Red bumps in children
Nappy rash - NHS
Around 1 in 4 babies and toddlers in nappies have nappy rash at any one time. It doesn't usually develop in newborns, but all babies can get nappy rash.
Nappy rash can be caused by:
- your baby's skin being in contact with wee or poo for a long time
- the nappy rubbing against your baby's skin
- not cleaning the nappy area or changing the nappy often enough
- soap, detergent or bubble bath
- alcohol-based baby wipes
- some types of medicines, such as antibiotics or laxatives (used to make a baby poo more often)
There may be red patches on your baby's bottom, or the whole area may be red. Their skin may look sore and feel hot to touch, and there may be spots, pimples or blisters.
Most babies with mild nappy rash don't feel sore, but if the rash is severe your baby may feel uncomfortable and be distressed.
If your baby gets nappy rash, you can usually treat their skin yourself.
If the rash isn't upsetting your baby, at each nappy change apply a thin layer of a barrier cream to protect their skin. Ask your health visitor or pharmacist to recommend one.
Follow this advice to help look after your baby's skin.
- Change wet or dirty nappies as soon as possible.
- Clean the whole nappy area gently but thoroughly, wiping from front to back. Use water or fragrance-free and alcohol-free baby wipes. Read more about how to clean your baby and change your baby's nappy.
- Bath your baby daily – but avoid bathing them more than twice a day as that may dry out their skin.
- Dry your baby gently after washing them – avoid vigorous rubbing.

- Lie your baby on a towel and leave their nappy off for as long and as often as you can to let fresh air get to their skin.
- Do not use soap, bubble bath, or lotions.
- Do not use talcum powder as it contains ingredients that could irritate your baby's skin.
- Make sure your baby’s nappy fits properly. If it is too tight then it can irritate the skin and if it is too loose, then the nappy will not be able to soak up pee properly.
Nappy rash usually clears up after about 3 days if you follow this advice. You should keep following this advice as this will help prevent nappy rash from coming back.
If the rash is causing your baby discomfort, your health visitor or pharmacist can recommend a nappy rash cream to treat it.
You should apply the cream first and wait a few minutes before you apply the barrier cream.
If the rash doesn't go away or your baby develops a persistent bright red, moist rash with white or red pimples that spreads into the folds of their skin, they may have an infection.
Ask a pharmacist or health visitor for advice. The pharmacist may recommend a cream for you to use.
If the rash is severe, take your baby to the GP who may prescribe cream or medicine. Follow a GP's instructions on whether and when to apply barrier cream as well as the prescribed cream.
It's normal for babies to develop skin rashes, but it's important to know the difference between a minor irritation and a condition that requires attention.
Read more about rashes in babies and children.
Page last reviewed: 17 September 2021
Next review due: 17 September 2024
Slapped cheek syndrome - NHS
Slapped cheek syndrome (also called fifth disease) is common in children and should get better on its own within 3 weeks. It's rarer in adults, but can be more serious.
It's rarer in adults, but can be more serious.
Check if it's slapped cheek syndrome
The first sign of slapped cheek syndrome is usually feeling unwell for a few days.
Symptoms may include:
- a high temperature
- a runny nose and sore throat
- a headache
Credit:
SCIENCE PHOTO LIBRARY https://www.sciencephoto.com/media/550792/view
A few days later, a spotty rash may appear on the chest, arms and legs. The rash can be raised and itchy. It may be harder to see on brown and black skin.Credit:
John Kaprielian/SCIENCE PHOTO LIBRARY https://www. sciencephoto.com/media/618192/view
sciencephoto.com/media/618192/view
How long it lasts
The cheek rash usually fades within 2 weeks.
The body rash also fades within 2 weeks, but sometimes lasts for up to a month, especially if you're exercising, hot, anxious or stressed.
Adults might also have joint pain and stiffness. This can happen in children too, but it's rare. Joint pain can continue for many weeks, even after the other symptoms have gone.
If you're not sure your child has slapped cheek syndrome
Look at other rashes in babies and children.
Things you can do yourself
You do not usually need to see a GP for slapped cheek syndrome.
There are some things you can do to ease the symptoms.
Do
-
rest
-
drink plenty of fluids to avoid dehydration – babies should continue their normal feeds
-
take paracetamol or ibuprofen for a high temperature, headaches or joint pain
-
use moisturiser on itchy skin
-
speak to a pharmacist about itchy skin – they can recommend the best antihistamine for children
Important: Important
Tell your midwife or a GP if you're pregnant or have a weakened immune system and have been near someone with slapped cheek syndrome.
Non-urgent advice: See a GP if:
you think you have slapped cheek syndrome and:
- you're pregnant – there's a very small risk of miscarriage or other complications
- you have a blood disorder, such as sickle cell disease or thalassaemia – there's a risk of severe anaemia
- you have a weakened immune system – for example, because of chemotherapy or diabetes
Ask for an urgent appointment if you have:
- very pale skin
- shortness of breath
- extreme tiredness
- fainting
These can be signs of severe anaemia and you might be sent to hospital for a blood transfusion.
How slapped cheek syndrome is spread
It's hard to avoid spreading slapped cheek syndrome because most people do not know they have it until they get the rash.
You can only spread it to other people before the rash appears.
Slapped cheek syndrome is caused by a virus (parvovirus B19). The virus spreads to other people, surfaces or objects by coughing or sneezing near them.
To reduce the risk of spreading the virus:
- wash your hands often with water and soap
- use tissues to trap germs when you cough or sneeze
- bin used tissues as quickly as possible
Information:
You do not have to stay off work or school after the rash appears.
Let the school or teacher know if your child has slapped cheek syndrome.
Page last reviewed: 18 February 2021
Next review due: 18 February 2024
Rash in a child on the body, legs, back
We treat children according to the principles of evidence-based medicine: we choose only those diagnostic and treatment methods that have proven their effectiveness. We will never prescribe unnecessary examinations and medicines!
We will never prescribe unnecessary examinations and medicines!
Make an appointment via WhatsApp
Prices Doctors
The first children's clinic of evidence-based medicine in Moscow
No unnecessary examinations and medicines! We will prescribe only what has proven effective and will help your child.
Treatment according to world standards
We treat children with the same quality as in the best medical centers in the world.
The best team of doctors in Fantasy!
Pediatricians and subspecialists Fantasy - highly experienced doctors, members of professional societies. Doctors constantly improve their qualifications, undergo internships abroad.
Ultimate treatment safety
We made pediatric medicine safe! All our staff work according to the strictest international standards JCI
We have fun, like visiting best friends
Game room, cheerful animator, gifts after the reception. We try to make friends with the child and do everything to make the little patient feel comfortable with us.
You can make an appointment by calling or by filling out the form on the site
Other Pediatric services
- Pediatrician's consultation
- Child Health Management Program
Frequent calls
- Acute bronchiolitis in children: diagnosis and treatment
- SARS
- Angina streptococcal tonsillitis
- Frequently ill child
- Intestinal infections
- Pneumonia (pneumonia) in children
- Colic
- Feeding problems
- Prolonged cough in a child: diagnosis and treatment
- Acute bronchitis in children: diagnosis and treatment
- Pneumonia (pneumonia) in children: diagnosis and treatment
- False croup in a child
- Coxsackie virus in a child
- The child was bitten by a tick! What to do?
Online payment
Documents online
Online services
Red pimples on the face of a newborn: symptoms, causes and treatment
Allergic rash in a newborn
An allergy in a baby is an unfavorable immune response of a child's body to a potentially dangerous substance. Most often, an allergic rash occurs against the background of the use by a nursing mother of products that can act as an irritant. This group includes:
Most often, an allergic rash occurs against the background of the use by a nursing mother of products that can act as an irritant. This group includes:
- cow's milk;
- soy [1] and egg white;
- fish;
- strawberry;
- nuts.
The first sign of developing allergic rash is peeling. Pathological foci with dry skin on the face of a newborn are formed symmetrically, localized on the cheeks and on the forehead.
It is necessary to consult a doctor if the appearance of rashes affects the general condition of the baby. Irritability, restless sleep, disorders of the gastrointestinal tract, fever and vomiting are dangerous symptoms that should be stopped immediately under the supervision of a pediatrician.
Neonatal acne
Neonatal acne may appear in the first weeks of a child's life on the forehead, nose and cheeks. In appearance, they resemble acne with purulent heads, characteristic of a teenage rash. It is assumed that the cause of the appearance of acne is increased production of sebum, which clogs the ducts of the sebaceous glands and provokes an inflammatory reaction.
It is assumed that the cause of the appearance of acne is increased production of sebum, which clogs the ducts of the sebaceous glands and provokes an inflammatory reaction.
The pathogenesis of the appearance of small pimples in newborns is also associated with the processes of the formation of the hormonal system. The body gets rid of the transplacental influence of maternal androgens [2], adrenal hormones begin to be produced more intensively, which affect the condition of the skin.
Neonatal acne does not require treatment [9] - standard daily care using delicate soap or baby cosmetics is sufficient. In most cases, pimples that appear on the face go away on their own by 4 months of age.
Sweating
Sweating is a skin lesion that is associated with hyperfunction of the sweat glands and irritation of the excretory ducts . The disease can develop due to improper skin care newborn, with a long stay in hot rooms and the wrong choice of clothing (the child is heavily wrapped up).
Miliaria resembles an allergic rash, but differs from it in localization. Signs of allergy most often appear on the skin of the child's face, and with miliaria, rashes form throughout the body - most often in natural folds, on the neck, lower abdomen and upper chest.
What prickly heat looks like:
- small blisters with clear contents, prone to burning and itching;
- in difficult cases, reddish nodules with an inflamed rim;
- with extensive skin lesions - weeping areas.
Prickly heat in itself is not dangerous for the health of the child. But damage to the skin is fraught with the addition of a bacterial or fungal infection. In this case, purulent processes develop, the skin becomes edematous, a putrid odor appears. Red pimples with prickly heat cause discomfort in the child - he becomes capricious and irritable, refuses to eat and sleeps poorly.
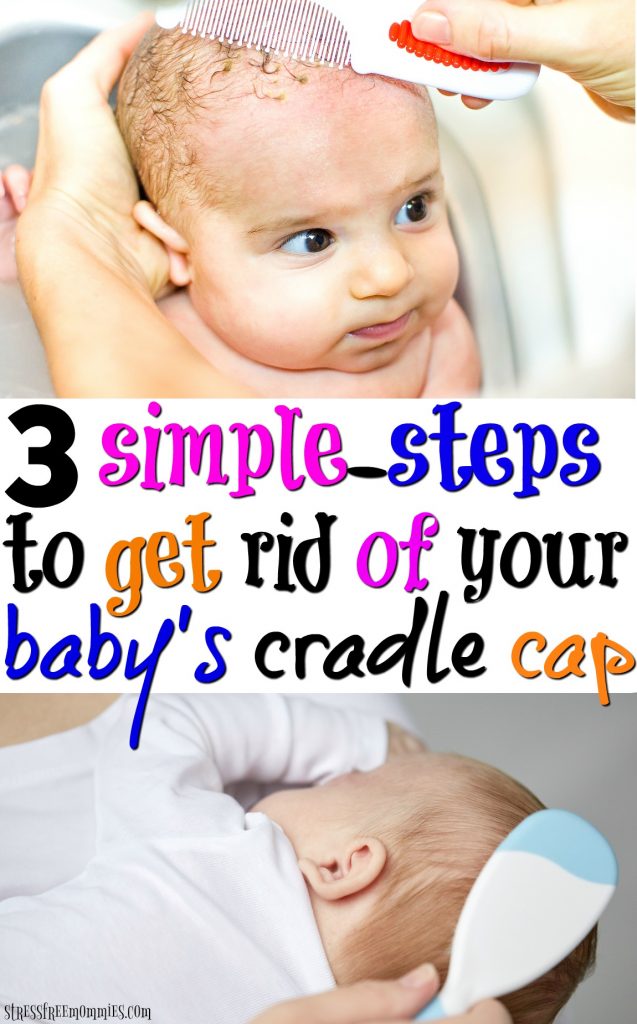
Seborrheic dermatitis
In addition to red pimples, yellowish scales may appear on the skin of a newborn. These are signs of seborrheic dermatitis, a disease associated with increased secretion of sebum. Scales are formed in the first month of life in areas of the body with a large accumulation of sebaceous glands - on the scalp, upper third of the back, on the face, chest and in the area of the auricles. Seborrheic dermatitis is sometimes called “milky crusts”, which may be associated with the use of inappropriate cosmetic products for baby skin care.
These are signs of seborrheic dermatitis, a disease associated with increased secretion of sebum. Scales are formed in the first month of life in areas of the body with a large accumulation of sebaceous glands - on the scalp, upper third of the back, on the face, chest and in the area of the auricles. Seborrheic dermatitis is sometimes called “milky crusts”, which may be associated with the use of inappropriate cosmetic products for baby skin care.
In fact, the disease is caused by high levels of maternal hormones in the blood or changes in the biochemical composition of lipids on the surface of the skin [4].
Most childhood seborrheic dermatitis resolves on its own. Parents need only to take care of proper care , but diligent removal of crusts is not recommended - you risk damaging delicate skin and causing infection. It is better to use specially designed products - such as Shampoo-foam from "milk crusts" for newborns. He facilitates the removal of scales in 90% of cases and soothes the scalp in 95% of babies [5.2]. The product contains 99% ingredients of natural origin. The shampoo is fragrance-free and has a tear-free formula.
He facilitates the removal of scales in 90% of cases and soothes the scalp in 95% of babies [5.2]. The product contains 99% ingredients of natural origin. The shampoo is fragrance-free and has a tear-free formula.
In the presence of thick, dense scales, which are located not only on the scalp, but also in other areas, a good helper will be Milk crust cream which helps to completely remove milk crusts in an average of 7 days [5.3].
Atopic dermatitis
Atopic dermatitis is an allergic disease that is accompanied by chronic inflammation of the skin. Causes of uncontrolled allergic reactions in infants are:
- food allergens - animal protein, soy products, some types of vegetables;
- airborne allergens - household dust, pollen, pet hair, tobacco smoke, etc.;
- pathogenic microflora - fungi, viruses, bacteria.

Newborns are most often diagnosed with erythematous-squamous form of atopic dermatitis with signs of an acute inflammatory reaction:
- hyperemia of the skin;
- peeling;
- flat small papules.
Red spots are localized on the arms and legs in the area of the folds , on the sides of the neck, on the back of the hands and on the cheeks.
Children with atopic dermatitis are advised to regularly cleanse and moisturize their skin [6]. Anti-inflammatory drugs are prescribed only for extensive skin lesions that impair the quality of life of the baby - in this case, you should contact your pediatrician.
For daily care it is recommended to use STELATOPIA Emollient Cream . Studies [5.1] have shown that emollient:
- In 90% of cases reduces increased dryness of the skin [5.1] and reduces the likelihood of clinical signs of AD by 51% [10]
- Soothes itching in 91% of cases [5.
 1]
1] - Reduces inflammation after 32 hours [11]
Diaper dermatitis
This disease is better known as diaper rash and is accompanied by inflammation of the skin in the diaper area zone in infants. The rash appears as a result of prolonged contact of the body with wet diapers - the skin becomes excessively moist and defenseless against damaging factors (chemical, physical, infectious). The situation is aggravated by the simultaneous effect on the skin of children's feces that remain in a diaper or diaper.
Diaper dermatitis is not localized on the face - pimples in newborns appear on the lower abdomen, on the convex surfaces of the thighs and buttocks.
For non-drug treatment of pathology, air baths [7], bathing in a decoction of string and celandine [8], and thorough hygiene procedures are indicated. For the prevention of diaper dermatitis and redness, it is recommended to use Diaper Cream 1 2 3.
Useful properties of the product:
- reduces redness and irritation by 80% from the first application [5];
- does not interfere with skin breathing;
- reduces the risk of exacerbations by 74% [5];
- protects, repairs and soothes inflamed skin.
A number of dermatological diseases of newborns develop as a result of improper care, so parents should pay special attention to children's hygiene, and if the baby's condition worsens, immediately consult a doctor.
____________________________________________________________________________________________
Literature:
1. Bhatia J, Greer F, for the Committee on Nutrition of the American Academy of Pediatrics. The use of mixtures based on soy protein in infant feeding.// Pediatrics, 2008; 121:1062–1068.
2. Herani M.I., Ando I. Acne in infancy and acne genetics // Dermatology 2003. Volume 206. Number 1. pp. 24-28. DOI: 10.1159/000067819
3.