Baby birth vacuum
What You Should Know About Vacuum Delivery
Written by WebMD Editorial Contributors
In this Article
- When is Vacuum Delivery Necessary?
- Risks of a Vacuum Delivery
- What to Expect During Vacuum Delivery
- What to Expect After Vacuum Delivery
A vacuum delivery, also known as a vacuum extraction, is a medical procedure that is sometimes done during vaginal childbirth. The doctor places a soft cup with a handle and vacuum pump to the baby’s head to help guide them down the birth canal. A vacuum delivery is typically done while the mother pushes during childbirth.
When is Vacuum Delivery Necessary?
During childbirth, the mother naturally tries to push their baby out through the vagina. In certain circumstances, your doctor may recommend the use of a vacuum delivery to help the process along.
The most common circumstances where a vacuum delivery is completed include:
Labor isn’t progressing. You’re pushing, but your labor isn’t progressing as expected. After a certain timeframe, your doctor may recommend using a vacuum to assist.
Your baby’s heartbeat. If your baby's heartbeat is irregular or your doctor suspects an issue, they may recommend a vacuum-assisted delivery.
You have a health concern. In these cases, your doctor may recommend a vacuum-assisted delivery. If you have certain medical conditions (especially heart conditions), your doctor may allow you to push but only for a limited amount of time.
If you’re less than 34 weeks pregnant, or in other circumstances, your doctor may advise against having a vacuum delivery. For instance, a vacuum-assisted delivery is not recommended if:
- Your baby has a medical condition that may affect their bone strength
- Your baby’s head hasn’t moved past the birth canal’s midpoint
- The position of your baby’s head is unknown
- Your baby’s shoulders, arms, buttocks, or feet are coming first down the birth canal
- Your baby, if they’re a certain size, might not be able to fit through your pelvis
Risks of a Vacuum Delivery
A vacuum delivery poses risks for both you and your baby. Potential risks for you may include:
Potential risks for you may include:
Pain in the area between your anus and vagina after delivery. This small area of tissue is very sensitive and often becomes stretched during childbirth. It’s not uncommon to have pain, but it usually gets better over time.
Vaginal tearing. During childbirth, sometimes the vagina tears. While this can be painful, the doctor can treat it with dissolvable stitches.
Short-term problems with urination. Especially after a vacuum-assisted delivery, you may experience trouble emptying your bladder fully or urinating.
Involuntary bowel movements. After vacuum-assisted delivery, you may have involuntary bowel movements and may also urinate involuntarily as well. These challenges are most often temporary.
Potential risks for your baby may include:
Wounds on their scalp. As a result of vacuum-assisted deliveries, the baby may have swelling on their scalp, giving a cone-shaped appearance. Typically the swelling goes down after a few days.
Typically the swelling goes down after a few days.
Skull fracture. The suction of the vacuum used to help during childbirth may fracture your baby’s head, but this is rare.
Bleeding inside the skull. This is a formation of blood under the skin that forms when a vein in your baby’s head has been injured. This can happen as a result of vacuum-assisted deliveries.
With vacuum delivery, there is also an increased risk of your baby’s shoulder getting stuck after the head has been delivered.
What to Expect During Vacuum Delivery
If your doctor feels you need a vacuum-assisted delivery, they will talk to you about your options, risks, and benefits of the procedure. They will also ask for your consent. After you consent, the doctor will provide you with medicine to help block the pain. This may be an epidural (pain medicine injected into the space around your spinal cord) or numbing medicine placed on the vagina.
As you lay on your back with your legs open, the doctor will place the plastic cup on your baby's head, and during the next contraction, you will be asked to push. During this same time, your doctor or midwife will use the vacuum, creating suction to help gently pull your baby. Once the doctor or midwife can see the baby's head, they will release the vacuum, and they will ask you to push your baby the rest of the way out.
During this same time, your doctor or midwife will use the vacuum, creating suction to help gently pull your baby. Once the doctor or midwife can see the baby's head, they will release the vacuum, and they will ask you to push your baby the rest of the way out.
In some cases, a vacuum delivery does not work, and your doctor will perform a c-section. A c-section is a medical surgery where your doctor cuts through your belly and uterus and gently removes your baby. This procedure can help protect the health of you and your baby, and in some cases, is safer than a vaginal birth.
What to Expect After Vacuum Delivery
Your doctor will examine your vagina and birth canal for any injuries that may have occurred during childbirth while using the vacuum. Any tears or injuries will be repaired. Your baby will also be examined to ensure they experienced no injuries during the vacuum delivery.
If you experienced a tear during childbirth, it’s normal to have some pain. Usually, the discomfort lasts only a few weeks and gradually gets better over time. If you’re not healing as expected, or are experiencing a fever or other signs of infection, contact your doctor right away.
If you’re not healing as expected, or are experiencing a fever or other signs of infection, contact your doctor right away.
Forceps or vacuum delivery - NHS
Assisted delivery
An assisted birth (also known as an instrumental delivery) is when forceps or a ventouse suction cup are used to help deliver the baby.
Ventouse and forceps are safe and only used when necessary for you and your baby. Assisted delivery is less common in women who've had a spontaneous vaginal birth before.
What happens during a ventouse or forceps delivery?
Your obstetrician or midwife should discuss with you the reasons for having an assisted birth, the choice of instrument and how it will be carried out. Your consent will be needed before the procedure can be carried out.
Find out more about consent to treatment.
You'll usually have a local anaesthetic to numb your vagina and the skin between your vagina and anus (perineum) if you have not already had an epidural.
If your obstetrician has any concerns, you may be moved to an operating theatre so a caesarean section can be carried out if needed.
It is likely a cut (episiotomy) will be needed to make the vaginal opening bigger. Any tear or cut will be repaired with stitches. Depending on the circumstances, your baby can be delivered and placed on your tummy, and your birth partner may still be able to cut the cord if they want to.
Ventouse
A ventouse (vacuum cup) is attached to the baby's head by suction. A soft or hard plastic or metal cup is attached by a tube to a suction device. The cup fits firmly on to your baby's head.
During a contraction and with the help of your pushing, the obstetrician or midwife gently pulls to help deliver your baby.
If you need an assisted birth and you are giving birth at less than 36 weeks pregnant, then forceps may be recommended over ventouse. This is because forceps are less likely to cause damage to your baby's head, which is softer at this point in your pregnancy.
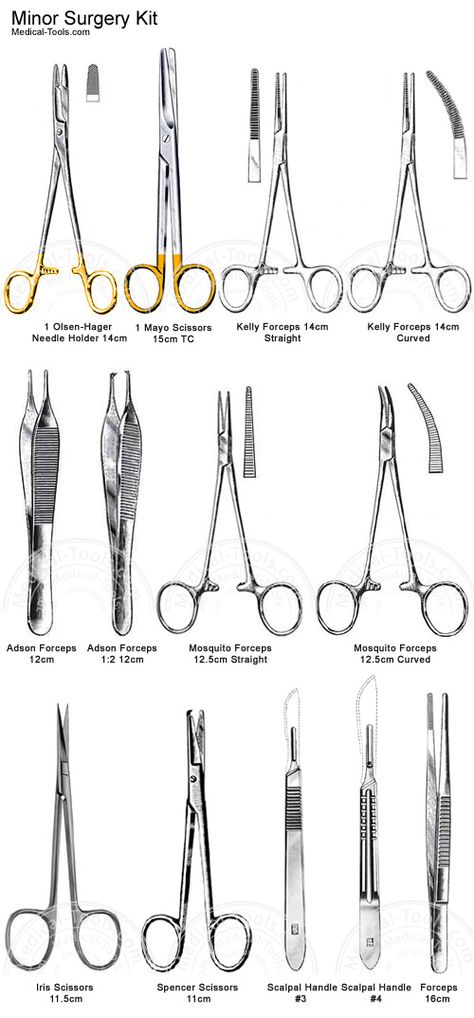
Forceps
Forceps are smooth metal instruments that look like large spoons or tongs. They're curved to fit around the baby's head. The forceps are carefully positioned around your baby's head and joined together at the handles.
With a contraction and your pushing, an obstetrician gently pulls to help deliver your baby.
There are different types of forceps. Some are specifically designed to turn the baby to the right position to be born, such as if your baby is lying facing upwards (occipito-posterior position) or to one side (occipito-lateral position).
Why might I need ventouse or forceps?
An assisted delivery is used in about 1 in 8 births, and may be needed if:
- you have been advised not to try to push out your baby because of an underlying health condition (such as having very high blood pressure)
- there are concerns about your baby's heart rate
- your baby is in an awkward position
- your baby is getting tired and there are concerns that they may be in distress
- you're having a vaginal delivery of a premature baby – forceps can help protect your baby's head from your perineum
A children's doctor (paediatrician) is usually present to check your baby's condition after the birth. After the birth you may be given antibiotics through a drip to reduce your risk of getting an infection.
After the birth you may be given antibiotics through a drip to reduce your risk of getting an infection.
What are the risks of a ventouse or forceps birth?
Ventouse and forceps are safe ways to deliver a baby, but there are some risks that should be discussed with you.
Vaginal tearing or episiotomy
This will be repaired with dissolvable stitches.
3rd or 4th degree vaginal tear
There's a higher chance of having a vaginal tear that involves the muscle or wall of the anus or rectum, known as a 3rd- or 4th-degree tear.
This kind of tear affects:
- 3 in every 100 women having a vaginal birth
- 4 in every 100 women having a ventouse delivery
- 8 to 12 in every 100 women having a forceps delivery
Higher risk of blood clots
After an assisted birth, there's a higher chance of blood clots forming in the veins in your legs or pelvis. You can help prevent this by moving around as much as you can after the birth.
You may also be advised to wear special anti-clot stockings and have injections of heparin, which makes the blood less likely to clot.
Urinary incontinence
Urinary incontinence (leaking pee) is not unusual after childbirth. It's more common after a ventouse or forceps delivery. You should be offered physiotherapy to help prevent this happening, including advice on pelvic floor exercises.
Anal incontinence
Anal incontinence (involuntary farting or leaking poo) can happen after birth, particularly if there's been a 3rd or 4th degree tear. Because there's a higher risk of these tears happening with an assisted delivery, anal incontinence is more likely.
Are there any risks to the baby?
The risks to your baby include:
- a mark on your baby's head (chignon) being made by the ventouse cup – this usually disappears within 48 hours
- a bruise on your baby's head (cephalohaematoma) – this happens to around 1 to 12 of all 100 babies during a ventouse assisted delivery – the bruise is usually nothing to worry about and should disappear with time
- marks from forceps on your baby's face – these usually disappear within 48 hours
- small cuts on your baby's face or scalp – these affect 1 in 10 babies born using assisted delivery and heal quickly
- yellowing of your baby's skin and eyes – this is known as jaundice, and should pass in a few days
Afterwards
You'll sometimes need a small tube that drains your bladder (a catheter) for up to 24 hours.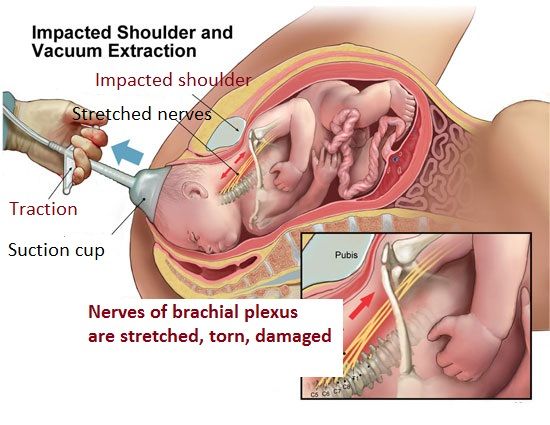
You're more likely to need this if you've had an epidural as you may not have fully regained sensation in your bladder and therefore do not know when it's full.
The Royal College of Obstretricians and Gynaecologists (RCOG) has further information about assisted delivery.
healthtalk.org has videos and written interviews of women talking about their experiences of vaginal birth, including forceps and ventouse.
Find out more about what happens in labour and pain relief in labour.
Video: what is involved in an assisted birth?
In this video, a midwife explains what an assisted birth is and what is involved.
Media last reviewed: 20 March 2020
Media review due: 20 March 2023
Page last reviewed: 9 June 2020
Next review due: 9 June 2023
Maternity department - Vacuum extraction of the fetus near the house
Vacuum extraction of the fetus is a delivery operation, extraction of the fetus by the head by creating a negative pressure between the fetal head and the inner surface of the cup of a special apparatus (vacuum extractor). In the normal course of childbirth, the absence of complications, there is no need to use it. Vacuum extraction is planned by doctors in advance, if it is impossible to remove the fetus in another way.
In the normal course of childbirth, the absence of complications, there is no need to use it. Vacuum extraction is planned by doctors in advance, if it is impossible to remove the fetus in another way.
INDICATIONS Vacuum extraction is performed in cases when the time for the CS is lost, and for the application of forceps has not yet come:
- persistent secondary weakness of labor, not amenable to drug correction;
- acute fetal hypoxia.
CONTRAINDICATIONS TO VACUUM ASPIRATION
- · all conditions that require stopping attempts: extragenital diseases and severe preeclampsia;
- · discrepancy between the size of the mother's pelvis and the size of the fetal head;
- extensor presentation;
- Premature birth.
CONDITIONS FOR OPERATION
- live fetus;
- complete opening of the uterine os;
- · the possibility of active participation of the woman in labor in the process of childbirth;
- position of the fetal head in the pelvic cavity;
- Full compliance with the size of the mother's pelvis and the size of the fetal head.

PREPARATION
Before the operation, the woman in labor must empty her bladder, the position of the woman in labor is on her back with her legs bent at the knee and hip joints. Immediately before the operation, a repeated vaginal examination is performed to assess the height of standing and insertion of the head into the pelvic cavity, the proportionality of the fetal head and the mother's pelvis, to clarify the completeness of the opening of the uterine os
TECHNIQUE
Due to the need for the active participation of the mother in labor, anesthesia is usually not performed, except in situations where epidural anesthesia has already been performed earlier in labor.
Fetal vacuum extraction operation consists of a number of successive steps:
- · introduction of the vacuum extractor cup and placing it on the fetal head;
- creation of negative pressure between the fetal head and the inner surface of the vacuum extractor cup;
- fetal retrieval traction;
- · Removing the cup of the vacuum extractor from the fetal head by gradually reducing the negative pressure.
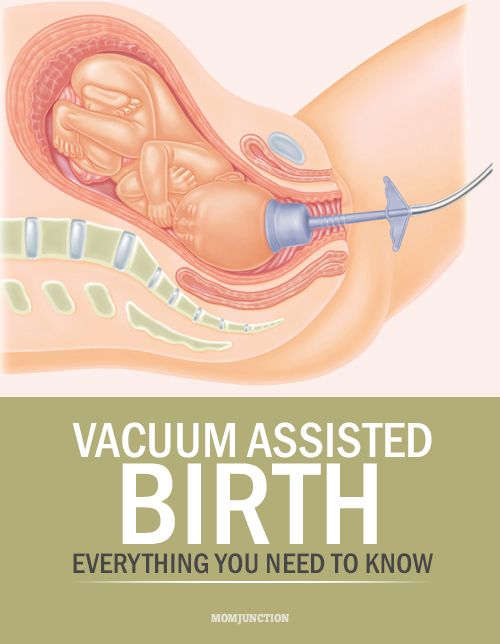
Each stage of the operation has its own characteristics. So, for example, the vacuum extractor cup can be inserted under manual control or when the fetal head is exposed in the mirrors. After inserting the cup into the vagina, it is placed on the head of the fetus as close as possible to the small fontanel, bypassing the large fontanel, and carefully pressed.
The position of the calyx must correspond to the “mid point of flexion”, i.e. its lateral edges should be located symmetrically on both sides of the sagittal suture, and the posterior edge should be 1–3 cm anterior to the small fontanel.
Then a vacuum apparatus is attached to the cup and gradually, over 2-3 minutes, a negative pressure is created in the system, guided by the pressure gauge readings. The initial pressure is approximately 100 mm Hg, it is necessary to make sure that the tissues of the soft birth canal do not get between the calyx and the head of the fetus, after which the pressure is adjusted to 500–600 mm Hg. and start traction.
and start traction.
The direction of traction depends on the position of the fetal head in the small pelvis and should mimic its natural progression through the birth canal. Usually they are carried out in the direction down, towards themselves and up (the obstetrician's feet are the plane of the wide part of the pelvic cavity, the chest is the narrow part of the pelvic cavity, the face is the pelvic exit plane). Traction is carried out synchronously with labor, stopping in between contractions.
Episiotomy is recommended to be avoided, as the resistance of the soft tissues of the perineum provides additional fixation of the cup of the vacuum extractor and contributes to a more natural process of passage of the fetal head through the birth canal due to its flexion and rotation.
The cup of the vacuum extractor is removed after the eruption of the parietal tubercles, gradually reducing the vacuum in the apparatus, and the head is removed using the usual manual manual delivery.
Although an increased risk of intracranial hemorrhage in newborns during vacuum extraction of the fetus has not been proven, careful monitoring of the condition of the child in the early neonatal period is necessary, if indicated, neurosonography is performed.
COMPLICATIONS OF VACUUM ASPIRATION
The following complications may occur:
· slippage of the vacuum extractor cup;
lack of advancement of the fetal head;
· fetal trauma: cephalohematoma, CNS damage of varying severity;
damage to the tissues of the mother's soft birth canal.
If the cup of the vacuum extractor again slips off the fetal head or if the head does not advance
, the operation is stopped and other methods are switched to
delivery.
Trauma to the mother and fetus during the operation of vacuum extraction, as a rule,
occur due to technical errors in the operation or untimely
its performance.
Vacuum extraction
- Material information
Vacuum extraction is a delivery operation in which the fetus is artificially removed through the natural birth canal using a special device - a vacuum extractor.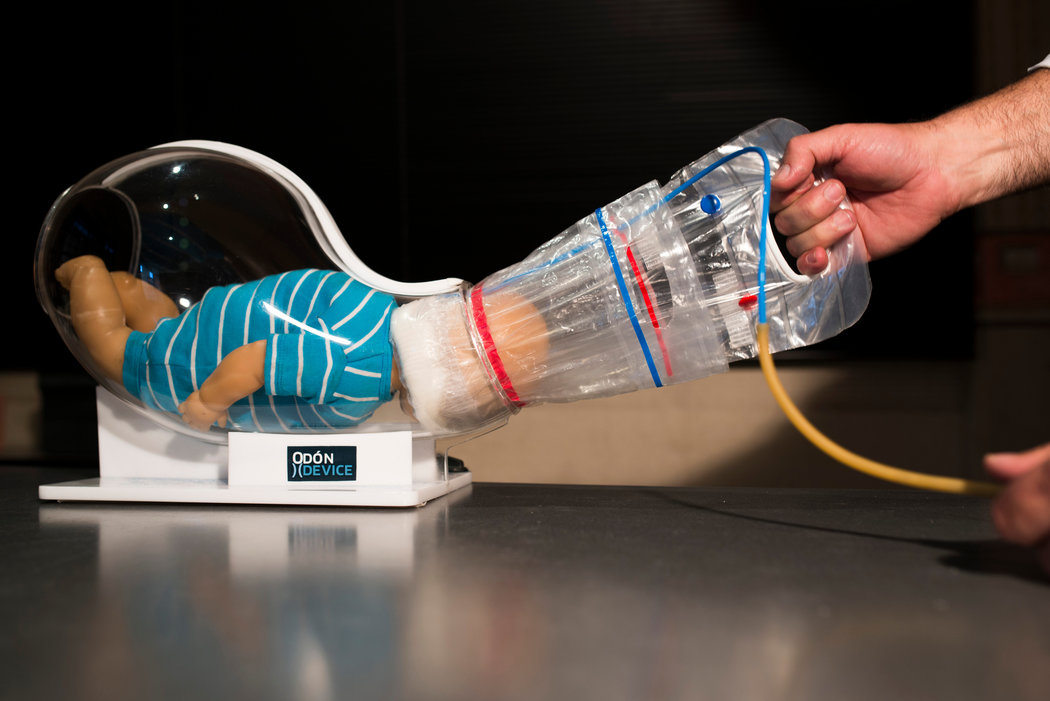 The first attempts to use vacuum to extract the fetus through the natural birth canal were made in the middle of 19century. In the second half of the 20th century, the Malström vacuum extractor developed in 1956 became widespread.
The first attempts to use vacuum to extract the fetus through the natural birth canal were made in the middle of 19century. In the second half of the 20th century, the Malström vacuum extractor developed in 1956 became widespread.
The main elements of the apparatus for vacuum extraction are: a sealed buffer container and an associated pressure gauge, manual suction to create negative pressure, a set of applicators (in the Maelstrom model - a set of metal cups from 4 to 7 numbers with a diameter of 15 to 80 mm) . The principle of operation of the device is to create a negative pressure between the inner surface of the cups and the head of the fetus. Vacuum extraction of the fetus is of limited use due to adverse effects on the fetus. Vacuum extraction is used only in cases where there are no conditions for performing other delivery operations.
Indications for vacuum extraction are weakness of labor activity, which started fetal asphyxia. Vacuum extraction is contraindicated in severe forms of preeclampsia, decompensated heart defects, high myopia, hypertension, since during vacuum extraction of the fetus, active laboring activity of the woman in labor is required; with a discrepancy between the size of the fetal head and the mother's pelvis; with extensor presentation of the fetal head; with prematurity of the fetus (less than 36 weeks). The last two contraindications are related to the peculiarity of the physical action of the vacuum extractor. Placement of cups on the head of a premature fetus or in the region of a large fontanel is fraught with serious complications. The conditions for the operation are: full opening of the uterine os; absence of a fetal bladder; matching the size of the pelvis of the mother and the head of the fetus. The fetal head should be in the pelvic cavity with a large segment at the entrance to the small pelvis.
The procedure for vacuum extraction of the fetus is as follows. First, the cup is inserted into the vagina with the side surface. Then it is turned and the working surface is pressed against the head of the fetus, as close as possible to the small fontanel. The cup is attached to the apparatus and negative pressure up to 0.7-0.8 atmospheres (500 mm Hg) is created within 3-4 minutes. Extraction of the fetus by the head is performed synchronously with attempts in the direction corresponding to the biomechanism of childbirth.