Examples of congenital disease
1.4 Congenital Anomalies - Definitions
- Chapter 1: Surveillance of Congenital Anomalies
- 1.1 Introduction
- 1.2 The Purpose of Congenital Anomalies Surveillance
- 1.3 Types of Surveillance Programmes
- 1.4 Congenital Anomalies - Definitions
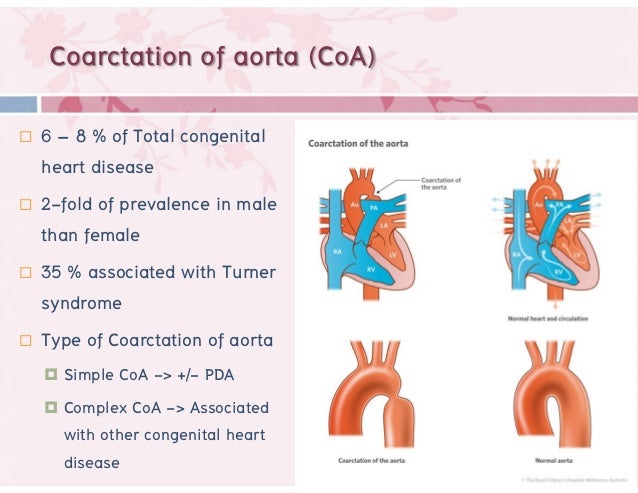
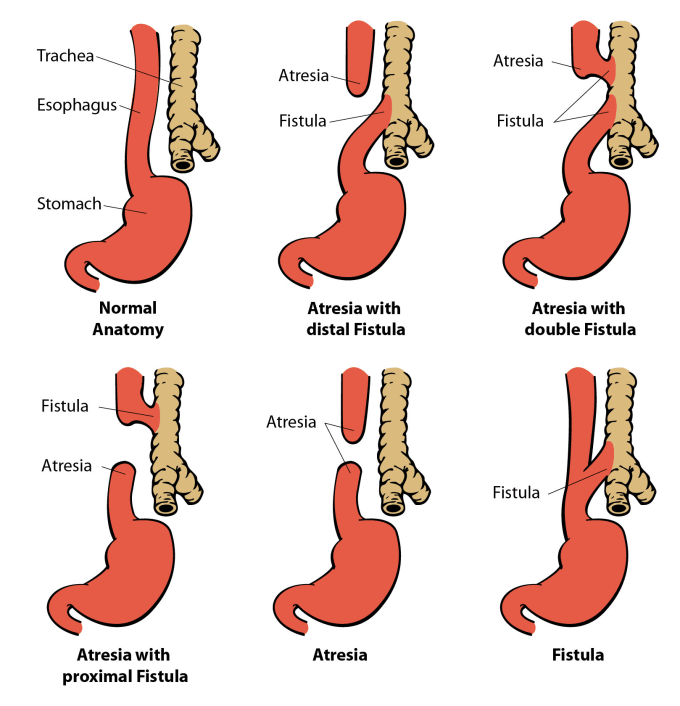
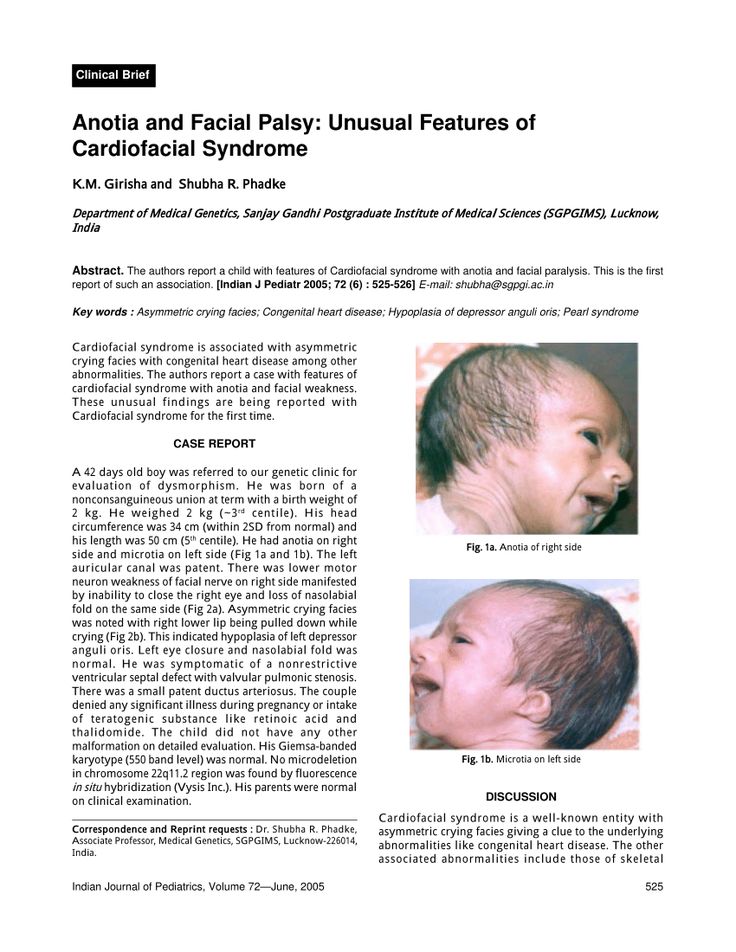
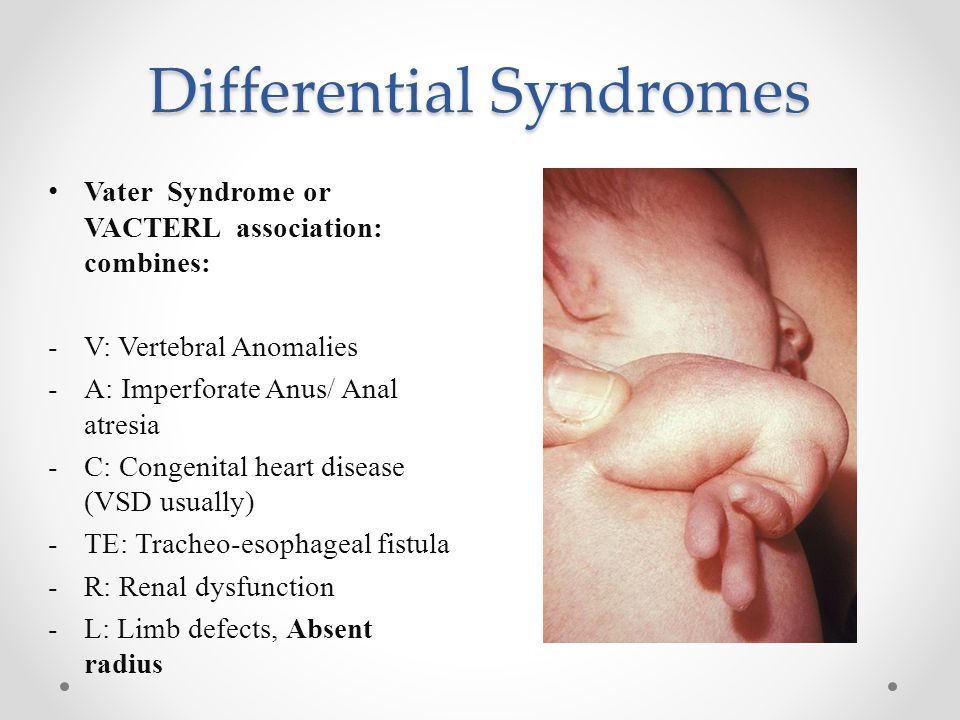
Congenital anomalies comprise a wide range of abnormalities of body structure or function that are present at birth and are of prenatal origin. For efficiency and practicality, the focus is commonly on major structural anomalies. These are defined as structural changes that have significant medical, social or cosmetic consequences for the affected individual, and typically require medical intervention. Examples include cleft lip and spina bifida.
Major structural anomalies are the conditions that account for most of the deaths, morbidity and disability related to congenital anomalies (see Box 1.1 for a list of selected external and internal major congenital anomalies). In contrast, minor congenital anomalies, although more prevalent among the population, are structural changes that pose no significant health problem in the neonatal period and tend to have limited social or cosmetic consequences for the affected individual. Examples include single palmar crease and clinodactyly.
| External | Internal |
|
|
| Chromosomal | |
| Trisomy 21 (Down syndrome) | |
Major anomalies are sometimes associated with minor anomalies, which might be objective (e.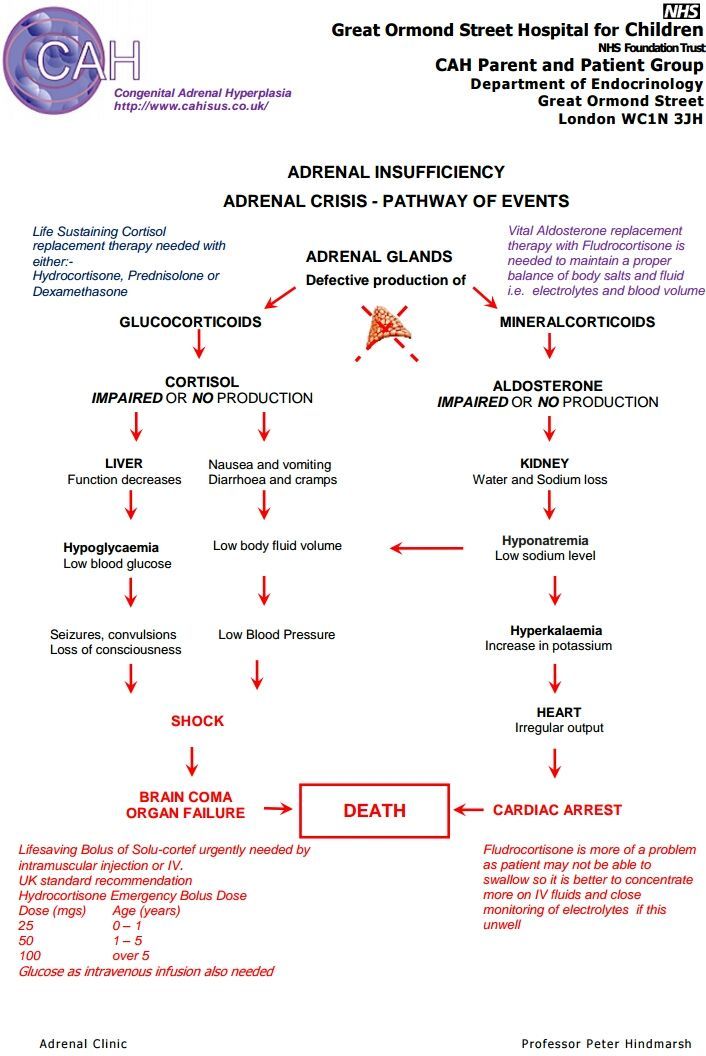 g. preauricular tags) or more subjective (e.g. low-set ears). Box 1.2 represents selected external minor congenital anomalies frequently captured by different surveillance systems, but only when associated with any of the major anomalies under surveillance. For a more detailed listing of minor anomalies, please refer to Appendix B. Often, surveillance systems will collect information on specific syndromes that are multiple anomalies pathogenetically related due to a single cause – for example, genetic or environmental causes that are known to cause birth defects. Certain syndromes caused by infectious diseases are of special interest in many low- and middle-income countries . For a detailed listing of selected syndromes of infectious origin that are of public health significance, please refer to Appendix B.
g. preauricular tags) or more subjective (e.g. low-set ears). Box 1.2 represents selected external minor congenital anomalies frequently captured by different surveillance systems, but only when associated with any of the major anomalies under surveillance. For a more detailed listing of minor anomalies, please refer to Appendix B. Often, surveillance systems will collect information on specific syndromes that are multiple anomalies pathogenetically related due to a single cause – for example, genetic or environmental causes that are known to cause birth defects. Certain syndromes caused by infectious diseases are of special interest in many low- and middle-income countries . For a detailed listing of selected syndromes of infectious origin that are of public health significance, please refer to Appendix B.
When establishing a new congenital anomalies surveillance programme, the initial anomalies that are included can be limited to structural anomalies that are readily identifiable and easily recognized on physical examination at birth or shortly after birth.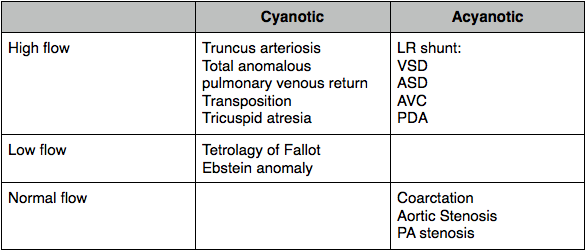 The list may vary, depending on the capacity and resources of the health-care system and surveillance programme, but typically includes major external congenital anomalies. Examples include:
The list may vary, depending on the capacity and resources of the health-care system and surveillance programme, but typically includes major external congenital anomalies. Examples include:
- orofacial clefts,
- neural tube defects, and
- limb deficiencies.
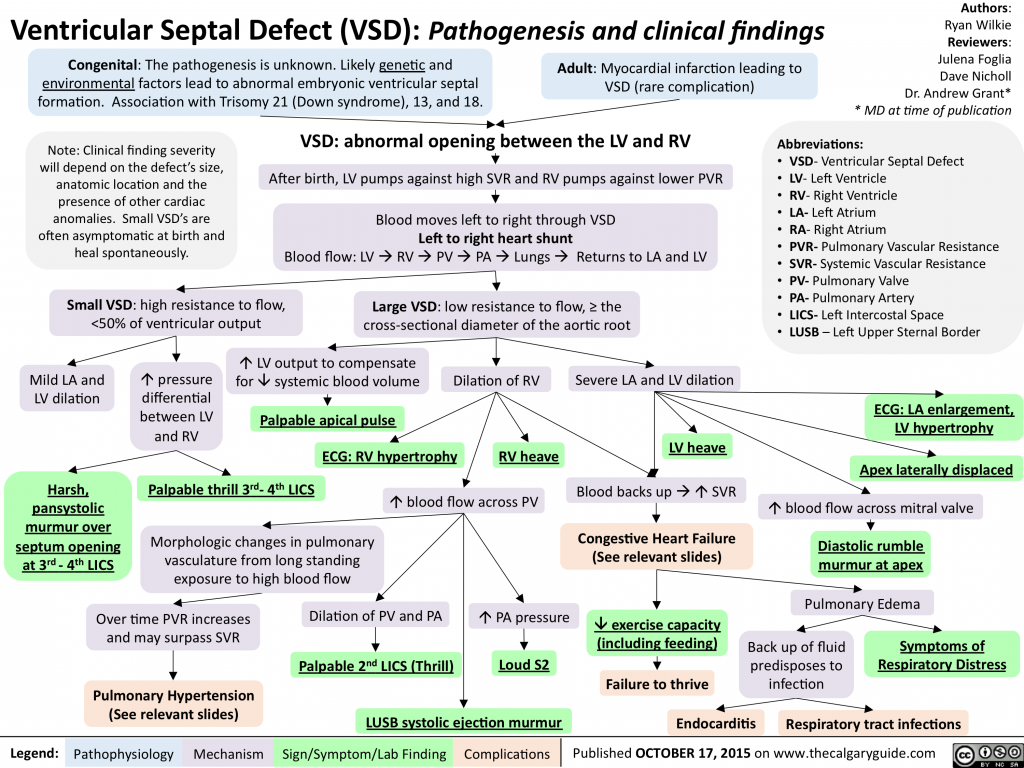
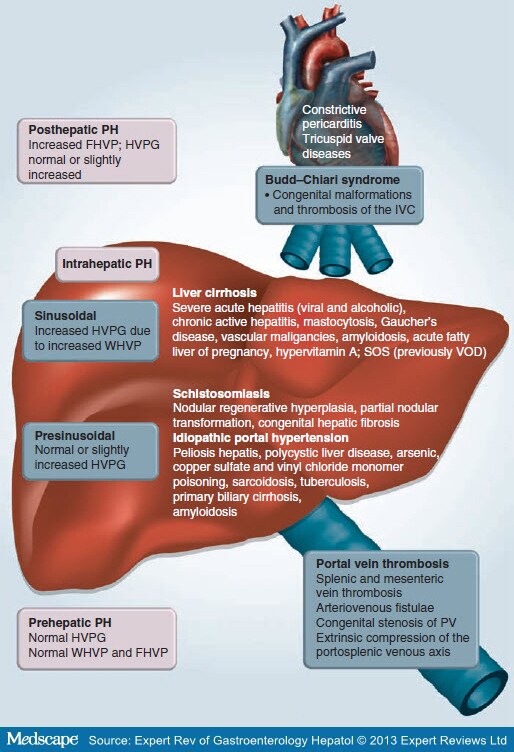
In contrast, detecting the vast majority of internal structural anomalies (e.g. congenital heart defects, intestinal malrotation and unilateral kidney agenesis) requires imaging techniques or other specialized procedures that may not be available consistently. In some cases, internal anomalies have external manifestations that allow the observer to suspect a particular diagnosis, as is the case with the urethral obstruction sequence. Similar to collecting information on internal defects, collecting information on syndromes often requires gathering data from multiple sources such as laboratory, imaging or genetic testing. Therefore, collecting surveillance data on internal defects and syndromes is typically not recommended when first starting a surveillance programme.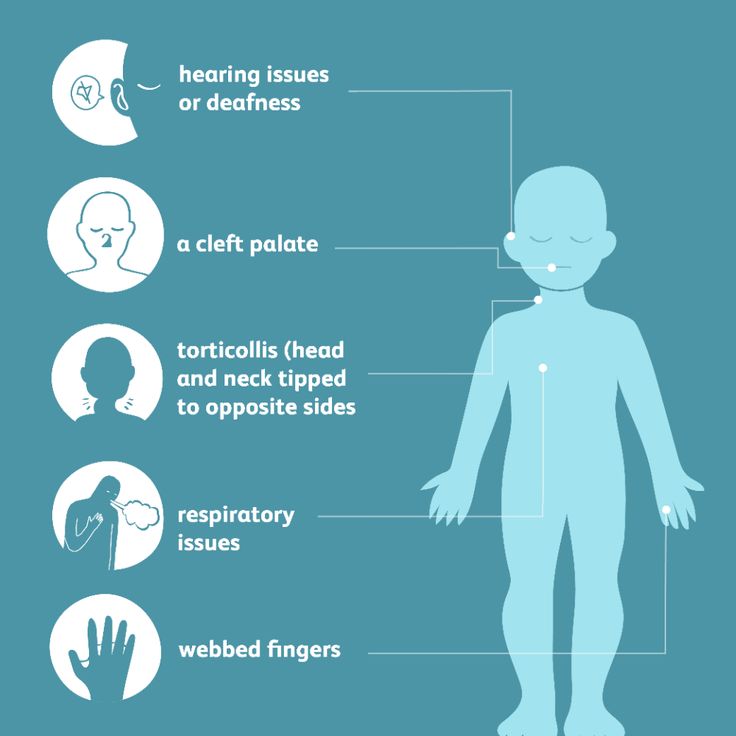
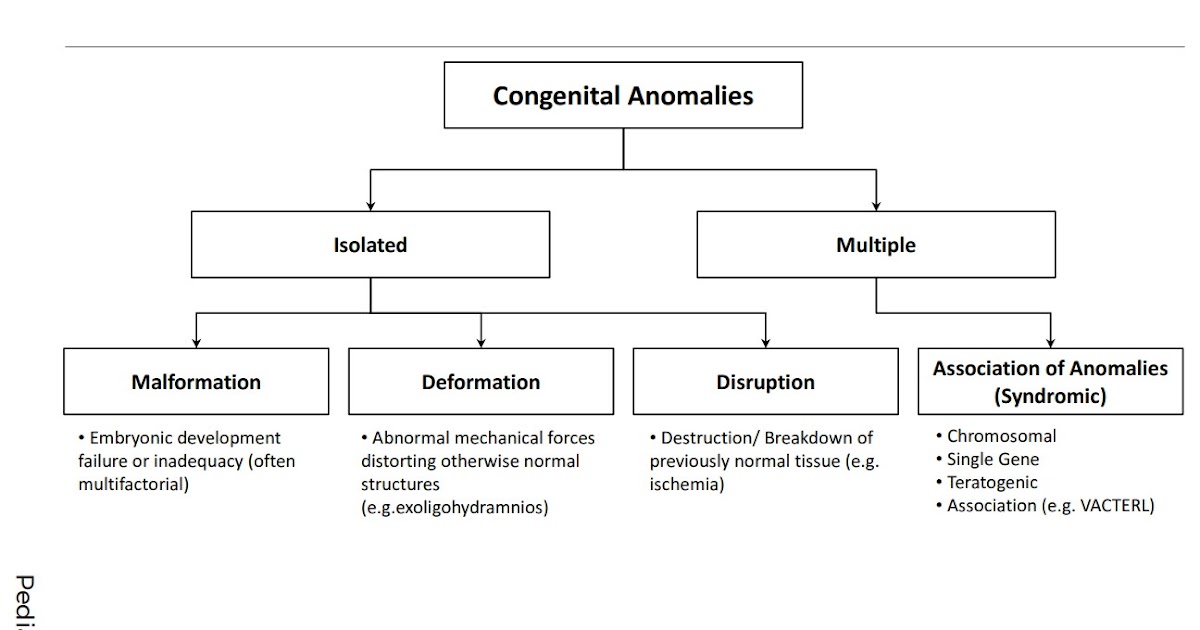
Classification by developmental mechanism or clinical presentation can be important in surveillance, because the same congenital anomaly can have different etiologies. Futhermore, the distinction may be important both clinically and in etiological studies. Please refer to Appendix C for more information about the causes of congenital anomalies and their classification according to developmental mechanism and clinical presentation.
| Box 1.2. Selected external minor congenital anomalies | |
|---|---|
| Absent nails Accessory tragus Anterior anus (ectopic anus) Auricular tag or pit Bifid uvula or cleft uvula Branchial tag or pit Camptodactyly Cup ear Cutis aplasia (if large, this is a major anomaly) Ear lobe crease Ear lobe notch Ear pit or tag Extra nipples (supernumerary nipples) Facial asymmetry Hydrocele Hypoplastic fingernails Hypoplastic toenails Iris coloboma | Lop ear Micrognathia Natal teeth Overlapping digits Plagiocephaly Polydactyly type B tag, involves hand and foot Preauricular appendage, tag or lobule Redundant neck folds Rocker-bottom feet Single crease, fifth finger Single transverse palmar crease Single umbilical artery Small penis (unless documented as micropenis) Syndactyly involving second and third toes Tongue-tie (ankyloglossia) Umbilical hernia Undescended testicle Webbed neck (pterygium colli) |
2. Planning Activities and Tools
Planning Activities and Tools
Congenital anomalies
Congenital anomalies- All topics »
- A
- B
- C
- D
- E
- F
- G
- H
- I
- J
- K
- L
- M
- N
- O
- P
- Q
- R
- S
- T
- U
- V
- W
- X
- Y
- Z
- Resources »
- Fact sheets
- Facts in pictures
- Multimedia
- Publications
- Questions & answers
- Tools and toolkits
- Popular »
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Monkeypox
- All countries »
- A
- B
- C
- D
- E
- F
- G
- H
- I
- J
- K
- L
- M
- N
- O
- P
- Q
- R
- S
- T
- U
- V
- W
- X
- Y
- Z
- Regions »
- Africa
- Americas
- South-East Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- WHO in countries »
- Statistics
- Cooperation strategies
- Ukraine emergency
- All news »
- News releases
- Statements
- Campaigns
- Commentaries
- Events
- Feature stories
- Speeches
- Spotlights
- Newsletters
- Photo library
- Media distribution list
- Headlines »
- Focus on »
- Afghanistan crisis
- COVID-19 pandemic
- Northern Ethiopia crisis
- Syria crisis
- Ukraine emergency
- Monkeypox outbreak
- Greater Horn of Africa crisis
- Latest »
- Disease Outbreak News
- Travel advice
- Situation reports
- Weekly Epidemiological Record
- WHO in emergencies »
- Surveillance
- Research
- Funding
- Partners
- Operations
- Independent Oversight and Advisory Committee
- WHO's Health Emergency Appeal 2023
- Data at WHO »
- Global Health Estimates
- Health SDGs
- Mortality Database
- Data collections
- Dashboards »
- COVID-19 Dashboard
- Triple Billion Dashboard
- Health Inequality Monitor
- Highlights »
- Global Health Observatory
- SCORE
- Insights and visualizations
- Data collection tools
- Reports »
- World Health Statistics 2022
- COVID excess deaths
- DDI IN FOCUS: 2022
- About WHO »
- People
- Teams
- Structure
- Partnerships and collaboration
- Collaborating centres
- Networks, committees and advisory groups
- Transformation
- Our Work »
- General Programme of Work
- WHO Academy
- Activities
- Initiatives
- Funding »
- Investment case
- WHO Foundation
- Accountability »
- Audit
- Programme Budget
- Financial statements
- Programme Budget Portal
- Results Report
- Governance »
- World Health Assembly
- Executive Board
- Election of Director-General
- Governing Bodies website
- Member States Portal
- Home/
- Health topics/
- Congenital anomalies
UNICEF/Noorani
Newborn baby in Timor-Leste
© Credits
Fact sheets
Questions and answers
Guidelines
Databases and tools
Resolutions and decisions
Technical work
- Newborn Health Unit
- Maternal, Newborn, Child and Adolescent Health and Ageing
- Nutrition and Food Safety
- Sensory Functions, Disability and Rehabilitation
- Sexual and Reproductive Health
Our work
News
All →Publications
All →A wide range of causes of congenital anomalies means that a portfolio of prevention approaches is needed including prevention of sexually transmitted infections,. ..
..
Congenital anomalies, also known as birth defects, are structural or functional abnormalities, including metabolic disorders, that are present from birth....
Survive and thrive: transforming care for every small and sick newborn maps out a pathway towards 2030. It is built upon epidemiology, historical trends,...
Feature stories
Related health topics
Malformations
Malformations- Healthcare issues »
- A
- B
- B
- G
- D
- E
- and
- 9000 O
- M
- R
- S
- T
- Y
- F
- X
- C
- W 0005
- B
- S
- B
- E
- S
- I
- Popular Topics
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Data and statistics »
- News bulletin
- The facts are clear
- Publications
- Find country »
- A
- B
- in
- g
- d
- E
- С
- and
- L
- m
- N 9000
- t
- in
- x
- 9000 WHO in countries »
- Reporting
- Regions »
- Africa
- America
- Southeast Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- Media Center
- Press releases
- Statements
- Media messages
- Comments
- Reporting
- Online Q&A
- Events
- Photo reports
- Questions and answers
- Update
- Emergencies "
- News "
- Disease Outbreak News
- WHO Data »
- Dashboards »
- COVID-19 Monitoring Dashboard
- Basic moments "
- About WHO »
- CEO
- About WHO
- WHO activities
- Where does WHO work?
- Governing Bodies »
- World Health Assembly
- Executive committee
- Main page/
- Media Center /
- Newsletters/
- Read more/
- Malformations
\n
- \n
- development and strengthening of registration and surveillance systems; \n
- experience and capacity building; \n
- strengthening research and scientific work in the field of etiology, diagnosis and prevention; \n
- strengthening international cooperation.
 \n
\n
\n
Definition
\n
\nCongenital malformations are also referred to as congenital malformations, congenital disorders, or congenital deformities. Congenital malformations can be defined as structural or functional abnormalities (eg, metabolic disorders) that appear in utero and may be identified before birth, during birth, or later in life.
\n
Causes and risk factors
\n
\nApproximately 50% of all malformations cannot be attributed to any specific cause, but some causes or risk factors are known.
\n
Socio-economic factors
\n
\nAlthough low income may be an indirect determinant, malformations are more likely to occur in families and countries with insufficient resources. It is estimated that approximately 94% of severe malformations occur in middle- and low-income countries, where women often do not have access to sufficient and good enough food and may be exposed to some agent or factor, such as infection or alcohol, that provokes or enhances deviations from the norm in prenatal development.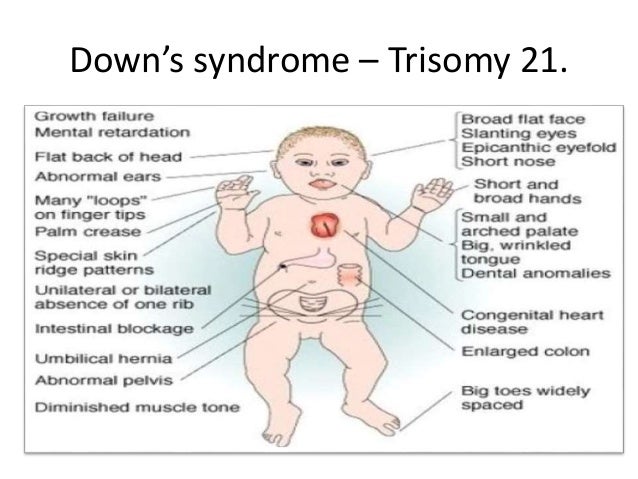 Moreover, motherhood in adulthood increases the risk of chromosomal abnormalities, including Down's syndrome, while motherhood at a young age increases the risk of certain congenital malformations.
Moreover, motherhood in adulthood increases the risk of chromosomal abnormalities, including Down's syndrome, while motherhood at a young age increases the risk of certain congenital malformations.
\n
Genetic factors
\n
\nIncest (consanguinity) increases the prevalence of rare genetic birth defects and almost doubles the risk of neonatal and infant mortality, mental retardation and severe birth defects in children born to first cousins . Some ethnic groups, such as Ashkenazi Jews and Finns, have a relatively high prevalence of rare genetic mutations that lead to an increased risk of malformations.\n
\n
Infections
\n
\nMaternal infections such as syphilis or measles are a common cause of birth defects in low- and middle-income countries.
\n
Maternal nutrition
\n
\nDeficiencies in iodine, folate, obesity, or conditions such as diabetes mellitus are associated with some malformations.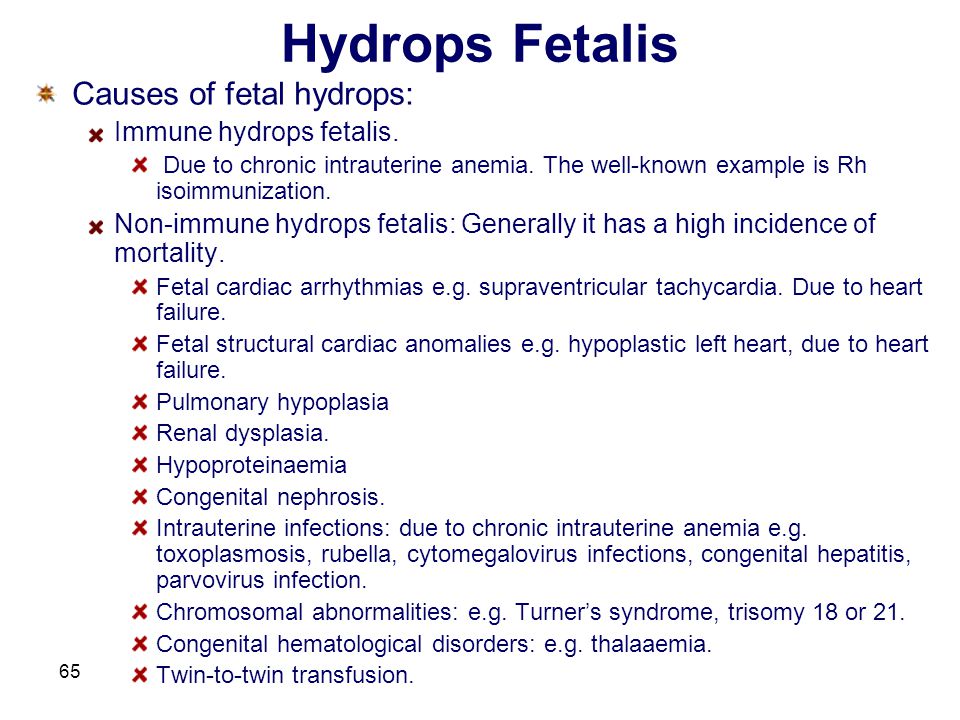 For example, folic acid deficiency increases the risk of having a baby with a neural tube defect. In addition, increased intake of vitamin A may affect the normal development of the embryo or fetus.
For example, folic acid deficiency increases the risk of having a baby with a neural tube defect. In addition, increased intake of vitamin A may affect the normal development of the embryo or fetus.
\n
Environmental factors
\n
\nMaternal exposure to certain pesticides and other chemicals, as well as certain drugs, alcohol, tobacco, psychoactive substances, or radiation during pregnancy may increase the risk of developing the fetus or a newborn baby with birth defects. Working or living near or close to landfills, smelters, or mines can also be a risk factor, especially if the mother is exposed to other environmental risk factors or malnutrition.
\n
Prevention
\n
\nPregnancy and conception preventive health care, and prenatal care, reduce the incidence of some birth defects. Primary prevention of malformations includes the following measures:
\n
- \n
- Improving the nutrition of women during the reproductive period by ensuring adequate intake of vitamins and minerals, especially folic acid, as a result of daily oral supplementation or fortification of staple foods, such as wheat or corn flour.
 \n
\n - Supervise that a pregnant woman does not consume or consume in a limited amount unhealthy foods, especially alcohol. \n
- Pre-pregnancy and pregnancy prevention of diabetes through counseling, weight management, proper nutrition, and, if necessary, insulin administration. \n
- Prevention of exposure to environmental hazardous substances (eg, heavy metals, pesticides, certain drugs) during pregnancy. \n
- Ensuring that any exposure of a pregnant woman to drugs or medical exposures (such as x-rays) is justified and based on a careful analysis of the health risks and benefits. \n
- Increase vaccination coverage for women and children, especially against rubella. This disease can be prevented by vaccinating children. Rubella vaccine may also be given at least one month before pregnancy to women who did not receive the vaccine or who did not have rubella in childhood. \n
- Increase vaccination coverage for women and children, especially against rubella virus.
 This disease can be prevented by vaccinating children. Rubella vaccine may also be given to women who are not immune to the disease at least one month before pregnancy. \n
This disease can be prevented by vaccinating children. Rubella vaccine may also be given to women who are not immune to the disease at least one month before pregnancy. \n - Scaling up and intensifying training for health professionals and other staff involved in strengthening malformation prevention. \n
\n
Identification
\n
\nPre-conception (pre-conception) and near conception (peri-conception) health care includes basic reproductive health care as well as medical genetic screening and counseling. Screening can be carried out during the three periods listed below.
\n
- \n
- Pre-pregnancy screening is designed to identify people who are at risk of developing certain health conditions or at risk of passing on any health conditions to their children. Screening includes family medical history and vector screening. Screening is especially important in countries where incestuous marriages are common.
 \n
\n - Preconception screening: Maternal characteristics may increase risk, and screening results should be used to provide appropriate care based on risk. During this period, screening of young and mature mothers, as well as screening for the use of alcohol, tobacco and other psychoactive substances, can be carried out. Ultrasound can be used to detect Down's syndrome during the first trimester of pregnancy and severe fetal malformations during the second trimester. Additional tests and amniocentesis help detect neural tube defects and chromosomal abnormalities during the first and second trimesters of pregnancy. \n
- Newborn screening includes a clinical examination and screening for hematological, metabolic, and hormonal disorders. Screening for deafness and heart disease, and early detection of birth defects, can facilitate life-saving treatment and prevent progression of the defect, which could lead to some form of physical, mental, or visual or hearing disability.
 In some countries, all newborns are screened for thyroid and adrenal abnormalities before being discharged from the maternity ward. \n
In some countries, all newborns are screened for thyroid and adrenal abnormalities before being discharged from the maternity ward. \n
\n
Treatment and care
\n
\nIn countries with adequate health services, structural congenital malformations can be corrected with pediatric surgery and children with functional problems such as thalassemia (inherited by recessive blood disease), sickle cell disorders, and congenital hypothyroidism.
\n
WHO activities
\n
\nIn 2010, the World Health Assembly published a report on birth defects. The report outlines the main components of establishing national programs for the prevention and care of birth defects before and after birth. The report also recommends priority actions for the international community to help establish and strengthen such national programs.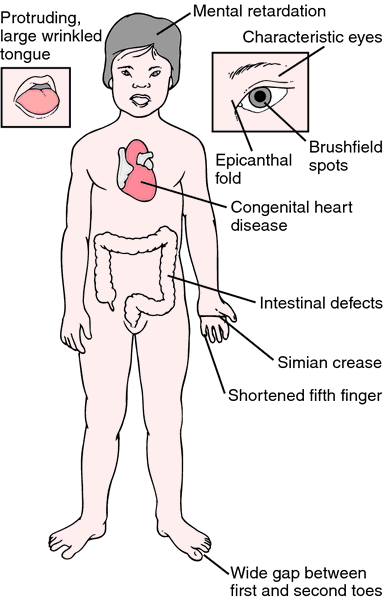
\n
\nThe Global Strategy for Women's and Children's Health, announced in September 2010 by the United Nations in collaboration with government leaders and other organizations such as WHO and UNICEF, plays a critical role in implementing efficient and cost-effective action to promote newborn and child health.\n
\n
\nWHO is also working with the National Center for Birth and Developmental Disorders, part of the US Centers for Disease Control and Prevention (CDC), and other partners to develop a global policy to fortify foods with salt folic acid at the country level. In addition, WHO is working with partners to provide the necessary technical expertise to conduct surveillance of neural tube defects, monitor efforts to fortify foods with folic acid salts, and strengthen laboratory capacity to assess risks for birth defects prevented by folic acid salts.
\n
\nThe International Clearing House for Surveillance and Research on Birth Defects is a voluntary, non-profit, international organization in official relations with WHO.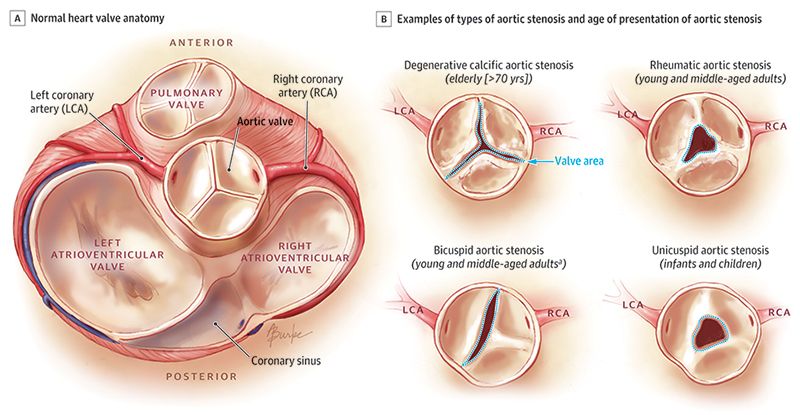 This organization collects surveillance data on birth defects and research programs around the world to study and prevent birth defects and mitigate their effects.
This organization collects surveillance data on birth defects and research programs around the world to study and prevent birth defects and mitigate their effects.
\n
\nThe WHO Departments of Reproductive Health and Research and Nutrition for Health and Development, in collaboration with the International Clearing House for Surveillance and Research on Birth Defects and the CDC National Center for Birth Defects and Development, organize annual seminars on surveillance and prevention of birth defects and preterm birth. The WHO Department of HIV/AIDS is collaborating with these partners to strengthen surveillance for malformations among women receiving antiretroviral drugs during pregnancy as an integral part of the monitoring and evaluation of national HIV programs.
\n
\nThe GAVI Alliance, partnered with WHO, is helping developing countries to increase the control and elimination of rubella and congenital rubella syndrome through immunization.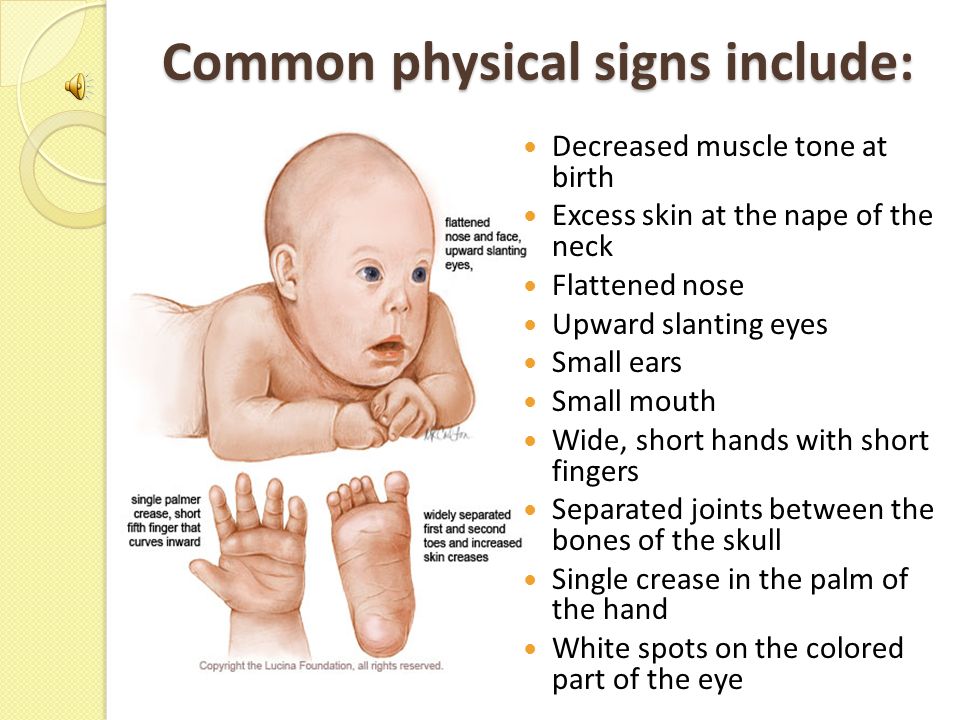
\n
\nWHO is developing normative tools, including guidelines and a global action plan to strengthen health care and rehabilitation services in support of the implementation of the Convention on the Rights of Persons with Disabilities. Similarly, WHO is helping countries integrate health care and rehabilitation services into general primary health care, supporting the development of community-based rehabilitation programs and strengthening specialized rehabilitation centers and their links with community-based rehabilitation centers.
\n
United Nations Convention on the Rights of Persons with Disabilities
\n
\nThe WHO Department of Public Health and Environment works across a range of activities and develops interventions to address the environmental and social determinants of child development. These include: child-only vulnerability to indoor and outdoor air pollution, water pollution, lack of basic hygiene, toxic compounds, heavy metals, waste components and radiation exposure; mixed impact of factors related to the social environment, professional activities and nutrition, as well as the living conditions of children (home, school).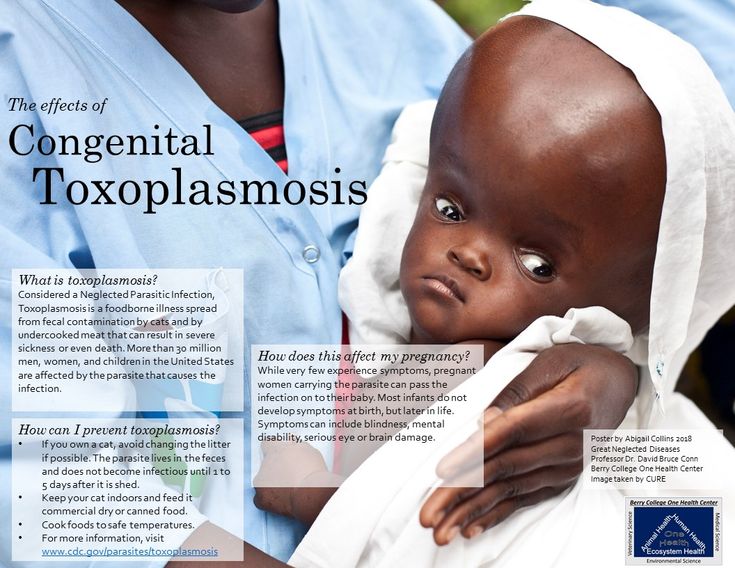
\n
","datePublished":"2022-02-28T22:52:00.0000000+00:00","image":"https://cdn.who.int/media/images/default -source/imported/preterm-birth-mother-jpg.jpg?sfvrsn=c5c1adf1_0","publisher":{"@type":"Organization","name":"World Health Organization: WHO","logo": {"@type":"ImageObject","url":"https://www.who.int/Images/SchemaOrg/schemaOrgLogo.jpg","width":250,"height":60}},"dateModified ":"2022-02-28T22:52:00.0000000+00:00","mainEntityOfPage":"https://www.who.int/ru/news-room/fact-sheets/detail/congenital-anomalies", "@context":"http://schema.org","@type":"Article"};
Key Facts
- It is estimated that 303,000 children die every year from malformations during the first 4 weeks of life.
- Developmental disabilities can lead to long-term disability, with significant impacts on individuals, their families, health systems and society.
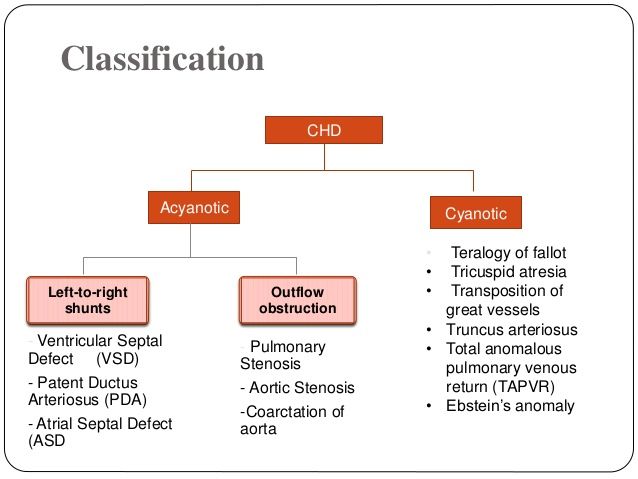
- The most severe malformations include heart defects, neural tube defects and Down's syndrome.
- Although malformations may be genetic, infectious or environmental in origin, the exact cause is often difficult to establish.
- Some birth defects can be prevented. The main elements of prevention are, inter alia, vaccination, adequate intake of folic acid or iodine through fortification of staple foods or provision of nutritional supplements, and proper prenatal care.
Malformations and preterm birth are major causes of childhood death, chronic disease and disability in many countries. In 2010, the World Health Assembly adopted a resolution calling on all Member States to promote primary prevention and health promotion for children with developmental disabilities through:
- development and strengthening of registration and surveillance systems;
- experience and capacity building;
- strengthening research and scientific work in the field of etiology, diagnosis and prevention;
- strengthening international cooperation.
Definition
Congenital malformations are also referred to as congenital malformations, congenital disorders or congenital deformities. Congenital malformations can be defined as structural or functional abnormalities (eg, metabolic disorders) that appear in utero and may be identified before birth, during birth, or later in life.
Causes and risk factors
Approximately 50% of all malformations cannot be attributed to any specific cause, but some causes or risk factors are known.
Socio-economic factors
While low income may be an indirect determinant, malformations are more likely to occur in under-resourced families and countries. It is estimated that approximately 94% of severe malformations occur in middle- and low-income countries, where women often do not have access to sufficient and good enough food and may be exposed to some agent or factor, such as infection or alcohol, that provokes or enhances deviations from the norm in prenatal development. Moreover, motherhood in adulthood increases the risk of chromosomal abnormalities, including Down's syndrome, while motherhood at a young age increases the risk of certain congenital malformations.
Moreover, motherhood in adulthood increases the risk of chromosomal abnormalities, including Down's syndrome, while motherhood at a young age increases the risk of certain congenital malformations.
Genetic factors
Incest (consanguinity) increases the prevalence of rare genetic birth defects and almost doubles the risk of neonatal and infant mortality, mental retardation and severe birth defects in children born to first cousins. Some ethnic groups, such as Ashkenazi Jews and Finns, have a relatively high prevalence of rare genetic mutations that lead to an increased risk of malformations.
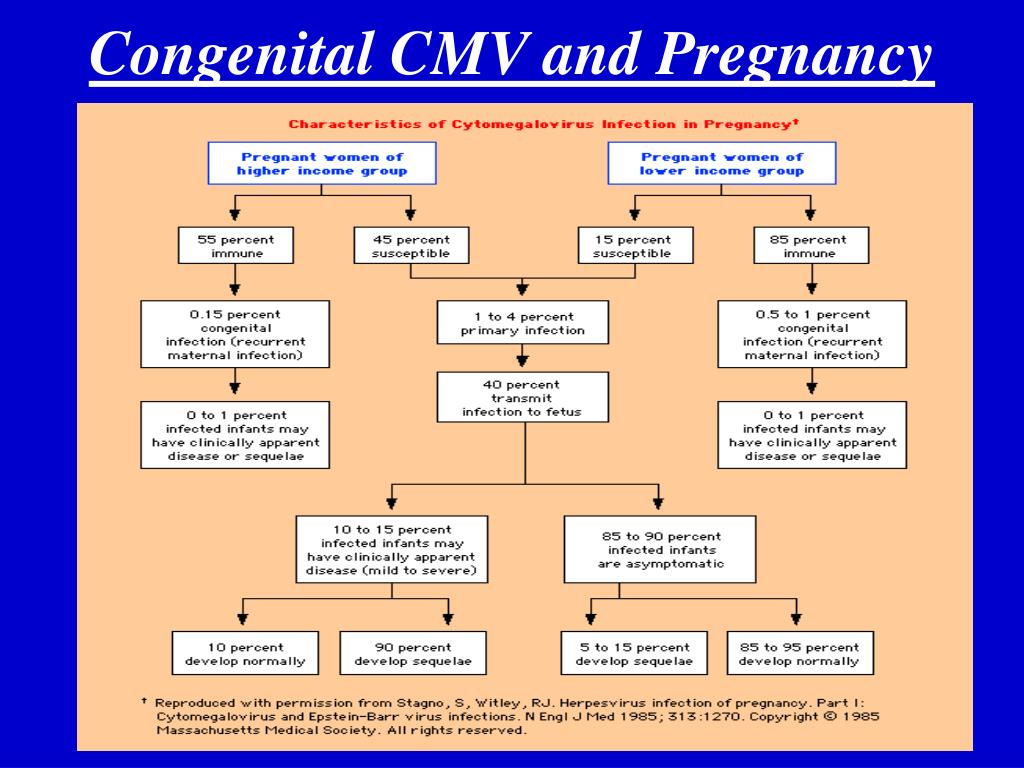
Infections
Maternal infections such as syphilis or measles are a common cause of birth defects in low- and middle-income countries.
Maternal nutrition
Deficiency of iodine, folic acid salts, obesity, or conditions such as diabetes mellitus are associated with some malformations. For example, folic acid deficiency increases the risk of having a baby with a neural tube defect.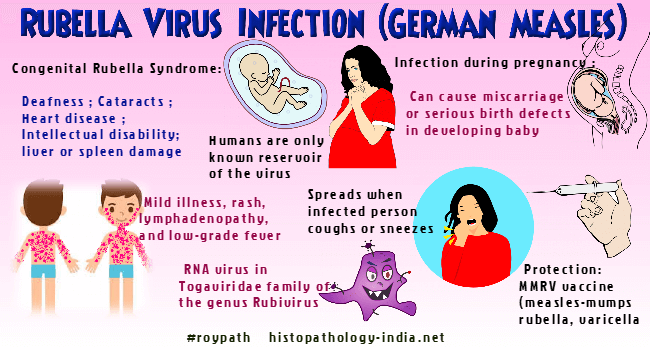 In addition, increased intake of vitamin A may affect the normal development of the embryo or fetus.
In addition, increased intake of vitamin A may affect the normal development of the embryo or fetus.
Environmental factors
Maternal exposure to certain pesticides and other chemicals, as well as certain drugs, alcohol, tobacco, psychoactive substances, or radiation during pregnancy may increase the risk of birth defects in the fetus or newborn. Working or living near or close to landfills, smelters, or mines can also be a risk factor, especially if the mother is exposed to other environmental risk factors or malnutrition.
Prevention
Preventive health care during pregnancy and conception, as well as antenatal care, reduce the incidence of some birth defects. Primary prevention of malformations includes the following:
- Improving the nutrition of women during the reproductive period by ensuring adequate intake of vitamins and minerals, especially folic acid, through daily oral supplementation or fortification of staple foods such as wheat or corn flour .
- Supervise that a pregnant woman does not consume or consume in a limited amount unhealthy foods, especially alcohol.
- Prevention of diabetes in pregnancy and during pregnancy through counseling, weight management, proper nutrition and, if necessary, insulin administration.
- Prevention during pregnancy of exposure to hazardous environmental substances (eg, heavy metals, pesticides, certain drugs).
- Ensuring that any exposure of a pregnant woman to drugs or radiation for medical purposes (eg x-rays) is justified and based on a careful analysis of the health risks and benefits.
- Increase vaccination coverage for women and children, especially against rubella virus. This disease can be prevented by vaccinating children. Rubella vaccine may also be given at least one month before pregnancy to women who did not receive the vaccine or who did not have rubella in childhood.
- Increase vaccination coverage for women and children, especially against rubella virus.
 This disease can be prevented by vaccinating children. Rubella vaccine may also be given to women who are not immune to the disease at least one month before pregnancy.
This disease can be prevented by vaccinating children. Rubella vaccine may also be given to women who are not immune to the disease at least one month before pregnancy. - Scaling up and intensifying training for health professionals and other staff involved in strengthening the prevention of malformations.
Identification
Medical care before conception (in the preconception period) and around the time of conception (in the periconceptional period) includes basic reproductive health care, as well as medical genetic screening and counseling. Screening can be carried out during the three periods listed below.
- Pre-pregnancy screening is designed to identify people who are at risk of developing certain health conditions or passing on any health conditions to their children. Screening includes family medical history and vector screening. Screening is especially important in countries where incestuous marriages are common.
- Preconception screening: Maternal characteristics may increase risk and screening results should be used to provide appropriate care based on risk.
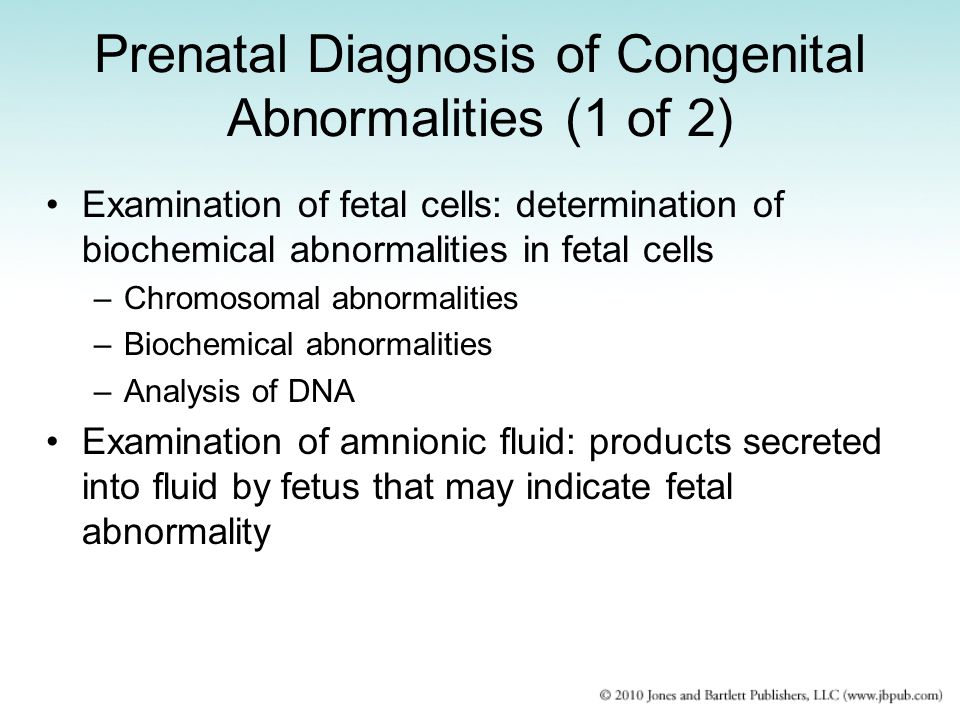
 During this period, screening of young and mature mothers, as well as screening for the use of alcohol, tobacco and other psychoactive substances, can be carried out. Ultrasound can be used to detect Down's syndrome during the first trimester of pregnancy and severe fetal malformations during the second trimester. Additional tests and amniocentesis help detect neural tube defects and chromosomal abnormalities during the first and second trimesters of pregnancy.
During this period, screening of young and mature mothers, as well as screening for the use of alcohol, tobacco and other psychoactive substances, can be carried out. Ultrasound can be used to detect Down's syndrome during the first trimester of pregnancy and severe fetal malformations during the second trimester. Additional tests and amniocentesis help detect neural tube defects and chromosomal abnormalities during the first and second trimesters of pregnancy. - Newborn screening includes a clinical examination, as well as screening for hematological, metabolic and hormonal disorders. Screening for deafness and heart disease, and early detection of birth defects, can facilitate life-saving treatment and prevent progression of the defect, which could lead to some form of physical, mental, or visual or hearing disability. In some countries, all newborns are screened for thyroid and adrenal abnormalities before being discharged from the maternity ward.
Treatment and medical care
In countries with adequate health services, structural birth defects can be corrected with pediatric surgery and timely treatment can be provided for children with functional problems such as thalassemia (a recessive blood disorder), sickle cell disorders, and congenital hypothyroidism.
WHO activities
In 2010, the World Health Assembly published a report on birth defects. The report outlines the main components of establishing national programs for the prevention and care of birth defects before and after birth. The report also recommends priority actions for the international community to help establish and strengthen such national programs.
The Global Strategy for Women's and Children's Health, launched in September 2010 by the United Nations in collaboration with government leaders and other organizations such as WHO and UNICEF, plays a critical role in achieving effective and cost-effective action to improve newborn health and children.
WHO is also working with the National Center for Birth and Developmental Disorders, part of the US Centers for Disease Control and Prevention (CDC), and other partners to develop a global policy for folic acid fortification at the country level. In addition, WHO is working with partners to provide the necessary technical expertise to conduct surveillance of neural tube defects, monitor efforts to fortify foods with folic acid salts, and strengthen laboratory capacity to assess risks for birth defects prevented by folic acid salts.
The International Clearing House for Surveillance and Research on Birth Defects is a voluntary, non-profit international organization in official relations with WHO. This organization collects surveillance data on birth defects and research programs around the world to study and prevent birth defects and mitigate their effects.
The WHO Departments of Reproductive Health and Research and Nutrition for Health and Development, in collaboration with the International Clearing House for Surveillance and Research on Birth Defects and the CDC National Center for Birth Defects and Development, organize annual workshops on surveillance and prevention of birth defects and premature birth. The WHO Department of HIV/AIDS is collaborating with these partners to strengthen surveillance for malformations among women receiving antiretroviral drugs during pregnancy as an integral part of the monitoring and evaluation of national HIV programs.
The GAVI Alliance, with WHO among its partners, is helping developing countries to accelerate the control and elimination of rubella and congenital rubella syndrome through immunization.
WHO is developing normative tools, including guidelines and a global action plan to strengthen health care and rehabilitation services in support of the implementation of the Convention on the Rights of Persons with Disabilities. Similarly, WHO is helping countries integrate health care and rehabilitation services into general primary health care, supporting the development of community-based rehabilitation programs and strengthening specialized rehabilitation centers and their links with community-based rehabilitation centers.
UN Convention on the Rights of Persons with Disabilities
The WHO Department of Public Health and Environment works across a range of activities and develops interventions to address the environmental and social determinants of child development. These include: child-only vulnerability to indoor and outdoor air pollution, water pollution, lack of basic hygiene, toxic compounds, heavy metals, waste components and radiation exposure; mixed impact of factors related to the social environment, professional activities and nutrition, as well as the living conditions of children (home, school).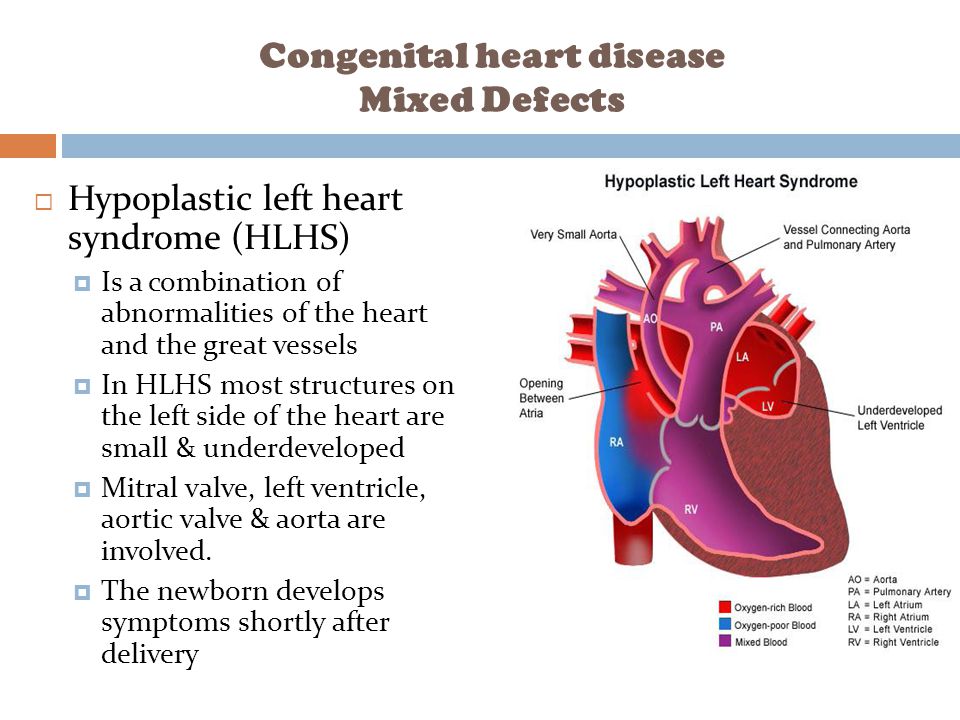
Congenital malformations of the fetus | Official website (Health Institution "Malorita Central District Hospital")
Congenital malformations (CM) are in third place among the factors leading to fetal death during pregnancy, childbirth and the postpartum period.
Complications caused by these defects can affect a person's health throughout life. Distinguish malformations:
- easily correctable;
- incompatible with life;
- compatible with life, but significantly complicating it.
Congenital malformations occur as a result of violations of intrauterine development of the fetus. Congenital malformations are the most serious threat to the normal development of pregnancy, which in most cases leads to childhood disability and mortality. Among congenital malformations, there are anencephaly (underdevelopment of the brain), malformations of the nervous system, heart defects, back Bifida (external hernia of the spinal cord), malformations of the limbs or their absence, maxillofacial deformities, in particular the cleft palate, cleft lip, etc.
Why is this happening?
The causes of congenital malformations can be very diverse.
Quite often, the cause is hereditary factors, in particular, deviations in the set of chromosomes of one or both parents. Various harmful factors, such as infections (measles, chicken pox, rubella, cytomegalovirus), drug use or large doses of alcohol, can also lead to the development of malformations in the fetus.
A common cause of congenital malformations is a deficiency of vitamins in the diet of a pregnant woman, in particular a lack of folic acid. Naturally, the correct lifestyle of a pregnant woman and the diet are important factors for the development of a healthy child. Conversely, a lack of vitamins often causes a failure in the development of the mental and physical abilities of the baby.
Influence of negative environmental factors: x-rays, ionizing radiation, atomic energy, etc. Exposure to negative chemical factors can lead to fetal hypoxia and cause the formation of congenital malformations of the fetus.
Substances of particular concern include nicotine, mercury, contraceptives, benzene, paints and certain drugs.
Mechanical factors such as uterine tumors, fetal malposition, egg implantation can cause anomalies such as spina bifida, neural tube abnormalities. Maternal injuries during pregnancy and endocrine diseases are also predisposing factors in the formation of congenital malformations.
It should be noted that in almost half of cases of congenital malformations in the fetus, the causes of their occurrence remain unclear.
Gross congenital malformations (CM) occur in 2-6% of newborns. The database of the Belarusian Register of VPR is replenished annually with more than 2.5 thousand observations. The first place in the structure of registered developmental anomalies is occupied by heart defects, which in total account for about a third of all diagnosed cases (1 per 150 newborns). A group of multiple congenital malformations and chromosomal pathology (1 out of 200 newborns), as well as neural tube defects (1 out of 600 newborns) is quite common. Cleft lip/palate is common (1 in 800 newborns). At the current level of development of prenatal diagnosis, more than ⅓ of CM is diagnosed in utero, which makes it possible to terminate a pregnancy with such a pathology in the fetus. In recent years, more than 600 pregnancies have been terminated in the Republic in connection with the detection of fetal congenital malformations.
Cleft lip/palate is common (1 in 800 newborns). At the current level of development of prenatal diagnosis, more than ⅓ of CM is diagnosed in utero, which makes it possible to terminate a pregnancy with such a pathology in the fetus. In recent years, more than 600 pregnancies have been terminated in the Republic in connection with the detection of fetal congenital malformations.
How are congenital malformations diagnosed?
In our time, thanks to the achievements of modern medicine, early diagnosis of congenital pathology in the prenatal period is possible.
There are indirect and direct methods for diagnosing congenital malformations of the fetus.
Indirect methods for diagnosing congenital malformations: blood tests for AFP, hCG, hormones, immunological, serological, genetic tests that pregnant women undergo during the first visit to a medical genetic consultation up to 13 weeks of pregnancy. Based on the results of these studies, the presence or high risk of congenital malformations of the fetus can be assumed.
In addition to these research methods, all pregnant women undergo non-invasive direct methods for diagnosing congenital malformations - this is an ultrasound examination of the fetus (ultrasound), which is performed 3 times during the entire pregnancy, but additional procedures are prescribed if necessary. Since by the 19-20th week almost all organs and systems have already been formed, congenital malformations of the fetus are visible on ultrasound in 80-86% of cases.
Information obtained after the diagnosis of congenital malformations is necessary to make a decision on further management of the patient:
emergency treatment of birth defects;
childbirth in specialized institutions for the timely treatment of congenital malformations;
termination of pregnancy in case of inability to treat a congenital defect and disorders incompatible with life.
Prevention of congenital malformations
Most pregnant women first go to the doctor for a period of 8-10 weeks of pregnancy or even later, that is, at those times when many potentially dangerous moments in fetal development have already passed.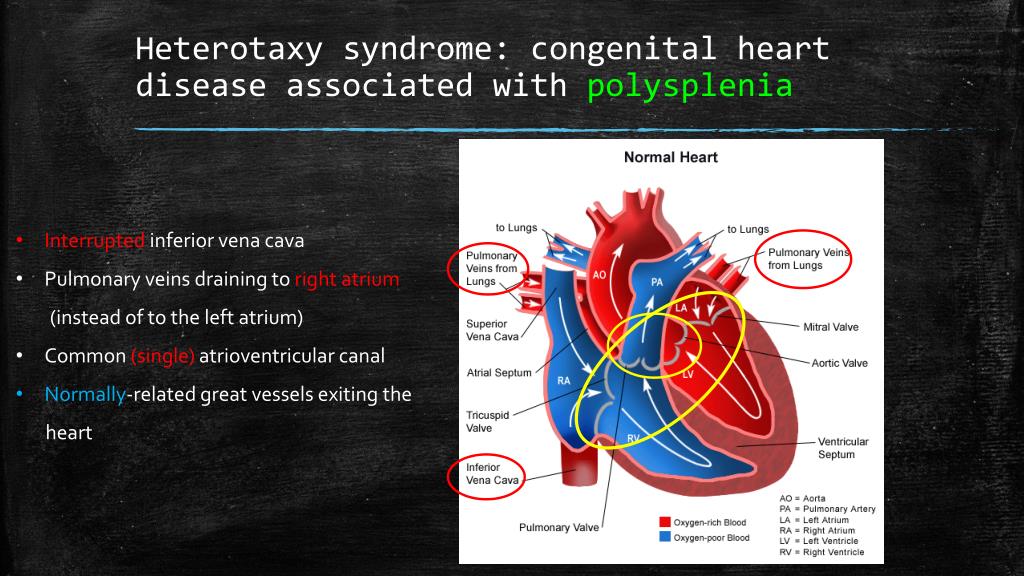
About half of all pregnancies are unplanned, often women are not aware of their situation in the early stages and continue to lead a normal life - smoking, drinking alcohol, taking various medications and dietary supplements, harming the development of their unborn child. In addition, in our time, there are still cases of non-appearance of patients for registration due to pregnancy, thereby depriving their unborn child, if he has congenital malformations, of timely surgical treatment in a specialized medical institution in Minsk and keeping him life.
The ideal situation is when a woman seeks advice at the stage of pregnancy planning. Then the doctor has time to conduct all the necessary studies, draw up an individual plan for periconceptual prophylaxis, which is able to provide the best conditions for the maturation of the egg, its implantation and early development of the embryo.
What measures should be taken if a couple is planning a pregnancy?
Medical genetic examination:
where a specialist determines the degree of risk of developing a congenital malformation of the fetus. Most often, families turn to genetics in which there are hereditary or congenital pathologies in one of the relatives, or the birth of a child with congenital malformations in a married couple, as well as age couples (a wife over 35 years old, a husband over 40 years old), taking into account the fact that that the risk of having children with chromosomal abnormalities increases with age. A geneticist is designing a set of genes that allows you to determine the risk of congenital malformation of the fetus due to violations of the genetic material or the compilation of incorrect combinations,
Most often, families turn to genetics in which there are hereditary or congenital pathologies in one of the relatives, or the birth of a child with congenital malformations in a married couple, as well as age couples (a wife over 35 years old, a husband over 40 years old), taking into account the fact that that the risk of having children with chromosomal abnormalities increases with age. A geneticist is designing a set of genes that allows you to determine the risk of congenital malformation of the fetus due to violations of the genetic material or the compilation of incorrect combinations,
determines the carriage of major mutations in phenylketonuria, cystic fibrosis, Duchenne myodystrophy, hereditary breast cancer, Tay-Sachs disease, thalassemia, sensorineural hearing loss, etc., HLA typing, determination of the level of homocysteine in blood plasma.
Test for infectious diseases
HIV, Syphilis, hepatitis B and C, toxoplasmosis, herpes, CMS, rubella. Research to identify common sexually transmitted infections.
Research to identify common sexually transmitted infections.
If necessary - immunization against hepatitis B, rubella, chickenpox
If necessary - treatment of chronic infectious diseases in both spouses.
Recommendations for uninfected women on how to reduce the risk of contracting viral infections and toxoplasmosis: frequent hand washing, reducing contact with preschool children, avoiding contact with raw meat, open ground, cats.
Industrial and environmental hazards
Assessment of the risk of industrial hazards. Exclusion of contact with solvents, dyes, pesticides.
Pay attention to chemicals commonly used in everyday life. Minimize contact with them, if possible, replace them with safe analogues - soda, laundry soap, etc.
General health assessment
You should undergo an annual medical examination and discuss with your doctor which drugs pose the least threat to the development of pregnancy. Write down the names of drugs that can be taken during pregnancy with fever, allergies, and other common situations.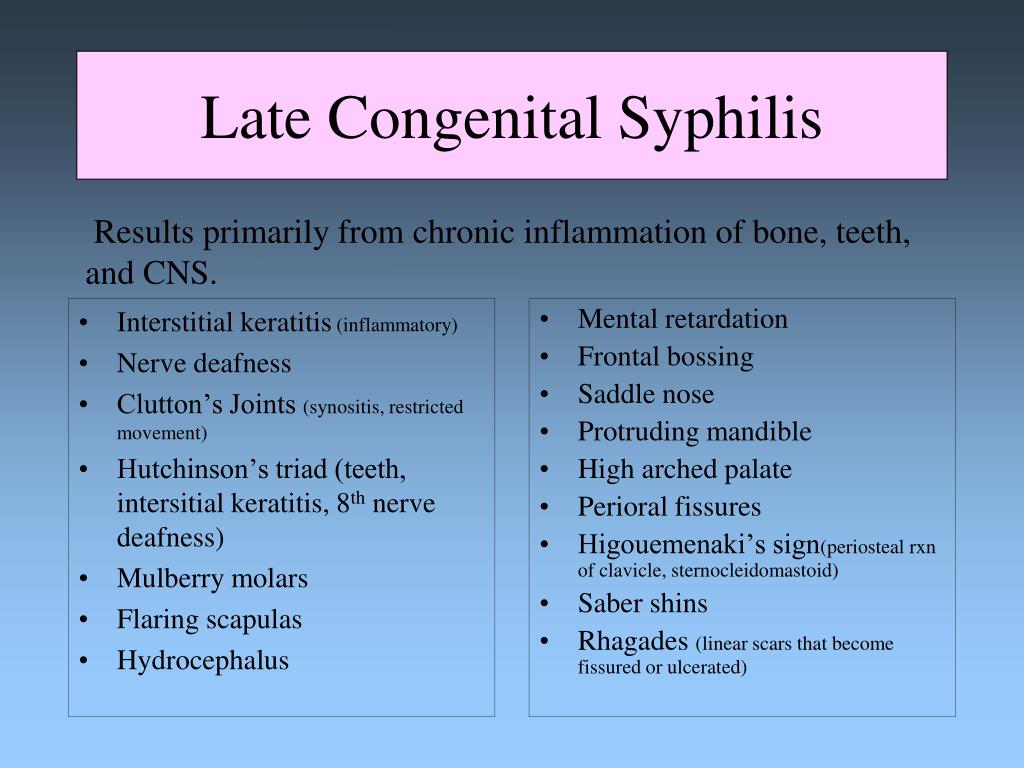
Visit a dentist and treat existing caries;
If you have a chronic disease that requires continuous medication, ask a specialist to choose the safest treatment regimen and follow it
Health and bad habits monitoring
Stop smoking;
Minimize the amount of alcoholic beverages;
Avoid taking narcotic and psychotropic substances;
Limit caffeinated drinks to two cups a day;
Normalization of nutrition
Eliminate the risk of nutritional deficiencies. Discuss with your doctor the problem of restrictive diets, if you follow them.
Avoid vitamin overdose, do not exceed:
Vitamin A no more than 3000 IU/day;
Vitamin D no more than 400 IU/day;
Folic acid supplementation at 400 mcg/day for healthy women and 1000 mcg per day for patients with diabetes and epilepsy. If a woman already has a child born with defects in the development of the neural tube, then the dose is increased to 4 mg per day. Folic acid intake should be started 3 months before conception and continued for the first 3 months of pregnancy;
Folic acid intake should be started 3 months before conception and continued for the first 3 months of pregnancy;
Remember that excess weight is just as dangerous for the normal development of pregnancy as underweight;
Normalize a varied diet;
Healthy lifestyle advice
Maintain regular moderate exercise, walk outdoors as a rule;
Avoid overheating: visits to the sauna, infrared cabins, solarium, etc.
Unfortunately, even in countries with active campaigning, the proportion of pregnant women who receive preconception training as recommended, as a rule, does not exceed one third. By the time a woman realizes that she is pregnant, many preventive opportunities have already been missed.
Therefore, in order to increase the effectiveness of ongoing measures to prevent the birth of children with congenital malformations, it is first of all necessary to significantly increase the percentage of planned pregnancies.
Separately, we should dwell on chronic diseases that affect young women who are planning a pregnancy.
Diabetes mellitus is the most well-studied disease in terms of adverse effects on pregnancy. If a woman with diabetes or impaired glucose tolerance plans to become pregnant, she should receive full treatment at least a few months before the intended conception.
Those women who have elevated glycated hemoglobin levels (>8.4%) have a 32% risk of miscarriage. In the case of full-term pregnancies in these cases, the risk of congenital fetal anomalies exceeds 7 times the risk compared to the risk that diabetic women have, whose disease is well controlled.
Treatment of diabetes mellitus, started a few months before conception, significantly reduces the risk of miscarriage and congenital malformations. General recommendations for those women who have carbohydrate metabolism disorders when planning pregnancy are:
Use of strict contraception until a thorough diagnosis and treatment is in place to control blood sugar levels;
Following a balanced diet, compulsory exercise;
Careful monitoring of glucose levels by regular determination of fructosamine or glycated hemoglobin;
Hypertension during pregnancy can provoke the development of quite serious complications. Therefore, in this case, more careful monitoring of the risk of developing preeclampsia, kidney damage and intrauterine fetal growth retardation is carried out. Women suffering from hypertension should avoid unplanned pregnancy.
Therefore, in this case, more careful monitoring of the risk of developing preeclampsia, kidney damage and intrauterine fetal growth retardation is carried out. Women suffering from hypertension should avoid unplanned pregnancy.
When planning pregnancy in a woman treated for high blood pressure, the attending physician should exclude drugs with a potential teratogenic effect from the regimen. During the 1st and 2nd trimester of pregnancy, angiotensin-converting factor inhibitors, angiotensin II receptor antagonists and thiazide diuretics should be discontinued. When planning a pregnancy, you should consult a doctor to select a treatment that is safe for the fetus.
Epilepsy. Children born to mothers with epilepsy have an increased risk of congenital malformations. This risk may be due to ongoing anticonvulsant treatment or reflect existing genetic prerequisites.
Women suffering from epilepsy should receive adequate treatment during pregnancy, as the fetus experiences significant hypoxia during the development of a convulsive episode.
Increased doses of folic acid should be given along with seizure control treatment. It is also mandatory to undergo genetic counseling to determine the risk of epilepsy in a child.
A large number of drugs used to treat epilepsy during pregnancy are unsafe due to their teratogenic risk. Optimal is the appointment of one drug in the lowest possible dosage. In the case of the treatment of a pregnant patient with epilepsy, it is not possible to recommend any one safe drug. Treatment should be carefully selected by the attending physician.
The general rule is to avoid prescribing new drugs that have been little studied in terms of teratogenic risk.
Thrombotic conditions and thromboembolism. Those women who have had an episode of thromboembolic or thrombotic disease, or in a family with an increased risk of thrombosis, should undergo a thorough examination when planning a pregnancy.
Women who have had a risk of deep venous thrombosis have a 10% risk of recurrence during pregnancy.