Baby red spots on stomach
Common childhood rashes | Pregnancy Birth and Baby
If your child has a seizure, call triple zero (000) immediately and ask for an ambulance.
If you think your child might have meningococcal rash, go to the nearest emergency department immediately.
Key facts
- There are many different types of childhood rashes. Many are not serious.
- If your child has a rash and fever, they should see their doctor.
- If your child has a meningococcal rash, go immediately to the emergency department.
Meningococcal rash
If you think your child might have meningococcal rash, go to the nearest emergency department immediately.
You can read more about serious childhood rashes here.
Rashes with no fever or itching
Milia (blocked oil glands)
Up to 1 in every 2 newborn babies develop small white spots called milia on their face, especially on the nose. These are just blocked pores, and they’re not itchy or contagious. They usually clear up without treatment within a few weeks.
Erythema toxicum
Many newborns develop a blotchy red skin reaction called erythema toxicum, which can appear between 2 days and 2 weeks after birth. Flat, red patches or small bumps often first appear on the face and spread to the body and limbs. The rash is harmless, not contagious, and will clear after a few days or a week.
Baby acne
Some babies get pimples on their cheeks and nose in the first three months of life. These pimples normally disappear without any treatment, usually within a few months.
Nappy rash
Nappy rash is inflammation of the skin in the nappy area. It can look red, sore and inflamed. Nappy rash is usually caused by urine (wee) or faeces (poo) irritating the skin.
To avoid nappy rash, keep the nappy area clean and dry with frequent nappy changes and nappy-free time. You can help protect the skin by putting on a barrier cream such as zinc or soft white paraffin at each nappy change.
Persistent nappy rash can be treated with a medicated cream. Don’t use talcum powder or antiseptics to treat nappy rash. If your baby develops a fungal infection, you’ll need to use an antifungal ointment. Ask your doctor or pharmacist for advice.
Erythema multiforme (minor)
Erythema multiforme is a rash triggered by an infection (most commonly herpes simplex virus), medicine or an illness. Your baby might feel unwell or have a mild fever before the rash appears. Red spots develop on the hands, feet, arms and legs and spread symmetrically across both sides of the body. The spots often become raised or blistered and then develop into classic target-like lesions.
Erythema multiforme is not contagious, and usually resolves without treatment in 3 to 6 weeks.
Keratosis pilaris (‘chicken skin’)
Keratosis pilaris is a harmless condition where the skin becomes rough and bumpy, as if permanently covered in goose pimples. These bumps most commonly occur on the upper arms and thighs.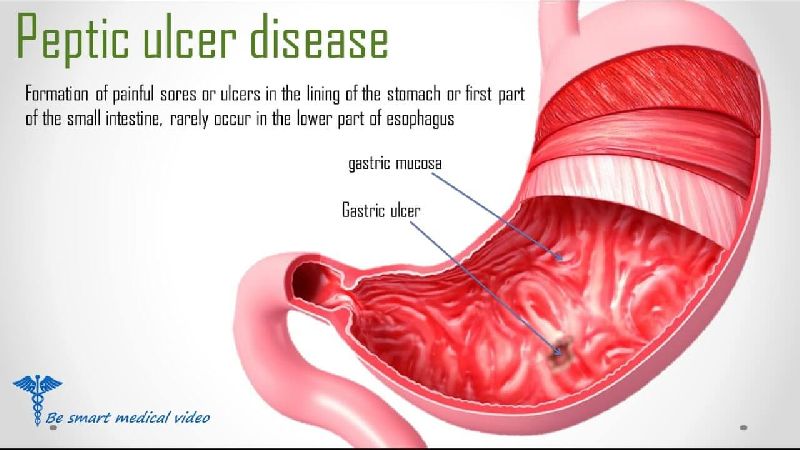 You can try several things to help the rash to clear up, including moisturising regularly.
You can try several things to help the rash to clear up, including moisturising regularly.
Rashes that might be itchy
Eczema (Atopic dermatitis)
Eczema is a very common skin condition affecting 1 in 3 Australians. It causes the skin to become itchy, red, dry and cracked, often in the creases at the knees and elbows.
Eczema commonly starts before a baby is 12 months old. Eczema follows a relapsing-remitting course. This means that there are flare-ups of the rash, followed by periods where there is no rash or a minimal rash.
Eczema management includes preventative treatment such as avoiding skin irritants, moisturising regularly and using bath oil. Treatment of flare-ups includes using steroid and anti-inflammatory creams.
Ringworm (tinea)
Ringworm is a common, contagious skin infection that causes a ring-like red rash with a clear centre. It commonly occurs on the scalp, feet and groin, but it can appear almost anywhere on the body.
Ringworm is caused by a fungus, not a worm, and is usually treated with over-the-counter antifungal creams. You should keep your child home from childcare or school until a day after you have started treatment to prevent spreading the infection.
You should keep your child home from childcare or school until a day after you have started treatment to prevent spreading the infection.
Prickly heat (heat rash)
Heat rash might appear if your baby gets hot in a humid environment. The rash shows as tiny red bumps or blisters on the skin, which can be very itchy. Cooling your baby down and avoiding humidity is the best way to prevent heat rash, which usually clears within 2 to 3 days without treatment.
Impetigo (school sores)
Impetigo is a highly contagious bacterial infection of the skin. It causes red sores and blisters that form a yellow crust. It is very common in children aged 2 to 6, and it is not usually serious in this age group, but it can be dangerous for newborn babies.
If your child has impetigo, you should see your doctor, who might prescribe an antibiotic cream, ointment or tablet. This should clear the infection within 7 to 10 days. Keep your child home from childcare or school and away from young babies until the sores have dried up, usually a few days after treatment starts.
Hives (urticaria)
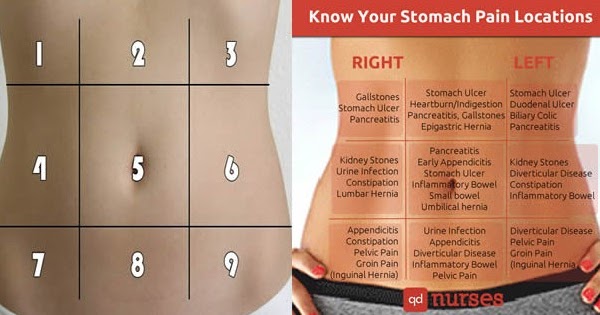
Hives is a raised, red, itchy rash. It is common on the chest, stomach and back, as well as the throat and limbs, but it can appear on any part of the body. Hives usually disappears within a few days without any treatment. Antihistamines can be given to relieve itching. If the rash doesn't go away, you should see your doctor.
Hives isn’t usually serious, but it can be a sign of a more serious allergic reaction (anaphylaxis). If your child develops hives after eating, or together with other symptoms such as vomiting, dizziness or trouble breathing, you should seek urgent medical attention.
If your child has symptoms of a serious allergic reaction (anaphylaxis), call triple zero (000) immediately and ask for an ambulance.
Pityriasis rosea
Pityriasis rosea is a mild skin rash that sometimes appears after a sore throat, cold or fever. It begins with a single pink or tan-coloured patch on the chest or back. Red, oval-shaped patches, which may be itchy, then appear on the chest or back and limbs over the next weeks.
The exact cause of pityriasis rosea is unclear, and it is not thought to be contagious. The rash usually clears up within a couple of months without treatment.
If you are pregnant, pityriasis rosea can in rare cases lead to complications. See your doctor if you are pregnant and have contact with a child who has pityriasis rosea.
Molluscum contagiosum
Molluscum contagiosum is a viral skin infection that is spread by skin-to-skin contact or by sharing swimming pool water, bath water or towels.
Molluscum contagiosum spots look like pimples and grow into round pearly white lumps, usually 2 to 5 millimetres in size. They can be itchy. They usually heal without treatment within 6 months, but sometimes longer.
Rashes with fever
Slapped cheek disease (fifth disease)
Slapped cheek disease is a viral infection that mainly affects pre-school and school-age children. It typically causes a bright red rash on both cheeks that spreads as a ‘lacy’ rash on the body and limbs. Occasionally, it causes a fever.
Occasionally, it causes a fever.
Slapped cheek disease is usually mild and clears up in a few days without treatment. The child is contagious before the rash appears, but not once it has appeared.
If you are pregnant and catch the virus, it may cause a type of anaemia in your unborn baby. It can also cause miscarriage. If you suspect you or your child has slapped cheek disease, you should avoid contact with people who might be pregnant.
Hand, foot and mouth disease
Hand, foot and mouth disease is a mild but highly contagious viral illness. It causes a rash on the palms of the hands and soles of the feet and blisters in the mouth. It is not the same as the foot-and-mouth disease that affects farm animals.
The disease is common in childcare and kindergartens. Your child might feel unwell and have a fever and blisters on the hands and feet and in the mouth and in the nappy area. The illness usually lasts about 7 to 10 days. Children with hand, foot and mouth disease should stay away from childcare or school until all the blisters have dried up.
Hand, foot and mouth disease usually resolves on its own without complications. In rare cases, it can be more serious, especially if you have a weakened immune system or are pregnant. Complications can include infections of the brain and heart muscle and miscarriage.
Roseola infantum
Roseola infantum is a contagious viral infection that can cause cold-like symptoms and a high fever. The high fever may last for a few days. Roseola infantum can also cause some children to have a febrile convulsion (seizure).
Children with roseola infantum develop a rash after the fever has resolved. The rash looks like raised pink spots that start on the chest, stomach and back and spread to the limbs. The child is contagious before the rash appears, but not after. The rash usually lasts 3 to 5 days.
Febrile convulsions can look scary but are generally not harmful.
If your child has a seizure, call triple zero (000) immediately and ask for an ambulance.
When to seek help
Many babies develop a skin rash in their first days or weeks of life as their sensitive skin adapts to a new environment. Most rashes are harmless and go away on their own, but if your baby seems unwell, or if you’re worried, you should see your doctor. They can advise about the cause and whether treatment is necessary.
Most rashes are harmless and go away on their own, but if your baby seems unwell, or if you’re worried, you should see your doctor. They can advise about the cause and whether treatment is necessary.
Whatever their age, you should take your child to the doctor if they have a rash and persistent high temperature, cold or cough symptoms or swollen neck glands.
Treatment of common childhood rashes
If you think your child might be contagious, they should stay at home. Keep them away from school, childcare and other children. You should also keep them away from people who are pregnant, or who might be pregnant, since some childhood infections can cause serious problems in unborn babies.
You can use paracetamol or ibuprofen (in babies aged over 3 months) to reduce fever — read the packet instructions carefully to ensure your child receives the right amount for their age and weight.
Your pharmacist can advise you on treating the symptoms of common rashes. For example, you can use over-the-counter creams to prevent itchiness.
If you are concerned about your child’s rash, call Pregnancy, Birth and Baby on 1800 882 436 to talk to a maternal child health nurse, or call Healthdirect on 1800 022 022 to talk to a registered nurse. Alternatively, contact your doctor.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Learn more here about the development and quality assurance of healthdirect content.
Rash or Redness - Widespread
Is this your child's symptom?
- Red or pink rash over large parts or most of the body (widespread)
- Sometimes, just on hands, feet and buttocks - but same on both sides of body
- Small spots, large spots or solid red skin
Causes of Widespread Rash or Redness
- Viral Rash. Most rashes are part of a viral illness. Viral rashes usually have small pink spots.
 They occur on both sides of the chest, stomach and back. Your child may also have a fever with some diarrhea or cold symptoms. They last 2 or 3 days. More common in the summer.
They occur on both sides of the chest, stomach and back. Your child may also have a fever with some diarrhea or cold symptoms. They last 2 or 3 days. More common in the summer. - Roseola. This is the most common viral rash in the first 3 years of life. (See details below).
- Chickenpox. A viral rash with a distinctive pattern. (see that Care Guide)
- Hand-Foot and-Mouth Disease. A viral rash with a distinctive pattern. It starts with tiny red spots and blisters on the palms and soles. (see that Care Guide)
- Monkeypox. A rare viral rash that often starts on the face or genital area. It then spreads to the arms and legs. Not usually seen in children unless someone in the home has monkeypox.
- Scarlet Fever. Scarlet Fever is a speckled, red rash all over. Has a sandpaper feel. Caused by the Strep bacteria. Starts on upper chest and quickly spreads to lower chest and stomach.
 No more serious than a Strep throat infection without a rash.
No more serious than a Strep throat infection without a rash. - Drug Rash. Most rashes that start while taking an antibiotic are viral rashes. Only 10% turn out to be allergic drug rashes. (see details below)
- Hives. Raised pink bumps with pale centers. Hives look like mosquito bites. Rashes that are bumpy and itchy are often hives. Most cases of hives are caused by a virus. Hives can also be an allergic reaction. (See that Care Guide for details)
- Heat Rash. A fine pink rash caused by overheating. Mainly involves neck, chest and upper back.
- Insect Bites. Insect bites cause small red bumps. Flying insects can cause many bumps on exposed skin. Non-flying insects are more likely to cause localized bumps.
- Hot Tub Rash. Causes small red bumps that are painful and itchy. Mainly occurs on skin covered by a bathing suit. Rash starts 12-48 hours after being in hot tub. Caused by overgrowth of bacteria in hot tubs.
- Petechiae Rash (Serious). Petechiae are purple or dark red colored tiny dots. They come from bleeding into the skin. Scattered petechiae with a fever are caused by Meningococcemia until proven otherwise. This is a life-threatening bacterial infection of the bloodstream. Peak age is 3 to 6 months old. Unlike most pink rashes, petechiae don't fade when pressed on.
- Purpura Rash (Serious). Purpura means bleeding into the skin. It looks like purple or dark red larger spots. Widespread purpura is always an emergency. It can be caused by a bacterial bloodstream infection. Rocky Mountain Spotted Fever is an example.
- Blister Rash (Serious). Widespread blisters on the skin are a serious sign. It can be caused by infections or drugs. Stevens Johnson Syndrome is an example.
- Caution. All widespread rashes with fever need to be seen. They need to be diagnosed. Reason: some serious infections that can cause this type of rash.

Drugs and Rashes
- Prescription medicines sometimes cause widespread rashes. Some are allergic, but most are not.
- Non-prescription (OTC) medicines rarely cause any rashes.
- Most rashes that occur while taking an OTC medicine are viral rashes.
- Fever medicines (acetaminophen and ibuprofen) cause the most needless worry. Reason: most viral rashes start with a fever. Hence, the child is taking a fever medicine when the rash starts.
- Drug rashes can't be diagnosed over the phone.
Roseola - A Classic Rash
- Most children get Roseola between 6 months and 3 years of age.
- Rash: pink, small, flat spots on the chest and stomach. Then spreads to the face.
- Classic feature: 3 to 5 days of high fever without a rash or other symptoms.
- The rash starts 12 to 24 hours after the fever goes away.
- The rash lasts 1 to 3 days.
- By the time the rash appears, the child feels fine.
- Treatment: the rash is harmless.
 Creams or medicines are not needed.
Creams or medicines are not needed.
Localized Versus Widespread Rash: How to Decide
- Localized means the rash occurs on one small part of the body. Usually, the rash is just on one side of the body. An example is a rash on 1 foot. Exceptions: athlete's foot can occur on both feet. Insect bites can be scattered.
- Widespread means the rash occurs on larger areas. Examples are both legs or the entire back. Widespread can also mean on most of the body surface. Widespread rashes always occur on matching (both) sides of the body. Many viral rashes are on the chest, stomach and back.
- The cause of a widespread rash usually spreads through the blood stream. Examples are rashes caused by viruses, bacteria, toxins, and food or drug allergies.
- The cause of a localized rash usually is just from contact with the skin. Examples are rashes caused by chemicals, allergens, insect bites, ringworm fungus, bacteria or irritants.

- This is why it's important to make this distinction.
When to Call for Rash or Redness - Widespread
Call 911 Now
- Purple or blood-colored spots or tiny dots with fever within the last 24 hours
- Trouble breathing or swallowing
- Not moving or too weak to stand
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Bright red skin that peels off in sheets
- Large blisters on skin
- Bloody crusts on the lips
- Taking a prescription medication within the last 3 days
- Fever
- Your daughter is having her period and using tampons
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Contact Doctor Within 24 Hours
- Widespread rash, but none of the symptoms above. Reason: all widespread rashes need to be checked by a doctor.
Seattle Children's Urgent Care Locations
If your child’s illness or injury is life-threatening, call 911.
- Bellevue
- Everett
- Federal Way
- Seattle
Care Advice for Widespread Rashes
- What You Should Know About Widespread Rashes:
- Most rashes with small pink spots all over are part of a viral illness.
- This is more likely if your child has a fever. Other symptoms (like diarrhea) also point to a viral rash.
- Here is some care advice that should help until you talk with your doctor.
- Non-Itchy Rash Treatment:
- If you suspect a heat rash, give a cool bath.

- Otherwise, no treatment is needed.
- If you suspect a heat rash, give a cool bath.
- Itchy Rash Treatment:
- Wash the skin once with soap to remove any irritants.
- Steroid Cream. For relief of itching, use 1% hydrocortisone cream (such as Cortaid). Put it on the most itchy areas. No prescription is needed. Do this 3 times per day.
- Cool Bath. For flare-ups of itching, give your child a cool bath. Do not use soap. Do this for 10 minutes. Caution: avoid any chill. Option: Can add 2 ounces (60 mL) of baking soda per tub.
- Scratching. Try to keep your child from scratching. Cut the fingernails short. Reason: prevents a skin infection from bacteria.
- Allergy Medicine for Itching. If itching becomes severe, give an allergy medicine, such as Benadryl. No prescription is needed. Age limit: 1 and older. If needed longer than a few days, switch to a long-acting antihistamine, such as Zyrtec. Age limit: 2 and older.
- Fever Medicine:
- For fevers above 102° F (39° C), give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Note: Fevers less than 102° F (39° C) are important for fighting infections.
- For all fevers: Keep your child well hydrated. Give lots of cold fluids.
- Return to School:
- Most viral rashes can be spread to others (especially if a fever is present).
- If your child has a fever, avoid contact with other children. Also, avoid pregnant women until a diagnosis is made.
- For minor rashes, your child can return after the fever is gone.
- For major rashes, your child can return to school after the rash is gone. If your doctor has given medical clearance, your child can return sooner.
- What to Expect:
- Most viral rashes go away within 48 hours.
- Call Your Doctor If:
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.

Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Last Reviewed: 12/03/2022
Last Revised: 09/16/2022
Copyright 2000-2022. Schmitt Pediatric Guidelines LLC.
Rash in a child on the body, legs, back
We treat children according to the principles of evidence-based medicine: we choose only those diagnostic and treatment methods that have proven their effectiveness. We will never prescribe unnecessary examinations and medicines!
Make an appointment via WhatsApp
Prices Doctors
The first children's clinic of evidence-based medicine in Moscow
No unnecessary examinations and medicines! We will prescribe only what has proven effective and will help your child.
Treatment according to world standards
We treat children with the same quality as in the best medical centers in the world.
The best team of doctors in Fantasy!
Pediatricians and subspecialists Fantasy - highly experienced doctors, members of professional societies. Doctors constantly improve their qualifications, undergo internships abroad.
Ultimate treatment safety
We made pediatric medicine safe! All our staff work according to the strictest international standards JCI
We have fun, like visiting best friends
Game room, cheerful animator, gifts after the reception. We try to make friends with the child and do everything to make the little patient feel comfortable with us.
You can make an appointment by calling or by filling out the form on the site
Other Pediatric services
- Pediatrician's consultation
- Child Health Management Program
Frequent calls
- Acute bronchiolitis in children: diagnosis and treatment
- SARS
- Angina streptococcal tonsillitis
- Frequently ill child
- Intestinal infections
- Pneumonia (pneumonia) in children
- Colic
- Feeding problems
- Prolonged cough in a child: diagnosis and treatment
- Acute bronchitis in children: diagnosis and treatment
- Pneumonia (pneumonia) in children: diagnosis and treatment
- False croup in a child
- Coxsackie virus in a child
- The child was bitten by a tick! What to do?
Online payment
Documents online
Online services
Parental leaflet on viral diseases
Parental leaflet..jpg)
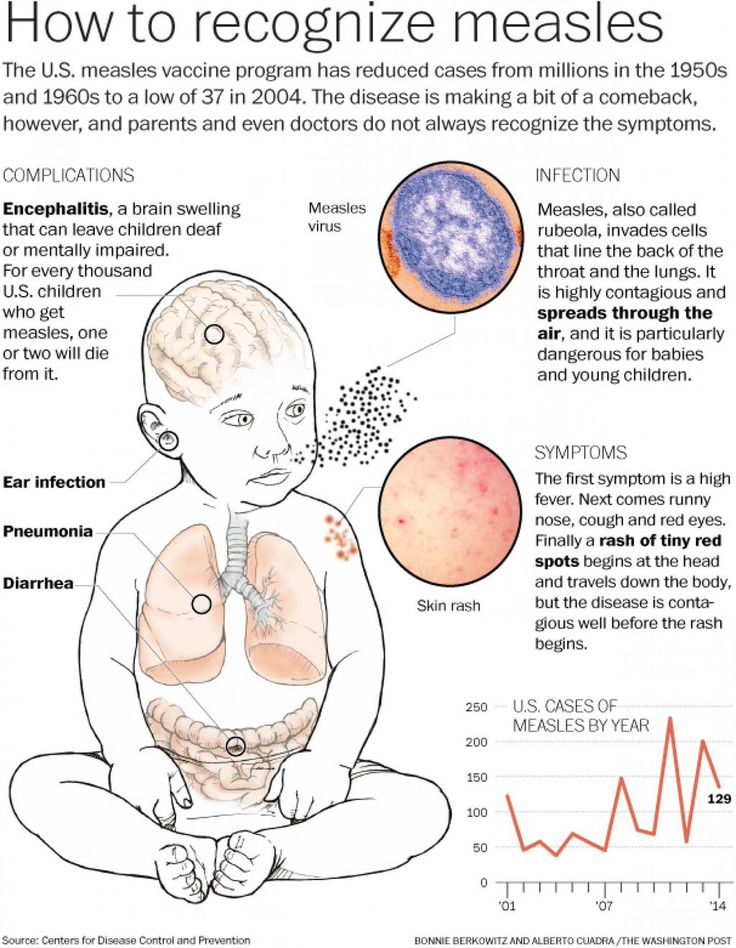
Measles is a viral infection with a very high susceptibility. If a person has not had measles or has not been vaccinated against this infection, then after contact with the patient, infection occurs in almost 100% of cases. The measles virus is highly volatile. The virus can spread through ventilation pipes and elevator shafts - at the same time, children living on different floors of the house get sick.
The period from contact with a person with measles to the appearance of the first signs of the disease lasts from 7 to 14 days.
The disease begins with a severe headache, weakness, fever up to 40 degrees C. A little later, a runny nose, cough and almost complete lack of appetite join these symptoms.
Very characteristic of measles is the appearance of conjunctivitis - inflammation of the mucous membrane of the eyes, which is manifested by photophobia, lacrimation, sharp redness of the eyes, and subsequently - the appearance of purulent discharge. These symptoms last 2 to 4 days.
These symptoms last 2 to 4 days.
On the 4th day of illness, a rash appears , which looks like small red spots of various sizes (from 1 to 3 mm in diameter), with a tendency to merge. The rash occurs on the face and head (it is especially characteristic of its appearance behind the ears) and spreads throughout the body for 3-4 days. It is very characteristic of measles that the rash leaves behind pigmentation (dark spots that persist for several days), which disappears in the same sequence as the rash appears.
Measles can cause serious complications . These include inflammation of the lungs (pneumonia), inflammation of the middle ear (otitis media), and sometimes such a formidable complication as encephalitis (inflammation of the brain).
It must be remembered that after suffering from measles for a sufficiently long period of time (up to 2 months) there is a suppression of immunity, so the child can get sick with some cold or viral disease, so you need to protect him from excessive stress, if possible from contact with sick children.
After measles, lifelong immunity develops. All those who have had measles become immune to this infection.
The only reliable protection against the disease is vaccination against measles, which is included in the National Immunization Schedule.
Reminder for parents.
Rubella is an airborne viral infection. As a rule, children who stay in a water room for a long time with a child who is a source of infection get sick. Rubella in its manifestations is very similar to measles, but it is much easier.
The period from contact to the appearance of the first signs of illness lasts from 14 to 21 days.
Rubella begins with an increase in the occipital lymph nodes and an increase in body temperature up to 38 degrees C. A runny nose, and sometimes a cough, joins a little later. A rash appears 2 to 3 days after the onset of the disease. Rubella is characterized by a pink, punctate rash that begins with a rash on the face and spreads throughout the body. Rubella rash, unlike measles, never merges, there may be a slight itch. The period of rashes can be from several hours, during which there is no trace of the rash, up to 2 days.
Rubella rash, unlike measles, never merges, there may be a slight itch. The period of rashes can be from several hours, during which there is no trace of the rash, up to 2 days.
The treatment of rubella is to relieve the main symptoms - the fight against fever, if any, the treatment of the common cold, expectorants.
Complications from rubella are rare.
After rubella, immunity also develops, re-infection is extremely rare, but can occur.
It is therefore very important to get vaccinated against rubella, which, like the measles vaccine, is included in the National Immunization Schedule.
Note for parents.
Mumps (mumps) is a childhood viral infection characterized by acute inflammation in the salivary glands.
Infection occurs by airborne droplets. Susceptibility to this disease is about 50-60% (that is, 50-60% of those who were in contact and who were not ill and not vaccinated get sick).
It can take 11 to 23 days from contact with a sick mumps to the onset of illness.
Mumps begins with an increase in body temperature up to 39 degrees C and severe pain in or under the ear, aggravated by swallowing or chewing. At the same time, salivation increases. Swelling quickly grows in the upper part of the neck and cheeks, touching this place causes severe pain in the child. Unpleasant symptoms disappear within three to four days: body temperature decreases, swelling decreases, pain disappears.
However, quite often mumps ends inflammation in glandular organs such as pancreas (pancreatitis), gonads. Past pancreatitis in some cases leads to diabetes mellitus . Inflammation of the gonads (testicles) is more common in boys. This significantly complicates the course of the disease, and in some cases may result in infertility. In especially severe cases, mumps can be complicated by viral meningitis (inflammation of the meninges), which is severe.
After a disease, a strong immunity is formed, but complications can lead to disability.
The only reliable protection against the disease is vaccination against mumps, which is included in the National Immunization Schedule.
Reminder for parents.
Varicella (chickenpox) is a common childhood infection. Mostly young children or preschoolers are ill. Susceptibility to the causative agent of chickenpox (the virus that causes chickenpox refers to herpes viruses) is also quite high. About 80% of contact persons who have not been ill before develop chickenpox.
14 to 21 days pass from the moment of contact with a patient with chickenpox until the first signs of the disease appear.
The disease begins with a rash. Usually it is one or two reddish spots, similar to a mosquito bite. These elements of the rash can be located on any part of the body, but most often they first appear on the stomach or face. Usually the rash spreads very quickly - new elements appear every few minutes or hours. Reddish spots, which at first look like mosquito bites, the next day take the form of bubbles filled with transparent contents. These blisters are very itchy. The rash spreads throughout the body, to the limbs, to the scalp. In severe cases, there are elements of the rash on the mucous membranes - in the mouth, nose, on the conjunctiva of the sclera, genitals, intestines. By the end of the first day of the disease, the general state of health worsens, the body temperature rises (up to 40 degrees C and above). The severity of the condition depends on the number of lesions. If there are elements of the rash on the mucous membranes of the pharynx, nose and on the conjunctiva of the sclera, then pharyngitis, rhinitis and conjunctivitis develop due to the addition of a bacterial infection. Bubbles open in a day or two with the formation of sores, which are covered with crusts. Headache, feeling unwell, fever persist until new rashes appear.
Usually the rash spreads very quickly - new elements appear every few minutes or hours. Reddish spots, which at first look like mosquito bites, the next day take the form of bubbles filled with transparent contents. These blisters are very itchy. The rash spreads throughout the body, to the limbs, to the scalp. In severe cases, there are elements of the rash on the mucous membranes - in the mouth, nose, on the conjunctiva of the sclera, genitals, intestines. By the end of the first day of the disease, the general state of health worsens, the body temperature rises (up to 40 degrees C and above). The severity of the condition depends on the number of lesions. If there are elements of the rash on the mucous membranes of the pharynx, nose and on the conjunctiva of the sclera, then pharyngitis, rhinitis and conjunctivitis develop due to the addition of a bacterial infection. Bubbles open in a day or two with the formation of sores, which are covered with crusts. Headache, feeling unwell, fever persist until new rashes appear. This usually happens within 3 to 5 days. Within 5-7 days after the last sprinkling, the rash disappears.
This usually happens within 3 to 5 days. Within 5-7 days after the last sprinkling, the rash disappears.
Treatment of chickenpox is to reduce itching, intoxication and prevent bacterial complications. The elements of the rash must be lubricated with antiseptic solutions (as a rule, this is an aqueous solution of brilliant green or manganese). Treatment with coloring antiseptics prevents bacterial infection of rashes, allows you to track the dynamics of the appearance of rashes. It is necessary to monitor the hygiene of the mouth and nose, eyes - you can rinse your mouth with a solution of calendula, the mucous membranes of the nose and mouth also need to be treated with antiseptic solutions.
Complications of chickenpox include myocarditis - inflammation of the heart muscle, meningitis and meningoencephalitis (inflammation of the meninges, brain matter), inflammation of the kidneys (nephritis). Fortunately, these complications are quite rare. After chickenpox, as well as after all childhood infections, immunity develops. Re-infection happens, but very rarely.
After chickenpox, as well as after all childhood infections, immunity develops. Re-infection happens, but very rarely.
Reminder for parents.
Scarlet fever is the only childhood infection caused not by viruses but by bacteria (group A streptococcus). This is an acute disease transmitted by airborne droplets. Infection through household items (toys, dishes) is also possible. Children of early and preschool age are ill. The most dangerous in terms of infection are patients in the first two to three days of the disease.
Scarlet fever begins very acutely with fever up to 39 degrees C, vomiting, headache. The most characteristic symptom of scarlet fever is tonsillitis in which the mucous membrane of the throat has a bright red color, swelling is pronounced. The patient notes a sharp pain when swallowing. There may be a whitish coating on the tongue and tonsils. The tongue subsequently acquires a very characteristic appearance ( “crimson ”) - bright pink and coarsely granular.
The tongue subsequently acquires a very characteristic appearance ( “crimson ”) - bright pink and coarsely granular.
By the end of the first beginning of the second day of illness, 9 appears0095 the second characteristic symptom of scarlet fever is a rash. It appears immediately on several parts of the body, most densely located in the folds (elbow, inguinal). Its distinguishing feature is that the bright red punctate scarlatinal rash is located on a red background, which gives the impression of a general confluent redness. When pressed against the skin, a white line remains . The rash may be spread over the entire body, but there is always a clean (white) area of skin between the upper lip and nose, and also the chin. Itching is much less pronounced than with chicken pox.
Rash lasts up to 2 to 5 days. The manifestations of sore throat persist a little longer (up to 7-9 days).
Scarlet fever is usually treated with antibiotics because the causative agent of scarlet fever is a microbe that can be eliminated with antibiotics and strict adherence to bed rest . Also very important is the local treatment of angina and detoxification (removal of toxins from the body that are formed during the vital activity of microorganisms - for this they give plenty of drink). Vitamins, antipyretics are shown. Scarlet fever also has enough serious complications . Before the use of antibiotics, scarlet fever often resulted in the development of rheumatism with the formation of acquired heart defects or kidney disease. Currently, subject to well-prescribed treatment and careful adherence to recommendations, such complications are rare.
Also very important is the local treatment of angina and detoxification (removal of toxins from the body that are formed during the vital activity of microorganisms - for this they give plenty of drink). Vitamins, antipyretics are shown. Scarlet fever also has enough serious complications . Before the use of antibiotics, scarlet fever often resulted in the development of rheumatism with the formation of acquired heart defects or kidney disease. Currently, subject to well-prescribed treatment and careful adherence to recommendations, such complications are rare.
Almost exclusively children suffer from scarlet fever because with age a person acquires resistance to streptococci. Those who have been ill also acquire strong immunity.
Memo for parents.
Whooping cough is an acute infectious disease characterized by a long course. The hallmark of the disease is a spasmodic cough.
The mechanism of transmission of infection is airborne. A feature of whooping cough is the high susceptibility of children to it, starting from the first days of life.
A feature of whooping cough is the high susceptibility of children to it, starting from the first days of life.
3 to 15 days pass from the moment of contact with a person with whooping cough until the first signs of the disease appear. Whooping cough feature is a gradual increase in cough within 2 to 3 weeks after its onset.
Typical signs of whooping cough:
- · persistent intensifying cough, gradually turning into spasmodic cough attacks (a series of coughing shocks rapidly following one after another on one exhalation) with convulsive inspiration, accompanied by a whistling lingering sound. In infants, such a cough can lead to respiratory arrest. Attacks of coughing are worse at night and end in the release of a small amount of viscous sputum, sometimes vomiting;
- puffiness of the face, hemorrhages in the sclera;
- ulcer on the frenulum of the tongue (due to injury from the edges of the teeth, since during a coughing fit the tongue protrudes to the limit, its tip bends upward).

Whooping cough is often complicated by bronchitis, otitis media, pneumonia, rectal prolapse, umbilical and inguinal hernias.
After suffering whooping cough for a long time (several months), coughing fits may return, especially if the child catches a cold or during physical exertion.
The only reliable prevention against pertussis is vaccination with DPT, a vaccine included in the National Immunization Schedule. Parents' fears about the harmful effects of the vaccine are unfounded. The quality of the DTP vaccine is not inferior in its properties to vaccines produced in other countries.
Memo for parents.
Acute intestinal infections is a large group of diseases that occur with more or less similar symptoms, but can be caused by a huge number of pathogens: bacteria, viruses, protozoa.
In summer, the number of intestinal infections in children inevitably increases. There are several reasons for this.
Firstly, , in summer a large amount of raw vegetables, fruits and berries are consumed, on the unwashed surface of which a huge number of microbes, including potentially dangerous ones, live.
Secondly, , children spend a lot of time outdoors in summer, and not always even their parents remember that eating with clean hands is a mandatory rule .
The third reason : in the summer, getting into foodstuffs (dairy products, meat, fish, broths), some pathogens multiply at a tremendous speed and quickly reach the amount that successfully breaks through the protective barriers of the gastrointestinal tract.
From the moment the pathogen enters the gastrointestinal tract to the onset of the disease, it can take from several hours to 7 days.
The disease begins with fever, malaise, weakness, lethargy. Appetite is sharply reduced, nausea, vomiting quickly joins. The chair is liquid, frequent with impurities. The consequence of fluid loss is dryness of the mucous membranes and skin, facial features are sharpened, the child loses weight, urinates little. Painful facial expression. If your child has the above signs of illness, call the doctor immediately. Self-treatment not allowed .
The chair is liquid, frequent with impurities. The consequence of fluid loss is dryness of the mucous membranes and skin, facial features are sharpened, the child loses weight, urinates little. Painful facial expression. If your child has the above signs of illness, call the doctor immediately. Self-treatment not allowed .
Prevention of intestinal infections requires strict adherence to general hygiene measures in the home, when preparing food and while eating.
In the summer, all foodstuffs should be protected from flies. Ready food should be stored in the refrigerator: at a low temperature, even if microbes get into the food, they will not be able to multiply. The disease can also be caused by illegibility when buying products that are eaten without heat treatment - from the hands, outside the markets, where they do not pass sanitary control. When swimming in open water, in no case should water be swallowed. If you eat on the beach, wipe your hands with at least special wet wipes.
And remember that parental example is the best way to teach a child.
Parent Guide .
Tuberculosis is a chronic infectious disease caused by mycobacterium human tuberculosis, affecting mostly the respiratory organs, as well as all organs and systems of the body.
The source of infection for is people with tuberculosis. The most common is the air way of infection. Transmission factors are nasopharyngeal mucus, sputum and dust containing bacteria.
Reproduction of tuberculosis bacteria in the child's body leads to significant functional disorders with symptoms of intoxication: irritability appears or, conversely, lethargy, fatigue, headache, sweating. With a long course of the disease, the child loses weight, the skin becomes pale, and there is a tendency to inflammatory diseases. For children, a reaction from the lymph nodes is typical: they increase in size, become dense.