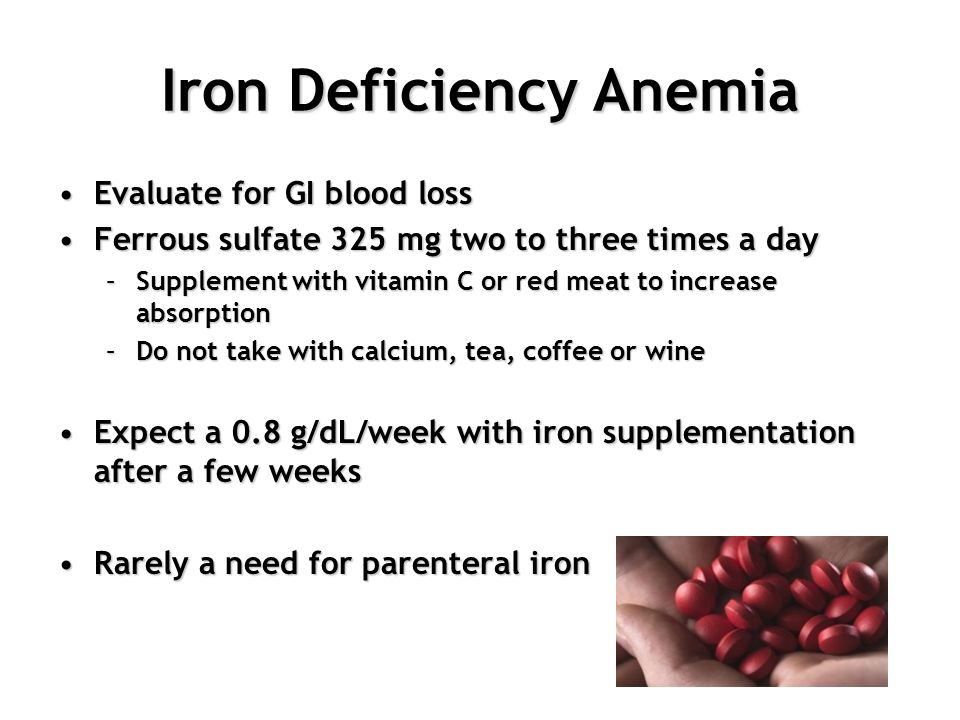
Ferro-foil gamma is a multifactorial hematopoietic agent that includes all the necessary components that stimulate the structural synthesis of hemoglobin and increase the reproduction of erythrocytes by the red growth of the bone marrow. The universality of the pharmacological effects of the drug is associated with its selective stimulating effect on the synthesis of not only the iron-containing, but also the protein parts of hemoglobin.
Changes in the skin, nails, hair, muscle weakness corresponding to the degree of anemia, taste perversion can be considered pathognomonic for IDA.
Thus, ferrous sulfate practically does not form inaccessible complex compounds in the gastrointestinal tract and has a high absorption coefficient. The active components of the ferro-foil gamma preparation are in a special neutral shell, which ensures their absorption, mainly in the upper part of the small intestine. The absorption coefficient is greatly enhanced by the presence of ascorbic acid in the preparation.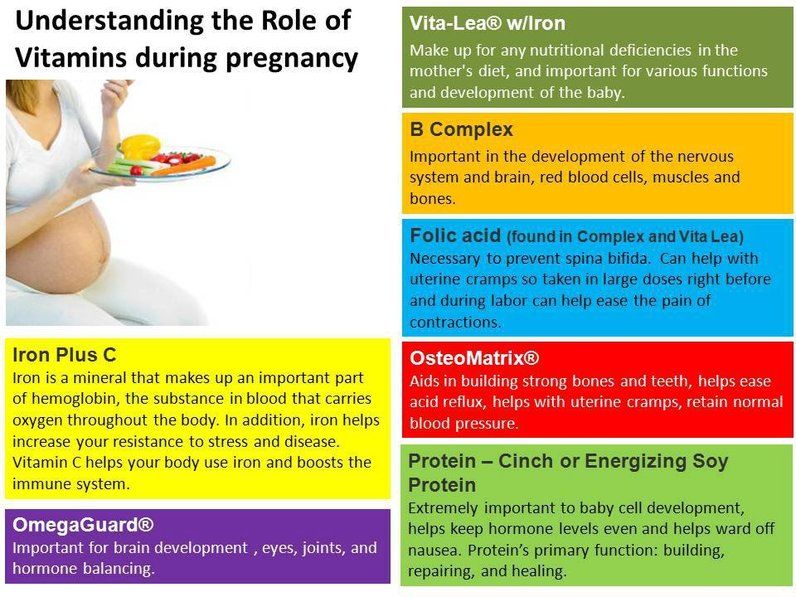
Ferro-foil was successfully used to treat anemia in various obstetric and gynecological pathologies: patients with uterine bleeding of various etiologies, preeclampsia in combination with anemia, placental insufficiency and chronic fetal hypoxia.
It is also important to emphasize that the ferro-foil gamma drug is also effective in cases of combination of pregnancy with other pathologies, and quite dangerous ones at that. In particular, we used the drug to treat anemia in pregnant women with epilepsy in the second half of pregnancy. The drug was prescribed 1 capsule 3 times a day before meals. The duration of therapy was 1 month. During the treatment, side effects, such as allergic reactions, gastrointestinal disorders, were not observed, since the presence of a special shell ensures the absorption of the drug from the intestines, which significantly improves its tolerability.
With a long course of anemia or in the absence of the effect of its treatment, despite a moderate decrease in hemoglobin, the function of the placenta is disturbed, placental insufficiency develops, which in case of anemia is caused by a sharp decrease in the level of iron not only in the maternal blood, but also in the placenta.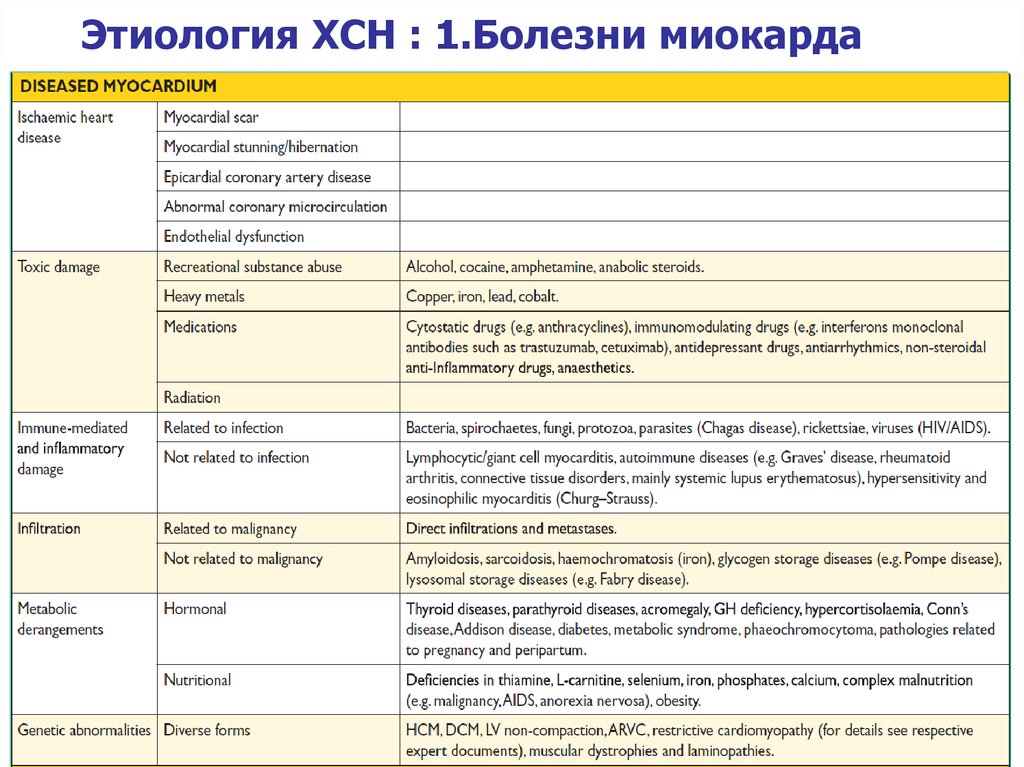 This leads to a violation of the activity of respiratory enzymes in the syncytiotrophoblast and a decrease in the transport of iron to the fetus. When anemia is combined with another pathology of pregnancy, not only gas exchange is disturbed, but also the nutritional function of the placenta.
This leads to a violation of the activity of respiratory enzymes in the syncytiotrophoblast and a decrease in the transport of iron to the fetus. When anemia is combined with another pathology of pregnancy, not only gas exchange is disturbed, but also the nutritional function of the placenta.
Against the background of ongoing therapy, after 10 days, the number of erythrocytes and the hematocrit value did not change significantly, the hemoglobin content slightly increased. After the full course of treatment, there was a significant increase in hemoglobin content compared to the initial data, on average, by almost 22%. In pregnant women, against the background of the therapy, an improvement in general well-being was observed, sleep and mood improved, and fatigue decreased. The use of ferro-foil in prophylactic doses can reduce the development of anemia after childbirth, especially after a caesarean section. For pregnant women with epilepsy, the presence of folic acid and cyanocobalamin in the preparation is unique, as it reduces the risk of developing neural tube defects in the fetus in this contingent of women.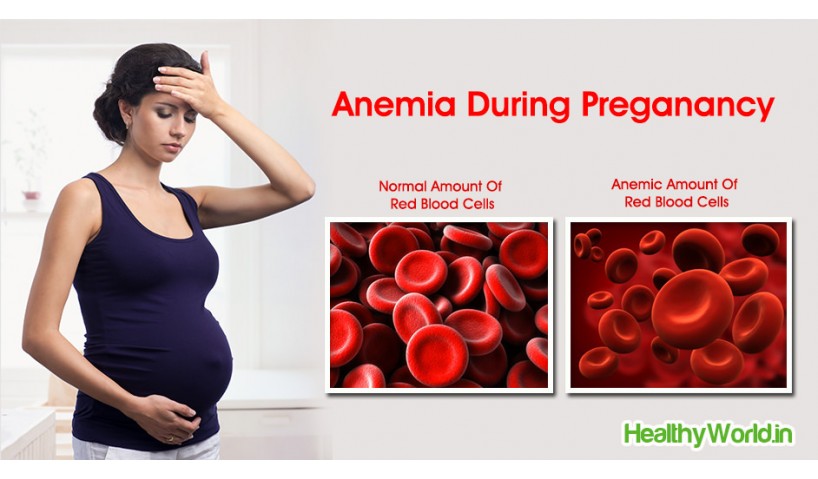
Anemia is a high risk for mother and fetus!
The group of increased risk of developing iron deficiency anemia includes pregnant women with a history of anemia, the presence of foci of chronic infection, chronic diseases of the gastrointestinal tract, exposed to adverse chemical factors, multiple births, with pregnancy characterized by multiple pregnancies, vomiting, repeated bleeding, especially when placenta previa.
The presence of IDA during pregnancy is associated with significant risk to both mother and fetus. An increase in the severity of anemia is accompanied by a more frequent development of severe forms of preeclampsia, pyelonephritis, and bleeding during childbirth in a pregnant woman. In addition, the risk of preterm birth, placental insufficiency and intrauterine fetal death increases.
In accordance with WHO recommendations, women during pregnancy should be prevented from iron deficiency anemia (at a dose of 50 mg / day), and in the presence of iron deficiency anemia (Hb
Anemia during pregnancy - iron arguments and dispelling myths
Anemia is one of the most common complications that occur during pregnancy.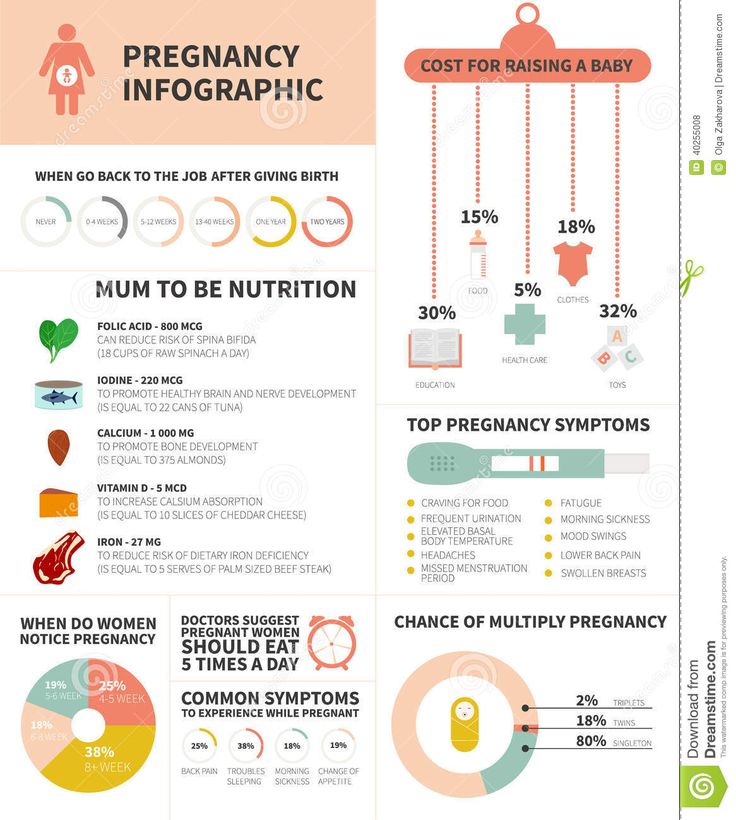 In Russia, this diagnosis is made to every third pregnant woman. However, not everyone, faced with this diagnosis, understands what is at stake and what needs to be done in order for the treatment to be as effective as possible.
In Russia, this diagnosis is made to every third pregnant woman. However, not everyone, faced with this diagnosis, understands what is at stake and what needs to be done in order for the treatment to be as effective as possible.
Anemia is a disease in which the level of hemoglobin in the blood decreases, often with a simultaneous decrease in the number of red blood cells. The main reason for the development of anemia is the discrepancy between the intake of iron in the body and its costs.
During pregnancy, the cost of the growing fetus causes a significant increase in iron requirements. In addition, a less common but possible cause of anemia may be insufficient intake of folic acid or vitamin B12.
Risk factors for developing iron deficiency anemia during pregnancy include:
- history of heavy menses;
- diseases of the gastrointestinal tract;
- infectious and inflammatory diseases;
- anemia in the past;
- short interval between pregnancies, including conception during lactation;
- multiple pregnancy.
Since the main task of hemoglobin is to deliver oxygen - a vital element - to all tissues and cells of a woman and fetus, it is easy to imagine the harm caused by its decrease during pregnancy. However, even after childbirth, the issue cannot be considered closed. It has been proven that a low level of hemoglobin is associated with a decrease in lactation, as well as with the development of anemia in a child.
Iron deficiency anemia is manifested by weakness, dizziness, pathological fatigue, perverted perception of tastes and smells, heart palpitations, shortness of breath, headache, fainting. The skin becomes dry and pale, and the hair and nails brittle.
The diagnosis of anemia is made based on the assessment of hemoglobin levels in the complete blood count. The lower limit of the hemoglobin norm during pregnancy is 110 g / l. However, before hemoglobin decreases, iron stores are depleted, which is manifested by a decrease in serum ferritin levels.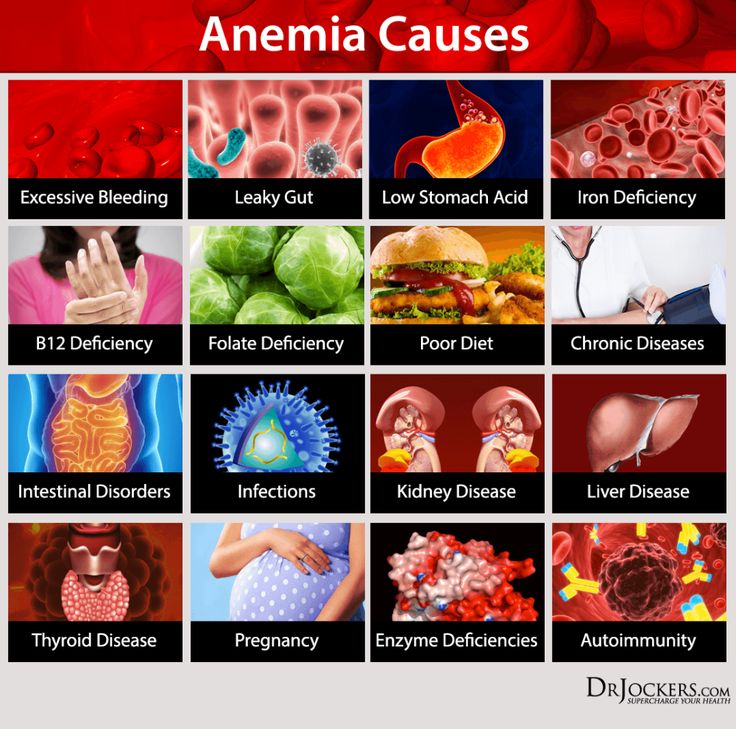 This condition is called latent iron deficiency and also requires correction.
This condition is called latent iron deficiency and also requires correction.
Treatment of anemia and latent iron deficiency is with iron supplements, most commonly given as tablets or oral solution, but sometimes intravenous solutions are used. This need arises when the hemoglobin level is very low or in case of impaired absorption of iron from the gastrointestinal tract.
It is also important to be aware of the potential of a protein diet in correcting iron deficiency. Since hemoglobin is a bond between two subunits - metal-containing heme and globin protein - then with insufficient protein intake, even an adequate amount of iron in the body has nothing to contact.
When diagnosing anemia, it is important for the patient to remember that the consumption of foods high in iron will only help maintain the existing hemoglobin level, but will not be able to increase its level and saturate iron stores to a sufficient extent.
Separately, I would like to dwell on what kind of products the iron content is really high.