Placenta not attached
Placental insufficiency | Pregnancy Birth and Baby
Placental insufficiency | Pregnancy Birth and Baby beginning of content2-minute read
Listen
Sometimes the placenta does not work properly. This will mean the baby does not get the oxygen and nutrients they need. If you have placental insufficiency, your baby may not grow well or may develop complications during labour.
The condition can lead to problems both for mother and baby. It's linked to pre-eclampsia and placental abruption, when the placenta peels away from the wall of the uterus.
It can also prevent the baby from growing at a normal rate in the womb, known as intrauterine growth restriction (IUGR). There can be serious complications for the baby, including lack of oxygen during the birth, premature labour, low blood sugar, too little calcium in the blood, or too many red blood cells and sometimes even stillbirth.
What causes placental insufficiency?
Placental insufficiency occurs either because the placenta doesn’t grow properly, or because it’s damaged.
Sometimes the placenta may not grow to be big enough — for example, if you are carrying twins or more. Sometimes it has an abnormal shape or it doesn’t attach properly to the wall of the uterus.
Your lifestyle can also damage the placenta. Placental insufficiency can occur if you smoke or take some kinds of illegal drugs while you’re pregnant. Medical conditions such as diabetes, pre-eclampsia and blood clotting conditions also increase your risk.
What are the symptoms of placental insufficiency?
Placental insufficiency has no symptoms. Sometimes it’s diagnosed when women realise their baby isn’t moving as much. Other signs the baby may not be developing properly are that your abdomen is smaller than in previous pregnancies.
The condition may be picked up during your routine antenatal tests, which measure the growth of your uterus and the baby. Sometimes it’s noticed during a routine ultrasound.
Sometimes it’s noticed during a routine ultrasound.
How is placental insufficiency treated?
If your doctor suspects placental insufficiency, they will keep a close eye on your baby's growth. You will be asked to keep a record of the baby's movements and let your medical team know if you notice any changes.
Treatment will depend on the stage of the pregnancy. If you’re under 37 weeks, your doctor may decide to wait for as long as possible and keep a close eye on the baby. But if you are full term or there are signs that your baby is under stress, they may decide to induce labour or deliver the baby with a caesarean.
Sources:
MedlinePlus (Placental insufficiency), Healthline (Placental insufficiency), Department of Health (Fetal growth restriction and well-being), RANZCOG (Intrauterine Growth Restriction: Screening, Diagnosis, and Management)Learn more here about the development and quality assurance of healthdirect content.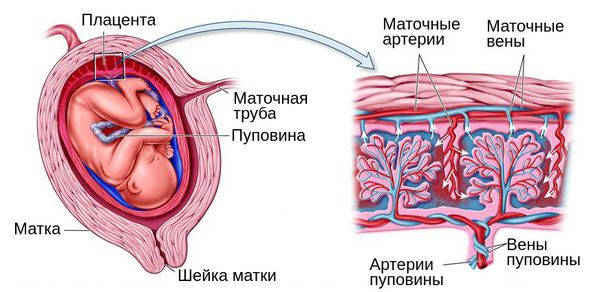
Last reviewed: February 2020
Back To Top
Related pages
- Placenta complications in pregnancy
- About the placenta
Need more information?
Causes of Preterm Labour - Miracle Babies
There are many causes of preterm birth
Read more on Miracle Babies Foundation website
Causes - Miracle Babies
Every year in Australia around 48,000 newborn babies require the help of a NICU or SCN, there are many factors linked to premature birth and also many that remain unexplained
Read more on Miracle Babies Foundation website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.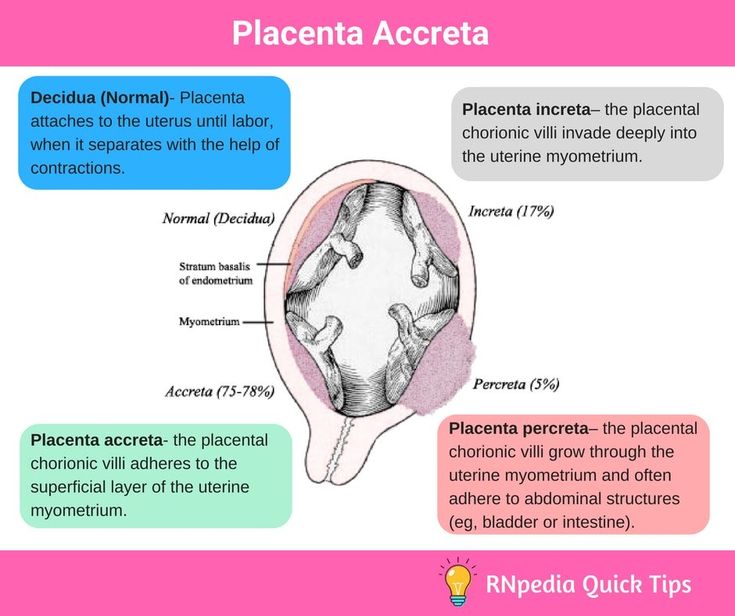
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.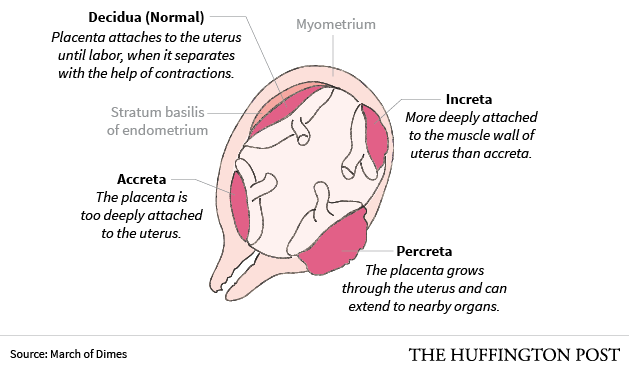
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari.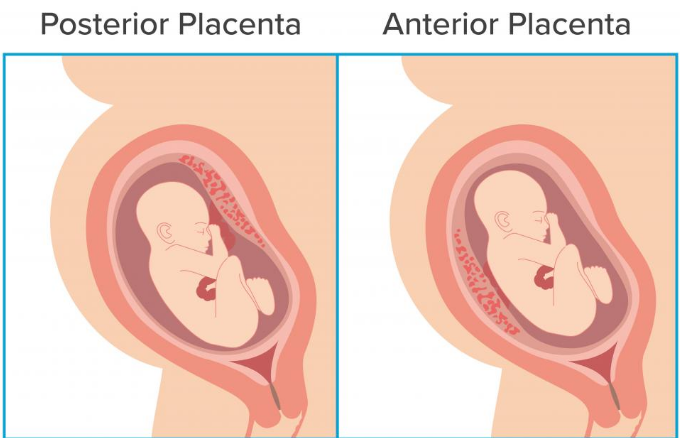 For more information, please visit the links below:
For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Causes, Symptoms, Treatment, and More
Written by WebMD Editorial Contributors
In this Article
- Causes
- Symptoms
- Complications
- Diagnosis
- Management
- Conclusion
Sometimes the placenta doesn’t grow as it should, or it may get damaged. The result may be a severe condition called placental insufficiency (also known as uteroplacental insufficiency, fetoplacental insufficiency, or placental dysfunction).
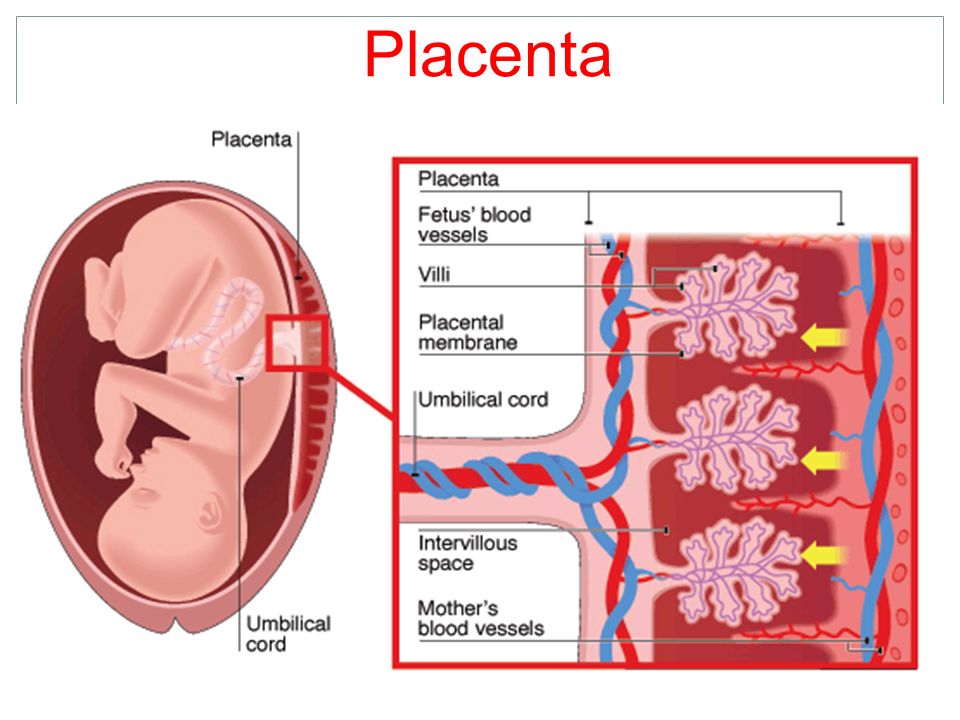
When the placenta gets damaged, the damage may reduce the amount of blood circulating between you and the placenta. This low blood flow means fewer nutrients for your baby.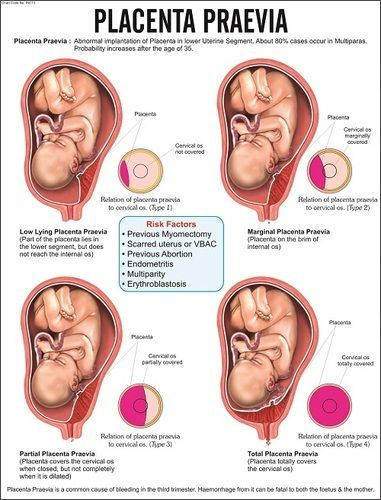 This could delay your baby’s growth in the womb.
This could delay your baby’s growth in the womb.
Causes
There are many reasons why the placenta may not be able to work well. These include:
- Diabetes
- Drug abuse (cocaine, smoking tobacco, amphetamines)
- Late delivery of the baby
- Heart and blood conditions like high blood pressure
- Medical conditions that may cause blood clots
Placental insufficiency can also occur if there are developmental issues with the placenta. Some of these issues include.
- Not holding on to the uterus as it should
- A small placenta
- The placenta being the wrong shape
- Bleeding
Symptoms
Placental insufficiency is hard to detect, especially for women experiencing pregnancy for the first time. There are usually few or no symptoms.
If you’re a mother pregnant with your second or third child, you may notice your belly is not getting as big as your previous pregnancy.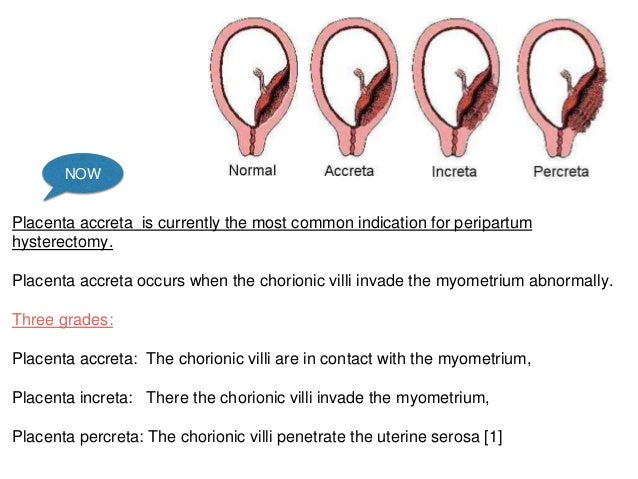 You may also realize that your child is moving less.
You may also realize that your child is moving less.
Complications
Placental insufficiency can have a severe impact on the baby. The condition leads to respiratory failure and dangerously low levels of oxygen in the baby. This can slow down the baby’s growth, induce premature labor, or kill the baby entirely.
Placental insufficiency also exposes children to multiple health problems, like:
- Anemia
- Chronic low blood sugar
- A low platelet count in the blood
- A lack of oxygen flowing to the brain
- Cognitive issues during childhood
Diagnosis
When you get to the doctor or obstetrician, they may perform some tests, like:
- Blood tests, which allow the doctors to determine the baby’s liver health.
- An ultrasound, which allows your doctor to view your placenta, estimate its size and measure how big the baby is.
- Fetal stress, a test that involves keeping track of how fast your baby’s heart is beating.

If you have been pregnant for over six months the doctor may measure the size of your belly to determine whether your baby is growing appropriately.
Quick detection of anything wrong with the placenta will improve your baby’s chances. Always consult a professional when you suspect something is wrong with your baby.
Management
Your doctor or obstetrician may choose to postpone treatment if you’ve been pregnant for less than six months and examination indicates that the baby is not in danger. You may have to get routine tests to make sure the baby is still developing healthily.
If your pregnancy has passed the thirty-seventh week or your baby is in danger, your doctor may induce labor. If labor can’t be induced with medication, you may have to give birth through a cesarean section.
There is no available effective treatment for placental insufficiency, but treating any other conditions that may be present, such as diabetes or high blood pressure may help the growing baby.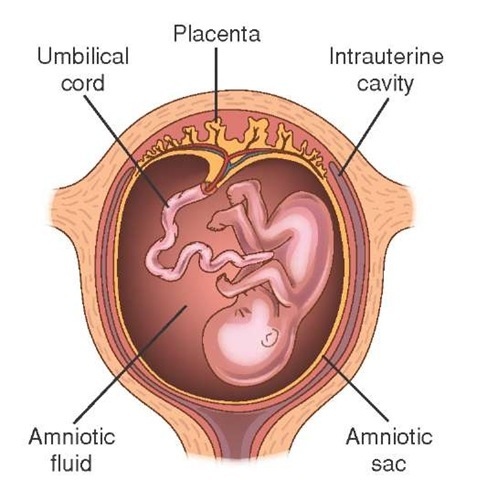
Once your doctor has diagnosed placental insufficiency, they may monitor you for hypertension. They may assign you to bed rest or refer you to a specialist. The specialist may prescribe some steroids, which may help speed up the development of your baby’s lungs. This may increase the baby’s chances of survival if you deliver prematurely.
You may get a prescription for low-dose aspirin and vitamin supplements. These may help the placenta attach itself to the uterus. If your pregnancy has reached a viable stage, the best treatment may be to induce labor.
Conclusion
The best way to manage placental insufficiency is early detection. Avoid abusing drugs, drinking alcohol, and smoking. Make sure you’re getting good prenatal care, and consult your obstetrician if you think anything’s wrong.
Low placenta
Home / Gynecologist / Low placenta
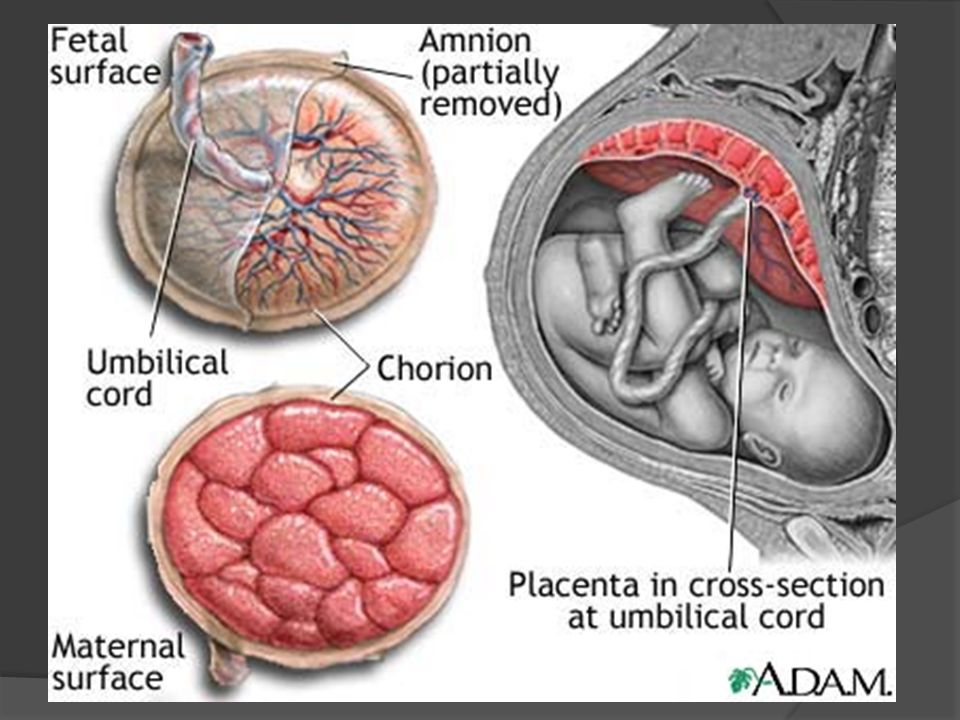
Placenta is a temporary organ that is formed in the body of a pregnant woman in order to maintain a connection between her body and the fetus.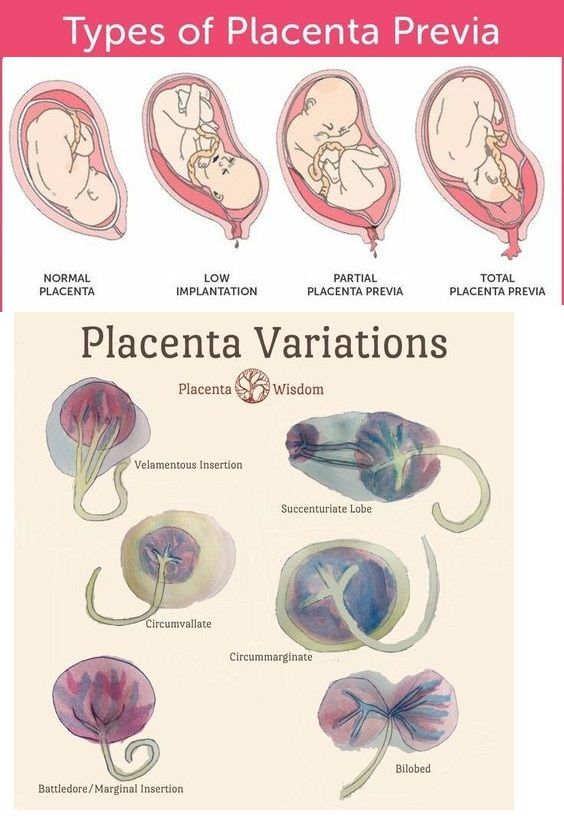 She filters the blood , which the unborn baby feeds on, cleansing it of toxins and other harmful substances.
She filters the blood , which the unborn baby feeds on, cleansing it of toxins and other harmful substances.
This pathology can be very dangerous in some cases, while in others it goes away without any treatment and does not bring problems.
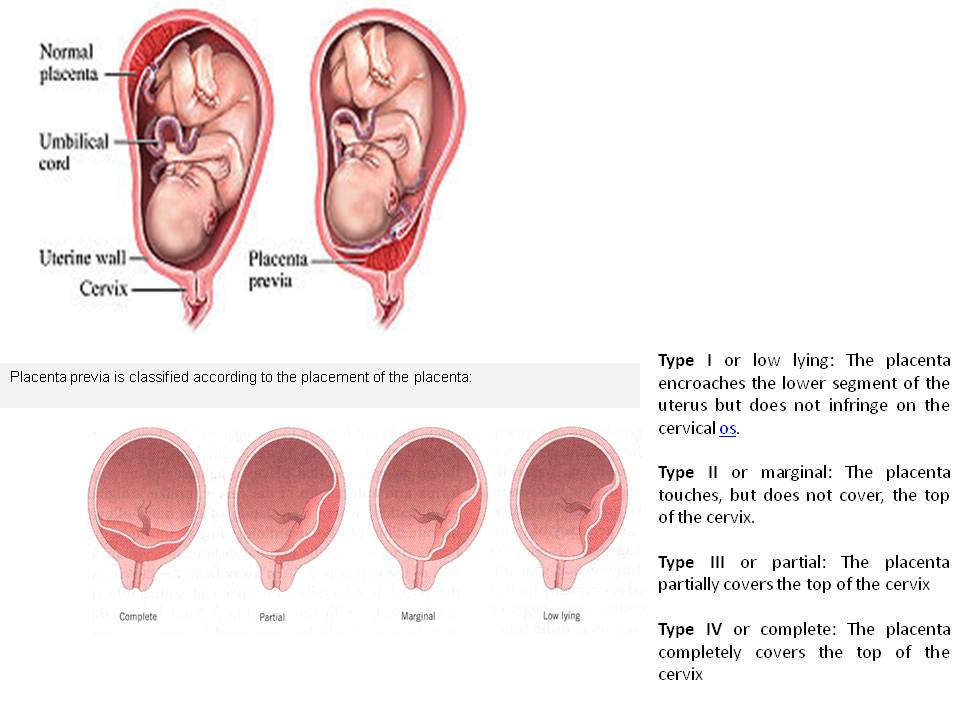
Types of location of the placenta
Usually the placenta is attached to the posterior wall of the uterus closer to its bottom . It is worth noting that the uterus is an inverted vessel, and its bottom is located on top. This is the best option for the location of the placenta. However, this does not always work out. In some cases, the placenta is attached to the anterior wall. Which is also not a pathology.
The low position of the placenta during pregnancy is much more dangerous. If the placenta is located low, it is subjected to stronger pressure from the fetus, and even with any external influence, the risk is damage to the placenta or its detachment increases. In addition, in the later stages, an actively moving baby can also damage the placenta, or squeeze the umbilical cord.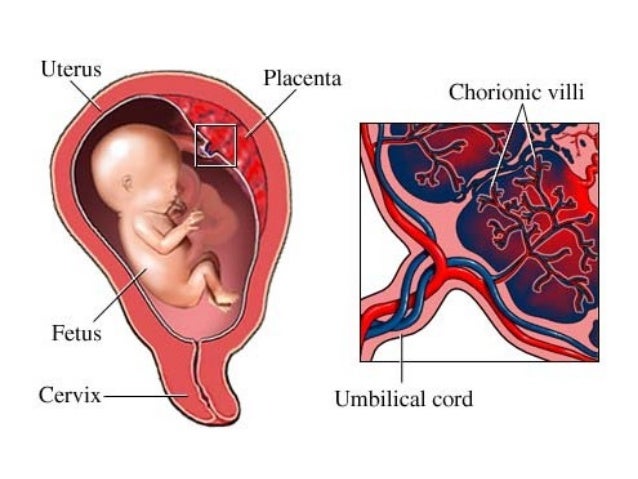
A placenta is said to be low when there is less than 6 cm between its lower edge and the os of the uterus. The anterior wall has a greater tendency to stretch, and migration is also characteristic of it, however, the direction of migration is opposite: usually the placenta moves in the opposite direction, down to the cervix.
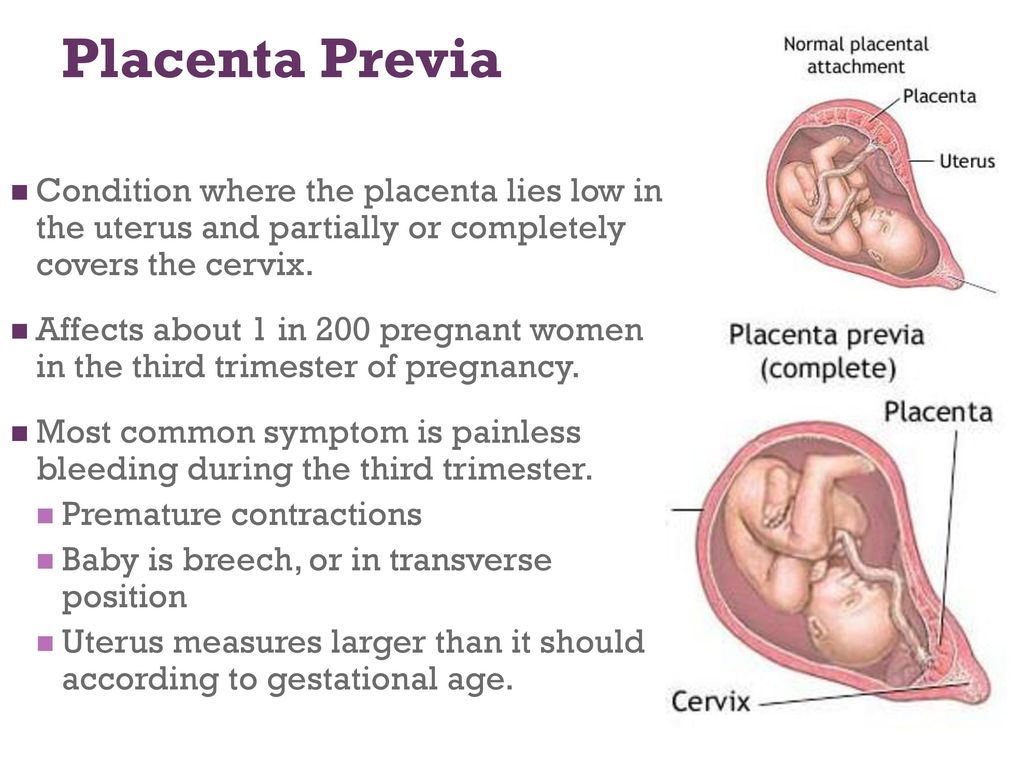
An even more complex and dangerous pathology of the location of the placenta is its partial or complete presentation . Previa is a condition when the placenta partially or completely obscures the cervix of the uterus.
Causes of low placenta
Many causes of low placenta are due to internal factors - diseases during pregnancy and the condition of the female genital organs . They can be:
- damage to the mucous membrane of the uterus;
- inflammatory processes;
- infections;
- previous abortions;
- miscarriages in the past;
- cesarean section;
- various gynecological operations;
- pathology of the structure, development, functioning of the uterus;
- multiple pregnancy;
- unhealthy lifestyle: active smoking, excessive alcohol consumption;
- previous diseases of the uterus: endometritis, fibroids;
- parity - many births in the past;
- the woman's age is over 35 years.
Curettage of the uterus in the past is the main cause of this pathology. Damage to the mucosa prevents the fetal egg from gaining a foothold in the upper segment of this organ, and it remains below, at the neck.
Symptoms of low placenta
The danger of this pathology is that it practically does not manifest itself. Usually, signs that not everything is in order with the placenta are the result of already running and irreversible processes - for example, its detachment. It can be:
- drawing pains, feeling of heaviness in the abdomen;
- bloody discharge with a low location of the placenta is an alarm signal that it is necessary to call an ambulance;
- freezing of the fetus in the womb for a long time, or, conversely, its too violent activity - this is caused by hypoxia;
- on ultrasound with such a pathology in 50% of cases is the wrong presentation of the fetus;
- in 30% of cases, women suffer from severe toxicosis.
A pregnant woman herself cannot suspect that she has a low placenta. This can only be seen on planned ultrasounds, which must be passed by everyone. After an ultrasound examination, they can not only clarify or refute the diagnosis, but also determine the type of pathology.
Treatment and prevention of low placentation
Management of pregnancy with low placentation is always very careful. A woman will have to undergo ultrasound many times, limit physical activity and stop sexual activity. For a long time, increased uterine tone can provoke detachment of an improperly located placenta, from there bleeding, and possible death of the fetus as a result of acute hypoxia, if placental abruption is large. Bleeding can even provoke a gynecological examination of the cervix, therefore, for no particular reason, doctors try not to conduct examinations on the chair.
Listen to the doctors and hope for the best. Many women give birth on their own or by caesarean section of healthy babies with low placenta previa.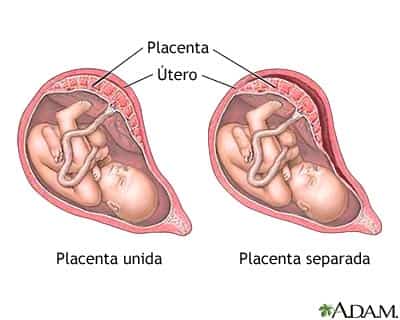
If you need help from an experienced gynecologist, sign up for a consultation by calling 8 (49244) 9-32-49, 8 (910) 174-77-72.
News All
Happy birthday, dear doctor!
Read more...
Murina Natalya Mikhailovna is the receptionist of small patients in our center. A good pediatrician becomes a reliable support for many years.
Read more...
Poll
What other doctors would you like to see in our center
| Traumatologist | |
| Surgeon | |
| ophthalmologist | |
| Dentist | |
| Allergist | |
| Oncologist | |
 This type of complication is increasingly being diagnosed in women with repeated pregnancies after caesarean section operations, the number of which continues to be high due to the expansion of indications for operative delivery. During delivery, massive bleeding inevitably occurs, which poses a danger to the life of the mother.
This type of complication is increasingly being diagnosed in women with repeated pregnancies after caesarean section operations, the number of which continues to be high due to the expansion of indications for operative delivery. During delivery, massive bleeding inevitably occurs, which poses a danger to the life of the mother. 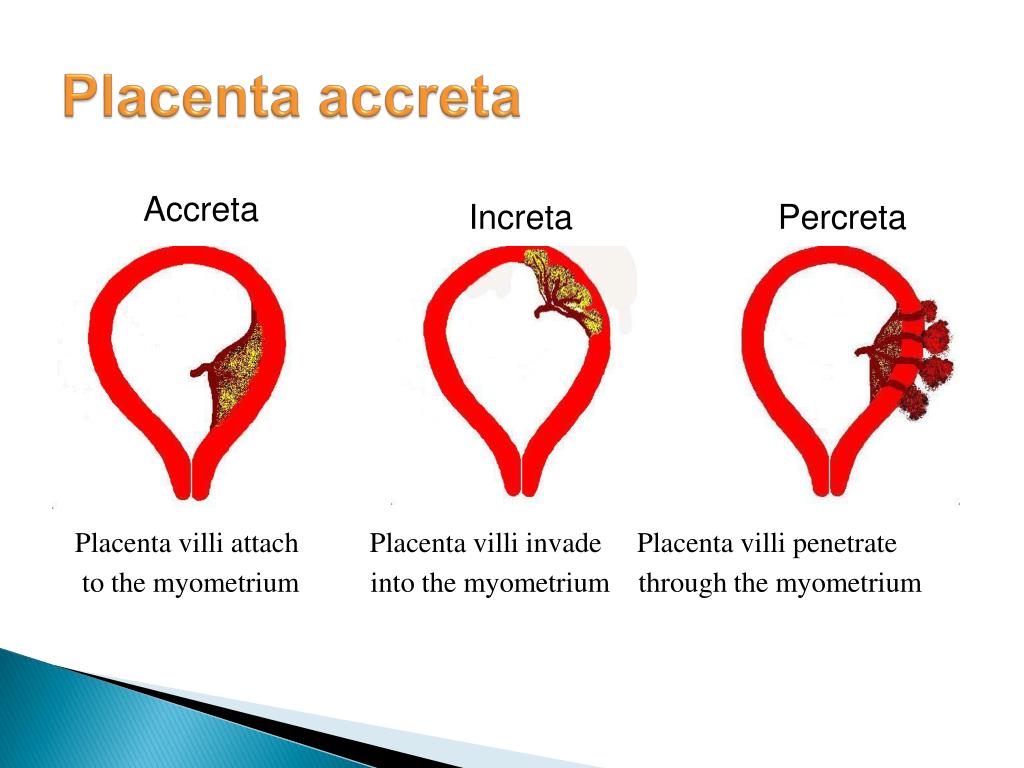 Blood loss is replenished by reinfusion of own blood using the Cell Saver apparatus.
Blood loss is replenished by reinfusion of own blood using the Cell Saver apparatus. 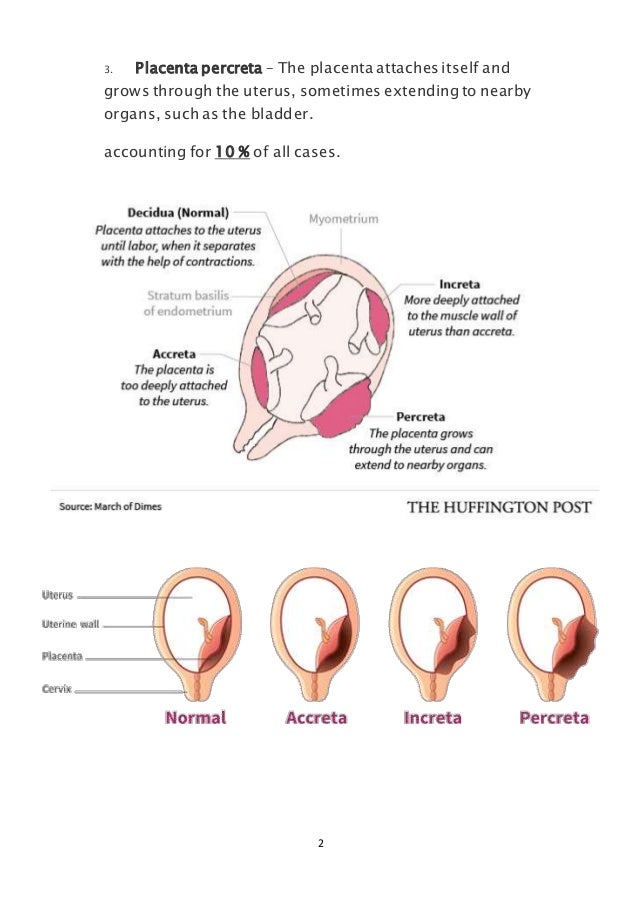 Given this feature, a caesarean section was performed in the area of the uterine fundus, as a result of which a live full-term baby was born.
Given this feature, a caesarean section was performed in the area of the uterine fundus, as a result of which a live full-term baby was born. 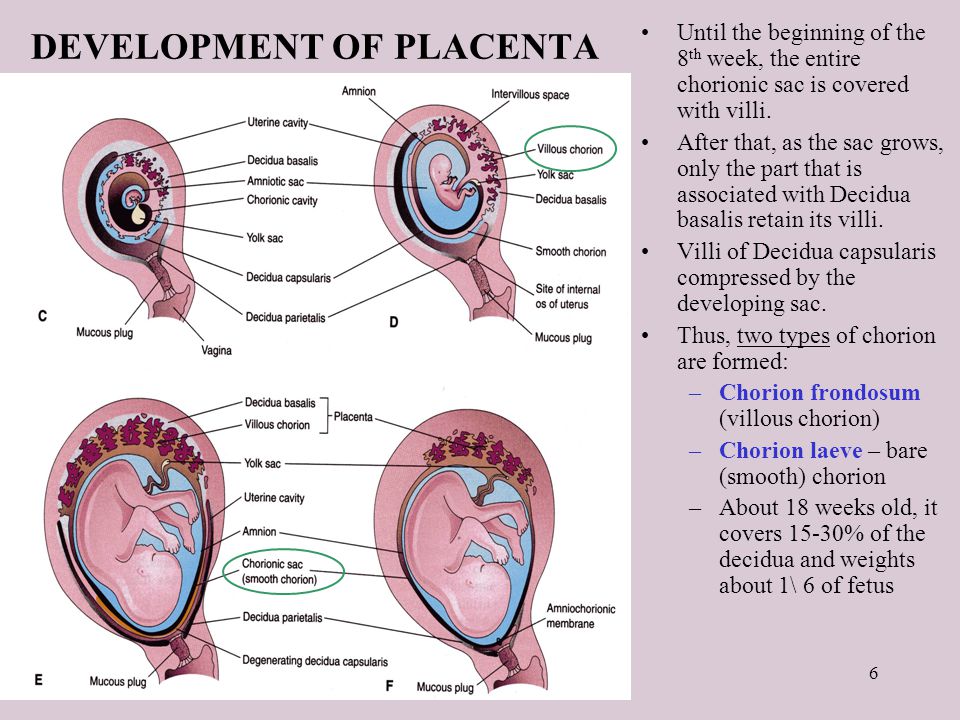 These are the arteries of the hand. Our part of the work begins after the birth of the child, so as not to expose the newborn to radiation exposure. Under x-ray navigation using a C-arm, a puncture of the left and right radial arteries was performed. Balloon catheters were passed through the aorta and placed in the left and right common iliac arteries. From that moment on, we were ready to perform intra-arterial hemostasis (ie stop bleeding) at any second. This time, emergency hemostasis was not required, and before surgeons began to separate the ingrown part of the placenta from the uterine body, we inflated the balloon catheters in the common iliac arteries, thereby cutting off the blood flow in the vessels supplying the uterus. When the placenta was removed and the body of the uterus was sutured, the balloons were deflated to ensure there was no bleeding. Then the balloons and guiding catheters were removed, and bandages were applied to the puncture site. This technique made it possible to preserve the uterus and avoid massive blood loss.
These are the arteries of the hand. Our part of the work begins after the birth of the child, so as not to expose the newborn to radiation exposure. Under x-ray navigation using a C-arm, a puncture of the left and right radial arteries was performed. Balloon catheters were passed through the aorta and placed in the left and right common iliac arteries. From that moment on, we were ready to perform intra-arterial hemostasis (ie stop bleeding) at any second. This time, emergency hemostasis was not required, and before surgeons began to separate the ingrown part of the placenta from the uterine body, we inflated the balloon catheters in the common iliac arteries, thereby cutting off the blood flow in the vessels supplying the uterus. When the placenta was removed and the body of the uterus was sutured, the balloons were deflated to ensure there was no bleeding. Then the balloons and guiding catheters were removed, and bandages were applied to the puncture site. This technique made it possible to preserve the uterus and avoid massive blood loss.