Flu like symptoms end of pregnancy
Flu and pregnancy: How it affects you and your baby
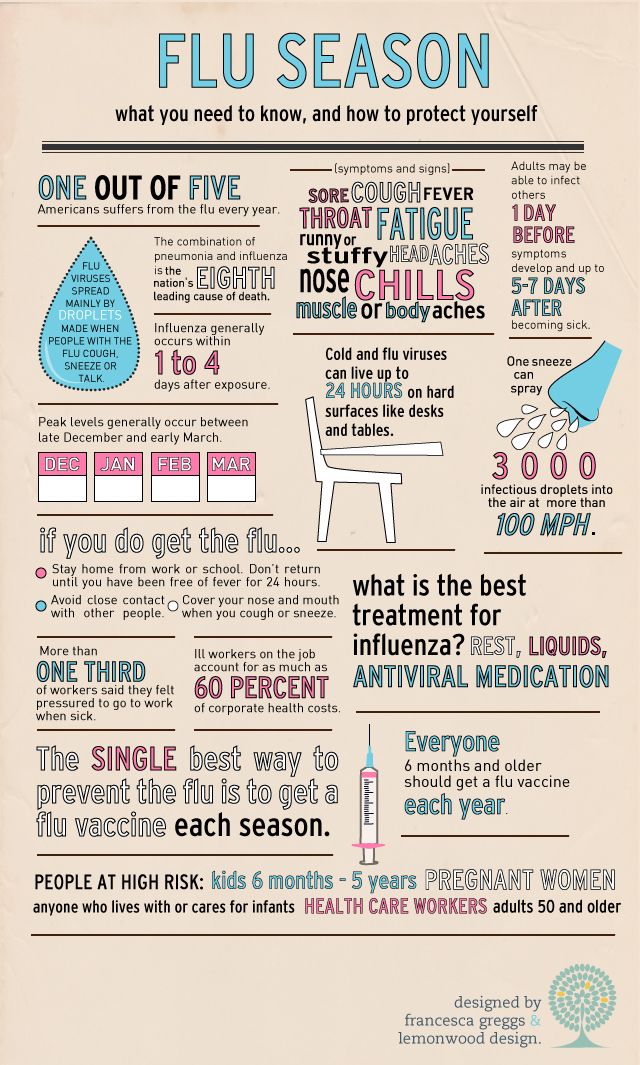
Most pregnant women who get the flu will recover normally and go on to have healthy pregnancies and babies. But you're at higher risk of catching the flu and having complications from the flu if you're pregnant. Early treatment is key, so if you think you have the flu during pregnancy, reach out to your healthcare provider. To lower your risk of getting the flu, it's important to get vaccinated each year.
Is getting the flu during pregnancy dangerous?
It can be. Many moms-to-be who become sick with the flu have no pregnancy complications. But statistically, you're more likely to develop a severe case of the flu when you're pregnant.
Why? During pregnancy, your body naturally reduces its ability to protect you from illness, so that your immune system won't see your baby as a threat to the system. Your heart and lungs are also working harder to supply blood and oxygen to both of you. What's more, your lungs have to function in a smaller space due to pressure from your growing baby. All of this puts stress on your body, making you more vulnerable to getting viruses and illnesses in general – and that includes the flu.
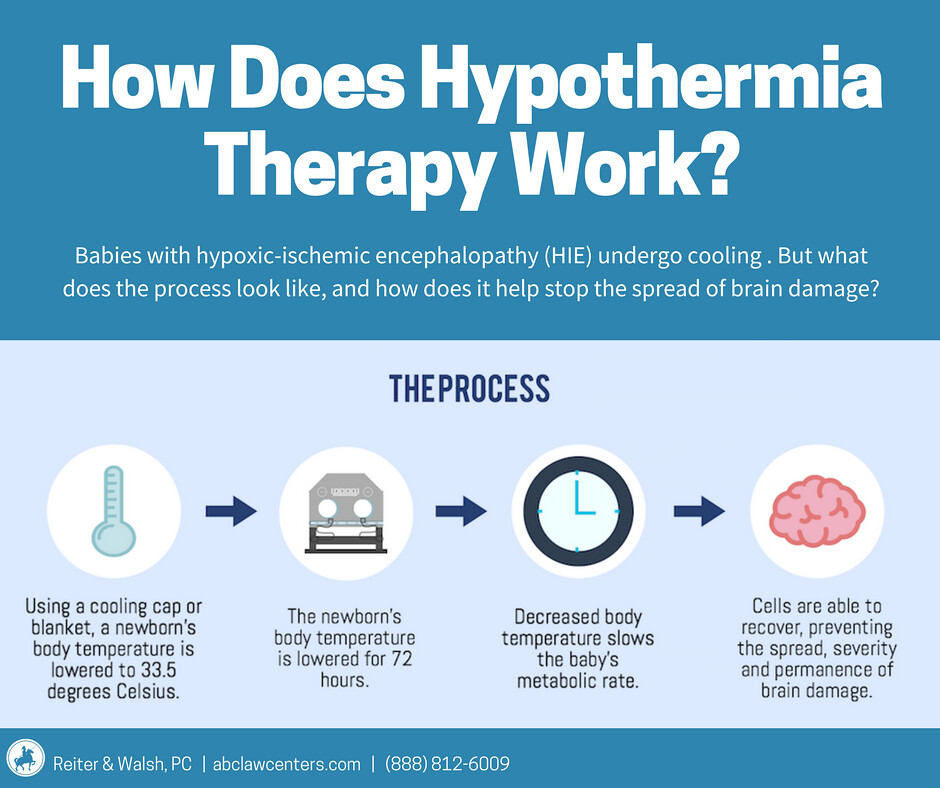
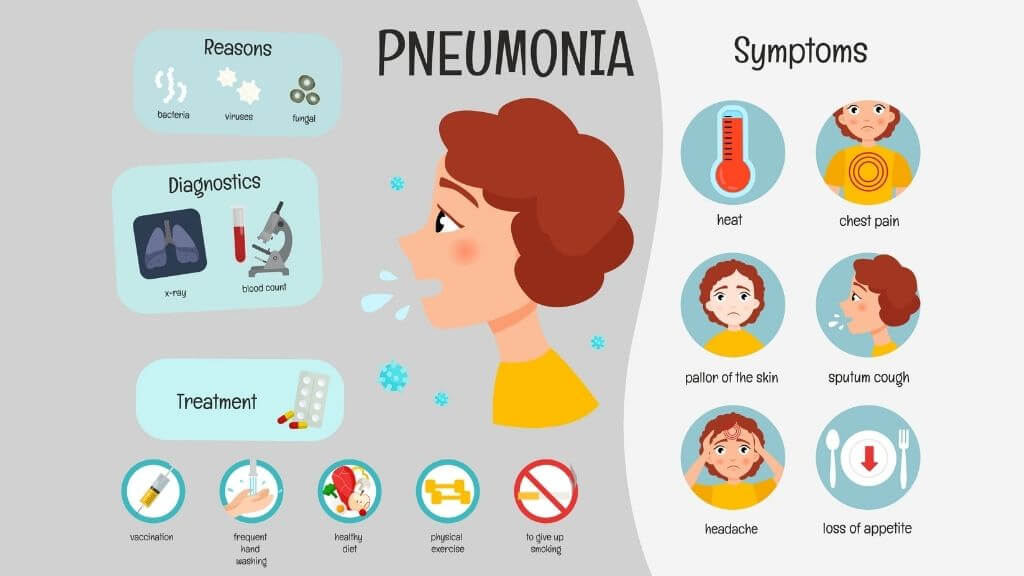
If you get the flu while pregnant, you have an increased chance of serious complications that could require hospitalization – and the odds are even higher if you have other underlying health conditions. The greatest concern is pneumonia, a potentially life-threatening lung infection. Your baby is also at higher risk of being born prematurely, and being small with low birth weight.
Flu symptoms during pregnancy
If you get the flu during pregnancy, you'll likely have the same symptoms as women who aren't pregnant.
Flu symptoms typically come on suddenly – and often make it feel like you've been hit by a bus. Symptoms of the flu usually include fever, achiness, fatigue, and headache, along with a runny or stuffy nose, sore throat, coughing, and chills. You may begin vomiting or have diarrhea, as well. Call your healthcare provider if you develop any of these symptoms, so they can decide whether you need a flu test to confirm, and also if you need treatment.
Call 911 and get emergency medical help immediately if you notice any of the following:
- Problems breathing or shortness of breath
- A fever or cough that improves, but then returns or worsens
- Persistent pain or pressure in your chest or abdomen
- Persistent dizziness, confusion, drowsiness, or lethargy
- Severe or persistent vomiting
- Less fetal movement
- A high fever that doesn't respond to acetaminophen
- Seizures
- Severe weakness or unsteadiness
- An inability to urinate
- Severe muscle pain
Check with your provider immediately if you have any other severe or concerning symptoms that aren't included on this list.
What's the difference between COVID-19 and the flu?
Like the flu, COVID-19 is a contagious and life-threatening respiratory disease often spread through close contact with someone who is infected. Pregnant women are at higher risk for both the flu and COVID.
Advertisement | page continues below
The flu and COVID-19 have similar symptoms, including fever, cough, fatigue, runny nose, breathing problems, and vomiting. Both conditions can cause you to lose your sense of smell and/or taste, though this seems to be more common in people with COVID-19.
There are some key differences, however, between the two diseases:
- flu symptoms usually arise within four days of being infected, while COVID-19 symptoms can take up to 14 days to appear.
- COVID-19 appears to spread more easily than the flu and remains contagious for a longer time.
- You're more likely to become severely ill with COVID-19 compared to the flu.
Hands down, the best way to protect yourself from COVID-19 when you're pregnant is by being fully vaccinated against the disease. The shot series and booster shots are safe during pregnancy and could help protect your baby from COVID as well. If you haven't had your vaccine already, reach out to your provider with any questions and make an appointment.
How is the flu treated in pregnancy?
Getting early treatment for the flu is important for both you and your baby it can prevent serious illness and complications. If you're pregnant and develop symptoms – or even if you come in close contact with a person who has the flu – call your provider right away.
Your provider will let you know whether you should go in for testing or treatment with an antiviral medication. Some providers will prescribe treatment over the phone or through online telemedicine portals. If you need to visit the office in person, your tests may include a nasal swab; it's best done within the first two days of noticing symptoms.
In the meantime, try the following to ease symptoms:
- Drink plenty of fluids.
- If you don't have an appetite, try eating small meals anyway to maintain your nutritional intake.
- Get lots of rest.
- If you're in the early stages of your pregnancy (first trimester), treat your temperature with acetaminophen.
 Fever in early pregnancy is linked to neural tube defects in newborns, so it's important to treat fevers as soon as possible.
Fever in early pregnancy is linked to neural tube defects in newborns, so it's important to treat fevers as soon as possible. - If you can, have your spouse – or a friend or family member – around to help you so you can get the rest you need.
To avoid spreading the flu, keep your distance from others while you're sick. Keep in mind that people with the flu are contagious starting the day before they notice symptoms, and they remain so for about a week.
Is it safe to take antiviral medicines like Tamiflu during pregnancy?
Yes. Oseltamivir (Tamiflu) and zanamivir (Relenza) are oral antiviral medications often recommended to expectant women. They're considered to be safe and effective during pregnancy.
Antivirals can ease your symptoms, help you feel better sooner, and prevent serious flu complications such as pneumonia. They work best when you start them within two days of noticing symptoms, but you can take them after that point, as well.
Sometimes a provider will prescribe an antiviral medication to reduce the chances you'll get sick.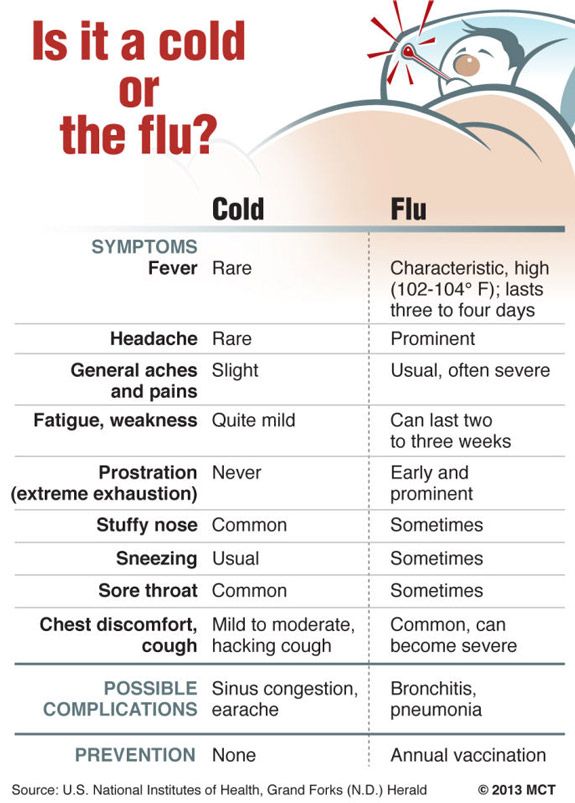 Or, your provider might decide that antivirals aren't needed unless you actually develop symptoms.
Or, your provider might decide that antivirals aren't needed unless you actually develop symptoms.
If antivirals are prescribed, you'll take them for five days – and you'll remain contagious most of this time. Taking the medicine with food may help prevent nausea and vomiting, the most common side effects of Tamiflu. (Nausea and vomiting can also be symptoms of both the flu and pregnancy, of course.)
Note: Tamiflu is not the same as Theraflu. Tamiflu is a prescription medication. Theraflu is the brand name of an over-the-counter medicine that contains a pain reliever and other ingredients. It may soothe some symptoms temporarily, but it won't stop the flu's progress. Speak with your provider first if you're pregnant and considering taking Theraflu, especially because Theraflu contains alcohol.
The flu shot and pregnancy: Is it safe?
Yes. The flu shot has been proven safe and effective for women and their developing babies at all stages of pregnancy, including the first trimester.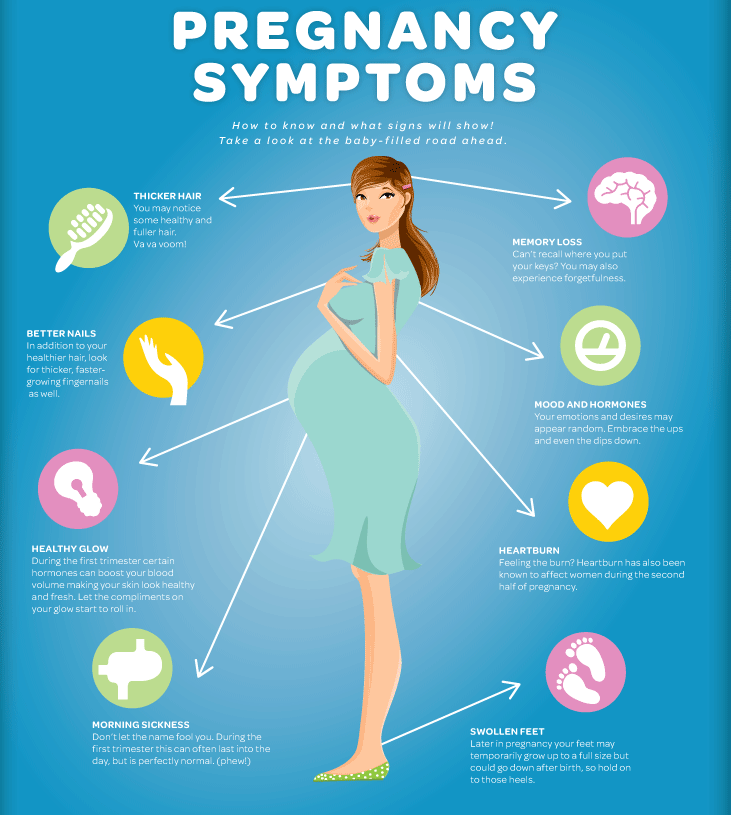 It will not infect you or your baby with the flu.
It will not infect you or your baby with the flu.
Not only is being vaccinated safe during pregnancy; it's strongly recommended. The American College of Obstetricians and Gynecologists calls the shot “an essential element of pre-pregnancy, prenatal, and postpartum care.” It significantly lowers your chances of developing severe flu symptoms and protects your baby from harm.
Whether you're pregnant or not, keep in mind you need a new flu shot annually, since different strains of the disease pop up each year. It's best to be vaccinated as soon as the shot is available in the fall, preferably by the end of October. It takes a few weeks for immunity to develop after vaccination, so you'll be protected before flu season begins to surge. It's important to get any vaccinations your provider recommends to you during your pregnancy.
What are some other ways I can lower my risk of getting the flu in pregnancy?
Though there's no failsafe way of preventing the flu while you're pregnant, you can greatly reduce your odds by taking some key steps.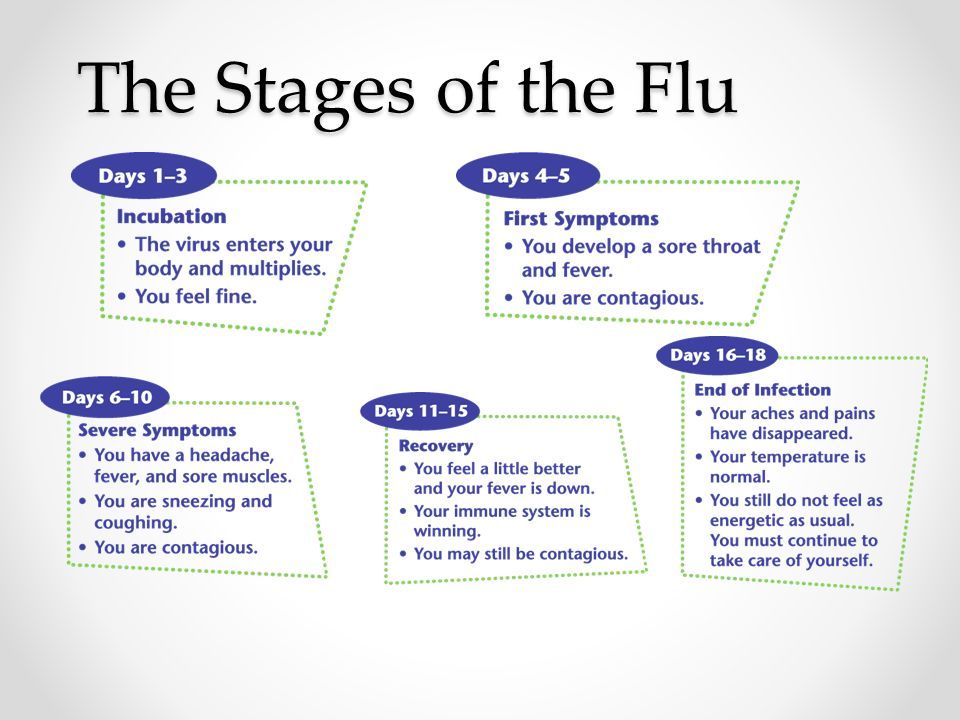
Get a flu shot ASAP each autumn. Even if you miss that fall window, it's still worth getting the shot as late as March, since flu activity can continue through May. Bonus: You'll help protect your infant from the flu for as long as six months after birth, too.
Wash your hands frequently. Always clean them at the following times:
- Before, during, and after food preparation
- Before and after eating
- Whenever you're caring for someone who is sick
- When you're treating a wound
- After sneezing, coughing, or blowing your nose
- After using the bathroom, changing a diaper, or cleaning a child who's used the bathroom
- After touching an animal, animal food, or animal waste
- After touching trash
Use proper hand-washing techniques. Spend at least 20 seconds scrubbing with soap and water, and make sure to get the backs of your hands, in between your fingers, and under your nails. If soap and water aren't available, use disposable hand wipes or alcohol-based gel sanitizers that contain at least 60 percent alcohol.
If soap and water aren't available, use disposable hand wipes or alcohol-based gel sanitizers that contain at least 60 percent alcohol.
Don't cough or sneeze into your bare hands. Instead, cover your mouth with your arm and cough or sneeze into your sleeve. Or, use a disposable tissue and throw it away afterward. Many experts recommend the sleeve method over a tissue because handling a tissue can still contaminate your hands. If you do end up using your bare hands, wash them right away.
Don't touch your eyes, nose, or mouth. You may think your hands are clean, but if you touch a doorknob, cup, refrigerator handle, or any other contaminated item, your hands can carry the virus and infect you.
Regularly wipe down surfaces at home. Disinfect high-touch surfaces such as toys, bedside tables, doorknobs, telephones, and bathroom and kitchen counters. Viruses and bacteria can live on certain surfaces for up to 48 hours, according to the CDC.
Stay away from people who are sick. This includes coworkers, friends, family, and people living in your home.
Reach out to your provider if you're exposed to or suspect you have the flu. Even if you don't yet have a positive flu test, you may be advised to start an antiviral medication.
Flu Like Symptoms Before Labor
When you’re pregnant, you always want to be ready for the big day. This is particularly true when you are already in your third trimester.
They want to be fully prepared when they go into labor.
But for first-time moms, this can be difficult. They don’t have any experience that will tell them when it’s time.
And as a result, they only rely on the information they have read or what their doctors tell them.
Some women end up going to the hospital because they feel that they are having contractions.
But once there, they are sent back home because it was a false alarm.
If you are an expecting mom, there are some surefire signs that your body is going into labor.
And one of these is experiencing flu like symptoms before labor.
If you feel like you’re coming down with the flu, it may be a sign that you are about to go into labor.
This is something that’s completely normal to experience, especially if you are a week or two away from your expected due date.
Read more about this symptom as an indicator of going into labor so you don’t panic when you suddenly start feeling fluish.
Flu like Symptoms Before Labor
Some of the flu like symptoms before labor that you may feel include sneezing, body pain, headache, and runny nose.
But there are also some women who have encountered a mild cough.
While these symptoms vary for each woman, they are pretty normal to experience just before going into labor.
And they will usually disappear in just a few days.
You can take this time as your body telling you to get your hospital bag ready and waiting by the door since labor can happen any day now.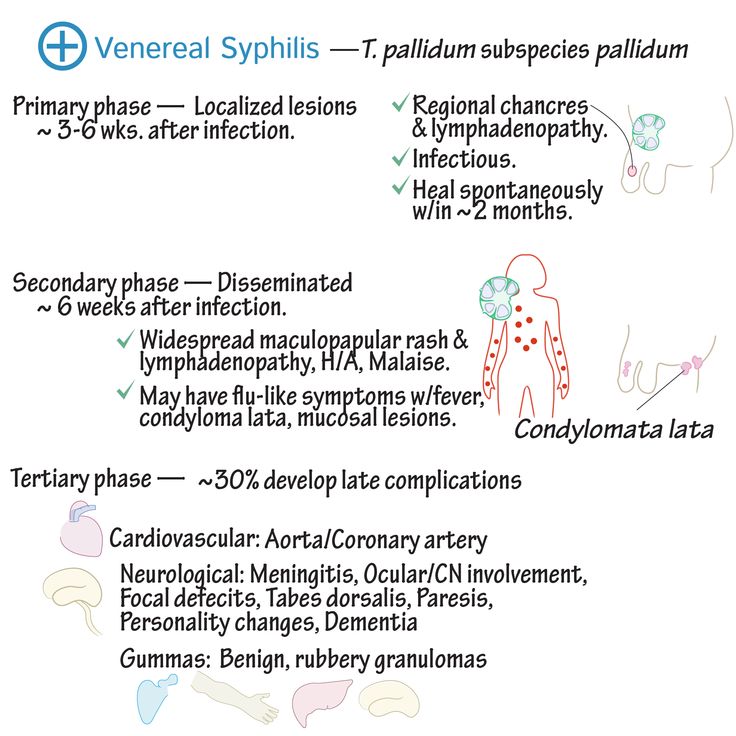
1.) What Flu-Like Symptoms Do You Feel?
Some of the flu-like symptoms that you may experience just before you go into labor include the following:
- Sneezing
- Body aches
- Runny nose
- Headaches
- Mild cough
- Body aches
- Fatigue
- Changes in bowel movements
You will usually feel these symptoms for a few days.
But if you are really worried about these symptoms, it may be best to call your doctor; especially with the COVID-19 pandemic still going on.
2.) How Soon Does Labor Start After These Symptoms
There is no definite date on when you could go into labor after you start feeling flu like symptoms before labor. It could happen a week or two before your due date.
As your body prepares for your coming baby, your hormones also change. This is why you experience these symptoms.
If you start to feel like you have a cold or flu and you’re in your ninth month of pregnancy, you can get a consultation with your doctor just to be sure that you’re okay.
3.) Do You Need To Call The Doctor?
Having flu-like symptoms while you’re pregnant can be very unpleasant. But they don’t usually warrant calling your doctor.
They usually go away on their own in just a few days and do not progress or worsen.
If these symptoms become intense or don’t disappear over the next few days, however, it may be time to give your doctor a call.
This is particularly true if you are experiencing chills, fever, or vomiting.
Subtle Signs You are in Labor
Now that you know flu-like symptoms can be a sign of going into labor, let’s talk about the other symptoms that you may experience.
It’s important to know that many of the early signs of labor are similar to pregnancy symptoms.
This is why it can be difficult to determine when labor actually begins.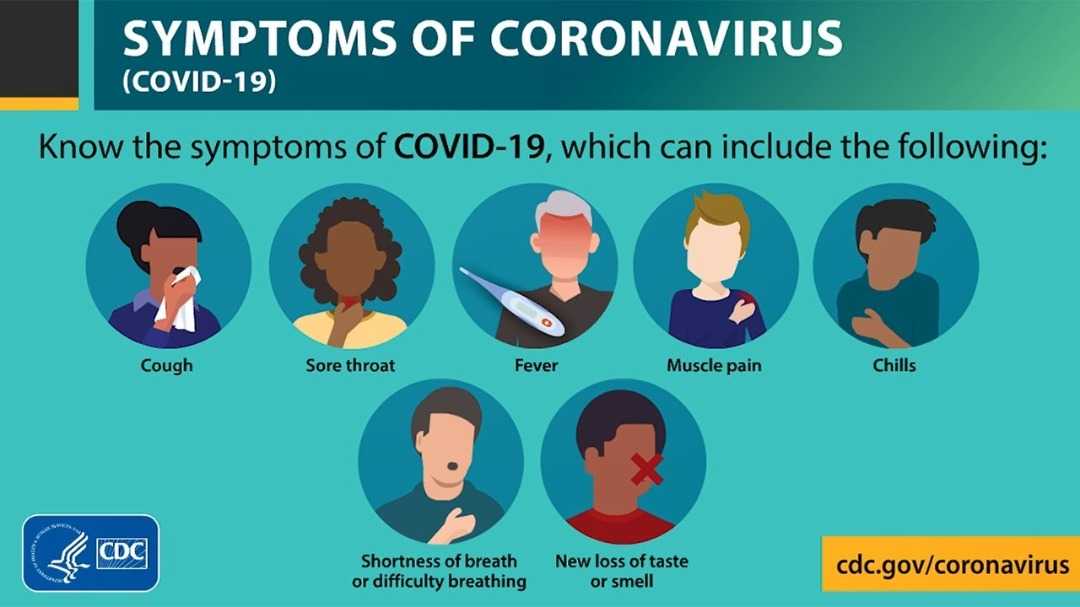
But knowing what you need to look out for can be a big help. Here are some of the subtle signs that you are going into labor:
1.) Nesting
Another indication that labor is approaching is nesting.
This is when you experience an abrupt burst of energy after several months of being physically exhausted.
Most women get a lot of stuff done when they are nesting. They are motivated to prepare everything they need for their baby’s arrival.
Nesting doesn’t always lead to labor right away. There are some who experience this a few weeks before they go into labor.
2.) Nausea & Diarrhea
If you think morning sickness only happens during the first trimester, think again.
There are some women who undergo gastrointestinal upset late in their pregnancy too.
When you experience nausea and diarrhea in the final weeks of your pregnancy, it is usually because your baby is already growing and your uterus is crowding into your GI tract.
At the same time, your hormones may let your muscles loosen and relax when labor is approaching.
This is why many consider diarrhea as a sign of going into labor.
3.) Lightening
There are some instances where your friends or loved ones will tell you that your baby has dropped.
This occurrence is known as lightening and usually means that your baby is preparing for delivery and has settled onto your pelvis.
The American Pregnancy Association says that this usually happens a few days or weeks before going into labor.
Lightning will also make you breathe easier since there’s less pressure on your diaphragm so you can use that as an indicator too.
4.) Back Ache
Most women experience lower back aches upon reaching the 37th week of pregnancy.
This is the time when your baby’s head will settle down your cervix. And because of this, the additional pressure will push towards your spine and nerves and make you feel pain.
You may also feel back aches that are increasing in intensity when you are going into labor.
When accompanied by contractions, it is an indication that you are in labor and you need to head to the hospital right away.
5.) Expulsion of the Mucus Plug
Another sign that you are about to go into labor is when your mucus plug gets expelled.
You will see a thick, mucus-like membrane that could either be released all at once or gradually from your body.
This is what doctors call the mucus plug. It helps block bacteria from entering your uterus.
When your mucus plug is expelled, it means that your cervix has started to thin out and open up.
It can be a sign that labor can happen in a few hours, days, or weeks.
6.) The Bloody Show
Yes, that’s really what it’s called.
Now that your mucus plug has been expelled, the surrounding blood vessels may also burst. And this can lead to some bloody discharge.
Doctors usually see this discharge as a sign that labor is near– from minutes or two weeks away.
If the bloody discharge is about the size of a quarter, it’s pretty normal to experience the bloody show.
However, if you are experiencing heavy bleeding, you need to call your doctor right away.
Related Posts:
- Weird Feeling Before Labor
- 13 Weeks Pregnant Belly Still Soft
- Can You Cut Your Hair While Pregnant?
Frequently Asked Questions
Why do I feel sick before labor?
When you are pregnant, it is normal for your immune system to be weaker.
Because of this, you are more susceptible to getting sick when you are pregnant.
Does labor feel like you have the flu?
Not entirely, but you may have flu-like symptoms just before you start going into labor.
This is particularly true if you experience these symptoms one or two weeks before your expected delivery date.
You will usually feel nausea, diarrhea, fatigue, or back aches. And these symptoms usually just go away on their own after a few days.
How did you feel right before going into labor?
Going into labor is different for every woman. Most women, however, feel like they have strong menstrual cramps, low back pain, or diarrhea.
Most women, however, feel like they have strong menstrual cramps, low back pain, or diarrhea.
One of the common signs that you are going into labor is when you have lower back pain that radiates into your legs.
And when you change positions, the pain doesn’t go away.
If this happens, you should head to your hospital right away.
Iesha Mulla
Iesha is a loving mother of 2 beautiful children. She’s an active parent who enjoys indoor and outdoor adventures with her family. Her mission is to share practical and realistic parenting advice to help the parenting community becoming stronger.
Influenza during pregnancy: symptoms
Pregnancy is a special condition for a woman, which is particularly vulnerable. Pregnancy lasts 9 months and during this time the expectant mother will have to deal with various viruses that can cause both a mild cold and severe illness. In the process of bearing a child, a woman's body works in an enhanced mode, so the immune system does not always manage to easily defeat a cold.
Pregnancy lasts 9 months and during this time the expectant mother will have to deal with various viruses that can cause both a mild cold and severe illness. In the process of bearing a child, a woman's body works in an enhanced mode, so the immune system does not always manage to easily defeat a cold.
One of the most dangerous viral infections for a woman who is expecting a baby is the flu. It can have a negative effect on the placenta, amniotic fluid and the fetus itself. Influenza in the early stages of pregnancy can cause miscarriage, in the later stages - premature birth and malformations in the baby. Therefore, with severe cold symptoms, the expectant mother needs to be under the supervision of doctors. Medical monitoring of the health of a pregnant woman will reduce the risk of complications and termination of pregnancy. If the disease is severe, the woman is hospitalized in a hospital.
How can you tell influenza from other viral infections?
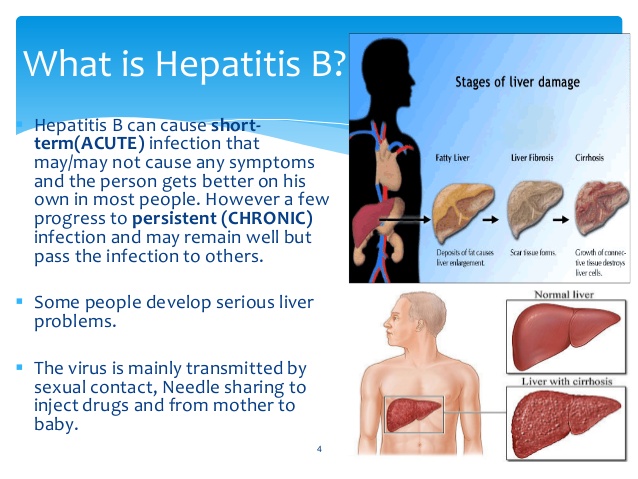
Influenza, like other SARS, is spread by airborne droplets. Once in the body, the virus begins to multiply very quickly. The main sign of this infection is a rapidly growing powerful intoxication of the body, which is manifested by the following symptoms:
Once in the body, the virus begins to multiply very quickly. The main sign of this infection is a rapidly growing powerful intoxication of the body, which is manifested by the following symptoms:
- severe weakness;
- pressing headache;
- redness and pain in the eyes;
- photophobia;
- muscle aches;
- lacrimation;
- chills;
- sweating.
The onset of the disease is always acute, with a sharp rise in temperature, which can reach 40 degrees. The virus infects the respiratory tract, which is manifested by a runny nose, cough, difficulty breathing, dry mucous membranes, pain and sore throat.
The disease is more severe than ordinary ARVI and carries a greater risk of complications. The patient may develop pneumonia, otitis, sinusitis, myocarditis. In addition to the threat of miscarriage and premature birth, the expectant mother may develop chronic diseases or develop a bacterial infection.
Consequences of influenza during pregnancy
The consequences of influenza in pregnant women are dangerous and unpredictable. Most often, complications occur in the second and third trimester. No less dangerous is the flu in the first weeks of pregnancy. Up to 12 weeks, all organs and tissues of the child are laid. Therefore, it is important that the body of the future mother is not exposed to viral loads during this period.
Illness in the last months can cause premature birth. The virus easily crosses the placenta and affects the auditory, visual, nervous system of the baby. Intrauterine infection sometimes causes deviations in mental and physical development, as well as the death of the child.
Influenza virus during pregnancy in the third trimester depresses the immunity of not only the mother, but also the baby. There is also a risk that the newborn will be susceptible to pathogens of various infections. But in fact, no doctor can say with accuracy how a viral infection affects a child, since each pregnancy proceeds individually. The consequences of the disease are influenced by many factors - the age of the expectant mother, the state of immunity, concomitant and past diseases.
The consequences of the disease are influenced by many factors - the age of the expectant mother, the state of immunity, concomitant and past diseases.
A woman who gets the flu during pregnancy needs to carefully monitor her condition to prevent the development of complications. If you feel unwell, call an ambulance. "Red flags" that indicate that the patient needs hospitalization:
- prolonged body temperature above 38 degrees, which does not go astray;
- palpitations;
- severe dyspnea;
- disturbance of consciousness;
- suspected development of pneumonia.
The risk of complications from influenza is increased by smoking and the presence of chronic diseases.
How to treat influenza during pregnancy?
Unfortunately, childbearing limits the choice of drugs for the treatment of colds. Pregnant women are contraindicated in vasoconstrictor drops, antipyretics based on acetylsalicylic acid, and some antitussives. Before taking the medicine, you need to make sure that it will not have a toxic effect on the fetus. Therefore, what to drink with the flu during pregnancy should be decided by the attending physician.
Before taking the medicine, you need to make sure that it will not have a toxic effect on the fetus. Therefore, what to drink with the flu during pregnancy should be decided by the attending physician.
What to do if the mother-to-be has flu-like symptoms:
- Stay at home and call the doctor if you have the first symptoms of a cold. He will examine the patient, listen to the lungs for wheezing, prescribe drugs that are allowed for pregnant women. Women carrying a child with colds are prescribed:
- antipyretics;
- antivirals - the doctor may recommend Flustop. The appointment of etiotropic therapy for influenza as early as possible from the onset of the disease is shown, taking into account the available data on the safety, pathogenicity of the circulating strain of the influenza virus and the condition of the pregnant woman in any trimester of pregnancy (instruction for the medical use of the drug Flustop).
- antitussives;
- nasal saline solutions;
- solutions for gargling.
- Plentiful warm drink is a prerequisite for the treatment of viral diseases. A large amount of liquid helps to cope with intoxication. It is allowed to drink tea, fruit drinks, cocoa, juices, fruit and berry compotes.
- It is advisable to take antipyretic drugs for influenza during pregnancy at a body temperature of at least 38 degrees. It is necessary to limit the number of tablets to four per day. To reduce the temperature, you can use rubbing with water at room temperature.
- Ask loved ones to ventilate and carry out daily wet cleaning in your room. This will help to avoid dry mucous membranes, as well as reduce the amount of viral particles in the room.
- Don't skip meals. Eat foods that are easy to digest. Give preference to liquid foods - broths, milk, yogurt, soups, fruit purees.
- Stay in bed to reduce stress on the immune, cardiovascular, and other systems of the body. Do not rush to do household and work chores until you feel that you have finally recovered.
If you get sick with a cold and flu during pregnancy, do not use folk remedies for treatment. It is strictly forbidden to soar the legs of pregnant women, inhalations with essential oils can provoke an allergic reaction, and some herbal preparations have a toxic effect on the fetus. Do not take antibiotics - they do not help with viral infections. A doctor may prescribe antibiotics only if a bacterial infection has joined the flu.
How can I avoid getting colds and flu during pregnancy?
To avoid contracting viral infections, follow these guidelines:
- Avoid crowded places.
- Wash your hands frequently with soap and use hand sanitizer when visiting crowded places.
- Restrict travel on public transport.
- Spend more time outdoors.
- If there are no contraindications, regularly engage in exercise, yoga or other form of physical activity.
- Try to touch your face less with your hands so as not to infect the mucous membranes.
- Ventilate the room before going to bed and the room in which you work.
- To avoid the negative impact of influenza on pregnancy, wear a protective mask in clinics, pharmacies, shops, shopping centers. Remember to change it every two to three hours.
- If someone in the household is sick, isolate yourself from him and do not forget about the mask mode.
- Eat a varied diet - the diet should be balanced.
- Avoid stress, sleep at least 8 hours a day.
- Flush your nose with saline before and after going to crowded places.
- Take vitamin complexes prescribed by your doctor.
Vaccination is an effective way to protect against influenza. Modern vaccines can be vaccinated while pregnant. Immunity from vaccination is transmitted to the baby and lasts up to six months. The expectant mother can discuss vaccination issues with her doctor.
If you do feel sick and get the flu during pregnancy, stay in bed and drink plenty of warm fluids.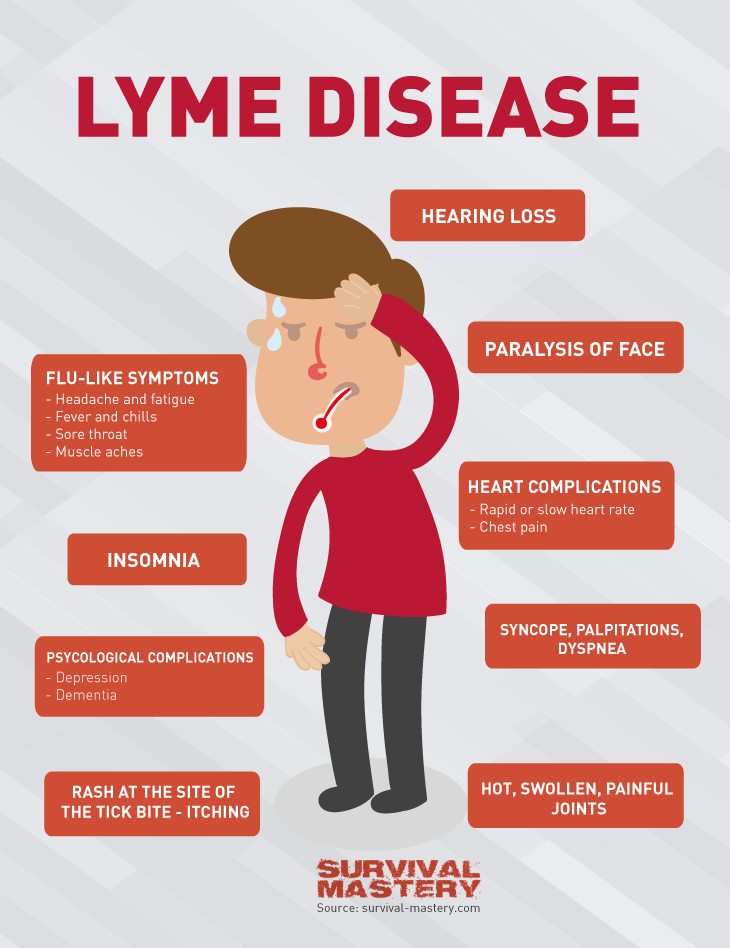 Do not be nervous and do not panic, so as not to harm the baby. For prescription of medications, contact your doctor. With a competent approach to treatment, the dangerous consequences of the disease for the child will be minimized.
Do not be nervous and do not panic, so as not to harm the baby. For prescription of medications, contact your doctor. With a competent approach to treatment, the dangerous consequences of the disease for the child will be minimized.
IMPORTANT
The information in this section cannot be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
SARS during pregnancy is a group of clinically similar acute respiratory infections caused by pneumotropic viruses and developed during gestation. It is manifested by a rapidly growing catarrhal syndrome: runny nose, dry cough, pain and sore throat, hoarse voice. There are phenomena of general intoxication: fever, headache, weakness, weakness, myalgia, arthralgia. Diagnosed by ELISA, PCR, complete blood count. In the course of treatment, antipyretic, expectorant, antitussive, mucolytic, anti-inflammatory, anti-obstructive drugs are used, in severe cases - donor immunoglobulin, interferon, its inducers, immunomodulators.
Diagnosed by ELISA, PCR, complete blood count. In the course of treatment, antipyretic, expectorant, antitussive, mucolytic, anti-inflammatory, anti-obstructive drugs are used, in severe cases - donor immunoglobulin, interferon, its inducers, immunomodulators.
ICD-10
J00 B34
- Causes
- Pathogenesis
- SARS symptoms during pregnancy
- Complications
- Diagnostics
- Treatment of SARS during pregnancy
- Prognosis and prevention
- Prices for treatment
General
According to experts in the field of infectious diseases, obstetrics and gynecology, the prevalence of SARS during pregnancy reaches 55-82%. The incidence of influenza and other acute respiratory infections in pregnant women is slightly higher than in the general population, and the diseases themselves are longer, more severe, with a large number of complications.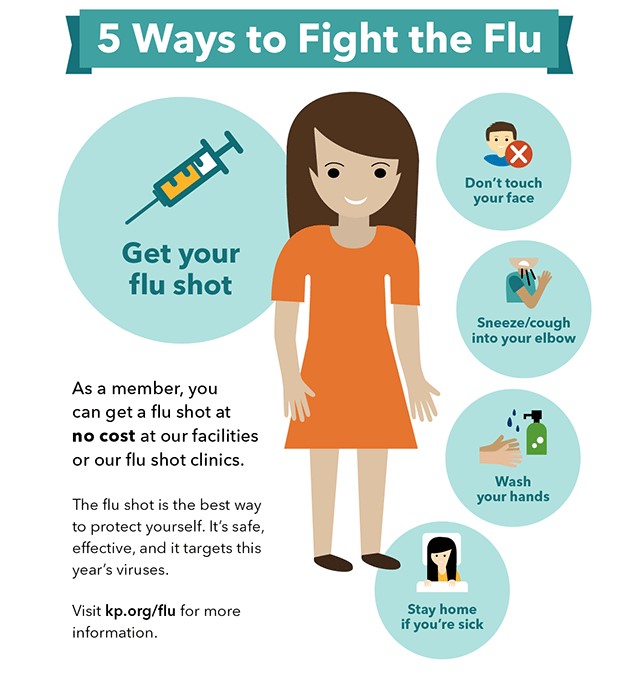 When gestation is combined with ARVI, especially influenza, there is a need for hospitalization more often, and the risk of perinatal and maternal mortality increases. Respiratory infections are characterized by an epidemic course with a peak incidence from December to March and a rapid spread among organized contingents of people, including in medical institutions.
When gestation is combined with ARVI, especially influenza, there is a need for hospitalization more often, and the risk of perinatal and maternal mortality increases. Respiratory infections are characterized by an epidemic course with a peak incidence from December to March and a rapid spread among organized contingents of people, including in medical institutions.
SARS during pregnancy
Causes
The causative agents of acute respiratory viral infections are the so-called pneumotropic viruses, which are transmitted mainly by airborne droplets. To date, more than 300 non-cellular infectious agents have been identified that cause the common cold during gestation. More than half of pregnant women develop the disease when infected with parainfluenza viruses, 15% with influenza viruses types A and B, 5% with adenoviruses, 4% with pathogens of respiratory syncytial infection, 1.2% with enteroviruses, less than in 1% of cases - rhinoviruses, coronaviruses, reoviruses. In 23% of patients, ARVI has a mixed etiology.
In 23% of patients, ARVI has a mixed etiology.
The more frequent occurrence and prolonged complicated course of respiratory infections during pregnancy is associated with the physiological changes that occur in the body of a woman carrying a child. According to most obstetrician-gynecologists, specific gestational factors that affect the development of SARS in pregnant women are:
- Reduced immunity. Immune restructuring during pregnancy is aimed at preventing rejection of the fetus, which is genetically alien to the female body. Immunosuppression occurs due to increased levels of progesterone and cortisol. The cellular link of the immune system, which plays a key role in the rapid elimination of the pathogen, is more strongly inhibited.
- Hyperventilation of the lungs. To ensure sufficient oxygenation of the tissues of the mother and the growing fetus, the bronchopulmonary system gradually switches to the diaphragmatic type of breathing.
 By strengthening the excursions of the diaphragm, better ventilation of the alveoli is provided. This creates optimal conditions for the penetration of viruses into the lower parts of the respiratory system.
By strengthening the excursions of the diaphragm, better ventilation of the alveoli is provided. This creates optimal conditions for the penetration of viruses into the lower parts of the respiratory system. - Swelling of the mucous membrane of the tracheobronchial tree. Due to the physiological increase in the volume of circulating blood and concomitant arteriolodilatation in a pregnant woman, there is a plethora of capillaries, leading to swelling of the mucous membranes. Since such changes are similar to inflammatory edema, the addition of an infection makes the clinical symptoms more pronounced.
Pathogenesis
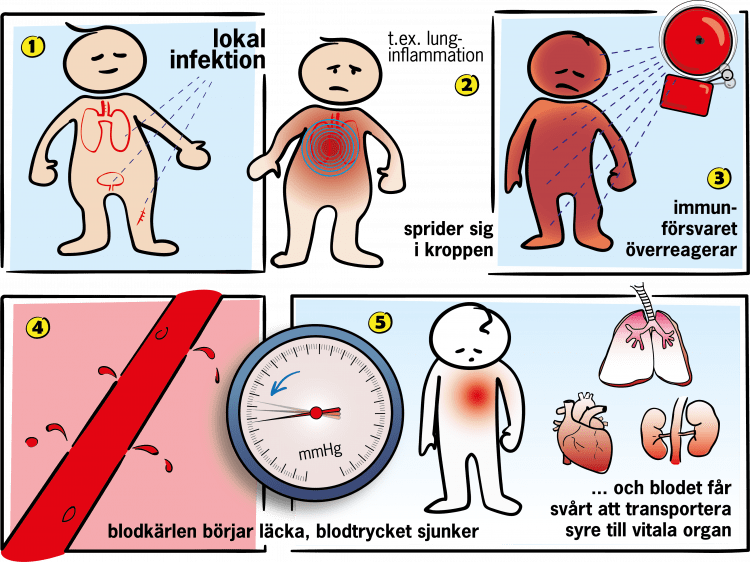
Most catarrhal infections caused by viruses are anthroponoses, less often the disease is spread by mammals and birds (swine flu, bird flu). The leading way of ARVI infection during pregnancy is the airborne transfer of the pathogen from the carrier, the patient, less often the convalescent. Sometimes viruses are transmitted by contact (through a handshake, contaminated environmental objects). The entrance gate usually becomes the epithelium of the nose, nasopharynx, larynx, trachea, bronchi, sometimes the virus is introduced into the mucous membranes of the eyes, gastrointestinal tract. First, the infectious agent attaches to the epithelial cell, then penetrates into it and begins to replicate. The destruction of epitheliocytes is accompanied by the spread of viral particles along the mucosa with the development of a local inflammatory reaction.
The entrance gate usually becomes the epithelium of the nose, nasopharynx, larynx, trachea, bronchi, sometimes the virus is introduced into the mucous membranes of the eyes, gastrointestinal tract. First, the infectious agent attaches to the epithelial cell, then penetrates into it and begins to replicate. The destruction of epitheliocytes is accompanied by the spread of viral particles along the mucosa with the development of a local inflammatory reaction.
The entry of the ARVI pathogen into the bloodstream leads to the occurrence of general intoxication. In response to the presence of viral antigens, protective reactions are activated in the form of proliferation of lymphocytes (mainly type T) and increased synthesis of interferon. After the complete elimination of the virus with an uncomplicated course of a cold, the respiratory tract is cleared of the affected layers of the epithelium. With a weakened immune system, the alveoli of the lungs, the mucous membranes of the paranasal sinuses, and the tympanic cavity are involved in the process.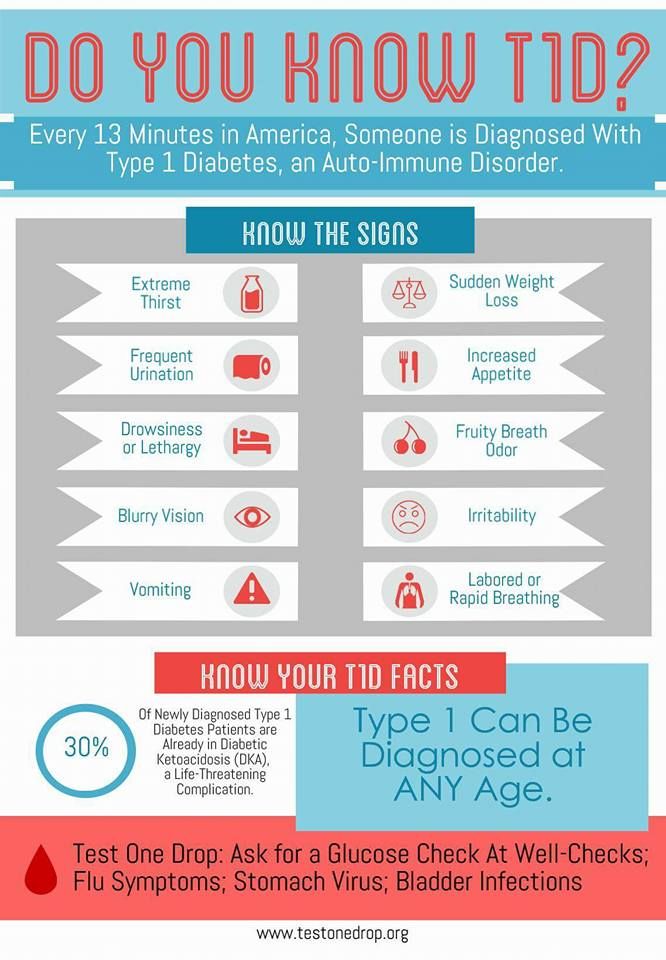 In severe cases, the placenta is infected, which leads to impaired fetoplacental blood flow, delayed development and death of the fetus.
In severe cases, the placenta is infected, which leads to impaired fetoplacental blood flow, delayed development and death of the fetus.
SARS symptoms during pregnancy
Due to a decrease in immunity in pregnant women, the incubation period is usually reduced to 2-3 days. With a high virulence of the pathogen, the first signs of infection may occur several hours after infection. The clinical picture of most catarrhal viral infections is similar. Catarrhal symptoms during pregnancy usually increase gradually, but more rapidly than out of gestation: a woman complains of a runny nose, perspiration, sore throat, dry cough, hoarseness of voice.
Viral intoxication is most pronounced with influenza, with other respiratory infections, dizziness, headache, weakness, weakness, soreness of muscles and joints are moderately expressed. Often there is a decrease in appetite. Sometimes there is nausea, vomiting, with adenovirus infection - photophobia, pain, pain in the eyes, enlargement of the cervical and submandibular lymph nodes. Within 3-5 days, hyperthermia up to 38 ° C is noted, with influenza - up to 39-40 ° C. Influenza infection is also characterized by redness of the face, neck, mucous membranes, injection of the sclera. The duration of the acute period is usually 7 to 10 days. During the period of convalescence, a wet cough is detected with the discharge of mucous sputum.
Within 3-5 days, hyperthermia up to 38 ° C is noted, with influenza - up to 39-40 ° C. Influenza infection is also characterized by redness of the face, neck, mucous membranes, injection of the sclera. The duration of the acute period is usually 7 to 10 days. During the period of convalescence, a wet cough is detected with the discharge of mucous sputum.
Complications
Intense coughing and sneezing caused by SARS is accompanied by an increase in pressure in the abdominal cavity. This can provoke an increased tone of the uterus and, as a result, increase the risk of termination of pregnancy by spontaneous miscarriage or premature birth up to 25-50%. Due to nasal congestion and deterioration of ventilation associated with mucosal edema, gas exchange in the lungs is disturbed, blood oxygen saturation decreases, resulting in fetal hypoxia. Viral damage to the placental tissue leads to the development of fetoplacental insufficiency, premature aging of the placenta.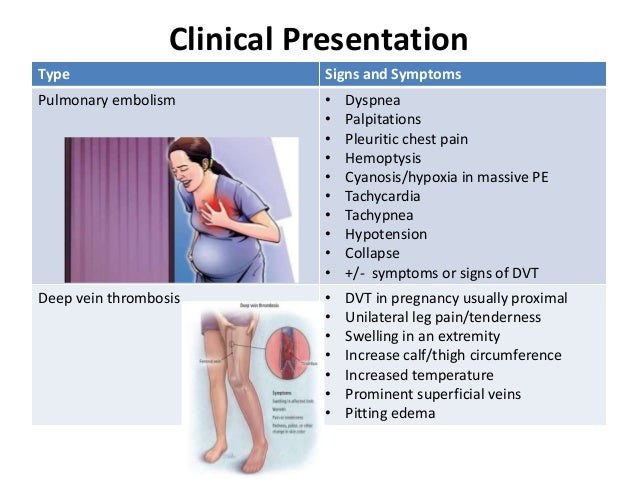 After suffering catarrhal infections, 3.2% of pregnant women have premature detachment of the placenta, more often there is weakness in labor, bleeding during childbirth.
After suffering catarrhal infections, 3.2% of pregnant women have premature detachment of the placenta, more often there is weakness in labor, bleeding during childbirth.
Infection with SARS in the first trimester of pregnancy with transplacental transmission of the virus provokes damage at the cellular level, leads to the formation of true malformations, fetal death, miscarriage. The risk of teratogenesis is especially high (up to 10% of all cases) in pregnant women with influenza. With intrauterine infection in the II-III trimesters, early and late fetopathy with inflammatory lesions of individual organs (meningitis, encephalitis, pneumonia), generalization of inflammation, the formation of multiple anomalies, antenatal death or delayed fetal development are detected. After birth, children often look lethargic, inactive, they have various respiratory problems.
During pregnancy, ARVI worsens the course of early toxicosis, gestosis, and can be complicated by secondary infections caused by the activation of opportunistic microflora against the background of immunosuppression.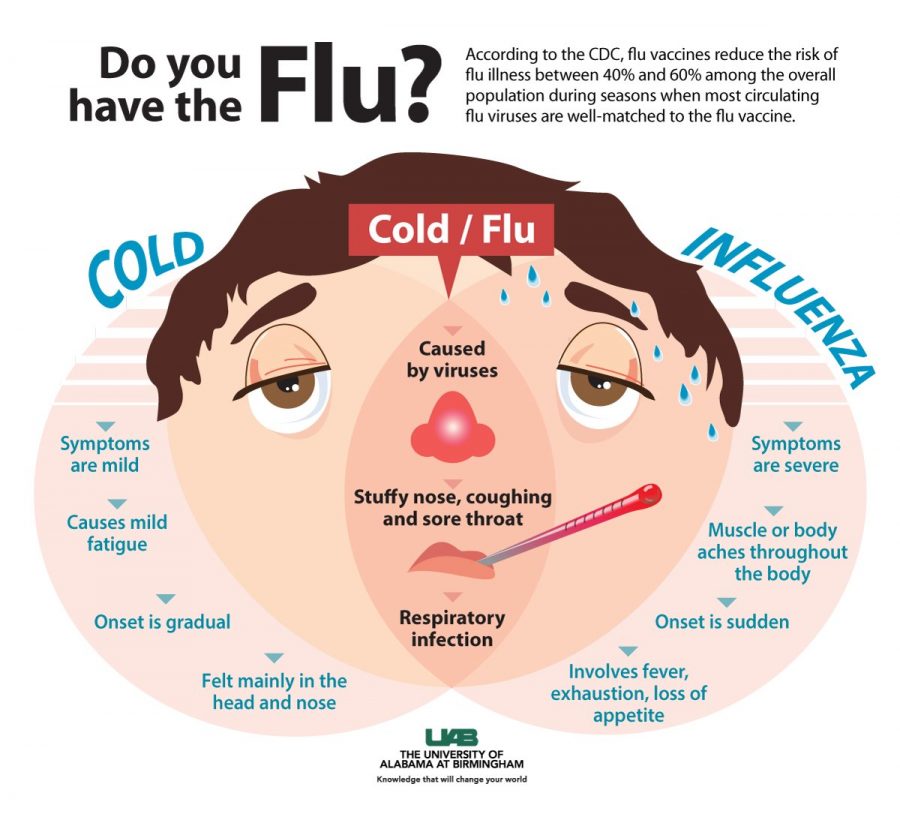 Most often, acute sinusitis, purulent otitis media, bronchitis, and bacterial pneumonia develop. Possible exacerbation of chronic infectious and somatic diseases - rheumatism, pancreatitis, cholecystitis, pyelonephritis, glomerulonephritis. Rare, but severe complications of SARS are secondary myocarditis, pericarditis, myositis, meningoencephalitis, polyneuritis, neuralgia, Reye's syndrome, toxic-allergic shock.
Most often, acute sinusitis, purulent otitis media, bronchitis, and bacterial pneumonia develop. Possible exacerbation of chronic infectious and somatic diseases - rheumatism, pancreatitis, cholecystitis, pyelonephritis, glomerulonephritis. Rare, but severe complications of SARS are secondary myocarditis, pericarditis, myositis, meningoencephalitis, polyneuritis, neuralgia, Reye's syndrome, toxic-allergic shock.
Diagnostics
During the epidemic, the diagnosis of acute respiratory viral infection during pregnancy does not present any difficulties. In such cases, the diagnosis is carried out on the basis of a characteristic clinical picture with catarrhal symptoms and intoxication. In case of sporadic cases of the disease that occurred outside the period of an epidemic outbreak, it is recommended:
- Complete blood count. Usually with ARVI, leukopenia, normal or reduced ESR is observed. The number of lymphocytes is often increased due to the T-fraction.
 A sharp increase in leukocytosis and ESR is a prognostically unfavorable sign and often indicates the addition of a secondary bacterial infection.
A sharp increase in leukocytosis and ESR is a prognostically unfavorable sign and often indicates the addition of a secondary bacterial infection. - Serological methods. For express diagnostics of seasonal influenza A, B, parainfluenza, adenoviruses, respiratory syncytial viruses, ELISA is used, with the help of which viral antigens are detected in epithelial cells, and PCR diagnostics, which makes it possible to detect the genetic material of pathogens in clinical samples.
Radiography of the lungs, paranasal sinuses is prescribed only for health reasons with reasonable suspicion of secondary pneumonia or sinusitis. To eliminate the risk of miscarriage and fetal malformations at 17-20 weeks, the determination of the levels of chorionic gonadotropin and alpha-fetoprotein is shown. The assessment of the probability of preterm birth in ARVI at 22-34 weeks of gestation is performed taking into account data on the content of hormones of the fetoplacental complex (placental lactogen, progesterone, estriol, cortisol).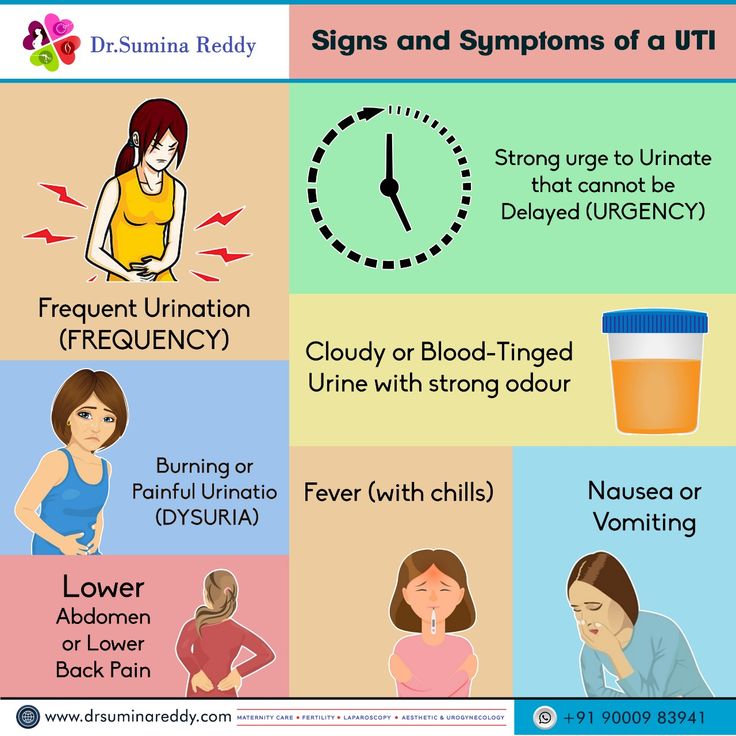
To control the condition of the fetus in the third trimester, CTG, fetometry, and phonocardiography are recommended. Possible pathology of the placenta is detected using ultrasound and Dopplerography of the uteroplacental blood flow. Differential diagnosis is carried out between different types of SARS, with highly contagious viral infections (rubella, measles, scarlet fever), bacterial diseases (tonsillitis, acute pharyngitis, laryngitis, tracheitis, bronchitis, pneumonia). According to the indications, the patient is examined by an infectious disease specialist, pulmonologist, ophthalmologist, otorhinolaryngologist, neuropathologist.
Treatment of SARS during pregnancy
When choosing medical tactics, the gestational age, the type of pathogen, and the characteristics of the course of the disease are taken into account. Early termination of pregnancy due to possible fetal abnormalities is recommended only for serologically confirmed influenza.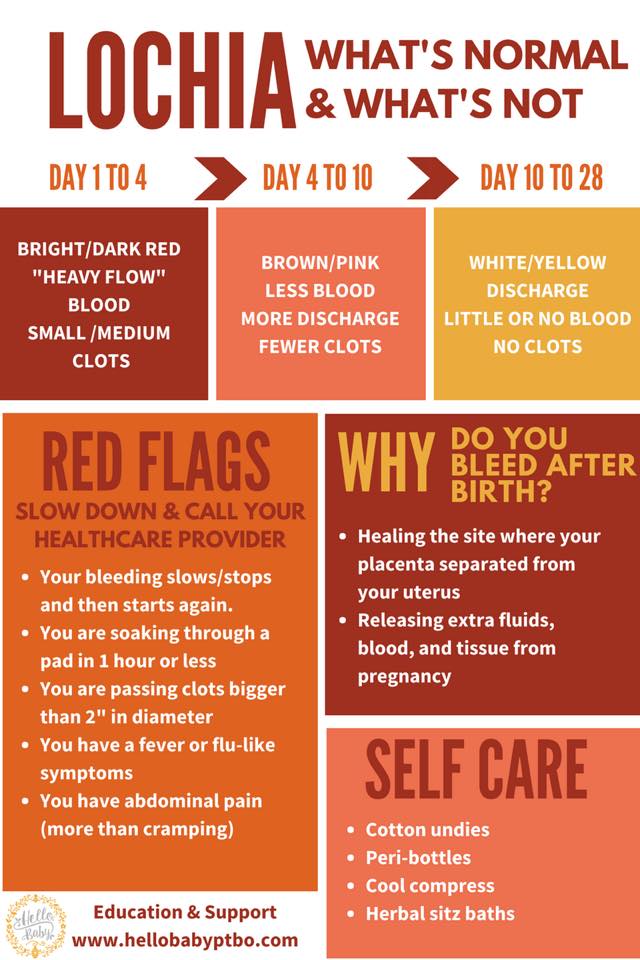 In other cases, gestation can be saved. An important role in correcting the condition of a pregnant woman is played by non-drug methods: ensuring physical and emotional rest, if necessary, bed rest, 7-8-hour night sleep, steam inhalations with decoctions of herbs or ready-made inhalation mixtures, aromatherapy. For faster removal of intoxication, it is useful to drink up to 1.5-2 liters of fluid per day, especially acidic drinks. A complete protein diet is recommended, supplemented with foods that contain vitamin C (citrus fruits, cabbage, currants, apples) and folic acid (legumes, potatoes).
In other cases, gestation can be saved. An important role in correcting the condition of a pregnant woman is played by non-drug methods: ensuring physical and emotional rest, if necessary, bed rest, 7-8-hour night sleep, steam inhalations with decoctions of herbs or ready-made inhalation mixtures, aromatherapy. For faster removal of intoxication, it is useful to drink up to 1.5-2 liters of fluid per day, especially acidic drinks. A complete protein diet is recommended, supplemented with foods that contain vitamin C (citrus fruits, cabbage, currants, apples) and folic acid (legumes, potatoes).
The possibilities of etiotropic treatment of ARVI are limited by the narrow spectrum of drugs, their damaging effect on the fetus, and the lack of knowledge of the side effects of some new drugs. In severe cases of influenza, the introduction of donor anti-influenza immunoglobulin is acceptable. To reduce the duration of the disease and reduce the likely complications during pregnancy, pathogenetic therapy can be carried out, including:
- Interferon and its inductors.
 Due to the risk of interruption of gestation, recombinant human interferon is prescribed from 32 weeks only for severe acute respiratory viral infections. Although modern interferonogenesis stimulants enhance the synthesis of their own α- and β-interferons with high antiviral activity, they are used in exceptional cases, since the effect of interferon inducers on the fetus has not yet been sufficiently studied.
Due to the risk of interruption of gestation, recombinant human interferon is prescribed from 32 weeks only for severe acute respiratory viral infections. Although modern interferonogenesis stimulants enhance the synthesis of their own α- and β-interferons with high antiviral activity, they are used in exceptional cases, since the effect of interferon inducers on the fetus has not yet been sufficiently studied. - Immunomodulators. During pregnancy without Rhesus conflict, regardless of the period, it is permissible to prescribe drugs based on imunofan. These agents enhance the production of specific antiviral antibodies, have a pronounced detoxifying effect, and increase the stability of epithelial membranes. Multivitamin complexes and some homeopathic remedies have a moderate immunostimulating effect.
Depending on the clinical symptoms, the patient undergoes symptomatic therapy using antipyretic, expectorant, antitussive, mucolytic, anti-inflammatory and anti-obstructive drugs approved for use during pregnancy.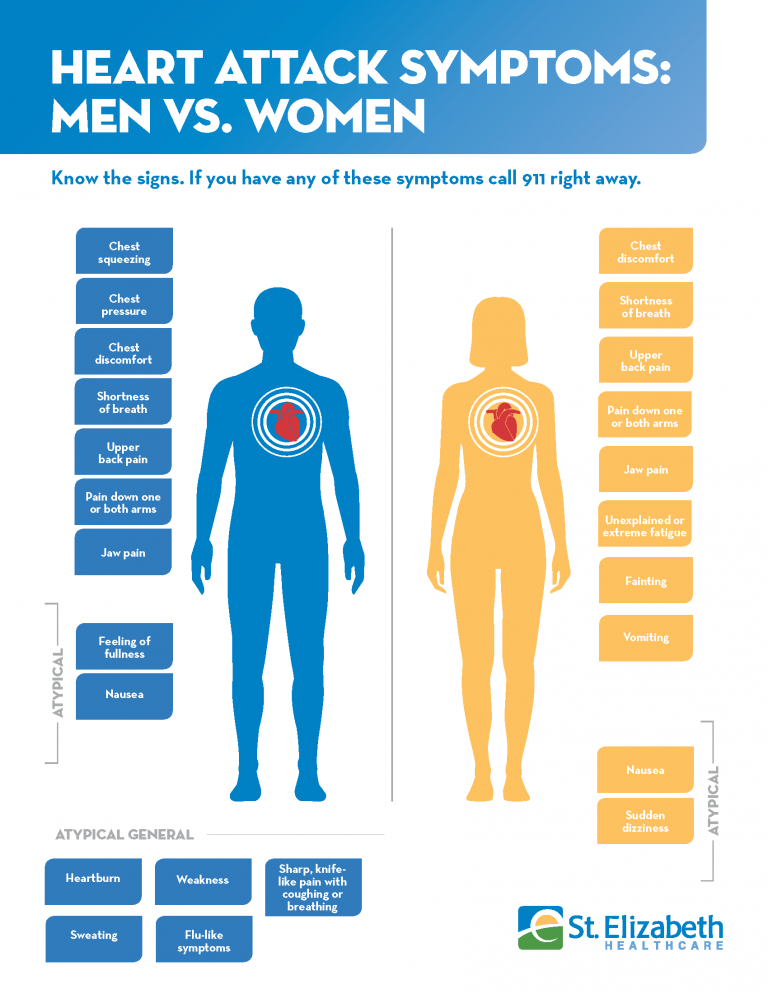 Antibiotics are prescribed only when bacterial complications occur.
Antibiotics are prescribed only when bacterial complications occur.
The preferred method of delivery is natural childbirth. Since in the acute period of ARVI the risk of labor anomalies, bleeding, postpartum purulent-septic diseases increases significantly, it is recommended to prolong pregnancy until clinically pronounced catarrhal symptoms subside with simultaneous prevention of fetal hypoxia. In childbirth, anesthesia is indicated, after childbirth - the introduction of uterotonics and prophylactic antibiotic therapy. Caesarean section is performed when obstetric indications are identified.
Prognosis and prevention
Uncomplicated forms of acute respiratory viral infections during pregnancy disappear on their own or against the background of minimal therapy within 7-10 days. When complications appear, the prognosis becomes more serious. Prevention during the epidemic is aimed at preventing viruses from entering the mucous membranes: limiting the time spent in crowded places, treating mucous membranes with oxolin ointment before leaving the house, wearing gauze or disposable bandages, gargling the throat and nose with saline after returning from a walk. The effectiveness of seasonal influenza immunization before pregnancy planning or in the I-II trimesters reaches 55-90%. To increase the overall resistance, sufficient rest and sleep, good nutrition, elimination of stress, and intake of vitamin and mineral complexes are recommended. Given the seriousness of possible complications, when the first signs of SARS appear, a pregnant woman should immediately contact a antenatal clinic.
The effectiveness of seasonal influenza immunization before pregnancy planning or in the I-II trimesters reaches 55-90%. To increase the overall resistance, sufficient rest and sleep, good nutrition, elimination of stress, and intake of vitamin and mineral complexes are recommended. Given the seriousness of possible complications, when the first signs of SARS appear, a pregnant woman should immediately contact a antenatal clinic.
You can share your medical history, what helped you in the treatment of SARS during pregnancy.
Sources
- Modern aspects of the treatment and prevention of influenza and SARS in pregnant women / Vernidub I.A., Sosnovskaya A.K., Volkova O.I.// International Student Scientific Bulletin. - 2017.
- Influenza in pregnant women/ Popov AF, Kiselev OI// Epidemiology and infectious diseases. – 2013.
- Modern approaches to the prevention and treatment of acute respiratory viral infections and influenza/ Malashenkova IK, Didkovsky NA// Russian Medical Journal.